Abstract
Mesenchymal stem cells (MSCs) participate in regenerative osteogenesis by generating bone-forming cells. To examine the proliferative capacity of MSC populations from bone marrow and their relationship to trauma severity (multiple trauma, monofracture, atrophic nonunion), we quantified colony properties of human MSCs in vitro. Serum levels of mediators associated with bone formation were also assessed. Fifty-five individuals were enrolled in this study (13 multiple trauma patients, 15 patients with monofracture, 20 patients with atrophic nonunions, 7 healthy volunteers). The colony forming unit-fibroblast (CFU-F) assay was used to quantify total colony number, mean cell density per colony, and mean colony area. MSC phenotype was established using flow cytometry and osteogenic differentiation. MSCs obtained from multiple-trauma patients yielded the highest reservoir. Significant differences in colony numbers of MSCs in female subjects were found between multiple-trauma patients (mean ± SD 48 ± 21 CFU-F/culture) and healthy volunteers (18.7 ± 3.3 CFU-F/culture, P < 0.05), patients with monotrauma (15 ± 10 CFU-F/culture, P < 0.05), and patients with atrophic nonunions (6.3 ± 4.1 CFU-F/culture, P < 0.05). In male participants, significant differences were found between patients with nonunions (14 ± 14 CFU-F/culture) and healthy volunteers (54 ± 17 CFU-F/culture, P < 0.05) as well as multiple-trauma patients (59 ± 25 CFU-F/culture, P < 0.05). The highest proliferative capacity (cell density) was seen in multiple-trauma patients. These data suggest that trauma severity and gender affect the reservoir and proliferation capacity of bone marrow-derived MSCs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Bone-forming cells originate from mesenchymal stem cells (MSCs), which are present in red bone marrow and in mesenchymal tissues. MSCs possess both the capacity for renewal and the potential to differentiate into multiple lineages of mesenchymal tissue and have been implicated in bone tissue regeneration [1].
MSCs were isolated initially by Friedenstein et al. [2] and subsequently by other investigators who named them plastic-adherent cells or colony-forming unit fibroblasts (CFU-Fs) based on their adherence to tissue culture surfaces. MSCs are phenotypically characterized by surface expression of CD71, CD73, CD90, and CD105 proteins (cultured MSCs do not typically express CD34 and CD45) [3]. These cells can be functionally characterized by their potential for osteogenic differentiation, which is regulated by growth factors and external signals staining for alkaline phosphatase, sudan black, esterase, fibronectin, collagen IV, and calcium deposition using von Kossa staining [4–7]. The CFU-F assay has been extensively used as a tool for quantification of mesenchymal progenitors in bone marrow [8, 9]. In addition, numerous in vitro studies have demonstrated that osteogenic differentiation of purified, culture-expanded human MSCs can be achieved by supplementation of the culture medium with dexamethasone, ß-glycerophosphate, and ascorbic acid-2-phosphate [10, 11].
Contradictory results have been reported regarding the osteogenic potential and functional capacity of MSCs in adult bone marrow. Some investigators have reported an age-related decrease in the number of MSCs [7, 12], while others have found no differences in MSC number between different age groups and patients with osteoporosis [13, 14] or osteoarthritis [15]. The use of heterogeneous patient populations and the lack of appropriate controls may have contributed to these discrepant results regarding MSCs.
Cytokines and hormones are known to exert various cellular effects, ranging from induction of apoptosis to activation of cellular function and proliferation, depending on the specificity of the target cell [16]. In a clinical study, trauma patients with severe head injury presented with an increase in osteogenesis with heterotopic ossification that correlated with an increased serum concentration of prolactin [17]. Although multiple trauma (MT) patients with multiple fractures show an overstimulated immune system, atrophic nonunion patients do not typically show a systemically or locally stimulated immune response. Studies attempting to characterize tissue-specific trauma markers that reflect type and severity of tissue injury have reported a marked increase in interleukin-6 (IL-6) concentrations in the first hours after trauma that correlated significantly with the extent of fracture trauma [18]. The aim of the present study was to delineate the reservoir and functional capabilities of MSCs in the bone marrow and their relationship to trauma severity in MT vs. single fracture vs. atrophic nonunion patients compared with healthy volunteers. Colony number and colony area as determined by CFU-F assay and the proliferation capacity of MSCs as measured by mean cell density per colony were evaluated. To examine the putative influence of IL-6 on the concentration of CFU/F in the bone marrow, serum levels of IL-6 were measured and correlated with the corresponding CFU-F number. Measurement of serum IL-6 was used as a marker for the systemic inflammatory state. The results of this study support the use of MSCs in eligible patient groups as a therapeutic application of autologous ex vivo expanded MSCs.
Subjects and Methods
Protocol Design and Patient Population
Trauma patients scheduled to receive pelvic surgery were enrolled in the protocol. The severity of trauma was calculated using the injury severity score (ISS) [19, 20]. Patients with an ISS > 16 points were assigned to the MT group. Depending on trauma severity and gender, participants were divided into eight study groups (Table 1). Exclusion criteria included pathological fractures due to a tumor or fractures which were accompanied by bacterial infections. All participants or close relatives and healthy volunteers were informed of all procedures prior to signing a consent form. The ethics committee of the Johann-Wolfgang-Goethe University Hospital (Frankfurt, Germany) approved all procedures.
Isolation, Cultivation, and Characterization of MSCs
Bone marrow cells were obtained from the iliac crest aspirate of voluntary trauma patients undergoing pelvic surgery or from healthy volunteers via pelvic puncture. MSCs were isolated from fresh bone marrow aspirate using Ficoll density gradient centrifugation (30 minutes, 1,100 g, d = 1,077 g/mL; Biochrom, Berlin, Germany). Cells in interphase were collected and washed twice using phosphate-buffered saline (PBS; 10 minutes, 900 g) containing 2% fetal bovine serum (FBS). Cells were resuspended in 3 mL MesenCult + Supplements (Cell-Systems, St. Katharinen, Germany) and counted using a Neubauer chamber.
The cell suspension was then divided and used for the CFU-F assay as well as for the determination of the phenotype of the outgrowing MSC population. Cells were cultured in MesenCult + Supplements at 37°C and 5% CO2. The medium was changed three times a week.
Each 4 × 106 cells were seeded in a 25 cm2 culture flask under identical conditions as described above. The cells were expanded over three passages and then subjected to flow cytometry. In brief, cells were detached by incubation of 10 minutes with Accutase (PAA Laboratories, Linz, Austria). After one wash (10 minutes, 300 g), the cells were resuspended in PBS without Ca2+ or Mg2+ which was supplemented with 2 mM ethylenediaminetetraacetic acid (EDTA; Sigma, Deisenhofen, Germany) and 0.5% FCS (Life Technologies, Karlsruhe, Germany). Each 100 μL cell suspension containing approximately 30,000 cells was incubated with 7.5 μL of monoclonal antibodies against CD34, CD45, CD71, CD73, CD90 (BD Biosciences, Heidelberg, Germany), CD105 (Serotec, Duesseldorf, Germany), or an appropriate isotype control for 20 minutes. After final centrifugation, the cells were analyzed using a FACScan (Becton-Dickinson, Heidelberg, Germany). If a preparation did not show a typical MSC phenotype, the results of the corresponding CFU-F-assay were discarded.
CFU-F Assay
Each 5 × 105, 1 × 106, and 2 × 106 cells were seeded in 25 cm2 culture flasks (Nunc, Roskilde, Denmark). The culture medium (Mesencult + Supplements) was changed three times weekly. The cells were cultured for 14 days and subsequentely stained using Diff-Quick (Baxter, Düdingen, Switzerland). The culture flasks were then photographed, digitized, and subsequently converted to an eight-bit gray level TIFF file (Multi Analyst; Bio-Rad, Munich, Germany). The digitized CFU-F assays were used for colony counting and determination of mean colony area and mean cell number per microscopic field of view (FOV, 0.1 × 0.1 mm). Colonies were counted using the software Cell Explorer (BioSciTek, Frankfurt, Germany).
Colony Area and Cell Number per Microscopic FOV (Cell Density)
The area of the colonies was determined using the software Cell Explorer. For evaluation of the mean cell number per microscopic FOV, the following procedure was applied. DiffQuick-stained cells within 15 randomized chosen colonies obtained from five different donors were counted microscopically (×100) using an ocular grid. Within each colony, the cells in four peripheral and one central areas were counted and the mean value was calculated. The processed colonies were marked and the mean gray level (including background correction) of the corresponding digitized colony was determined using the software Multi Analyst (Bio-Rad). The mean cell number per colony was then blotted against the corresponding gray level, and a calibration curve was generated. The mean cell number per FOV was subsequently calculated by applying linear regression. All counts were performed by a single observer blinded to the donor status of the samples.
Osteogenic Differentiation
For confirmation of the plasticity, the osteogenic capacity of control samples was assessed. Osteogenic differentiation was induced by adding 0.1 μM dexamethasone, 10 mM ß-glycerophosphate, and 50 μM ascorbic acid-2-phosphate (all from Cell Systems) to the culture medium [10, 11]. After 12 days, calcium deposition was qualitatively determined using von Kossa staining.
Serum Level of Prolactin and IL-6
Serum levels of prolactin (Bayer Healthcare, Leverkusen, Germany) and IL-6 (RayBiotech; Hoelzel Diagnostika, Köln, Germany) were measured as directed by the manufacturers.
Statistics
All values are expressed as a mean ± standard deviation (SD). Statistical evaluation was performed using the Kruskall-Wallis test with the Dunn test as post-hoc analysis. At most, four groups were compared (e.g., male healthy volunteers vs. male patients with nonunions vs. male patients with a monofracture vs. male MT patients). P < 0.05 was considered significant. Correlation analysis was carried out using the Spearman-Rank test. SPSS V9.0 (SPSS, Chicago, IL) was used for all statistical analyses.
Results
Patients
A total of 55 patients and volunteers (18 female, 37 male) were enrolled in the study (mean age ± SD, 41 ± 15 years), including 20 patients with atrophic nonunions, 15 patients with monofracture, 13 MT patients, and 7 healthy volunteers (control) (Table 1).
Cell and Colony Morphology
After 12 days in culture, MSCs had a fusiform and spindle-shaped appearance (Fig. 1a,b). They proliferated and formed colonies with a morphologically homogenous cell population.
Phenotype of Cultured MSCs
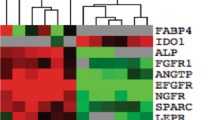
All cultures evaluated expressed a phenotype (CD34−, CD45−, CD71+, CD73+, CD90+, and CD105+) that was consistent with MSCs (Fig. 2a–e). Control samples could be successfully differentiated to an osteogenic phenotype.
Correlation between Optical Density of the Colonies and Cell Number per
Microscopic FOV (Cell Density)
The mean cell number per FOV (cell density) correlated significantly with the corresponding gray level of the colony (rho = 0.92, P < 0.00001; Fig. 3). Thus, the optical CFU-F density reflected the true cell number per colony and represents an appropriate surrogate measure of the proliferative capacity of MSCs.
Correlation of cell number/colony and gray level. Cell number/colony was blotted against the corresponding gray level of the same colony, and subsequently a calibration curve was generated. Cell number/colony correlated significantly with the corresponding gray level (rho = 0.92, P < 0.00001). Mean cell number/colony was calculated by applying linear regression.
Effect of Trauma Severity on Colony Number (Reservoir)
The mean number of colonies obtained from female MT patients was significantly higher (48 ± 21 CFU-F/culture) than that from female patients with atrophic nonunions (6.3 ± 4.1 CFU-F/culture, P < 0.05) or healthy female volunteers (control, 18 ± 3.3 CFU-F/culture, P < 0.05). Moreover, female healthy volunteers had higher CFU-F values than female patients with atrophic nonunions (6.3 ± 4.1 CFU-F/culture, P < 0.05; Fig. 4a), but no differences from female patients with monofracture (15 ± 10 CFU-F/culture) were found.
Altered properties of MSCs when cultured for 12 days. (a) Total number of colonies measured in healthy female/male volunteers (control) and in female/male patients with nonunions, monofracture, or MT. (b) Cell density was quantified for male/female patients with nonunions, monofracture, or MT. (c) Colony area of CFU-F colonies derived from patients with nonunions, monofracture, or MT. All results are presented as mean values ± SD. ⋆
P < 0.05 vs. control,  P < 0.05 vs. nonunions, and ⊕
P < 0.05 vs. monotrauma.
P < 0.05 vs. nonunions, and ⊕
P < 0.05 vs. monotrauma.
In male patients, the mean number of colonies in MT patients was significantly higher (59 ± 25 CFU-F/culture) than in patients with nonunions (14 ± 14 CFU-F/culture, P < 0.05) or with monofracture (14 ± 11 CFU-F/culture, P < 0.05). Moreover, healthy volunteers (54 ± 17 CFU-F/culture) had significantly higher CFU-F values than patients with nonunions (14 ± 14 CFU-F/culture, P < 0.05) or with monofracture (14 ± 11 CFU-F/culture, P < 0.05; Fig. 4a).
Effect of Cell Density and Mean Colony Area (Proliferative Capacity)
Significant differences were observed in colony cell density from male patients subjected to MT (57 ± 23 cells/FOV) vs. those suffering from monofracture (26 ± 19 cells/FOV, P < 0.05; Fig. 4b). Significant differences were also noted for mean colony area values between patients with monotrauma (3 mm2) and healthy volunteers (7 mm2, P < 0.05) as well as MT patients (6.6 mm2, P < 0.05). Female MT patients, healthy female volunteers, and female patients with monofracture or atrophic nonunions showed mean cell densities of 60, 26, 38, and 26 cells/FOV, respectively, and mean colony areas of 5.2, 4.2, 8.5, and 4.4 mm2, respectively.
Effect of Gender on MSC Number and MSC Proliferation
A significant difference between female and male healthy volunteers in the number and proliferative capacity of cultured MSCs was found (Fig. 4a–c). The colony number of MSCs in cultures obtained from male volunteers (54 ± 17 CFU-F) was significantly higher than that in cultures obtained from female volunteers (18 ± 3.3 CFU-F, P < 0.05). The mean cell density was also higher in male volunteers (45 cells/FOV) than in female volunteers (26 cells/ FOV). Furthermore, the mean colony area was increased in male volunteers (7 mm2) in comparison to female volunteers (4.2 mm2).
Serum Levels of Prolactin and IL-6
No significant correlation was found between the number of CFU-Fs and serum levels of prolactin and IL-6.
Discussion
The present study demonstrates the relationship between injury severity (multiple trauma, monotrauma, atrophic nonunions) and the reservoir and proliferative capacity of MSCs in bone marrow. Although previous studies have shown that the generation of MSCs in bone marrow is influenced by age and gender of the donor [9, 21, 22], our study extends the current knowledge by documenting, for the first time, that the CFU-F frequency is enhanced in patients (female) with multiple injuries and depressed in patients with atrophic nonunions (female/male) and monofractures (male).
To evaluate the presence of MSCs, several investigators have used assays for quantifying MSC number in bone marrow based solely on their ability to adhere to plastic surfaces. Previous human studies on MSCs demonstrated that the discrepancies in study results can be attributed to differences in study subjects or sampling site of bone marrow, which may influence the composition of bone marrow MSCs [23–25]. Moreover, techniques used for establishing MSC cultures have differed between studies [23, 26, 27]. Taken together, these differences demonstrate the difficulties involved in comparing diverse studies. To overcome the limitation of heterogeneous and contaminated culture assays, we used FACS analysis to unequivocally determine the mesenchymal phenotype of the cultured cells. In addition to the total number of colonies (CFU-F), which indicates the reservoir of MSCs in bone marrow, the number of cells within a colony (cell density) provides important information regarding the proliferative potential of the CFU-Fs. Accordingly, we assessed the cell density per colony and found a good correlation between the mean cell number per FOV (cell density) and the corresponding gray level of the colony (Fig. 3). Thus, the optical CFU-F density reflects the true cell number per colony and accurately indicates the proliferation capacity of the cells within the colony.
In our study, we found significantly different trauma-related changes in female and male patients. In general, the number of CFU-Fs is gender-dependent. MSCs obtained from female patients showed lower colony numbers (reservoir) compared to those from male patients. Interestingly, in female, MT patients, we detected a strong increase in colony number (reservoir) of MSCs compared to colony numbers from male MT patients.
In addition, we observed prolonged upregulation of MSC proliferation in patients with MT.
It is well known that in MT patients an increased rate of bone remodeling and turnover occurs, which requires continuous recruitment of osteoprogenitor cells. Thus, it is possible that, in MT patients, distinct mediators are released that exert MSC-promoting effects. This idea is supported by the finding that enhanced concentrations of the mediators vascular endothelial growth factor (VEGF) and transforming growth factor ß (TGF-ß) in serum from MT patients promote the differentiation of another type of progenitor cell (endothelial progenitor cells) in vitro [28]. Moreover, a review of the literature suggests that factors derived from platelets (e.g., platelet-derived growth factor [PDGF], basic fibroblast growth factor [bFGF], insulin-like growth factor I [IGF-I], TGF-ß) contribute to enhanced MSC proliferation [29]. Although it has been reported that IGF-1 is decreased [30] while TGF-ß is increased [28] following MT, whether other factors including PDGF and bFGF are also increased following MT and their influence on MSCs remains unclarified.
Evidence also exists that progenitor cells are harmed by excessive amounts of proinflammatory mediators [31] like IL-6. MT patients with multiple fractures show an overstimulated immune system, whereas atrophic nonunion patients do not typically show a systemically or locally stimulated immune response. Strecker et al. [18], attempting to characterize tissue-specific trauma markers that reflect type and severity of tissue injury, reported a marked increase in IL-6 concentrations in the first hours after trauma that correlated significantly with the extent of fracture trauma.
In our study, the measurement of serum IL-6 was used as a marker for the systemic inflammatory state, but no correlation with CFU-F number and cell density was found.
It has been previously reported that prolactin stimulates osteogenesis associated with heterotopic ossification in patients with severe head injury [17]. Additionally, other authors have described a modulating effect of prolactin on the differentiation of MSCs [32]. In the present study, we did not observe a significant correlation between serum prolactin concentrations and the corresponding MSC colony number. Taken together, our study indicates that the concentration of MSCs in bone marrow and the proliferative capacity of MSCs during MT are likely regulated by the interaction of different and as yet unknown factors.
In patients with atrophic nonunions, the reservoir of MSCs in bone marrow was found to be significantly decreased. Additionally, we could not detect a compensatory increase in the proliferative capacity in those patients with disorder of bone healing. Interestingly, in patients with a monofracture, we were able to detect also a decrease in MSC reservoir in the absence of an increase in proliferative capacity, suggesting that in local bone defects MSCs migrating from bone marrow may be beneficial [33]. It seems that a local bone defect without systemic release of mediators does not give a feedback for proliferation of MSCs in the bone marrow.
In addition to circulating hormones and serum factors, other cellular pathways may be involved in mediating the activation and inactivation of MSCs. Evidence exists that the length of telomeres determines survival and number of population doublings [34], suggesting that the frequency of MSCs in the bone marrow of elderly humans remains high but the cells cannot proliferate enough to form sufficient colonies.
In skeletal maturation, a major decline occurs up to the age of 30, with a minimally progressive decrease thereafter [23, 26, 27]. The latter is an established estimate of the in vivo osteoblastic bone-forming capacity [35, 36], indicative of a change in the skeletal dynamics from a “modeling” mode characteristic of skeletal growth to a “remodeling” mode for maintenance of the adult skeleton. This point of view was reinforced in a recent publication in which the reducing effect of sera obtained from elderly patients on the osteoblastic differentiation of an immortalized MSC line was described [37]. Interestingly, even in elderly female patients, who have a lower concentration of MSCs in the bone marrow, our study demonstrates that in the presence of MT as yet unidentified serum factors are released which may enhance the number of MSCs in bone marrow during the posttraumatic course.
Moreover, our study demonstrates clearly that patients with a high need for a cell-based therapy (nonunions) had the lowest concentration of MSCs in the bone marrow. These observations underscore the importance for future studies of identifying physiologically relevant mediators capable of enhancing the number and proliferative capacity of MSCs.
References
Buckwalter JA, Glimcher MJ, Cooper RR, Recker R (1996) Bone biology, part II. Formation, modelling, remodelling and regulation of cell function. Instr Course Lect 45:371–386
Friedenstein AJ, Petrakova KV, Kurolesova AL, Frolova GP (1968) Heterotopic transplants of bone marrow. Analysis of precursor cells for osteogenic and hematopoietic tissues. Transplantation 6:230–247
Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR (1999) Multilineage potential of adult human mesenchymal stem cells. Science 284:143–147
Bruder SP, Fink DJ, Caplan AI (1994) Mesenchymal stem cells in bone development, bone repair, and skeletal regeneration therapy. J Cell Biochem 56:283–294
Horch RE, Bannasch H, Kopp J, Andree C, Stark GB (1998) Single-cell suspensions of cultured human keratinocytes in fibrin glue reconstitute the epidermis. Cell Transplant 7:309–317
Long MW, Robinson JA, Ashcraft EA, Mann KG (1995) Regulation of human bone marrow derived osteoprogenitor cells by osteogenic growth factors. J Clin Invest 95:881–887
Quarto R, Thomas D, Liang D (1995) Bone progenitor cell deficits and the age-associated decline in bone repair capacity. Calcif Tissue Int 56:123–129
Friedenstein AJ, Chailakhjan RK, Lalykina KS (1970) The development of fibroblast colonies in monolayer cultures of guinea-pig bone marrow and spleen cells. Cell Tissue Kinet 3:393–403
Clarke E, McCann SR (1989) Age dependent in vitro stromal growth. Bone Marrow Transplant 4:596–597
Bruder SP, Jaiswal N, Haynesworth SE (1997) Growth kinetics, self renewal, and the osteogenic potential of purified human mesenchymal stem cells during extensive subcultivation and following cryopreservation. J Cell Biochem 64:278–294
Jaiswal N, Haynesworth SE, Caplan AI, Bruder SP (1997) Osteogenic differentiation of purified, culture-expanded, human mesenchymal stem cells in vitro. J Cell Biochem 64:295–312
Muschler GF, Nitto H, Boehm CA, Easley KA (2001) Age- and gender-related changes in the cellularity of human bone marrow and the prevalence of osteoblastic progenitors. J Orthop Res 19:117–125
Stenderup K, Justesen J, Eriksen EF, Rattan SI, Kassem M (2001) Number and proliferative capacity of osteogenic stem cells are maintained during aging and in patients with osteoporosis. J Bone Miner Res 16:1120–1129
Justesen J, Stenderup K, Eriksen EF, Kassem M (2002) Maintenance of osteoblastic and adipocytic differentiation potential with age and osteoporosis in human marrow stromal cell cultures. Calcif Tissue Int 71:36–44
Muschler GF, Boehm C, Easley K (1997) Aspiration to obtain osteoblast progenitor cells from human bone marrow: the influence of aspiration volume. J Bone Joint Surg Am 79:1699–1709
Lin E, Calvano SE, Lowry SF (2000) Inflammatory cytokines and cell response in surgery. Surgery 127:117–126
Wildburger R, Zarkovic N, Tonkovic G, Skoric T, Frech S, Hartleb M, Loncaric I, Zarkovic K (1998) Post-traumatic hormonal disturbances: prolactin as a link between head injury and enhanced osteogenesis. J Endocrinol Invest 21:78–86
Strecker W, Gebhard F, Rager J, Brückner UB, Steinbach G, Kinzl L (1999) Early biochemical characterization of soft-tissue trauma and fracture trauma. J Trauma 47:358–364
Baker SP, O’Neill B, Haddon W Jr, Long WB (1974) The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 14:187–196
Greenspan L, McLellan BA, Greig RN (1985) Abbreviated injury scale and injury severity score: a scoring chart. J Trauma 25:60–64
Mareschi K, Ferrero I, Rustichelli D, Aschero S, Gammaitoni L, Aglietta M, Madon E, Fagioli F (2006) Expansion of mesenchymal stem cells isolated from pediatric and adult donor bone marrow. J Cell Biochem 97:744–754
Bergman RJ, Gazit D, Kahn AJ, Gruber H, McDougall S, Hahn TJ (1996) Age-related changes in osteogenic stem cells in mice. J Bone Miner Res 11:568–577
Majors AK, Boehm CA, Nitto H, Midura RJ, Muschler GF (1997) Characterization of human bone marrow stromal cells with respect to osteoblastic differentiation. J Orthop Res 15:546–557
Oreffo RO, Bennett A, Carr AJ, Triffitt JT (1998) Patients with primary osteoarthritis show no change with aging in the number of osteogenic precursors. Scand J Rheumatol 27:415–424
Oreffo RO, Bord S, Triffitt JT (1998) Skeletal progenitor cells and ageing human populations. Clin Sci (Lond) 94:549–555
Nishida S, Endo N, Yamagiwa H, Tanizawa T, Takahashi HE (1999) Number of osteoprogenitor cells in human bone marrow markedly decreases after skeletal maturation. J Bone Miner Metab 17:171–177
D’Ippolito G, Schiller PC, Ricordi C, Roos BA, Howard GA (1999) Age-related osteogenic potential of mesenchymal stromal stem cells from human vertebral bone marrow. J Bone Miner Res 14:1115–1122
Henrich D, Hahn P, Wahl M, Wilhelm K, Dernbach E, Dimmeler St, Marzi I (2004) Serum derived from multiple trauma patients promotes the differentiation of endothelial progenitor cells in vitro: possible role of transforming growth factor-ß1 and vascular endothelial growth factor165. Shock 21:13–16
Doucet C, Ernou I, Zhang Y, Llense R, Begot L, Holy X, Lataillade JJ (2005) Platelet lysates promote mesenchymal stem cell expansion: a safety substitute for animal serum in cell-based therapy applications. J Cell Physiol 205:228–236
Clark MA, Hentzen BT, Plank LD, Hill GI (1996) Sequential changes in insulin-like growth factor 1, plasma proteins, and total body protein in severe sepsis and multiple injury. JPEN J Parenter Enteral Nutr 20:363–370
Henrich D, Seebach C, Wilhelm K, Marzi I (2006) High dosage of simvastatin reduces TNF-α induced apoptosis of endothelial progenitor cells but fails to prevent apoptosis induced by IL-1β in vitro. J Sur Res (in press)
Ogueta S, Munoz J, Obregon E, Delgado-Baeza E, Garcia-Ruiz JP (2002) Prolactin is a component of the human synovial liquid and modulates the growth and chondrogenic differentiation of bone marrow-derived mesenchymal stem cells. Mol Cell Endocrinol 25:51–63
Roufosse CA, Direkze NC, Otto WR, Wright NA (2004) Circulating mesenchymal stem cells. Int J Biochem Cell Biol 36:585–597
Sethe S, Scutt A, Stolzing A (2005) Aging of mesenchymal stem cells. Ageing Res Rev 5:91–116
Brockstedt H, Kassem M, Eriksen EF, Mosekilde L, Melsen F (1993) Age- and sex-related changes in iliac cortical bone mass and remodeling. Bone 14:681–691
Kragstrup J, Melsen F, Mosekilde L (1983) Thickness of bone formed at remodeling sites in normal human iliac trabecular bone: variations with age and sex. Metab Bone Dis Relat Res 5:17–21
Abdallah BM, Haack-Sorensen M, Fink T, Kassem M (2006) Inhibition of osteoblast differentiation but not adipocyte differentiation of mesenchymal stem cells by sera obtained from aged females. Bone 39:181–188
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Seebach, C., Henrich, D., Tewksbury, R. et al. Number and Proliferative Capacity of Human Mesenchymal Stem Cells Are Modulated Positively in Multiple Trauma Patients and Negatively in Atrophic Nonunions. Calcif Tissue Int 80, 294–300 (2007). https://doi.org/10.1007/s00223-007-9020-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-007-9020-6