Abstract
Non-pulsatile tinnitus is considered to be an auditory phantom percept. The extremely emotional context of disabling tinnitus often leads to a higher level of selective attention directed toward the tinnitus. As such, tinnitus is a continuously distracting auditory event. Auditory attention is associated with the activation of the intraparietal sulcus (IPS), and modulating the IPS with 10 Hz transcranial magnetic stimulation (TMS) creates the ability to ignore salient distractors. Thus, it can be expected that modulating the parietal area might interfere with the perception of tinnitus. The effect of TMS on tinnitus is evaluated using a double-cone coil tilted to the left parietal area in 24 individuals (study 1) and in 40 individuals with the double-cone coil symmetrically overlying both parietal areas (study 2). When transient tinnitus suppression is noted, the patient is asked to estimate the decrease in tinnitus in percentage using the numeric rating scale. The procedure is repeated with stimulations at sham, 1 and 10 Hz, each stimulation session consisting of 200 pulses for study 1 and for study 2 stimulations at sham, 1, 5, and 10 Hz, each stimulation session consisting of 200 pulses. For both studies, the order of the different stimulation frequencies was randomized over the participants. For study 1, patients report a significant transient reduction of the tinnitus percept for 10 Hz stimulation in comparison with, respectively, pre-treatment, sham, and 1 Hz stimulation, with a suppression effect of 11.36 %. No significant effect was obtained for 1 Hz stimulation with the coil tilted toward the left parietal area. For study, 2 patients revealed a significant suppression effect on 1, 5, and 10 Hz in comparison with pre-treatment. However, only stimulation at 5 and 10 Hz had a significant difference in comparison with sham with a suppression effect of, respectively, 8.78 and 9.50 %. Our data suggest that the parietal area is involved in tinnitus perception and that 10 Hz TMS using the double-cone coil overlying the parietal area can modulate tinnitus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-pulsatile tinnitus is considered to be an auditory phantom percept (Jastreboff 1990). Approximately 5–15 % of the population experience tinnitus, and in about 1–3 % of the population, tinnitus has a severe impact on the quality of daily life. Tinnitus is often associated with insomnia, anxiety, and depression (Hoffman and Reed 2004).
Over the last decade, transcranial magnetic stimulation (TMS) received increasing attention as a potential therapy for the treatment of tinnitus. TMS is a non-invasive tool provoking a strong impulse of magnetic field that induces an electrical current to a specific region of the brain through an intact scalp. An increasing number of clinical studies indeed have demonstrated that TMS targeting the temporal lobe can alter tinnitus (De Ridder et al. 2005, 2007a, b Kleinjung et al. 2005; Eichhammer et al. 2007). Typically, TMS in tinnitus is applied with a figure-eight coil. TMS modulates the superficial cortical areas directly but has an indirect effect on remote areas functionally connected to the stimulated area such as the auditory thalamus (May et al. 2007). A recent study using positron emission tomography (PET) revealed that TMS using a double-cone coil (DCC) can modulate deeper structures as well as a number of more distal cortical areas (Hayward et al. 2007). Interestingly, it was shown that frontal TMS on tinnitus using a double-cone coil with large angled windings can modulate tinnitus loudness and tinnitus annoyance (Vanneste et al. 2011c).
The emotional context of disabling tinnitus can lead to a higher level of selective attention directed toward the tinnitus signal, leading to increasing distress and preventing adaptive responses (Searchfield et al. 2007). Impaired concentration and reduced ability to undertake cognitively demanding tasks are frequently reported in tinnitus patients (Hallam et al. 2004; Stevens et al. 2007). It has been suggested that activation of attentional and cognitive brain networks contributes to the annoyance, the distress, and the inability to habituate to tinnitus (Zenner and Zalaman 2004), since attentional guidance can modulate perceptual processing of information in the brain (Kastner et al. 1998; Beck and Kastner 2005). Many studies have shown that the parietal brain regions are linked to a top-down attentional control (Serences and Yantis 2006). More specifically, auditory attention activates the left IPS (Salmi et al. 2009), and activity in the left IPS correlates negatively with the presence of salient auditory distractors (Watkins et al. 2007). A recent paper modulating the left intraparietal sulcus (IPS) with 10 Hz transcranial magnetic stimulation (TMS) shows the ability to ignore salient distractors (Mevorach et al. 2010).
In the present study, we hypothesized that the parietal lobe might also be involved in tinnitus perception. As the IPS is involved in ignoring salient distracting auditory events and tinnitus is a distracting auditory event, we expect that modulating the parietal lobe could lead to a reduction in the perception of tinnitus. A second question is whether a potential TMS modulating effect might be frequency specific. And a third question relates to whether the effect is specific for a side and location, that is, should TMS target the superior or inferior parietal lobe, and predominantly the left or right side.
Hence, we conducted a TMS study verifying whether modulating the parietal lobe can modulate tinnitus perception.
Study 1
Methods
Patients
Twenty-four tinnitus patients (13 males and 11 females) participated in this experiment at the tinnitus clinic of the Antwerp University Hospital. The mean age was 52.22 years (SD = 9.84). Thirteen patients presented with narrow band noise and 11 patients presented with pure tone tinnitus, while 11 patients had bilateral tinnitus and 13 unilateral tinnitus. The mean tinnitus duration was 9.13 years (SD = 8.37). All participants underwent a complete audiological, ENT, and neurological investigation to rule out possible treatable causes for their tinnitus.
The study has been approved by the Antwerp University Hospital IRB (‘Comité voor medische ethiek’). Patients gave an oral informed consent before the procedure. The TMS was performed as a diagnostic test in a screening for potential treatment. For all patients, it was the first TMS session.
TMS
Before the TMS session, patients graded their tinnitus perception (‘How loud do you perceive your tinnitus?’) on a numeric rating scale from 0 to 10. The motor threshold to TMS is first determined by placing the figure-eight coil over the motor cortex using EMG. The coil was positioned tangentially to the scalp and oriented so that the induced electrical currents would flow approximately perpendicular to the central sulcus, at 45° angle from the mid-sagittal line. TMS is performed using a super rapid stimulator (Magstim Inc, Wales, UK) with a double-cone coil (DCC) (P/N 9902-00; Magstim Co. Ltd) placed over the parietal cortex, 4 cm behind the motor strip, as localized by TMS at motor threshold. We opt to use a DCC as recent research revealed that placing the coil over the medial parietal cortex activates both the left and right IPS (Hayward et al. 2007). This is approximately halfway between the inion and the zenith of the vertex. In the first study, the coil is maximally tilted toward the left IPS (Fig. 1a). The intensity of the stimulation was set at 80 % of the motor threshold. Patients received repeated stimulation in random order at 1 and 10 Hz, and sham stimulation, each stimulation session consisting of 200 pulses. The frequency during sham was randomized over the participants. When transient tinnitus suppression is perceived, the amount of improvement in tinnitus perception (“How much in percentage is your tinnitus perception reduced?”) is noted. When tinnitus perception is back to its initial score, the next TMS frequency is applied. The presence of a control procedure (i.e., placebo effect) is tested perpendicular over the same area at 1 or 10 Hz for 200 pulses. All patients were wearing earplugs during the TMS sessions.
In contrast to the TMS study modulating the left intraparietal sulcus (IPS) with 10 Hz TMS inducing the ability to ignore salient distractors (Mevorach et al. 2010), we did not apply a specific distractor task as the tinnitus patients are already distracted, by their tinnitus. In contrast to that study which was performed in a healthy population doing a global/local task applying TMS for 20 min, this study was performed in patients with tinnitus, delivering only 200 pulses, typically used in single session TMS tinnitus research (De Ridder et al. 2007a, b; Vanneste et al. 2010c, 2011c).
Statistical analysis
Calculations were performed using SPSS software package. A repeated-measure ANOVA was conducted with as within-subjects variable the different stimulation protocols (pre-treatment, 1 and 10 Hz as well as the sham treatment). A similar analysis was conducted with stimulation protocol as within-subjects variable and stimulation order as between-subjects variable.
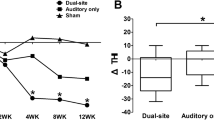
Results
Patients report a mean tinnitus perception of 5.73/10 before the TMS treatment. A repeated-measure ANOVA revealed a significant effect for the stimulation protocol (pre-treatment, 1 and 10 Hz as well as the sham treatment) F = 4.32, p < .01 (see Table 1). After correcting for multiple comparisons (Fisher Least Significant Difference (LSD) test), analyses revealed that 10 Hz significantly differ from pre-treatment, sham, and 1 Hz. A significant suppression was found of 15.01 % compared to pre-treatment, 14.41 % compared to sham, and 14.26 % compared to 1 Hz stimulation. No effect was obtained between pre-treatment, sham and 1 Hz stimulation.
In addition, a repeated-measures ANOVA controlling for the stimulation order revealed no significant effect for order (F = .54, p = .59) as well as the interaction effect between stimulation protocol and stimulation order (F = 1.39, p = .27), indicating that the order of stimulation had no influence on the obtained effect.
As we define responders as patients that have a suppression effect of more than 10 % in comparison with pre-treatment, 29 % responded with a suppression effect of 43.06 % for 10 Hz stimulation.
Study 2
To verify whether the suppression effect is limited to left IPS stimulation, we conducted a second study placing the TMS coil halfway between the inion and the zenith of the vertex symmetrically with the handle pointing up at the midline. Tilting of the coil could modulate a large part of parietal cortex. Apart from 1 and 10 Hz stimulation, we also included 5 Hz stimulation to verify whether a lower level of stimulation also can modulate the IPS. Previous research conducted at our research lab using a DCC shows significant difference when applying 1, 5, or 10 Hz targeting the anterior cingulate cortex (Vanneste et al. 2011b).
Patients
Forty tinnitus patients (24 males, 16 females) participated in this experiment at the TRI tinnitus clinic of the Antwerp University Hospital, Belgium. The mean age was 53.67 years (SD = 7.56). Twenty-four patients presented with narrow band noise and 16 patients with pure tone tinnitus. Twenty-nine patients had bilateral tinnitus and 11 patients unilateral tinnitus. The mean tinnitus duration was 7.12 years (SD = 3.24). All prospective participants undergo a complete audiological, ENT, and neurological investigation to rule out possible treatable causes for their tinnitus.
The study has been approved by the Antwerp University Hospital IRB (‘Comité voor medische ethiek’). Patients gave an oral informed consent before the procedure. The TMS was performed as a diagnostic test in a screening for potential treatment. For all patients, it was the first TMS session.
TMS
Similarly to study 1 before the TMS session, patients graded their tinnitus perception (‘How loud do you perceive your tinnitus?’) on a numeric rating scale from 0 to 10. The motor threshold to TMS is first determined by placing the figure-eight coil over the motor cortex using EMG similar to study 1. The DCC is then placed over the parietal cortex, 4 cm behind the motor strip, as localized by TMS at motor threshold. This is approximately halfway between the inion and the zenith of the vertex. The coil is held symmetrically with the handle pointing up at the midline (Fig. 1b). The intensity of the stimulation is set at 80 % of the motor threshold. Patients received repeated stimulation in random order all simulation protocols, namely 1, 5, and 10 Hz, and sham stimulation. Each stimulation session consists of 200 pulses. When transient tinnitus suppression is perceived using a Visual Analogue Scale (“How much is your tinnitus perception?”) is noted. When tinnitus perception is back to its initial score, the next TMS frequency is applied. The presence of a control procedure (i.e., placebo effect) is tested perpendicular over the same area at 1, 5, or 10 Hz for 200 pulses. The frequency during sham was randomized over the participants. All patients were wearing earplugs during the TMS sessions.
Statistical analysis
Calculations were performed using SPSS software package. A repeated-measure ANOVA was conducted with as within-subjects variable the different stimulation protocols (pre-treatment, 1, 5 and 10 Hz as well as the sham treatment).
Results
Patients report a mean tinnitus perception of 6.14/10 before TMS. A repeated-measure ANOVA revealed a significant effect for the stimulation protocol (pre-treatment, 1, 5 and 10 Hz as well as the sham treatment) F = 4.32, p < .01 (see Table 1). After correcting for multiple comparisons (LSD-test), further analyses revealed that 1, 5, and 10 Hz stimulation induce a suppression effect in comparison with pre-treatment. That is, compared to pre-treatment stimulation, a suppression effect was found for 1 Hz of 11.07 %, for 5 Hz of 17.01 %, and for 10 Hz of 17.10 %. However, comparing to sham only an effect remained for 5 and 10 Hz stimulation of 8.78 and 9.50 %, respectively.
A second repeated-measures ANOVA controlling for the stimulation order revealed no significant effect for order (F = 1.38, p = .46) as well as the interaction effect between stimulation protocol and stimulation order (F = .46, p = .98), indicating that the order of stimulation had no influence on the obtained effect.
Responders were defined as patients that have a suppression effect of more than 10 %. We found for 5 Hz stimulation in comparison with pre-treatment that 45 % of patients respond to stimulation with a suppression effect of 40 % and for 10 Hz stimulation in comparison with pre-treatment that 40 % of patients respond to stimulation with a suppression effect of 42.81 %.
A comparison between study 1 and study 2
A comparison was made between study 1 and 2 for the effect obtained at 10 Hz to verify whether coil placement is an influence in the results obtained.
Statistical analysis
Calculations were performed using the SPSS software package. A repeated-measure ANOVA was conducted with as within-subjects variable the 10 Hz treatment (pre versus post treatment) and between-subjects variable coil location (left IPS or biparietal cortex).
Results
Our analysis showed that a significant effect was obtained for treatment, F = 17.23, p < .001, revealing that post-treatment (M = 4.99, SD = 2.43) a significant suppression was obtained in comparison with pre-treatment (M = 5.99, SD = 2.16). No significant main effect was obtained for coil location nor for the interaction effect treatment × coil location.
To make sure that our findings are not the result of an overpowering of the study 2 (i.e., larger sample size in comparison with the study 1), we applied a resampling technique. Hence, we conducted a resampling analysis (i.e., bootstrapping) on which we draw 24 participants from study 2 and compare these with study 1 and test whether we still can obtain the same results. We repeated this process 20 times. Based on this technique, we also find a significant main effect for treatment (range of F = 14.39–16.81, p < .001) indicating the same effects as with the unbalanced sample size, thus suggesting a robust effect. Again, no significant main effect was demonstrated for coil location as well as for the interaction effect treatment × coil location.
Discussion
This is the first study to describe the effect of parietal lobe TMS on tinnitus using a DCC with large angled windings. Our results show that stimulation of the parietal lobe can change tinnitus perception with 10 Hz stimulation when the double-cone coil is tilted to the left as well as when the coil is positioned symmetrically over the parietal midline. When placing the coil over the biparietal cortex, a significant effect was obtained for both 5 and 10 Hz. Whether the coil is tilted or not does not seem to be important as there was no significant difference between the two studies for 10 Hz. This might be due to the low focality of TMS or to the fact that the effect is a non-specific effect, for example, arousal, distraction, or other effect.
The present data complement with previous investigations by providing direct evidence that the ability to ignore salient auditory distractors depends on a neural circuit involving the left IPS (Watkins et al. 2007). It has been shown that activity in the left IPS correlates negatively with the presence of salient auditory distractors (Watkins et al. 2007), and 10 Hz TMS can modulate the salience of the distractor (Mevorach et al. 2010). Previous research revealed that low- (1 Hz) and high-frequency (>5 Hz) TMS of the prefrontal cortex exert opposing effects (Speer et al. 2000), with low frequency TMS being predominantly inhibitory, decreasing metabolism, while high frequency TMS has an excitatory effect increasing metabolism (Kimbrell et al. 1999; Speer et al. 2000). As the salience of an auditory distractor depends on low activity in the left IPS, stimulating the left IPS with high frequency TMS, increasing metabolism, could reduce the salience of the auditory distractor.
However, whether the left or both parietal lobe cortices are modulated by TMS cannot be determined by this study. This should be determined by using a figure of 8 coil. It is possible that when stimulating both parietal lobe cortices, the effect is mediated by both parietal lobes, or the posterior cingulate cortex (Dosenbach et al. 2007) which is involved in one of the attention networks (Dosenbach et al. 2007, 2008) and tinnitus distress (Vanneste et al. 2010a). Indeed, a PET study evaluating metabolic changes associated with parietal lobe double-cone coil TMS demonstrates that this kind of stimulation also modulates PCC activity (Hayward et al. 2007).
A third possible explanation can also be proposed. Transcutaneous electrical nerve stimulation (TENS) via the second cervical nerve (C2) modulates tinnitus perception as well (Vanneste et al. 2010b). In a recent study, it was suggested that TMS of the temporal area could exert its tinnitus modulating effect both directly influencing the auditory cortex and indirectly via somatosensory afferents in the occipital branch of the C2 nerve (Vanneste et al. 2011a). Thus, the TMS effect obtained via parietal stimulation could actually be related to a C2 modulatory effect, as the C2 nerve innervates the back of the head, overlying the parietal area.
In addition, the claim that low frequency TMS exerts an inhibitory effect and high frequency TMS an excitatory effect has to be considered with care as the mechanisms of how TMS modulates neurons and interferes with neural functions are still incompletely understood. Auditory attention is mediated via a frontoparietal control mechanism, in which focal gamma band activity in parietal and frontal areas is nested on theta activity (Doesburg et al. 2012), and gamma band connectivity of frontal and parietal areas has been implicated in tinnitus as well (Schlee et al. 2009). This would suggest that the high frequency magneticstimulation hypothetically disrupts ongoing gamma band activity better than low frequency TMS. This is similar to the better results obtained with high frequency (10 and 25 Hz) TMS of the auditory cortex in comparison with low frequency TMS (Khedr et al. 2009). As tinnitus is associated with gamma band activity in the auditory cortex, a similar mechanism of high frequency TMS could be involved in altering the gamma band activity in temporal and parietal areas, possibly nothing more than a disruption of ongoing network activity.
Applying parietal TMS as a routine treatment is unlikely to be successful in its current form as only in 29 % of the patients in experiment 1 and 40 % in experiment 2 demonstrated a transient suppressive effect during the magnetic stimulation. The suppressive effect remains only as long as the stimulation lasts. The lack of neuronavigation use is a limitation of the study. Even though recent studies suggest that a probabilistic approach (i.e., non-neuronavigated) is equally good, this is only related to the auditory cortex (Langguth et al. 2006; Sparing and Mottaghy 2008). As for the prefrontal cortex there seems to be a different tendency, it should be considered that fMRI-guided stimulation might be more accurate, and it could influence the results as one of the multiple factors explaining inter-individual variability. Another limitation of this study is the sham control condition. As the sham coil mimics the sound of active TMS but without somatosensory sensation, it is not an optimal control condition. As patients in this study were naïve for TMS, they might not be able to identify whether they were stimulated with active or sham TMS. In addition, no patient had a worsening of their tinnitus. Yet, this might be due to the questions asked to the patient (i.e., “How much in percentage is your tinnitus perception reduced?”). Based on these questions, it is possible that patients only report improvement or non-improvement, but not a worsening. Lastly, it is possible that due to the different stimulation protocols, there is a carry-over effect from the previous to the next stimulation, even though the stimulation was only continued when the tinnitus was back to the initial level. Previous research has indeed revealed that preconditioning of cortical excitability exerts an influence on subsequent TMS (Suppa et al. 2008). The order of stimulations was randomized over the patients, preventing an order effect, but not excluding a preconditioning effect. This has to be taken into account as a potential weakness when interpreting the data. Future research might also include a specific distractor task similar to the TMS study modulating the left IPS with 10 Hz TMS inducing the ability to ignore salient distractors (Mevorach et al. 2010). This could further help to explore the specific function of the IPS in auditory attention.
Conclusion
In summary, our data suggest that 10 Hz TMS using the double-cone coil targeting the parietal can modulate tinnitus.
References
Beck DM, Kastner S (2005) Stimulus context modulates competition in human extrastriate cortex. Nat Neurosci 8:1110–1116. doi:10.1038/nn1501
De Ridder D, Verstraeten E, Van der Kelen K et al (2005) Transcranial magnetic stimulation for tinnitus: influence of tinnitus duration on stimulation parameter choice and maximal tinnitus suppression. Otol Neurotol 26:616–619
De Ridder D, van der Loo E, Van der Kelen K, Menovsky T, van de Heyning P, Moller A (2007a) Do tonic and burst TMS modulate the lemniscal and extralemniscal system differentially? Int J Med Sci 4:242–246
De Ridder D, van der Loo E, Van der Kelen K, Menovsky T, van de Heyning P, Moller A (2007b) Theta, alpha and beta burst transcranial magnetic stimulation: brain modulation in tinnitus. Int J Med Sci 4:237–241
Doesburg SM, Green JJ, McDonald JJ, Ward LM (2012) Theta modulation of inter-regional gamma synchronization during auditory attention control. Brain Res 1431:77–85. doi:10.1016/j.brainres.2011.11.005
Dosenbach NU, Fair DA, Miezin FM et al (2007) Distinct brain networks for adaptive and stable task control in humans. Proc Natl Acad Sci USA 104:11073–11078. doi:10.1073/pnas.0704320104
Dosenbach NU, Fair DA, Cohen AL, Schlaggar BL, Petersen SE (2008) A dual-networks architecture of top-down control. Trends Cogn Sci 12:99–105. doi:10.1016/j.tics.2008.01.001
Eichhammer P, Kleinjung T, Landgrebe M, Hajak G, Langguth B (2007) TMS for treatment of chronic tinnitus: neurobiological effects. Prog Brain Res 166:369–375. doi:10.1016/S0079-6123(07)66035-X
Hallam RS, McKenna L, Shurlock L (2004) Tinnitus impairs cognitive efficiency. Int J Audiol 43:218–226
Hayward G, Mehta MA, Harmer C, Spinks TJ, Grasby PM, Goodwin GM (2007) Exploring the physiological effects of double-cone coil TMS over the medial frontal cortex on the anterior cingulate cortex: an H2(15)O PET study. Eur J Neurosci 25:2224–2233. doi:10.1111/j.1460-9568.2007.05430.x
Hoffman HJ, Reed GW (2004) Epidemiology of tinnitus. In: Snow JB Jr (ed) Tinnitus, theory and management. BC Decker Inc, London, pp 16–41
Jastreboff PJ (1990) Phantom auditory perception (tinnitus): mechanisms of generation and perception. Neurosci Res 8:221–254
Kastner S, De Weerd P, Desimone R, Ungerleider LG (1998) Mechanisms of directed attention in the human extrastriate cortex as revealed by functional MRI. Science 282:108–111
Khedr EM, Rothwell JC, El-Atar A (2009) One-year follow up of patients with chronic tinnitus treated with left temporoparietal rTMS. Eur J Neurol 16:404–408. doi:10.1111/j.1468-1331.2008.02522.x
Kimbrell TA, Little JT, Dunn RT et al (1999) Frequency dependence of antidepressant response to left prefrontal repetitive transcranial magnetic stimulation (rTMS) as a function of baseline cerebral glucose metabolism. Biol Psychiatry 46:1603–1613
Kleinjung T, Eichhammer P, Langguth B et al (2005) Long-term effects of repetitive transcranial magnetic stimulation (rTMS) in patients with chronic tinnitus. Otolaryngol Head Neck Surg 132:566–569. doi:10.1016/j.otohns.2004.09.134
Langguth B, Zowe M, Landgrebe M et al (2006) Transcranial magnetic stimulation for the treatment of tinnitus: a new coil positioning method and first results. Brain Topogr 18:241–247. doi:10.1007/s10548-006-0002-1
May A, Hajak G, Ganssbauer S, Steffens T, Langguth B, Kleinjung T, Eichhammer P (2007) Structural brain alterations following 5 days of intervention: dynamic aspects of neuroplasticity. Cereb Cortex 17:205–210
Mevorach C, Hodsoll J, Allen H, Shalev L, Humphreys G (2010) Ignoring the elephant in the room: a neural circuit to downregulate salience. J Neurosci 30:6072–6079. doi:10.1523/JNEUROSCI.0241-10.2010
Salmi J, Rinne T, Koistinen S, Salonen O, Alho K (2009) Brain networks of bottom-up triggered and top-down controlled shifting of auditory attention. Brain Res 1286:155–164. doi:10.1016/j.brainres.2009.06.083
Schlee W, Hartmann T, Langguth B, Weisz N (2009) Abnormal resting-state cortical coupling in chronic tinnitus. BMC Neurosci 10:11. doi:10.1186/1471-2202-10-11
Searchfield GD, Morrison-Low J, Wise K (2007) Object identification and attention training for treating tinnitus. Prog Brain Res 166:441–460. doi:10.1016/S0079-6123(07)66043-9
Serences JT, Yantis S (2006) Selective visual attention and perceptual coherence. Trends Cogn Sci 10:38–45. doi:10.1016/j.tics.2005.11.008
Sparing R, Mottaghy FM (2008) Noninvasive brain stimulation with transcranial magnetic or direct current stimulation (TMS/tDCS)-From insights into human memory to therapy of its dysfunction. Methods 44:329–337. doi:10.1016/j.ymeth.2007.02.001
Speer AM, Kimbrell TA, Wassermann EM, Repella JD, Willis MW, Herscovitch P, Post RM (2000) Opposite effects of high and low frequency rTMS on regional brain activity in depressed patients. Biol Psychiatry 48:1133–1141
Stevens C, Walker G, Boyer M, Gallagher M (2007) Severe tinnitus and its effect on selective and divided attention. Int J Audiol 46:208–216. doi:10.1080/14992020601102329
Suppa A, Bologna M, Gilio F, Lorenzano C, Rothwell JC, Berardelli A (2008) Preconditioning repetitive transcranial magnetic stimulation of premotor cortex can reduce but not enhance short-term facilitation of primary motor cortex. J Neurophysiol 99:564–570. doi:10.1152/jn.00753.2007
Vanneste S, Plazier M, der Loo E, de Heyning PV, Congedo M, De Ridder D (2010a) The neural correlates of tinnitus-related distress. Neuroimage 52:470–480. doi:10.1016/j.neuroimage.2010.04.029
Vanneste S, Plazier M, Van de Heyning P, De Ridder D (2010b) Transcutaneous electrical nerve stimulation (TENS) of upper cervical nerve (C2) for the treatment of somatic tinnitus. Exp Brain Res 204:283–287. doi:10.1007/s00221-010-2304-5
Vanneste S, Plazier M, van der Loo E, Ost J, Van de Heyning P, De Ridder D (2010c) Burst transcranial magnetic stimulation: which tinnitus characteristics influence the amount of transient tinnitus suppression? Eur J Neurol. doi:10.1111/j.1468-1331.2010.02987.x
Vanneste S, Langguth B, De Ridder D (2011a) Do tDCS and TMS influence tinnitus transiently via a direct cortical and indirect somatosensory modulating effect? A combined TMS-tDCS and TENS study. Brain Stimul 4:242–252. doi:10.1016/j.brs.2010.12.001
Vanneste S, Plazier M, Van de Heyning P, De Ridder D (2011b) Repetitive transcranial magnetic stimulation frequency dependent tinnitus improvement by double cone coil prefrontal stimulation. J Neurol Neurosurg Psychiatry 82:1160–1164. doi:10.1136/jnnp.2010.213959
Vanneste S, Plazier M, Van de Heyning P, De Ridder D (2011c) Repetitive transcranial magnetic stimulation frequency dependent tinnitus improvement by double cone coil prefrontal stimulation. J Neurol Neurosurg Psychiatry. doi:10.1136/jnnp.2010.213959
Watkins S, Dalton P, Lavie N, Rees G (2007) Brain mechanisms mediating auditory attentional capture in humans. Cereb Cortex 17:1694–1700. doi:10.1093/cercor/bhl080
Zenner HP, Zalaman IM (2004) Cognitive tinnitus sensitization: behavioral and neurophysiological aspects of tinnitus centralization. Acta Otolaryngol 124:436–439
Acknowledgments
The authors thank Ana Belen Elgoyhen for the suggestion that the IPS might be involved in attentional processes in tinnitus. The authors also thank Jan Ost, Bram Van Achteren, Bjorn Devree, and Pieter van Looy for their help in preparing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vanneste, S., van der Loo, E., Plazier, M. et al. Parietal double-cone coil stimulation in tinnitus. Exp Brain Res 221, 337–343 (2012). https://doi.org/10.1007/s00221-012-3176-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-012-3176-7