Abstract
The inhibition of proliferation or functional alteration of osteoblasts by glucocorticoids (GCs) has been recognized as an important etiology of GC-induced osteoporosis (GIO). Connexin 43 (Cx43) is the most abundant connexin isoform in bone cells and plays important roles in bone remodeling. Despite the important role of Cx43 in bone homeostasis and the prevalence of GIO, the direct action of GCs on Cx43 expression in osteoblasts has been poorly described. The aim of the present study was to evaluate how GCs affect Cx43 expression in osteoblasts. Dexamethasone (Dex) treatment decreased expression of Cx43 RNA and protein in MC3T3-E1 mouse osteoblastic cells. Reduction of Cx43 expression by Dex was dependent on the glucocorticoid receptor (GR), as it was abolished by pretreatment with a GR blocker. Treatment with PTH (1–34), a medication used for GIO management, counteracted the suppression of Cx43 by Dex. Akt or mTOR signaling modulators revealed the involvement of the Akt/mTOR signaling pathway in Dex-induced reduction of Cx43 expression. Moreover, overexpression of Cx43 significantly attenuated Dex-inhibited cell viability and proliferation, as evidenced by MTT and bromodeoxyuridine (BrdU) incorporation assay of MC3T3-E1 cells. To account for possible species or cell type differences, human primary osteoblasts were treated with Dex and similar downregulation of Cx43 by Dex was observed. In addition, immunofluorescent staining for Cx43 further demonstrated an apparent decrease in Dex-treated human osteoblasts, while analysis of lucifer yellow propagation revealed reduced gap junction intercellular communication by Dex. Collectively, these findings indicate that GCs suppress Cx43 expression in osteoblasts via GR and the Akt/mTOR signaling pathway and overexpression of Cx43 may, at least in part, rescue osteoblasts from GC-induced reductions in proliferation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glucocorticoids (GCs) are a powerful tool used to treat a range of human illnesses, including autoimmune diseases and cancer, and to prevent rejection following organ transplantation [1]. However, the side effects of GCs are a major drawback, and one of the most severe is GC-induced osteoporosis (GIO). GIO is considered to be the most common form of iatrogenic osteoporosis and secondary osteoporosis [2]. Bone loss and an increased rate of fractures occur early after the initiation of GC therapy, and are then related to dosage and treatment duration [3]. Moreover, despite similar bone mineral density (BMD) levels, patients receiving GCs are at greater risk of fracture than patients suffering from other forms of osteoporosis [4]. Aging is also associated with endogenous hyperglucocorticoidism [5].
The skeleton is a dynamic system, and undergoes continuous remodeling after full development to maintain structural integrity, mechanical competence, and mineral homeostasis [6]. Control of bone modeling and remodeling requires a tightly orchestrated interplay among osteoblasts, osteocytes, and osteoclasts [6]. Although osteoclast numbers and bone resorption rapidly increase during the initial disease phase of GIO, bone resorption then decreases to sub-physiological levels, but persistent and severe inhibition of bone formation leads to further bone loss and progressively increased fracture risk [7, 8]. Thus, the inhibition of proliferation or functional alteration of osteoblasts by GCs has been recognized as an important etiology of GIO.
Gap junctions have long been considered important in their role as membrane channels, but it is now clear that the proteins that form these channels, connexins, are multi-modal in their structure and function [9]. Connexin 43 (Cx43), the most abundant connexin in bone cells, is expressed in osteoblasts, osteocytes, and osteoclasts [10] and is required for full differentiation and function of cells of both osteoblastic and osteoclastic lineages and for the maintenance of osteocyte viability [11, 12]. Missense mutations in human Cx43 result in an autosomal dominant disorder called oculodentodigital dysplasia (ODDD) [13]. Patients with ODDD exhibit major skeletal malformations and craniofacial abnormalities [14]. Conventional Cx43 knockout mice die prenatally. Osteoblast-enriched cultures from calvaria of Cx43-deficient mice exhibit reduced expression of marker genes and stunted mineralization in vitro, which are associated with poor cell-to-cell diffusion of negatively charged dyes [15]. In addition, modulation of Cx43 in osteoblasts could impact growth factor responses and signal transduction cascades, leading to altered gene expression and osteoblast function [16, 17]. Moreover, a recent study using osteoblast/osteocyte-specific ablation of the Cx43 gene in a mouse model confirmed reduced cortical bone thickness and density [18, 19].
Cx43 also plays an important role in the effect of anti-osteoporotic medications such as parathyroid hormone (PTH) (1–34) or bisphosphonate. PTH increases gap junctional communication between osteoblasts by modulating Cx43 expression or function [20]. Mice lacking Cx43 in osteoblastic cells exhibit a deficient response to intermittent PTH administration [21]. In vivo, Cx43 is required for the anti-apoptotic effect of bisphosphonates on osteocytes and osteoblasts [22].
Although GIO is prevalent disease and evidence for the role Cx43 in bone homeostasis is accumulating, the direct effect of GCs on Cx43 expression in osteoblasts, as far as we know, has not been well described. In the current study, we examined whether Cx43 expression in MC3T3-E1 cells or human primary osteoblasts was affected by GC treatment and evaluated the involvement of corresponding signaling pathways.
Materials and Methods
Materials
Antibodies against Cx43, Akt, phospho-Akt (p-Akt), mTOR, and phospho-mTOR (p-mTOR) were obtained from Cell Signaling Technology (Danvers, MA, USA) and rabbit anti-GAPDH antibody from Bioworld Technology (Dublin, OH, USA). Alexa 568 anti-rabbit antibody, CAS-Block, and ProLong Gold Antifade Reagent with DAPI were from Life Technologies (Carlsbad, CA, USA). Dex was purchased from Santa Cruz Biotechnology. Akt activator (SC79) was obtained from Tocris (Bristol, UK). Rapamycin was obtained from Cayman (Ann Arbor, Michigan, USA). Torin 1, mTOR activator (MHY1485), human recombinant PTH (1–34), and other reagents were obtained from Sigma-Aldrich (St. Louis, MO, USA) or Life Technologies.
Cell Culture
MC3T3-E1 mouse osteoblastic cells were obtained from the American-Type Culture Collection (Rockville, MD, USA). Cells were cultured in α-MEM supplemented with 10 % fetal bovine serum (FBS; Life Technologies), 100 U/ml penicillin, and 100 µg/ml streptomycin. Human primary osteoblasts from the knee joint and femoral head were purchased from PromoCell (Heidelberg, Germany). These cells were each obtained from a single donor and stored in a liquid nitrogen tank at passage 2. The osteoblasts were grown in osteoblast growth culture medium (PromoCell) supplemented with 10 % FBS (Life Technologies). The medium was replaced every 2 days and the cultured cells were frozen at passages 4–8. For the experiments, cells were thawed and grown in M199 medium (Sigma-Aldrich) supplemented with 10 % FBS and 2 mM GlutaMAX (Life Technologies). All cell cultures were kept at 37 °C in a humidified 5 % CO2 incubator.
Quantitative Real-Time PCR (qRT-PCR)
Total RNA was extracted using the FavorPrep Blood/Cultured Cell Total RNA Purification Mini Kit (Favorgen, Ping Tung, Taiwan) according to the manufacturer’s instructions. The QuantiTect Reverse Transcription Kit (Qiagen, Germantown, MD, USA) was used to synthesize cDNA from total RNA according to the manufacturer’s protocol. The qRT-PCR reaction mixture consisted of 20 ng reverse-transcribed RNA, 200 nM forward and reverse primers, and 2× SYBR Green PCR Master Mix (Applied Biosystems, Carlsbad, CA) in a final volume of 10 μl. Primers were as follows: GGCGTGAGGAAAGTACCAAA (forward) and ACGCCAAGTGATTGAACTCC (reverse) for Cx43, CTGGGACCCAACTGGTAAGA (forward) and CCTGTTATGCTGTGGGGACT (reverse) for RPS3 in primary human osteoblasts, GGCGTGAGGAAAGTACCAAA (forward) and AGCTTTGAGCAGGAATCCAA (reverse) for Cx43, CCTCCAGGAAACCTTTGACA (forward) and AGGGCTGGATCTCAAACTCA (reverse) for RUNX2, AAGCTGGGAAGAACACTCCA (forward) and TCCAAACAGGAGAGCCACTT (reverse) for alkaline phosphatase (ALP), and TACAGCTTCACCACCACAGC (forward) and TCTCCAGGGAGGAAGAGGAT (reverse) for β-actin in MC3T3-E1 cells. PCR reactions were carried out using an ABI Prism 7900HT Sequence Detection System (Applied Biosystems) with the following program: 95 °C for 15 min, 94 °C for 15 s, and 57 °C for 30 s for 40 cycles. Relative RNA levels were calculated by comparison to RPS3 or β-actin RNA levels using a comparative cycle threshold method [23].
Western Blotting
Whole cell lysates were prepared in a radioimmunoprecipitation assay (RIPA) lysis buffer (ELPIS, Taejon, Republic of Korea) containing 50 mM Tris–HCl, pH 7.5, 150 mM NaCl, 1 % NP-40, 0.5 % deoxycholic acid, 0.1 % sodium dodecyl sulfate, and 1 mM phenylmethylsulfonyl fluoride. Protein concentrations were determined using bicinchoninic acid solution (Sigma-Aldrich). Samples were subjected to 10 % SDS-PAGE and then transferred onto a PVDF membrane (Bio-Rad, Munich, Germany). Immunoblotting was performed using primary antibodies against Cx43, Akt, phospho–Akt (Ser473), mTOR, phospho-mTOR (Ser2448), and GAPDH followed by horseradish peroxidase-conjugated anti-rabbit IgG secondary antibody (Amersham Pharmacia, San Francisco, CA, USA). Signals were visualized with a chemiluminescent detection kit (GE Healthcare, London, UK). Band images were obtained using Fusion FX7 (Peqlab, Torcy, France) and quantitative image analysis was performed using Image J software (National Institutes of Health, Bethesda, MD, USA).
Preparation of Recombinant Adenovirus
Adenoviruses containing Cx43 (Ad-Cx43) were kindly provided by Dr. Seul (University of Chicago) [24]. Recombinant replication-defective adenoviruses containing β-galactosidase (Ad-lacZ) were used as a control. HEK293 cells were used for virus transfection and amplification. Viruses from the culture supernatants of HEK 293 cells with cytopathogenic effects were purified by cesium chloride banding. Adenovirus infection of MC3T3-E1 cells was performed using a multiplicity of infection (MOI) of 400. After 24 h of infection with either an Ad-LacZ or an Ad-Cx43, cells were subcultured into 96-well and 6-well plates to perform the MTT assay and Western blotting, respectively.
Cell Viability Assay
Viability of the osteoblasts was determined by MTT assay, which is based on the ability of mitochondrial dehydrogenases to oxidize thiazolyl blue (MTT), a tetrazolium salt (3-[4,5-dimethylthiazole-2-yl]-2,5-diphenyltetrazolium bromide), to an insoluble blue formazan product. Cells were incubated with MTT (5 mg/ml) at 37 °C for 2 h. After the supernatant was removed, 100 μl of DMSO was added to each well and the optical density of the solution was detected using a VERSA MAX Microplate Reader (Molecular Devices, Sunnyvale, CA) at a wavelength of 570 nm. Cell viability was expressed as a ratio relative to control cells.
Cell Apoptotic Assays
Apoptotic cell death was determined via staining cells with annexin V-fluorescein isothiocyanate (FITC; Invitrogen Life Technologies, Camarillo, CA, USA; Ex/Em = 488/519 nm). MC3T3-E1 cells were seeded onto six-well plates and transfected using adenovirus (Ad-Lacz or Ad-Cx43. After 48 h, cells were exposed to Dex for 24 h. The cells were then washed twice with cold PBS and resuspended in 300 μl of binding buffer (10 mM HEPES/NaOH pH 7.4, 140 mM NaCl, 2.5 mM CaCl2). Annexin V-FITC (5 μl) and propidium iodide (PI) (1 μg/ml) were then added and the cells were analyzed with a BD FACS Canto II Flow Cytometer (Becton–Dickinson, NJ, USA).
Cell Proliferation Assays
Cell proliferation was measured by incorporation of bromodeoxyuridine (BrdU). After 24-h transfection by adenovirus (Ad-LacZ or Ad-Cx43), MC3T3-E1 cells were seeded onto 96-well plates for 24 h and then exposed to Dex. After 24 h, BrdU labeling solution was added with fresh medium for 16 h and BrdU incorporation was determined with a BrdU Labeling and Detection Kit III (Roche Diagnostics, Mannheim, Germany) according to the manufacturer’s protocol.
Confocal Microscopy
Human primary osteoblasts were grown to 80 % confluence in 2-well chambered dishes (SPL, Pocheon, Korea) and treated with DMSO (control) or Dex for 24 h. Next, the cells were fixed in 4 % paraformaldehyde in PBS for 20 min and then permeabilized with 0.5 % saponin in PBS for 15 min. After 10-min incubation with chemical block solution (Life Technologies), the cells were incubated with anti-Cx43 antibody (1:250 dilution; Cell Signaling) for 1 h at room temperature, washed in PBS, and then incubated with secondary antibody conjugated with Alexa Fluor 568 for 1 h. Finally, the cells were rinsed with PBS and mounted with ProLong Gold Antifade Reagent with DAPI. The cells were visualized with a Zeiss LSM 510 confocal laser scanning microscope (Carl Zeiss, Göttingen, Germany).
Assessment of Gap Junction Intercellular Communication (GJIC) by Dye Transfer Assay
Cells were grown to confluence in 6-well culture dishes. To determine the effects of Dex on gap junction intercellular communication (GJIC) between human osteoblasts, a scrape loading and dye transfer assay, based on monitoring the transfer of lucifer yellow fluorescent dye from one cell into the adjacent cell via functional gap junctions, was performed [25]. After the medium was removed, the cells were rinsed three times with pre-warmed Hanks’ balanced salt solution (HBSS), and then 1 ml of a 0.05 % lucifer yellow solution in calcium- and magnesium-free HBSS was added to each well. The cell monolayer was scraped with a scalpel blade. After incubation for 5 min, the cells were thoroughly washed with HBSS to remove background fluorescence and fixed with 3.7 % (v/v) formaldehyde in PBS for 15 min. Two drops of 90 % (v/v) glycerol were added to each well and covered with a glass coverslip. The cells were photographed with a Zeiss Axiophot fluorescence microscope equipped with a digital camera under blue excitation (450–490 nm).
Data Analysis
Data in this study are shown as mean ± standard error of the mean (SEM) of at least three independent experiments. Comparisons among groups were analyzed by Student’s t test. For all experiments, a p value less than 0.05 was considered statistically significant.
Results
Dex Decreases Expression of Cx43 RNA and Protein in MC3T3-E1 Cells
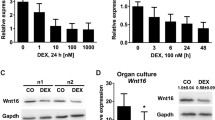
To examine whether Dex affects the expression of Cx43 RNA, MC3T3E1 cells were first treated with 10, 100 nM, and 1 μM concentrations of Dex for 4 h. As shown in Fig. 1a, all doses of Dex resulted in a significant reduction in Cx43 RNA expression compared with the control. To evaluate the time course, we treated cells with 100 nM Dex for 8 or 24 h, with controls. Cx43 downregulation by 100 nM Dex was sustained for 24 h (Fig. 1b). Western blot analyses also revealed that levels of Cx43 protein were significantly decreased at the dose of 10, 100 nM, and 1 μM of Dex 8 h after treatment (Fig. 1c). We also examined the Cx43 protein response to Dex 100 nM at 2 and 4 h and showed that the protein level started to decrease at 4 h after Dex treatment (Fig. 1d).
Dex suppresses Cx43 expression in MC3T3-E1 cells. MC3T3-E1 cells were treated with a Dex for 4 h or b Dex for 8 and 24 h. Total RNA was isolated from the cells and Cx43 RNA expression was measured by quantitative real-time PCR and normalized against β-actin. Values are presented as mean ± SEM of three independent experiments. c MC3T3-E1 cells were treated with Dex for 8 h or d Dex for 2, 4, and 8 h. Cx43 protein levels from treated cell lysates were analyzed by Western blotting and normalized against GAPDH. Band density values are presented as mean ± SEM of three independent experiments. *p < 0.05 versus control
Glucocorticoid Receptor (GR) Blockage or PTH (1–34) Treatment Prevents Dex-Induced Downregulation of Cx43 in MC3T3-E1 Cells
To examine whether GR is involved in Dex-induced Cx43 expression, RU486, a GR blocker, was used. As shown in Fig. 2a, pretreatment with RU486 significantly prevented the decrease of Cx43 expression caused by 10 or 100 nM Dex in MC3T3-E1 cells, indicating GR-dependent action of Dex in Cx43 downregulation. When the RU486-only treatment group was compared with the control group, no statistically significant differences were detected. Next, we determined whether treatment with PTH (1–34) affects Dex-induced downregulation of Cx43. Cells pretreated with PTH (1–34) for 1 h were subjected to see Cx43 expression with Dex or without Dex for 4 h. PTH (1–34) treatment duration was determined based on its short plasma half-life of 1 h and a total peptide exposure duration of approximately 4 h in intermittent PTH administration in humans [26]. Pretreatment with PTH (1–34) counteracted the suppression of Cx43 RNA and protein levels by Dex (Fig. 2b, c). In addition, consistent with previous findings [27, 28], PTH (1–34) significantly upregulated Cx43 RNA and protein levels. Among osteoblast genes such as RUNX2 and ALP, ALP RNA expression also showed significant increases with PTH (1–34) treatment.
Glucocorticoid receptor (GR) blockage and PTH (1–34) treatment prevent Dex-induced downregulation of Cx43 in MC3T3-E1 cells. a After 1 h pretreatment with GR agonist RU486, MC3T3-E1 cells were treated with Dex for 8 h. Cx43 protein levels of from treated cell lysates were analyzed by Western blotting and normalized against GAPDH. Band density values are presented as mean ± SEM of three independent experiments. b After 1 h pretreatment with PTH (1–34), MC3T3-E1 cells were treated with Dex for 4 h. Cx43 protein levels from treated cell lysates were analyzed by Western blotting and normalized against GAPDH. Band density values are presented as mean ± SEM of three independent experiments. c Total RNA was isolated from the cells and RUNX2 and ALP RNA expression as well as Cx43 RNA was measured by quantitative real-time PCR and normalized against β-actin. Values are presented as mean ± SEM of four independent experiments. *p < 0.05; **p < 0.01 versus the Dex-treated group, † p < 0.05; †† p < 0.01 versus control
Dex Reduces Akt/mTOR Phosphorylation and Akt/mTOR Modulators Affect Cx43 Expression in MC3T3-E1 Cells
To elucidate the molecular mechanisms responsible for Cx43 downregulation of Dex, we examined the Akt signaling pathway by considering the inhibiting effect of GCs on Akt in osteoblasts [29]. Dex treatment caused a significant decrease in Akt phosphorylation in MC3T3-E1 cells (Fig. 3a). The role of Akt in Dex-induced Cx43 downregulation was evaluated using an inhibitor or activator of Akt. LY294002 is a PI3K inhibitor and thus blocks PI3K-dependent Akt phosphorylation. Treatment of MC3T3-E1 cells with LY294002 reduced Cx43 expression dose-dependently (Fig. 3b). In contrast, treatment with SC79, a specific Akt activator, induced significant upregulation of Cx43 expression with concordant Akt activation (Fig. 3c). To further confirm the signaling pathway, we measured mTOR activation by Dex, as mTOR is one molecule of the Akt signaling pathway. Significant reductions in mTOR phosphorylation were seen at 10, 100 nM, and 1 μM doses of Dex, respectively (Fig. 3a). The effects of mTOR modulators on Cx43 expression were further investigated. The mTOR inhibitors rapamycin and Torin 1 reduced Cx43 expression in MC3T3-E1 cells, while MHY1485, an mTOR activator, induced upregulation of Cx43 with stimulated mTOR phosphorylation (Fig. 3d, e). Collectively, these findings suggest that Akt/mTOR signaling plays a role in the regulation of Cx43 expression by Dex in MC3T3-E1 cells.
Dex reduces Akt/mTOR phosphorylation and Akt/mTOR modulators affect Cx43 expression in MC3T3-E1 cells. MC3T3-E1 cells were treated with a Dex for 8 h, b Akt inhibitor LY294002 for 4 h, c Akt activator SC79 5 µM for the indicated time, d mTOR inhibitors rapamycin (1 μM) and torin 1 (250 nM) for 4 h, and e mTOR activator MHY1485 (2 μM) for the indicated time period. Protein levels of Cx43, phospho-Akt, and phospho-mTOR from treated cell lysates were analyzed by Western blotting and normalized against GAPDH, total Akt and mTOR, respectively. Band density values are presented as mean ± SEM of three independent experiments. *p < 0.05; **p < 0.01 versus control
Enhanced Cx43 Expression Attenuates Dex-Induced Cell Viability and Reduces Cell Proliferation
As shown in Fig. 4a, Dex significantly reduced cell viability at 24, 48, and 72 h both dose- and time-dependently. To investigate whether enhanced Cx43 expression could improve the viability of osteoblasts treated with Dex, MC3T3-E1 cells were infected with Ad-Cx43 (Fig. 4b) and the MTT assay was used to analyze cell viability. As shown in Fig. 4c, Cx43 overexpression in MC3T3-E1 cells significantly attenuated the viability reduction induced by 1 μM Dex compared to Ad-LacZ-infected cells at 24, 48, and 72 h. We also tested whether Cx43 overexpression affects anti-proliferative or pro-apoptotic action by Dex. Fluorescence-activated cell sorting (FACS) analysis of annexin V/PI staining was used to identify apoptotic cells and the BrdU incorporation assay was used for cell proliferation analysis. Dex significantly increased apoptosis in Ad-lacZ-infected MC3T3-E1 cells in accordance with previous studies. Compared with Dex-treated Ad-lacZ-infected cells, Dex-treated Ad-Cx43-infected cells had a lower mean apoptosis value, but this did not reach statistical significance (Fig. 4d). On the other hand, Dex-treated Ad-Cx43-infected cells showed significant attenuation of reductions in BrdU incorporation compared with Dex-treated Ad-lacZ-infected cells (Fig. 4e), suggesting a protective role for Cx43 against reduced proliferation in osteoblasts by Dex.
Enhanced Cx43 expression attenuates Dex-induced reductions in cell viability and proliferation. a MC3T3-E1 cells were treated with Dex for the indicated time period and cell viability was measured via MTT assay. Values are presented as mean ± SEM of three independent experiments. *p < 0.05; **p < 0.01 versus control. b MC3T3-E1 cells were infected with Ad-LacZ or Ad-Cx43 and Cx43 expression was determined by Western blotting. Representative images of experiments repeated three times are shown. c After infection by Ad-LacZ or Ad-Cx43 for 24 h, MC3T3-E1 cells were treated with 1 μM Dex for the indicated time periods. MTT assay was performed separately indicated each time and d FACS analysis of annexin V/PI staining and e BrdU incorporation assay was performed 24 h after Dex treatment. MTT assay data are from three independent experiments and FACS analysis data of annexin V/PI staining and BrdU incorporation assay are from four independent experiments. Values are presented as mean ± SEM. *p < 0.05; **p < 0.01 versus Dex-treated Ad-LacZ, NS non-significant, † p < 0.05 versus Ad-LacZ control
Dex Downregulates Cx43 Expression and PTH (1–34) Attenuates Dex-Induced Cx43 Reduction in Human Primary Osteoblasts
To evaluate possible variation in the effects of GCs on Cx43 according to species or cell type, we treated human primary osteoblasts with Dex. Dex treatment exhibited the same trend seen in MC3T3-E1 cells, reduced expression of Cx43 RNA or protein (Fig. 5a, b, c). Immunofluorescent staining of primary human osteoblasts with a Cx43 antibody revealed immunoreactivity on the plasma membrane as well as the intracytoplasmic region (Fig. 5d). The distribution of Cx43 in the cell membrane and intracytoplasmic region was shown and 100 nM Dex treatment for 24 h significantly reduced the immunofluorescent staining intensity of Cx43 in both regions, suggesting that Cx43 expression is downregulated by Dex (Fig. 5d).
Dex downregulates Cx43 expression and PTH (1–34) attenuates Dex-induced reductions of Cx43 in human primary osteoblasts. Human primary osteoblasts were treated with a Dex for 4 h and b Dex for 8 and 24 h. Total RNA was isolated from the cells and Cx43 RNA expression was measured by quantitative RT-PCR and normalized against RPS3. Values are presented as mean ± SEM of three independent experiments. *p < 0.05; **p < 0.01 versus control. c Human primary osteoblasts cells were treated with Dex for 8 h. Cx43 protein levels from treated cell lysates were analyzed by Western blotting and normalized against GAPDH. Band density values are presented as mean ± SEM of three independent experiments. **p < 0.01 versus control. d Representative images of four independent immunofluorescent staining procedures for Cx43 on confocal microscopy (×600). Human primary osteoblasts were treated with Dex 100 nM or control for 24 h. e Representative images of four independent lucifer yellow dye transfers on fluorescent microscopy (×100). Human primary osteoblasts were treated with 100 nM Dex or control for 24 h. f After 1 h pretreatment with Dex, human primary osteoblasts were treated with PTH (1–34) for 4 h. Cx43 protein levels from treated cell lysates were analyzed by Western blotting and normalized against GAPDH. Band density values are presented as mean ± SEM of three independent experiments. *p < 0.05; **p < 0.01 versus the Dex-treated group. † p < 0.05 versus control
Moreover, Dex perturbed GJIC (Fig. 5e). Lucifer yellow dye transfer was used to determine gap junction permeability to small molecules in Dex-treated osteoblasts. This dye transfer experiment examined the distance or amount of fluorescent dye moved from the central scrape line. Lucifer yellow propagation decreased after Dex treatment in human primary osteoblasts compared with that of control groups. Representative photomicrographs are shown in Fig. 5e. Attenuation of Dex-induced downregulation of Cx43 expression by PTH (1–34) was also seen in human primary osteoblasts (Fig. 5f).
Discussion
The deleterious effects of GC excess in bone result from direct activity on osteoblasts and their progenitors, osteocytes, and osteoclasts as well as indirect actions of GCs [5]. The rapid and profound suppression of bone formation by GCs is caused by potent suppression of osteoblastogenesis, a decrease in mature osteoblast function, diversion of mesenchymal stem cells to the adipocyte lineage, and the promotion of osteoblastic cell cycle arrest and apoptosis [30–32]. This study observed a clear influence of GCs on Cx43 expression via GR in osteoblasts.
Cx43 deletion driven by the alpha1 collagen promoter results in low BMD, thin cortical bone, decreased bone strength, and attenuated response to PTH and mechanical loading, whereas Cx43 deletion in mature osteoblasts using a human-osteocalcin-driven promoter does not yield abnormalities in bone mass [21, 22, 33]. Thus, the role of Cx43 in osteoblasts may depend on differentiation stage, although a recent study found slightly lower bone mass as a result of increased bone resorption and osteoclastogenesis in osteoblast and osteocyte specific Cx43 deficient mice using an osteocalcin Cre-lox system [34]. However, there is accumulating evidence for the role of Cx43 in osteoblast and osteocyte differentiation, survival, and function [11]. Unlike the effects on bone mass and on cancellous bone in particular, the consequences in cortical bone have been reproduced in mice lacking Cx43 in osteochondroprogenitors, immature osteoblasts, mature osteoblasts, and even osteocytes [19, 35, 36]. In addition, stimuli that increase bone mass have been shown to increase Cx43 expression, localization in the cell membrane, activation of gap junctions, and hemichannel activity [37]. Furthermore, PTH (1–34), the only currently available anabolic anti-osteoporotic agent with a treatment duration limited to 2 years due to osteosarcoma risk, counteracted the inhibition of Cx43 by Dex in osteoblasts. It will be interesting to determine the underlying mechanism by which Cx43 is involved in osteoblast proliferation or function in response to GCs.
Cx43 in osteoblasts and osteocytes indirectly modulates skeletal muscle growth and function, potentially via an undercarboxylated isoform of osteocalcin, indicating that Cx43 is involved in bone-muscle crosstalk [18]. Indeed, myopathy is an indirect effect of GCs on the skeleton. GC-induced muscle weakness is one determinant of the risk of falls and fractures in GIO patients [38]. Altogether, the Cx43 downregulation following GC treatment of mouse MC3T3-E1 cells and human primary osteoblasts shown in this study may result in harmful effects on the skeleton through osteoblast dysfunction or by compromising bone-muscle crosstalk. However, more research is required to understand the pathophysiological role of Cx43 changes caused by GCs in bone.
The inhibition of PI3K/Akt signaling results in a decrease in Cx43 mRNA and protein levels in MC3T3E1 cells [39]. We confirmed this reaction with a PI3K inhibitor, LY294002. In addition, we demonstrated that GC inhibited Akt and activation of the downstream signaling molecule mTOR. mTOR functions in two distinct protein complexes, namely mTORC1 and mTORC2 [40]. Although we did not examine the specific involvement of the mTORC1 or mTORC2 pathway in Cx43 expression in the present study, rapamycin or torin1 was shown to decrease Cx43 expression, indicating that mTOR signaling is involved in Cx43 expression.
As findings of the last decade have uncovered, Cx43 not only functions in the communication between bone cells and their extracellular milieu, but also serves as a scaffolding protein that associates with structural and signaling molecules, leading to regulation of intracellular signaling independent of channel activity [11, 41]. Its subcellular localization, including surrounding the cell nucleus as well as in non-junctional plasma membranes of osteoblasts and osteocytes, supports a potential role of Cx43 in functions beyond its role in gap junction communication in bone [11]. In this study, primary human osteoblasts exhibited an ability to transfer lucifer yellow, which indicates functional gap junctions. Although a clear decrease in dye transfer was shown after Dex treatment, our immunofluorescent staining of human osteoblasts also supports findings of a subcellular location surrounding the cell nucleus, indicating a possible role beyond that of intercellular transmission of small molecules.
In summary, GC treatment can affect Cx43 expression in MC3T3-E1 cells and human primary osteoblasts. Furthermore, we provide evidence for the involvement of Akt/mTOR in Dex-mediated Cx43 downregulation and for Cx43 overexpression-related rescue of GC-induced reductions in cell proliferation in MC3T3-E1 cells. Although the efficacy of anti-osteoporotic drugs such as bisphosphonate or PTH (1–34) in preventing and treating GIO has been shown in randomized controlled clinical trials, there remains an unmet need for fracture prevention in GIO. GC-specific mechanisms related to increased fracture risk are needed to identify more efficient prevention and treatment strategies. Improved understanding of the pathophysiologic role of Cx43 downregulation by GCs may lead to more specific therapeutic targets for bone under conditions of excess GCs.
References
Ferris HA, Kahn CR (2012) New mechanisms of glucocorticoid-induced insulin resistance: make no bones about it. J Clin Invest 122:3854–3857
Shi J, Wang L, Zhang H, Jie Q, Li X, Shi Q, Huang Q, Gao B, Han Y, Guo K, Liu J, Yang L, Luo Z (2015) Glucocorticoids: dose-related effects on osteoclast formation and function via reactive oxygen species and autophagy. Bone 79:222–232
Briot K, Roux C (2015) Glucocorticoid-induced osteoporosis. RMD Open 1:e000014
Kanis JA, Johansson H, Oden A, Johnell O, de Laet C, Melton IL, Tenenhouse A, Reeve J, Silman AJ, Pols HA, Eisman JA, McCloskey EV, Mellstrom D (2004) A meta-analysis of prior corticosteroid use and fracture risk. J Bone Miner Res 19:893–899
Manolagas SC (2010) From estrogen-centric to aging and oxidative stress: a revised perspective of the pathogenesis of osteoporosis. Endocr Rev 31:266–300
Civitelli R (2008) Cell-cell communication in the osteoblast/osteocyte lineage. Arch Biochem Biophys 473:188–192
Frenkel B, White W, Tuckermann J (2015) Glucocorticoid-induced osteoporosis. Adv Exp Med Biol 872:179–215
O’Brien CA, Jia D, Plotkin LI, Bellido T, Powers CC, Stewart SA, Manolagas SC, Weinstein RS (2004) Glucocorticoids act directly on osteoblasts and osteocytes to induce their apoptosis and reduce bone formation and strength. Endocrinology 145:1835–1841
Matsuuchi L, Naus CC (2013) Gap junction proteins on the move: connexins, the cytoskeleton and migration. Biochim Biophys Acta 1828:94–108
Civitelli R, Beyer EC, Warlow PM, Robertson AJ, Geist ST, Steinberg TH (1993) Connexin43 mediates direct intercellular communication in human osteoblastic cell networks. J Clin Invest 91:1888–1896
Plotkin LI, Bellido T (2013) Beyond gap junctions: connexin43 and bone cell signaling. Bone 52:157–166
Pacheco-Costa R, Davis HM, Sorenson C, Hon MC, Hassan I, Reginato RD, Allen MR, Bellido T, Plotkin LI (2015) Defective cancellous bone structure and abnormal response to PTH in cortical bone of mice lacking Cx43 cytoplasmic C-terminus domain. Bone 81:632–643
Lloyd SA, Loiselle AE, Zhang Y, Donahue HJ (2013) Connexin 43 deficiency desensitizes bone to the effects of mechanical unloading through modulation of both arms of bone remodeling. Bone 57:76–83
Paznekas WA, Boyadjiev SA, Shapiro RE, Daniels O, Wollnik B, Keegan CE, Innis JW, Dinulos MB, Christian C, Hannibal MC, Jabs EW (2003) Connexin 43 (GJA1) mutations cause the pleiotropic phenotype of oculodentodigital dysplasia. Am J Hum Genet 72:408–418
Lecanda F, Warlow PM, Sheikh S, Furlan F, Steinberg TH, Civitelli R (2000) Connexin43 deficiency causes delayed ossification, craniofacial abnormalities, and osteoblast dysfunction. J Cell Biol 151:931–944
Lima F, Niger C, Hebert C, Stains JP (2009) Connexin43 potentiates osteoblast responsiveness to fibroblast growth factor 2 via a protein kinase C-delta/Runx2-dependent mechanism. Mol Biol Cell 20:2697–2708
Niger C, Buo AM, Hebert C, Duggan BT, Williams MS, Stains JP (2012) ERK acts in parallel to PKCdelta to mediate the connexin43-dependent potentiation of Runx2 activity by FGF2 in MC3T3 osteoblasts. Am J Physiol Cell Physiol 302:C1035–1044
Shen H, Grimston S, Civitelli R, Thomopoulos S (2015) Deletion of connexin43 in osteoblasts/osteocytes leads to impaired muscle formation in mice. J Bone Miner Res 30:596–605
Bivi N, Condon KW, Allen MR, Farlow N, Passeri G, Brun LR, Rhee Y, Bellido T, Plotkin LI (2012) Cell autonomous requirement of connexin 43 for osteocyte survival: consequences for endocortical resorption and periosteal bone formation. J Bone Miner Res 27:374–389
Civitelli R, Ziambaras K, Warlow PM, Lecanda F, Nelson T, Harley J, Atal N, Beyer EC, Steinberg TH (1998) Regulation of connexin43 expression and function by prostaglandin E2 (PGE2) and parathyroid hormone (PTH) in osteoblastic cells. J Cell Biochem 68:8–21
Chung DJ, Castro CH, Watkins M, Stains JP, Chung MY, Szejnfeld VL, Willecke K, Theis M, Civitelli R (2006) Low peak bone mass and attenuated anabolic response to parathyroid hormone in mice with an osteoblast-specific deletion of connexin43. J Cell Sci 119:4187–4198
Plotkin LI, Lezcano V, Thostenson J, Weinstein RS, Manolagas SC, Bellido T (2008) Connexin 43 is required for the anti-apoptotic effect of bisphosphonates on osteocytes and osteoblasts in vivo. J Bone Miner Res 23:1712–1721
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(−ΔΔC(T)) Method. Methods 25:402–408
Han JH, Kim KA, Shah A, Park BH, Park WH, Kim SH (2010) Regulation of renin release by connexin 43 in As 4.1 cell line. Peptides 31:899–902
el-Fouly MH, Trosko JE, Chang CC (1987) Scrape-loading and dye transfer. A rapid and simple technique to study gap junctional intercellular communication. Exp Cell Res 168:422–430
Satterwhite J, Heathman M, Miller PD, Marin F, Glass EV, Dobnig H (2010) Pharmacokinetics of teriparatide (rhPTH[1-34]) and calcium pharmacodynamics in postmenopausal women with osteoporosis. Calcif Tissue Int 87:485–492
Schiller PC, Roos BA, Howard GA (1997) Parathyroid hormone up-regulation of connexin 43 gene expression in osteoblasts depends on cell phenotype. J Bone Miner Res 12:2005–2013
Mitchell JA, Ou C, Chen Z, Nishimura T, Lye SJ (2001) Parathyroid hormone-induced up-regulation of connexin-43 messenger ribonucleic acid (mRNA) is mediated by sequences within both the promoter and the 3′untranslated region of the mRNA. Endocrinology 142:907–915
Almeida M, Han L, Ambrogini E, Weinstein RS, Manolagas SC (2011) Glucocorticoids and tumor necrosis factor alpha increase oxidative stress and suppress Wnt protein signaling in osteoblasts. J Biol Chem 286:44326–44335
Weinstein RS, Jilka RL, Parfitt AM, Manolagas SC (1998) Inhibition of osteoblastogenesis and promotion of apoptosis of osteoblasts and osteocytes by glucocorticoids. Potential mechanisms of their deleterious effects on bone. J Clin Invest 102:274–282
Kauh E, Mixson L, Malice MP, Mesens S, Ramael S, Burke J, Reynders T, Van Dyck K, Beals C, Rosenberg E, Ruddy M (2012) Prednisone affects inflammation, glucose tolerance, and bone turnover within hours of treatment in healthy individuals. Eur J Endocrinol 166:459–467
Henneicke H, Gasparini SJ, Brennan-Speranza TC, Zhou H, Seibel MJ (2014) Glucocorticoids and bone: local effects and systemic implications. Trends Endocrinol Metab 25:197–211
Grimston SK, Brodt MD, Silva MJ, Civitelli R (2008) Attenuated response to in vivo mechanical loading in mice with conditional osteoblast ablation of the connexin43 gene (Gja1). J Bone Miner Res 23:879–886
Zhang Y, Paul EM, Sathyendra V, Davison A, Sharkey N, Bronson S, Srinivasan S, Gross TS, Donahue HJ (2011) Enhanced osteoclastic resorption and responsiveness to mechanical load in gap junction deficient bone. PLoS ONE 6:e23516
Stains JP, Watkins MP, Grimston SK, Hebert C, Civitelli R (2014) Molecular mechanisms of osteoblast/osteocyte regulation by connexin43. Calcif Tissue Int 94:55–67
Grimston SK, Watkins MP, Stains JP, Civitelli R (2013) Connexin43 modulates post-natal cortical bone modeling and mechano-responsiveness. Bonekey Rep 2:446
Plotkin LI (2014) Connexin 43 hemichannels and intracellular signaling in bone cells. Front Physiol 5:131
Canalis E, Mazziotti G, Giustina A, Bilezikian JP (2007) Glucocorticoid-induced osteoporosis: pathophysiology and therapy. Osteoporos Int 18:1319–1328
Bhattacharjee R, Kaneda M, Nakahama K, Morita I (2009) The steady-state expression of connexin43 is maintained by the PI3K/Akt in osteoblasts. Biochem Biophys Res Commun 382:440–444
Chen J, Holguin N, Shi Y, Silva MJ, Long F (2015) mTORC2 signaling promotes skeletal growth and bone formation in mice. J Bone Miner Res 30:369–378
Plotkin LI, Manolagas SC, Bellido T (2002) Transduction of cell survival signals by connexin-43 hemichannels. J Biol Chem 277:8648–8657
Acknowledgments
This work was supported by research funds from Chonbuk National University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Chen Shen, Mi Ran Kim, Jeong Mi Noh, Su Jin Kim, Sun-O Ka, Ji Hye Kim, Byung-Hyun Park, and Ji Hyun Park have no conflicts of interest to report.
Human and Animal Rights and Informed Consent
This study was ethically approved by the Institutional Animal Care and Use Committee of Chonbuk National University and performed in accordance with the criteria defined by the rules of the committee.
Rights and permissions
About this article
Cite this article
Shen, C., Kim, M.R., Noh, J.M. et al. Glucocorticoid Suppresses Connexin 43 Expression by Inhibiting the Akt/mTOR Signaling Pathway in Osteoblasts. Calcif Tissue Int 99, 88–97 (2016). https://doi.org/10.1007/s00223-016-0121-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-016-0121-y