Abstract
The objectives of this study were to (1) obtain both femoral neck strength (FNS) and hip axis length (HAL) values from left and right femurs (regardless of hip dominance) measured by DXA and evaluate their relationship with BMD of all hip regions including total hip, (2) determine if there is a difference between dominant and nondominant hip BMD in any of the hip regions, and (3) determine how physical activity influences hip BMD. Participants were 136, generally healthy Caucasian women (57.4–88.6 years). BMD was measured by DPX-MD. Past and present activity was assessed by the Allied Dunbar National Fitness Survey for older adults and normal/brisk walking pace was measured in a straight hallway. FNS analysis uses femoral geometry to calculate stresses at the femoral neck for two loading conditions: Safety Factor Index (SF) indicates risk of fracture for forces generated during a one-legged stance, and Fall Index (FI) indicates risk of fracture for forces generated during a fall on the greater trochanter. Simple and multiple regression analyses were used to determine predictive ability of HAL, SF, and FI for respective hip BMD values. There was no statistical difference in BMD between two hips in any of the measured regions, however, the nondominant hip correlated better with other skeletal sites. Subjects with a faster normal walking speed had higher neck BMD in the nondominant hip, 0.832 ± 0.12 vs. 0.791 ± 0.10 g/cm2 (P < 0.05). Longer HAL of the left hip was negatively related to neck, trochanter, shaft, and total hip BMD. FI was significantly associated with all sites of the hip BMD, while SF was associated only with neck and wards BMC (P < 0.05). In summary: (1) a longer HAL is associated with lower BMD and a higher FI with higher BMD, (2) it might be sufficient to measure BMD in only the nondominant hip, and (3) walking at a faster pace may positively benefit femoral neck BMD. Therefore, it appears that HAL, SF, and FI all play important roles in estimating fracture risk and should be assessed along with BMD when using DXA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hip geometry, including hip axis length (HAL) and femoral neck strength (FNS), have previously been suggested to relate independently to hip fracture risk; however, studies showing this relationship have mainly been limited to radiographic assessment [1, 2]. Software for measuring HAL and FNS with DXA became available in late eighties for research purposes only. This software evaluates hip strength via two components: Safety Factor (SF), indicating forces generated during a one-legged stance, and Fracture Index (FI), indicating forces generated during a fall on the greater trochanter. These values are calculated using femoral neck/shaft angle, neck diameter, bone mineral density (BMD), and bone mineral content (BMC). There are just a few studies examining hip geometry assessed by dual-energy X-ray absorptiometry (DXA) as a potential indicator of fracture risk [3] or as a predictor of BMD [2].
Both HAL and FNS influence hip fracture, although these relationships are not always clear due to different radiological tools used to calculate these values and different study conditions. Long HAL and larger neck-shaft angles have often been considered independent risk factors for osteoporosis, but studies do not always show this to be the case. Some studies reported a longer HAL and larger femoral neck-shaft angle in patients with fractures compared with controls [4, 5, 6, 7]. Others found no difference in HAL in fracture vs. control groups, which these authors suggest could be due to differences in measurement setup or to an artifact of positioning [1, 8]. Some studies have reported FNS to be positively associated with hip BMD [3, 9, 10], indicating FNS may be an important factor in estimating fracture risk and should be measured along with BMD. However, previous studies that assessed HAL and FNS failed to assess calcium intake in their subjects, which is an important nutrient to bone health and should be assessed as a confounder in statistical analyses.
Typically, one’s fracture risk and the presence of osteoporosis are determined by measuring BMD of the hip and spine [11]. Conventionally, the nondominant hip, determined based on the forearm dominance, has been used for the assessment of bone status. With the development of the dual hip software, both hips are measured, though it is not clear if this is necessary. Previous studies report high correlations between the hips at the femoral neck, Ward’s triangle, and trochanter regions [12, 13, 14, 15, 16, 17]. However, some of these same studies also report significant mean differences between specific hip regions which suggest both hips might need to be measured [12, 14 15, 17, 18], while others suggest one hip is sufficient [13, 14, 15, 16]. This discrepancy in the literature could be due to different subject populations, the use of different technologies, or the failure to take into consideration hip dominance when comparing left to right hip. Only one of these studies considered hip dominance when comparing hip BMD [17]. Hip dominance should be considered when assessing hip BMD since daily activities could favor one’s dominant side. If there truly were a difference between the hips, estimates of BMD of only one hip could result in misclassification of osteoporosis diagnosis and ultimately one’s fracture risk. On the other hand, if the BMDs of the two hips were similar, then BMD estimates of either hip could be used for the above purposes.
Numerous studies show hip BMD measured in one hip correlates well with other measured skeletal sites including the spine, whole body, and forearm. However, hip dominance is not addressed making it unclear if the nondominant or dominant hip could provide a better estimate of BMD in these skeletal sites [14, 19].
This study was conducted to (1) obtain both FNS and HAL values from left and right femurs (regardless of hip dominance) and evaluate their relationship with femoral BMD; (2) determine if BMD of both hips needs to be measured using DXA and whether dominant or nondominant hip correlates better with other skeletal sites, and (3) determine how past and present physical activity relates to hip BMD and hip geometry.
In our previous analysis of this population we found calcium intake and lean and fat tissue to influence BMD of various skeletal sites; therefore, they were included as confounders [20].
Experimental Subjects
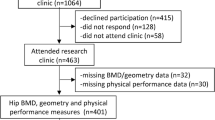
This study is part of a larger longitudinal clinical trial and includes 136 Caucasian, generally healthy, postmenopausal women, ages 57.4–88.6 years, free of medications known to affect bone, including hormone replacement therapy. Forty-six subjects reported having osteoarthritis. Study population is described in detail elsewhere [21, 22]. The Institutional Human Subjects Review Board approved the study protocol and subjects signed informed consent.
Materials and Methods
Study Design
Data from the baseline visit were used for measuring hip geometry, including hip strength and hip axis length. Hip dominance was not taken into consideration when hip geometry was measured. The 6-month-visit data, which consisted of the same study cohort but fewer subjects (N = 123), was used to assess whether both hips need to be measured and to determine if the average of both hips or one of the hips correlates better with other skeletal sites. We used two different data sets because at baseline only about 75% of subjects had both hips measured (when the dual software became available). In the 6-month visit, each subject had both hips measured, which allowed for direct comparison of their hips. For subjects missing one of the hips at baseline, we used their 6-month data for the missing hip and, therefore, had a larger data set for measuring hip geometry. The subjects with hip implants were excluded. The 6-month data were also used to determine how walking speed and past activity influence hip BMD. Subjects’ hips in the 6-month visit were labeled as either dominant or nondominant based on hand dominance. If subjects were left handed, their left hip was considered their dominant hip. Therefore, left-handed subjects had their left hip categorized with right-handed subjects’ dominant right hips.
Anthropometry and Bone Densitometry
Weight and height were measured in light clothes without shoes to calculate BMI (kg/m2). BMD (g/cm2) was measured by dual X-ray absorptiometry with a Lunar DPX-MD instrument (GE Medical Systems, Madison, WI) using specialized software for total body, lumbar spine, dual femur (neck, trochanter, Ward’s triangle, shaft, and total femur) and forearm (ulna and radius at ultradistal and 1/3 distal region measured from the styloid process and total forearm) as described previously [23]. Dual femur acquisition was obtained with subjects lying supine with both feet secured in a brace provided by the manufacturer. Each leg was rotated inward to a maximum internal rotation without subjects feeling uncomfortable. Quality assurance was performed daily. The in vivo and in vitro precision of our densitometer was reported previously [23].
The total body scan provided a measure of lean and fat tissues, which were used in multiple regression analysis as confounders. Hip axis length and hip strength were calculated from the DPX 3.7 beta version software. This software never received FDA approval due to limited accuracy in research studies and therefore is used for research purposes only. Currently, the only FDA approved method for measuring HAL is with the Lunar “Prodigy-Vision” which recently became available for clinical use. The HAL measurement includes the length of the femur and a portion of the pelvis. Hip strength analysis uses femoral neck geometry to calculate stresses at the femoral neck for two loading conditions, forces generated during a one-legged stance (SF), and forces generated by a fall on the greater trochanter (FI). SF and FI are referred to as safety factors and are obtained from four hip regions: shaft axis, neck axis, femoral head, and femoral neck. As SF and FI values get closer to “1,” the risk of fracture increases. The FI is calculated as the ratio of the yield stress of the superior femoral neck in comparison to Cstress (total compressive stress) [2]. SF force is calculated by the same principles as FI using the force generated during walking. This force is equal to 2.5 times one’s body weight at an angle of 13° measured from a vertical position and indicates the resistance to fracture of the femoral neck while walking [2]. The calculated coefficients of variation in our laboratory for HAL, SF, and FI were comparable to other published values [2].
Calcium Intake/Physical Activity
Ca intake from food was assessed during the baseline visit using a shortened food frequency questionnaire [24]. Physical activity was assessed using the Allied Dunbar National Fitness Survey for older adults [25] and described earlier [20]. This is a validated questionnaire used since the late 1980s to assess activity patterns and fitness levels in adults aged 16 and over. There are two versions of the questionnaire, one for adults under age 70, and one for age 70 and over, which was used in this study. In short, past-activity was assessed as percent of adult life, from age 18 to present, engaged in sport and recreational activities of an intensity of at least 4 kcal/min. Activities such as tennis, aerobics, swimming, and cycling had to be conducted on a basis of at least once a week for at least 3 months of the year. Percent of adult life was calculated based on the number of years since age 18, and the number of years actually engaged in regular activity with 3–12 months of regular activity equaling 1 year.
Normal and brisk walking speed was measured in an 8-m straight hallway. Subjects were told to first walk from one end of the hall to the other as if they were walking in their home down a hallway. Brisk walking was measured the same as normal walking except subjects were told to walk as fast as they can without running. Time was measured in seconds with a stopwatch, rounded to the nearest hundredth of a second. The average of two trials for both normal and brisk walking was taken. Present hours of walking per week were also recorded, as well as the time and frequency of continuous walks of at least 20 minutes in a 4-week period [20]. Stair climbing was assessed as number of flights climbed a day on average both at home and outside of the home. The number of steps per flight was recorded to assess the total daily number of stairs climbed [20].
Statistical Analysis
All data are presented as mean ± SD, unless otherwise stated, and are analyzed using statistical package Data Desk® (Odesta Corp, Northbrook, IL). Pearson correlation coefficient r was calculated to determine the degree of association between nondominant and dominant hip and other skeletal sites, as well as the relationship between hip geometry and hip BMD. Subjects from the 6-month data set were divided into groups below and above the mean for past activity, brisk and normal walking speed, and stair climbing to assess group differences in hip BMD. Two sample t-tests were conducted to determine group differences in past activity, brisk and normal walking speed, and stair climbing for each hip site.
Multiple regression models were created to evaluate the influence of hip strength and hip axis length on hip BMD. Each model was corrected for age, lean and fat tissue, past activity, and calcium intake. Level of significance was set at P ≤ 0.05.
Results
Baseline Data—Hip Geometry
Table 1 lists descriptive characteristics for all subjects participating in the baseline visit, including anthropometry, bone and soft tissue measurements, hip geometry, present walking, steps climbed per day, past activity, and calcium intake.
Both left and right HAL were significantly related to standing height, r = 0.45 and 0.53, respectively, P ≤ 0.0001. Left HAL had a significant negative relationship to BMD in the left femoral neck, trochanter, shaft, and total hip regions in multiple regression models (Table 2), which were corrected for age, lean and fat tissue, calcium intake, and past physical activity. Left and right HAL had a negative relationship with other hip regions, though it did not reach statistical significance.
Hip strength was represented by two values: FI represents a fall index indicating risk of fracture for forces generated on a fall on the greater trochanter, and SF represents risk of fracture for forces generated during a one-legged stance. As both values get closer to “1,” the fracture risk increases. In simple regression, left and right SF and FI were not significantly related to any skeletal sites. In multiple regression (Table 2), left FI was a significant predictor of the left femoral neck, trochanter, shaft, and total hip regions. Right FI was a significant predictor for all regions of the right hip. Left SF was a significant predictor of only left femoral neck BMC in multiple regression (data not presented). Similarly, right SF was a significant predictor of only right femoral neck and Ward’s triangle BMC in multiple regression (data not presented). Present activity, including total hours of walking a week and steps climbed per day, were significantly related to SF and FI in the right hip only (P < 0.05).
Six-Month Data—Hip Dominance and Influence of Physical Activity
Table 3 lists the mean ± standard deviatioin (SD) for subjects’ dominant and nondominant hips. Pearson’s r and mean percent differences were calculated to examine simple relationships between five regions of the dominant and the nondominant hip (Table 3). Both hips were significantly correlated at all five regions of the hip, with the strongest relationship in the total hip region, r = 0.96, P ≤ 0.0001 (Fig. 1) and the weakest in the Ward’s triangle, r = 0.88, P ≤ 0.0001. The Ward’s triangle region showed the largest and the femoral neck the smallest percent mean difference (1.6% and 0.2%, respectively).
The normal and brisk walking speed was 1.4 and 2.2 m/second, respectively, and ranged 0.76–2.45 and 1.10–3.12 m/second, respectively. Subjects were stratified into groups below and above the mean for normal and brisk walking speed, stair climbing, and past physical activity. Two sample t-tests were used to assess group differences. There were no significant differences in BMD between brisk walking speed, stair climbing, and past physical activity. Subjects with a faster normal walking speed had higher femoral neck BMD in the nondominant hip, 0.832 ± 0.12 vs. 0.791 ± 0.10 g/cm2 (P < 0.05) (Fig. 2).
Table 4 lists correlations between the hips and other skeletal sites. The nondominant hip correlated better than the dominant hip with total body and forearm BMD. All regions of both hips correlated similarly with the lumbar spine, except for the nondominant Ward’s triangle and the dominant total hip region which both had stronger correlations with spine. Averaging the two hips together produced smaller correlations with other skeletal sites compared with the nondominant hip for the whole body and forearm and the dominant hip for the lumbar spine.
Discussion
Our data suggest the following: (1) A longer HAL is associated with lower hip BMD, while a higher fracture index value is associated with higher hip BMD, (2) The nondominant hip appears sufficient for measuring hip BMD, (3) Walking at a faster pace may benefit hip BMD.
Our results are in agreement with other studies that show a longer HAL is associated with lower BMD. Gnudi et al. [5] found a longer HAL in postmenopausal women with a hip fracture compared with controls. Similarly, Boonen et al. [4] found a significantly higher HAL in postmenopausal women with hip fracture compared with osteoporotic women. Michelotti and Clark [8] found femoral neck length to be position sensitive which may explain why some studies show fracture groups to have a greater HAL and others do not [1]. Michelotti and Clark [8] found a larger femoral neck/shaft angle in their fracture group, indicating that hip geometry plays a role in determining hip fracture risk. Crabtree et al. [3] found both hip strength and HAL improved the ability to identify women at high risk of hip fracture. In an earlier study they found substantial geographical differences in femoral neck geometry as well as in BMD, and these variations may contribute to the large variations in hip fracture risk [2].
No studies could be found assessing the relationship between BMD and risk of fracture indices (SF and FI) calculated from GE DPX beta software, or investigating hip dominance and the relationship with other skeletal sites. However, Crabtree et al. [3] did use DPX beta versions of hip strength analysis to determine compressive strength (Cstress) which occurs as a result of a typical fall on the greater torchanter. They found Cstress and HAL combined with age and BMI provided a significantly better prediction of hip fracture than femoral neck BMD alone. We found both the left and right Fall Index (value calculated using Cstress) to be significant predictors of left and right femoral BMD. Present walking and stair climbing were found to be positively associated with SF and FI. It therefore appears that physical activity may have a positive influence on hip strength, and studies which do not find a significant association with activity and BMD may find it with hip strength. Including FI in multiple regression analysis significantly improved the adjusted R 2 (Table 2) for all sites of the hip, except for Ward’s triangle. Therefore, our results agree with Crabtree et al. [3] connotations that identifying women at high risk of hip fracture is likely to be significantly enhanced by combining bone density with age, simple anthropometry, and hip geometry, the latter including both hip axis length and hip strength analysis.
There were no significant differences in BMD between the dominant and nondominant hip in any of the hip sites. The BMD of the nondominant hip did tend to be slightly higher (not statistically significant) than BMD of the dominant hip for all regions except the neck. Yang et al. [17] also found the nondominant hip to be slightly higher than the dominant hip, with significant differences in the femoral neck and trochanter regions. Due to a large interfemur paired difference, Yang et al. [17] indicated the need to measure BMD in both hips to achieve an optimal evaluation of BMD status. Overall we found low mean differences in BMD (neck = 0.2%, Ward’s = 1.6%, trochanter = 1.5%, and shaft = 1.3%). These values are comparable with Franck et al. [12] and Bonnick et al. [15] who found mean differences in BMD of neck = 0.7%, Ward’s = 0.2%, and trochanter = 1.9%. Although Bonnick et al. [15] found high individual variations similar to those of Yang et al. [17] they concluded it is not necessary to measure both hips since the risk of misclassifying an individual for fracture is low. Therefore, it appears, based on our results and previous studies, measuring one hip is sufficient for estimating fracture risk. Since we found the nondominant hip correlated better than the dominant with other skeletal sites except the lumbar spine, it may be the hip of choice for measuring BMD.
When we compared subjects with greater than or less than the average normal walking speed (mean = 1.42 m/second), we found faster walkers to have significantly higher nondominant hip BMD in the femoral neck region. Faster walkers also had higher dominant femoral neck BMD, but it did not reach statistical significance. This may indicate that physical activity influences BMD in each hip differently or it is possible that osteoarthritis (self-reported by about one-third of our subjects) may contribute to the difference. Yang et al. [17] found hip dominance to have little effect on hip BMD, suggesting that osteoarthritis may be influencing hip BMD, especially if subjects tend to favor one side over the other. Our results are in agreement with Aoyagi et al. [26] who found faster female walkers over age 40 to have significant calcaneus BMD increases of 4.4–5.4% per standard deviation increase in walking speed. Intervention trials have also found that, in postmenopausal women, walking at a speed that kept their heart rate above their anaerobic threshold for seven months was effective in preventing bone loss in the lumbar spine [27]. Based on the above evidence, it appears brisk walking may positively benefit both hip and spine BMD in postmenopausal women. We did not find a relationship between stair climbing and hip BMD, probably because of less engagement of our participants in those activities. Our previous analysis in this population revealed a significant association of present walking (h/wk) and past physical activity with BMD of various hip regions [20]. Those were either multiple regression and/or subgroup analyses controlled for dietary intake, anthropometry, body composition, and other lifestyle modifiers. The main focus of this article was the relation of hip geometry to BMD and evaluation of dominant and nondominant hip. Elaborating more on various other lifestyle parameters (affecting BMD) would have detracted from the main focus.
The results of this cross-sectional analysis emphasize several key points: When measuring hip BMD with DXA, HAL and FNS may help improve the ability to identify women at risk of hip fracture. A more precise method for measuring hip strength needs to be developed in order for future studies to assess the relationship between hip geometry parameters and hip BMD/fracture risk. It does not appear necessary to measure both hips, and if measuring only the hip region for osteoporosis diagnosis, the nondominant hip should be measured since it correlates better with other skeletal sites. Finally, walking at a faster pace should be recommended as a form of activity that may positively affect hip BMD in postmenopausal women.
References
J Partanen T Jamsa P Jalovaara (2001) ArticleTitleInfluence of the upper femur and pelvic geometry on the risk and type of hip fractures. J Bone Miner Res 16 1540–1546 Occurrence Handle1:STN:280:DC%2BD3Mvltlejtw%3D%3D Occurrence Handle11499877
N Crabtree M Lunt G Holt H Kroger H Burger S Graizo KT Khaw RS Lorenc J Nijs J Stepan JA Falch T Miazgowski P Raptou P Pols J Dequeker S Havelka K Hoszowski I Jajic S Czekalski G Lyritis AJ Silman J Reeve (2000) ArticleTitleHip geometry, bone mineral distribution, and bone strength in European men and women: the EPOS study. Bone 27 151–159 Occurrence Handle10.1016/S8756-3282(00)00300-8 Occurrence Handle1:STN:280:DC%2BD3cvisVCgtw%3D%3D Occurrence Handle10865223
NJ Crabtree H Kroger A Martin HA Pols R Lorenc J Nijs J Stepan JA Falch T Miazgowski S Grazio P Raptou J Adams A Collings KT Khaw N Rushton M Lunt AK Dixon J Reeve (2002) ArticleTitleImproving risk assessment: hip geometry, bone mineral distribution and bone strength in hip fracture cases and controls. The EPOS study. European Prospective Study. Osteoporos Int 13 48–54 Occurrence Handle10.1007/s198-002-8337-y
S Boonen R Koutri J Dequeker J Aerssens G Lowet J Nijs E Lesaffre P Geusens (1995) ArticleTitleMeasurement of femoral geometry in type I and type II osteoporosis: differences in hip axis length consistent with heterogeneity in the pathogenesis of osteoporotic fractures. J Bone Miner Res 10 1908–1912 Occurrence Handle1:STN:280:BymC1M3ntFU%3D Occurrence Handle8619371
S Gnudi C Ripamonti G Gualtieri N Malavolta (1999) ArticleTitleGeometry of proximal femur in the prediction of hip fracture in osteoporotic women. Br J Radiol 72 729–733 Occurrence Handle1:STN:280:DC%2BD3c%2FovFClsQ%3D%3D Occurrence Handle10624337
S Gnudi C Ripamonti L Lisa M Fini R Giardino G Giavaresi (2002) ArticleTitleProximal femur neck fractures from trochanteric fractures in postmenopausal women. Osteoporos Int 13 69–73 Occurrence Handle10.1007/s198-002-8340-2
CG Alonso MD Curiel FH Carranza RP Cano AD Perez (2000) ArticleTitleFemoral bone mineral density, neck-shaft angle and mean femoral neck width as predictors of hip fractures in men and women. Multicenter Project for Research in Osteoporosis. Osteoporos Int 11 714–720 Occurrence Handle10.1007/s001980070071 Occurrence Handle1:STN:280:DC%2BD3M%2FlsFarug%3D%3D Occurrence Handle11095176
J Michelotti J Clark (1999) ArticleTitleFemoral neck length and hip fracture risk. J Bone Miner Res 14 1714–1720 Occurrence Handle1:STN:280:DyaK1MvitFCksw%3D%3D Occurrence Handle10491219
XG Cheng G Lowet S Boonen PHF Nicholson P Brys J Nijs J Dequeker (1997) ArticleTitleAssessment of strength of proximal femur in vitro: relationship to femoral bone mineral density and femoral geometry. Bone 20 213–218 Occurrence Handle10.1016/S8756-3282(96)00383-3 Occurrence Handle1:STN:280:ByiB38rgvFw%3D Occurrence Handle9071471
XG Cheng G Lowet S Boonen PH Nicholson G Van der Perre J Dequeker (1998) ArticleTitlePrediction of vertebral and femoral strength in vitro by bone mineral density measured at different skeletal sites. J Bone Miner Res 13 1439–1443 Occurrence Handle1:STN:280:DyaK1cvgvVyqtA%3D%3D Occurrence Handle9738516
InstitutionalAuthorNameWorld Health Organization (1994) ArticleTitleStudy Group on assessment of fracture risk and its application to screening and postmenopausal osteoporosis. WHO Technical Report Series 843 1–29
H Franck M Munz M Scherrer (1997) ArticleTitleBone mineral density of opposing hips using dual energy x-ray absorptiometry in single-beam and fan-beam design. Calcif Tissue Int 61 445–447 Occurrence Handle10.1007/s002239900365 Occurrence Handle1:CAS:528:DyaK2sXnvVWjtbY%3D Occurrence Handle9383269
RS Yang PU Chieng KS Tsai TK Liu (1996) ArticleTitleSymmetry of bone mineral density in the hips is not affected by age. Nucl Med Commun 17 711–718 Occurrence Handle1:STN:280:ByiD3s3itlM%3D Occurrence Handle8878133
AD Rao S Reddy DS Rao (2000) ArticleTitleIs there a difference between right and left femoral bone density? J Clin Densitom 3 57–61
SL Bonnick DL Nicholos CF Sanborn SG Payne SM Moen CJ Heiss (1996) ArticleTitleRight and left proximal femur analyses: Is there a need to do both? Calcif Tissue Int 58 301–310 Occurrence Handle10.1007/s002239900049
KG Faulkner HK Genant M McClung (1995) ArticleTitleBilateral comparison of femoral bone density and hip axis length from single and fan beam DXA scans. Calcif Tissue Int 56 26–31 Occurrence Handle1:CAS:528:DyaK2MXkvV2hsLo%3D Occurrence Handle7796342
RS Yang KS Tsai PU Chieng TK Liu (1997) ArticleTitleSymmetry of bone mineral density at the proximal femur with emphasis on the effect of side dominance. Calcif Tissue Int 61 189–191 Occurrence Handle10.1007/s002239900321 Occurrence Handle1:CAS:528:DyaK2sXlslKjsLg%3D Occurrence Handle9262508
J Balseiro FH Fahey HA Ziessman TV Le (1988) ArticleTitleComparison of bone mineral density in both hips. Radiology 167 151–153 Occurrence Handle1:STN:280:BieC2MfmsVA%3D Occurrence Handle3347717
K Bjarnason C Hassager OL Svendsen J Stang C Christiansen (1996) ArticleTitleAnteroposterior and lateral spinal DXA for the assessment of vertebral body strength: comparison with hip and forearm measurement. Osteoporos Int 6 37–42 Occurrence Handle1:STN:280:BymH3c3gtFE%3D
JZ Ilich–Ernst RA Brownbill MA Ludemann R Fu (2002) ArticleTitleCritical factors for bone health in women across the age span: How important is muscle mass? Medscape Women’s Health, eJournal 7 . .
RA Brownbill JZ Ilich (2002) ArticleTitleValidation of the use of the hand for estimating bone mineral density in other skeletal sites by DXA in healthy and osteoarthritic women. J Clin Densitom 5 273–282 Occurrence Handle12357065
JZ Ilich RA Brownbill L Tamborini (2003) ArticleTitleBone and nutrition in elderly women: protein, energy and calcium as main determinants of bone mineral density. Eur J Clin Nutr 57 554–565 Occurrence Handle10.1038/sj.ejcn.1601577 Occurrence Handle1:CAS:528:DC%2BD3sXivFGku7o%3D Occurrence Handle12700617
JZ Ilich M Zito RA Brownbill M Joyce (2000) ArticleTitleChange in bone mass after Colles’ fracture: a case report of unique data collection and long term implications. J Clin Densitom 3 383–389
InstitutionalAuthorNameNational Osteoporosis Foundation (1998) Osteoporosis: Physician’s guide to preventing and treating osteoporosis. National Osteoporosis Foundation Washington DC
InstitutionalAuthorNameNational Osteoporosis FoundationFenton PH, Health Education Authority of London Sports Council (1992) ArticleTitleThe Allied Dunbar National Fitness Survey. London Sports Council . 195–206
K Aoyagi PD Ross T Hayashi K Okano K Moji H Sasayama Y Yahata T Takemoto (2000) ArticleTitleCalcaneus bone mineral density is lower among men and women with lower physical performance. Calcif Tissue Int 67 106–110 Occurrence Handle10.1007/s00223001116 Occurrence Handle1:CAS:528:DC%2BD3cXmtFCjtrw%3D Occurrence Handle10920213
M Hatori A Hasegawa H Adachi A Shinozaki R Hayashi H Okano H Mizunuma K Murata (1993) ArticleTitleThe effects of walking at the anaerobic threshold level on vertebral bone loss in postmenopausal women. Calcif Tissue Int 52 411–414 Occurrence Handle1:STN:280:ByyA2sbptVM%3D Occurrence Handle8369985
Acknowledgements
The authors thank all the women who participated in this study. The authors are in debted to the University of Connecticut, Kinesiology Department, Human Performance Lab, where the study was conducted. This study was funded in part by NRI/USDA 2001-00836, Donaghue Medical Research Foundation DF98-056, and the University of Connecticut Office for Sponsored Programs.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brownbill, R., Lindsey, C., Crncevic–Orlic, Z. et al. Dual Hip Bone Mineral Density in Postmenopausal Women: Geometry and Effect of Physical Activity . Calcif Tissue Int 73, 217–224 (2003). https://doi.org/10.1007/s00223-002-1066-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-002-1066-x