Abstract
Recent studies have highlighted a significant association between the severity of atherosclerosis and bone mineral density (BMD) among healthy subjects, although its connection to angiographically determined peripheral artery disease (PAD) has never been investigated. We evaluated the connection between the angiographic severity and site specificity of peripheral atherosclerosis and osteoporosis among patients with chronic lower limb ischemia. In our cross-sectional study we investigated 172 patients with PAD. The anatomic sites of the lesions were analyzed. The severity of atherosclerosis was diagnosed using the Bollinger angiographic score (BS). BMD was measured at the lumbar spine (l-BMD) and at femoral (f-BMD) and radial (r-BMD) sites by dual-energy X-ray absorptiometry. Dyslipidemia, the level of vitamin D3, and different bone turnover markers were also noted. Among PAD patients, regardless of the lesion site, we did not find any association between BMD and BS. Among patients with iliac disease, BS was associated with l-BMD (p = 0.038, r = −0.467) and with f-BMD (p = 0.002, r = −0.642). The level of r-BMD among patients with iliac disease was not associated with BS (p = 0.233, r = −0.306). We did not find any difference between the group of patients with and that without dyslipidemia and low or normal levels of vitamin D3. Our results show a connection between the severity of atherosclerosis and osteoporosis among patients with PAD, specific to the site of the lesion. The findings regarding dyslipidemia, bone markers, and site specificity support the hypothesis that reduced blood flow is the key factor responsible for the inverse association of BMD with atherosclerosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
It is well known among vascular specialists that patients with severe atherosclerosis often suffer from osteoporosis as well. Some of the risk factors for these diseases are common, but many others are not; hence, it is difficult to demonstrate a connection which links them. Recent evidence suggests a strong connection between atherosclerosis and bone mineral density (BMD) [1], although the association is not fully understood.
Several studies have reported increased prevalence of peripheral artery disease (PAD) among patients with osteoporosis [2], while other reports [3] have shown a weak, age-related association between the two diseases among female patients. It is also specified that increased cardiovascular morbidity is associated with the presence of osteoporosis [4]. The exact mechanism behind this connection has not been clarified yet.
Some studies [3] suggest that decreased BMD is due to compromised blood flow. Laroche et al. [5] found that lower femoral BMD was associated with the leg affected more by atherosclerosis. These measurements were based on ankle brachial Doppler index and clinical assessments of the patient.
Another hypothesis suggests that dyslipidemia can be the link between atherosclerosis and osteoporosis [6–8]. Higher low-density lipoprotein (LDL) levels and lower high-density lipoprotein (HDL) levels were found in postmenopausal women with low BMD [9]. The same oxidized lipids that induce atherosclerosis also induce mineralization and differentiation of the osteoblastic cells in the artery wall [10].
A third theory posits vitamin D3 as one of the possible links between atherosclerosis and osteoporosis [11]. Supplementation with vitamin D3 reduces the risk of fractures and slightly improves BMD [12] as well as having an effect on cardiovascular mortality [13].
The diagnosis of osteoporosis is based on BMD, but the importance of bone turnover is highlighted as well [14]. Several markers of bone absorption and formation have been identified. Their level is moderately associated with BMD in postmenopausal women [14].
Fetuin-A is an inhibitor of extraosseal calcification; its level is associated to lumbar spine BMD (l-BMD) in elderly women [15] and to vascular calcification in healthy [16] and PAD [17] patients. Regardless of these findings, the level of fetuin-A among chronic kidney disease (CKD) and hemodialyzed patients appears to be an independent risk factor [18, 19] for vascular calcification, while its role in patients without CKD has not been fully discovered [16].
Studies focusing on patients with PAD use indirect methods to assess the severity of vascular calcification, such as measurements of intima media thickness [20] or the presence of calcification in the aorta [1]. A recent study found a connection between the angiographic symptoms of coronary sclerosis and BMD [21] in female patients, while other authors were unable to establish the same connection in male patients [22].
Although the mechanism of the development of osteoporosis and atherosclerosis is better understood, the existing connection among these diseases has not yet been fully evaluated and explained. To the best of our knowledge, angiographic symptoms and the severity of osteoporosis have never been investigated among PAD patients.
The aim of this study was to evaluate the connection between the angiographic severity and site specificity of peripheral atherosclerosis and osteoporosis among patients with PAD and to examine the potential effect of dyslipidemia and serum D3 levels on this association.
Materials and Methods
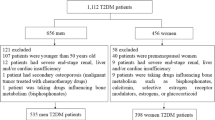
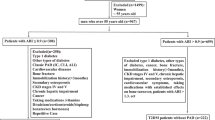
In this cross-sectional study 172 consecutive patients with advanced chronic lower limb ischemia were recruited at the Semmelweis University Department of Vascular Surgery, Budapest, Hungary, between January and July 2009.
At the first visit to the outpatient clinic a medical history was recorded and all patients underwent physical examination. A study questionnaire was used for recording the relevant demographic and clinical data (age, weight, height, abdominal girth, smoking habit, and concomitant disease). Anticholesterol therapy, osteoporosis treatment, and the use of other medications were also noted. Patients were considered hypertensive or diabetic if they were treated for these conditions at the time of their visit to the center. Body mass index (BMI) was calculated as weight (kilograms) divided by height squared (meters). Exclusion criteria were emergency admission, clinical or laboratory signs of acute infection, inflammation, malignant tumor, hepatic disease, end-stage renal disease (dialysis), immune suppression, and severe medical or surgical conditions (myocardial infarction, stroke, trauma, surgical procedure) in the 6 months prior to the visit to the outpatient clinic. All of our patients had severe, clinically significant lower limb atherosclerosis.
All of our patients underwent a surgical procedure, endovascular repair, or diagnostic angiography. A radiologist, who was excluded from other parts of the study performed lower limb angiography. The puncture was performed using local anesthesia with the Seldinger technique in all of the cases via radial, brachial, or femoral access. Angiograms were performed using a 4-Fr diagnostic pigtail-shaped flush catheter and a power injector. Digital subtraction angiography was performed using Axiom Artis (Siemens Medical Solutions, Erlangen, Germany) standard angiography suite. Vital signs and oxygen saturation were monitored in all patients. For angiography, non-ionic contrast material—iopromide Ultravist 370 (Bayer Schering Pharma, Berlin, Germany) or iodixanol (Visipaque; GE Healthcare, Little Chalfont, UK)—was used, depending on the renal function.
We chose an angiography-based scoring system created by Bollinger et al. [23], called the Bollinger score (BS). Two experienced radiologists, who were blinded from each other’s results, analyzed the pictures. An additive score was calculated in order to assess the extent of arteriosclerosis of the infrarenal aorta and the iliac, femoral, popliteal, and crural arteries on each side. Stenotic lesions and occlusions were noted in each arterial segment on both sides. Four categories of occlusive lesions were defined in descending order of severity: complete occlusion and stenosis narrowing the lumen by more than 50, 25–50 %, and less than 25 %. (Lower values were assigned to less severe stenosis.) If the stenotic area exceeded more than half of the length of the vessel, higher values were given and occlusion received the highest scores, especially if it was observed in the full length of the artery. This system is particularly suitable to assess systemic atherosclerosis because it is able to judge stenoses and occlusions in a long segment of the vascular system. The site of the atherosclerotic lesion was noted and compared to the BMD measurements, which were also site-specific.
Patients were referred to an internist specialized in osteoporosis, who was excluded from other parts of the study. BMD measurements were carried out using dual-energy X-ray absorptiometry (DXA) (Lunar Prodigy; General Electric, Madison, WI) at three different sites: total femoral neck, lumbar spine (L2–L4), and radius midshaft. BMD was calculated by the ratio of bone mineral content and the observed area (grams per square centimeter).
Fasting serum samples were collected and used to analyze laboratory parameters. Conventional standardized methods were performed in the core laboratory of Semmelweis University (diagnostic instruments: D-Cell 5D from Diagon, Budapest, Hungary; Cobas Integra 400 from Roche, Indianapolis, IN: STA-Compact from Diagnostica Stago, Parsippany, NJ). To evaluate dyslipidemia, total cholesterol (TC), HDL and LDL cholesterol, and triglyceride levels were measured. According to Natarajan et al. [24], dyslipidemia was considered if the patient was previously diagnosed with it or the ratio of TC to HDL was higher than 5. During the laboratory tests we also investigated the level of C-reactive protein, HbA1c, liver and kidney function, and electrolytes. Levels of vitamin D3, beta crosslaps (bCTx), bone alkaline phosphatase (BAP), osteocalcin (BGLAP), and parathyroid hormone (PTH) were also noted and compared to BMD. We divided our study cohort into high– and low–vitamin D subgroups. According to Holick [25], low level of vitamin D was noted if the patient had 20 ng/mL or lower serum concentration.
Statistical analysis was performed with Prism for Windows 5.01 (GraphPad Software, San Diego, CA) and SPSS for Windows 15.0.1 (SPSS, Inc., Chicago, IL). As many of the variables had non-gaussian distributions, nonparametric tests were applied. Spearman’s rho coefficient was calculated for correlations, and the Mann-Whitney U test and Fisher’s exact test were performed to compare two independent groups. For regression analysis, a linear regression test was used. All statistical analyses were two-tailed, and p < 0.05 was considered significant. Values presented in the text are medians [interquartile range (IQR)], unless otherwise stated.
The study protocol was approved by the Semmelweis University Regional and Institutional Committee of Science and Research Ethics.
Results
The baseline clinical characteristics of our 172 PAD patients and the presence of osteoporosis or osteopenia, according to WHO guidelines, are displayed in Table 1.
The median age was 65.58 years (60.26–70.49) among female patients and 63.18 years (57.64–69.73) among male patients. The current smoking rate was 55 %, although 88 % of our patients had smoked for longer than a 10-year period in their lives. After the BMD measurements, we estimated the percentage of patients having osteoporosis or osteopenia. In our study cohort 50 % of the patients had osteopenia and 31 % suffered from osteoporosis at any of the examined sites. The median BS was 63.50 (37.00–84.00); this corresponds with the severity of atherosclerosis in our cohort. The inter-rater reliability for BS examiners was found to be in good agreement (kappa = 0.794, p < 0.05). Only 9 % of our 172 patients had been previously diagnosed with and treated for osteoporosis. The median BMD, T scores and Z scores and their Spearman correlation to BS are shown in Table 2. Without considering the site of the atherosclerotic lesion, in our study cohort we found no correlation among BS and l-BMD (p = 0.294, r = −0.147), BS and femoral site BMD (f-BMD) (p = 0.169, r = –0.192), or BS and radial site BMD (r-BMD) (p = 0.052, r = −0.285).
As described previously, we divided our patients in two subgroups according to the site of the atherosclerotic lesion. The patient characteristics of the different subgroups mentioned below are displayed in Table 3. We compared the different patient groups to each other using the Mann-Whitney U- and Fisher’s exact tests and did not find any significant difference among them. We found significant correlation among patients with iliac disease between BS and l-BMD (p = 0.038, r = −0.467) and f-BMD (p = 0.002, r = −0.642), but we were unable to establish a significant correlation between BS and r-BMD (p = 0.233, r = −0.306). Linear regression analysis showed that the connection between f-BMD and BS was independent from sex, age, BMI, and smoking habits within this patient group (p = 0.001, RR= −1.5, 95 % CI of RR −2.35 to −0.684). Among patients with infrainguinal disease we did not find any association between BS and l-BMD (p = 0.514, r = 0.118), BS and f-BMD (p = 0.505, r = 0.120), or BS and r-BMD (p = 0.202, r = −0.240).
We divided our patients into two subgroups according to dyslipidemia. We did not find any significant correlation between BS and BMD within these subgroups. Comparison of BS to l-BMD (p = 0.457, r = −0.121), BS to f-BMD (p = 0.169, r = −0.192), and BS to r-BMD (p = 0.052, r = −0.285) did not show an association among patients with dyslipidemia. The association of angiographic signs with BMD among patients without dyslipidemia was as follows: BS to l-BMD (p = 0.457, r = −0.121), BS to f-BMD (p = 0.018, r = −0.378), and BS to r-BMD (p = 0.223, r = −0.208).
We divided our study cohort according to the levels of vitamin D3 into two subgroups. In the low–vitamin D3 subgroup we found the following nonsignificant differences: BS to l-BMD (p = 0.668, r = −0.108) BS to f-BMD (p = 0.990, r = 0.003), and BS to r-BMD (p = 0.087, r = −0.442). The BS among patients with normal vitamin D3 did not correlate significantly with l-BMD (p = 0.465, r = −0.128) or with r-BMD (p = 0.355, r = −0.172). At the femoral site BS was associated with f-BMD (p = 0.046, r = −0.340). We also compared vitamin D3 levels according to the site of atherosclerosis, but no significant difference was found (p = 0.771) between the subgroups.
We evaluated the connection among BMD values and different bone turnover markers. These results are shown in Table 4. We found an association between l-BMD, D3, and fetuin-A as well as between f-BMD and BAP in the infrainguinal patient group. We also divided our patients into two groups according to gender but did not find any association within these subgroups.
Discussion
In this study we evaluated the connection between the angiographic severity of lower limb atherosclerosis and osteoporosis. Our study population’s median age and smoking habits were typical for PAD patients. The prevalence of osteoporosis within this group of patients was unexpectedly high; therefore, the treatment and screening of osteoporosis in PAD patients may need reconsideration. We did not find a significant connection between BS and bone density regardless of the site of the atherosclerotic lesion. Our findings were congruent with previous studies [1], although within this group of patients according to our knowledge angiographic measurements have never been compared to osteoporosis.
As previously described, the connection between atherosclerosis and osteoporosis could be due to the compromised blood flow. The reduction in oxygen saturation can cause bone degradation, hence osteoporosis [26, 27]. As atherosclerosis is a systemic disease, its manifestation is general and may occur in any part of the circulatory system. It can affect all arteries, although the factors influencing the development of clinically significant stenosis are not yet fully understood. As our results show, in patients having significant stenoses in the iliac arteries, which supply blood to the femoral head and lumbar spine, a significant association was found between BS and BMD at these anatomic sites. At the femoral site a linear regression test found that the connection was independent of age, sex, BMI, and smoking habit. Among patients suffering from infrainguinal lesions there was no significant connection between BMD and BS. These findings suggest that among lower limb atherosclerotic patients one of the causes of the higher incidence of osteoporosis is the reduced blood flow.
Dyslipidemia is one of the mechanisms suspected of having an effect on osteoporosis and atherosclerosis. Earlier studies showed a stronger connection between osteoporosis and atherosclerosis among patients with dyslipidemia. As our results show, in our lower limb ischemic study cohort, no association was found between atherosclerosis and osteoporosis in the subgroups regarding to dyslipidemia. This can be due to several factors. The prevalence of dyslipidemia in our patients was higher than that in a healthy or osteoporotic population, and most of them were already on anticholesterol treatment. Among patients without dyslipidemia a weak connection was found between BS and f-BMD, which was not considered relevant. Our results show that dyslipidemia does not have an effect on the previously found association within this group of patients.
Vitamin D3 has an effect on the cardiovascular system [13] and plays an important role in bone metabolism. A reduced level of vitamin D3 causing secondary hyperparathyroidism has negative implications in both of these diseases. A recent review highlighted vitamin D3 as a possible link between atherosclerosis and osteoporosis [11]. To establish the previously described associations, we created two subgroups, patients with vitamin D3 insufficiency and patients with normal vitamin D3 levels [25]. We did not find any correlation between BS and BMD within the first subgroup. Among patients with normal vitamin D3 levels we found a weak connection between BS and f-BMD. We did not find any association between l-BMD or r-BMD and BS. We also compared vitamin D3 levels among patients with iliac and infrainguinal diseases but found only a weak connection with l-BMD. These data suggest that in our study cohort vitamin D3 did not affect the association of BS and BMD.
We estimated the connection between different bone turnover markers and BMD, but we did not find any clinically significant association within this group of patients. Previous studies have described associations between these measurements only in elderly women; however, in our study cohort this connection cannot be affirmed.
There are many other factors that might explain the negative connection between vascular calcification and BMD. The levels of phosphate and of fetuin-A are independent risk factors for vascular calcification in patients with CKD [18, 19, 28], and the ratio of phosphate to pyrophosphate also plays an important role in the regulation of mineralization. The inhibition of bone resorption can slow down the progress of vascular calcification [29]. One of the well-known inhibitors of systemic calcification is fetuin-A. Its importance has been highlighted several times in the development of vascular calcification, although the exact role of this glycoprotein has not been fully understood. It has been also suggested that fetuin-A may be able to play a role in future therapies [29]. In our study cohort we found the same previously described [15] connection between fetuin-A and l-BMD but did not find any association between fetuin-A and f-BMD or r-BMD.
Among the strengths of the present study is the detailed angiographic method to determine the extent of site-specific atherosclerosis and the sensitivity of the BS regarding side branches and analysis of a large area of the arterial tree. We integrated a wide variety of cofactors between atherosclerosis and osteoporosis. Our study also has limitations. The cross-sectional design did not allow evaluation of a longitudinal association between the two diseases. Methods of assessing atherosclerosis measure different entities, such as calcification, occlusion, stenosis, and arterial flow, so it is not clear which is the best method to evaluate the severity of it.
In conclusion we found a strong connection among patients with clinically significant iliac stenosis between BS and BMD scores measured at the bone region supplied by the iliac artery. We did not find any association between angiographic severity and BMD score regardless of the site of the lesion. In our study cohort neither the presence of dyslipidemia nor vitamin D levels influenced the connection between BS and BMD.
References
Hyder JA, Allison MA, Criqui MH, Wright CM (2007) Association between systemic calcified atherosclerosis and bone density. Calcif Tissue Int 80:301–306
Mangiafico RA, Russo E, Riccobene S, Pennisi P, Mangiafico M, D’Amico F, Fiore CE (2006) Increased prevalence of peripheral arterial disease in osteoporotic postmenopausal women. J Bone Miner Metab 24:125–131
von Muhlen D, Allison M, Jassal SK, Barrett-Connor E (2009) Peripheral arterial disease and osteoporosis in older adults: the Rancho Bernardo Study. Osteoporos Int 20:2071–2078
von der Recke P, Hansen MA, Hassager C (1999) The association between low bone mass at the menopause and cardiovascular mortality. Am J Med 106:273–278
Laroche M, Pouilles JM, Ribot C, Bendayan P, Bernard J, Boccalon H, Mazieres B (1994) Comparison of the bone mineral content of the lower limbs in men with ischaemic atherosclerotic disease. Clin Rheumatol 13:611–614
Samelson EJ, Cupples LA, Hannan MT, Wilson PW, Williams SA, Vaccarino V, Zhang Y, Kiel DP (2004) Long-term effects of serum cholesterol on bone mineral density in women and men: the Framingham Osteoporosis Study. Bone 34:557–561
Jensky NE, Hyder JA, Allison MA, Wong N, Aboyans V, Blumenthal RS, Schreiner P, Carr JJ, Wassel CL, Ix JH, Criqui MH (2011) The association of bone density and calcified atherosclerosis is stronger in women without dyslipidemia: the multi-ethnic study of atherosclerosis. J Bone Miner Res 26:2702–2709
Lupattelli G, Scarponi AM, Vaudo G, Siepi D, Roscini AR, Gemelli F, Pirro M, Latini RA, Sinzinger H, Marchesi S, Mannarino E (2004) Simvastatin increases bone mineral density in hypercholesterolemic postmenopausal women. Metabolism 53:744–748
Yamaguchi T, Sugimoto T, Yano S, Yamauchi M, Sowa H, Chen Q, Chihara K (2002) Plasma lipids and osteoporosis in postmenopausal women. Endocr J 49:211–217
Parhami F, Morrow AD, Balucan J, Leitinger N, Watson AD, Tintut Y, Berliner JA, Demer LL (1997) Lipid oxidation products have opposite effects on calcifying vascular cell and bone cell differentiation. A possible explanation for the paradox of arterial calcification in osteoporotic patients. Arterioscler Thromb Vasc Biol 17:680–687
Stojanovic OI, Lazovic M, Vuceljic M (2011) Association between atherosclerosis and osteoporosis, the role of vitamin D. Arch Med Sci 7:179–188
Cranney A, Horsley T, O’Donnell S, Weiler H, Puil L, Ooi D, Atkinson S, Ward L, Moher D, Hanley D, Fang M, Yazdi F, Garritty C, Sampson M, Barrowman N, Tsertsvadze A, Mamaladze V (2007) Effectiveness and safety of vitamin D in relation to bone health. Evid Rep Technol Assess (Full Rep) 158:1–235
Anagnostis P, Athyros VG, Adamidou F, Florentin M, Karagiannis A (2010) Vitamin D and cardiovascular disease: a novel agent for reducing cardiovascular risk? Curr Vasc Pharmacol 8:720–730
Biver E, Chopin F, Coiffier G, Brentano TF, Bouvard B, Garnero P, Cortet B (2012) Bone turnover markers for osteoporotic status assessment? A systematic review of their diagnosis value at baseline in osteoporosis. Joint Bone Spine 79:20–25
Chailurkit L, Kruavit A, Rajatanavin R, Ongphiphadhanakul B (2011) The relationship of fetuin-A and lactoferrin with bone mass in elderly women. Osteoporos Int 22:2159–2164
Mori K, Emoto M, Inaba M (2012) Fetuin-A and the cardiovascular system. Adv Clin Chem 56:175–195
Szeberin Z, Fehervari M, Krepuska M, Apor A, Rimely E, Sarkadi H, Szeplaki G, Prohaszka Z, Kalabay L, Acsady G (2011) Serum fetuin-A levels inversely correlate with the severity of arterial calcification in patients with chronic lower extremity atherosclerosis without renal disease. Int Angiol 30:474–475
Ford ML, Tomlinson LA, Smith ER, Rajkumar C, Holt SG (2010) Fetuin-A is an independent determinant of change of aortic stiffness over 1 year in non-diabetic patients with CKD stages 3 and 4. Nephrol Dial Transplant 25:1853–1858
Shioi A, Nishizawa Y (2009) Vascular calcification in chronic kidney disease: pathogenesis and clinical implications. J Ren Nutr 19:78–81
Fodor D, Bondor C, Albu A, Muntean L, Simon SP, Poanta L, Craciun A (2011) Relation between intima-media thickness and bone mineral density in postmenopausal women: a cross-sectional study. Sao Paulo Med J 129:139–145
Choi SH, An JH, Lim S, Koo BK, Park SE, Chang HJ, Choi SI, Park YJ, Park KS, Jang HC, Shin CS (2009) Lower bone mineral density is associated with higher coronary calcification and coronary plaque burdens by multidetector row coronary computed tomography in pre- and postmenopausal women. Clin Endocrinol (Oxf) 71:644–651
Beer S, Saely CH, Hoefle G, Rein P, Vonbank A, Breuss J, Gaensbacher B, Muendlein A, Drexel H (2010) Low bone mineral density is not associated with angiographically determined coronary atherosclerosis in men. Osteoporos Int 21:1695–1701
Bollinger A, Breddin K, Hess H, Heystraten FM, Kollath J, Konttila A, Pouliadis G, Marshall M, Mey T, Mietaschk A, Roth FJ, Schoop W (1981) Semiquantitative assessment of lower limb atherosclerosis from routine angiographic images. Atherosclerosis 38:339–346
Natarajan S, Glick H, Criqui M, Horowitz D, Lipsitz SR, Kinosian B (2003) Cholesterol measures to identify and treat individuals at risk for coronary heart disease. Am J Prev Med 25:50–57
Holick MF (2000) Calcium and vitamin D. Diagnostics and therapeutics. Clin Lab Med 20:569–590
Maes C, Carmeliet G, Schipani E (2012) Hypoxia-driven pathways in bone development, regeneration and disease. Nat Rev Rheumatol 8:358–366
Hung SP, Ho JH, Shih YR, Lo T, Lee OK (2012) Hypoxia promotes proliferation and osteogenic differentiation potentials of human mesenchymal stem cells. J Orthop Res 30:260–266
Kestenbaum B, Sampson JN, Rudser KD, Patterson DJ, Seliger SL, Young B, Sherrard DJ, Andress DL (2005) Serum phosphate levels and mortality risk among people with chronic kidney disease. J Am Soc Nephrol 16:520–528
Persy V, D’Haese P (2009) Vascular calcification and bone disease: the calcification paradox. Trends Mol Med 15:405–416
Acknowledgments
We warmly thank Rachel Ewings and Daniel Loganathan for English correction, Renáta Dudás for data management, and Edit Máté for the BMD screening.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have stated that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Fehérvári, M., Sarkadi, H., Krepuska, M. et al. Bone Mineral Density is Associated with Site-Specific Atherosclerosis in Patients with Severe Peripheral Artery Disease. Calcif Tissue Int 93, 55–61 (2013). https://doi.org/10.1007/s00223-013-9727-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-013-9727-5