Abstract
The cerebrospinal fluid (CSF) biomarkers amyloid-β42 (Aβ42), total Tau, and phospho-181-Tau represent important diagnostic tools to support the clinical diagnosis of Alzheimer’s disease (AD). Acquiring CSF by lumbar puncture is considered a moderately invasive procedure, while blood sampling is minimally invasive with calculable risks and can be performed by trained non-medical staff. Thus, the identification of reliable and robust blood biomarkers of AD-related neuropathology would be significantly advantageous in daily practice and would allow more patients to be screened. In this study, we performed a multiplex amyloid-β assay to simultaneously measure Aβ40 and Aβ42. We analyzed how well Aβ40, Aβ42, and the Aβ42 to Aβ40 ratio (Aβ42/40) could differentiate between patients suffering from dementia either due or not due to AD. In addition, we studied different factors affecting Aβ levels in plasma. Plasma Aβ42/40 level was significantly lower in patients with dementia due to AD than in those with dementia due to other causes. Aβ42/40 correlated weakly between plasma and CSF, but did not differ between amyloid-PET positive or negative patients. Furthermore, we found that kidney function influences Aβ40 and Aβ42 plasma levels, but not Aβ42/40 level. Liver function, age, and sex do not affect Aβ levels in plasma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is the most common progressive neurodegenerative dementing disorder. AD is clinically characterized by a preclinical stage, followed by mild cognitive impairment (MCI) due to the progression of the disease into AD dementia (Dubois et al. 2007; Jack Jr et al. 2011). Currently, AD is diagnosed at a relatively late stage when there are already substantial irreversible cognitive deficits. Intervention at an early stage would most likely increase the effectiveness of existing symptomatic therapies, such as cholinesterase inhibitors and glutamate (NMDA) receptor antagonists (Klafki et al. 2006). Therefore, many clinical trials aim to control AD at an early stage to prevent cognitive deficits from severely impacting the functionality of the patient. A pre-dementia diagnostic technique is imperative to detect AD pathology and prevent further irreversible brain damage. To reduce the number of invasive procedures on patients, we aim to implement a plasma assay as an enrichment tool to increase the number of patients with possible AD pathology for further invasive diagnosis.
Different types of dementia and other neuropsychiatric disorders show a high overlap in their clinical appearance. Therefore, novel guidelines support the use of cerebrospinal fluid (CSF) biomarkers in addition to medical history, neurological examination, neuropsychiatric testing, and structural imaging to differentiate between dementias due to AD and other types of dementias (Deuschl and Maier; Dubois et al. 2007; McKhann et al. 2011; Cummings et al. 2013). Commonly accepted CSF biomarkers include total Tau (tTau), phospho-181-Tau (pTau), and amyloid-β42 (Aβ42). Recent studies have suggested that the ratio of Aβ42 to Aβ40 (Aβ42/40) is superior to the Aβ42 concentration level alone in diagnosing AD dementia (Lewczuk et al. 2004, 2016).
While CSF biomarkers are currently one of the most accepted methods to identify AD pathology, lumbar punctures for CSF diagnosis cannot be performed routinely and repeatedly at preclinical stages of AD. Intermediate circulation disturbances, tinnitus, or headache are frequent but harmless side effects of lumbar punctures, whereas infections, bleeding and paralysis are the most dangerous, but very rare complications. Thus, new AD diagnostic methods should focus on using blood biomarkers. Compared with the time consuming and risky procedure required to collect CSF, blood collection is an easy procedure that can be performed by non-medical staff. Using peripheral biomarkers in blood, such as Aβ to verify amyloid pathology at an early stage of the disease as well as monitor the effectiveness of Aβ lowering therapies would be markedly impactful.
Studies investigating plasma Aβ levels as a biomarker for AD diagnosis have yielded contradictory findings (Mehta et al. 2000; Hansson et al. 2012; Lövheim et al. 2017). In a systematic meta-analysis, Olssen et al. (2016) concluded that neither Aβ40 nor Aβ42 can currently be considered reliable biomarkers for the diagnosis of AD. However, Kaneko et al. (2014a) recently showed that the ratio between Aβ− 3−40 and Aβ1 − 42 discriminates between amyloid-PET positive and negative subjects. Therefore, we hypothesized that the combination of different Aβ peptides is superior in the diagnosis of AD to Aβ40 or Aβ42 alone.
In addition, the quality of plasma Aβ peptides as potential biomarkers highly depends on the used assay. Aβ concentration levels are approximately 20-fold lower in plasma than when compared with CSF (Janelidze et al. 2016); therefore, thus not all immunoassays are sensitive enough to detect Aβ species in plasma samples. Recent studies with highly sensitive immunoassays have reported on different Aβ peptides as potential biomarkers. For example, Kaneko et al. (2014a, b) performed a modified immunoprecipitation using F(ab′) fragments of two independent monoclonal antibodies, followed by mass spectrometry, a sensitive method to detect unknown peptides. Another study (Janelidze et al. 2016) analyzed plasma samples with the highly sensitive single molecule array (SIMOA) technology (Quanterix) and found that Aβ40, Aβ42, and Aβ42/40 plasma levels were significantly reduced in AD patients compared to both mild cognitive impairment (MCI) and subjective cognitive impairment (SCI) patients and healthy controls. Following these reports, we believe that immunoassays need to be validated specifically for plasma.
To evaluate whether the chemiluminescence immuno-multiplex assay (V-PLEX Aβ [6E10], Mesoscale Discovery) is suitable to detect plasma Aβ38, Aβ40, and Aβ42, we performed a “fit for purpose” assay validation. Our assay validation protocol was adapted from the guidelines by Andresson et al. (2015). Furthermore, we investigated if plasma Aβ40, Aβ42, and Aβ42/40 are biomarkers for AD and examined the effect of age and sex as well as kidney and liver function on plasma Aβ levels.
To our knowledge, this is the first report to validate this multiplex chemiluminescence immunoassay as a useful tool for providing detectable concentrations of Aβ40 and Aβ42 in plasma.
Materials and methods
Study population
In the current study, we analyzed plasma Aβ40, Aβ42, and Aβ42/40 to determine if it is a reliable biomarker for the identification of cerebral AD pathology. According to the NIA-AA criteria (McKhann et al. 2011), 23 patients were diagnosed with “probable AD dementia” or “possible AD dementia with AD pathology” (e.g., mixed vascular and Alzheimer’s dementia), referred to as “AD dementia (AD-D).” AD pathology was identified by biomarkers for both axes, Tau and Aβ (CSF analysis and/or PET imaging). 18 patients fulfilled the clinical and neuropsychological criteria for dementia without any evidence of AD pathology (CSF diagnostic, neuropsychological profile, or FDG- and amyloid-PET), defined as “demented controls” (DC; Table 1).
In total, 14 patients received FDG- and amyloid-PET scans, additionally eight respectively six patients received a single FDG-PET or amyloid-PET scan. 37 patients underwent a lumbar puncture for CSF analysis. Four patients refused a lumbar puncture or could not be punctured; all these four patients received an amyloid-PET to evaluate the Aβ burden to identify an AD pathology (Table 1).
In detail, the clinical diagnosis of dementia is defined by the following cognitive and behavioral symptoms: the symptoms interfere with the ability to function at work or perform usual activities and have significantly declined from previous levels of functioning and performance for at least 6 months; this cognitive impairment cannot be explained by delirium or a major psychiatric disorder and is detected and diagnosed by a clear history of reported or observed worsening cognition and an objective cognitive assessment (neuropsychological testing should be performed when the routine history and bedside mental status examination cannot provide a confident diagnosis); and the cognitive or behavioral impairment involves a minimum of two of the following domains:
-
Impaired ability to acquire and remember new information
-
Impaired reasoning and handling of complex tasks; poor judgment
-
Impaired visuospatial ability
-
Impaired language function
-
Change in personality, behavior, or demeanor
Dementia was differentiated from MCI based on how much the symptoms interfered with daily life; dementia was classified as a significant interference (McKhann et al. 2011).
The mean age of patients in the AD-D and DC groups were 69.0 ± 10.9 and 64.9 ± 10.9 years (p = 0.238), respectively. In the AD-D group, 43.5% of participants were men, while 72.2% were men in the DC group (p = 0.113; Table 1). There was a significant difference in the Mini-Mental State Examination (MMSE) scores, but no significant difference in clock drawing test (CDT) scores in the AD-D and DC groups, respectively. Patients in the AD-D and DC groups scored 22.6 ± 4.4 and 25.3 ± 2.4 points (p = 0.037), respectively, on the MMSE. On the CDT, patients in the AD-D and DC groups scored 3.05 ± 1.3 and 2.44 ± 1.2 points (p = 0.158), respectively.
We studied the effect of age and sex as well as kidney and liver function on plasma Aβ levels. In total, 128 EDTA-plasma samples (including the AD-D and DC patients) were measured. All samples were collected by the biobank of the Department of Psychiatry and Psychotherapy, University Medical Centre Goettingen. Patients from this cohort suffered from psychiatric disorders, including organic mental disorders (ICD-10 code F00-F09); mental and behavioral disorders due to psychoactive substances (ICD-10 code F10-F09); schizophrenia, schizotypal, and delusional disorders (ICD-10 code F20-F29); affective disorders (ICD-10 code F30-F39); neurotic, stress-related, and delusional disorders (ICD-10 code F40-F49); and adult personality and behavior disorders (ICD-10 code F60-F69). All psychiatric disorders were diagnosed according to the respective ICD-10 criteria. Nine samples were excluded from the analysis: one patient had a ventricular-peritoneal shunt, one patient had plasma Aβ levels below the lower limits of detection (LLOD), and seven participants had plasma Aβ levels which were later defined as outliers.
The mean age for the entire cohort was 63.1 ± 15.0 years with an MMSE of 25.4 ± 3.9 points. MMSE was missing for some non-demented patients. 61.7% of the participants were males.
Biomaterial sampling and ethical commitment
The current study was performed using samples from the biobank of the Department of Psychiatry and Psychotherapy, University Medical Centre Goettingen. The ethical vote (9/2/16) was approved by the ethics committee of the University Medical Centre Goettingen, Germany. All samples were collected and processed according to the current version of the Declaration of Helsinki. All included participants gave their informed consent prior to the collection of blood samples.
Sample preparation and storage
All samples were prepared in accordance with the local standard operating procedures. Serum samples (serum monovettes without clotting activator, Sarstedt) were allowed to coagulate for 45 min, while plasma samples (EDTA-K monovettes, Sarstedt) were centrifuged immediately. Both were centrifuged for 10 min at 2000×g at room temperature. Samples were stored as 500 µl aliquots in polypropylene tubes at − 80 °C until used. Samples were stored for a maximum of 15 months.
Analysis of Aβ in plasma and CSF
Aβ peptides were measured using a chemiluminescence immuno-multiplex assay (V-PLEX Aβ [6E10], Mesoscale Discovery).
The assay was carried out according to the manufacturer’s instructions. Briefly, the assay plate was blocked for 60 min with 150 µl blocking buffer and washed afterwards. We then pre-diluted 100 µl plasma with 100 µl dilution buffer and centrifuged the dilution at 10,000×g for 10 min at room temperature. We then transferred 100 µl supernatant to a separate reaction vial and diluted it with 100 µl dilution buffer for a final dilution of 1:4 (one part plasma, three parts dilution buffer). CSF was diluted to a final dilution of 1:16 (10 µl CSF diluted with 150 µl dilution buffer), as described previously (Klafki et al. 2016).
Then, 25 µl detection antibody solution, which contained 2% (v/v) sulfo-tag labeled anti-Aβ antibody (6E10) and 1% (v/v) Aβ40 blocker, and 25 µl diluted samples or standards were incubated for 120 min on the assay plate at room temperature while gently shaking. After three consecutive washing steps, 150 µl “read buffer” was added and the plate was measured immediately with the MESO QuickPlex SQ 120 reader (Mesocale Discovery). All steps were performed in polypropylene LoBind PCR clean tubes (Eppendorf).
To validate our assay, we analyzed the lower limits of detection (LLOD) and quantification (LLOQ), defined as the concentration corresponding to the signal three or ten standard deviations (SD) above the blank, respectively (Gilfrich and Birks 1984; Thomsen et al. 2003). Five different plasma samples from healthy volunteers were used to study the effect of parallelism, spike recovery, and intra- and inter-assay variance (Klafki et al. 2016). Spike recoveries were calculated at three different spiking levels: 25, 50, and 150 pg/ml Aβ40 as well as 2.22, 4.45, and 13.36 pg/ml Aβ42. Intra-assay variance was calculated from six technical replicates analyzed on the same assay plate and inter-assay variance was calculated from three independent runs.
Analysis of cystatin C and cholinesterase in serum
Cholinesterase and cystatin C were assessed using MULTIGENT assays (Abbott) on a fully automated Architect c (Abbott) system according to the manufacturer’s protocol. Both markers were measured in serum, which was available for 127 of the 128 samples. The estimated glomerular filtration rate (GFR) was calculated according to the CKD-EPI formula for cystatin C (Fan et al. 2015).
Statistics
The data were analyzed using GraphPad Prism 7.03. All results are presented as mean ± SD unless otherwise noted. The impact of age as well as kidney and liver function on Aβ plasma levels was analyzed using Pearson’s correlation coefficient followed by linear regression (age) or Deming regression (cholinesterase, GFR). Differences between the AD-D and DC groups were analyzed using two-tailed unpaired Student’s t tests and receiver operating characteristics (ROC) curves. Outliers were identified by Grubbs’ test with significance set as α = 0.01.
Results
Aβ-plasma assay validation
To evaluate if the V-Plex Aβ (6E10) multiplex immunoassay kit (Mesoscale Discovery) is suitable to detect Aβ38, Aβ40, and Aβ42 in human EDTA-plasma, we performed a partial “fit for purpose” assay validation as described previously (Klafki et al. 2016).
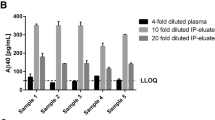
LLODs and LLOQs were calculated by averaging data from six independent runs. We found that the LLODs were 13.97 ± 8.88 pg/ml for Aβ38, 11.93 ± 2.31 pg/ml for Aβ40, and 0.64 ± 0.14 pg/ml for Aβ42, while the LLOQs were 26.89 ± 19.35 pg/ml for Aβ38, 24.22 ± 5.51 pg/ml for Aβ40, and 1.27 ± 0.38 pg/ml for Aβ42. In most plasma samples, Aβ38 was below the LLOD and thus could not be further analyzed. Parallelism was demonstrated for both Aβ40 and Aβ42, with 108.0 ± 7.2 and 80.4 ± 4.0% in range, respectively. Spiking recoveries were determined at three different spiking levels. The mean spike recoveries were 114.0 ± 8.4% for Aβ40 and 90.1 ± 6.9% for Aβ42 (Table 2). We also found that both intra- and inter-assay variance were less than 10% for both Aβ40 and Aβ42 (Table 3).
Plasma Aβ measurements in a clinical cohort
We analyzed Aβ40, Aβ42, and Aβ42/40 in a fourfold dilution of plasma using MSD multiplex technology in a clinical cohort which included 23 AD-D and 18 DC patients. Due to low Aβ40 plasma levels, higher dilutions were not possible. In general, the Aβ38 signals we obtained were below the LLOD and thus were excluded from further evaluation. Plasma levels of Aβ40 and Aβ42 did not differ significantly between the AD-D and DC groups, with plasma levels of 249.7 ± 49.9 and 230.3 ± 35.8 pg/ml, respectively, for Aβ40 (p = 0.170) and 18.4 ± 3.2 and 18.6 ± 2.7 pg/ml, respectively, for Aβ42 (p = 0.862; Fig. 1). However, Aβ42/40 was significantly lower (p = 0.003) in the AD-D compared to DC group, with plasma levels of 0.0744 ± 0.0060 and 0.0812 ± 0.0076, respectively. The area under the calculated ROC curve to discriminate Aβ42/40 levels between the AD-D and DC groups (Fig. 1) was 0.7585 (p = 0.005; Table 4).
In addition, we compared Aβ40, Aβ42, and Aβ42/40 in a subgroup of patients that received an amyloid-PET scan to identify amyloid positivity. Both Aβ40 and Aβ42 plasma levels, as well as Aβ42/40, did not differ significantly between amyloid-PET positive or negative patients, with plasma levels of 231.7 ± 38.0 and 240.3 ± 45.9 pg/ml for Aβ40 (p = 0.655), 17.3 ± 2.6 and 18.6 ± 2.6 pg/ml for Aβ42 (p = 0.234), and 0.0743 ± 0.0069 and 0.0780 ± 0.0072 for Aβ42/40 (p = 0.255), respectively (Fig. 2).
Plasma Aβ as an indicator for central amyloid pathology: plasma Aβ levels indicated for patients with increased amyloid load (amyloid-PET +) or normal amyloid-PET (amyloid-PET −) (a–d). Peripheral Aβ40 and Aβ42 levels as well as Aβ42/40 were comparable for patients with amyloid + and amyloid − PET scans. For 33 patients, additional CSF Aβ levels were analyzed and compared with plasma Aβ levels (d–f). No correlation could be seen for Aβ40 and Aβ42, whereas Aβ42/40 significantly correlated between CSF and plasma
Correlation between central and peripheral Aβ levels
33 patients from the AD-D and DC cohort also donated CSF and plasma. Aβ levels in CSF and plasma were analyzed using the identical immunoassay and correlated afterwards. Neither Aβ40 nor Aβ42 levels correlated between CSF and plasma. Notably, Aβ42/40 showed a weak but significant correlation between CSF and plasma (r = 0.425, p = 0.014; Fig. 2; Table 5).
Systemic factors influencing plasma Aβ levels
In addition to the validation of plasma Aβ40 and Aβ42, we assessed the impact of age and sex as well as liver and kidney function on the production and degradation of these plasma levels. Age and sex information was available for all patients, while cystatin C and cholinesterase were available for only 127 of 128 patients. Both cystatin C and cholinesterase were measured in serum which was collected along with the plasma and stored at − 80 °C.
Using Pearson’s correlation coefficient, we found that there was not a statistically significant correlation between age and Aβ levels (R2 = 0.013, p = 0.213 for Aβ40; R2 = 0.002, p = 0.627 for Aβ42; R2 = 0.021, p = 0.112 for Aβ42/40). Furthermore, there were no statistically significant correlation between cholinesterase activity, which measures liver function, and Aβ plasma levels (R2 < 0.001, p = 0.884 for Aβ40; R2 = 0.001, p = 0.695 for Aβ42; R2 < 0.001, p = 0.837 for Aβ42/40). Thus, neither liver function nor age affected plasma Aβ40 and Aβ42 levels.
We calculated the estimated GFR using CKD-EPI for cystatin C as an indicator for kidney function. A reduced GFR led to a slight accumulation of Aβ40 (R2 = 0.106, p < 0.001) and Aβ42 (R2 = 0.056, p = 0.010), while there was no apparent effect on Aβ42/40 (R2 = 0.033, p = 0.050).
In this cohort, female participants showed a trend towards higher Aβ42 levels [male 19.0 ± 3.2 pg/ml; female 20.4 ± 3.9 pg/ml; p = 0.026 (due to Bonferroni correction for multiple testing α < 0.0167)]. In contrast, both plasma Aβ40 (male 252.1 ± 55.5 pg/ml; female 263.7 ± 60.0 pg/ml; p = 0.284) and Aβ42/40 (male 0.0768 ± 0.0132; female 0.0788 ± 0.0114; p = 0.397) levels were not significantly affected by sex (Fig. 3; Table 6).
Systemic factors affecting plasma Aβ levels: age (a–c), cholinesterase as a marker for liver function (d–f), GFR calculated by CKE-EPI for cystatin c (g–i) and sex (j–l). Neither age (a–c), liver function (d–f) nor sex (j–l) showed significant effects on plasma Aβ levels. Aβ40 and Aβ42, but not Aβ42/40 was significantly increased due to a reduced kidney function (g–i)
Discussion
Here, we report on a multiplex immunoassay for the detection of amyloid-β peptides in plasma. According to the manufacturer’s recommendations, the kit was developed for CSF, cell culture supernatant, and tissue homogenate. In this study, we were able to use this kit to measure plasma Aβ40 and Aβ42 at a 1:4 dilution. Except for the Aβ42 LLOQ, our protocol confirmed the detection limits published by the manufacturer. For Aβ42, we calculated an LLOQ (1.27 pg/ml) which was less than half of the LLOQ indicated by the kit (3.13 pg/ml). Parallelism for Aβ42 was 80.4% in range, marginally out of our predefined performance criteria between 85 and 115%. Spike recoveries as well as intra- and inter-assay variances for both Aβ40 and Aβ42 were within our accepted range. Our findings suggest that a 1:4 dilution is sufficient to reduce interfering matrix effects and allow reliable Aβ40 and Aβ42 concentrations to be measured.
There are multiple studies investigating the detection of amyloid-β peptides in plasma by various assays as a potential biomarker for AD [reviewed in (Irizarry 2004; Olsson et al. 2016)]. Measuring Aβ42/40 in plasma might be useful as a screening tool, because the blood collection procedure is easy, minimally invasive, and can be performed by general practitioners. The results from this simple procedure could be used to determine if further time consuming, expensive, and invasive procedures are necessary. Recent studies have found that changes in plasma Aβ42 and Aβ42/40 occur as a result of cortical Amyloid deposition (Fandos et al. 2017; Ovod et al. 2017). Using a stable isotope labeling kinetics protocol, Ovod et al. (2017) suggested that there is an active transport of Aβ42 across the blood–brain barrier. Fandos et al. (2017) analyzed the Australian Imaging, Biomarker and Lifestyle Flagship (AIBL) cohort and identified plasma Aβ42/40 as a possible biomarker for cerebral Aβ depletion in preclinical participants. In that study, AD pathology was identified by Amyloid-PET and participants were followed for up to 4.5 years.
As such, in the current study, we were interested in investigating plasma Aβ40, Aβ42, and Aβ42/40. To our knowledge, this is the first study to validate the Mesoscale multiplex assay for the simultaneous detection of plasma Aβ40 and Aβ42 which can be used to calculate Aβ42/40. Our results show equal levels of Aβ40 and Aβ42 in the plasma of patients from both the AD-D and DC groups. The ratio of plasma Aβ42 to Aβ40 (Aβ42/40) can be used as a surrogate marker for total Aβ, improving diagnostic significance. Thus, we investigated if Aβ42/40 can be used to differentiate between patients with dementia due and not due to AD. We found that there was a significant difference in plasma Aβ42/40 levels between AD dementia patients and controls (0.0812 vs. 0.0744). The calculated area under the ROC curve was 0.76. Hence, Aβ42/40 measured with the assay presented here cannot replace CSF or PET as a diagnostic tool. Our results support that plasma Aβ42/40 needs to be further investigated in a cohort of patients with MCI during their follow-up and specifically, during the critical conversion into AD dementia.
The present assay could be a useful as an early tool within the diagnostic cascade. Patients with cognitive impairments could be easily screened to plan further diagnostic steps and make better use of the limited clinical resources in the healthcare system. However, more experience should to be gained using this assay. In particular, reasonable cut-off values need to be defined with high sensitivity. Positive and negative predictive values should be calculated in larger cohorts to estimate the significance of such a screening instrument.
So far, the localization of the production and degradation of Aβ peptides in blood has not been identified. Different studies have investigated the involvement of the liver and kidneys in Aβ degradation (Irizarry 2004; Toledo et al. 2011; Huang et al. 2012; Gronewold et al. 2015). Gronewold et al. (2015) reported an accumulation of plasma Aβ levels in patients with chronic kidney disorders, which were reduced after kidney transplantation. Toledo et al. (2011) analyzed factors affecting plasma Aβ levels within the Alzheimer’s Disease Neuroimaging Initiative (ADNI) cohort. Amongst others, the group found significant effects of gender, age, and creatinine on Aβ40 and Aβ42, but not on Aβ42/40. Instead of using cholinesterase as we used in this study, they measured bilirubin, γ-glutamyltransferase (γGT), glutamate–pyruvate–transferase (GPT), and albumin as markers for liver injury and found that none of these markers correlated with plasma Aβ levels.
Concerning the impact of cardiovascular disorders on plasma Aβ levels, Janelidze et al. (2016) found that Aβ levels in plasma were affected by hypertension, ischemic heart disease, diabetes mellitus, and anti-hypertensive or cardio-protective medication. As all these cardiovascular disorders lead to a reduced kidney function, we speculate that the impact of cardiovascular disorders on increased Aβ levels is mediated by kidney function, which can be quantified by the estimated GFR.
In this study, we found no correlation between liver function, measured as cholinesterase activity, and plasma Aβ40, Aβ42, and Aβ42/40 levels. In contrast, low estimated GFRs, which we used to assess kidney function, were associated with higher levels of Aβ40 and Aβ42. We found a poor, but significant correlation of R2 = 0.106 and R2 = 0.056 for Aβ40 and Aβ42, respectively. However, the calculated Aβ42/40 ratio was not influenced by kidney function. As there was no correlation between Aβ42/40 and GFR, we do believe that Aβ42/40 is superior to Aβ40 or Aβ42 alone for the detection of Alzheimer’s pathology.
Interestingly, plasma Aβ levels did not reflect central amyloid pathology, as displayed by amyloid-PET (Fig. 2). However, only a small subgroup of 20 patients received an amyloid-PET; therefore, the concordance between Aβ42/40 should be further studied in larger cohorts. In addition, a correlation between quantified amyloid-PET scans and plasma Aβ levels might provide further insights into the relationship between central amyloid pathology and peripheral Aβ as potential biomarker.
The only correlation between central amyloid pathology and peripheral Aβ was observed for Aβ42/40. These finding support the observation that not one single Aβ peptide can be used as a peripheral biomarker, but the combination of Aβ42 and Aβ40 rather reflects central amyloid disposition as a marker for AD.
Conclusion
Aβ peptides can be sufficiently measured in plasma using the immuno-multiplex assay (V-PLEX Aβ [6E10], Mesoscale Discovery). Using this assay, we found that plasma Aβ42/40 is significantly lower in patients with AD dementia than in those with dementia not due to AD. Aβ levels in plasma are slightly influenced by the GFR, but not by age, sex, or liver function. These data suggest that Aβ42/40 is a biomarker that is moderately sensitive and specific for the differential diagnosis of dementia. We believe that plasma Aβ42/40 can serve as an enrichment tool to power larger study cohorts, as the use of Aβ42/40 as a biomarker for the differential diagnosis of different kinds of dementia need to be confirmed in larger cohorts. In particular, early diagnostic and follow-up studies with MCI patients are required to investigate if measurement of plasma Aβ42/40 levels can be used as an early screening tool for the development of AD.
References
Andreasson U, Perret-Liaudet A, van Waalwijk van Doorn LJC et al (2015) A practical guide to immunoassay method validation. Front Neurol 6:1–8. https://doi.org/10.3389/fneur.2015.00179
Cummings JL, Dubois B, Molinuevo JL, Scheltens P (2013) International work group criteria for the diagnosis of Alzheimer disease. Med Clin N Am 97:363–368. https://doi.org/10.1016/j.mcna.2013.01.001
Deuschl G, Maier W (2016) S3-Leitlinie “Demenzen”. http://www.dgn.org/leitlinien. Accessed 29 November 2017. In: Deuschl G, Maier W S3-leitlin. Demenzen. Dtsch. Gesellschaft für Neurol. Hrsg. Leitlinien für Diagnostik und Ther. der Neurol. http://tinyurl.com/hkwk6lf. Accessed 29 Nov 2017
Dubois B, Feldman HH, Jacova C et al (2007) Research criteria for the diagnosis of Alzheimer’s disease: revising the NINCDS-ADRDA criteria. Lancet Neurol 6:734–746. https://doi.org/10.1016/S1474-4422(07)70178-3
Fan L, Levey AS, Gudnason V et al (2015) Comparing GFR estimating equations using cystatin C and creatinine in elderly individuals. J Am Soc Nephrol 26:1982–1989. https://doi.org/10.1681/ASN.2014060607
Fandos N, Pérez-Grijalba V, Pesini P et al (2017) Plasma Aβ42/40 ratios as biomarkers for Aβ cerebral deposition in cognitively normal individuals. Alzheimer’s Dement Diagn Assess Dis Monit 8:179–187. https://doi.org/10.1016/j.dadm.2017.07.004
Gilfrich JV, Birks LS (1984) Estimation of detection limits in X-ray fluorescence spectrometry. Anal Chem 56:77–79. https://doi.org/10.1021/ac00265a021
Gronewold J, Klafki H-W, Baldelli E et al (2015) Factors responsible for plasma β-amyloid accumulation in chronic kidney disease. Mol Neurobiol 53:3136–3145. https://doi.org/10.1007/s12035-015-9218-y
Hansson O, Stomrud E, Vanmechelen E et al (2012) Evaluation of plasma Abeta as predictor of Alzheimer’s disease in older individuals without dementia: a population-based study. J Alzheimers Dis 28:231–238. https://doi.org/10.3233/JAD-2011-111418
Huang Y, Potter R, Sigurdson W et al (2012) β-Amyloid dynamics in human plasma. Arch Neurol 69:1591–1597. https://doi.org/10.1001/archneurol.2012.1810
Irizarry MC (2004) Biomarkers of Alzheimer disease in plasma. NeuroRx 1:226–234. https://doi.org/10.1602/neurorx.1.2.226
Jack CR Jr, Albert M, Knopman DS et al (2011) Introduction to revised criteria for the diagnosis of Alzheimer’s disease: National Institute on Aging and the Alzheimer Association Workgroups. Alzheimer’s Dement 7:257–262. https://doi.org/10.1016/j.jalz.2011.03.004
Janelidze S, Stomrud E, Palmqvist S et al (2016) Plasma β-amyloid in Alzheimer’s disease and vascular disease. Sci Rep 6:26801. https://doi.org/10.1038/srep26801
Kaneko N, Nakamura A, Washimi Y et al (2014a) Novel plasma biomarker surrogating cerebral amyloid deposition. Proc Jpn Acad Ser B 90:353–364. https://doi.org/10.2183/pjab.90.353
Kaneko N, Yamamoto R, Sato T-A, Tanaka K (2014b) Identification and quantification of amyloid beta-related peptides in human plasma using matrix-assisted laser desorption/ionization time-of-flight mass spectrometry. Proc Jpn Acad Ser B Phys Biol Sci 90:104–117. https://doi.org/10.2183/pjab.90.104
Klafki H-W, Staufenbiel M, Kornhuber J, Wiltfang J (2006) Therapeutic approaches to Alzheimer’s disease. Brain 129:2840–2855. https://doi.org/10.1093/brain/awl280
Klafki H-W, Hafermann H, Bauer C et al (2016) Validation of a commercial chemiluminescence immunoassay for the simultaneous measurement of three different amyloid-β peptides in human cerebrospinal fluid and application to a clinical cohort. J Alzheimers Dis 54:691–705. https://doi.org/10.3233/JAD-160398
Lewczuk P, Esselmann H, Otto M et al (2004) Neurochemical diagnosis of Alzheimer’s dementia by CSF Aβ42, Aβ42/Aβ40 ratio and total tau. Neurobiol Aging 25:273–281. https://doi.org/10.1016/S0197-4580(03)00086-1
Lewczuk P, Matzen A, Blennow K et al (2016) Cerebrospinal fluid Aβ42/40 corresponds better than Aβ42 to amyloid PET in Alzheimer’s disease. J Alzheimer’s Dis 55:813–822. https://doi.org/10.3233/JAD-160722
Lövheim H, Elgh F, Johansson A et al (2017) Plasma concentrations of free amyloid β cannot predict the development of Alzheimer’s disease. Alzheimer’s Dement 13:778–782. https://doi.org/10.1016/j.jalz.2016.12.004
McKhann GM, Knopman DS, Chertkow H et al (2011) The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dement 7:263–269. https://doi.org/10.1016/j.jalz.2011.03.005
Mehta PD, Pirttilä T, Mehta SP et al (2000) Plasma and cerebrospinal fluid levels of amyloid beta proteins 1–40 and 1–42 in Alzheimer disease. Arch Neurol 57:100–105. https://doi.org/10.1001/archneur.57.1.100
Olsson B, Lautner R, Andreasson U et al (2016) CSF and blood biomarkers for the diagnosis of Alzheimer’s disease: a systematic review and meta-analysis. Lancet Neurol 15:673–684. https://doi.org/10.1016/S1474-4422(16)00070-3
Ovod V, Ramsey KN, Mawuenyega KG et al (2017) Amyloid β concentrations and stable isotope labeling kinetics of human plasma specific to central nervous system amyloidosis. Alzheimer’s Dement 13:841–849. https://doi.org/10.1016/j.jalz.2017.06.2266
Thomsen V, Schatzlein D, Mercuro D (2003) Limits of detection in spectroscopy. Pure Appl Chem 18:112–114
Toledo JB, Vanderstichele H, Figurski M et al (2011) Factors affecting Aβ plasma levels and their utility as biomarkers in ADNI. Acta Neuropathol 122:401–413. https://doi.org/10.1007/s00401-011-0861-8
Acknowledgements
We thank Ulrike Heinze and Anke Jahn-Brodmann for the processing of biomaterial and their support with the Aβ assay performance. We would like to thank Editage (http://www.editage.com) for English language editing. Prof. Dr. Jens Wiltfang is supported by an Ilídio Pinho professorship and Institute of Biomedicine of Aveiro (iBiMED) (UID/BIM/04501/2013), at the University of Aveiro, Portugal.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants are in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Vogelgsang, J., Shahpasand-Kroner, H., Vogelgsang, R. et al. Multiplex immunoassay measurement of amyloid-β42 to amyloid-β40 ratio in plasma discriminates between dementia due to Alzheimer’s disease and dementia not due to Alzheimer’s disease. Exp Brain Res 236, 1241–1250 (2018). https://doi.org/10.1007/s00221-018-5210-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-018-5210-x