Abstract
Recent research has provided evidence suggesting a link between inefficient processing of multisensory information and incidence of falling in older adults. Specifically, Setti et al. (Exp Brain Res 209:375–384, 2011) reported that older adults with a history of falling were more susceptible than their healthy, age-matched counterparts to the sound-induced flash illusion. Here, we investigated whether balance control in fall-prone older adults was directly associated with multisensory integration by testing susceptibility to the illusion under two postural conditions: sitting and standing. Whilst standing, fall-prone older adults had a greater body sway than the age-matched healthy older adults and their body sway increased when presented with the audio–visual illusory but not the audio–visual congruent conditions. We also found an increase in susceptibility to the sound-induced flash illusion during standing relative to sitting for fall-prone older adults only. Importantly, no performance differences were found across groups in either the unisensory or non-illusory multisensory conditions across the two postures. These results suggest an important link between multisensory integration and balance control in older adults and have important implications for understanding why some older adults are prone to falling.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although it is well known that older adults exhibit increased postural instability and are more prone to encountering problems in maintaining balance than younger adults (for a review, see Horak et al. 1989), relatively little is understood about the perceptual and cognitive factors underpinning posture control as we age. More particularly, ageing is associated with falls, with between 33 % and 50 % of people older than 65 falling each year (Kenny et al. 2009), which can seriously affect the quality of life for the older adult (Painter et al. 2012). It is, therefore, important to provide a better understanding of the underlying causes of falling in order to develop efficient interventions and rehabilitation programmes to prevent loss of balance control in older adults.
Previous studies have suggested that what determines whether a person is fall-prone is a complex interaction between a number of sensory, cognitive, and physiological factors. For example, sensory decline, as a consequence of the ageing process, is suspected to be one of the main causes for falling in older adults. In particular, decline in visual and auditory function with increasing age has been associated with falls risk and risk of recurrent falling (Tromp et al. 2001; Abdelhafiz and Austin 2003; Rubenstein 2006; Kulmala et al. 2009; Lord et al. 2010). Other research has implicated various risk factors for falls including balance and gait abnormalities (Tinetti and Williams 1998), cognitive impairment (Wolfson et al. 1985), and physiological factors, such as orthostatic hypotension, and cardiovascular disorders, such as carotid sinus hypersensitivity or vasovagal hypersensitivity (Davies and Kenny 1996). Several studies also indicate psychosocial factors such as fear of falling and balance confidence as risk factors for further falls (Cumming et al. 2000; Friedman et al. 2002). Thus, there seems to be no one causal factor for falling, nor have interventions based on any single factor been completely successful in preventing recurrent falls (for a review of existing intervention strategies and their efficacy, see Gillespie et al. 2010).
Although it is well known that inputs from the vestibular system provide internal information concerning postural control (Allen et al. 2004; Angelaki and Cullen 2008), recent research into vestibular function has highlighted the role of information from other sensory modalities on factors related to efficient postural control, such as balance, self-motion, and heading direction (e.g. Fetsch et al. 2010; deAngelis and Angelaki 2012). For example, visual information provides external information concerning the physical and spatial attributes of the environment being navigated, which can affect posture control (Allen et al. 2004; Rump and McNamara 2007). It is argued that these visual and vestibular inputs are integrated in a statistically optimal fashion, i.e. dependent on the reliability of the component sensory inputs, in order to achieve efficient self-motion perception (Fetsch et al. 2009; Butler et al. 2010; Fetsch et al. 2010). Also, the updating of spatial information as we navigate through our environment is achieved by the integration of information from the vestibular system as well as from other sensory systems such as vision (Durgin 2009; Durgin et al. 2005a, b). When vision is reduced, other sensory modalities, such as audition and touch, can provide information about the spatial properties of the environment (Gagnon et al. 2012; Klatzky et al. 2006). Thus, it is evident that the ability to integrate and organise relevant information from different sensory inputs is very important in successfully maintaining balance whilst navigating our environment.
However, few studies have investigated the role of multisensory integration on balance control in older adults. Those studies that have investigated this issue have typically reported that older adults have difficulties in recalibrating the relative reliability of different sensory inputs, particularly vision and proprioception, in response to environmental changes for the purpose of balance control (Horak et al. 1989; Jeka et al. 2010; Barrett et al. 2013). Multisensory recalibration, also known as sensory reweighting, refers to the adaptive use of changing or conflicting sensory inputs for the purpose of efficiently perceiving one’s environment (Ernst and Bülthoff 2004). During changes to the environment (e.g. when walking from a light to dark room), or in the individual’s internal state (e.g. walking or driving), this sensory reweighting is necessary for estimating body dynamics and maintaining successful postural control (Carver et al. 2006; Maurer et al. 2006). It has been shown that the ability to effectively reweight visual, vestibular, proprioceptive, and other sensory inputs, when one of more inputs becomes less reliable, declines as a function of ageing (Horak et al. 1989; Teasdale et al. 1991). Moreover, efficient reweighting of sensory inputs for perception may be further impaired in fall-prone older adults in comparison with healthy older adults (Jeka et al. 2010), especially when visual (Barrett et al. 2013) or auditory (Lin and Ferrucci 2012) information is unreliable.
Other research, however, suggests that perception in older adults benefits from the combination of redundant information from across the senses. Previous studies have shown that when sensory information is noisy and unreliable, perception can be enhanced by integrating redundant multisensory inputs relative to perception based on either of the unisensory stimuli alone (Laurienti et al. 2005). This process may be explained by the principle of inverse effectiveness (Stein and Meredith 1993), which states that responsiveness to a multisensory stimulus increases when the responsiveness to the best of the modality-specific component stimuli decreases (Stein and Stanford 2008). In other words, multisensory stimulation has a greater effect on perception when the ability to perceive the unisensory components stimuli is reduced. It is possible that this process also occurs to the benefit of perception in older adults. For example, perception in older adults may rely more on multisensory integration to compensate for the decline in sensory acuity and function as a result of ageing. An increasing number of studies provide support for enhanced multisensory integration in older adults, with a particular facilitation on response speeds to cross-modal combinations of visual, auditory, or tactile stimuli over their unisensory components (Laurienti et al. 2006; Peiffer et al. 2007; Mahoney et al. 2011).
However, the processes mediating enhanced multisensory integration may also sometimes result in a cost to perception in older adults. Specifically, efficient cross-modal integration depends on a certain temporal and spatial proximity between the stimuli (see, e.g. Sarko et al. 2012; Stein and Meredith 1993), otherwise, this integration can result in an erroneous percept as stimuli with fall outside the spatial or temporal window of integration should be perceived as discrete. The width of these windows of integration is, however, dependent on developmental processes (Hillock et al. 2011), and it has been suggested that a widening of the time window of integration occurs with ageing (Diederich et al. 2008). This widening of the temporal window may facilitate the integration of congruent cross-sensory information as sensory acuity declines. However, as Poliakoff et al. (2006) have shown, this process may result in increasing distractibility in older adults from cross-modal, task-irrelevant information. In support of this idea, Setti et al. (2011) reported increasing susceptibility to the multisensory ‘sound-induced flash illusion’ with ageing, and that susceptibility to this illusion appears to be sustained in older than in younger adults over longer temporal delays between the auditory and visual stimuli. The sound-induced flash illusion occurs when the presentation of two auditory ‘beeps’ paired with a single brief visual stimulus (flash) results in the perception of two visual ‘flashes’ (Shams et al. 2000, 2002). The illusion occurs due to the temporal proximity of the auditory stimuli to the visual stimulus resulting in the auditory inputs being integrated with the visual information (Shams et al. 2002). Setti et al. (2011) also reported that perception in older adults who experience postural control problems and suffer unexplained falls (which require medical attention) is more susceptible than that in a healthy cohort to this sound-induced flash illusion. This relatively greater susceptibility to the illusion with ageing is in accordance with previous research suggesting that multisensory integration is generally ‘enhanced’ in older adults, as both are possibly mediated by a change in the temporal window during which cross-modal stimuli are integrated (e.g. Laurienti et al. 2006; Diederich et al. 2008). Although a widening of the temporal window of integration may render it more likely that redundant, cross-modal signals are integrated to benefit perception in older adults, such a process may also be inefficient if it sometimes leads to the integration of unrelated stimuli that fall within this temporal window.
The results reported by Setti et al. (2011), that older adults with a history of falling are relatively more susceptible to the sound-induced flash illusion, suggest that the integration of information from the environment may be inefficient in this cohort. Moreover, that multisensory perception in this group is particularly inefficient suggests that it is associated with impaired balance control in older adults, likely resulting in a fall. Specifically, as balance control is dependent on both the integration of internal (e.g. Maurer et al. 2006) as well as the external cues from the environment (e.g. visual, auditory, and tactile), the inefficient processing of these cues may lead to an incoherent percept of the environment. As a consequence, several perceptual functions may be affected, particularly those relating to balance control. For example, an increase in distractibility (Poliakoff et al. 2006), or impaired spatial updating (Barrett et al. 2013), may lead to a rapid change in the maintenance of postural control.
However, a direct link between balance maintenance and the integration of multiple sensory cues from the environment has hitherto not been established in older adults. In this study, our aim was to investigate how the integration of external multisensory information was linked to posture control in older adults. Specifically, we wanted to elucidate the link between susceptibility to the sound-induced flash illusion and balance maintenance in fall-prone and healthy older adults. To that end, we measured susceptibility to the sound-induced flash illusion during both standing and sitting positions (control task) and participants’ postural sway (i.e. a measure of balance maintenance when standing) in these two older adult groups.
We hypothesised that if optimal balance control depends on the efficient integration of multisensory information from the environment, then balance control in older adults with a history of falling may benefit from redundant multisensory inputs in the same way that other perceptual processes, such as discrimination (Laurienti et al. 2006), benefit from multisensory integration. In other words, if perceptual performance was equivalent across the fall-prone and healthy older adults to AV congruent stimuli, then we expected no difference across the groups in their ability to control balance. However, multisensory integration has been shown to be less efficient in the fall-prone older adult group relative to their healthy counterparts when presented with AV incongruent stimuli; therefore, we expected greater susceptibility to the sound-induced flash illusion to be observed in this group. Furthermore, if inefficient integration is linked to balance control, then greater susceptibility to the sound-induced flash illusion in this older group should, in turn, be found in situations in which balance control is required, such as when standing, relative to when it is not, such as when sitting. Moreover, we expected that fall-prone older adults would have increased postural sway compared to healthy older adults during the AV incongruent (i.e. illusory) compared with AV congruent trials. In contrast, whilst we expected healthy older adults to be susceptible to the sound-induced flash illusion due to ageing, we did not expect this susceptibility to be associated with balance control, since balance function is not compromised in this group and they are more efficient at integrating external, multisensory inputs relative to fall-prone adults. Finally, to ensure that there were no underlying perceptual differences across the groups, we expected no differences between fall-prone and healthy older adults on performance to either of the two audio–visual congruent conditions.
Method
Participants
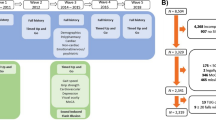
We recruited participants through the Technology Research for Independent Living (TRIL) centre in St James’s Hospital, Dublin. The TRIL cohort is a sample of more than 500 self-referred or clinician-referred persons who are over 60 years of age and who either have a history of falls or are healthy and not prone to falls. Of this cohort, 44 older adults (22 females, mean age = 73.1, SD = 4.9) volunteered to take part in this experiment. All participants were living independently in the community at the time of testing.
Each participant took part in a wide battery of clinical and behavioural assessments prior to the experiment. First, participants provided a detailed history of any fall incidents and each participant completed a falls risk assessment involving the following standardised tasks: BERG balance scale and timed up and go test (TUG), as well as tests designed to measure frailty including cardiovascular instability (Delta SBP) and grip strength (i.e. hand dynamometer measurement). We also tested sensory function including visual sensory acuity (LogMar chart), contrast sensitivity (Pelli–Robson chart), and hearing (Hughson–Westlake test). Cognitive function was assessed using the mini-mental state examination (MMSE). We recorded medical usage, particularly polypharmacy (indicating 4 or more medications). None of the participants had a history of psychiatric or neurological illness. Table 1 summarises the characteristics of the participants.
On the basis of their falls history, participants were assigned into one of two groups: healthy older adults (i.e. no history of falls) or older adults who can be described as ‘fall-prone’. Fall-prone older adults were defined as those who reported experiencing at least one unexplained fall (i.e. excluding tripping, slipping, and similar incidents) requiring medical attention in the last 5 years. Of the 23 fall-prone older adults (13 females, mean age = 73.95, SD = 4.94), 8 reported having had 1 fall, whereas 15 reported having recurrent falls. In contrast, 21 healthy older adults (9 females, mean age = 72.2, SD = 4.69) were those who reported never having experienced an unexplained fall.
The experiment was approved by both the St. James Hospital Ethics Committee and by the School of Psychology Research Ethics Committee, Trinity College Dublin and conformed to the Declaration of Helsinki. All participants provided informed, written consent prior to taking part in the experiment.
Stimuli and apparatus
The experiment was conducted using a Dell XPS M1530 laptop computer that was positioned such that the centre of the screen was at eye height and at a distance of approximately 57 cm for each participant whilst they were either standing or seating. The laptop was placed on a mobile, adjustable stand that was adjusted in both height and location accordingly. A nurse remained beside the participant during the entire experiment for safety reasons.
The stimuli consisted of a visual disc that was briefly presented on the screen (i.e. a ‘flash’) and an auditory tone (i.e. a ‘beep’). Specifically, the visual stimulus comprised of a white disc with a diameter subtending a visual angle of 1.5 degrees and a luminance of 31.54 fl. This disc was projected against a black background and appeared approximately 5 degrees below fixation. The visual stimulus was briefly flashed for 12 ms. The auditory stimulus was comprised of a brief burst of 3.5 kHz presented of 10 ms at 79 dB, which had the subjective experience of a ‘beep’. The auditory stimuli were delivered through integrated, stereo laptop speakers that were positioned just below the laptop monitor.
Postural sway was measured using a body-worn inertial ‘SHIMMER™’ sensor (developed by Shimmer Research, Dublin, Ireland). This sensor contains a tri-axial accelerometer that was used to measure postural sway along two axes: anterior–posterior (AP) and mediolateral (ML) (see Burns et al. 2010). The sensor was attached to the participant’s lower back, at approximately the level of L4 (i.e. the 4th vertebrae of the lumbar spine), using surgical tape. The participant wore the sensor throughout the experiment, although recordings were taken only when the participant was standing.
Design
There were two main testing blocks to the experiment: participants were presented with audio–visual trials that were blocked into audio–visual congruent or audio–visual incongruent (i.e. ‘illusory’) trials. The audio–visual illusory trials always consisted of 1 flash and 2 beeps. In these illusory trials, one of the auditory ‘beeps’ was always delivered simultaneously with a visual flash and the onset of the second auditory beep could either precede or lag behind the other ‘beep’ with a stimulus onset asynchrony (SOA) of either 70, 150, or 270 ms. The congruent audio–visual trials consisted of either 1 flash synchronously presented with 1 beep, or 2 flashes synchronously presented with 2 beeps. In the case of the 2 beeps and 2 flashes, the same SOA delays were presented between the beep and flash stimuli as in the illusory trials. Within a ‘congruent’ block, each trial was repeated 12 times yielding a total number of 12 single ‘flash–beep’ trials and 36 double ‘flash–beep’ trials (i.e. 6 repetitions at each of the three SOAs of 70, 150, 270 ms). Within an ‘illusory’ block, each trial was repeated 6 times for each of the six SOAs (i.e. −270, −150, −30, +30, +150, and +270 ms) yielding a total of 36 trials. Each participant conducted the congruent and illusory (incongruent) block twice: once from a seated position and once from a standing position, yielding a total of four experimental blocks. Block order, including both postural position (sitting or standing) and audio–visual blocks (illusory or congruent) conditions, was counterbalanced across participants. Trials were randomly presented within these blocks across participants.
The experiment was based on a mixed design with participant group as the between-subjects factor. For each of the participant groups, the experiment was based on a 2 × 2 × 3 design with posture (sitting or standing), audio–visual congruency (congruent or illusory), and SOA (preceding or lagging by 70, 150, or 270 ms) as within-subject factors.
Procedure
Participants completed both the illusory and congruent blocks of trials twice, once whilst seated and once whilst standing. Prior to the experiment, the experimenter adjusted the height and the position of the apparatus in order that the participant could comfortably view the scene from either a sitting or standing position, depending on the assigned block order. The participant was required to maintain a distance of 57 cm from the screen whilst sitting or standing.
Before the participant began the task, a baseline measure of balance sway, measured as acceleration, was taken during a 30-s trial. During this time, participants were required to maintain fixation on a visual cross that was presented on the computer screen and to maintain an upright position whilst remaining as still as possible. A reading of the participant’s baseline acceleration was taken to compare with their acceleration whilst completing the task. During this baseline measure, the participant had no secondary task to complete.
Once the baseline balance measure was taken, the participant was required to take a sitting or standing position, depending on the experimental design to which they were assigned. They were then presented with the audio–visual trials. They were informed that they would be presented with brief flashes and beeps and were instructed to verbally report to the experimenter the number of flashes they saw on the screen. During the audio–visual trials, a fixation cross was presented at the centre of the screen and remained on display throughout the experiment. Participants were instructed to maintain fixation throughout each trial. Following each trial, the experimenter recorded the participant’s response and initiated the next trial.
Before the experimental trials began, the participants conducted a block of 10 practice trials that they could repeat until they reported feeling comfortable with the task. These practice trials included examples of both congruent (i.e. ‘1 flash with 1 beep’ or ‘2 flashes with 2 beeps’ across different SOAs) and illusory (‘1 flash and 2 beeps’ across different SOAs) trials. Two participants asked to complete the practice block a second time before moving on to the experiment. All the other participants completed the practice block once before completing the experiment.
During the trials in which the participant was required to stand, acceleration data were sampled at 102.4 Hz and streamed via Bluetooth to a PC using a custom application developed in BioMOBIUS™, and were subsequently analysed using Matlab 7.10 (The Mathworks Inc., Natick, MA, USA). Acceleration data were band-pass filtered between 0.1 and 10 Hz, calibrated (Ferraris et al. 1995) and the influence of gravity was accounted for (Moe-Nilssen and Helbostad 2002). Recording started when the first stimulus was delivered in each block. The initial 5 s of data were removed, and the subsequent 25 s of data per block were considered for further analysis. Finally, low frequency drift was removed using a second-order polynomial fit (O’Sullivan et al. 2009). The root mean square (RMS) amplitude of the mediolateral (ML), anterior–posterior (AP), and cumulative horizontal acceleration signals was calculated for each trial.
Results
Assessment results
Prior to the experiment, we examined whether there were any differences in demographics or performance on a range of relevant assessments across groups. The results from these analyses are included in Table 1. Both groups were matched for age. There were no significant differences found between the fall-prone and healthy older adult groups in sensory acuity scores (i.e. vision or hearing), or in cognitive performance (i.e. MMSE), with both groups demonstrating normal cognitive functioning. As expected, performance on the BERG balance test and the TUG was significantly worse for the fall-prone older adults (Schoene et al. 2013). There was also a difference between the groups on polypharmacy with the fall-prone older adults taking more medications than the healthy older adults. However, on closer examination of the nature of the medication taken, we found that none of the older adults were prescribed medications that were psychotropic in nature. As such, we had no reason to assume that their medication should interfere with the participants’ sensory perception.
Balance results
The balance measures were analysed by comparing group differences between fall-prone and healthy older adults on their root mean squared (RMS) acceleration across the anterior–posterior (AP) and mediolateral (ML) directions, as well as the mean RMS acceleration, which is measured in units of acceleration due to gravity (1 g = 9.81 m/s2). Comparisons were made across trials on the RMS acceleration generated during the presentation of the illusory trials, congruent trials, and during the baseline trial (i.e. standing position when no auditory or visual stimulation was presented). Group differences were compared using independent t tests. The balance sway results are presented in Table 2 and plotted in Fig. 1. First, although we found significantly more body sway on average for fall-prone than healthy older adults during the baseline condition, this difference failed to reach significance for each of the ML and AP directions separately. This difference, with greater RMS sway in older adults with a history of falling than their healthy counterparts, is consistent with higher BERG test scores for fall-prone older adults (see Table 1). We found a significant difference in RMS acceleration across the fall-prone and healthy older adults during the presentation of the illusory trials only across both the mediolateral and anterior–posterior sway directions and overall postural sway. No group difference was found in body sway during any of the congruent conditions.
We then conducted a mixed ANOVA on the balance data, with fall status (fall-prone or healthy older adults) as the between groups factor and audio–visual (AV) trial type (illusory or congruent trials) as the within-group factor. We found a main effect of fall status [F (1, 42) = 3.997, p = 0.05], indicating increased postural sway for fall-prone older adults compared with healthy older adults. There was no effect of AV trial type [F (1, 42) < 1]. An interaction between fall status and AV trial type approached significance [F (1, 42) = 3.669, p = 0.06]. Due to the trend towards significance, and our previously stated hypothesis that fall-prone older adults would experience increased postural sway when exposed to illusory trials over congruent audio–visual trials and that this would not differ for healthy older adults, we conducted planned comparisons on the balance data to examine this interaction further. In accordance with our hypothesis, we found increased postural sway in the fall-prone group when exposed to illusory audio–visual stimuli (1 flash with 2 beeps) compared with congruent audio–visual stimuli (1 flash paired with 1 beep or 2 flashes paired with 2 beeps) [F (1, 42) = 5.052, p = 0.02]. In contrast, there was no difference in postural sway across the illusory and congruent audio–visual trials for healthy older adults [F (1, 42) < 1].
Behavioural results
We first compared the overall correct number of responses made by the fall-prone and healthy older adults, to both the illusory (2 beeps with 1 flash) and congruent (1 beep paired with 1 flash or 2 beeps paired with 2 flashes) multisensory trials. There were no differences in performance across groups in each of the conditions. Overall, we found fewer correct responses to the illusory conditions compared to either of the congruent conditions suggesting that both groups were susceptible to the illusion. These results are illustrated in Table 3.
We analysed accuracy performance using a mixed, four-way ANOVA with fall status (fall-prone or healthy older adults) as a between-subject measure and body stance (sitting or standing), AV trial type (illusory or congruent based on 2 flashes paired with 2 beeps) and SOA (70, 150, and 270 ms) as within-subject measures. We found no effect of fall status [F (1, 42) < 1] or body stance [F (1, 42) < 1]. There was a main effect found for trial type [F (1, 42) = 51.331, p < 0.001], with more accurate performance to the AV congruent than the illusory trials. There was also a main effect of SOA [F (2, 84) = 54.8032, p < 0.001], suggesting an overall increase in accuracy with increasing SOA between the auditory and visual stimuli. The two-way interaction between fall status and body stance approached significance [F (1, 42) = 3.295, p = 0.076]. None of the other interactions were significant nor were they approaching significance.
On the basis of the near-significant interaction between falls status and body stance, we analysed performance in the fall-prone and healthy groups separately using repeated measures ANOVAs with body stance (sitting or standing), AV trial type (illusory or congruent), and SOA (70, 150, and 270 ms) as within-subject measures. For the healthy older adults, we found significant main effects of trial type [F (1, 20) = 28.036, p < 0.001] and SOA [F (2, 40) = 30.719, p < 0.001] but there was no effect of body stance [F (1, 20) < 1]. The only interaction to reach significance was that between trial type and SOA [F (2, 40) = 22.198, p < 0.001]; otherwise, no other interactions reached significance level for this group. For the fall-prone older adults, we also found significant main effects of trial type [F (1, 22) = 24.501, p < 0.001), and SOA [F (2, 44) = 30.966, p < 0.001], and a trend to a main effect of body stance [F (1, 22) = 3.136, p < 0.09]. The interaction between trial type and SOA was significant [F (2, 44) = 19.939, p < 0.001], as it was for the healthy older adults. However, unlike the performance in the healthy older adult group, here we found a significant interaction between body stance and trial type [F (1, 22) = 4.490, p < 0.05], which is shown in Fig. 2. Following on from our previously stated hypothesis, i.e. that fall-prone older adults would be more susceptible to illusory audio–visual stimuli whilst in a standing position, in which their balance would be compromised, compared with a seated position, we conducted planned comparisons examining the proposed hypothesis. For the fall-prone older adults, significantly fewer correct responses were made to the illusory trials when in a standing position compared with a sitting position [F (1, 22) = 4.496, p < 0.05]. In contrast, there was no difference between the number of correct responses made to the congruent trials across either of the sitting or standing positions [F (1, 22) < 1] for this group. For healthy older adults, there was no difference between performance in a sitting or standing posture either for the AV illusory trials [F (1, 20) < 1] or the AV congruent trials [F (1, 20) < 1].
Finally, for completeness and in line with the previous studies (Setti et al. 2011; Foss-Feig et al. 2010), we compared performance to trials in which the second auditory beep preceded or lagged behind the audio–visual ‘flash’ stimulus for each of the participant groups. We found that performance for both the healthy and the fall-prone older adult groups was affected by the sequence of stimuli suggesting that older adults were more susceptible to the illusion when the ‘beep’ preceded than lagged behind the audio–visual ‘flash’ stimulus [F (1, 19) = 5.948, p < 0.03 and F (1, 22) = 8.625, p < 0.01, respectively].
Discussion
The present study was designed as an attempt to elucidate the relationship between multisensory integration and balance control in older adults. The results of the current study suggest two main findings. First, we found that there was greater body sway for fall-prone older adults than healthy older adults in both mediolateral and anterior–posterior directional planes. Interestingly, apart from the baseline measures, this difference in body sway across the groups was found under certain multisensory conditions only, specifically for conditions in which participants were presented with the sound-induced flash illusion trials but not when they conducted the multisensory congruent trials. Also, postural sway increased from the presentation of the audio–visual congruent to the audio–visual illusory conditions for the fall-prone older adults only. This distinction was not present for healthy older adults, in that postural sway was unaffected by the nature of the multisensory stimulation. The second main finding was that fall-prone older adults were more susceptible to the illusion when they were standing than when sitting, whilst, in contrast, no such difference was found across the body stance conditions for the healthy older adults.
These findings suggest that the multisensory illusory trials were more challenging for fall-prone older adults when compared to their healthy counterparts. On the face of it, these results may seem compatible with a previous literature which suggests that posture control in older adults with a history of falls is affected by dual-task conditions (for a review, see Schaefer and Schumacher 2011). For example, Maylor and Wing (1996a, b) found that when older adults had to maintain balance whilst performing one of a variety of cognitively demanding tasks (e.g. random digit generation, Brooks’ spatial memory, backward digit recall, or counting tasks), their postural stability decreased. Moreover, postural stability was particularly affected when older adults performed tasks based on visuospatial processing (Maylor and Wing 1996a, b). Recent findings have also suggested that training programmes based on dual tasks were successful in improving measures of standing balance and mobility (Li et al. 2010) as well as improving dual-task cognitive performance such as the Stroop task (Hiyamizu et al. 2012). It has also been shown that dual-task paradigms may be useful as clinical assessments for measuring the effects of cognitive impairment on postural control and are sensitive in predicting the risk of falls in older adults (Woollacott and Shumway-Cook 2002; Shumway-Cook et al. 1997).
In the present study, it could be speculated that the additional cognitive demands brought about by the dual-task situation of balance control as well as the perceptual task had a detrimental effect on postural control for fall-prone older adults but not for healthy older adults. However, such an explanation of the performance is not completely satisfactory for several reasons. First, under the same audio–visual stimulus conditions, albeit when the auditory and visual stimuli were congruent, no group differences emerged. Moreover, accuracy performance in this condition, as well as the overall accuracy performance to the illusory trials, did not differ across groups. Second, it is reasonable to suggest that the effect of a dual task on balance would increase dependant on the amount of stimuli involved in a cognitive secondary task. However, we found no evidence of a deficit in task performance or postural sway with an increasing number of stimuli presented: accuracy was lower and body sway was greater when participants were presented with 3 stimuli (1 visual and 2 auditory) as in the sound-induced flash illusion trials than when presented with 4 stimuli (2 visual and 2 auditory) as in the multisensory congruent trials (see Tables 2, 3 above). Moreover, task difficulty increased (less accurate performance) between the ‘1 flash with 1 beep’ and ‘2 flashes with 2 beeps’ congruent conditions, but this was not associated with a change in balance sway. Finally, the task remained the same throughout all of the multisensory conditions (i.e. to report the number of visual stimuli). Therefore, we would argue that any task-related, demand factors involved do not explain our findings.
Because of a concern that body sway may affect performance on the SIFI simply because of the concomitant effect on the properties of the visual stimulus (i.e. stimulus size and distance from fixation), we investigated whether any relationship existed between the degree of body sway and performance on the SIFI. First, susceptibility to the sound-induced flash illusion was not significantly correlated with postural sway for either fall-prone older adults (r = 0.06, p = 0.77) or healthy older adults (r = 0.17, p = 0.45). We then looked specifically at body sway along the anterior–posterior dimension (i.e. the direction most likely to affect the properties of the visual stimulus). There was no correlation between postural sway and susceptibility to the sound-induced flash illusion for either the fall-prone (r = 0.02, p = 0.90), or healthy (r = 0.26, p = 0.24) older adults. Secondly, evidence from previous studies has shown that the sound-induced flash illusion is robust to the visual angle of the stimulus. For example, different studies report the effects of the illusion across different visual angles from 1° (Bizley et al. 2012) to 1.5° (Setti et al. 2011; Rosenthal et al. 2009) or 2° (Kamke et al. 2012), and when the visual angle of the eccentricity from fixation varied from 5° (Setti et al. 2011) to 7° (Rosenthal et al. 2009) or even 12° (Shams et al. 2005). In the present experiment, participant sway by ±10 cm along the anterior–posterior axis may result in a deviation of ±0.3° in stimulus size and a deviation of ±1° in eccentricity from fixation. As our and previous findings suggest, it is unlikely that these slight variations in the visual angle subtended by the visual stimulus due to participant movement would affect their susceptibility to the sound-induced flash illusion.
In accordance with the previous findings (Setti et al. 2011), we found that the older adults were susceptible to the sound-induced flash illusion with no significant recovery as the SOA increased from 70 to 150 ms and 270 ms. However, we found no overall group difference in susceptibility to the illusion across the fall-prone and healthy older adult groups. This finding is in contrast with a previous report by Setti et al. (2011) in which older, fall-prone adults were found to be more susceptible to the sound-induced flash illusion than their healthy counterparts. Although it is not clear why we did not find an overall difference in susceptibility across the older adult groups, there are some differences across the studies, which may have affected the results. First, the average age of both the fall-prone and healthy participants in the present study was 2 years older than the age of the participants recruited to the Setti et al. study. As Setti et al. (2011) reported, ageing is associated with an increase in susceptibility to the sound-induced flash illusion, therefore, the relative increase in age of the participants in the present study may have masked any group differences which may have been present. Second, a wider range of SOAs was tested in the Setti et al. (2011) study compared to the present study (7 and 3, respectively), which may have reduced the possibility of observing differences across the groups.
The results of the present experiment suggest a direct association between balance maintenance and multisensory processing. Previous research has suggested an age-related decline in the efficient integration of information across multiple senses (e.g. Barrett et al. 2013; Setti et al. 2011) or in reweighting sensory information (Poliakoff et al. 2006; Hugenschmidt et al. 2009; Shumway-Cook and Woollacott 2000). The present result suggests that when inefficient multisensory integration is linked to posture control, this could, in turn, increase the risk of falls. Moreover, balance maintenance (as measured by postural sway during standing) in fall-prone older adults increased during the presentation of incongruent (i.e. illusory) multisensory trials relative to congruent multisensory stimulation. No such effect of multisensory stimulation on postural sway was found in healthy older adults. Moreover, although postural sway increased in fall-prone older adults in general compared to healthy older adults, the magnitude of this group difference was greatest when the participants were exposed to incongruent audio–visual stimuli. Previous studies have suggested that perception in older adults benefits from audio–visual stimulation particularly when the audio–visual stimuli are congruent (Laurienti et al. 2006; Peiffer et al. 2007; Mahoney et al. 2011; Diederich et al. 2008). Indeed, we observed a slight reduction (albeit not significant) in postural sway between the baseline condition and the AV congruent condition in the fall-prone older adults only. This observation is consistent with a reliance on congruent multisensory stimulation for efficient perception particularly in the fall-prone older adult group. However, this over-reliance on multisensory stimulation comes at a cost in that fall-prone older adults have a specific difficulty in processing incongruent audio–visual stimuli that, in turn, may have a direct effect on their ability to maintain postural control. This challenge to balance maintenance evoked by inefficient multisensory processing may result in increased postural sway and thus lead to increased fall-risk.
For fall-prone older adults relative to healthy older adults, the debilitative effect of maintaining posture control during a multisensory perceptual task cannot be accounted for by either a difference across groups in sensory processing or in general cognitive function as both groups of older adults were matched on a number of assessments including visual acuity, visual contrast sensitivity, auditory acuity, and MMSE. Moreover, there were no group differences between performance on the unisensory and multisensory trials in the task, suggesting that there were no underlying differences in perceptual function across the groups. However, previous findings suggest that performance on cognitive tasks whilst performing the secondary task of maintaining balance may become impaired, especially if the difficulty of the balance task is increased (Andersson et al. 2002; Yardley et al. 2001; Kerr et al. 1985). There is evidence for a “posture-first” strategy in which participants in dual-task scenarios sacrifice performance on cognitive tasks and prioritize maintaining balance control (for a review, see Bloem et al. 2006). Thus, whilst the fall-prone older adults were in a standing position, in which they had to maintain balance, perhaps there is a smaller allocation of attentional resources to the multisensory task and thus irrelevant stimuli may be more automatically processed. This may result in an increase in erroneous, or illusory, percepts when the cross-modal information is incongruent, such as in the sound-induced flash illusion. Healthy older adults may not require the same amount of attentional resources as fall-prone older adults to maintain balance, thus perhaps they would have more resources to allocate to the perceptual task.
In sum, our findings suggest an interesting link between balance maintenance and multisensory integration in ageing. The results suggest that maintaining balance control is compromised by an increased inefficiency in multisensory processing for fall-prone older adults but not healthy older adults. Inefficient multisensory integration may lead to distractibility and sensory confusion resulting in an increase in the risk of having a fall. What is unclear, however, is whether multisensory information processing in general is less efficient in older persons with a history of falling, or whether this inefficiency is related to the specific processing of information relevant to balance control. Future research on the link between balance maintenance and audio–visual integration could focus on the longitudinal effects of multisensory processing on gait and balance maintenance in order to determine the specificity of the effects and elucidate causal factors. Our current results, however, suggest that multisensory training may be an important factor in rehabilitation and may provide an effective intervention in reducing the risk of falls in older adults.
References
Abdelhafiz AH, Austin CA (2003) Visual factors should be assessed in older people presenting with falls or hip fracture. Age Ageing 32:26–30
Allen GL, Kirasic KC, Rashotte MA, Haun DB (2004) Aging and path integration skill: Kinesthetic and vestibular contributions to wayfinding. Percept Psychophys 66:170–179
Andersson G, Hagman J, Talianzadeh R, Svedberg A, Larsen HC (2002) Effect of cognitive load on postural control. Brain Res Bull 58:135–139
Angelaki DE, Cullen KE (2008) Vestibular system: the many facets of a multimodal sense. Annu Rev Neurosci 31:125–150. doi:10.1146/annurev.neuro.31.060407.125555
Barrett MM, Doheny EP, Setti A, Foran TG, Kenny RA, Newell Fiona N (2013) Reduced vision selectively impairs spatial updating in fall-prone older adults. Multisens Res 26:69–94. doi:10.1163/22134808-00002412
Bizley JK, Shinn-Cunningham BG, Lee AK (2012) Nothing is irrelevant in a noisy world: sensory illusions reveal obligatory within-and across-modality integration. J Neurosci 32:13402–13410. doi:10.1523/JNEUROSCI.2495-12.2012
Bloem BR, Grimbergen YA, van Dijk JG, Munneke M (2006) The “posture second” strategy: a review of wrong priorities in Parkinson’s disease. J Neurol Sci 248:196–204. doi:10.1016/j.jns.2006.05.010
Burns A, Doheny E, Greene B, Foran T, Leahy D, O’Donovan K, McGrath M (2010) SHIMMER™: an extensible platform for physiological signal capture. In: engineering in medicine and biology society (EMBC), 2010 annual international conference of the IEEE. IEEE, pp 3759–3762
Butler JS, Smith ST, Campos JL, Bulthoff HH (2010) Bayesian integration of visual and vestibular signals for heading. J Vis 10:23. doi:10.1167/10.11.23
Carver S, Kiemel T, Jeka JJ (2006) Modeling the dynamics of sensory reweighting. Biol Cybern 95:123–134. doi:10.1007/s00422-006-0069-5
Cumming RG, Salkeld G, Thomas M, Szonyi G (2000) Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. J Gerontol Ser A: Biol Sci Med Sci 55:M299–M305
Davies A, Kenny R (1996) Falls presenting to the accident and emergency department: types of presentation and risk factor profile. Age Ageing 25:362–366
DeAngelis GC, Angelaki DE (2012) Visual-vestibular integration for self-motion perception. In: Murray MM, Wallace MT (eds) The neural bases of multisensory processes. CRC Press, Boca Raton
Diederich A, Colonius H, Schomburg A (2008) Assessing age-related multisensory enhancement with the time-window-of-integration model. Neuropsychologia 46:2556–2562. doi:10.1016/j.neuropsychologia.2008.03.026
Durgin FH (2009) When walking makes perception better. Curr Dir Psychol Sci 18:43–47
Durgin FH, Gigone K, Scott R (2005a) Perception of visual speed while moving. J Exp Psychol Hum Percept Perform 31:339–353. doi:10.1037/0096-1523.31.2.339
Durgin FH, Pelah A, Fox LF, Lewis J, Kane R, Walley KA (2005b) Self-motion perception during locomotor recalibration: more than meets the eye. J Exp Psychol Hum Percept Perform 31:398–419. doi:10.1037/0096-1523.31.3.398
Ernst MO, Bülthoff HH (2004) Merging the senses into a robust percept. Trends Cognit Sci 8:162–169. doi:10.1016/j.tics.2004.02.002
Ferraris F, Grimaldi U, Parvis M (1995) Procedure for effortless in-field calibration of three-axis rate gyros and accelerometers. Sens Mater 7:311–330
Fetsch CR, Deangelis GC, Angelaki DE (2010) Visual-vestibular cue integration for heading perception: applications of optimal cue integration theory. Eur J Neurosci 31:1721–1729. doi:10.1111/j.1460-9568.2010.07207.x
Fetsch CR, Turner AH, DeAngelis GC, Angelaki DE (2009) Dynamic reweighting of visual and vestibular cues during self-motion perception. J Neurosci 29:15601–15612. doi:10.1523/JNEUROSCI.2574-09.2009
Foss-Feig JH, Kwakye LD, Cascio CJ, Burnette CP, Kadivar H, Stone WL, Wallace MT (2010) An extended multisensory temporal binding window in autism spectrum disorders. Exp Brain Res 203:381–389. doi:10.1007/s00221-010-2240-4
Friedman SM, Munoz B, West SK, Rubin GS, Fried LP (2002) Falls and fear of falling: which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatr Soc 50:1329–1335
Gagnon L, Schneider FC, Siebner HR, Paulson OB, Kupers R, Ptito M (2012) Activation of the hippocampal complex during tactile maze solving in congenitally blind subjects. Neuropsychologia 50:1663–1671. doi:10.1016/j.neuropsychologia.2012.03.022
Gillespie L, Robertson M, Gillespie W, Lamb S, Gates S, Cumming R, Rowe B (2010) Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2(CD007146)
Hillock AR, Powers AR, Wallace MT (2011) Binding of sights and sounds: age-related changes in multisensory temporal processing. Neuropsychologia 49:461–467. doi:10.1016/j.neuropsychologia.2010.11.041
Hiyamizu M, Morioka S, Shomoto K, Shimada T (2012) Effects of dual task balance training on dual task performance in elderly people: a randomized controlled trial. Clin Rehabil 26:58–67. doi:10.1177/0269215510394222
Horak FB, Shupert CL, Mirka A (1989) Components of postural dyscontrol in the elderly: a review. Neurobiol Aging 10:727–738
Hugenschmidt CE, Mozolic JL, Tan H, Kraft RA, Laurienti PJ (2009) Age-related increase in cross-sensory noise in resting and steady-state cerebral perfusion. Brain Topogr 21:241–251. doi:10.1007/s10548-009-0098-1
Jeka JJ, Allison LK, Kiemel T (2010) The dynamics of visual reweighting in healthy and fall-prone older adults. J Mot Behav 42:197–208. doi:10.1080/00222895.2010.481693
Kamke MR, Vieth HE, Cottrell D, Mattingley JB (2012) Parietal disruption alters audiovisual binding in the sound-induced flash illusion. Neuroimage 62:1334–1341. doi:10.1016/j.neuroimage.2012.05.063
Kenny RA, Dishongh T, Newell F, Ni Scanail C (2009) Research to reduce falls in older people: the TRIL centre. Geriatr Med 39:326–327
Kerr B, Condon SM, McDonald LA (1985) Cognitive spatial processing and the regulation of posture. J Exp Psychol Human 11:617
Klatzky RL, Marston JR, Giudice NA, Golledge RG, Loomis JM (2006) Cognitive load of navigating without vision when guided by virtual sound versus spatial language. J Exp Psychol Appl 12:223–232
Kulmala J, Viljanen A, Sipila S et al (2009) Poor vision accompanied with other sensory impairments as a predictor of falls in older women. Age Ageing 38:162–167. doi:10.1093/ageing/afn228
Laurienti PJ, Burdette JH, Maldjian JA, Wallace MT (2006) Enhanced multisensory integration in older adults. Neurobiol Aging 27:1155–1163. doi:10.1016/j.neurobiolaging.2005.05.024
Laurienti PJ, Perrault TJ, Stanford TR, Wallace MT, Stein BE (2005) On the use of superadditivity as a metric for characterizing multisensory integration in functional neuroimaging studies. Exp Brain Res 166:289–297. doi:10.1007/s00221-005-2370-2
Li KZ, Roudaia E, Lussier M, Bherer L, Leroux A, McKinley PA (2010) Benefits of cognitive dual-task training on balance performance in healthy older adults. J Gerontol A Biol Sci Med Sci 65:1344–1352. doi:10.1093/gerona/glq151
Lin FR, Ferrucci L (2012) Hearing loss and falls among older adults in the United States. Arch Intern Med 172:369–371. doi:10.1001/archinternmed.2011.728
Lord SR, Smith ST, Menant JC (2010) Vision and falls in older people: risk factors and intervention strategies. Clin Geriatr Med 26:569–581. doi:10.1093/ageing/afl084
Mahoney JR, Li PC, Oh-Park M, Verghese J, Holtzer R (2011) Multisensory integration across the senses in young and old adults. Brain Res 1426:43–53. doi:10.1016/j.brainres.2011.09.017
Maurer C, Mergner T, Peterka RJ (2006) Multisensory control of human upright stance. Exp Brain Res 171:231–250
Maylor EA, Wing AM (1996a) Age differences in postural stability are increased by additional cognitive demands. J Gerontol Ser B: Psychol Sci Soc Sci 51:143–154
Maylor EA, Wing AM (1996b) Age differences in postural stability are increased by additional cognitive demands. J Gerontol Ser B: Psychol Sci Soc Sci 51:P143–P154
Moe-Nilssen R, Helbostad JL (2002) Trunk accelerometry as a measure of balance control during quiet standing. Gait Posture 16:60–68
O’Sullivan M, Blake C, Cunningham C, Boyle G, Finucane C (2009) Correlation of accelerometry with clinical balance tests in older fallers and non-fallers. Age Ageing 38:308–313. doi:10.1093/ageing/afp009
Painter JA, Allison L, Dhingra P, Daughtery J, Cogdill K, Trujillo LG (2012) Fear of falling and its relationship with anxiety, depression, and activity engagement among community-dwelling older adults. Am J Occup Ther 66:169–176. doi:10.5014/ajot.2012.002535
Peiffer AM, Mozolic JL, Hugenschmidt CE, Laurienti PJ (2007) Age-related multisensory enhancement in a simple audiovisual detection task. NeuroReport 18:1077–1081
Poliakoff E, Ashworth S, Lowe C, Spence C (2006) Vision and touch in ageing: crossmodal selective attention and visuotactile spatial interactions. Neuropsychologia 44:507–517. doi:10.1016/j.neuropsychologia.2005.07.004
Rosenthal O, Shimojo S, Shams L (2009) Sound-induced flash illusion is resistant to feedback training. Brain Topogr 21:185–192. doi:10.1007/s10548-009-0090-9
Rubenstein LZ (2006) Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing 35(Suppl 2):ii37–ii41. doi:10.1093/ageing/afl084
Rump B, McNamara TP (2007) Updating in models of spatial memory. In: Spatial cognition V reasoning, action, interaction. Springer, Berlin, pp 249–269
Schaefer S, Schumacher V (2011) The interplay between cognitive and motor functioning in healthy older adults: findings from dual-task studies and suggestions for intervention. Gerontology 57:239–246. doi:10.1159/000322197
Schoene D, Wu SM, Mikolaizak AS, Menant JC, Smith ST, Delbaere K, Lord SR (2013) Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: systematic review and meta-analysis. J Am Geriatr Soc 61:202–208. doi:10.1111/jgs.12106
Setti A, Burke KE, Kenny RA, Newell FN (2011) Is inefficient multisensory processing associated with falls in older people? Exp Brain Res 209:375–384. doi:10.1007/s00221-011-2560-z
Shams L, Kamitani Y, Shimojo S (2000) What you see is what you hear. Nature 408:6814
Shams L, Kamitani Y, Shimojo S (2002) Visual illusion induced by sound. Cognit Brain Res 14:147–152
Shams L, Ma WJ, Beierholm U (2005) Sound-induced flash illusion as an optimal percept. NeuroReport 16:1923–1927
Shumway-Cook A, Woollacott M (2000) Attentional demands and postural control: the effect of sensory context. J Gerontol Ser A: Biol Sci Med Sci 55:M10
Shumway-Cook A, Woollacott M, Kerns KA, Baldwin M (1997) The effects of two types of cognitive tasks on postural stability in older adults with and without a history of falls. J Gerontol Ser A: Biol Sci Med Sci 52:M232–M240
Sarko DK, Nidiffer AR, Powers AR III, Ghose D, Hillock-Dunn A, Fister MC, Krueger J, Wallace MT (2012) Spatial and temporal features of multisensory processes: bridging animal and human studies. In: Murray MM, Wallace MT (eds) The neural bases of multisensory processes. CRC Press, Boca Raton
Stein BE, Meredith A (1993) The merging of the senses. MIT Press, Cambridge
Stein BE, Stanford TR (2008) Multisensory integration: current issues from the perspective of the single neuron. Nature Rev Neurosci 9:255–266
Teasdale N, Stelmach GE, Breunig A (1991) Postural sway characteristics of the elderly under normal and altered visual and support surface conditions. J Gerontol 46:B238–B244
Tinetti ME, Williams CS (1998) The effect of falls and fall injuries on functioning in community-dwelling older persons. J Gerontol Ser A: Biol Sci Med Sci 53:M112–M119
Tromp A, Pluijm S, Smit J, Deeg D, Bouter L, Lips P (2001) Fall-risk screening test: a prospective study on predictors for falls in community-dwelling elderly. J Clin Epidemiol 54:837–844
Wolfson LI, Whipple R, Amerman P, Kaplan J, Kleinberg A (1985) Gait and balance in the elderly. Two functional capacities that link sensory and motor ability to falls. Clin Geriatr Med 1:649–659
Woollacott M, Shumway-Cook A (2002) Attention and the control of posture and gait: a review of an emerging area of research. Gait Posture 16:1–14
Yardley L, Gardner M, Bronstein A, Davies R, Buckwell D, Luxon L (2001) Interference between postural control and mental task performance in patients with vestibular disorder and healthy controls. J Neurol Neurosur Ps 71:48–52
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stapleton, J., Setti, A., Doheny, E.P. et al. A standing posture is associated with increased susceptibility to the sound-induced flash illusion in fall-prone older adults. Exp Brain Res 232, 423–434 (2014). https://doi.org/10.1007/s00221-013-3750-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-013-3750-7