Abstract
We studied spatial orientation before and after 21 days of 6° head-down bed rest in 15 subjects. During bed rest, 8 subjects were treated daily with 1 h Gz centrifugation (artificial gravity) (2.5 g at the feet; 1.0 g at the heart), with 7 subjects serving as controls. Ocular counter-rolling and subjective visual vertical were assessed during 90° whole body roll tilt to the left and right. Ocular counter-rolling was unaffected by bed rest and bed rest + artificial gravity. Performance on the subjective visual vertical task was unchanged in the control group, but exhibited a significant increase in error for 48 h after bed rest in the treatment (artificial gravity) group. Intermittent application of linear acceleration along the long body axis may have increased the weighting of the idiotropic vector, resulting in an increased bias of the subjective visual vertical toward the long body axis during 90° roll tilt.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Exposure to microgravity adversely affects bone, muscle, cardiovascular, and sensorimotor function. Up to 9% of bone mineral is lost on flights of 4–6 months duration (Sibonga et al. 2007); decrements in skeletal muscle performance and morphological changes occur on flights as short as 5 days (Greenisen et al. 1999); cardiovascular effects range from post-flight orthostatic tachycardia to cardiac rhythm disturbances during extra-vehicular activities (EVA) (Charles et al. 1999); and post-flight sensorimotor dysfunction impairs gait (Bloomberg et al. 1999), gaze (Moore et al. 2001, 2005), and pilot performance (Moore et al. 2008). Artificial gravity (AG) is a potential countermeasure to bone, muscle, and cardiovascular deconditioning. Two basic approaches have been proposed: a large radius, low-angular velocity rotation of the spacecraft (von Braun 1952) and small radius, high angular velocity intermittent rotation on a centrifuge. Both techniques generate linear (centripetal) acceleration in the radial direction to replicate the gravitational load experienced on Earth.
We participated in a multi-system investigation into the efficacy of one particular intermittent AG prescription in mitigating bone, muscle, and cardiovascular deconditioning associated with 21 days of 6° head-down bed rest. Bed rest has been used extensively to simulate aspects of the physiological deconditioning associated with spaceflight (Pavy-Le Traon et al. 2007), reducing mechanical loading along the long-body axis, eliminating the need for coordinated contractions of the anti-gravity muscles, and causing cephalad fluid shifts and relative hypovolemia. Bed rest is effective at simulating (at least qualitatively) the deconditioning effects of spaceflight on bone, muscle, and cardiovascular system function. The primary aim of our portion of the study was to evaluate whether the intermittent AG protocol had any adverse effects on central processing of spatial orientation. The unusual gravito-inertial stimuli presented by this high-angular velocity (~30 rpm), high G-gradient (2.5 g at the feet; 1.0 g at the heart) countermeasure paradigm, with its attendant potential for Coriolis and cross-coupled stimuli, may have untoward effects on sensorimotor function. An ancillary aim was to objectively assess the effects of bed rest on spatial orientation. Presumably, the vestibular system is well adapted to a condition it experiences approximately 8 h each day, so head-down bed rest has not been considered a realistic analog of vestibular adaptation to microgravity exposure.
We utilized two measures of spatial orientation: ocular counter-rolling (OCR) and perception of the subjective visual vertical (SVV). OCR, an otolith-ocular reflex that generates rotation about the line of sight toward the gravitational vertical when the head tilts laterally, provides a direct measure of otolith function (Diamond and Markham 1983). OCR responses are sustained during static roll head tilts with a gain of approximately 0.1, which is reduced by 30–50% in a number of astronauts tested following spaceflight (Young and Sinha 1998; Clarke and Kornilova 2007). We found no change in OCR gain in response to in-flight and post-flight centrifugation on a short duration (17 days) shuttle mission, but one subject developed a marked asymmetry in OCR response to leftward and rightward gravito-inertial acceleration (GIA) tilts (Moore et al. 2001) as previously observed post-flight (Young and Sinha 1998), possibly due to unmasking of an inherent asymmetry in afferent otolith information in microgravity (von Baumgarten and Thumler 1979). Perception of the body vertical also changes during spaceflight (Clement et al. 2001). SVV is a measure of the ability to judge the spatial vertical that depends on input from the visual, vestibular, and somatosensory systems (see (Howard 1982) for an extensive review), used clinically to assess lesions of the CNS and vestibular function. Healthy subjects can typically set a luminous line to Earth-vertical with a standard deviation of 1.1° when upright in an otherwise dark environment (Kingma 2006). As the body is tilted in roll beyond 60°, large systematic errors in SVV develop toward the long-body axis. This Aubert- or A-effect (Aubert 1861), which has been modeled using an estimate of tilt from the otoliths combined with an internal signal representing the long-body axis (idiotropic) vector (Mittelstaedt 1983), causes a bias of the percept of verticality toward the long-body axis at large roll tilts.
In the current study, we tested the hypothesis that bed rest adapted subjects treated with an intermittent AG prescription (N = 8) would exhibit no significant differences in spatial orientation function when compared to control subjects (N = 7) receiving no countermeasure. An ancillary hypothesis, that head-down bed rest does not affect spatial orientation, was also assessed.
Materials and methods
Subjects
Fifteen male subjects (age: 26–38 years, height: 172–189 cm, weight: 67–95 kg) participated in this study, which was performed at the General Clinical Research Center (GCRC) at the University of Texas Medical Branch (UTMB) in Galveston, TX. The protocol was approved in advance by the Johnson Space Center Committee for the Protection of Human Subjects, the UTMB Institutional Review Board and GCRC Advisory Committee, and the Mount Sinai School of Medicine Institutional Review Board. Each subject provided written informed consent before being enrolled in the study.
Subject screening
All subjects were required to have normal vestibular function, similar to that of the US astronaut corps. Each passed a clinical vestibular examination and scored within the normal range (5th–95th percentile) of astronaut performance on a standard battery of computerized dynamic posturography sensory organization tests of balance control (Paloski et al. 1999). Subjects were also screened for motion sickness susceptibility (Golding 1998) to eliminate potential recruits with a high sensitivity to Coriolis and cross-coupled stimuli during rotation. Prior to enrollment, all subjects demonstrated centrifuge tolerance by completing a 90-min spin under the planned study conditions. Subjects who passed the screening tests were assigned randomly to either the control group or the treatment (centrifugation) group.
Study schedule
Subjects remained ambulatory for the first 11 days of the study, during which they acclimated physiologically and psychologically to the GCRC bed rest facility, the study diet regimen, and the circadian cycle regulation. Two pre-bed rest test sessions (~10 and 3 days before bed rest) were scheduled for each subject during this phase to establish a baseline for OCR and SVV performance. Subjects began the 21-day bed rest phase on the 12th day of the study, throughout which they were confined to strict 6° head-down bed rest. Test subject monitors (one for every two bed rest subjects) were present 24/7 to ensure compliance with standard experimental conditions, and each subject was continuously observed by remote video cameras. All subjects were transported daily to the centrifuge, where the treatment group, but not the control group, received 1-h AG exposures. Following the bed rest phase, subjects began an 8-day recovery phase during which they remained in the bed rest facility but returned to ambulation. Each subject completed five post-bed rest (BR) test sessions beginning on the first day of return to ambulation (BR+0) and 1, 2, 4, and 8 days thereafter (BR+1, BR+2, BR+4 and BR+8).
Centrifuge protocol
Each subject was transferred to the centrifuge facility daily by a short (5–10 min), 6° head-down gurney ride. After the placement of electrodes for physiological monitoring, the subject was transferred to the centrifuge and secured to the subject station in the supine position (6° head-down) using a 5-point harness system. The subject was oriented radially (feet out) with the feet placed against a support surface containing a force plate for monitoring ‘ground’ reaction forces. After verifying physiological signals and safety controls, the 1-h centrifugation period began for the treatment subjects. Control subjects were placed on the centrifuge for 1 h in the same manner as for treatment subjects but without rotation. Loading was standardized for treatment subjects of varying body heights by adjusting the radial distance of the feet support surface from the center of rotation (218–229 cm) and the angular velocity of the centrifuge arm (30.7–32.1 rpm) to achieve long-body axis loading of 2.5 g at the feet and 1.0 g at the (estimated) level of the heart (approximately 0.6 g at the level of the otolith organs). Angular accelerations during spin-up and spin-down were limited to <5°/s2 to minimize potential motion sickness symptoms.
The padded subject station extended from above the subject’s head to just below the hips and was designed to glide freely in the radial direction over a range of 10 cm on a set of low-friction bearings. This ensured that the full AG load would be borne by the subjects’ feet and legs, and it allowed the subjects to perform anti-orthostatic maneuvers (ad lib. heel raises and shallow knee bends) while spinning. A counterweight system minimized (<4 kg) the loading added to the subject by the moving components of the subject station.
Subjects were centrifuged with the room lights switched off. A centrifuge-mounted overhead light was used to illuminate the subject’s face for medical monitoring purposes, and the subjects watched videos on a monitor fixed approximately 1 m above their faces throughout each spin. Head movements about any axis were found to be provocative in preliminary evaluations, and subjects were instructed to minimize head movements during rotation.
Spatial orientation evaluation
OCR was determined from images of the left eye acquired at a rate of 30 Hz by a digital firewire video camera mounted on lightweight swimming goggles (MacDougall and Moore 2005). Baseline torsional eye position was obtained from 10 s of video data acquired while subjects sat upright on a bed in a lighted room while visually fixating an imaginary point on a blank wall approximately 3 m distant. Subjects then lay on their right side (right ear down; RED). After a period of 60 s (to allow semicircular canal activity to diminish), 10 s of video data were acquired as subjects again fixated an imaginary target. This process was then repeated with subjects lying on their left side (left ear down; LED). Torsional eye position was calculated from the digital video records using polar cross-correlation to compute the relative rotation about the line of sight between sequential images (Moore et al. 1996). OCR was characterized by the amount of ocular torsion in the RED or LED position relative to upright. Following the right-hand rule, clockwise roll motions of the body or eyes (from the subject’s point of view) were considered positive (e.g., the RED position was designated +90°, and the counter-clockwise rotation of the eye back toward the spatial vertical [from the subject’s point of view] was negative in sign).
SVV was measured following removal of the video goggles. Subjects were placed within a shroud that eliminated ambient light and asked to adjust the orientation of a luminous line displayed on a laptop computer screen visible through a circular cut-out in the shroud (to minimize orientation cues). Baseline measures were acquired while seated on a bed with the head in the upright position; subjects set the luminous line to the perceived vertical from start positions randomly offset (up to 15°) either side of Earth-vertical. The angular orientation of the luminous line was controlled using a three-button mouse held by the subject. The left button rotated the luminous line counter-clockwise, the right rotated it clockwise, and the center button was used to indicate when the subject perceived that the line was oriented vertically. Ten measures were acquired in the upright position. SVV measures (10) were then obtained with the subject lying in the RED position (after allowing 60 s for semicircular canal activity to diminish) and again with the subject lying in the LED position.
Results
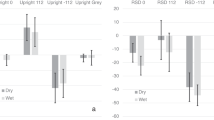
The magnitude and symmetry of the OCR response to ±90° roll body tilts (RED/LED) were unchanged by bed rest alone (Fig. 1a) or bed rest with intermittent AG (Fig. 1b). There was no effect of test day on OCR magnitude in either the control group (Fig. 1a) (ANOVA; LED P = 0.47; RED P = 0.63) or the treatment group (Fig. 1b) (LED P = 0.99; RED P = 0.93). Pre-bed rest OCR magnitude (median and semi-interquartile range of two pre-BR test sessions) for control subjects (N = 6; video images from one subject were unable to be processed due to an excessively droopy eyelid) were 5.5° (1.5) in the LED position and −6.3° (1.0) in the RED position; post-bed rest values (median and semi-interquartile range of bed rest + 0, 1, 2, 4, 8 days) were LED 4.5° (1.4) and RED −6.6° (1.4). Although there was an apparent increase in OCR on the last day of testing (BR+8 days; Fig. 1a) this was not significant when compared to the previous (BR+4 days) data point (Wilcoxon Signed Rank Test; LED P = 0.44; RED P = 0.15). Similarly, median pre-bed rest OCR (4.8° [1.2] LED; −5.8° [1.5] RED) did not differ significantly from post-bed rest (5.2° [1.4] LED; −6.3° [0.6] RED) for the treatment subjects (N = 8).
Ocular counter-rolling (OCR) pre- and post-bed rest (median and semi quartile range) during 90° roll-body tilts to the left (LED) and right (RED). a Control group (N = 6). b Treatment (centrifuged) group (N = 8). OCR was not affected by bed rest alone or bed rest + AG. Subjective visual vertical (SVV) error relative to pre-bed rest baseline when upright and during LED and RED body tilts. c Control group (N = 7). d Treatment group (N = 8). SVV was unaffected by bed rest alone, but subjects in the treatment group exhibited a significant post-bed rest increase in SVV error relative to pre-bed rest baseline during roll tilt that persisted for 48 h after resuming ambulation
There was a baseline disparity in performance on the SVV task between the control (N = 7) and treatment (N = 8) groups. Pre-bed rest error (median and semiquartile range) when setting the bar to the visual vertical in the LED position was −15.6° (4.1) for controls and −8.4° (4.2) for treatment subjects (Wilcoxon Signed Rank Test; P < 0.001); when RED 12.3° (6.3) for controls and 4.3° (3.1) for the treatment group (Wilcoxon Signed Rank Test; P < 0.001). There was no significant difference in SVV error when upright (controls −0.8° [0.9]; treatment −1.8° [1.0]). Due to this performance difference between groups, each subject served as their own control, and the difference in SVV error post-bed rest was calculated relative to each subject’s own pre-bed rest baseline (Fig. 1c, d). Day of testing had no effect on the relative SVV error for the control group (ANOVA; LED P = 0.10; RED P = 0.43) (Fig. 1c), but there was a significant effect for the treatment group. SVV error increased toward the body vertical during roll tilt for up to 48 h after bed rest in subjects receiving AG treatment (Fig. 1d). When RED, SVV error (median and semiquartile range) increased significantly relative to pre-bed rest 24 h after return to ambulation (Wilcoxon Signed Rank Test; BR+0: +9.2° [4.9] P < 0.001) was still higher (but not significantly so) on BR+1 (+1.7° [2.4] P = 0.31), recovering to baseline on BR+2 (+0.9° [1.9] P = NS). Similarly, SVV error when LED significantly increased relative to baseline on BR+0 (−1.7° [4.0] P = 0.04) and BR+1 (−7.6° [3.9] P < 0.001), recovering by R+2 (+0.6° [3.1] P = NS).
Discussion
In this centrifuge and bed rest study, we found that 21 days of 6˚ head-down bed rest had no effect on spatial orientation as assessed by ocular counter-rolling and the subjective visual vertical. Application of the daily 1 h rotational AG prescription to bed rested subjects (treatment group) had no significant effects on ocular counter-rolling, but caused a transient impairment in the perception of the visual vertical for 48 h after bed rest.
Despite the frequent use of head-down bed rest as a model for spaceflight deconditioning, little is known about the vestibular effects of long duration partial unloading of the otolith organs due to the 6° downward pitch of the head. Our finding that OCR was unchanged by bed rest alone suggests that head-down bed rest does not affect otolith sensitivity or symmetry to tilts of the GIA vector as observed in some astronauts following spaceflight. Our finding that OCR was also unchanged by the intermittent AG prescription suggests no untoward affects of intermittent Gz stimulation on otolith sensitivity.
Subjective visual vertical was used in the current study as an integrated measure of the effects of bed rest and centrifugation on the perception of the spatial vertical. We found that SVV was unchanged by 21 days of 6° head-down bed rest. This is in contrast to a Soviet-era study (Yakovleva et al. 1976) reporting an increase in SVV error of up to 15° immediately after 30 days 6° head-down bed rest that did not return to baseline over 16 days of post-bed rest testing. However, the latter result must be interpreted with caution, as no details were provided for the SVV procedure, number of subjects tested or variance of the SVV measures, and no statistical testing was performed.
SVV error increased after bed rest in the treatment group, who received intermittent centrifugation during the bed rest period. A possible explanation is that periodic application of linear acceleration increased weighting of the idiotropic vector (Mittelstaedt 1983), increasing the bias (A-effect) toward the body vertical when tilted laterally. There was some evidence for this hypothesis from body pitch perception during the centrifuge runs (Jarchow and Young 2009). Perceived head-up tilt was essentially veridical at 30° (corresponding to the 31° tilt of the GIA at the level of the otoliths due to the 0.6 g imparted by the centrifuge) during the tolerance runs prior to entering the study. Over the first week of bed rest, there was a small (~5°) decrease in perceived pitch orientation during centrifugation (Jarchow and Young 2009), consistent with the hypothesis of an increased weighting of the body vertical. Our perception studies aboard the STS-90 (Neurolab) Spacelab mission found that the idiotropic vector was more heavily weighted during the first week of weightlessness than on Earth in astronauts exposed to intermittent in-flight centrifugation (Clement et al. 2001). The question remains of whether this adaptation is due to a unique combination of bed rest (or spaceflight) + centrifugation or due to centrifugation alone. That is, does unloading of the otoliths, either partial (bed rest) or near total (microgravity), render the idiotropic vector more amenable to adaptation? There is some evidence that centrifugation alone can induce adaptation; prolonged (90 min) 3Gx centrifugation (3 g linear acceleration parallel with the naso-occipital axis when supine) impaired subjective estimates of the body vertical for 2–3 min post-rotation (Bles and De Graaf 1993) (although motion sickness and postural effects lasted up to 6 h in some individuals (Bles and De Graaf 1993; De Graaf and De Roo 1996)). However, in the current study, perception of the subjective vertical was impaired more than 48 h after the final centrifuge run.
The control group exhibited a larger median baseline error in SVV (by approximately 8°) relative to the treatment group in both the LED and RED orientations. Yakovleva et al. (1976) reported a similar disparity (8°) between subject groups with mean error ranging from 8° to 16°. This may reflect a high inter-subject variability in SVV error at large roll tilt angles in the population at large (as opposed to the finely tuned response in the upright position (Kingma 2006)), resulting in significant differences when sampling small groups. However, the SVV error in the current study demonstrated consistency within each group across the 39 days of testing. Median LED and RED SVV error for both control and treatment groups on day 39 (BR+8 days) was within 2° of the first test session (10 days pre-bed rest).
The results of this study suggest that 6° head-down bed rest is not an effective analog of vestibular deconditioning during spaceflight, and that AG generated by intermittent centrifugation can produce undesirable effects on perception of the spatial vertical. The functional impact (if any) of the observed decrement in the SVV response is unknown, and further investigation is warranted to determine possible side effects of long-term artificial gravity on spatial orientation and operator proficiency.
References
Aubert H (1861) Eine scheinbare Drehung von Objekten bei Neigung des Kopfes nach rechts oder links. Virchows Archiven 20:381–393
Bles W, De Graaf B (1993) Postural consequences of long duration centrifugation. J Vest Res 3:87–95
Bloomberg JJ, Layne CS, McDonald PV, Peters BT, Huebner WP, Reschke MF, Berthoz A, Glasauer S, Newman D, Jackson DK (1999) Effects of spaceflight on locomotor control. In: Sawin CF (ed) Extended duration orbiter medical project, NASA/SP 1999–534. NASA Johnson Space Center, Houston
Charles J, Fritsch-Yelle J, Whitson P, Wood M, Brown T, Fortner G (1999) Cardiovascular deconditioning. In: Sawin C, Taylor G, Smith W (eds) Extended duration orbiter medical project, NASA/SP 1999-534. NASA Johnson Space Center, Houston, pp 1.1–1.18
Clarke AH, Kornilova L (2007) Ocular torsion response to active head-roll movement under one-g and zero-g conditions. J Vestib Res 17:99–111
Clement G, Moore ST, Raphan T, Cohen B (2001) Perception of tilt (somatogravic illusion) in response to sustained linear acceleration during spaceflight. Exp Brain Res 138:410–418
De Graaf B, De Roo AJ (1996) Effects of long duration centrifugation on head movements and a psychomotor task. J Vestib Res 6:23–29
Diamond SG, Markham CH (1983) Ocular counter rolling as an indicator of vestibular otolith function. Neurology 33:1460–1469
Golding JF (1998) Motion sickness susceptibility questionnaire revised and its relationship to other forms of sickness. Brain Res Bull 47:507–516
Greenisen MC, Hayes J, Siconolfi S, Moore A (1999) Functional performance evaluation. In: Sawin C, Taylor G, Smith W (eds) Extended duration orbiter medical project, NASA/SP 1999-534. NASA Johnson Space Center, Houston, pp 3.1–3.24
Howard IP (1982) Human visual orientation. Wiley, New York
Jarchow T, Young L (2009) Neurovestibular effects of bed rest and centrifugation In: Strategic planning activity on aerospace medical and human factors challenges and celebration honoring Dr. Charles M. Oman, Director of the MVL on this 65th Birthday, Massachusetts Institute of Technology, Cambridge MA. http://mvl.mit.edu/MVLpubs/MVL_09.16_JarchowYoung.pdf
Kingma H (2006) Function tests of the otolith or statolith system. Curr Opin Neurol 19:21–25
MacDougall HG, Moore ST (2005) Functional assessment of head-eye coordination during vehicle operation. Optom Vis Sci 82:706–715
Mittelstaedt H (1983) A new solution to the problem of the subjective vertical. Naturwissenschaften 70:272–281
Moore ST, Haslwanter T, Curthoys IS, Smith ST (1996) A geometric basis for measurement of three-dimensional eye position using image processing. Vision Res 36:445–459
Moore ST, Clement G, Raphan T, Cohen B (2001) Ocular counter rolling induced by centrifugation during orbital spaceflight. Exp Brain Res 137:323–335
Moore ST, Cohen B, Raphan T, Berthoz A, Clement G (2005) Spatial orientation of optokinetic nystagmus and ocular pursuit during orbital spaceflight. Exp Brain Res 160:38–59
Moore ST, MacDougall HG, Lesceu X, Speyer JJ, Wuyts F, Clark JB (2008) Head-eye coordination during simulated orbiter landing. Aviat Space Environ Med 79:888–898
Paloski WH, Reschke MF, Black FO (1999) Recovery of postural equilibrium control following spaceflight (DSO 605). In: Sawin CF, Taylor GR, Smith WL (eds) Extended duration orbiter medical project final report 1989–1995 (NASA/SP-1999-534). NASA, Houston, pp 5.4: 1–16
Pavy-Le Traon A, Heer M, Narici MV, Rittweger J, Vernikos J (2007) From space to earth: advances in human physiology from 20 years of bed rest studies (1986–2006). Eur J Appl Physiol 101:143–194
Sibonga JD, Evans HJ, Sung HG, Spector ER, Lang TF, Oganov VS, Bakulin AV, Shackelford LC, LeBlanc AD (2007) Recovery of spaceflight-induced bone loss: bone mineral density after long-duration missions as fitted with an exponential function. Bone 41:973–978
von Baumgarten RJ, Thumler R (1979) A model for vestibular function in altered gravitational states. Life Sci Space Res 17:161–170
von Braun W (1952) Crossing the last frontier. In: Collier’s, vol 129(12), p 24
Yakovleva I, Bokhov B, Kornilova L (1976) Study of space perception functioning during simulation of certain space flight factors. Life Sci Space Res 14:295–300
Young LR, Sinha P (1998) Spaceflight influences on ocular counter rolling and other neurovestibular reactions. Otolaryngol Head Neck Surg 118:S31–S34
Acknowledgments
The successful implementation of our spatial orientation test paradigm would not have been possible without the careful oversight and suggestions provided by the review committees, the subjects who persisted throughout the bed rest, and the support and assistance provided by the staff of the JSC Flight Analogs Project and UTMB GCRC, and the Neurosciences Laboratory at JSC. This project was supported by the NASA Human Research Program (WHP) and NASA grants NNJ04HD66G, and NNJ04HF51G (STM). The study was conducted at the NIH-funded (M01 RR 0073) GCRC at the University of Texas Medical Branch, Galveston, TX.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moore, S.T., MacDougall, H.G. & Paloski, W.H. Effects of head-down bed rest and artificial gravity on spatial orientation. Exp Brain Res 204, 617–622 (2010). https://doi.org/10.1007/s00221-010-2317-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-010-2317-0