Abstract
Abnormal bone metabolism is an integral part of the chronic kidney disease-mineral bone disorder (CKD-MBD). For several reasons, the difficult bone compartment was neglected for some time, but there has been renewed interest as a result of the conception of bone as a new endocrine organ, the increasing recognition of the cross-talk between bone and vessels, and, especially, the very high risk of osteoporotic fractures (and associated mortality) demonstrated in patients with CKD. Therefore, it has been acknowledged in different guidelines that action is needed in respect of fracture risk assessment and the diagnosis and treatment of osteoporosis in the context of CKD and CKD-MBD, even beyond renal osteodystrophy. These updated guidelines clearly underline the need to improve a non-invasive approach to these bone disorders in order to guide treatment decisions aimed at not only controlling CKD-MBD but also decreasing the risk of fracture. In this report, we review the current role of the most often clinically used or promising biochemical circulating biomarkers such as parathyroid hormone, alkaline phosphatases, and other biochemical markers of bone activity as alternatives to some aspects of bone histomorphometry. We also mention the potential role of classic and new imaging techniques for CKD patients. Information on many aspects is still scarce and heterogeneous, but many of us consider that it is indeed time for action, recognizing our definitely limited ability to base certain treatment decisions only on our current non-comprehensive knowledge.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Abnormal bone metabolism is an integral part of the chronic kidney disease-mineral bone disorder (CKD-MBD) “syndrome” [1, 2]. Nevertheless, the bone compartment was neglected for a certain period because of the difficulty of performing and analyzing transiliac tetracycline double-labeled bone biopsies, considered the gold standard for the diagnosis and classification of the different forms of renal osteodystrophy (ROD) [3, 4]. The term ROD was coined in 1942 by Liu and Chu [5], 61 years after an association was identified between “late rickets and albuminuria” [6], 30 years after the first definite recognition of the etiologic connection between CKD and “renal rickets” [7], and 11 years following the suggestion that parathyroid gland hyperplasia occurs secondary to advanced CKD [8]. ROD was used as “the generic name to include cases of osseous disorder associated with renal insufficiency, while the exact nature of the pathologic process in the skeleton is still undetermined,” and the usage of the term remained until the relatively recent recommendation that it should be used exclusively to define the bone pathology associated with CKD [9].
Bones protect and support vital organs and work with joints and muscles to help movement, a fundamental function of life on Earth. In addition, bone stores minerals, and bone marrow is the primary site of hematopoiesis. There has also been renewed interest in the bone compartment as a result of the conception of bone as a new endocrine organ “at the heart” of CKD-MBD [10] and the increasing recognition of the cross-talk between bone and vessels and of the intertwining between bone with inflammation. Thus, investigations have aimed to discover possible pathogenic links with increased and accelerated cardiovascular burden and aging (now nicknamed inflammaging) in both the general population and patients with CKD [11,12,13]. Moreover, it has been acknowledged that action is needed in respect of fracture risk assessment and the diagnosis and treatment of osteoporosis in the context of CKD and CKD-MBD [14,15,16,17,18,19,20], including advanced stages of CKD as endorsed by several European working groups in the just released European Consensus Statement on the diagnosis and management of osteoporosis in CKD stages G4–G5D [20]. Since CKD is a state of accelerated aging, primary osteoporosis may also play a more prominent role in bone fragility than previously recognized and may eventually overcome the impact of ROD itself [20]. In fact, the recent 2017 Kidney Disease Improving Global Outcomes (KDIGO) clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of CKD-MBD [1] had already recognized that (a) patients with CKD G3a-G5D have increased fractures rates and associated mortality compared with the general population [1, 21]; (b) as reported in post-hoc analyses, osteoporosis medications have a similar efficacy in improving bone mineral density (BMD) and reducing fracture incidence, at least in individuals with a moderately reduced estimated glomerular filtration rate (eGFR) compared with those with mildly decreased or normal eGFR [1, 20,21,22,23,24,25,26]; and (c) inability to perform a bone biopsy may not justify withholding antiresorptive therapy from patients at high risk of fracture [1, 14, 16, 18, 20]. Hence, the guidelines clearly underline the need for a non-invasive approach to bone disorders in patients with CKD in order to guide treatment decisions, which should be aimed at not only controlling CKD-MBD but also decreasing the risk of fracture.
Many available treatments for ROD and/or osteoporosis [e.g., antiparathyroid drugs (vitamin D derivatives and/or calcimimetics), bisphosphonates, denosumab, teriparatide] target bone turnover (a dynamic biological process indicating cellular activity), with bone volume and strength being a net resultant of the intervention on the dynamics of bone cells [27]. However, their real effect in preventing fractures in CKD patients is not yet well known since the etiology of fractures in CKD is multifactorial and fractures are not fully explained by reduced BMD or histomorphometry findings alone. Moreover, transiliac bone biopsy analyzes trabecular bone, is not straightforward, and is subject to limitations that can impact on clinical diagnosis and decision making [3, 27]. In fact, the non-evaluated cortical bone thickness and porosity are equally important in determining fracture risk. It also has to be taken into account that bone biopsy provides information only at a single time point and consequently does not allow easy longitudinal monitoring of changes in bone turnover or morphology because the performance of serial biopsies in individual patients is not clinically practical. For all these reasons, in this report, we review the current role of the most often clinically used or promising biochemical circulating markers as alternatives to some aspects of bone histomorphometry, as well as briefly mentioning the potential role of new imaging techniques.
Bone Biomarkers
Several biomarkers of ROD (including biomarkers of bone turnover and/or bone remodeling regulators) are being regularly used in clinical practice, but some are employed solely in clinical research. Although these biomarkers are easy to measure and reflect changes in bone turnover more rapidly than changes with other tests, certain common limitations should be kept in mind. The most important is that to date, a causal role in the pathogenesis of ROD (necessary in order for the biomarker to qualify as a treatment target) has been established only for parathyroid hormone (PTH). Moreover, the clinical relevance of the different bone biomarkers in terms of their predictive power in respect of incident clinical events (e.g., future fractures, cardiovascular events, or death), varies greatly among different cohorts (e.g., CKD stages 3 vs CKD 4–5D), and further limitations include the scarcity of available data and the inherent variability of assays. The distinct prevalence of low- vs non-low vs normal- or high-turnover bone disease which depends on many demographic factors (e.g., age, diabetes prevalence, and ethnicity) definitely contributes to the lack of homogeneity. Optimal targets are commonly disputed, especially in patients with CKD, and this issue is further complicated by the diminished renal clearance of some biomarkers or their altered metabolism, which thereby no longer reflects their production rate. Interestingly, some of the bone biomarkers used as a proxy to establish the type, and severity of ROD are not specific to metabolic processes in bone tissue alone, but can also be expressed in cells of cardiovascular tissues or reflect non-primary bone diseases [20, 27, 28], thus occasionally lacking tissue specificity [20]. Finally, since bone markers may differ in their origin and function, the absence of a clear correlation among biomarkers may be expected even if they reflect the same general biological process in bone [27].
Parathyroid Hormone, Alkaline Phosphatases, and Bone Turnover
Both PTH [second-generation intact (iPTH) or third-generation “whole” 1–84 PTH (BioPTH)] and alkaline phosphatases [(APs), total (tAP), or bone-specific alkaline phosphatase (BSAP)] have classically been associated with bone formation and regarded as reliable markers of bone turnover in CKD [28,29,30]. AP levels, unlike iPTH levels, are not affected by renal function [30], but in the mid-1990s and early 2000s, tAP fell out of favor when commercial PTH assays became available and the Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines on CKD-MBD chose not to mention APs because target ranges were uncertain [31]. Moreover, at the time, it was felt that PTH is the main regulator of bone remodeling. However, the currently available BSAP is generally considered more sensitive and specific for bone disease [32], especially given the interference of liver isoenzymes in the measurement of tAP. Moreover, BSAP seemed better than both iPTH and tAP in distinguishing between the clinical situations of normal/low-turnover bone disease and high-turnover bone disease in dialysis patients [29]. Accordingly, BSAP was found to show a better correlation with bone turnover (histomorphometrically determined) than tAP, and outperformed iPTH in detecting high-turnover bone disease [29]. It has been reported that BSAP ≥ 20 ng/ml, alone or combined with iPTH ≥ 200 pg/ml, has the highest sensitivity, specificity, and predictive values for the diagnosis of high-turnover bone disease and allows the exclusion of normal- or low-turnover bone disease [30, 32,33,34]. On the other hand, several observations have suggested that low-turnover bone disease should be suspected when iPTH levels are less than 150 pg/ml or when BSAP levels are lower than 27 U/L [29, 33]. As mentioned above, the KDOQI guidelines chose not to mention the uncertain target values for tAP [31], and in the recent 2017 KDIGO guidelines, different predictive values have been described for iPTH according to the different cut-off values employed (i.e., KDOQI 150–300 pg/ml or KDIGO 2X-9X the upper limit of normal for assay, respectively) [1, 30, 31]. It is of note that a high-risk cut-off for tAP (> 120 U/L) has frequently been reported [32, 35]. More specifically, Coen et al. reported that a BSAP < 12.9 ng/ml has a sensitivity of 100%, a specificity of 94%, and a positive predictive value of 72% in the prediction of low-turnover bone disease [36]. In the more recent BONAFIDE prospective study of hemodialysis patients who were treated with calcimimetics (inclusion criteria: PTH ≥ 300 pg/ml, BSAP > 20.9 ng/ml, and calcium > 8.4 mg/dl), no basal adynamic bone disease (ABD) was detected, and most subjects had either mild or severe hyperparathyroid bone disease, with only 10.4% of patients having mixed lesions [37].
On the other hand, in an important KDIGO-led multinational cross-sectional retrospective diagnostic study of biomarkers (all run in a single laboratory but without consideration of therapy) and bone biopsies, the authors combined databases from four countries including 492 dialysis patients [38]. In this study, the best BSAP cut-off value for discrimination of low- from non-low turnover bone disease was found to be 33.1 U/L, while that for the discrimination of high- from non-high-turnover bone disease was 42.1 U/L [38]. Using iPTH (Roche assay, upper limit of normal = 65 pg/ml), the best cut-off value for discrimination of low- from non-low turnover bone disease was < 103.8 pg/mL, and that for the discrimination of high- from non-high turnover bone disease was > 323.0 pg/mL [38]. However, although biomarkers such as iPTH and BSAP or combinations thereof allowed discrimination of low- from non-low and high- from non-high turnover bone disease, the area under the receiver operating characteristic (AUROC) curves was > 0.70 but < 0.80. The authors also found BSAP to be only slightly better than iPTH for diagnosing low- vs non-low-turnover bone disease (AUROC = 0.757 vs 0.701, respectively), while no difference was noted in respect of high- vs non-high-turnover bone disease (AUROC = 0.724 vs 0.711, respectively). In contrast with previous studies, the combination of iPTH and BSAP did not significantly increase the AUROC curve in any differential diagnosis (AUROC = 0.718). Thus, addition of AP or BSAP measurements to iPTH results has not always been shown to improve diagnostic accuracy [38, 39]. Actually, AP can reflect not only osteoblastic activity in bone but also osteoblast-like cell activity in vascular smooth muscle, whereas iPTH is only indirectly associated with bone formation (as a secondary impact) and represents parathyroid activity at a certain time point much better than it represents bone dynamics [34]. Moreover, distinct from most other turnover markers or regulators, PTH secretion is not dictated by local demand in bone, as is the case for several other biomarkers which are triggered by osteocytes via mechanical stimuli [40].
In any case, some authors have recently underlined a lower variability for serum BSAP and consider that it may thus be better suited for the diagnosis, prognosis, and longitudinal follow-up of bone turnover [32, 41, 42]. Furthermore, all these data on BSAP, as well as the other biomarkers, can still be very useful because the positive predictive value for low-turnover bone disease can easily be increased by applying a lower cut-off value (e.g., BSAP ≪ 33.1 U/L) while, conversely, that for high-turnover bone disease can be improved by applying a higher value (e.g., BSAP > 42.1 U/L) [27, 35].
Several circulating human BSAP isoforms have also been described (including the recently reported B1x, which seems to circulate only in the serum of patients with CKD G4-G5 and not in normal subjects) [43]. This B1x isoform was the only biochemical parameter that correlated inversely with histomorphometric parameters of osteoblastic number and activity, and whose AUROC curves showed that it could be used for the diagnosis of low-turnover bone disease (AUROC = 0.83) [42]. The clinical utility of different APs, their role in the process of vascular calcification and cardiovascular disease, their association with BMD/hip fractures, their linear association with survival in CKD patients, and their role as a potential novel and independent target for treatment are beyond the scope of this review, but interested readers are encouraged to consult recent publications [28, 32, 34, 44, 45].
In summary, although serum PTH levels mainly reflect the degree of parathyroid gland function, serial PTH measurements either alone or in combination with BSAP still remains the best surrogate biomarker of bone turnover in CKD patients. BSAP improves the performances of PTH for the diagnosis of low- vs high-bone turnover but recent results have disputed the best cut-off values.
Parathyroid Hormone and Alkaline Phosphatases in Guidelines
Finally, it is necessary to mention that the correlation between serum iPTH and “whole” PTH as measured by a central laboratory is very strong (r = 927; 95% confidence interval 0.897–0.950) [38]. Guidelines only recommend monitoring serum levels of calcium, phosphate, PTH, and AP activity beginning in CKD G3a in adults (Guideline 3.1.1, evidence grade 1C), whereas in children, it is suggested that monitoring is begun in CKD G2 (evidence grade 2D) [1]. No further specification is made about the type of PTH and/or AP with the exception of Guideline 3.2.3 (Table 1). In today’s clinical practice, second-generation iPTH assays are the most widely used. The KDOQI guidelines [31] recommended the “classical” 150–300 pg/ml as the desirable iPTH concentration in CKD G5D patients, based on measurements using the old iPTH Nichols® Allegro immunoradiometric assay. However, this assay is no longer commercially available, and many recent studies report a very significant variability between the currently available “generic” iPTH kits and the Nichols® Allegro assay, as well as among the “generic” iPTH assays themselves [46]. Nevertheless, iPTH levels in this range have also been associated with improved survival [47, 48]. Importantly, comparison of bone histologic changes at similar levels of PTH has shown over- or underestimation of bone turnover with the use of current iPTH assays. Moreover, a significant number of patients had histologic signs of low-turnover bone disease while having serum iPTH levels above the classical 300 pg/ml. This is why the 2009 and 2017 KDIGO guidelines suggest the use of values “X” times normal (e.g., 2X–9X for CKD G5D patients), instead of absolute values [1]. These “more extreme” values obviously not only improve the predictive value of bone findings but they are also associated with increased mortality; therefore, they are considered to represent “extremes of risk” [1]. In order to increase the predictive value of PTH measurements for bone turnover, results from the PTH 1–84 assay (“whole” PTH) have been published, but the available data do not allow one to conclude that there have been substantial improvements [42]. Calculation of a PTH ratio between the level of PTH 1–84 and the level of carboxy-terminal PTH fragments has also been reported to be of potential value [49]. Levels of carboxy-terminal fragments are calculated by subtracting the measured value of “whole” PTH 1–84 from the iPTH level. It has been reported that this PTH ratio may improve the assessment of bone turnover [39] and may be helpful in diagnosing both low and high bone turnover, at least in black CKD G5D patients, whereas it aids only in the diagnosis of low bone turnover in CKD G5D whites [49]. A racial distinction between the bone phenotype and iPTH had been described previously, with low-turnover bone disease being more prevalent in Afro-American dialysis patients for the same value of PTH [50, 51]. Only limited clinically relevant data are as yet available on the newly described oxidized PTH [52].
In summary, measuring PTH and paying adequate attention to a marker that is truly of bone source makes sense [34], especially considering the potential use of antiresorptive agents. In addition, all antiparathyroid agents (vitamin D derivatives and/or calcimimetics) effectively lower APs by ameliorating high bone turnover but they could theoretically induce ABD [37]. The conflicting information on the use of biomarkers to predict underlying bone histology is also unsurprising given the short half-lives of most of the circulating biomarkers and the long (3–6 months) bone remodeling (turnover) cycle [1]. Thus, although neither PTH nor BSAP alone or both in combination is sufficiently robust to diagnose high, normal, or low bone turnover in an individual patient, the current KDIGO guidelines suggest that, in patients with CKD G3a-5D, measurements of serum PTH or BSAP can be used to evaluate bone disease because markedly high or low values predict underlying bone turnover (Table 1). Despite all these described controversies [53, 54], serum PTH levels are considered one of the most useful biomarkers in the diagnosis of ROD and an important treatment target [34, 53]. Moreover, there is general agreement that low PTH levels (i.e., < 2X the upper limit of normality for the assay) are associated with ABD (and its potential complications) in dialysis patients [1, 18, 55], and that PTH levels should not be > 9X the upper limit of normality for the assay in dialysis patients because such levels indicate not only a higher probability of a high-turnover bone disease but also a potential “extreme of risk” for death [1]. Therefore, in agreement with guidelines [1, 18, 20], PTH trends between 2X and 9X (in dialysis patients) should also be considered, rather than reacting to each individual iPTH values.
If CKD-MBD laboratory parameters are reasonably under control, and bearing in mind that osteoporosis medications are considered to improve an unacceptable high risk of fracture, the new guidelines and consensus consider that a bone biopsy is no longer mandatory though it remains an option [1, 18, 20]. It is generally accepted that ABD should be reasonably excluded before antiresorptive treatments are prescribed [1, 11, 15,16,17,18,19,20], although the implications of drug-induced suppression of bone turnover for bone strength and bone material properties are intensely debated [20]. It also remains a matter of debate whether low-turnover bone disease per se or the disease-causing low bone turnover accounts for the perceived increased fracture risk [20]. While studies in patients with CKD have not definitively demonstrated that bisphosphonates or denosumab cause clinically significant ABD [1], it remains prudent to use these drugs with caution since ABD is increasing in prevalence [55]. This observation is attributable to various factors [55] and is at least partially explained by the higher number of diabetic patients, the more frequent initiation of dialysis therapy in the elderly, and probably the excessive use of antiparathyroid medications that lower bone turnover. Interestingly, a low AP level is associated with greater survival, a finding that appears to question the harmfulness of ABD [35]. It is of note that direct PTH-independent anabolic effects have recently been described for calcimimetics [56, 57]. Interestingly, PTH is a known critical regulator of skeletal development that promotes both bone formation (i.e., in pulses) and bone resorption (as in chronic hyperparathyroidism), and it was recently shown in microbiota-depleted female mice that microbiota are required for PTH to stimulate bone formation and increase bone mass [58]. Microbiota depletion lowered the levels of butyrate, a metabolite responsible for gut-bone communication [58]. Reestablishment of physiologic levels of butyrate restored PTH-induced anabolism via T-cell-dependent stimulated activation of the osteogenic Wnt-dependent bone formation pathway [58].
Other Bone Biomarkers
There are several other commercially available serum biomarkers of bone activity (bone formation or bone resorption) (Table 2). However, it is beyond the scope of this review to comprehensively analyze them, especially considering that current Nephrology guidelines do not recommend their measurement in patients with CKD G3a-G5D (Table 1) [1]. This is because many biomarkers are significantly affected by renal function (Table 2), and also, as mentioned previously, because of the scarcity of available data, their lack of homogeneity, and the distinct prevalence of low- vs high-turnover bone disease in different cohorts. It is also to be noted that the presence of CKD may go unnoticed if only serum creatinine (not eGFR) is considered, especially in thin elderly women with a low muscular mass. Nevertheless, we will briefly mention some of their main characteristics; for further information, we encourage interested readers to consult recent reviews on these biochemical markers [20, 27, 42, 59,60,61,62], including their relationship with PTH and other aspects of the CKD-MBD complex [34, 42, 63, 64].
The protein matrix of bone consists to a large extent (85%) of collagen-1 [34]. Collagen-1 is formed by osteoblasts as procollagen-1 and, on maturation, both the N-terminal and C-terminal endings are cleaved. The small cleavage fragments, procollagen type 1 N-terminal propeptide (P1NP), and procollagen type 1 C-terminal propeptide (P1CP), are detectable in the circulation and are therefore indicative of the formation rate of collagen [27, 62]. The only potentially reliable assay in patients with CKD is the intact P1NP because it detects the trimeric form as opposed to the CKD-accumulating monomeric form and is not affected by either GFR or dialysis [27, 42, 65]. P1CP, in particular, has a short half-life, and therefore, PN1P is the bone formation marker recommended in the general population (Table 2). P1NP recently performed worse than iPTH or BSAP in distinguishing between low- and non-low-turnover bone disease and had no additional value over iPTH for diagnosing high-turnover bone disease; however, total P1NP was used in that study [27, 38]. Interestingly, in another previous study, serum levels of intact P1NP were correlated with PTH, BSAP, osteocalcin, and bone resorption markers (see below) [66], and a negative correlation was described with annual changes in distal radius BMD in hemodialysis patients [66]. More recently, higher levels of P1NP were associated with higher odds of fracture as compared with levels in the lowest tertile, even after adjustment for femoral neck T-score, in predialysis CKD [67].
Bone-derived osteocalcin, the most abundant non-collagenous protein of bone, has poor specificity in the diagnosis of ROD, in part because it is broken down after 3–6 months, the release into the circulation of multiple osteocalcin fragments and the renal clearance of the molecule [30]. Moreover, osteocalcin (also known as bone Gla protein or BGP) exists in various carboxylation (vitamin K dependent) and phosphorylation states (similarly to the tissue calcification inhibitor matrix Gla protein or MGP) which can be distinguished only with dedicated assays [11, 42]. Vitamin K availability is additionally affected in CKD patients, impacting on the clinical value of osteocalcin as a bone turnover marker, especially compared with others [27, 68]. It also needs to be considered that PTH and vitamin D are renowned promoters of osteocalcin synthesis by osteoblasts [42]. Renewed interest in osteocalcin is also attributable to its association with glucose and energy metabolism, as well as newly described associations with decreased bone mass and/or fractures [10, 42, 67, 69].
On the other hand, lysosomal enzymes derived from osteoclasts (including TRAPs and cathepsin K) are responsible for breakdown of the collagenous bone matrix at specific sites. Resultant products such as carboxy-terminal crosslinking telopeptide of type 1 collagen (CTX) are considered reference markers for bone resorption in the general population [62] but are highly dependent on kidney function for their removal from the circulation; therefore, the use of CTX cannot be recommended in patients with CKD [26, 41]. Bone biopsy studies in CKD patients exploring the utility of CTX are limited and overall have yielded disappointing results [60]. However, it remains to be seen whether trends in patients with stable renal function, especially in early stages of CKD, may provide useful clinical information, as in the general population. On the other hand, measurement of N-terminal telopeptide collagen (NTX) (as well as pyridoline and the related deoxypyridoline cross-links) in urine is obviously unreliable in patients with CKD. Finally, it is worth mentioning that osteoclast-derived TRAP5b (tartrate resistant acid phosphatase 5b—the adjective acid indicates that its optimal activity occurs in acidic conditions, as might be expected for a bone resorption-related enzyme) is strongly associated with both the number and the size of the osteoclast-like cells and is not affected by either renal function or dialysis [70, 71]; it thus represents a good candidate biomarker for bone resorption in patients with CKD. Serum levels of TRAP5b have been found to correlate strongly with histomorphometric parameters of bone resorption and with the rate of cortical bone loss in dialysis patients [71, 72]. Low TRAP5b levels could be of value for the recognition of ABD, and this could help explain the predictive role of TRAP5b in respect of cardiovascular events in patients with CKD G1–G5 who were followed up for 4 years (OR 0.86; 95% confidence interval 0.75–0.99; p = 0.04) [73]. However, in this same study, higher levels of BSAP were reported to be related to cardiovascular events (OR 1.01; 95% confidence interval 1.01–1.02; p = 0.03) [73]. Moreover, in 82 patients with predialysis CKD G3–G5, 23 of whom had prevalent fractures, the highest tertile of not only formation markers (as measured by the previously mentioned P1NP) but also resorption markers (as measured by TRAP5b) were positively and independently associated with higher odds of prevalent fractures as compared with levels in the lowest tertile [67]. Compared with the DXA T-score alone, combination of the highest tertile of P1NP or TRAP5b with the DXA T-score at the femoral neck was found to result in improved discrimination of those with a prior fracture [67]. One possible explanation for the rather limited use of TRAP5b in CKD is that the available assays are still not entirely specific for bone TRAP5b, and therefore, development of more specific monoclonal antibodies will be welcome [42].
With regard to regulators of bone remodeling, fibroblast growth factor-23 (FGF23) levels have been found to be inversely correlated with both static and dynamic indices of osteoid mineralization in CKD G5D, but more studies are needed to confirm FGF23 as a marker of mineralization or bone remodeling [74]. It has been reported that FGF23 is a suppressor of non-specific AP transcription via the FGF receptor-3 (FGFR3) signaling, leading to inhibition of mineralization through accumulation of the AP substrate pyrophosphate [75]. FGF23 may thereby link local mineral needs with regulation at the level of the kidney and/or intestine [74]. However, FGF23 levels are affected by many factors beyond bone metabolism, and many renal and extrarenal effects have been attributed to FGF23 [10, 76]. Sclerostin and Dickkopf-1 (Dkk-1) are soluble inhibitors of the canonical wingless-type mouse mammary tumor virus integration site (Wnt)/β-catenin signaling pathway and also components of the PTH signal transduction. Wnt-signaling activation reduces osteoblast and osteoclast apoptosis, induces osteoblastogenesis, and inhibits osteoclastogenesis [77]. These actions result in a subsequent increase in bone formation and BMD and may be crucial in CKD-MBD pathogenesis, but these markers are far from being clinically valuable as surrogates for bone fragility [78,79,80,81]. Thus, sclerostin has been positively associated with BMD in older men and patients with advanced CKD, including those receiving maintenance hemodialysis or peritoneal dialysis [82,83,84,85]. This positive association between sclerostin and BMD is not well explained by the BMD-lowering effects of sclerostin, which have been demonstrated by interventional studies demonstrating a lower risk of vertebral fractures in postmenopausal women with osteoporosis after antagonizing sclerostin with romosozumab [86]. CKD-MBD is a complex disease condition in which sclerostin antibodies may interfere at different levels and distinctly influence the relationship among secondary hyperparathyroidism, ROD, and/or vascular calcification, “but the clinical sequelae remain obscure” [87]. Moreover, CKD is closely associated with cardiovascular disease [10, 11], and warnings have been issued even regarding the indication for romosozumab in the general population. Of note, sclerostin was also reported to be superior to iPTH for the positive prediction of high bone turnover and number of osteoblasts. In contrast, iPTH was superior to sclerostin for the negative prediction of high bone turnover and had similar predictive values to sclerostin for the number of osteoblasts [79]. Opposite results have also been described [74]. Serum levels of Dkk-1 have been found not to correlate with iPTH or with any histomorphometric parameter [79]. It remains to be determined whether a ratio between markers of the anabolic PTH-Wnt pathway and the inhibitory sclerostin-Wnt pathway could be clinically useful. In fact, increased inhibitors can oppose the action of PTH already in early CKD [88, 89], as well as contribute to the well-known CKD-induced multifactorial skeletal resistance (also recently called hyporesponsiveness) to PTH in CKD [90].
Interestingly, many of these markers were recently evaluated in patients with different stages of CKD [74]. Bone expression of sclerostin and PTHR1 seemed to be increased in earlier stages of CKD, whereas phosphorylated β-catenin showed increased expression in the late stages of CKD [74]; however, levels of all these proteins were elevated relative to those in healthy individuals. Moreover, these authors also showed that FGF23 and sclerostin did not co-localize, suggesting that distinct osteocytes in different areas of the trabecular bone produce these proteins [74]. It is to be noted that changes in circulating biomarkers after kidney transplantation could not be easily extrapolated to concomitant changes occurring in the bone [74]. In summary, results with these biomarkers encourage new directions for clinical research, but their utility is not firmly established [81].
Finally, it seems that in CKD, the receptor activator of nuclear factor-κB (RANK)/receptor activator of nuclear factor-κB ligand (RANKL)/osteoprotegerin (OPG) system, which is essential for the coupled activity of osteoblasts and osteoclasts and is involved critically with bone remodeling and mass, is more closely linked with CKD-associated cardiovascular disease than with bone disease [42]. The importance of the SIBLING (Small Integrin-Binding Ligand N-linked Glycoprotein) family of proteins for skeletal mineralization and bone remodeling in CKD remains to be explored [42, 91]. These proteins are in some ways related to FGF23 and may represent a novel bone-renal pathway impacting not only on bone formation and mineralization but also on renal phosphate homeostasis and energy metabolism [92]. Similarly, Sirtuin 1 (SIRT1) has been implicated in a number of cellular processes which constitute a common denominator of chronic diseases and aging. Thus, the activation of SIRT1 has also become a potential novel therapeutic target to improve the clinical outcome in patients with CKD [93]. In this regard, SIRT1 has recently been described as a positive regulator of the master osteoblast transcription factor RUNX2 [94]. All these new pathways may become relevant for the development of therapies for a number of diseases, including CKD, ROD, and CKD-MBD [92, 93].
Taking into account all this information, the previously mentioned European Consensus Statement on the diagnosis and management of osteoporosis in CKD stages 4-5D [20], stated that (a) non-kidney-retained bone turnover markers, such as BSAP, intact P1NP and TRAP5b, should be preferentially monitored in CKD patients; and (b) monitoring of these markers may provide information on the early therapeutic response or the need for reintroduction of potential treatments after therapy withdrawal. These biomarkers should preferentially be used in the setting of CKD, especially in patients with non-stable kidney function [20, 60]. It is also stated that these non-kidney-retained bone turnover markers, especially BSAP, may be useful for fracture risk prediction in CKD G4-G5D, though this awaits confirmation [20]. A variety of other molecules and the emerging role of microRNAs in bone remodeling [95] might also be of interest in CKD, but their use still needs further investigation across the different CKD stages and distinct bone turnover status.
Imaging
In contrast to histomorphometry or circulating biomarkers, imaging techniques are not capable of measuring bone turnover; on the other hand, biomarkers do not offer information about other features of bone, such as mineralization, geometry, connectivity, and cross-linking, which also determine bone strength and are clearly affected by CKD. In this context, combined information and longitudinal follow-up may be helpful in risk categorization and decision making.
Dual-Energy X-ray Absorptiometry
Dual-energy X-ray absorptiometry (DXA) is the most widely used non-invasive technique for measuring BMD in the general population [15]. Low BMD on DXA is a robust and consistent risk factor for fracture, and treatments that increase BMD usually reduce fracture risk [15]. Thus, the 2017 updated KDIGO CKD-MBD guideline changed gear as compared to the previous 2009 KDIGO guideline and KDIGO now supports the use of DXA to assess fracture risk in patients with CKD G1-G2, insofar as it recommends that management of these patients with osteoporosis and/or high risk of fracture, as identified by the World Health Organization (WHO) criteria, should be as for the general population (Guideline 4.3.1, evidence grade 1A). In patients with CKD G3a–G3b with PTH in the normal range and osteoporosis and/or high risk of fracture, it is suggested that treatment should be as for the general population (Guideline 4.3.2, evidence grade 2B). The main reason behind this significant change is that multiple new prospective studies have now documented that lower BMD assessed by DXA does predict incident fractures across the spectrum from CKD3a to G5D as well as in transplant patients [1, 15, 61, 96,97,98,99]. BMD was also found to predict fractures in the recent Regina CKD-MBD study [100]. Moreover, as mentioned previously, the inability to perform a bone biopsy may not justify withholding antiresorptive therapy from patients at high risk of fractures [1, 11, 14, 18, 20]. Consequently, considering that CKD patients are at high risk of fracture, these changes have also been recently endorsed by the previously mentioned European Consensus Statement [20], which states that DXA testing may now be considered even in patients with CKD G4-G5D, at least in postmenopausal women or men > 50 years of age [20].
Nevertheless, DXA does not correlate with bone histomorphometry or provide information on bone microarchitecture, nor does it properly assess bone compartments (cortical vs trabecular bone) even though it allows valid assessment of cortical bone at the ultradistal radius. With respect to this location, however, one should be aware of operator-dependent variability and potential bias by arteriovenous fistula [20]. The inability of DXA to indicate the histologic type of bone disease (mainly to discriminate among high-, normal-, and low-turnover bone disease) sometimes makes it difficult to reach clear-cut therapeutic decisions. As a matter of fact, BMD only provides information on the quantity (g/cm2) and not the quality (structure and composition) of bone. In other words, DXA is promising in terms of its ability to non-invasively quantify some components of ROD (such as combined bone volume and mineralization) and is proven to assist in fracture prediction even in patients with CKD, but it does not provide information on the important bone turnover and thereby the underlying type of ROD. Nevertheless, DXA is inexpensive, is widely available, uses minimal radiation, is easily standardized across sites, and has good reproducibility and reliable reference ranges for age, gender, and race [59, 101].
Currently, the DXA-derived assessment of the trabecular bone score (TBS) may help in providing some information on bone architecture, even in dialysis patients, partially correcting the calculation of the absolute 10-year fracture risk [102]. TBS is a novel tool using a gray-level textural index derived by an algorithm that analyzes the special organization of pixel intensity from lumbar spine DXA images to assess trabecular bone microarchitecture [81]. Some but not all studies in patients with CKD suggest that TBS may be helpful in assessment of fracture risk [103,104,105]. Importantly, even in multivariate analysis, TBS remained an independent predictor of trabecular bone volume (BV/TV) and trabecular width measured by bone biopsy in CKD patients [106]. Therefore, DXA may also be a good tool for the serial assessment of BMD (and/or TBS) in response to interventions, although much information is still lacking. It is also important to know that TBS response to pharmacological interventions is lower than that of BMD. During BMD assessment by DXA, the diagnosis of vertebral fractures could also be improved by quantitative vertebral morphometry or vertebral fracture assessment (VFA) [20, 107, 108]. Whenever possible, VFA is especially recommended when the T-score is < − 1.0 and if one or more of the following is present: age ≥ 70 years in women or ≥ 80 years in men, historical height loss > 4 cm, kyphosis, self-reported but undocumented vertebral fracture, or recent or current long-term glucocorticoid therapy (equivalent to ≥ 5 mg of prednisone or equivalent per day ≥ 3 months) [20]. Of note, the use of specific 3D-DXA software in conventional densitometers may also help in the analysis of structural parameters of cortical bone (i.e., vBMD and cortical thickness), as has been demonstrated in primary hyperparathyroidism [109]. Other novel imaging techniques provide information about bone quality and/or architecture (Table 3), but there is a lack of standardization and data to validate their ability to predict fracture risk in CKD.
In summary, DXA measurement is inexpensive and widely available, and predicts the risk of fractures in CKD patients in a comparable way to risk prediction in the general population. However, DXA alone cannot estimate the severity or the degree of bone turnover in CKD. Similar BMD values can be observed in low- and in high-turnover bone disease. DXA-derived TBS and/or VFA may also be helpful in the assessment of fracture risk. In addition, it is worth mentioning that repeat DXA provides information on the long-term treatment effect on BMD. The time interval when treatment effect can be detected may vary depending on the treatment modality and underlying type of ROD [20].
Quantitative Computerized Tomography and Peripheral Quantitative Computerized Tomography
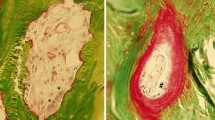
Quantitative computerized tomography (QCT) and peripheral quantitative computerized tomography (pQCT) allow 3D imaging of cross sections of the central and axial skeleton (QCT) or tibia and distal radius (pQCT) in order to provide volumetric BMD (as opposed to areal BMD for DXA). They also allow distinction between the cortical and the trabecular compartment, and the calculation of some biochemical parameters related to bone resistance.
In CKD patients, QCT measurements at the spine have been correlated with histomorphometry and prediction of vertebral fractures [111]. Vertebral bone density has repeatedly been shown to be associated with coronary artery calcification and even to be an independent predictor of poor outcomes, linking osteoporosis with atherosclerosis [112, 113]. pQCT parameters were significantly associated with the probability of a fracture [114]. Newly developed high-resolution (HR) pQCT (HR-pQCT) [resolution = 100 µm (82 µm3) vs QCT = 0.5 mm] allows the evaluation of bone geometry and microarchitecture (trabecular thickness, separation, number, etc.) in addition to the measurements provided by QCT and pQCT. However, use of HR-pQCT is limited to research centers, and an additive value over available biomarkers or even DXA has not been proven. For example, HR-pQCT did not demonstrate a better performance than DXA in terms of fracture prediction in patients with CKD G3-G5 after 2 years of follow-up [98]. In this study, bone loss occurred in all participants but was significantly greater among those with incident fractures. Low BMD (on both DXA and radial HR-pQCT) and a greater annualized percentage decrease in BMD were found to be risk factors for subsequent fracture in men and women with non-dialysis CKD [98]. Similar findings were previously described elsewhere [115]. In patients with CKD G2-G4, HR-pQCT showed early impairment of trabecular bone before the onset of secondary hyperparathyroidism, at least partially explaining the high risk of fractures not only in patients with early CKD but also in those with a long history of CKD [116, 117]. In other more recent studies, HR-pQCT showed significant differences in bone microstructure in men with CKD G4 vs CKD G3, influenced by hormonal changes and body composition [118], and HR-pQCT findings were in agreement with bone biopsy parameters and provided some uncertain clues on the turnover status through measurements of cortical density at the radius together with biochemical parameters [119]. Interestingly, the biomarkers BSAP, intact P1NP, and TRAP5b (AUROC = 0.82, 0.79, and 0.80, respectively) and radius HR-pQCT parameters (total volumetric BMD and cortical bone volume; AUROC = 0.81 and 0.80, respectively) were recently found to be able to discriminate low- from non-low bone turnover, whereas iPTH discriminated high bone turnover (AUROC = 0.76), with an accuracy similar to that of the other biomarkers, including CTX [120]. These data confirm that the quest to find better biomarkers of turnover or a panel thereof in CKD patients is far from over, and it even has been recently challenged [60, 121, 122].
In summary, pQCT and HR-pQCT provide better spatial resolution of bone microarchitecture than other techniques. They accurately differentiate trabecular from cortical bone in metabolic bone disorders with a lower radiation dose. Tibial HR-pQCT already predicts relatively well the risk of fractures in patients with early CKD.
Magnetic Resonance Imaging
High-resolution magnetic resonance imaging (HR-MRI) also allows 3D-imaging of the bone geometry and trabecular architecture at peripheral sites but without ionizing radiation. For example, using AUROC analysis, the highest diagnostic performance was found for a combination of BMD and architecture measures in a small cohort of kidney transplant patients [123]. On the other hand, micro-MRI is a technique with an excellent spatial resolution, almost similar to an actual bone biopsy [59]. For example, disruptions of the distal tibial trabecular network were described in hemodialysis patients with secondary hyperparathyroidism as compared with controls [124].
In summary, although HR-MRI does not use ionizing radiation, it has largely been replaced by HR-pQCT due to the complicated nature of the scanning equipment, which is not routinely available. In the future, HR-MRI may help in characterizing functional aspects of cortical and trabecular bone as well as bone marrow, beyond the mineralized component. It may also assist in quantifying cortical water and collagen content and quality in CKD.
Conclusions and Perspectives
Although current guidelines consider that the inability to perform a bone biopsy may not justify withholding antiresorptive therapy from patients at high risk of fracture [1, 14, 16,17,18, 20], they also conclude that in patients with CKD G3a-5D, it is reasonable to perform a bone biopsy if knowledge of the type of ROD will impact treatment decisions (Guideline 3.2.2; not graded) [1]. A bone biopsy should also be considered in patients with unexplained fractures, refractory hypercalcemia, suspicion of osteomalacia, an atypical response to standard therapies for elevated PTH, or progressive decreases in BMD despite therapies [1]. Discrepancies between, for instance, serum PTH and BSAP levels are uncommon and reflect an uncoupling between bone resorption and formation, but in some patients, they may be found beyond hyporesponsiveness to PTH in CKD [4, 28, 90, 125, 126]. The clinical value of the much less invasive measurement of the bone material strength index (BMSi) [127] in vivo with the impact microindentation system (Osteoprobe®) remains to be further evaluated in CKD and/or kidney transplant patients [127, 128].
In conclusion, (a) the available biochemical markers are limited, (b) even a reliable estimate of turnover would not indicate changes in bone balance, (c) harmonization and standardization of available assays are needed, in conjunction with bone biopsy studies, and (d) fracture risk is also dependent on bone features that cannot be assessed by biomarkers or even by bone histomorphometry. Nevertheless, it is important to stress that recent analyses show that PTH is still currently the most useful surrogate biomarker for bone histology in CKD, while also implementing APs and identifying new biomarkers and/or panels of bone formation/resorption markers of potential clinical value [20, 53, 54, 81]. This is the case despite the existence of some ongoing controversies involving renowned experts [53, 54]. We also agree with the 2017 KDIGO guidelines regarding the use of trends (e.g., in serum iPTH levels) rather than individual values when making decisions on whether to start or stop antiparathyroid treatments [1]. Revised guidelines have now included the term persistently above the upper normal PTH level as well as progressively rising PTH level, rather than above the upper normal limit for the assay [1, 18]. Moreover, some guidelines underline that PTH levels should not be normalized with antiparathyroid treatments in patients with CKD once modifiable factors (e.g., hyperphosphatemia, high phosphate intake, vitamin D deficiency) are corrected [1, 18]. At least initial increments in PTH play an adaptive role; however, it may not be reasonable to reserve the use of antiparathyroid agents only for patients in whom severe and progressive hyperparathyroidism is present [18]. Future treatments should probably aim to overcome hormone resistance in CKD [90]. If osteoporosis medications are considered to decrease the risk of fracture, a bone biopsy is no longer mandatory, but ABD should be reasonably excluded before antiresorptive treatments are prescribed [11, 15, 17,18,19,20]. Ultimately, the optimal diagnostic strategy for ROD will probably be the combination of several biomarkers with imaging techniques (gender and race specific), with the new goal of predicting fracture risk and optimizing therapy/bone turnover [20, 59, 60]. Moreover, one must not forget that BMD assessment by DXA reflects bone loss accumulated over a period of years, whereas biochemical markers reflect acute changes in bone metabolism and as such may be less convenient as risk markers and serve different purposes [20, 60, 61]. Several diagnostic and treatment algorithms based on non-invasive methods, which at least partially limit the need for bone biopsies, have already been published [81, 129, 130]. Finally, it is to be emphasized that reduction in fractures, not improvement in biomarkers and/or DXA results, is the real end-point for approval of new therapeutics for osteoporosis [26]. It remains to be seen in prospective multi-ethnic studies whether these “old” or new bone biomarkers will increase the diagnostic accuracy of imaging techniques for identification of patients with CKD at high risk for fracture or significant bone disease, and whether they are useful for decision making.
Meanwhile, many consider that it is time for action [14, 17, 18, 77]. Moreover, the previously mentioned European Consensus Statement in CKD patients aims to stimulate a cohesive approach to the management of these patients in order to reduce current variations in care and treatment nihilism [20]. Nevertheless, considering that information on many aspects is still scarce, especially in advanced CKD and dialysis patients, it would be an advisable approach to share risks and benefits with the patient [20]. Formal informed consent has been suggested and may be required when considering off-label use [20]. Especially in view of the current emphasis on patient-centered, individualized management scenarios [131], we need to recognize our certainly limited ability to impose or base certain treatment decisions only on our current non-comprehensive knowledge [132, 133].
References
Ketteler M, Block GA, Evenepoel P, Fukagawa M, Herzog CA, McCann L, Moe SM, Shroff R, Tonelli MA, Toussaint ND, Vervloet MG, Leonard MB (2017) Executive summary of the 2017 KDIGO Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD) Guideline Update: what’s changed and why it matters. Kidney Int 92(1):26–36
Cozzolino M, Ureña-Torres P, Vervloet MG, Brandenburg V, Bover J, Goldsmith D, Larsson TE, Massy ZA, Mazzaferro S, CKD-MBD Working Group of ERA-EDTA (2014) Is chronic kidney disease-mineral bone disorder (CKD-MBD) really a syndrome? Nephrol Dial Transplant. 29(10):1815–1820
Torres PU, Bover J, Mazzaferro S, de Vernejoul MC, Cohen-Solal M (2014) When, how, and why a bone biopsy should be performed in patients with chronic kidney disease. Semin Nephrol 34(6):612–625
Llach F, Bover J (2000) Renal osteodystrophies. In: Brenner BM (ed) The kidney, 6th edn. W.B. Saunders Company, Philadelphia, pp 2103–2186
Liu SH, Chu HI (1942) Treatment of renal osteodystrophy with dihydrotachysterol (a.t.10) and iron. Science (Washington) 95(2467):388–389
Lucas RC (1883) On a form of late rickets associated with albuminuria, rickets of adolescence. Lancet 1:993–994
Fletcher HM (1910) Case of infantilism with polyuria and chronic renal disease. Proc Roy Soc Med Sect Stud Dis Child 11(4):95
Langmead FS, Orr JW (1933) Renal rickets associated with parathyroid hyperplasia. Arch Dis Child 8:265–278
Moe S, Drüeke T, Cunningham J, Goodman W, Martin K, Olgaard K, Ott S, Sprague S, Lameire N, Eknoyan G, Kidney Disease: Improving Global Outcomes (KDIGO) (2006) Definition, evaluation, and classification of renal osteodystrophy: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int 69(11):1945–1953
Vervloet MG, Massy ZA, Brandenburg VM, Mazzaferro S, Cozzolino M, Ureña-Torres P, Bover J, Goldsmith D, CKD-MBD Working Group of ERA-EDTA (2014) Bone: a new endocrine organ at the heart of chronic kidney disease and mineral and bone disorders. Lancet Diabetes Endocrinol 2(5):427–436
Covic A, Vervloet M, Massy ZA, Ureña-Torres P, Goldsmith D, Brandenburg V, Mazzaferro S, Evenepoel P, Bover J, Apetri M, Cozzolino M (2018) Bone and mineral disorders in chronic kidney disease: implications for cardiovascular health and ageing in the general population. Lancet Diabetes Endocrinol 6(4):319–331
Mazzaferro S, De Martini N, Rotondi S, Tartaglione L, Ureña-Torres P, Bover J, Pasquali M, ERA-EDTA Working Group on CKD-MBD (2020) Bone, inflammation and chronic kidney disease. Clin Chim Acta. 506:236–240
Mazzaferro S, Cianciolo G, De Pascalis A, Guglielmo C, Urena Torres PA, Bover J, Tartaglione L, Pasquali M, La Manna G (2018) Bone, inflammation and the bone marrow niche in chronic kidney disease: what do we know? Nephrol Dial Transplant 33(12):2092–2100
Moe SM, Nickolas TL (2016) Fractures in patients with CKD: time for action. Clin J Am Soc Nephrol 11(11):1929–1931
Goldenstein PT, Jamal SA, Moysés RMA (2015) Fractures in chronic kidney disease: pursuing the best screening and management. Curr Opin Nephrol Hypertens 24(4):317–323
Bover J, Ureña-Torres P, Torregrosa JV, Rodríguez-García M, Castro-Alonso C, Górriz JL, Laiz Alonso AM, Cigarrán S, Benito S, López-Báez V, Lloret Cora MJ, daSilva I, Cannata-Andía J (2018) Osteoporosis, bone mineral density and CKD-MBD complex (I): diagnostic considerations. Nefrologia 38(5):476–490
Bover J, Ureña-Torres P, Laiz Alonso AM, Torregrosa JV, Rodríguez-García M, Castro-Alonso C, Górriz JL, Benito S, López-Báez V, Lloret Cora MJ, Cigarrán S, DaSilva I, Sánchez-Bayá M, Mateu Escudero S, Guirado L, Cannata-Andía J (2019) Osteoporosis, bone mineral density and CKD-MBD (II): therapeutic implications. Nefrologia 39(3):227–242
Torregrosa V, Bover J, Rodriguez M et al (2020) Spanish Society of Nephrology recommendations for controlling mineral and bone disorders in chronic kidney disease patients. Nefrologia 31:3–32
Bover J, Bailone L, López-Báez V, Benito S, Ciceri P, Galassi A, Cozzolino M (2017) Osteoporosis, bone mineral density and CKD-MBD: treatment considerations. J Nephrol 30(5):677–687
Evenepoel P, Cunningham J, Ferrari S, Haarhaus M, Javaid MK, Lafage-Proust MH, Prieto-Alhambra D, Torres PU, Cannata-Andia J (2020) European Renal Osteodystrophy (EUROD) workgroup, an initiative of the CKD-MBD working group of the ERA-EDTA, and the committee of Scientific Advisors and National Societies of the IOF. Nephrol Dial Transplant. https://doi.org/10.1093/ndt/gfaa192
Nickolas TL, McMahon DJ, Shane E (2006) Relationship between moderate to severe kidney disease and hip fracture in the United States. J Am Soc Nephrol 17:3223–3232
Ishani A, Blackwell T, Jamal SA et al (2008) The effect of raloxifene treatment in postmenopausal women with CKD. J Am Soc Nephrol 19:1430–1438
Jamal SA, Bauer DC, Ensrud KE et al (2007) Alendronate treatment in women with normal to severely impaired renal function: an analysis of the fracture intervention trial. J Bone Miner Res 22:503–508
Miller PD, Roux C, Boonen S et al (2005) Safety and efficacy of risedronate in patients with age-related reduced renal function as estimated by the Cockcroft and Gault method: a pooled analysis of nine clinical trials. J Bone Miner Res 20:2105–2115
Miller PD, Schwartz EN, Chen P et al (2007) Teriparatide in postmenopausal women with osteoporosis and mild or moderate renal impairment. Osteoporos Int 18:59–68
Jamal SA, Ljunggren O, Stehman-Breen C et al (2011) Effects of denosumab on fracture and bone mineral density by level of kidney function. J Bone Miner Res 26:1829–1835
Vervloet MG, Brandenburg VM, CKD-MBD working group of ERA-EDTA (2017) Circulating markers of bone turnover. J Nephrol 30(5):663–670
Bover J, Ureña P, Aguilar A, Mazzaferro S, Benito S, López-Báez V, Ramos A, daSilva I, Cozzolino M (2018) Alkaline phosphatases in the complex chronic kidney disease-mineral and bone disorders. Calcif Tissue Int 103(2):111–124
Ureña-Torres P, Hruby M, Ferreira A, Ang KS, de Vernejoul MC (1996) Plasma total versus bone alkaline phosphatase as markers of bone turnover in hemodialysis patients. J Am Soc Nephrol 7(3):506–512
Ureña-Torres P, de Vernejoul C (1999) Circulating biochemical markers of bone remodelling in uremic patients. Kidney Int 55(6):2141–2156
National Kidney Foundation (2003) K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis 42(4 Suppl 3):S1-201
Nizet A, Cavalier E, Stenvinkel P, Haarhaus M, Magnusson P (2020) Bone alkaline phosphatase: an important biomarker in chronic kidney disease—mineral and bone disorder. Clin Chim Acta 501:198–206
Couttenye M, D’Haese PC, Van Hoof VO, Lemoniatou E, Goodman W, Verpooten GA, De Broe ME (1996) Low serum levels of alkaline phosphatase of bone origin: a good marker of adynamic bone disease in haemodialysis patients. Nephrol Dial Transplant 11(6):1065–1072
Ureña-Torres PA, Bover J, Cohen-Solal M (2020) Relation between PTH and biochemical markers of MBD. In: Covic A, Goldsmith G, Ureña-Torres PA (eds) Parathyroid glands in chronic kidney disease. Berlin, Springer, pp 103–116
Lau WL, Kalantar-Zadeh K (2014) Towards the revival of alkaline phosphatase for the management of bone disease, mortality and hip fractures. Nephrol Dial Transplant 29(8):1450–1452
Coen G, Ballanti P, Bonucci E, Calabria S, Centorrino M, Fassino V, Manni M, Mantella D, Mazzaferro S, Napoletano I, Sardella D, Taggi F (1998) Bone markers in the diagnosis of low turnover osteodystrophy in haemodialysis patients. Nephrol Dial Transplant 13(9):2294–2302
Behets GJ, Spasovski G, Sterling LR, Goodman WG, Spiegel DM, De Broe ME, D’Haese PC (2015) Bone histomorphometry before and after long-term treatment with cinacalcet in dialysis patients with secondary hyperparathyroidism. Kidney Int 87(4):846–856
Sprague SM, Bellorin-Font E, Jorgetti V, Carvalho AB, Malluche HH, Ferreira A, D’Haese PC, Drüeke TB, Du H, Manley T, Rojas E, Moe SM (2016) Diagnostic accuracy of bone turnover markers and bone histology in patients with CKD treated by dialysis. Am J Kidney Dis 67(4):559–566
Monier-Faugere MC, Geng Z, Mawad H, Friedler RM, Gao P, Cantor TL, Malluche HH (2001) Improved assessment of bone turnover by the PTH-(1–84)/large C-PTH fragments ratio in ESRD patients. Kidney Int 60(4):1460–1468
Ardawi MSM, Rouzi AA, Qari MH (2012) Physical activity in relation to serum sclerostin, insulin-like growth factor-1, and bone turnover markers in healthy premenopausal women: a cross-sectional and a longitudinal study. J Clin Endocrinol Metab 97(10):3691–3699
Sardiwal S, Gardham C, Coleman AE, Stevens PE, Delaney MP, Lamb EJ (2012) Bone-specific alkaline phosphatase concentrations are less variable than those of parathyroid hormone in stable hemodialysis patients. Kidney Int 82(1):100–105
Mazzaferro S, Tartaglione L, Rotondi S, Bover J, Goldsmith D, Pasquali M (2014) News on biomarkers in CKD-MBD. Semin Nephrol 34(6):598–611
Haarhaus M, Monier-Faugere MC, Magnusson P, Malluche HH (2015) Bone alkaline phosphatase isoforms in hemodialysis patients with low versus non-low bone turnover: a diagnostic test study. Am J Kidney Dis 66(1):99–105
Kim DW, Hwang SY, Nam YJ, Kim D, Shin SJ, Yoon HE (2020) The combined prognostic significance of alkaline phosphatase and vascular calcification in patients with end-stage kidney disease. Nutr Metab Cardiovasc Dis 30(9):1476–1483
Haarhaus M, Brandenburg V, Kalantar-Zadeh K, Stenvinkel P, Magnusson P (2017) Alkaline phosphatase: a novel treatment target for cardiovascular disease in CKD. Nat Rev Nephrol 13(7):429–442
Souberbielle JC, Boutten A, Carlier MC, Chevenne D, Coumaros G, Lawson-Body E, Massart C, Monge M, Myara J, Parent X, Plouvier E, Houillier P (2006) Inter-method variability in PTH. Kidney Int 70:345–350
Floege J, Kim J, Ireland E, Chazot Ch, Drueke T, de Francisco A, Kronenberg F, Marcelli D, Passlick-Deetjen J, Schernthaner G, Fouqueray B, Wheeler DC, ARO Investigators (2011) Serum iPTH, calcium and phosphate, and the risk of mortality in a European haemodialysis population. Nephrol Dial Transplant 26(6):1948–1955
Naves-Díaz M, Passlick-Deetjen J, Guinsburg A, Marelli C, Fernández-Martín JL, Rodríguez-Puyol D, Cannata-Andía JB (2011) Calcium, phosphorus, PTH and death rates in a large sample of dialysis patients from Latin America. The CORES Study. Nephrol Dial Transplant 26(6):1938–1947
Herberth J, Branscum AJ, Mawad H, Cantor T, Monier-Faugere MC, Malluche HH (2010) Intact PTH combined with the PTH ratio for diagnosis of bone turnover in dialysis patients: a diagnostic test study. Am J Kidney Dis 55(5):897–906
Sawaya BP, Butros R, Naqv S, Geng Z, Mawad H, Friedler R, Fanti P, Monier-Faugere MC, Malluche HH (2003) Differences in bone turnover and intact PTH levels between African American and Caucasian patients with end-stage renal disease. Kidney Int 64(2):737–742
Moore C, Yee J, Malluche H, Rao DS, Monier-Faugere MC, Adams E, Daramola-Ogunwuyi O, Fehmi H, Bhat S, Osman-Malik Y (2009) Relationship between bone histology and markers of bone and mineral metabolism in African-American hemodialysis patients. Clin J Am Soc Nephrol 4(9):1484–1493
Hocher B, Armbruster FP, Stoeva S, Reichetzeder C, Grön HJ, Lieker I, Khadzhynov D, Slowinski T, Roth HJ (2012) Measuring parathyroid hormone (PTH) in patients with oxidative stress–do we need a fourth generation parathyroid hormone assay? PLoS ONE 7(7):e40242
Sprague SM, Moe SM (2013) The case for routine parathyroid hormone monitoring. Clin J Am Soc Nephrol 8(2):313–318
Garrett G, Sardiwal S, Lamb EJ, Goldsmith DJA (2013) PTH–a particularly tricky hormone: why measure it at all in kidney patients? Clin J Am Soc Nephrol 8(2):299–312
Bover J, Ureña P, Brandenburg V, Goldsmith D, Ruiz C, DaSilva I, Bosch RJ (2014) Adynamic bone disease: from bone to vessels in chronic kidney disease. Semin Nephrol 34(6):626–640
Díaz-Tocados JM, Rodríguez-Ortiz ME, Almadén Y, Pineda C, Martínez-Moreno JM, Herencia C, Vergara N, Pendón-Ruiz de Mier MV, Santamaría R, Rodelo-Haad C, Casado-Díaz A, Lorenzo V, Carvalho C, Frazão JM, Felsenfeld AF, Richards WG, Aguilera-Tejero E, Mariano Rodríguez M, López I, Muñoz-Castañeda JR (2019) Calcimimetics maintain bone turnover in uremic rats despite the concomitant decrease in parathyroid hormone concentration. Kidney Int 95(5):1064–1078
Mazzaferro S, Pasquali M (2019) Direct bone effects of calcimimetics in chronic kidney disease? Kidney Int 95(5):1012–1026
Li JL, Yu M, Pal S, Tyagi AM, Dar H, Adams J, Weitzmann MN, Jones RM, Pacifici R (2020) Parathyroid hormone-dependent bone formation requires butyrate production by intestinal microbiota. J Clin Invest 130(4):1767–1781
Moorthi RN, Moe SM (2013) Recent advances in the noninvasive diagnosis of renal osteodystrophy. Kidney Int 84(5):886–894
Evenepoel P, Cavalier E, D’Haese PC (2017) Biomarkers predicting bone turnover in the setting of CKD. Curr Osteoporos Rep 15(3):178–186
Evenepoel P, Claes K, Meijers B, Laurent MR, Bammens B, Naesens M, Sprangers B, Pottel H, Cavalier E, Kuypers D (2019) Bone mineral density, bone turnover markers, and incident fractures in de novo kidney transplant recipients. Kidney Int 95(6):1461–1470
Eastell R, Szulc P (2017) Use of bone turnover markers in postmenopausal osteoporosis. Lancet Diabetes Endocrinol 5(11):908–923
Ureña-Torres PA, Vervloet M, Mazzaferro S, Oury F, Brandenburg V, Bover J, Cavalier E, Cohen-Solal M, Covic A, Drüeke TB, Hindié E, Evenepoel P, Frazão J, Goldsmith D, Kazama JJ, Cozzolino M, Massy ZA, ERA-EDTA CKD-MBD Working Group (2018) Novel insights into parathyroid hormone: report of The Parathyroid Day in Chronic Kidney Disease. Clin Kidney J 12(2):269–280
Reiss AB, Miyawaki N, Moon J, Kasselman LJ, Voloshyna I, D’Avino R, de Leon J (2018) CKD, arterial calcification, atherosclerosis and bone health: interrelationships and controversies. Atherosclerosis 278:49–59
Alvarez L, Torregrosa JV, Peris P, Monegal A, Bedini JL, Martinez De Osaba MJ, Filella X, Martin G, Ricos C, Oppenheimer F, Ballesta AM (2004) Effect of hemodialysis and renal failure on serum biochemical markers of bone turnover. J Bone Miner Metab 22(3):254–259
Ueda M, Inaba M, Okuno S, Nagasue K, Kitatani K, Ishimura E, Shimizu M, Miki T, Kim M, Nishizawa Y (2002) Clinical usefulness of the serum N-terminal propeptide of type I collagen as a marker of bone formation in hemodialysis patients. Am J Kidney Dis 40(4):802–809
Nickolas TL, Cremers S, Zhang A, Thomas V, Stein E, Cohen A, Chauncey R, Nikkel L, Yin MT, Liu XS, Boutroy S, Staron RB, Leonard MB, McMahon DJ, Dworakowski E, Shane E (2011) Discriminants of prevalent fractures in chronic kidney disease. J Am Soc Nephrol 22(8):1560–1572
Nagata Y, Inaba M, Imanishi Y, Okazaki H, Yamada S, Mori K, Shoji S, Koyama H, Okuno S (2015) Increased undercarboxylated osteocalcin/intact osteocalcin ratio in patients undergoing hemodialysis. Osteoporos Int. 26(3):1053–1061
Marchelek-Mysliwiec M, Wisniewska M, Nowosiad-Magda M, Safranow K, Kwiatkowska E, Banach B, Dołegowska B, Dołegowska K, Stepniewska J, Domanski L, Pawlik A, Ciechanowski K (2018) Association between plasma concentration of klotho protein, osteocalcin, leptin, adiponectin, and bone mineral density in patients with chronic kidney disease. Horm Metab Res 50(11):816–821
Henriksen K, Tanko LB, Qvist P, Delmas PD, Christiansen C, Karsdal MA (2007) Assessment of osteoclast number and function: application in the development of new and improved treatment modalities for bone diseases. Osteoporos Int 18(5):681–685
Shidara K, Inaba M, Okuno S, Yamada S, Kumeda Y, Imanishi Y, Yamakawa T, Ishimura E, Nishizawa Y (2008) Serum levels of TRAP5b, a new bone resorption marker unaffected by renal dysfunction, as a useful marker of cortical bone loss in hemodialysis patients. Calcif Tissue Int 82(4):278–287
Chu P, Chao TY, Lin YF, Janckila AJ, Yam LT (2003) Correlation between histomorphometric parameters of bone resorption and serum type 5b tartrate-resistant acid phosphatase in uremic patients on maintenance hemodialysis. Am J Kidney Dis 41(5):1052–1059
Fahrleitner-Pammer A, Herberth J, Browning SR, Obermayer-Pietsch B, Wirnsberger G, Holzer H, Dobnig H, Malluche HH (2008) Bone markers predict cardiovascular events in chronic kidney disease. J Bone Miner Res 23(11):1850–1858
Graciolli FG, Neves KR, Barreto F, Barreto DV, Dos Reis LM, Canziani ME, Sabbagh Y, Carvalho AB, Jorgetti V, Elias RM, Schiavi S, Moysés RMA (2017) The complexity of chronic kidney disease-mineral and bone disorder across stages of chronic kidney disease. Kidney Int 91(6):1436–1446
Murali SK, Andrukhova O, Clinkenbeard EL, White KE, Erben RG (2016) Excessive osteocytic Fgf23 secretion contributes to pyrophosphate accumulation and mineralization defect in Hyp mice. PLoS Biol 14(4):e1002427
Vervloet M (2019) Renal and extrarenal effects of fibroblast growth factor 23. Nat Rev Nephrol 15(2):109–120
Johnson ML, Kamel MA (2007) The Wnt signaling pathway and bone metabolism. Curr Opin Rheumatol 19(4):376–382
Amrein K, Dobnig H, Wagner D, Piswanger-Sölkner C, Pieber TR, Pilz S, Tomaschitz A, Dimai HP, Fahrleitner-Pammer A (2014) Sclerostin in institutionalized elderly women: associations with quantitative bone ultrasound, bone turnover, fractures, and mortality. J Am Geriatr Soc 62(6):1023–1029
Cejka D, Herberth J, Branscum AJ, Fardo DW, Monier-Faugere MC, Diarra D, Haas M, Malluche HH (2011) Sclerostin and Dickkopf-1 in renal osteodystrophy. Clin J Am Soc Nephrol 6(4):877–882
Araújo MJCLN, Bacelar Marques ID, Graciolli FG, Fukuhara L, Machado Dos Reis L, Custódio M, Jorgetti V, Elias RM, David-Neto E, Moysés RMA (2019) Comparison of serum levels with bone content and gene expression indicate a contradictory effect of kidney transplantation on sclerostin. Kidney Int 96(5):1100–1104
Pimentel A, Ureña-Torres P, Zillikens MC, Bover J, Cohen-Solal M (2017) Fractures in patients with CKD-diagnosis, treatment, and prevention: a review by members of the European Calcified Tissue Society and the European Renal Association of Nephrology Dialysis and Transplantation. Kidney Int 92(6):1343–1355
Kuo TH, Lin WH, Chao JY, Wu AB, Tseng C-C, Chang YT, Liou HH, Wang MC (2019) Serum sclerostin levels are positively related to bone mineral density in peritoneal dialysis patients: a cross-sectional study. BMC Nephrol 20(1):266
Cejka D, Jäger-Lansky A, Kieweg H, Weber M, Bieglmayer C, Haider DG, Diarra D, Patsch JM, Kainberger F, Bohle B, Haas M (2012) Sclerostin serum levels correlate positively with bone mineral density and microarchitecture in haemodialysis patients. Nephrol Dial Transplant 27(1):226–230
Thambiah S, Roplekar R, Manghat P, Fogelman I, Fraser WD, Goldsmith D, Hampson G (2012) Circulating sclerostin and Dickkopf-1 (DKK1) in predialysis chronic kidney disease (CKD): relationship with bone density and arterial stiffness. Calcif Tissue Int 90(6):473–480
Ishimura E, Okuno S, Ichii M, Norimine K, Yamakawa T, Shoji S, Nishizawa Y, Inaba M (2014) Relationship between serum sclerostin, bone metabolism markers, and bone mineral density in maintenance hemodialysis patients. J Clin Endocrinol Metab 99(11):4315–4320
Cosman F, Crittenden DB, Adachi JD, Binkley N, Czerwinski E, Ferrari S, Hofbauer LC, Lau E, Lewiecki EM, Miyauchi A, Zerbini CAF, Milmont CE, Chen L, Maddox J, Meisner PD, Libanati C, Grauer A (2016) Romosozumab Treatment in Postmenopausal Women with Osteoporosis. N Engl J Med 375(16):1532–1543
Brandenburg VM, Verhulst A, Babler A, D’Haese PC, Evenepoel P, Kaesler N (2019) Sclerostin in chronic kidney disease-mineral bone disorder think first before you block it! Nephrol Dial Transplant 34(3):408–414
Carrillo-López N, Panizo S, Alonso-Montes C, Román-García P, Rodríguez I, Martínez-Salgado C, Dusso AS, Naves M, Cannata-Andía JB (2016) Direct inhibition of osteoblastic Wnt pathway by fibroblast growth factor 23 contributes to bone loss in chronic kidney disease. Kidney Int 90(1):77–89
Sabbagh Y, Graciolli FG, O’Brien S, Tang W, dos Reis LM, Ryan S, Phillips L, Boulanger J, Song W, Bracken C, Liu S, Ledbetter S, Dechow P, Canziani ME, Carvalho AB, Jorgetti V, Moyses RM, Schiavi SC (2012) Repression of osteocyte Wnt/beta-catenin signaling is an early event in the progression of renal osteodystrophy. J Bone Miner Res 27(8):1757–1772
Evenepoel P, Bover J, Ureña-Torres P (2016) Parathyroid hormone metabolism and signaling in health and chronic kidney disease. Kidney Int 90(6):1184–1190
Staines KA, MacRae VE, Farquharson C (2012) The importance of the SIBLING family of proteins on skeletal mineralisation and bone remodelling. J Endocrinol 214(3):241–255
Rowe PSN (2012) Regulation of bone-renal mineral and energy metabolism: the PHEX, FGF23, DMP1, MEPE ASARM pathway. Crit Rev Eukaryot Gene Expr 22(1):61–86
Kong L, Wu H, Zhou W, Luo M, Tan Y, Miao L, Cai L (2015) Sirtuin 1: a target for kidney diseases. Mol Med 21(1):87–97
Zainabadi K, Liu CJ, Guarente L (2017) SIRT1 is a positive regulator of the master osteoblast transcription factor, RUNX2. PLoS ONE 5:e0178520
Feng Q, Zheng S, Zheng J (2018) The emerging role of microRNAs in bone remodeling and its therapeutic implications for osteoporosis. Biosci Rep 38(3):BSR20180453
Iimori S, Mori Y, Akita W, Kuyama T, Takada S, Asai T, Kuwahara M, Sasaki S, Tsukamoto Y (2012) Diagnostic usefulness of bone mineral density and biochemical markers of bone turnover in predicting fracture in CKD stage 5D patients–a single-center cohort study. Nephrol Dial Transplant 27(1):345–351
Naylor KL, Garg AX, Zou G, Langsetmo L, Leslie WD, Fraser LA, Adachi JD, Suzanne Morin S, Goltzman D, Lentle B, Jackson SA, Josse RG, Jamal SA (2015) Comparison of fracture risk prediction among individuals with reduced and normal kidney function. Clin J Am Soc Nephrol 10(4):646–653
West SL, Lok CE, Langsetmo L, Cheung AM, Szabo E, Pearce D, Fusaro M, Wald R, Weinstein J, Jamal SA (2015) Bone mineral density predicts fractures in chronic kidney disease. J Bone Miner Res 30(5):913–919
Yenchek RH, Iuuux JH, Shlipak MG, Bauer DC, Rianon NJ, Kritchevsky SB, Harris TB, Newman AB, Cauley JA, Fried LF (2012) Bone mineral density and fracture risk in older individuals with CKD. Clin J Am Soc Nephrol 7(7):1130–1136
Prasad B, Ferguson T, Tangri N, Ng CY, Nickolas TL (2019) Association of bone mineral density with fractures across the spectrum of chronic kidney disease: the regina CKD-MBD study. Can J Kidney Health Dis 6:2054358119870539
Hind K, Oldroyd B, Truscott JG (2010) In vivo precision of the GE Lunar iDXA densitometer for the measurement of total-body, lumbar spine, and femoral bone mineral density in adults. J Clin Densitom 13(4):413–417
Dusceac R, Niculescu DA, Dobre R, Dragne MD, Tacu C, Peride I, David C, Checherita I, Poiana C (2018) Chronic hemodialysis is associated with lower trabecular bone score, independent of bone mineral density: a case-control study. Arch Osteoporos 13(1):125
Naylor KL, Prior J, Garg AX, Berger C, Langsetmo L, Adachi JD, Goltzman D, Kovacs CS, Josse RG, Leslie WD (2016) Trabecular bone score and incident fragility fracture risk in adults with reduced kidney function. Clin J Am Soc Nephrol 11(11):2032–2040
Pocock N (2017) Use of dual energy X-ray absorptiometry, the trabecular bone score and quantitative computed tomography in the evaluation of chronic kidney disease-mineral and bone disorders. Nephrology (Carlton) 22(Suppl 2):19–21
Rampersad C, Whitlock RH, Leslie WD, Rigatto C, Komenda P, Bohm C, Hans D, Tangri N (2020) Trabecular bone score in patients with chronic kidney disease. Osteoporos Int 31(10):1905–1912
Ramalho J, Marques IDB, Hans D, Dempster D, Zhou H, Patel P, Pereira RMR, Jorgetti V, Moyses RMA, Nickolas TL (2018) The trabecular bone score: relationships with trabecular and cortical microarchitecture measured by HR-pQCT and histomorphometry in patients with chronic kidney disease. Bone 116:215–220
Fusaro M, D’Angelo A, Gallieni M (2008) Vertebral fractures in patients on dialysis: a clinically relevant problem with insufficient investigation. NDT Plus 1(6):464–465
Fusaro M, Aghi A, Mereu MC, Giusti A (2017) Fragility fracture in the Chronic Kidney Disease (CKD). G Ital Nefrol 34:2017-vol6
Gracia-Marco L, García-Fontana B, Ubago-Guisado E, Vlachopoulos D, García-Martín A, Muñoz-Torres M (2020) Analysis of bone impairment by 3D DXA hip measures in patients with primary hyperparathyroidism: a pilot study. J Clin Endocrinol Metab 105(1):dgz060
Ghesani N, Jung J, Patel S, Ramchand T (2013) Superscan caused by renal osteodystrophy: Observed on 18F FDG PET/CT scan. Indian J Nucl Med 28(4):251–252
Torres A, Lorenzo V, Gonzalez-Posada JM (1986) Comparison of histomorphometry and computerized tomography of the spine in quantitating trabecular bone in renal osteodystrophy. Nephron 44(4):282–287
Chen Z, Qureshi AR, Ripsweden J, Wennberg L, Heimburger O, Lindholm B, Barany P, Haarhaus M, Brismar TB, Stenvinkel P (2016) Vertebral bone density associates with coronary artery calcification and is an independent predictor of poor outcome in end-stage renal disease patients. Bone 92:50–57
Filgueira A, Carvalho AB, Tomiyama C, Higa A, Rochitte CE, Santos RD, Canziani ME (2011) Is coronary artery calcification associated with vertebral bone density in nondialyzed chronic kidney disease patients? Clin J Am Soc Nephrol 6(6):1456–1462
Jamal SA, Gilbert J, Gordon C, Bauer DC (2006) Cortical pQCT measures are associated with fractures in dialysis patients. J Bone Miner Res 21(4):543–548
Jamal S, Cheung AM, West S, Lok C (2012) Bone mineral density by DXA and HR pQCT can discriminate fracture status in men and women with stages 3 to 5 chronic kidney disease. Osteoporos Int 23(12):2805–2813
Bacchetta J, Boutroy S, Vilayphiou N, Juillard L, Guebre-Egziabher F, Rognant N, Sornay-Rendu E, Szulc P, Laville M, Delmas PD, Fouque D, Chapurlat R (2010) Early impairment of trabecular microarchitecture assessed with HR-pQCT in patients with stage II-IV chronic kidney disease. J Bone Miner Res 25(4):849–857
Cejka D, Patsch JM, Weber M, Diarra D, Riegersperger M, Kikic Z, Krestan C, Schueller-Weidekamm C, Kainberger F, Haas M (2011) Bone microarchitecture in hemodialysis patients assessed by HR-pQCT. Clin J Am Soc Nephrol 6(9):2264–2271
Paranhos-Neto FP, Lima GAC, Silva LC, Madeira M, Neto LV, Mendonça LMC, Lima ICB, Delgado AG, Leite M Jr, Gomes CP, Farias MLF (2018) HR-pQCT detects alterations in bone microstructure in men with CKD stages 3 and 4, which are influenced by hormonal changes and body composition. Clin Nephrol 89(1):10–17
Marques ID, Araújo MJ, Graciolli FG, Reis LM, Pereira RM, Custódio MR, Jorgetti V, Elias RM, David-Neto E, Moysés RM (2017) Biopsy vs. peripheral computed tomography to assess bone disease in CKD patients on dialysis: differences and similarities. Osteoporos Int 28(5):1675–1683
Salam S, Gallagher O, Gossiel F, Paggiosi M, Khwaja A, Eastell R (2018) Diagnostic accuracy of biomarkers and imaging for bone turnover in renal osteodystrophy. J Am Soc Nephrol 29(5):1557–1565
Nickolas TL (2018) The quest for better biomarkers of bone turnover in CKD. J Am Soc Nephrol 29:1353–1355
Crandall CJ, Vasan S, LaCroix A, LeBoff MS, Cauley JA, Robbins JA, Jackson RD, Bauer DC (2018) Bone turnover markers are not associated with hip fracture risk: a case-control study in the women’s health initiative. J Bone Miner Res 33(7):1199–1208
Link TM, Saborowski O, Kisters K, Kempkes M, Kosch M, Newitt D, Lu Y, Waldt S, Majumdar S (2002) Changes in calcaneal trabecular bone structure assessed with high-resolution MR imaging in patients with kidney transplantation. Osteoporos Int 13(2):119–129
Wehrli FW, Leonard MB, Saha PK, Gomberg BR (2004) Quantitative high-resolution magnetic resonance imaging reveals structural implications of renal osteodystrophy on trabecular and cortical bone. J Magn Reson Imaging 20(1):83–89
Bover J, Jara A, Trinidad P, Rodriguez M, Martin-Malo A, Felsenfeld AJ (1994) The calcemic response to PTH in the rat: effect of elevated PTH levels and uremia. Kidney Int 46(2):310–317
Bover J, Jara A, Trinidad P, Rodriguez M, Felsenfeld AJ (1999) Dynamics of skeletal resistance to parathyroid hormone in the rat: effect of renal failure and dietary phosphorus. Bone 25(3):279–285
Holloway-Kew KL, Rufus-Membere P, Anderson KB, Betson A, Gaston J, Kotowicz MA, Diez-Perez A, Hyde NK, Pasco JA (2020) Bone material strength index is associated with prior fracture in men with and without moderate chronic kidney disease. Bone 133:115241
Pérez-Sáez MJ, Prieto-Alhambra D, Díez-Pérez A, Pascual J (2018) Advances in the evaluation of bone health in kidney transplant patients. Nefrologia 38(1):27–33
Salam SN, Eastell R, Khwaja A (2014) Fragility fractures and osteoporosis in CKD: pathophysiology and diagnostic methods. Am J Kidney Dis 63(6):1049–1059
Khairallah P, Nickolas TL (2018) Management of osteoporosis in CKD. Clin J Am Soc Nephrol 13(6):962–969
Bover J, Ureña-Torres P, Mateu S, DaSilva I, Gràcia S, Sánchez-Baya M, Arana C, Fayos L, Guirado L, Cozzolino M (2020) Evidence in chronic kidney disease-mineral and bone disorder guidelines: is it time to treat or time to wait? Clin Kidney J 13(4):513–521
Wilson LM, Rebholz CM, Jirru E, Liu MC, Zhang A, Gayleard J, Chu Y, Robinson KA (2017) Benefits and harms of osteoporosis medications in patients with chronic kidney disease: a systematic review and meta-analysis. Ann Intern Med 166(9):649–658
Hara T, Hijikata Y, Matsubara Y, Watanabe N (2019) Pharmacological interventions for osteoporosis in people with chronic kidney disease stages 3–5D. Cochrane Datab Syst Rev. https://doi.org/10.1002/14651858.CD013424
Acknowledgements
We thank Mr Ricard Pellejero for his extremely valuable bibliographic assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest related to this topic. JB declares advisory/lecture fees and/or travel funding from Amgen, Abbvie, Sanofi-Genzyme, Shire, Vifor-Fresenius-Renal Pharma, and Sanifit. PUT declares advisory/lecture fees and/or travel funding from Abbvie, Amgen, Astellas, Medici, Sanofi, Vifor-Pharma FMC, and Hémotech. MC declares advisory/lecture fees from Amgen, Abbvie, Shire, Vifor-Pharma, and Baxter. CGA declares advisory/lecture fees and/or travel funding from Amgen, Kiowa-Kirin, and FAES.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jordi Bover, Pablo Ureña-Torres and Mario Cozzolino are members of the ERA-EDTA CKD-MBD Working Group.
Rights and permissions
About this article
Cite this article
Bover, J., Ureña-Torres, P., Cozzolino, M. et al. The Non-invasive Diagnosis of Bone Disorders in CKD. Calcif Tissue Int 108, 512–527 (2021). https://doi.org/10.1007/s00223-020-00781-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-020-00781-5