Abstract
Left unilateral neglect is frequently reported after right hemispheric lesions of the middle cerebral artery (MCA) damaging the parietal–frontal cortical–subcortical network subserving space representation and awareness. However, accumulating evidence shows that neglect can also follow lesions of the posterior cerebral artery (PCA) that do not directly affect this parietal–frontal network. Surgical studies in the monkeys have demonstrated that complete callosal resection combined with lesion of the right optic tract entirely deprives the right hemisphere of visual inputs from the left hemispace provoking severe left unilateral neglect. Here, through the detailed study of two patients we show, for the first time, that PCA lesions selectively affecting the splenium of the corpus callosum and the adjacent right primary visual cortex provoke severe neglect selectively restricted to the visual domain. No trace of personal, motor or representational-imagery neglect was found. Also at variance with previous case studies in which neglect followed lesion of the trunk or the genu of the corpus callosum, no restriction of neglect to tasks performed with the right hand, no left hemispatial limb akinesia, no tactile extinction for the left hand and no tactile anomia for stimuli explored with the left hand were observed. These findings demonstrate that brain lesions depriving intact parietal and frontal attentional areas from specific sensory inputs can yield spatial neglect limited to specific sensory modalities or sectors of space.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spatial neglect is a clinically multifaceted invalidating syndrome, most frequently suffered by patients with right brain damage (Doricchi et al. 2008). It is characterised by the fundamental inability of orienting attention or taking into consideration events in the contralesional left side of extrapersonal or personal-body space. In some cases, a difficulty in conjuring up the left side of mental images can be present (Bisiach and Luzzatti 1978), and this can occur independently of other neglect symptoms (Guariglia et al. 1993). Originally and still traditionally considered a “parietal sign” (Critchley 1953), spatial neglect most frequently results from cortical–subcortical lesions in the territory of the middle cerebral artery area (MCA) and also from lesion affecting the basal ganglia (see for review Bartolomeo et al. 2007; Doricchi et al. 2008). These lesions disrupt the integrated functioning of parietal–frontal networks subserving space representation and awareness in the right hemisphere. Recent anatomical, surgical and brain imaging evidences (Doricchi and Tomaiuolo 2003; Thiebaut de Schotten et al. 2005; He et al. 2007; Shinoura et al. 2009; Verdon et al. 2009) have revived the proposal that damage of white matter fibre bundles connecting the parietal to the frontal lobe is a relevant pathophysiological component of the neglect syndrome (Critchley 1953; Geschwind 1965a, b; Gaffan and Hornak 1997; Leibovitch et al. 1998).
Interestingly, a number of studies have demonstrated that spatial neglect can also result from lesions in the posterior cerebral artery area (PCA; Park et al. 2006; Bird et al. 2006). Since this type of lesion largely or entirely spares parietal and frontal attentional areas, specific pathophysiological mechanisms were proposed to explain neglect in these cases. In particular, surgical lesion studies in monkeys demonstrated that callosal damage combined with lesions producing homonymous hemianopia can engender severe spatial neglect for the blind hemispace. In a seminal investigation in the monkey, Gaffan and Hornak (1997) found that the most severe form of neglect was indeed produced by unilateral resection of the optic tract (causing complete contralateral hemianopia) combined with complete callosal commisurotomy. These authors argued that in this case “the blind hemisphere is not only deprived of information arriving from the contralateral field but it is also cut off from information arriving from the ipsilateral spared visual field, and therefore cannot build a memory-based representation of the currently contralateral visible world”. Clinical–anatomical investigations have spotted functionally equivalent pathophysiological mechanisms in patients with PCA (Park et al. 2006; Bird et al. 2006). These studies showed that PCA strokes causing splenial-callosal lesion and concomitant unilateral damage of the adjacent striate cortex provoke severe contralesional neglect accompanied by hemianopia. Following the suggestion proposed by Gaffan and Hornak (1997), it could be concluded that a right brain damaged patient suffering this type of lesion might still acquire visual information from the left portion of visual space by rotating the eyes leftward and inspecting this space with the seeing right visual field: however, due to callosal lesion, acquired visual input would remain segregated in the left hemisphere without reaching the right hemisphere parietal–frontal networks specialised for space awareness, thus causing left unilateral neglect. In the absence of callosal lesion, only contralateral hemianopia, without neglect, should be observed.
Based on the same interpretation, it could be further argued that impaired interhemispheric transfer in patients with PCA lesion might selectively or predominantly affect visual information, since PCA lesions might selectively or predominantly affect the posterior sector of the corpus callosum, i.e. the splenium. Importantly, this would imply that in these cases one should observe a dissociation between the presence of contralesional visual neglect and the absence of motor and personal-body neglect, as well as the absence of symptoms as hemispatial limb akinesia, contralesional tactile extinction or contralesional tactile anomia, that can be caused or exacerbated by callosal disconnection. This is because splenial disconnection would leave the interhemispheric transfer of somatosensory and motor information in more anterior sectors of the corpus callosum (see for review, Caminiti et al. 2009) entirely spared. Through the study of two patients with PCA suffering selective splenial damage here, we demonstrate that this is the case, thus expanding on the original suggestions by Gaffan and Hornak (1997).
Patients and methods
Patient 1
MP is a right-handed 76-year-old housewife. She was admitted to the rehabilitation hospital (Auxilium Vitae, Volterra) twenty-five days after a right hemisphere ischaemia induced by embolic stroke. On clinical examination, she showed left-sided weakness, left hemiparesis and left hemianopia. She was disoriented in time though she was oriented in space.
Two months after the stroke, she entirely recovered motor function in the left hand and was able to walk with a tripod. She also recovered from temporal disorientation. Humphreys visual field testing revealed complete (i.e. no macular sparing) left homonymous hemianopia. The patient complained for her visual disabilities, even though she was unaware of her severe left spatial neglect. Detailed neuropsychological assessment of verbal abilities, including sentence comprehension, naming, reading, writing, phonologic and semantic verbal fluency tasks, did not show signs of language impairments. The patient had normal short-term verbal memory (digit-span: raw score = 5, cut off <4; Orsini et al. 1987) and short-term spatial memory skills (Corsi-span: raw score = 4, cut off <3; Orsini et al. 1987).
Preliminary clinical testing revealed clear signs of left spatial neglect. When requested to draw a daisy, the patient sketched only the right side of it. She omitted reading or misread parts of the text on the left side of newspapers pages (i.e. spatial dyslexia) and showed a strong tendency to write only on the right side of the paper sheet (i.e. spatial dysgraphia). No personal-body neglect was observed when the patient was asked to simulate simple activities (Zoccolotti and Judica 1991) such as combing her hair, powdering her face or wearing glasses. The patient was also able to indicate on verbal command all parts of the contralesional side of her own body, both in free vision and in blindfolded. There was no tactile extinction for stimuli on the left hand and no tactile anomia for both hands (18/20). The patient could readily move the eyes to both lateral sides on verbal command.
Patient 2
MB is a right-handed 81-year-old retired clerk. Forty days before admittance in the rehabilitation hospital (Auxilium Vitae, Volterra), he had suffered a right hemisphere haemorrhage. Surgical evacuation of the blood clot was performed 15 days after the stroke. Clinical examination on admittance revealed left-sided weakness, left hemiparesis and left homonymous hemianopia. He was confused and bradipsychic.
At the moment of neuropsychological investigation, 4 month after stoke, he had entirely recovered from the motor impairments and was able to walk and perform daily activities autonomously. He also recovered from mental confusion and bradypsychism. Goldman perimetric testing revealed complete left homonymous hemianopia. The patient complained for visual disabilities and for frequently bumping on obstacles on the left. Standard neuropsychological assessment of verbal comprehension, naming, reading, writing, phonologic and semantic verbal fluency did not reveal impairments. The patient had normal short-term verbal memory (forward digit-span: raw score = 4, cut off <4; Orsini et al. 1987) and short-term spatial memory (Corsi-span: raw score = 5, cut off ≤3; Orsini et al. 1987).
On preliminary clinical testing, the patient showed clear left-side neglect in the spontaneous drawing of a daisy. He also showed left spatial dyslexia and left spatial dysgraphia. His relatives reported that he usually left food on the left side of his plate and that they were obliged to turn the dish by 180° to allow the patient to finish his meal. This was also observed by two of the authors (FT and FD) while the patient was having his breakfast at the hospital’s restaurant. By contrast, when donning his coat, the patient always started by the left sleeve, thus showing good allocation of attention to the left side of his own body. Absence of personal-body neglect was also observed when the patient was asked to simulate simple activities (Zoccolotti and Judica 1991) as combing his hair, shaving his face or wearing his glasses (see video recording in supplemental data material; file name: TomaiuoloDoricchi-Pat2-CombRazorTest.mp4). Upon verbal command, the patient readily indicated all parts of the contralesional side of his own body, both in free vision and in blindfolded. When asked to recognise objects by touch, his performance was well above chance level and equivalent across hands (16/20). No tactile extinction for stimuli delivered to the contralesional left hand was found. The patient could readily move his eyes to both lateral sides on verbal command.
Methods
Perceptual-visual neglect
Visual neglect for the peripersonal space was assessed through: (a) the Line Bisection Task (line length 2 and 200 cm; five trials per line length). Patient 1 performed the task with the right hand whereas Patient 2 both with the right and the left hand; (b) the Line Cancellation task (Albert 1973) performed with the right hand); (c) the Letter Cancellation task (Diller et al. 1974) performed with the right hand.
Visual neglect for the extrapersonal space was assessed by asking patients to indicate and name pictures attached to the walls of a testing room (3 m × 3 m.). Patients sat close to the centre of one wall. One picture was attached on the front wall, five on the wall on the patient’s left side and five on the wall on the right side.
Personal-body neglect
Neglect for personal-body space was assessed through the Fluff Test (Beschin and Robertson 1997; Cocchini et al. 2001). The test was administered twice, in separate sessions, once in blindfolded condition and once in free vision. In this, test patients are required to reach and remove with the ipsilesional right-hand 15 targets (i.e. 2 × 4 cm paper strips) attached to their body. Three targets are attached to the right side and three to the left side of the torso (with respect to the sagittal body-midline). Three targets are attached to the right leg, three to the left leg and three to the left arm. No target is attached on the right arm used for performing the task.
Representational-topographical neglect
Neglect for the representational space was tested by asking patients to mentally visualise a familiar square from their hometown and describe the square from two directionally opposing viewpoints (by 180°). Topographical descriptions and picture-maps provided by healthy relatives living in the same hometown were taken for comparison with patient’s description.
Neuroanatomical investigation
For each patient, an MRI scan of the brain was obtained 4 months past stroke onset. The T2-weighted images were produced with a Siemens Magnetom Simphony 1.5 T MR system. Mapping of brain lesions was performed using DISPLAY, (J.D. McDonald, Brain Imaging Center, Montreal Neurological tute www.bic.mni.mcgill.ca/software/Display/Display.html). This program allows labelling of voxel regions on each slice of the MRI volume and allows a simultaneous visualisation of the movement of the cursor on the screen within the sagittal, axial and coronal planes of the MRI. The simultaneous 3D view of the MRI planes allows an unambiguous identification of lesioned area and of its anatomical boundaries. Once the lesion was delimited, the sulcal patterns were identified using the Economo and Koskinas sulci and gyri map (1925) and the neuroanatomical atlas of Duvernoy (1991). A similar procedure has been used in a previous study (Tomaiuolo et al. 2001).
Patients gave their informed consent prior to their inclusion in the study.
Results
Results from the tests for the assessment of Visual neglect for peripersonal space, Visual neglect for extrapersonal space, Neglect for personal-body space and Neglect for Representational-topographical space are summarised in Table 1. Cut-off scores for the different tests (when available) are reported in the corresponding legend.
Patient 1 (P1)
Behavioural investigation
MP (P1) suffered severe chronic neglect for the Visual peripersonal and Visual extrapersonal space. In the line bisection task, the concomitance of contralesional neglect and hemianopia caused a dramatic rightward shift in the bisection of long 20 cm lines together with cross-over (i.e. leftward bisection shift) in the bisection of short 2 cm lines. In the cancellation task, neglect was extremely severe in Letter cancellation with target letters interspersed among distracters (only two targets were cancelled on the extreme right of the test sheet). A much weaker asymmetry was observed in Line cancellation with no distracters, suggesting a relevant influence on cancellation performance of the higher attentional load required by the Letter cancellation task. No neglect was evident for the Representational and the Personal-body space. The absence of asymmetry in self-body exploration, motor neglect or hemispatial limb akinesia is appreciable on the video recording in the supplemental data material (file name: TomaiuoloDoricchi-Pat1-FluffTest.mp4).
Anatomical investigation
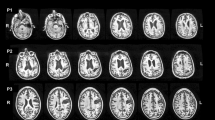
P1’s lesion was localised in the right hemisphere (see upper panel in Fig. 1). A clear damage of the posterior portion of splenium of the corpus callosum was present. The lesion extended in the striate and parastriate cortex (BA 17, 18, 19) including the cortex of the Truncus fissurae parieto-occipitalis et calcarinae. Part of the mesial extrastriate cortex above the occipitalis primis was spared (BA 18, BA 19).
MRI scans of Patient 1 MB (P1, upper row) and Patient 2 MP (P2, lower row). Red arrow = calcarine sulcus, black arrow = central sulcus, green arrow = parietal–occipital sulcus, purple arrow = forceps maior of the splenium of the corpus callosum. P1’s lesion is localised in the right hemisphere: a clear damage of the posterior portion of splenium of the corpus callosum is present. The lesion extends in the striate and parastriate cortex (BA 17, 18, 19) including the cortex of the Truncus fissurae parieto-occipitalis et calcarinae. Mesially, part of the extrastriate cortex above the occipitalis primis is spared (BA 18, BA 19). P2’s lesion is localised in the right hemisphere. The lesion encompasses the visual cortex (BA 17, BA 18, BA 19) and the cortex in the most caudal part of the medial parietal lobe (BA 7, BA 7a). A spared area of grey matter is present mesially and below the calcarine sulcus: this area probably includes a little part of the BA 17, part of the BA 18 and part of the BA 19. White matter lesions were evident within contiguous areas of the parietal and temporal lobe next to the posterior horn of the lateral ventricle, including part of the optic radiation, the forceps maior of the corpus callosum and the tapetum the inferior longitudinal fasciculus. An area of hypodensity is also present in the left forceps maior of the corpus callosum
Patient 2 (P2)
The pattern of neglect impairments suffered by P2 MB was very similar to that suffered by P1 MP. P2 had severe chronic neglect for the Visual peripersonal and Visual extrapersonal space. As in the case of P1, in P2 the concomitance of neglect and hemianopia produced a very relevant ipsilesional rightward shift in the bisection of long 20 cm lines and cross-over (i.e. paradoxical leftward bisection shift) in the bisection of short 2 cm lines. Interestingly, the same pattern of bisection deviations was present when P2 performed the task with the left hand (see Table 1; right-hand vs. left-hand comparisons, two-tailed t-test not significant). In the Letter cancellation task with target letters interspersed among distractors, though outperforming P1, P2 showed clear neglect cancelling only 9 out of the 53 targets on the left side of the test sheet (see Table 1). Exactly as in the case of P1, no neglect was evident for the Representational and the Personal-body space. A video recording of P2’s performance in the Fluff test (file name: TomaiuoloDoricchi-Pat2-FluffTest.mp4) clearly shows the complete absence of personal neglect, motor neglect or hemispatial limb akinesia in both arms.
Anatomical investigation
P2’s lesion was localised in the right hemisphere (see lower panel in Fig. 1). The lesion encompassed the visual cortex (BA 17, BA 18, BA 19) and the cortex in the most caudal part of the medial superior parietal lobe (BA 7, BA 7a). A spared area of grey matter is present mesially and below the calcarine sulcus: this area probably includes a little part of the BA 17, part of the BA 18 and part of the BA 19. White matter lesions were evident within the contiguous parietal and temporal lobe areas adjacent to the posterior horn of the lateral ventricle, including part of the optic radiation, the forceps maior of the corpus callosum (splenial fibres), the tapetum and a small sector of the inferior longitudinal fasciculus.
Discussion
Following callosal damage selectively affecting the right side of the splenium (P1) or the callosal fibres emanating from the splenium (P2), and concomitant left hemianopia caused by damage of the right primary visual cortex (P1 and P2) and the optic radiations (P2), the two patients described in this study developed severe spatial neglect exclusively restricted to the visual domain. No spatial neglect was found for the Personal-body and the Representational-imagery space. At the motor level, no motor neglect or hemispatial limb akinesia were present. At the somatosensory level, no contralesional tactile extinction or contralesional tactile anomia were found. To the best of our knowledge, this pattern of clinical dissociations was never previously described in cases of spatial neglect following callosal disconnection. In particular, the absence of motor neglect, hemispatial limb akinesia, contralesional tactile anomia and contralesional tactile extinction in the two cases from the present study marks a clear clinical difference with respect to previous case studies in which these symptoms were observed. As detailed in the following, we noted that this difference has a rather precisely corresponding anatomical counterpart, because in previously published cases, the callosal lesion always spared the splenium or entirely encompassed the corpus callosum.
The case described by Goldenberg (1986) had complete destruction of the two anterior thirds of the callosum due to bleeding from an anterior cerebral aneurysm. Callosal disconnection of the right hemisphere from the language-dominant left hemisphere provoked tactile anomia, agraphia and ideomotor apraxia of the left hand. The disconnection also caused extinction of left-side touch upon simultaneous stimulation of either arms or legs, and even neglect of unilateral left-side touch. By contrast, the patient correctly named visual geometrical figures, short words and single letters that were tachistoscopically presented for 150 ms in the left visual field: this suggests preserved access of visual inputs initially conveyed to the right hemisphere to language centres in the left hemisphere through spared splenial connections. The patient was also asked to bisect multiple lines (n = 9) scattered on the same test sheet. The task was performed with the left or the right hand. Both hands showed ipsilateral bisection deviation (left hand-leftward, right hand-rightwards): however, more lines were omitted on the left side of the sheet when the task was performed with the right hand (i.e. left hemisphere). This suggests that, due to disconnection, right-hand motor commands in the left hemisphere could not be correctly guided by the right hemisphere towards the left hemispace.
The patient studied by Kashiwagi et al. (1990) suffered a vascular lesion of the posterior part of the genu and of the entire trunk of the corpus callosum. As an effect of callosal disconnection, he showed clear-cut left spatial neglect when performing copy of line drawings, line bisection and figure-matching with the right hand. As in the case described by Goldenberg (1986), this was probably due to disconnection of right-hand motor commands in the left hemisphere from the attentional representation of the left hemispace in the right hemisphere. By contrast, no neglect was found when the same tasks were performed with the left hand directly guided by the right hemisphere, an evidence that is in keeping with the hypothesis that the right hemisphere promotes orienting towards both sides of space ((Heilman and Van Den Abell 1980; Mesulam 1981, 1999, 2002). Importantly, our Patient 2 showed severe left spatial neglect with both hands in line bisection and multiple item cancellation tasks. This suggests that while in the patients described by Goldenberg (1986) and by Kashiwagi et al. (1990), the right hemisphere had unimpaired representation of the left hemispace, in our Patient 2, the combination of left hemianopia and splenial disconnection deprived the intact right parietal–frontal attentional network from any visual input, precluding representing and orienting attention towards the left hemispace. In the patients studied by Goldenberg (1986) and by Kashiwagi et al. (1990), disconnection of the right from the language-dominant left hemisphere caused tactile anomia for stimuli explored with the left hand. On the contrary, both of our patients did not suffer tactile anomia for the left hand, demonstrating that somatosensory inputs arriving to the right hemisphere had normal access to language structures in the left hemisphere, due to anatomical and functional integrity of the central sectors of the corpus callosum.
The patient studied by Heilman and Adams (2003) had removal of a right frontal tumour at age 14. The patient also suffered a vascular lesion of the right striate cortex producing left hemianopia. Following tumour resection, she only suffered transient left hemiparesis. Ten years later, the patient developed severe left visual neglect after complete callosal section for the treatment of epileptic seizures. At variance with our cases with selective splenial disconnection, in this patient, visual neglect was accompanied by directional leftward akinesia of the eyes, motor neglect and akinesia of the left arm and leg. Importantly, the akinesia disappeared when the left arm was placed in the right hemispace, (i.e. hemispatial limb akinesia). Personal-body neglect was not explicitly investigated: however, following callosal section the patient necessitated “..help with activities such as dressing and showering”.
The only case that has some anatomical analogy with those described in the present study is one of two patients (Patient 2) studied by Ortigue et al. (2006). Following an ischaemia in the territory of the right posterior cerebral artery, this patient suffered a lesion involving the inferolateral thalamus, the splenium of the corpus callosum and parts of the medial temporal and occipital lobes. The patient had an upper left quadrantanopia and suffered neglect for the Representational-topographical space but no Visual-perceptual or Personal-body neglect. Sparing of the upper sector of the contralesional visual field makes an important difference between this patient and our two cases, who suffered complete hemianopia, because the seeing upper quadrant allowed direct access of visual information from the contralesional visual space to the right hemisphere of the patient, bypassing the consequences of splenial disconnection and preventing the development of visual neglect. The other relevant difference is the lesion involvement of the inferolateral thalamus. Based on the results of a previous case study (Ortigue et al. 2003) in which a selective thalamic lesion engendered pure representational neglect, Ortigue and coworkers attributed to this lesion the Representational-topographical neglect suffered by their patient. Both of our patients had no thalamic involvement and did not suffer Representational-topographical neglect.
Our observations expand upon the original proposal by Gaffan and Hornak (1997) and are in agreement with the hypothesis that lesions sparing the right fronto-parietal hemispheric network subserving spatial awareness can still yield spatial neglect limited to specific modalities or sectors of space by depriving this network from specific sensory inputs (Mesulam 2002). As it was briefly mentioned in the course of the discussion, with the exception of the study by Ortigue et al. (2006), previous enquiries on callosal patient with spatial neglect never tested personal neglect. This unfortunate lack of evidence leaves open to investigation whether in order to develop personal neglect, a patient with a lesion of the somatosensory sectors of the corpus callosum must also suffer concomitant unilateral damage of the primary somatosensory cortex, as in the case of visual neglect from concomitant splenial and striate cortex damage. The only evidence available to this regard is a recent case study by Balsamo et al. (2008), who found neither personal nor extrapersonal neglect in a patient suffering left-hand tactile anomia due to selective lesion of the posterior trunk of the corpus callosum. Otherwise, both single cases of selective personal neglect with anatomical documentation (Peru and Pinna 1997; Tei 2000; Marangolo et al. 2003) and anatomical group studies on personal neglect, motor neglect and anosognosia for hemiplegia (Berti et al. 2005; Committeri et al. 2007) document quite consistently the lesion involvement of the primary somatosensory and motor cortex together with direct cortical and subcortical involvement of the parietal–frontal attentional network. Finally, in a very recent neurosurgical study in humans, Shinoura et al. (2010) showed that removal of brain tumours compressing the U-shaped fibres connecting the right hemispheric hand motor area in the primary motor cortex with the primary sensory cortex determines regression of motor neglect.
Several neurocognitive models are currently proposed to explain the greater incidence and severity of contralesional neglect following right rather than left brain lesion. Some authors (Heilman and Van Den Abell 1980; Mesulam 1999, 2002) argue that this is so because the right hemisphere orients attention towards both side of space whereas the left hemisphere only towards the right hemispace. This implies that after right brain damage, attention can only be directed rightwards whereas after left brain damage the intact right hemisphere maintains orienting towards both hemispaces. More recently, it has been proposed that neglect depends primarily on damage of functional areas (TPJ-IFG) that subserve non-spatial functions as vigilance and novelty detection, strongly lateralised in the right hemisphere (Corbetta and Shulman 2002). Anatomical disruption of these areas would also produce a unilateral hypoactivation of adjacent right dorsal spatial attentional areas (SPL) provoking asymmetrical distribution of spatial attention (He et al. 2007). Although explaining the greater incidence of the neglect syndrome after right brain lesion is a crucial theoretical challenge, the manifold clinical dissociations encountered in clinical and experimental practice (that most commonly pertain to the modality, the sector of space, the spatial reference frame or the different attentional processes engaged by different screening tasks; Doricchi et al. 2008) together with the behavioural and anatomical dissociations summarised in the present study further demonstrate that neglect cannot be considered a homogenous collection of symptoms engendered by damage of a specific anatomical location. In our opinion, this view should guide the careful use of different diagnostic tools (Pizzamiglio et al. 1989, 1992) and the careful examination of patient’s lesion. The refusal of a strict and simple a-priori equivalence between spatial-neglect and parietal-damage, which is so widely diffused in experimental cognitive neuroscience, can thus provide the researcher with useful insights on the symptomatological and anatomical richness of the neglect syndrome and allow the clinician to better understand and meet the specific needs of each neglect patient.
References
Albert ML (1973) A simple test of visual neglect. Neurology 23:658–664
Azouvi P, Samuel C, Louis-Dreyfus A, Bernati T, Bartolomeo P, Beis J-M, Chokron S, Leclercq M, Marchal F, Martin Y, de Montety G, Olivier S, Perennou D, Pradat-Diehl P, Prairial C, Rode G, Sieroff E, Wiart L, Rousseaux M (2002) Sensitivity of clinical and behavioural tests of spatial neglect after right hemisphere stroke. J Neurol Neurosurg Psychiatry 73:160–166
Balsamo M, Trojano L, Giamundo A, Grossi D (2008) Left hand tactile agnosia after posterior callosal lesion. Cortex 44(8):1030–1036
Bartolomeo P, Thiebaut de Schotten M, Doricchi F (2007) Left unilateral neglect as a disconnection syndrome. Cereb Cortex 45:3127–3148
Berti A, Bottini G, Gandola M, Pia L, Smania N, Stracciari A, Castiglioni I, Vallar G, Paulesu E (2005) Shared cortical anatomy for motor awareness and motor control. Science 309(5733):488–491
Beschin N, Robertson IH (1997) Personal versus extrapersonal neglect: a group study of their dissociation using a reliable clinical test. Cortex 33:379–384
Bird CM, Malhotra P, Parton A, Coulthard E, Rushworth MF, Husain M (2006) Visual neglect following right posterior cerebral artery infarction. J Neurol Neurosurg Psychiatry 77:1008–1012
Bisiach E, Luzzatti C (1978) Unilateral neglect of representational space. Cortex 14:129–133
Caminiti R, Ghaziri H, Galuske R, Hof PR, Innocenti GM (2009) Evolution amplified processing with temporally dispersed slow neuronal connectivity in primates. Proc Natl Acad Sci USA 106(46):19551–19556
Carlesimo GA, Buccione I, Fadda L et al (2002) Standardizzazione di due test di memoria: Breve Racconto e Figura di Rey. Nuova Riv Neurol 12:1–13
Cocchini N, Beschin N, Jehkonen M (2001) The Fluff Test: a simple task to assess body representation neglect. Neuropsychol Rehabil 11:17–31
Committeri G, Pitzalis S, Galati G, Patria F, Pella G, Sabatini U, Castriota Scanderberg A, Piccardi L, Guariglia C, Pizzamiglio L (2007) Neural bases of personal and extrapersonal neglect in humans. Brain 130:431–441
Corbetta M, Shulman GL (2002) Control of goal-directed and stimulus-driven attention in the brain. Nat Rev Neurosci 3:201–215
Critchley M (1953) The parietal lobes. Hafner, New York
Diller L, Ben-Yishay Y, Gerstman LJ, Goodkin R, Gordon W, Weinberg J (1974) Studies in cognition and rehabilitation in hemiplegia. University Medical Center, New York, p 50
Doricchi F, Tomaiuolo F (2003) The anatomy of neglect without hemianopia: a key role for parietal-frontal disconnection? NeuroReport 14:2239–2243
Doricchi F, Thiebaut de Schotten M, Tomaiuolo F, Bartolomeo P (2008) White matter (dis)connections and gray matter (dys)functions in visual neglect: gaining insights into the brain networks of spatial awareness. Cortex 44(8):983–995
Duvernoy H (1991) The human brain, surface, three-dimensional sectional anatomy and MRI. Springer, Wien
Economo C, Koskinas GN (1925) Die Cytoarchitektonik der Hirnrinde des Erwachsenen Menschen. Springer, Wien
Gaffan D, Hornak J (1997) Visual neglect in the monkey. Representation and disconnection. Brain 120:1647–1657
Geschwind N (1965a) Disconnexion syndromes in animals and man. I. Brain 88:237–294
Geschwind N (1965b) Disconnexion syndromes in animals and man. II. Brain 88:585–644
Goldenberg G (1986) Neglect in a patient with partial callosal disconnection. Neuropsychologia 24(3):397–403
Guariglia C, Padovani A, Pantano P, Pizzamiglio L (1993) Unilateral neglect restricted to visual imagery. Nature 364:235–237
He BJ, Snyder AZ, Vincent JL, Epstein A, Shulman GL, Corbetta M (2007) Breakdown of functional connectivity in frontoparietal networks underlies behavioral deficits in spatial neglect. Neuron 53:905–918
Heilman KM, Adams DJ (2003) Callosal neglect. Arch Neurol 60(2):276–279
Heilman KM, Van Den Abell T (1980) Right hemisphere dominance for attention: the mechanism underlying hemispheric asymmetries of inattention (neglect). Neurology 30:327–330
Kashiwagi A, Kashiwagi T, Nishikawa T, Tanabe H, Okuda J (1990) Hemispatial neglect in a patient with callosal infarction. Brain 113:1005–1023
Leibovitch FS, Black SE, Caldwell CB, Ebert PL, Ehrlich LE, Slazai JP (1998) Brain-behavior correlations in hemispatial neglect using CT and SPECT: the Sunnybrook Stroke Study. Neurology 50:901–908
Marangolo P, Piccardi L, Rinaldi MC (2003) Dissociation between personal and extrapersonal neglect in a crossed aphasia study. Neurocase 9(5):414–420
Mesulam MM (1981) A cortical network for directed attention and unilateral neglect. Ann Neurol 10:309–325
Mesulam MM (1999) Spatial attention and neglect: parietal, frontal and cingulate contributions to the mental representation and attentional targeting of salient extrapersonal events. Phil Trans Royal Soc London B 354:1325–1346
Mesulam MM (2002) Functional anatomy of attention and neglect: from neurons to networks. In: Karnath H, Milner D, Vallar G (eds) The cognitive and neural bases of spatial neglect. Oxford University Press, Oxford, pp 33–45
Orsini A, Grossi D, Capitani E, Laiacona M, Papagno C, Vallar G (1987) Verbal and spatial immediate memory span: normative data from 1355 adults and 1112 children. Ital J Neurol Sci 8(6):539–548
Ortigue S, Viaud-Delmon I, Michel C et al (2003) Pure imagery hemi-neglect of far space. Neurology 60:2000–2002
Ortigue S, Megevand P, Perren F, Landis T, Blanke O (2006) Double dissociation between representational personal and extrapersonal neglect. Neurology 66:1414–1417
Park KC, Lee BH, Kim EJ, Shin MH, Choi KM, Yoon SS, Kwon SU, Chung CS, Lee KH, Heilman KM, Na DL (2006) Deafferentation-disconnection neglect induced by posterior cerebral artery infarction. Neurology 66(1):56–61
Peru A, Pinna G (1997) Right personal neglect following a left hemisphere stroke. A case report. Cortex 33(3):585–590
Pizzamiglio L, Judica A, Razzano C, Zoccolotti P (1989) Toward a comprehensive diagnosis of visuo-spatial disorders in unilateral brain-damaged patients. Psychol Assess 5:199–218
Pizzamiglio L, Antonucci G, Judica A, Montenero P, Razzano C, Zoccolotti P (1992) Cognitive rehabilitation of the hemineglect disorder in chronic patients with unilateral brain damage. J Clin Exp Neuropsychol 14:901–923
Shinoura N, Suzuki Y, Yamada R, Tabei Y, Saito K, Yagi K (2009) Damage to the right superior longitudinal fasciculus in the inferior parietal lobe plays a role in spatial neglect. Neuropsychologia 47(12): 2600–2603. Epub 2009 May 22
Shinoura N, Yoshida M, Yamada R, Tabei Y, Saito K, Suzuki Y, Yagi K (2010) Combined damage to the right hemispheric hand area in the primary motor and sensory area plays a critical role in motor hemineglect. Eur Neurol 63(1): 17–23. Epub 2009 Nov 14
Tei H (2000) Right ipsilateral in a case of anosognosia for hemiplegia and personal neglect with the patient’s subjective experience hypersensation. J Neurol Neurosurg Psychiatry 69:274–275
Thiebaut de Schotten M, Urbansy M, Duffau H, Volle E, Lévy R, Dubois B, Bartolomeo P (2005) Direct evidence for a parietal-frontal pathway subserving spatial awareness in humans. Science 309:2226–2228
Tomaiuolo F, Nocentini U, Grammaldo L, Caltagirone C (2001) Interhemispheric transfer time in a patient with a partial lesion of the corpus callosum. Neuroreport 12(7):1469–1472
Verdon V, Schwartz S, Lovblad KO, Hauert CA, Vuilleumier P (2009) Neuroanatomy of hemispatial neglect and its functional components: a study using voxel-based lesion-symptom mapping. Brain. Dec 22. [Epub ahead of print]
Zoccolotti P, Judica A (1991) Functional evaluation of hemineglect by means of a semistructured scale: personal extrapersonal differentiation. Neuropsychol Rehabil 1:33–34
Acknowledgments
We thank BIC people from the Montreal Neurological Institute, Mc Gill University, Canada, for providing us with software for brain images investigations. Thanks to Franco Malasoma for his help in MRI data acquisition and preprocessing. F.T. wishes to thank the ‘‘Cassa di Risparmio di Volterra’’ for providing technical equipment and Dr. G. Mariani (General Manager) and G. Brunale (President) for their support in setting up the ‘‘Laboratory of Neuroanatomy’’ at the ‘‘Auxilium Vitae’’ Volterra (Pisa). We thank Francesca Costagli for help with video recordings. This study was supported by grants from the Fondazione Cassa di Risparmio di Volterra (FT) and from the Fondazione Santa Lucia (FD), Rome.
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tomaiuolo, F., Voci, L., Bresci, M. et al. Selective visual neglect in right brain damaged patients with splenial interhemispheric disconnection. Exp Brain Res 206, 209–217 (2010). https://doi.org/10.1007/s00221-010-2230-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-010-2230-6