Abstract
The etiology of primary osteoporosis in young and middle-aged men is unknown. We have studied osteoblast function in cells derived from men with idiopathic osteoporosis and in control cells from age-matched men with osteoarthrosis. Osteoblasts were isolated from transiliac bone biopsies. Osteoblast function was measured as vitamin D-stimulated osteocalcin production and production of cytokines and factors involved in osteoclast activation and bone formation. Cell proliferation was measured as 3H-thymidine incorporation. Parathyroid hormone-related peptide (PTHrP) mRNA was measured using reverse-transcriptase polymerase chain reaction. In osteoporotic men, bone mineral density at the femoral neck was correlated to in vitro production of osteocalcin. Osteoblasts from osteoporotic men produced significantly less osteocalcin after vitamin D stimulation but had increased production of macrophage colony-stimulating factor (M-CSF) compared to controls. The osteocalcin response was negatively correlated to production of M-CSF, interleukin-6, and C-terminal propeptide of type I collagen. Basal 3H-thymidine incorporation was similar in cells from osteoporotic patients and controls. PTHrP (10−9 M) significantly increased cell proliferation in control cells but not in osteoporotic cells. Basal PTHrP mRNA levels were significantly higher in osteoporotic cells than in cells from controls. The results are in agreement with previous histomorphologic studies indicating that men with idiopathic osteoporosis have an osteoblast dysfunction with decreased osteocalcin production and increased production of factors stimulating osteoclast activation. This indicates a catabolic cellular metabolic balance leading to negative bone turnover, resulting in osteoporosis. The cause of such cellular dysfunction needs further evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Male osteoporosis is often related to secondary causes, such as hypogonadism, glucocorticoid treatment, excessive alcohol intake, or malabsorption. In approximately 40% of the male patients with osteoporosis, the etiology is unknown; male idiopathic osteoporosis (MIO). Histomorphologic data from MIO patients suggest a disturbed balance with an increase in bone resorption and decreased bone formation [1]. Studies of biochemical bone turnover markers in men with osteoporosis have indicated increased bone turnover [2–4].
There are increasing data supporting an important role for estrogen in the male skeleton [5, 6]. In MIO, low levels of serum estradiol [4, 7, 8] and high levels of sex hormone-binding globulin (SHBG) [4, 7] have been reported. A lower abundance of estrogen receptor α has been found in osteoblasts and osteocytes from MIO patients [9]. Polymorphisms of estrogen receptor α and estrogen receptor β have been related to bone mineral density (BMD) in both men and women [10–12]. Estradiol stimulates osteoprotegerin (OPG) synthesis [13] and decreases interleukin-6 (IL-6) production [14] in cultured human osteoblast-like cells. Estradiol has also been reported to regulate vitamin D receptor (VDR) expression in vitro [15] and in vivo [16]. Thus, low estradiol or decreased receptor activation would negatively influence osteoblast function. Decreased bone formation in MIO due to low circulating insulin-like growth factor I (IGF-I) has also been suggested [17, 18].
Parathyroid hormone (PTH) and PTH-related peptide (PTHrP) are peptide hormones that have anabolic effects on bone. PTHrP is produced in the osteoblast and stimulates cell proliferation [19]. A decreased proliferative response to PTHrP could be hypothesized in conditions with low bone formation.
Vitamin D-stimulated osteocalcin production is commonly used to characterize osteoblasts in culture. Osteocalcin is involved in the mineralization process and is considered a marker for a mature osteoblast [20]. Osteoblast function has been evaluated in vitro in cells isolated from bone specimens of women with postmenopausal osteoporosis [21, 22] and of men with osteoporosis [23]. In both sexes, cell proliferation was decreased in patients with low bone formation. However, osteocalcin production and alkaline phosphatase (ALP) activity were not correlated to histomorphologic parameters of bone formation. In the present study, we investigated whether osteoblast-like cells derived from bone biopsies of MIO patients were different from those of age-matched men with osteoarthrosis with respect to osteocalcin production, production of cytokines involved in regulation of bone turnover, or cell proliferation. We also studied a possible correlation between these parameters of osteoblast function and the degree of osteoporosis or serum levels of sex hormones and IGF-I.
Materials and Methods
Experimental Subjects
Transiliac bone biopsies from men with MIO were obtained when the patients underwent a clinical biopsy for histomorphologic analysis. From March 1999 through May 2002, 24 Caucasian men with MIO were evaluated with bone biopsies at the Department of Endocrinology and Diabetology, Karolinska Hospital (Stockholm, Sweden). Nineteen accepted enrollment in the study, which included an additional biopsy for bone cell culture. In six patients, the orthopedic surgeon refrained from the second biopsy for technical or medical reasons (e.g., local pain). Thirteen biopsies were used for isolation of osteoblast-like cells. The material from one patient was lost due to infection of the cell culture.
The 12 male patients evaluated had a median age of 56.5 years (range 29–68). They had osteoporosis diagnosed by BMD, using dual-energy X-ray absorptiometry (DXA) and T score <−2.5 standard deviations (SD) compared to the male reference at the lumbar spine and/or hip. Ten of the 12 had a history of fractures: seven had vertebral fractures, one had a hip fracture, and two had other peripheral fractures. The fractures occurred at least 5 months prior to the bone biopsy. The patients had no clinical or laboratory signs of secondary osteoporosis. They were not on any medication that could interfere with bone metabolism except for calcium and vitamin D supplementation. At the time of biopsy, all of the patients had a diet sufficient in calcium or supplementation with calcium and vitamin D3. Clinical data are presented in Table 1.
As controls, we obtained transiliac bone biopsies from 12 age-matched men with coxarthrosis (n = 10) or low back pain (n = 2). Biopsies were taken during hip replacement surgery or lumbar fusion surgery, respectively. Controls were selected by age to obtained matched material. They accepted enrollment in the study. Except for arthrosis, they were healthy and had no history of osteoporosis, low-energy trauma fractures, or treatment with glucocorticoids. Half of the osteoarthrosis patients were on regular medication with nonsteroidal anti-inflammatory drugs until 2 weeks prior to surgery. The 12 controls had a median age of 56 years (range 38–62) and body mass index (BMI) of 25.2 ± 2.5 kg/m2 (mean ± SD). No BMD measurements or hormone levels were analyzed in the control group.
The study was approved by the committee for medical ethics at the Karolinska Institute.
BMD Measurements
BMD at total body, lumbar spine, and femoral neck was measured with Hologic (Waltham, MD) QDR 4500 DXA and Lunar (Madison,WI) DPX-L. The data are given as T score, with SD from the mean of normal young adult males given from a reference population provided by the manufacturer.
Biochemical Analysis
Serum concentrations of sex hormones, SHBG, IGF-I, IGF-binding protein-1 (IGFBP-1), and serum and urine markers of bone formation and resorption were analyzed in the osteoporotic patients. Serum concentrations of estradiol-17ß (E2) were determined by radioimmunoassay (RIA) using a commercial kit obtained from Orion Diagnostica (Borgå, Finland). The detection limit was 5 pmol/L. Serum concentrations of testosterone (T) and SHBG were measured by time-resolved fluorescence immunoassays using commercial kits obtained from PE Wallac (Turku, Finland; Autodelfia®). E2-free index and T-free index are given as the ratio between E2 or T, respectively, and SHBG. IGF-I was determined in serum by RIA after separation of IGFs from IGFBPs by acid-ethanol extraction and cryoprecipitation and with des(1–3)IGF-I as the radioligand to minimize interference of remaining IGFBPs in the extract [24]. The detection limit was 8 μg/L. The intra- and interassay variations were 4% and 11%, respectively. Normal range of IGF-I was established in 448 healthy subjects [25]. IGFBP-1 was analyzed by the method described by Povoa and coworkers [26]. The detection limit was 3 μg/L, and the intra- and interassay variations were 3% and 10%, respectively.
Serum concentrations of bone-specific alkaline phosphatase (BALP) were determined by immunoradiometric assay using a commercial kit from Hybritech (San Diego, CA). Urinary N-telopeptide of collagen cross-links (NTX) was determined by enzyme-linked immunosorbent assay (ELISA) using a commercial kit Osteomark from Unipath Limit (Bedford, UK).
Isolation of Osteoblast-Like Cells
The biopsy was kept in α-minimal essential medium (MEM; GIBCO, Grand Island, NY) supplemented with 2 mM L-glutamine (GIBCO), 50 IU/L penicillin, and 50 μg/mL streptomycin (GIBCO) at 4°C. Within 8 hours, the biopsy was carefully dissected and the trabecular bone isolated. Thereafter, the bone was cut into 2 × 2 mm fragments and incubated in α-MEM with 1 mg/mL type IV collagenase for 15 minutes at 37°C under continuous shaking. This procedure was repeated three times with changes of collagenase solution. Finally, fragments were transferred to 75 cm2 culture flasks containing α-MEM with v/v 10% fetal calf serum, L-glutamine, penicillin, and streptomycin in the same concentrations as before to allow osteoblast migration. Cells were then grown to confluence (4–6 weeks) with changes of cell medium twice a week.
Calcitriol-Induced Osteocalcin Production
Cells from MIO patients and controls were seeded in 24-well plates, 50,000 cells/well, in cell culture medium (as above). After 4 days of incubation, cells were rinsed twice with phosphate-buffered saline (PBS) before incubation with or without 10−8 M 1,25-dihydroxyvitamin D3 in serum-free cell culture medium with 0.1% bovine serum albumin (BSA) for 96 hours. The conditioned medium was then removed from the cells and immediately frozen at −20°C for later analysis. Osteocalcin was analyzed with a commercial RIA purchased from Electra-Box Diagnostics (Tyresö, Sweden). The detection limit of the assay was 0.4 ng/mL, and the intra- and interassay variations were 3% and 5%, respectively. Duplicate wells were used for every observation. Basal osteocalcin production without vitamin D stimulation was very low in all samples. Data are presented as the increase (Δ) seen after vitamin D stimulation. In the MIO group, two samples were lost (n =10).
ALP Staining
After removal of cell medium for osteocalcin analysis, the cells remaining in the wells were stained for ALP. Cells were washed twice with 1 mL of a cytochemical staining assay buffer (50 mM Tris, 100 mM NaCl, 1 mM CaCl2, 5 mM KCl, 1 mM MgCl2, pH 8.6) and incubated in 1 mg/mL naphthol AS-TR phosphate with 0.2 mg/mL diazonium salt fast-red LB in assay buffer at 37°C for 20–30 minutes. After removal of the substrate, three washes with PBS and fixation with ice-cold 95% ethanol were made. Staining of ALP activity was evaluated semiquantitatively. All cells were positive for ALP staining, indicating an osteoblastic phenotype.
Analysis of Cytokines in the Cell Medium
Cells from MIO men and control men were seeded in six-well plates, 50,000 cells/well, in cell culture medium (as above). After 4 days of incubation, cells were rinsed twice with PBS before incubation with serum-free cell culture medium (as above) for 24 hours. The conditioned medium was then removed from the cells and immediately frozen at −20°C for later analysis. Samples from all patients and controls were analyzed with the same kit to minimize interassay variation.
Production of type 1 collagen C-terminal propeptide (P1CP) was analyzed using an RIA from Orion Diagnostica, with a detection limit of 1.2 μg/L.
IL-6 production was measured by a solid-phase ELISA (Milenia Biotech, Bad Nauheim, Germany) performed on microtiter plates. The detection limit for the assay was 1.2 pg/mL.
Human macrophage colony-stimulating factor (M-CSF) production was determined by a sandwich enzyme immunoassay, Quantikine (R&D Systems Europe, Abingdon, UK). The detection limit of the assay was 9 pg/mL.
OPG production was measured by a sandwich-type ELISA (Immundiagnostik, Bensheim, Germany). The detection limit of the assay was 0.14 pmol/L. tRNA was extracted from cells as described below. Results are given as units per micrograms of tRNA in the well.
RNA Extraction and Reverse-Transcriptase Polymerase Chain Reaction
The cells from the experiments described above were used for extraction of tRNA with Trizol reagent for 5 minutes. Chloroform (0.2 mL/mL Trizol) was added. Tubes were shaken strongly for 15 seconds and left at room temperature for 2–3 minutes before centrifugation at 12,000g for 15 minutes at 4°C. The upper phase was removed to a new tube, and isopropanol (0.6 mL/mL Trizol) was added. After incubation for 5–10 minutes at room temperature, samples were centrifuged at 12,000g for 20 minutes at 4°C. The supernatant was discarded and the pellet washed with ice-cold 75% ethanol. After centrifugation at 10,000g for 5 minutes at 4°C, the supernatant was discarded and the dried sample dissolved in diethylpyrocarbonate-treated RNAse-free water and denaturated at 65°C for 10 minutes. RNA concentrations were measured by spectrophotometry (GeneQuant II; Pharmacia Biotech Cambridge, England). Reverse transcription was performed with the commercial 1st cDNA Synthesis Kit for reverse-transcriptase polymerase chain reaction (RT-PCR; Boehringer-Mannheim, Mannheim, Germany).
PTHrP mRNA expression was determined by quantitative RT-PCR assay with time-resolved fluorometry as described previously [27, 28]. The amount of PTHrP mRNA in the sample was determined by a linear regression equation derived from a calibration curve with a PTHrP cDNA standard and standardized to copies of PTHrP cDNA/μg tRNA.
3H-Thymidine Incorporation
Proliferation of osteoblast-like cells was determined by quantifying DNA synthesis through incorporation of 3H-thymidine, applied as an index of cell proliferation. Briefly, osteoblast-like cells were seeded into 12-well tissue culture plates at a density of 20,000–40,000/well in culture medium (see above) and allowed to grow for approximately 4 days until subconfluence. Cells were washed twice with PBS and cultivated for 24 hours in serum-free culture medium with 0.1% BSA. Cells were then incubated with PTHrP(1–34) (10−9 M) for 48 hours in serum-free culture medium together with 3H-thymidine (1 μCi/mL) for the last 24 hours. Serum-free medium was used as negative control. Fetal bovine serum was used as positive control. The medium was removed, and cells were rinsed twice with 1 mL ice-cold 0.09 % NaCl. Cells were incubated with 1 mL ice-cold 5% trichloroacetic acid for 15 minutes. After removal of trichloroacetic acid, the precipitated layer was solubilized in 0.5 mL of 0.1 M NaOH for 2 hours at room temperature under constant shaking. Radioactivity was counted in a β-counter after addition of Ultima Gold scintillation liquid to the samples. Basal 3H-thymidine incorporation was evaluated in 10 patients with MIO and in 12 controls. Cells from six MIO and six age-matched controls were evaluated for PTHrP-stimulated cell proliferation. Data for each individual represent an average from four to six wells.
Statistical Analysis
Statistical analysis was performed by Mann-Whitney U-test. A nonparametric test was chosen as the number of patients was small and the data in most cases were not normally distributed. Data in the graphs are given as mean ± SD or as median and range. Correlations were calculated using Spearman’s rank order correlation. P < 0.05 was considered statistically significant.
Results
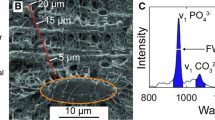
Cultures of osteoblast-like cells from MIO were compared to cells from control men. In order to evaluate differences in osteoblast maturation, we analyzed vitamin D-stimulated osteocalcin production. Basal production of osteocalcin was low in both study groups. In 8/12 MIO cases and 5/12 controls, levels were undetectable and there was no significant difference between the groups (median, range): MIO 0.10 ng/mL (0.1–2.0) and control 0.55 ng/ml (0.1–1). Incubation with 1,25-vitamin D3 stimulated osteocalcin production in all cell cultures. Cells from MIO had a decreased response to 1,25-vitamin D3; Δosteocalcin 10.7 ± 5.3 (mean ± SD) compared to controls 18.3 ± 8.2, P < 0.01 (Fig. 1). There was no correlation between the age of the donor and stimulated osteocalcin production.
Cell proliferation was evaluated by measuring DNA synthesis by 3H-thymidine incorporation. Basal thymidine incorporation did not differ between MIO and control cells: 16,802 ± 14,577 cpm and 10,333 ± 4,407 cpm, respectively, P > 0.05. In order to study if cells from MIO cases had a different proliferative response to an anabolic stimulus, osteoblast cultures were incubated with PTHrP. Incubation with PTHrP (10−9 M) significantly stimulated 3H-thymidine incorporation in control cells but had no effect in MIO cells (Fig. 2). Basal expression of PTHrP mRNA was significantly increased in MIO cells compared to controls (Fig. 3).
Production of cytokines involved in bone remodelling was analyzed in medium from MIO and control cells. MIO cells had increased production of M-CSF compared to controls. There were no statistically significant differences between MIO and control cells in the production of P1CP, OPG, or IL-6 (Table 2). Production of IL-6 was correlated to the age of the donor in controls (r = 0.67, P < 0.05) but not in MIO patients. There were no correlations with age and in vitro production of M-CSF, OPG, or P1CP.
In osteoblast-like cell cultures, there was a positive correlation between production of factors associated with bone formation and bone resorption (Table 3).
Calcitriol-stimulated osteocalcin production was negatively correlated to production of M-CSF (Fig. 4), IL-6 (Fig. 5), and P1CP (Fig. 6) in osteoblast cultures when all observations from MIO and control samples were evaluated together. There were significant correlations between Δosteocalcin and IL-6 in MIO cases and between Δosteocalcin and IL-6 and P1CP in controls.
To evaluate if the in vitro findings could mirror the clinical presentations, correlations to BMD, levels of circulating hormones, or bone turnover markers were tested.
When calcitriol-stimulated osteocalcin production in vitro was correlated to BMD, a significant correlation to femoral neck BMD was observed (Fig. 7). There was no correlation with other BMD sites, e.g., lumbar spine or total body.
A significant correlation between the in vitro production of P1CP and free E2 index was observed, r = 0.78, P < 0.01.
Discussion
The in vitro data presented in this study are in agreement with the histomorphologic findings in MIO, indicating impaired formation and increased bone resorption. The increased production of M-CSF seen in MIO osteoblasts could be related to increased bone resorption. M-CSF is produced by bone marrow stromal cells and osteoblasts and is necessary for the recruitment and activation of osteoclasts [29]. It has also been suggested that M-CSF inhibits osteoblast maturation [30]. The resorption marker urinary NTX was elevated in 7/11 MIO patients, indicating increased bone resorption. However, there was no correlation between urinary NTX and in vitro M-CSF production.
Only a few studies on osteoblast function in men have been published. In men without osteoporosis, the response to calcitriol with increased ALP activity and osteocalcin production was similar in cells from young and older men [31]. We have similar results. No age-dependent effect on osteocalcin production was seen. In the present study, cells from MIO patients had a significantly lower osteocalcin response to calcitriol compared to controls. Contrary to our results, Marie and coworkers [23] reported normal osteocalcin production in cells from eugonadal osteoporotic men. In our study, all bone cells were isolated from transiliac biopsies, whereas control cells in the other studies were isolated from trabecular bone specimens obtained during surgery. This may explain the differences in results. Bone cells of different skeletal origin have different osteocalcin responses to vitamin D [32].
There was an inverse relationship between osteocalcin production and the production of IL-6, M-CSF, and P1CP. Osteoblast cultures with the lowest production of osteocalcin had higher production of all of the three factors. M-CSF and IL-6 are related to increased bone turnover and resorption. A negative correlation to M-CSF and IL-6 would be in agreement with a disturbed balance between formation and resorption. However, we also observed a negative correlation with P1CP, which is considered an anabolic factor related to synthesis of collagen-1. In osteoblast cultures, basal production of factors related to bone formation (OPG and P1CP) was positively correlated to cytokines of bone resorption (M-CSF and IL-6). The pattern of cytokines produced by the MIO osteoblast would favor increased bone turnover with increased osteoclast activiation.
In the MIO patients, the osteocalcin response to calcitriol stimulation in vitro was correlated to BMD at the femoral neck. Cells from patients with more severe osteoporosis had a lower osteocalcin response. No correlation was observed between basal osteocalcin production and BMD. The significance of this finding needs to be confirmed since the number of patients is low.
A possible mechanism for the impaired bone formation in MIO could be a difference in osteoblast proliferation and the response to anabolic hormones. We previously demonstrated stimulatory effects of PTHrP on cell proliferation in bone marrow stromal cells [19]. In the present study, the interindividual variation in basal cell proliferation was large and no significant difference between MIO and control cells could be seen. However, PTHrP(1–34) significantly stimulated proliferation in control cells, but this could not be seen in MIO cells. We also measured mRNA levels for PTHrP to evaluate endogenous production in bone cells. Cells from MIO cases had significantly higher levels than controls. PTH/PTHrP can exhibit both anabolic and catabolic effects on bone. Continuous PTH activity stimulates bone resorption, whereas intermittent administration increases bone formation [33]. We hypothezise that the higher constitutive PTHrP production in MIO cells downregulates the anabolic response to exogenous PTHrP.
We have demonstrated differences in osteocalcin response and M-CSF production in cells cultivated for several weeks. This indicates a genomic effect. One possible explanation is differences in VDR content or activity. Polymorphism in the VDR has been correlated to osteocalcin response. Osteoblasts with VDR alleles of the BB, tt, or A type have a lower osteocalcin response to calcitriol [34]. Alleles of the At type have also been associated with lower BMD in men [35].
MIO patients had serum E2 levels in the low or low/normal range, as in several other published reports on male osteoporosis [4, 7, 8]. A relative vitamin D resistance is in agreement with low E2 levels. It has been shown that E2 regulates VDR expression in osteoblast-like cells [15]. It has further been suggested that calcitriol inhibits PTHrP production in osteoblast-like cells [36]. An attenuated effect of calcitriol is in accordance with a decreased osteocalcin response and increased PTHrP expression. However, the present data do not provide evidence for this speculation, which needs further study.
In the control osteoblast cultures, IL-6 production increased with the age of the donor. Bone resorption markers increase with age, and this has partly been explained by a decrease in sex hormones. Changes in osteoblast cytokine production may also be involved. However, the number of observations in the present study is small and the finding needs to be confirmed.
No correlations between serum hormones and in vitro production of osteocalcin or cytokines could be demonstrated except for a positive correlation between P1CP and free E2 index. The significance of this finding is uncertain. Hormone measurements were performed only in MIO patients, so the number of observations is small.
Most of the studies on human osteoblast-like cells are performed on cells isolated from bone specimens obtained during surgery, often from patients with osteoarthrosis. The control cells in the present study were from patients with osteoarthrosis and not from normal healthy individuals. This is a limitation since it cannot be ruled out that the osteoarthrosis condition may influence osteoblast function.
In conclusion, osteoblast-like cells isolated from men with MIO have decreased production of osteocalcin, indicating impaired bone formation and increased production of M-CSF and PTHrP, which could be related to increased bone resorption.
References
Chavassieux P, Meunier PJ (2001) Histomorphometric approach of bone loss in men. Calcif Tissue Int 69:209–213
Khosla S, Melton JL III, Atkinson AT, O´Fallon WM, Klee GG, Riggs LB (1988) Relationship between serum sex steroid levels and bone turnover markers with bone mineral density in men and women: a key role for bioavailable estrogen. J Clin Endocrinol Metab 83:2266–2274
Resch H, Pietschmann P, Woloszczuk W, Krexner E, Bernecker P, Willvonseder R (1992) Bone mass and biochemical parameters of bone metabolism in men with spinal osteoporosis. Eur J Clin Invest 22:542–545
Pietschmann P, Kudlacek S, Grisar J, Spitzauer S, Woloszczuk W, Willvonseder R, Peterlik M (2001) Bone turnover markers and sex hormones in men with idiopathic osteoporosis. Eur J Clin Invest 31:444–451
Byers RJ, Hoyland JA, Braidman IP (2001) Osteoporosis in men: a cellular endocrine perspective of an increasingly common clinical problem. J Endocrinol 168:353–362
Szuluc P, Munoz F, Claustrat B, Garnero P, Marchand F, Duboeuf F, Delmas PD (2001) Bioavailable estradiol may be an important determinant of osteoporosis in men: the MINOS study. J Clin Endocrinol Metab 86:192–199
Gillberg P, Johansson AG, Ljunghall S (1999) Decreased estradiol levels and free androgen index and elevated sex hormone-binding globulin levels in male idiopathic osteoporosis. Calcif Tissue Int 64:209–213
Carlsen CG, Soerensen TH, Eriksen EF (2000) Prevalence of low serum estradiol levels in male osteoporosis. Osteoporosis Int 11:697–701
Braidman I, Baris C, Wood L, Selby P, Adams J, Freemont A, Hoyland J (2000) Preliminary evidence for impaired estrogen receptor α-protein expression in osteoblasts and osteocytes from men with idiopathic osteoporosis. Bone 26:423–427
Ongphiphadhanakul B, Rajatanavin R, Chanprasertyothin S, Piaseu N, Chailurkit L (1998) Serum oestradiol and oestrogen receptor gene polymorphism are associated with bone mineral density independently of serum testosterone in normal males. Clin Endocrinol 49:803–809
Ioannidis JP, Stavrou I, Trikalinos TA, Zois C, Brandi ML, Genari L, Albagha O, Ralston SH, Tsatsoulis A (2002) Association of polymorphisms of the estrogen receptor alpha gene with bone mineral density and fracture risk in women: a meta-analysis. J Bone Miner Res 17:2048–2060
Shearman AM, Karasik D, Gruenthal KM, Demissie S, Cupples A, Housman DE, Kiel DP (2004) Estrogen receptor β polymorphisms are associated with bone mass in women and men: the Framingham study. J Bone Miner Res 19:773–781
Bord S, Ireland DC, Beavan SR, Compston JE (2003) The effects of estrogen on osteoprotegerin, RANKL and estrogen receptor expression in human osteoblasts. Bone 32:136–141
Chen FP, Lee N, Wang KC, Soong YK, Huang KE (2002) Effect of estrogen and 1α,25(OH)2-vitamin D3 on the activity and growth of human osteoblast-like cells in vitro. Fertil Steril 77:1038–1043
Liel Y, Kraus S, Levy J, Shany S (1992) Evidence that estrogens modulate activity and increase the number of 1,25-dihydroxyvitamin D receptors in osteoblast-like cells (ROS17/2,8). Endocrinology 130:2597–2601
Duque G, Abdaimi KE, Macoritto M, Miller MM, Kremer R (2002) Estrogens (E2) regulate expression and response of 1,25-dihydroxyvitamin D3 receptors in bone cells: changes with aging and hormone deprivation. Biochem Biophys Res Commun 299:446–454
Johansson AG, Eriksen EF, Lindh E, Langdahl B, Blum WF, Lindahl A, Ljunggren O, Ljunghall S (1997) Reduced serum levels of the growth hormone dependent insulin-like growth factor binding protein and a negative bone balance at the level of individual remodeling units in idiopathic osteoporosis in men. J Clin Endocrinol Metab 82:2795–2798
Kurland ES, Rosen CJ, Cosman F, McMahon D, Chan F, Shane E, Lindsay R, Dempster D, Bilezikian JP (1997) Insulin-like growth factor-I in men with idiopathic osteoporosis. J Clin Endocrinol Metab 82:2799–2805
Lagumdzija A, Oh G, Petersson M, Bucht E, Gonon A, Pernow Y (2004) Inhibited anabolic effect of insulin-like growth factor-I on stromal bone marrow cells in endothelial nitric oxide synthase-knockout mice. Acta Physiol Scand 182:29–35
Lian JB, Stein GS, Aubin JE (2003) Bone formation: maturation and function activities of osteoblast linage cells. In: Primer on the metabolic bone diseases and disorders of mineral metabolism, 5th ed., ASBMR, Washington, DC, pp 13–28
Marie PJ, Sabbagh A, de Vernejoul MC, Lomri A (1989) Osteocalcin and deoxyribonucleic acid synthesis in vitro and histomorphometric indices of bone formation in postmenopausal osteoporosis. J Clin Endocrinol Metab 69:272–279
Marie PJ, Hott M, Launay JM, Graulet AM, Gueris J (1993) In vitro production of cytokines by bone-surface-derived osteoblastic cells in normal and osteoporotic postmenopausal women: relationship with cell proliferation. J Clin Endocrinol Metab 77:824–830
Marie PJ, de Vernejoul MC, Connes D, Hott M (1991) Decreased DNA synthesis by cultured osteoblastic cells in eugonadal osteoporostic men with defective bone formation. J Clin Invest 88:1167–1172
Bang P, Eriksson U, Sara V, Wivall IL, Hall K (1991) Comparison of acid ethanol extraction and acid gel filtration prior to IGF-1 and IGF-2 radioimmunoassays: improvement of determination in acid ethanol extracts by the use of truncated IGF-I as radioligand. Acta Endocrinol (Copenh) 124:620–629
Hilding A, Hall K, Wivall-Helleryd IL, Sääf M, Melin AL, Thoren M (1999) Serum levels of insulin-like growth factor-I in 152 patients with growth hormone deficiency, aged 19–82 years, in relation to those in healthy subjects. J Clin Endocrinol Metab 84:2013–2019
Povoa G, Roovete A, Hall K (1984) Cross reaction of somatomedin-binding protein a radioimmunoassay developed for somatomedin binding protein isolated from human amniotic fluid. Acta Endocrinol (Copenh) 107:563–570
Rong H, Hong J, Pernow Y, Sjöstedt U, Bucht E (1997) Quantitation of parathyroid hormone-related protein mRNA by competitive PCR using time-resolved lanthanide fluorometry. Clin Chem 43:2268–2273
Tsai JA, Rong H, Torring O, Matsushita H, Bucht E (2000) Interleukin-1β?upregulates PTHrP-mRNA expression and protein production and decreases TGF-β in normal human osteoblast-like cells. Calcif Tissue Int 66:363–369
Mundy GR, Chen D, Oyajobi BO (2003) Bone remodeling. In: Primer on the metabolic bone diseases and disorders of mineral metabolism, 5th ed., ASBMR, Washington, DC, pp 46–58
Gyda M, Corisdeo S, Zaidi M, Troen BR (2001) Macrophage colony stimulating factor suppresses osteoblast formation. Biochem Biophys Res Commun 285:328–334
Katzburg S, Lieberherr M, Ornoy A, Klein BY, Hendel D, Somjen D (1999) Isolation and hormonal responsiveness of primary cultures of human bone-derived cells: gender and age differences. Bone 25:667–673
Martinez P, Moreno I, de Miguel F, Vila V, Esbrit P, Martinez ME (2001) Changes in osteocalcin response to 1,25-dihydroxyvitamin D3 stimulation and basal vitamin D receptor expression in human osteoblastic cells according to donor age and skeletal origin. Bone 29:35–41
Karaplis AC, Goltzman D (2000) Parathyroid hormone and parathyroid hormone-related peptide effects on the skeleton. Rev Endocr Metab Disord 1:331–341
Naves M, Alvarez-Hernandez D, Fernandez-Martin JL, Paz-Jimenez J, Garcia Prado P, Fernandex-Coto T, Santamaria I, Cannata-Andia J (2003) Effect of VDR gene polymorphisms on osteocalcin secretion in calcitriol-stimulated human osteoblasts. Kidney Int Suppl 85:23–27
Van Pottelbergh I, Goemaere S, de Barquer D, de Paepe A, Kaufman M (2002) Vitamin D receptor gene allelic variants, bone density and bone turnover in community-dwelling men. Bone 31:631–637
Gomez-Garcia L, Esbrit P, Carrena L, Sabando P, Garcia-Flores M, Martinez ME (2003) Alendronate interacts with the inhibitory effect of 1,25(OH)2D3 on parathyroid hormone-related protein expression in human osteoblastic cells. J Bone Miner Res 18:78–87
Acknowledgments
This study was supported by grants from the Novo Nordic Foundation, Karolinska Institute, Magn Bergwall Foundation, and Stiftelsen Gamla Tjänarinnor. We thank Associate Professor Elisabeth Bucht for the measurement of PTHrP mRNA. We thank Dr. Tycho Tullberg (Stockholm Spine Center) for support and help in finding young control patients.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pernow, Y., Granberg, B., Sääf, M. et al. Osteoblast Dysfunction in Male Idiopathic Osteoporosis. Calcif Tissue Int 78, 90–97 (2006). https://doi.org/10.1007/s00223-005-0158-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-005-0158-9