Abstract
The objective of the study was to determine the association between AAC and neuromuscular function over 5 years. Participants in this study were ambulant women over 70 years old residing in Perth, Western Australia who participated in the Calcium Intake Fracture Outcomes Study, a randomised controlled trial of calcium supplementation. 1046 women (mean age = 74.9 ± 2.6 years; BMI = 27.1 ± 4.4 kg/m2) were included. Lateral spine images captured during bone density testing were scored for AAC (AAC24; 0–24) at baseline. Severe AAC (AACsev) was defined using established cut points (AAC24 ≥ 6). At baseline and follow-up, isometric grip strength was assessed using a dynamometer. Mobility was assessed by the Timed-Up-and-Go (TUG) test. Using pre-defined criteria, muscle weakness was considered as grip strength < 22 kg and poor mobility defined as TUG > 10.2 s. A subset of women had appendicular lean mass (ALM) determined by dual-energy X-ray absorptiometry at baseline and follow-up (n = 261). AACsev was evident in 193 (18.5%) women. Average decline in grip strength after 5 years was greater in those with AACsev than those without (3.6 ± 3.7 vs. 2.9 ± 4.2 kg; p = 0.034). This remained significant after adjustment for age, treatment allocation, diabetes, smoking history, renal function, medical record-derived prevalent vascular disease, BMI and physical activity (β = − 0.184; 95% confidence interval: − 0.361, − 0.008; p = 0.040). AACsev was not associated with 5-year changes in TUG or ALM in univariable or multivariable analyses (all p > 0.05). In older women, severe aortic calcification was associated with greater 5-year decline in muscle strength, but not TUG or ALM. These findings support the concept that vascular disease may have an effect on the loss of muscular strength.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With advancing age, there is a progressive loss of muscle mass and function which promotes the onset of disability and increases the risk of falls and fractures [1]. Numerous factors are thought to promote this functional decline, including progressive worsening of co-morbidities such as diabetes and heart disease as well as lifestyle factors such as poor nutrient intake, smoking and reduced amounts of physical activity [2]. One area that has not been adequately described is the effects of vascular disease on the neuromuscular system.
Atherosclerotic vascular diseases also contribute to the development of functional decline. Calcification in the aorta is indicative of generalised atherosclerosis at other vascular beds and coronary artery calcification [3]. It is also associated with future cardiovascular events and deaths [4, 5]. Early abdominal aortic atherosclerotic lesions consisting of lipid-laden macrophages and vascular smooth muscle cells are common in adolescents and can either disappear or progress further to become more advanced atherosclerotic lesions [6]. Calcified abdominal aortic lesions are evidence of advanced atherosclerotic plaques that are easily visualised as raised areas by non-invasive imaging modalities [7]. Additionally, abdominal aortic calcification (AAC) may arise as a consequence of medial arteriosclerosis, or both processes can occur concurrently [8].
Epidemiological studies have reported that vascular calcification and musculoskeletal function are both predictive of fractures. Additionally, vascular calcification and musculoskeletal function may share common biological pathways [9]. The composition of calcified atherosclerotic lesions shares some features of bone. Similarly, the biological processes involved in vascular calcification share a number of features with age-related musculoskeletal decline such as decreased endothelial expression of the vitamin D receptor and downregulation of sclerostin in tissue [10, 11].
Recent studies implicate vascular disease as a contributor to age-related changes in muscle. A previous cross-sectional study of healthy older men and women demonstrated that the presence and severity of AAC was associated with low muscle mass [12]. Functional decline likely precedes and may even exceed rates of loss of muscle mass during ageing [13], but the association between AAC and physical function and decline is unknown. Previous observational studies of advanced atherosclerosis (such as carotid intima-media thickness and arterial stiffness) have shown that these surrogates of advanced atherosclerosis are higher in individuals with low handgrip strength [14] and that walking speeds and mobility decline with the presence of arterial plaques [15, 16]. However, it is unclear if AAC is a cause or consequence of functional decline based on these observations. We therefore sought to determine whether AAC measured at a single time point was associated with functional decline in a population of community-dwelling older women over 5 years.
Methods
This study was a secondary analysis of the Calcium Intake Fracture Outcome Study (CAIFOS) [17]. Participants in this study were originally recruited in 1998 for a 5-year, double-blind, randomised controlled trial (RCT) of daily calcium supplementation to prevent osteoporotic fracture, whose recruitment strategy has been detailed elsewhere [17]. Briefly, women aged 70 years and older were recruited from the general population in Western Australia. Of the 5586 women approached, 1500 were recruited into the study. All participants were ambulant, did not receive medication or have co-morbidities that could affect bone metabolism. Participants received 1.2 g of calcium carbonate daily or a matching placebo.
For the present study, participants who had AAC24 scores assessed from lateral spine dual-energy X-ray absorptiometry (DXA) scans at entry to the study at baseline in 1998 (n = 207) or 1999 (n = 839), and muscle strength and mobility assessed at baseline and the 5 year follow-up from their initial study visit in 2003, were included (total n = 1046) (Fig. 1). All participants completed anthropometry and a validated food frequency questionnaire [18]. Creatinine was measured using an isotope dilution mass spectrometry (IDMS) traceable Jaffe kinetic assay on a Hitachi 917 analyzer (Roche Diagnostics GmbH, Mannheim Germany). Estimated glomerular filtration rate (eGFR) using creatinine and cystatin C was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) [19]. Impaired renal function was defined as an eGFR < 60 mL/min/1.73 m2. Prevalent atherosclerotic vascular disease (ASVD) was determined by atherosclerotic hospitalisations which were retrieved from the Western Australian Data Linkage System (WADLS) for each of the study participants. Prevalent atherosclerotic disease were defined using the principal Hospital discharge diagnosis codes with a lookback period of approximately 18 years depending on the date of clinic visit (1980 to date of clinical visit) from the International Classification of Diseases, Injuries and Causes of Death Clinical Modification (ICD-9-CM) [21]. These codes included ischemic heart disease (ICD-9-CM codes 410–414); heart failure (ICD-9-CM code 428); cerebrovascular disease excluding haemorrhage (ICD-9-CM codes 433–438); and peripheral arterial disease (ICD-9-CM codes 440–444). Diabetes status was determined by the medical history of study participants and verified by their primary care provider where possible. These data were coded using the International Classification of Primary Care—Plus (ICPC-Plus) method [20]. The coding methodology allows aggregation of different terms for similar pathologic entities as defined by the International Classification of Diseases and related Health Problems, 10th Revision (ICD-10) coding system. These data were then used to determine the presence of pre-existing diabetes (T89001-90009).
Hand grip strength was determined using a Jamar hand dynamometer (Lafayette Instrument Company, USA). Three repeated measures were taken for each hand and the highest recorded strength in the dominant hand was considered the maximum grip strength. Muscle weakness was defined as a maximum grip strength < 22 kg, as this threshold identified clinically relevant weakness in older women [21]. Mobility was assessed by the timed up and go (TUG) test, in which a participant was timed while rising from a chair, walking 3 m, turning and returning to sit on the chair. A TUG time > 10.2 s was considered to be slow, and was referred to as “mobility impairment”. This threshold was previously shown to be predictive of fractures in older women [1]. Physical activity was assessed by a demographic questionnaire where participants reported their type of activity and hours per week to the question “Please list any sports recreation or regular physical activity, including walking, that you undertook in the last 3 months” [22]. The energy cost of such activities is given in METs (1 MET accounts for an individual’s basal metabolic rate and equals ~ 1 kcal/kg/h). Activity levels (kcal/day) were calculated by multiplying frequency, duration, energy cost of the activities and the body weight of individuals [23]. Total cholesterol concentrations were determined using a Hitachi 917 auto analyser (Roche diagnostics). Plasma 25OHD2 and 25OHD3 concentrations were determined using a validated LC-MS/MS (Liquid Chromatography Tandem Mass Spectrometry) method at the RDDT Laboratories (Bundoora, VIC, Australia) according to published methodology and summed to obtained total plasma 25OHD concentration for each individual [24]. Between-run coefficients of variation (CVs) were 10.1% at a 25OHD2 mean concentration of 12 nmol/L and 11.3% at a 25OHD3 mean concentration of 60 nmol/L. These were categorised into normal (≥ 50 nmol/L), insufficient (< 50 nmol/L) and deficient (< 25 nmol/L). All AAC scores from 0 to 24 were derived from digitally enhanced lateral single-energy images of the thoraco-lumbar spine using a Hologic 4500A bone densitometer (Hologic, Bedford, MA, USA). A single experienced investigator (JTS) read all images using the validated semi quantitative scoring system [25]. The use of DXA to detect AAC has been validated against radiography where inter-class correlation coefficient between two readers on DXA was high (0.89: 0.80–0.94) and comparable to radiography (0.92; 0.88–0.95) [26]. Two other studies have shown similar agreement between methods [27, 28]. The AAC24 point system scores aortic calcification relative to each vertebral height (L1–L4) and is scored as 0 (no calcification), 1 (< one-third of the aortic wall), 2 (> one-third to two-thirds of the aortic wall) or 3 (> two-thirds of the aortic wall) for both the anterior and posterior aortic walls giving a maximum possible score of up to 24. Severity of AAC was also categorised using previously published groupings: low (AAC24 score 0 or 1); moderate (AAC24 score 2–5); and severe (AAC24 score > 5). AAC was categorised as not severe (AAC24 score ≤ 5) or severe (AAC24 score > 5). In those women who had AAC measured, 261 had appendicular lean mass (ALM) determined by whole-body dual-energy X-ray absorptiometry (DXA) (Hologic, Bedford, MA, USA) at baseline and again at 5 years [29].
Statistical Analyses
Normally distributed variables were reported as mean ± standard deviation (SD), non-normally distributed variables were presented as median and interquartile range (IQR), while categorical variables were reported as frequency and percentage. Comparison of demographic, physical and clinical variables stratified by AAC severity was performed using t test, Mann–Whitney U test, χ2 test or Mantel–Haenszel Chi-squared test for trend as appropriate to data distribution. Given that the aortic calcification score is not normally distributed, Spearman’s rank correlation and age-adjusted partial correlation statistics were calculated for the correlation between calcification scores and functional measures, energy expenditure and anthropometric measures. Logistic regression models were constructed to determine if severe AAC was cross-sectionally associated with muscle weakness or mobility impairment at baseline. Linear regression models were constructed to determine if severe AAC was cross-sectionally associated with handgrip strength or TUG at baseline. Further, linear regression models were constructed to determine if severe AAC was associated with 5-year changes in handgrip strength or TUG. All regression models were constructed first as a minimally adjusted model controlling for age and treatment allocation and subsequently adjusted for body mass index (BMI) and relevant risk factors which included diabetes status, smoking status, ASVD, renal function and metabolic equivalents. As only a subset of women had ALM both at baseline and follow-up (n = 261), these analyses were repeated in women with these measures stratified by skeletal muscle mass to determine if changes in physical function may be attributable to underlying conditions already affecting muscle mass. Low muscle mass was considered to be an ALM relative to BMI less than 0.512 in line with the Foundation for National Institute of Health (FNIH) definition of sarcopenia [30]. Regression coefficients are presented as the standard deviation increases/decreases in outcome associated with having severe AAC. All data were analysed using STATA v14.2 [StataCorp, 4905 Lakeway Dr College Station, TX, USA]. Values were considered statistically significant if p < 0.05 and if the 95% confidence interval (95% CI) did not cross unity.
Results
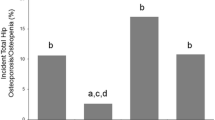
Baseline data are shown in Table 1. Evidence of any calcification was seen in 762 (73%) of individuals and severe calcification (AAC24 score > 5) was evident in 193 (18%) individuals. Grip strength weakness, defined as maximum grip strength < 22 kg, was evident in 629 women (60.1%) and 32.6% had mobility impairment (n = 341) defined as a TUG time > 10.2 s. Of those women with severe AAC, the frequency of allocation to calcium treatment was 45.6% (n = 88/193) and this did not differ significantly (p = 0.331) from those women with not severe AAC (49.4%; n = 422/853). There were no differences in total cholesterol or vitamin D status amongst women with and without severe AAC.
Individuals with severe AAC were significantly older, had lower mean BMI, upper arm girth, triceps skin folds, and were more likely to be smokers, have ASVD, and use statins, low-dose aspirin, and any cardiovascular medication. Neither grip strength nor TUG time at baseline differed between those with and without severe AAC (Table 1). There were no significant correlations for AAC24 scores with baseline handgrip strength, TUG or ALM. AAC24 was negatively but weakly correlated with baseline BMI in an age-adjusted partial correlation model (r = − 0.067; p = 0.030) (Table 2).
One hundred and twenty-six women did not have grip strength recorded and 130 women did not have TUG recorded at follow-up. These women were slightly older (75.3 ± 2.8 vs. 74.8 ± 2.5 years; p = 0.052) but were not heavier (BMI = 27.2 ± 5.1 vs. 27.1 ± 4.3 kg/m2; p = 0.792). In addition, women lost to follow-up had a lower baseline grip strength (19.7 ± 4.8 vs. 20.8 ± 4.7; p = 0.019) and a slower baseline TUG (10.4 ± 2.9 vs. 9.5 ± 2.6; p = 0.005). In women with follow-up functional measures, the median reduction in grip strength over 5 years was 3.0 kg (interquartile range: − 5.5 to − 0.75 kg; n = 920). The average decline in grip strength in individuals with severe AAC (3.6 ± 3.7 kg) was greater than in those without (2.9 ± 4.2 kg) (p = 0.034). The median increase in TUG times was 1.26 s (IQR: − 0.02, 2.64; n = 917). However, the average change in TUG times was similar between individuals with and without severe AAC. There were no significant correlations for AAC24 scores with change from baseline in handgrip strength or TUG (Table 2).
In minimally adjusted regression analyses controlling for age and treatment, and a fully adjusted model controlling for important risk factors, having severe AAC at baseline was associated with a greater decline in grip strength over 5 years (Table 3). Excluding outliers the results remained unchanged [standardised β = − 0.176 (95% confidence interval: − 0.337, − 0.015) p = 0.032]. After adjusting instead for upper arm girth (as a proxy for muscle mass in the arm), the association remained significant (β = − 0.187; − 0.363, − 0.011; p = 0.037). In a subgroup analysis including only women with ALM measurements and adjusting for ALM and not BMI, the association trended towards significance (β = − 0.226; − 0.487, 0.034; p = 0.088) (Table 3). For women with a relative muscle mass above the FNIH threshold (n = 194), AAC was associated with accelerated five-year declines in handgrip strength (Table 4). Additional adjustment for vitamin D status at baseline did not alter findings (Supplementary Table 1). Additional adjustment for total cholesterol attenuated the regression coefficients and trended towards significance (Supplementary Table 1).
Discussion
In this longitudinal analysis of older women who participated in a randomised controlled trial of calcium supplementation on fracture outcomes, we determined that having severe aortic calcification (measured at a single time point) was associated with 5-year declines in grip strength after accounting for multiple co-morbidities. Interestingly, having severe AAC was not associated with 5-year declines in mobility or ALM. Overall, these findings suggest that detection of AAC in individuals, a robust indicator of cardiovascular disease and easily detectable on routine lateral spine imaging, may identify these individuals as being at a greater risk of muscle strength decline and thus may benefit from interventions to improve muscular strength. Interestingly, no association was evident regarding the association between AAC and ALM (likely due to low power) and this may suggest that any affects of AAC on muscular strength may be related more to neuromuscular factors and not muscle atrophy per se. Thus, it is unclear if vascular calcification has a direct or indirect effect, or both, on muscular strength. Aortic calcification promotes aortic stiffening which can lead to a multitude of adverse effects on peripheral blood vessels and the neuromuscular system. In skeletal muscle, arteries supplying this tissue absorb most of the pulsatile energy content of propagating pressure and flow waveforms proximal to the capillaries. Sustained high central (aortic) stiffness reduces the protective stiffness gradients usually present between the heart and periphery and thus amplify the transfer of excessive, potentially harmful pulsatile energy into the periphery and tissues sensitive to high-flow and low-impedance such as the neuromuscular junction possibly impacting on efficient neuromuscular function [31]. Furthermore, occlusion of large vessels can restrict or diminish blood and thus nutrient supply to other conduit vessels hampering the proper functioning of limbs, resulting in functional decline [32]. Vascular calcification may be reflective of poor lifestyle behaviours and therefore physical decline may be inevitable but accelerated in these individuals. Other indirect factors such as circulating proteins regulating bone metabolism (for example sclerostin and Wnt signalling molecules), as well as inflammatory mediators (such as TNF-α and IL-6), may help explain the relationship demonstrated in this study as these factors are involved in both calcification and the loss of muscle mass and function [33,34,35,36]. We investigated a number of circulating factors including total cholesterol and also the vitamin D status of individuals. Adjustment for vitamin D status did not change the association; however, inclusion of cholesterol in analyses slightly attenuated the strength of the association and widened the confidence intervals, given the smaller sample size having data on cholesterol (n = 734–736/1046). Thus, these results may indicate a possibility of confounding by cholesterol, although there is no known direct physiologic connection between cholesterol and muscle strength, which would be needed to consider cholesterol a confounder. It is more likely the smaller sample size led to the slight reduction in statistical significance.
To our knowledge, no previous study has directly investigated the association of AAC and muscular strength. The present data support a previous study in older men (mean age at baseline approximately 77 years), in which greater carotid intima-media thickness (cIMT) at baseline was associated with lower handgrip strength at follow-up four years later [37]. The cIMT is a measure of atherosclerotic burden in the carotid artery and may represent both deposition of plaque on the intimal surface of the vascular wall as well as inflammatory and calcific infiltrates in the medial layer of the vascular wall [38]. No association was observed between cIMT and physical performance (determined by the short physical performance battery), or activities of daily living either at baseline or follow-up which aligns with observations from the present study. Further, despite reporting the change in cIMT from baseline to follow-up and having functional measures at baseline and follow-up, no data were reported on the association of changes in cIMT and changes in functional measures over time making it difficult to infer if worsening subclinical atherosclerosis parallels declines in physical function suggestive of a shared relationship. Another observational study of healthy middle-aged men and women (mean age approximately 47 years) has reported an inverse association between arm extensibility and the sit-and-reach test with cIMT [39]. In high-functioning middle-aged adults (mean age approximately 43 years), cIMT was higher in individuals in the lowest quartile of handgrip strength and systolic flow velocity (a measure of vessel resistance) [14]. Some literature, however, has reported no association between handgrip strength and atherosclerosis and thus the literature regarding the possible effect of vascular calcification and atherosclerosis on physical function is mixed [40]. It is interesting to note that the mean age of participants in studies reporting poor physical function as a risk factor for ASVD appears to be substantially lower than in studies reporting prevalent ASVD as a risk factor for poor physical function. That is to say that the effects of physical function on ASVD appear to become less pronounced over time (i.e. physical function contributes more to vascular risk in middle age and that in older age, prevalent vascular disease contributes to functional decline). This concept is supported by studies in autopsies of individuals 2–15 years old which have revealed that the prevalence of fibrotic/atherosclerotic lesions is as high as 20% [41]. The effects of these lesions in early life would likely accumulate such that small decrements in blood supply and sustained central stiffness impacting on neuromuscular function throughout the life course may manifest as clinically relevant functional deficits in middle age. At this point, a vicious cycle would likely ensue in which poor physical function would promote further vascular deterioration from an inability/difficulty in performing a sufficient amounts of physical exertion in a manner that would favourably evoke endothelial cell nitric oxide production, inhibit sympathetic nerve activity and ultimately allow for adequate tissue perfusion [42, 43]. Manifest vascular disease has already been demonstrated to negatively impact physical fitness and exercise capacity [44]. This may promote the progression of subclinical vascular disease to overt, clinically significant macrovascular disease due to a lack of physical activity from compromised cardio-respiratory fitness.
A previous study demonstrated that calcification in the coronary artery was associated with 9-year declines in walking speeds in older adults (mean age approximately 62 years), and in another study of older adults (mean age approximately 73 years) free of known cardiovascular disease, carotid plaque burden was associated with greater 12-month increases in TUG [15, 16]. However, in the present study we observed no association between AAC and TUG times as a continuous variable or between AAC and having mobility impairment (a TUG time > 10.2 s) at baseline or at follow-up. Also, AAC was not a significant predictor of 5-year changes in TUG. Associations of AAC may be more closely related to more discrete assessments of muscle function such as handgrip strength which involves markedly fewer muscle groups and less neuromuscular involvement.
Individuals in the present study, while not having sustained a clinical cardiovascular event, were likely to have subclinical cardiovascular disease as evidenced by the relatively high prevalence of cardio-protective medications. Exercise is commonly recommended in those with identified cardiovascular disease as part of disease management. Exercise, particularly resistance training, has proven benefits in improving muscular strength and physical function in all age groups and is safe and effective in the elderly frail [45]. Thus, those with identified AAC may benefit from muscular strength training to both improve cardiovascular risk and prevent functional decline. In a previous study, but not in this study, we identified a cross-sectional relationship between AAC severity and low relative muscle mass [12]. In this study, lean muscle mass was only available in a small subset which may have reduced power to have detected a significant association. Nevertheless, these data demonstrate that AAC may be independently related to muscle mass and function.
There are a number of important limitations to this study that must be considered when interpreting the results. Firstly, as this was an observational study, we cannot infer causality. Secondly, this study was limited by measurement of calcification at only one time point. Given an association between AAC and changes in handgrip strength was evident, it may be more informative to determine if changes in calcification correlate with changes in physical function. Given the advanced age of this cohort, it is likely that aortic calcification is already well established. Thirdly, the participants in this cohort were Caucasian women aged over 70 years and thus the results may not be generalisable to older men and non-Caucasian populations. Therefore, longitudinal analyses conducted in cohorts of men and women at an earlier age are needed to investigate if functional decline precedes the development/progression of AAC or vice versa. This is particularly important as men and women have different profiles of functional decline and cardiovascular risk during ageing. Fourth, other performance assessments, such as the 400-m walk test, may assist in clarifying the association between AAC and physical function. Fifth, DXA, while a useful tool to determine body composition, does not adequately separate out non-muscle contributors to lean mass such as fibrous tissue and water and is probably best suited to determining fat mass. Finally, we only observed modest and inconsistent associations between AAC and functional measures meaning our findings should be interpreted cautiously particularly considering some women were lost to follow-up. These women had poorer baseline functional measures meaning that we may have underestimated the true effect in this population.
In conclusion, older women with severe AAC experienced decline in handgrip strength, a measure of muscular weakness, independent of established risk factors. As such, this study supports other evidence for a potential muscle function–vascular calcification relationship. Women identified to have severe AAC may be at risk of functional decline and thus may also likely benefit from interventions aimed at promoting physical function. Future studies with longitudinal measures of AAC and comprehensive muscle phenotypes are needed to elucidate potential mechanisms. These studies should include both men and women to validate these findings.
References
Zhu K, Devine A, Lewis JR et al (2011) Timed up and go test and bone mineral density measurement for fracture prediction. Arch Intern Med 171:1655. https://doi.org/10.1001/archinternmed.2011.434
Hebert R, Brayne C, Spiegelhalter D Factors associated with functional decline and improvement in a very elderly community-dwelling population. Am J Epidemiol 150:501–510
Lewis JR, Schousboe JT, Lim WH et al (2016) Abdominal aortic calcification identified on lateral spine images from bone densitometers are a marker of generalized atherosclerosis in elderly women. Arterioscler Thromb Vasc Biol 36:166–173. https://doi.org/10.1161/ATVBAHA.115.306383
Lewis JR, Schousboe JT, Lim WH et al (2018) Long-term atherosclerotic vascular disease risk and prognosis in elderly women with abdominal aortic calcification on lateral spine images captured during bone density testing: a prospective study. J Bone Miner Res. https://doi.org/10.1002/jbmr.3405
Schousboe JT, Taylor BC, Kiel DP et al (2007) Abdominal aortic calcification detected on lateral spine images from a bone densitometer predicts incident myocardial infarction or stroke in older women. J Bone Miner Res 23:409–416. https://doi.org/10.1359/jbmr.071024
Jayalath RW, Mangan SH, Golledge J (2005) Aortic calcification. Eur J Vasc Endovasc Surg 30:476–488. https://doi.org/10.1016/j.ejvs.2005.04.030
Schousboe JT, Lewis JR, Kiel DP (2017) Abdominal aortic calcification on dual-energy X-ray absorptiometry: methods of assessment and clinical significance. Bone 104:91–100
Tanimura A, McGregor DH, Anderson HC (1983) Matrix vesicles in atherosclerotic calcification. Proc Soc Exp Biol Med 172:173–177
Szulc P, Blackwell T, Kiel DP et al (2015) Abdominal aortic calcification and risk of fracture among older women—the SOF study. Bone 81:16–23. https://doi.org/10.1016/j.bone.2015.06.019
Krishna SM, Seto S-W, Jose RJ et al (2017) Wnt signaling pathway inhibitor sclerostin inhibits angiotensin II–induced aortic aneurysm and atherosclerosis highlights. Arterioscler Thromb Vasc Biol 37:553–566. https://doi.org/10.1161/ATVBAHA.116.308723
Xiang W, Liao W, Yi Z et al (2017) 25-Hydroxyvitamin D-1-α-hydroxylase in apoliporotein E knockout mice: the role of protecting vascular smooth muscle cell from calcification. Biomed Pharmacother 88:971–977. https://doi.org/10.1016/j.biopha.2017.01.093
Rodriguez AJ, Scott D, Khan B et al (2016) Low relative lean mass is associated with increased likelihood of abdominal aortic calcification in community-dwelling older Australians. Calcif Tissue Int 99:340–349
Delmonico MJ, Harris TB, Visser M et al (2009) Longitudinal study of muscle strength, quality, and adipose tissue infiltration. Am J Clin Nutr 90:1579–1585. https://doi.org/10.3945/ajcn.2009.28047
Park J, Park H (2017) Muscle strength and carotid artery flow velocity is associated with increased risk of atherosclerosis in adults. Cardiol J 24:385–392. https://doi.org/10.5603/CJ.a2017.0007
Abizanda Soler P, Paterna Mellinas G, Martín Sebastiá E et al (2010) Aterosclerosis subclínica, un predictor de limitación funcional al año en ancianos con alto nivel funcional: estudio Albacete. Rev Esp Geriatr Gerontol 45:125–130. https://doi.org/10.1016/j.regg.2009.09.005
Everson-Rose SA, Mendes de Leon CF, Roetker NS et al (2018) Subclinical cardiovascular disease and changes in self-reported mobility: multi-ethnic study of atherosclerosis. J Gerontol Ser A 73:218–224. https://doi.org/10.1093/gerona/glx103
Prince RL, Devine A, Dhaliwal SS et al (2006) Effects of calcium supplementation on clinical fracture and bone structure. Arch Intern Med 166:869. https://doi.org/10.1001/archinte.166.8.869
Hodge A, Patterson AJ, Brown WJ et al (2000) The anti cancer council of Victoria FFQ: relative validity of nutrient intakes compared with weighed food records in young to middle-aged women in a study of iron supplementation. Aust N Z J Public Health 24:576–583
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Britt H, Scahill S, Miller G (1997) ICPC PLUS© for community health? A feasibility study. Health Inf Manag 27:171–175. https://doi.org/10.1177/183335839802700406
Duchowny KA, Peterson MD, Clarke PJ (2017) Cut points for clinical muscle weakness among older Americans. Am J Prev Med 53:63–69. https://doi.org/10.1016/j.amepre.2016.12.022
Devine A, Dhaliwal SS, Dick IM et al (2004) Physical activity and calcium consumption are important determinants of lower limb bone mass in older women. J Bone Miner Res 19:1634–1639. https://doi.org/10.1359/JBMR.040804
McArdle WD, Katch FI, Katch VL (1996) Exercise physiology: energy, nutrition, and human performance. Williams & Wilkins, Philadelphia
Maunsell Z, Wright DJ, Rainbow SJ (2005) Routine isotope-dilution liquid chromatography-tandem mass spectrometry assay for simultaneous measurement of the 25-hydroxy metabolites of vitamins d2 and D3. Clin Chem 51:1683–1690. https://doi.org/10.1373/clinchem.2005.052936
Kauppila LI, Polak JF, Cupples LA et al (1997) New indices to classify location, severity and progression of calcific lesions in the abdominal aorta: a 25-year follow-up study. Atherosclerosis 132:245–250
Schousboe JT, Wilson KE, Kiel DP (2006) Detection of abdominal aortic calcification with lateral spine imaging using DXA. J Clin Densitom 9:302–308
Schousboe JT, Wilson KE, Hangartner TN (2007) Detection of aortic calcification during vertebral fracture assessment (VFA) compared to digital radiography. PLoS ONE 2(8):e715
Golestani R, Tio RA, Zeebregts CJ et al (2010) Abdominal aortic calcification detected by dual X-ray absorptiometry: a strong predictor for cardiovascular events. Ann Med 42:539–545
Radavelli-Bagatini S, Zhu K, Lewis JR et al (2013) Association of dairy intake with body composition and physical function in older community-dwelling women. J Acad Nutr Diet 113:1669–1674. https://doi.org/10.1016/j.jand.2013.05.019
Studenski SA, Peters KW, Alley DE et al (2014) The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol Ser A 69:547–558. https://doi.org/10.1093/gerona/glu010
Mitchell GF (2008) Effects of central arterial aging on the structure and function of the peripheral vasculature: implications for end-organ damage. J Appl Physiol 105:1652–1660. https://doi.org/10.1152/japplphysiol.90549.2008
Efstratiadis G, Kirmizis D, Papazoglou K et al (2004) The walking man with a completely occluded aorta. Nephrol Dial Transplant 19:227–229. https://doi.org/10.1093/ndt/gfg379
Brack AS, Conboy MJ, Roy S et al (2007) Increased Wnt signaling during aging alters muscle stem cell fate and increases fibrosis. Science 317:807–810. https://doi.org/10.1126/science.1144090
Pickering M-E, Simon M, Sornay-Rendu E et al (2017) Serum sclerostin increases after acute physical activity. Calcif Tissue Int 101:170–173. https://doi.org/10.1007/s00223-017-0272-5
Han XH, Jin Y-R, Tan L et al (2014) Regulation of the follistatin gene by RSPO-LGR4 signaling via activation of the WNT/-catenin pathway in skeletal myogenesis. Mol Cell Biol 34:752–764. https://doi.org/10.1128/MCB.01285-13
Schaap LA, Pluijm SMF, Deeg DJH, Visser M (2006) Inflammatory markers and loss of muscle mass (Sarcopenia) and strength. Am J Med 119:526-e9. https://doi.org/10.1016/j.amjmed.2005.10.049
Den Ouden MEM, Schuurmans MJ, Arts EMA et al (2013) Atherosclerosis and physical functioning in older men, a longitudinal study. J Nutr Health Aging 17:97–104. https://doi.org/10.1007/s12603-012-0424-2
Hellings WE, Peeters W, Moll FL et al (2010) Composition of carotid atherosclerotic plaque is associated with cardiovascular outcome: a prognostic study. Circulation 121:1941–1950. https://doi.org/10.1161/CIRCULATIONAHA.109.887497
Suwa M, Imoto T, Kida A et al (2018) Association of body flexibility and carotid atherosclerosis in Japanese middle-aged men: a cross-sectional study. BMJ Open 8:e019370. https://doi.org/10.1136/bmjopen-2017-019370
Shimizu Y, Sato S, Koyamatsu J et al (2017) Handgrip strength and subclinical carotid atherosclerosis in relation to platelet levels among hypertensive elderly Japanese. Oncotarget 8:69362–69369. https://doi.org/10.18632/oncotarget.20618
Berenson GS, Srinivasan SR, Bao W et al (1998) Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. N Engl J Med 338:1650–1656. https://doi.org/10.1056/NEJM199806043382302
DiCarlo SE, Stahl LK, Bishop VS (1997) Daily exercise attenuates the sympathetic nerve response to exercise by enhancing cardiac afferents. Am J Physiol Circ Physiol 273:H1606–H1610. https://doi.org/10.1152/ajpheart.1997.273.3.H1606
Green D, Cheetham C, Mavaddat L et al (2002) Effect of lower limb exercise on forearm vascular function: contribution of nitric oxide. Am J Physiol Circ Physiol 283:H899–H907. https://doi.org/10.1152/ajpheart.00049.2002
Williams MC, Murchison JT, Edwards LD et al (2014) Coronary artery calcification is increased in patients with COPD and associated with increased morbidity and mortality. Thorax 69:718–723. https://doi.org/10.1136/thoraxjnl-2012-203151
Reid KF, Martin KI, Doros G et al (2015) Comparative effects of light or heavy resistance power training for improving lower extremity power and physical performance in mobility-limited older adults. J Gerontol Ser A 70:374–380. https://doi.org/10.1093/gerona/glu156
Acknowledgements
The authors would like to thank all the participants of the CAIFOS study and all study personnel involved in data collection and the operation of the study.
Author information
Authors and Affiliations
Contributions
AJR: Study concept and design, data analysis, interpretation of data and manuscript preparation. JRL: Interpretation of data and manuscript preparation. DSS: Interpretation of data and manuscript preparation. DPK: Interpretation of data and manuscript preparation. JTS: Acquisition of data, interpretation of data and manuscript preparation. PRE: Interpretation of data and manuscript preparation. RLP: Study concept and design, acquisition of data, interpretation of data and manuscript preparation.
Corresponding author
Ethics declarations
Conflict of interest
Alexander J. Rodríguez, Joshua R. Lewis, David S. Scott, Douglas P. Kiel, John T. Schousboe, Peter R. Ebeling and Richard L. Prince declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
Trial registration: Australian New Zealand Clinical Trials Registry ACTRN12615000750583. The study conformed to all ethical requirements according to the Human Research Ethics Committee of the Western Australian Department of Health (DOHWA HREC), project number #2009/24. All participants gave informed consent.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rodríguez, A.J., Lewis, J.R., Scott, D.S. et al. Aortic Calcification is Associated with Five-Year Decline in Handgrip Strength in Older Women. Calcif Tissue Int 103, 589–598 (2018). https://doi.org/10.1007/s00223-018-0458-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-018-0458-5