Abstract
We examined whether or not BMD or bone markers were useful for assessing the risk of vertebral fractures in 248 Japanese men with type 2 diabetes. We analyzed the relationships between bone markers (osteocalcin [OC], bone-specific alkaline phosphatase [BAP], urinary N-terminal cross-linked telopeptide of type-I collagen) or BMD and HbA1c, urinary C-peptide, insulin-like growth factor-I (IGF-I), parathyroid hormone, 1,25(OH)2 vitamin D, and the presence of prevalent vertebral fractures. Multiple regression analysis adjusted for age, body height, weight, duration of diabetes, and serum creatinine showed that serum OC and OC/BAP ratio were correlated negatively with HbA1c (P < 0.01) and positively with IGF-I (P < 0.01). Multivariate logistic regression analysis adjusted for the above parameters showed that serum OC/BAP ratio was inversely associated with the presence of vertebral fractures (odds ratio = 0.695, P < 0.05). This association was still significant after additional adjustment for lumbar or femoral neck BMD. Our results suggest that poor diabetic control and lower IGF-I level are linked to impaired bone formation and resultant reduction in OC/BAP ratio in men with type 2 diabetes. The OC/BAP ratio could be clinically useful for assessing the risk of vertebral fractures independent of BMD in diabetic men.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The number of patients with diabetes mellitus and osteoporosis is rapidly increasing in industrialized countries, where Western-style aging societies are prevalent. A relationship between diabetes and osteoporotic fractures is becoming increasingly recognized [1]. Vertebral and hip fractures are the most important osteoporotic fractures because they frequently occur and increase the mortality of elderly people as high as six- to ninefold [2, 3]. Although patients with type 2 diabetes show no bone mineral density (BMD) reduction, fracture risks are known to increase approximately up to 1.5-fold at the hip, proximal humerus, forearm, and foot [4–6]. Moreover, our recent study revealed that Japanese patients with type 2 diabetes have an increased risk of vertebral fractures independent of BMD [7].
Bone fragility in patients with type 2 diabetes may be caused by low bone turnover [8]. Hyperglycemia in type 2 diabetes might be associated with factors that influence bone strength and quality independently of BMD [9–11]. Several studies have indicated that hyperglycemia induces a low turnover bone with osteoblast dysfunction [12, 13]. Hyperglycemia and advanced glycation end products (AGEs) promote the apoptosis of osteoblastic cells [14, 15] and restrain the differentiation of cells [16–19]. These findings suggest that hyperglycemia may cause diminished bone formation. A previous clinical study has indicated that serum osteocalcin (OC) was low before treatments and elevated after treatments of diabetes, while bone-specific alkaline phosphatase (BAP) was reduced [20]. Previous in vitro studies have shown that chronic hyperglycemia increased the activity and expression of BAP and decreased OC expression and cellular calcium uptake [10]. It is well-known that BAP is expressed in the early period of osteoblastic differentiation, whereas OC is expressed in the later period [21]. Thus, hyperglycemia could cause impaired osteoblastic maturation, resulting in bone fragility in patients with type 2 diabetes.
It is thought that bone metabolism in type 2 diabetes is affected by abnormal hormonal actions. Patients with type 2 diabetes appear to have increased BMD, possibly due in part to an anabolic effect of hyperinsulinemia [22, 23] and in part to obesity [24]. In addition, patients with type 2 diabetes have reduced bone turnover and may have reduced levels of parathyroid hormone (PTH) [25]. These factors may protect patients from reduction of BMD and fracture risks. On the other hand, insulin-like growth factor-I (IGF-I), which is anabolic for bone, may also be reduced in patients with type 2 diabetes [26, 27]. However, it is still unclear how these factors are associated with BMD, bone markers, or bone fragility in patients with type 2 diabetes.
In this study, to examine these issues, we investigated the relationships between bone markers (OC, BAP, and urinary N-terminal cross-linked telopeptide of type-I collagen [uNTX]) or BMD and HbA1c, urinary C-peptide (uC-peptide), IGF-I, PTH, 1,25(OH)2 vitamin D, and the presence of vertebral fractures in Japanese men with type 2 diabetes.
Subjects and Methods
Subjects
The subjects in this study were 248 Japanese men with type 2 diabetes aged 20–83 years (mean 59.0). We consecutively recruited subjects who visited Shimane University Hospital for education, evaluation, or treatment of diabetes. Subjects agreed to participate in this study and gave informed consent. This study was approved by the institutional review board of our institution. None had hepatic or renal dysfunction or nutritional derangements that might cause changes in bone metabolism. We excluded patients with histories of falls and traffic accidents in order to eliminate the possibility of injury-associated fractures. Forty-two patients had received insulin treatment, 95 patients had taken oral hypoglycemic agents (sulfonylurea, 82; metformin, 28; alpha-glucosidase inhibitor, 28), and 121 patients had not previously been under any medications for diabetes. All subjects were free of drugs known to influence bone and calcium metabolism like vitamin D and bisphosphonate as well as thiazolidinedione until the time of the present study.
Radiography
Lateral X-ray films of the thoracic and lumbar spine were taken in the same week as the serum collection. The anterior, central, and posterior heights of each of the 13 vertebral bodies from Th4 to L4 were measured. A vertebral fracture was diagnosed if at least one of three height measurements along the length of the same vertebrae had decreased by >20% compared to the height of the nearest uncompressed vertebral body [28]. None of the subjects had a history of serious trauma.
BMD and Biochemical Measurements
BMD values of the lumbar spine (L), femoral neck (F), and one-third of the radius (1/3R) were measured by dual-energy X-ray absorptiometry (QDR-4500; Hologic, Waltham, MA). The same operator tested all of the subjects during the study to eliminate operator discrepancies. The coefficients of variation (precision) of measurements of the lumbar spine, femoral neck, and mid-radius by our methods were 0.9, 1.7, and 1.9%, respectively. Values were also expressed relative to the standard deviation (SD) of age- and sex-matched normal Japanese mean values provided by the manufacturer (Z score).
After overnight fasting, serum and first void urine samples were collected. Biochemical markers were measured by standard biochemical methods, as previously described [29, 30]. Hemoglobin A1c (HbA1c) was determined by high-performance liquid chromatography (HPLC). BAP in serum and uC-peptide pooled for 24 h were measured by enzyme immunoassay and chemiluminescent enzyme immunoassay, respectively. Intact PTH was measured by electrochemiluminescent immunoassay. 1,25(OH)2 vitamin D, OC, and IGF-I were measured by radioimmunoassay. uNTX was measured by enzyme linked immunosorbent assay.
Statistical Analysis
Data were expressed as mean ± SD. Because uC-peptide and intact PTH showed a markedly skewed distribution, logarithmic (log) transformation of these values was carried out before performing correlation and regression analyses. Statistical significance between the groups was determined using Student’s t-test. Simple, multiple, and logistic regression analyses were performed using the statistical computer program StatView (Abacus Concepts, Berkeley, CA). P < 0.05 was considered significant.
Results
Relationships between BMD or Bone Markers Versus HbA1c, uC-Peptide, IGF-I, Intact PTH, and 1,25(OH)2 Vitamin D
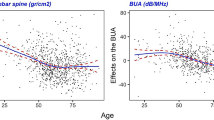
Baseline characteristics of subjects are shown in Table 1. Since our simple regression analysis showed that HbA1c, uC-peptide, IGF-I, intact PTH, and 1,25(OH)2 vitamin D were affected by age, body stature, and renal function (data not shown), multiple regression analyses were performed with each of these parameters adjusted for age, body height, weight, duration of diabetes, and serum creatinine as an independent variable versus BMD at each skeletal site or bone markers as a dependent variable (Table 2). OC and OC/BAP ratio were correlated significantly and negatively with HbA1c (P = 0.0057 and P < 0.0001, respectively) and positively with IGF-I (P = 0.0095). BAP was correlated significantly and negatively with IGF-I (P = 0.0304) and positively with log(intact PTH) (P = 0.0247). Although L- and F-BMD were not significantly correlated with HbA1c or any hormonal parameters, 1/3R-BMD was correlated positively with HbA1c (P = 0.0416) and negatively with log(intact PTH) (P = 0.0324).
Comparison of Demographic and Biochemical Parameters, Bone Markers, and BMD Between Patients with and Without Vertebral Fractures
Next, we compared various parameters including HbA1c, uC-peptide, IGF-I, intact PTH, 1,25(OH)2 vitamin D, bone markers, and BMD values at each site between patients with and without vertebral fractures (Table 3). Patients with vertebral fractures were significantly older (P = 0.0071), were shorter (P = 0.0203), and had lower absolute L-BMD (P = 0.0441) than patients without vertebral fractures. IGF-I and OC/BAP ratio in patients with vertebral fractures tended to be lower than in patients without them (P = 0.0620 and P = 0.0940, respectively). On the other hand, no significant differences in the levels of HbA1c, uC-peptide, IGF-I, intact PTH, 1,25(OH)2 vitamin D, or bone markers were observed between subjects with and without fractures.
When multivariate logistic regression analysis was performed with the presence of vertebral fractures as a dependent variable and levels of HbA1c, uC-peptide, IGF-I, intact PTH, 1,25(OH)2 vitamin D, bone markers, and BMD adjusted for age, body weight, height, duration of diabetes, and serum creatinine as independent variables (Table 4), OC/BAP ratio was selected as an index affecting the presence of vertebral fractures (P = 0.0345). L-BMD tended to affect the presence of vertebral fractures (P = 0.0559) but was not significant. In contrast, F-BMD, 1/3R-BMD, and any other bone markers or hormones were not associated with the presence of vertebral fractures. OC/BAP ratio was still significantly and inversely associated with the presence of vertebral fractures after additional adjustment for L- or F-BMD, HbA1c, or IGF-I (Table 5).
Discussion
In this study, OC/BAP ratio was correlated negatively with HbA1c and positively with IGF-I in men with type 2 diabetes. Moreover, OC/BAP ratio was significantly and inversely associated with the presence of vertebral fractures independently of BMD. These findings suggest that poor glycemic control and lower IGF-I level may cause impaired osteoblastic differentiation and resultant reduction in OC/BAP ratio, which in turn may cause bone fragility and vertebral fractures independently of BMD in diabetic men. Thus, our findings seem to support the previous observations that hyperglycemia and reduced IGF-I are involved in bone fragility in type 2 diabetes [8–19, 26, 27]. However, multivariate logistic regression analysis showed that OC/BAP ratio was associated with the presence of vertebral fractures independently of HbA1c or IGF-I (Table 5). This result as well as no association of HbA1c or IGF-I with the presence of vertebral fractures (Table 4) suggest that hyerglycemia or reduced IGF-I themselves are not directly linked to bone fragility but indirectly related to it by causing osteoblast dysfunction.
A recent meta-analysis showed that patients with type 2 diabetes had higher hip BMD than nondiabetic controls, despite an increased risk of hip fracture [4], suggesting that BMD values may not reflect bone fragility in type 2 diabetes. Recently, we also reported that L-BMD was not associated with the presence of prevalent vertebral fractures in women with type 2 diabetes, suggesting that L-BMD was not sensitive enough to assess the risk of vertebral fractures in this group [31]. In this study, we found that BMD at any site was not associated with the presence of vertebral fractures in men with type 2 diabetes, although L-BMD showed a tendency (P = 0.0559). Therefore, BMD, which is considered the gold standard for evaluating fracture risk in primary osteoporosis, seems to be not useful for assessing the risk of vertebral fractures in both men and women with type 2 diabetes. In postmenopausal women with type 2 diabetes, we have recently shown that serum IGF-I and pentosidine levels were associated with the presence of vertebral fractures independently of BMD, suggesting that they become surrogate markers for assessing the risk of vertebral fractures [29, 32]. In this study, we have shown that serum OC/BAP ratio could predict the presence of vertebral fractures in men with type 2 diabetes and could compensate for the insensitivity of BMD in the population.
IGFs are thought to be linked to the pathogenesis of diabetes-related complications [33]. Impaired production of IGFs could also cause bone complication in diabetes because IGFs are among the most important regulators of bone cell function [34]. Indeed, we previously found that serum IGF-I level was inversely associated with the risk of vertebral fractures in nondiabetic postmenopausal women [35, 36] as well as in their type 2 diabetic counterparts [29]. However, in men with type 2 diabetes, the relationship between serum IGF-I level and bone metabolism has been little documented. In this study, serum IGF-I level was correlated negatively with OC and OC/BAP ratio and positively with BAP, while the hormone was not significantly associated with BMD or the presence of vertebral fractures. Thus, in patients with type 2 diabetes, serum IGF-I level could predict the presence of vertebral fractures in postmenopausal women but not in men, although the significant positive correlation between IGF-I and OC/BAP ratio (Table 2) suggests that its reduction in the circulation was associated with impaired osteoblast function in men.
Several studies have shown that hyperglycemia causes hypercalciuria [37], which might result in enhancement of PTH secretion, while hyperglycemia could also cause suppressed PTH secretion from the parathyroid [25, 38]. Thus, impaired PTH and vitamin D metabolism might be involved in diabetic bone fragility. However, our present findings show that intact PTH and 1,25(OH)2 vitamin D are not associated with any bone markers or the presence of vertebral fractures in men with type 2 diabetes.
Although circulating insulin is considered to stimulate osteoblastogenesis and enhance bone formation [22, 39], the present study shows that uC-peptide, as a surrogate marker for residual insulin secretion, was not significantly associated with BMD or bone markers in men with type 2 diabetes. We also found that its level was not different between patients with and those without vertebral fractures. These findings are consistent with our previous ones in patients with type 2 diabetes, in which there were no associations between serum fasting C-peptide and BMD, bone metabolic markers, or vertebral fractures [29, 30]. However, subjects in our studies had received several treatments including insulin administration. Therefore, we should be cautious about the relationship between the capacity of residual insulin secretion and bone metabolism.
This study has some limitations. First, the sample size was not large enough to make definite conclusions. Second, we analyzed only subjects who visited Shimane University Hospital, a tertiary center, for evaluation or treatment of diabetes mellitus and osteoporosis. Therefore, the patients enrolled in this study might have relatively severe states of the disorders and might not be representative of Japanese men with the disorders. Third, the subjects in this study were only Japanese. The capacity of insulin secretion and degree of obesity in Asians are known to be different compared to Western people [40]. Therefore, it needs to be clarified whether or not our findings are universal. Fourth, we did not measure the fraction of undercarboxylated OC in men with and without fractures compared with healthy age-matched men. Increased metabolic bioactivity of undercarboxylated OC increased pancreatic β-cell proliferation, energy expenditure, insulin sensitivity, and adiponectin production and decreased adiposity [41, 42]. Thus, the undercarboxylated form of OC appears to regulate glucose homeostasis and to be one of the important bone markers when diabetes is studied. Finally, the conclusions of this study are weakened by its cross-sectional design and absence of age-matched healthy controls. Moreover, several other important variables were missing, such as 25-hydroxyvitamin D, estradiol, sex hormone binding globulin, and free testosterone. More than 50% of subjects were treated.
In conclusion, we found that serum OC/BAP ratio was more potently associated with the presence of vertebral fractures than BMD or other bone markers in men with type 2 diabetes, and it could be used as a surrogate marker for assessing the risk of vertebral fractures in that population. Thus, our previous and current studies together suggest that serum IGF-I and pentosidine levels in postmenopausal women [29, 32] and serum OC/BAP ratio in men may compensate for the ineffectiveness of BMD in evaluating the risk of vertebral fractures in type 2 diabetes. We need to determine their cut-off values that most effectively detect incident vertebral fractures by conducting a prospective study on larger populations in future.
References
Barrett-Connor E, Holbrook TL (1992) Sex differences in osteoporosis in older adults with non-insulin-dependent diabetes mellitus. JAMA 268:3333–3337
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353:878–882
Cauley JA, Thompson DE, Ensrud KC, Scott JC, Black D (2000) Risk of mortality following clinical fractures. Osteoporos Int 11:556–561
Vestergaard P (2007) Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes—a meta-analysis. Osteoporos Int 18:427–444
Lipscombe LL, Jamal SA, Booth GL, Hawker GA (2007) The risk of hip fractures in older individuals with diabetes: a population-based study. Diabetes Care 30:835–841
Strotmeyer ES, Cauley JA, Schwartz AV, Nevitt MC, Resnick HE, Bauer DC, Tylavsky FA, de Rekeneire N, Harris TB, Newman AB (2005) Nontraumatic fracture risk with diabetes mellitus and impaired fasting glucose in older white and black adults: the health, aging, and body composition study. Arch Intern Med 165:1612–1617
Yamamoto M, Yamaguchi T, Yamauchi M, Kaji H, Sugimoto T (2009) Diabetic patients have an increased risk of vertebral fractures independent of bone mineral density or diabetic complications. J Bone Miner Res 24:702–709
Saito M, Fujii K, Mori Y, Marumo K (2006) Role of collagen enzymatic and glycation induced cross-links as a determinant of bone quality in spontaneously diabetic WBN/Kob rats. Osteoporos Int 17:1514–1523
Terada M, Inaba M, Yano Y, Hasuma T, Nishizawa Y, Morii H, Otani S (1998) Growth-inhibitory effect of a high glucose concentration on osteoblast-like cells. Bone 22:17–23
Botolin S, MacCabe LR (2006) Chronic hyperglycemia modulates osteoblast gene expression through osmotic and non-osmotic pathways. J Cell Biochem 99:411–424
Gopalakrishnan V, Vignesh RC, Arunakaran J, Aruldhas MM, Srinivasan N (2006) Effects of glucose and its modulation by insulin and estradiol on BMSC differentiation into osteoblastic lineages. Biochem Cell Biol 84:93–101
Verhaeghe J, Suiker AM, Nyomba BL, Visser WJ, Einhorn TA, Dequeker J, Bouillon R (1989) Bone mineral homeostasis in spontaneously diabetic BB rats. II. Impaired bone turnover and decreased osteocalcin synthesis. Endocrinology 124:573–582
Gerdhem P, Isaksson A, Akesson K, Obrant KJ (2005) Increased bone density and decreased bone turnover, but no evident alteration of fracture susceptibility in elderly women with diabetes mellitus. Osteoporos Int 16:1506–1512
Li YM, Schilling T, Benisch P, Zeck S, Meissner-Weigl J, Schneider D, Limbert C, Seufert J, Kassem M, Schutze N, Jakob F, Ebert R (2007) Effects of high glucose on mesenchymal stem cell proliferation and differentiation. Biochem Biophys Res Commun 363:209–215
Alikhani M, Alikhani Z, Boyd C, MacLellan CM, Raptis M, Liu R, Pischon N, Trackman PC, Gerstenfeld L, Graves DT (2007) Advanced glycation end products stimulate osteoblast apoptosis via the MAP kinase and cytosolic apoptotic pathways. Bone 40:345–353
Brenner RE, Riemenschneider B, Blum W, Morike M, Teller WM, Pirsig W, Heinze E (1992) Defective stimulation of proliferation and collagen biosynthesis of human bone cells by serum from diabetic patients. Acta Endocrinol 127:509–514
Balint E, Szabo P, Marshall CF, Sprague SM (2001) Glucose-induced inhibition of in vitro bone mineralization. Bone 28:21–28
Yamamoto T, Ozono K, Miyauchi A, Kasayama S, Kojima Y, Shima M, Okada S (2001) Role of advanced glycation end products in adynamic bone disease in patients with diabetic nephropathy. Am J Kidney Dis 38:S161–S164
Ogawa N, Yamaguchi T, Yano S, Yamauchi M, Yamamoto M, Sugimoto T (2007) The combination of high glucose and advanced glycation end-products (AGEs) inhibits the mineralization of osteoblastic MC3T3-E1 cells through glucose-induced increase in the receptor for AGEs. Horm Metab Res 39:871–875
Okazaki R, Totsuka Y, Hamano K, Ajima M, Miura M, Hirota Y, Hata K, Fukumoto S, Matsumoto T (1997) Metabolic improvement of poorly controlled noninsulin-dependent diabetes mellitus decreases bone turnover. J Clin Endocrinol Metab 82:2915–2920
Stein GS, Lian JB (1993) Molecular mechanisms mediating proliferation/differentiation interrelationships during progressive development of the osteoblast phenotype. Endocr Rev 14:424–442
Reid IR, Evans MC, Cooper GJ, Ames RW, Stapleton J (1993) Circulating insulin levels are related to bone density in normal postmenopausal women. Am J Physiol Endocrinol Metab 265:E655–E659
Abrahamsen B, Rohold A, Henriksen JE, Beck-Nielsen H (2000) Correlations between insulin sensitivity and bone mineral density in non-diabetic men. Diabet Med 17:124–129
Ravn P, Cizza G, Bjarnason NH, Thompson D, Daley M, Wasnich RD, McClung M, Hosking D, Yates AJ, Christiansen C (1999) Low body mass index is an important risk factor for low bone mass and increased bone loss in early postmenopausal women. Early Postmenopausal Intervention Cohort (EPIC) study group. J Bone Miner Res 14:1622–1627
Sugimoto T, Ritter C, Morrissey J, Hayes C, Slatopolsky E (1990) Effects of high concentrations of glucose on PTH secretion in parathyroid cells. Kidney Int 37:1522–1527
Hanaire-Broutin H, Sallerin-Caute B, Poncet MF, Tauber M, Bastide R, Rosenfeld R, Tauber JP (1996) Insulin therapy and GH-IGF-I axis disorders in diabetes: impact of glycemic control and hepatic insulization. Diabetes Metab 22:245–250
Flyvbjerg A (1990) Growth factors and diabetic complications. Diabet Med 7:387–399
Genant HK, Jergas M, Palermo L, Nevitt M, Valentin RS, Black D, Cummings SR (1996) Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis. The Study of Osteoporotic Fractures Research Group. J Bone Miner Res 11:984–996
Kanazawa I, Yamaguchi T, Yamamoto M, Yamauchi M, Yano S, Sugimoto T (2007) Serum insulin-like growth factor-I is associated with the presence of vertebral fractures in postmonopausal women with type 2 diabetes mellitus. Osteoporos Int 18:1675–1681
Kanazawa I, Yamaguchi T, Yamamoto M, Yamauchi M, Yano S, Sugimoto T (2008) Combination of obesity with hyperglycemia is a risk factor for the presence of vertebral fractures in type 2 diabetic men. Calcif Tissue Int 83:324–331
Yamamoto M, Yamaguchi T, Yamauchi M, Kaji H, Sugimoto T (2007) Bone mineral density is not sensitive enough to assess the risk of vertebral fractures in type 2 diabetic women. Calcif Tissue Int 80:353–358
Yamamoto M, Yamaguchi T, Yamauchi M, Yano S, Sugimoto T (2008) Serum pentosidine levels are positively associated with the presence of vertebral fractures in postmenopausal women with type 2 diabetes. J Clin Endocrinol Metab 93:1013–1019
Thrailkill KM (2000) Insulin-like growth factor-I in diabetes mellitus: its physiology, metabolic effects, and potential clinical utility. Diabetes Technol Ther 2:69–80
McCarthy TL, Centrella M, Canalis E (1989) Insulin-like growth factor (IGF) and bone. Connect Tissue Res 20:277–282
Sugimoto T, Nishiyama K, Kuribayashi F, Chihara K (1997) Serum levels of insulin-like growth factor (IGF) I, IGF-binding protein (IGFBP)-2, and IGFBP-3 in osteoporotic patients with and without spinal fractures. J Bone Miner Res 12:1272–1279
Yamaguchi T, Kanatani M, Yamauchi M, Kaji H, Sugishita T, Baylink DJ, Mohan S, Chihara K, Sugimoto T (2006) Serum levels of insulin-like growth factor (IGF); IGF-binding protein-3, -4, and -5; and their relationships to bone mineral density and the risk of vertebral fractures in postmenopausal women. Calcif Tissue Int 78:18–24
Raskin P, Stevenson MR, Barilla DE, Pak CY (1978) The hypercalciuria of diabetes mellitus: its amelioration with insulin. Clin Endocrinol 9:329–335
Kawagishi T, Morii H, Nakatsuka K, Sasao K, Kawasaki K, Miki T, Nishizawa Y (1991) Parathyroid hormone secretion in diabetes mellitus. Contrib Nephrol 90:217–222
Reid IR (2002) Relationships among body mass, its components, and bone. Bone 31:547–555
Fujimoto WY (1996) Overview of non-insulin-dependent diabetes mellitus (NIDDM) in different population groups. Diabet Med 13:S7–S10
Lee NK, Sowa H, Hinoi E, Ferron M, Ahn JD, Confavreux C, Dacquin R, Mee PJ, McKee MD, Jung DY, Zhang Z, Kim JK, Mauvais-Jarvis F, Ducy P, Karsenty G (2007) Endocrine regulation of energy metabolism by the skeleton. Cell 130:456–469
Ferron M, Hinoi E, Karsenty G, Ducy P (2008) Osteocalcin differentially regulates beta cell and adipocyte gene expression and affects the development of metabolic diseases in wild-type mice. Proc Natl Acad Sci USA 105:5266–5270
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kanazawa, I., Yamaguchi, T., Yamamoto, M. et al. Serum Osteocalcin/Bone-Specific Alkaline Phosphatase Ratio Is a Predictor for the Presence of Vertebral Fractures in Men with Type 2 Diabetes. Calcif Tissue Int 85, 228–234 (2009). https://doi.org/10.1007/s00223-009-9272-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-009-9272-4