Abstract
We studied whether stimulation of the primary motor cortex (M1) attenuates pain-related spinal withdrawal responses of neuropathic and healthy control rats, and whether the descending antinociceptive effect is relayed through the noradrenergic locus coeruleus (LC). The assessments of the noxious heat-evoked limb withdrawals reflecting spinal nociception and recordings of single LC units were performed in spinal nerve-ligated neuropathic and sham-operated control rats under light pentobarbital anesthesia. Electric stimulation of M1 produced equally strong spinal antinociception in neuropathic and control rats. Following microinjection into M1, a group I metabotropic glutamate receptor agonist (DHPG; 10 nmol) and a high (25 nmol) but not low (2.5 nmol) dose of glutamate slightly increased on-going discharge rates of LC neurons in neuropathic but not in control animals. Influence of electric stimulation of M1 on LC neurons was studied only in the neuropathic group, in which discharge rates of LC neurons were increased by electric M1 stimulation. Lidocaine block of the LC or block of descending noradrenergic influence by intrathecal administration of a α2-adrenoceptor antagonist failed to produce a significant attenuation of the spinal antinociceptive effect induced by electric M1 stimulation in the neuropathic or the sham group. The results indicate that stimulation of the rat M1 induces spinal antinociception in neuropathic as well as control conditions. While M1 stimulation may activate the LC, particularly in the neuropathic group, the contribution of coeruleospinal noradrenergic pathways may not be critical for the spinal antinociceptive effect induced by M1 stimulation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Invasive stimulation of the primary motor cortex (M1) has served for almost two decades as a clinical treatment for chronic pain (Tsubokawa et al. 1991), particularly for alleviation of nerve injury-induced neuropathic pain (e.g., Hosomi et al. 2008; Lazorthes et al. 2007; Nguyen et al. 1999). High-frequency stimulation of M1 by noninvasive transcranial electric or magnetic pulses has also attenuated chronic pain (Lefaucheur 2006) and increased the threshold for experimental pain stimuli in human patients and healthy subjects, although not under all conditions and in all individuals (Johnson et al. 2006; Summers et al. 2004; Valmunen et al. 2009). Electric stimulation of M1 may modulate pain-related responses also in experimental animals as shown by suppression of pain-related limb withdrawal response (Fonoff et al. 2009), attenuation of responses in nociceptive spinal dorsal horn neurons (Senapati et al. 2005) and the reduction in sensory abnormalities induced by nerve injury (Rusina et al. 2005; Vaculin et al. 2008).
Mechanisms involved in the antinociceptive effect of M1 stimulation are still poorly understood. M1 not only projects to motor areas of the brainstem and spinal cord, such as the red nucleus and the spinal ventral horn, respectively, but also sends projections or collateral branches to areas that contribute to the relay of ascending somatosensory signals or descending modulation of pain (Canedo 1997). M1 projections to the spinal dorsal horn, dorsal column nuclei, and the somatosensory thalamus provide a mechanism through which M1 may directly modulate ascending afferent signals. Alternatively, M1 may modulate somatosensory signals indirectly through its projections to various brain areas, such as the superior colliculus (Keizer et al. 1987), bulbar medial reticular formation (Keizer and Kuypers 1984), and the striatum (McGeorge and Faull 1989) that also contribute to pain regulation (see for reviews, Millan 2002; Pertovaara and Almeida 2006) and provides potential relays for an antinociceptive circuitry activated by M1 stimulation. The hypothesis that M1 stimulation activates descending pain modulatory pathways is supported by a recent study showing that systemic administration of an opioid receptor antagonist reversed the spinal antinociceptive effect induced by M1 stimulation in the rat (Fonoff et al. 2009). This finding, however, still leaves open which of the major descending pain-regulatory pathways (Millan 2002; Pertovaara and Almeida 2006) are involved in M1-induced antinociception and whether their efficacy is changed in pathophysiological conditions, such as peripheral nerve injury-induced neuropathy.
In the present study, we assessed whether M1 stimulation attenuates pain-related spinal responses of the rat as effectively in neuropathic as control conditions and whether the locus coeruleus (LC), a major source of descending noradrenergic pain regulatory pathways (Pertovaara 2006), mediates spinal antinociception induced by M1 stimulation. For this purpose, we assessed the influence of M1 stimulation on the noxious heat-evoked spinal withdrawal response in spinal nerve-ligated neuropathic and sham-operated control animals under light anesthesia. Moreover, we assessed whether M1 stimulation influences discharge rates and responses to heat of putative pain regulatory neurons in the LC. Furthermore, we attempted to reverse the M1 stimulation-induced spinal antinociceptive effect by administering a local anesthetic into the LC or a selective α2-adrenoceptor antagonist into the spinal cord to study further whether noradrenergic pathways descending from the LC and acting on spinal α2-adrenoceptors are relaying the antinociceptive influence from M1 to the spinal cord.
Materials and methods
Experimental animals
The experiments were performed in adult, male Hannover-Wistar rats (Harlan, Horst, Netherlands, and Biomedicum, Helsinki, Finland; weight: 200–300 g). The Experimental Animal Ethics Committee of the Provincial Government of Southern Finland (Hämeenlinna, Finland) approved methods and the experiments were performed according to the guidelines of European Communities Council Directive of 24 November 1986 (86/609/EEC). All efforts were made to limit distress and to use only the number of animals necessary to produce reliable scientific data. Rats were housed in a 12-h light/dark cycle with free access to food and water.
Techniques for producing neuropathy
The unilateral ligation of two spinal nerves (L5 and L6) was performed under sodium pentobarbital anesthesia (50 mg/kg i.p.) as described in detail earlier (Kim and Chung 1992). Briefly, left paraspinal muscles were separated from the spinous processes at the L4–S2 levels. The L6 transverse process was partly removed to identify visually the L4 and L6 spinal nerves. The left L5 and L6 spinal nerves were isolated and tightly ligated with 6–0 silk thread. After nerve ligation, the wound was sutured and the rats were allowed to recover. Development of nerve injury-induced mechanical hypersensitivity was assessed in awake animals 10–14 days following the operation. Of the spinal nerve-ligated rats, only those with a marked hypersensitivity to mechanical stimulation with monofilaments (hind limb withdrawal thresholds in the operated side <2 g) and with no motor impairment were selected for the neuropathic study group. As controls, we used a group of sham-operated animals that underwent the same surgical procedures as the spinal nerve-ligated animals (including partial removal of the L6 transverse process), except that their spinal nerves were not ligated. Sham-operated animals were not hypersensitive to mechanical stimulation. Influence of cortical stimulation on neuronal or limb withdrawal responses was studied 3–4 weeks after ligation of spinal nerves or sham operation.
Preparation for cerebral drug injections and electric stimulations
For chemical or electric stimulation of M1, a small hole was drilled in the skull for a 26-gauge electrode cannula-guide (C315G-MS303/2/SPC, PlasticsOne, Roanoke, VA, USA), 26-gauge guide cannula (C315G, PlasticsOne) or a concentric bipolar electrode (Rhodes NE-100, David Kopf Instruments, Tujunga, CA, USA). The desired injection and stimulation site in M1 was between 1.7 mm anterior and 0.26 mm posterior from the bregma, 1–3 mm lateral from the midline and 0.7–2.2 mm ventrally from the dura mater (Paxinos and Watson 1998).
For drug delivery into the LC, a hole was drilled for a 26-gauge guide cannula (C315G, PlasticsOne). The desired injection site in the LC was 0.68–1.3 mm posterior from the ear bar, 1.3 mm lateral from the midline and 6.8–7.6 mm from the dura mater (Paxinos and Watson 1998). The tip of the guide cannula was positioned 1 mm above the desired injection site in the LC.
Chemical and electric stimulations of M1 were performed ipsilateral to the spinal nerve ligation or sham operation, except that in one group of nerve-injured animals, electric M1 stimulation was applied contralateral to the limb that was studied. The focus of the present study was on effects ipsilateral to M1 stimulation and nerve injury or sham surgery for the following of reasons: (a) although some corticospinal axons descend ipsilaterally in the rat (Joosten et al. 1992), a possible confounding effect due to activation of limb muscles by M1 stimulation was expected to be negligible when testing sensory responses in the side that was ipsilateral to M1 stimulation. (b) Recent results using identical parameters for electric M1 stimulation as in the present study indicate that the antinociceptive effect in the rat spinal dorsal horn is of the same magnitude ipsi- as contralateral to M1 stimulation (Senapati et al. 2005). (c) Among our working hypotheses was that M1 might induce spinal antinociception through its pontine projection potentially influencing the noradrenergic brainstem nuclei. Alternatively or additionally, we hypothesized that M1 stimulation might produce spinal antinociception through a pathway involving the striatum, the superior colliculus and the RVM (Basso and Evinger 1996; Basso et al. 1996). Previous results indicated that projections of M1 to the brainstem (e.g., Keizer et al. 1987) and the striatum (McGeorge and Faull 1989) are strongest ipsilaterally. Moreover, our recent results in the rat indicated that stimulation of brainstem nuclei located lateral to the midline (e.g., Viisanen and Pertovaara 2007) or striatal stimulation (Ansah et al. 2007; Pertovaara and Wei 2008) produce descending antinociception that may be stronger ipsi- than contralaterally.
Preparation for intrathecal drug injections
A group of animals had an intrathecal (i.t.) catheter for drug delivery to the spinal cord level. The catheter (Intramedic PE-10, Becton–Dickinson and Company, Sparks, MD, USA) was administered into the lumbar level of the spinal cord under pentobarbital anesthesia (50 mg/kg i.p.) as described in detail elsewhere (Størkson et al. 1996). I.t. catheter was administered in the same procedure as nerve injury or sham surgery at least 3 weeks before actual drug testing. Following recovery from anesthesia, the correct placing of the catheter was verified by administering lidocaine (4%, 7–10 μl followed by a 10 μl of saline for flushing) with a 50 μl Hamilton syringe (Hamilton Company, Bonaduz, Switzerland). Only those rats that had no motor impairment before lidocaine injection but had a bilateral paralysis of hind limbs following i.t. administration of lidocaine were studied further.
Microinjections
Drugs or saline were microinjected into M1 and LC through a 33-gauge stainless steel injection cannula (C315I, PlasticsOne) inserted through and protruding to 1 mm below the tip of the 26-gauge guide cannula (C315G, PlasticsOne) or to level of the a 26-gauge electrode cannula-guide (C315G-MS303/2/SPC, PlasticsOne). The microinjections were performed using a 10-μl Hamilton syringe (Hamilton Company) connected to the injection cannula by polyethylene (Intramedic PE-10, Becton–Dickinson and Company) tubing. The volume of the injections was 0.5 μl. The efficacy of the injection was monitored by watching the movement of a small air bubble through the tubing. The injection lasted 30 s and the injection cannula was left in place at least for an additional 30 s and in most cases, until the next injection was performed. Intrathecal drug injections were performed using a 50-μl Hamilton syringe. The volume of intrathecal drug injections was 5 μl that was followed by a flush with 15 μl of saline.
Electric stimulation of M1
The experiment assessing the relationship between the magnitude of spinal antinociception and the intensity of electric stimulation of the cerebral cortex was performed using an electrode-cannula guide (C315G-MS303/2/SPC, PlasticsOne) or a concentric bipolar electrode (Rhodes NE-100, David Kopf Instruments). Tip of the stimulus electrode was placed in M1. Electric stimuli were generated by a constant current stimulator (PSIU6 and Grass S88, Grass Instruments, Quincy, MA, USA). Electric stimulation of M1 was performed at the frequency of 300 Hz (duration of each stimulus pulse: 0.1 ms) as earlier (Senapati et al. 2005). Intensity of electric stimulation was chosen for each experiment as described below (see sections on course of the experiments). Duration of electric M1 stimulation was 15 s. In each experimental condition, only one type of electrode was used and the results were compared with the results obtained in the identical saline/control condition.
Electrophysiological recordings of LC neurons
Single unit recordings of LC neurons were performed under sodium pentobarbital anesthesia, which was induced by administering 50 mg/kg of sodium pentobarbital i.p. Following induction of anesthesia, the animal was placed in a standard stereotaxic frame according to the atlas of Paxinos and Watson (1998) and anesthesia was continued by administering sodium pentobarbital at the dose of 15–20 mg/kg/h. The level of anesthesia was frequently monitored by assessing the size of the pupils, general muscle tone and by assessing withdrawal responses to noxious stimulation. Supplemental doses of sodium pentobarbital were given as required. At the time of testing, the response properties of LC neurons, the level of anesthesia were kept at a level at which no spontaneous movements of extremities was observed and the noxious test stimuli applied to the hind paw produced a brief withdrawal response. The rats were spontaneously breathing and the body temperature was maintained within a physiological range with a warming blanket. The peripheral perfusion was checked by examining the color of the ears and extremities.
The skull was exposed and a hole drilled for placement of a recording electrode in the LC The desired recording site in the LC was 0.68–1.3 mm posterior from the ear bar, 1.3 mm lateral from the midline and 6.8–7.6 mm from the dura mater (Paxinos and Watson 1998). Single neuron activity was recorded extracellularly with lacquer-coated tungsten electrodes (impedance 5–7 MΩ at 1 kHz; FHC Inc., Bowdoin, ME, USA). The signal was amplified and filtered by using standard techniques. Data sampling was performed with a computer connected to a CED Micro 1401 interface and using Spike 2 software (Cambridge Electronic Design, Cambridge, Cambridge, UK).
When searching for and characterizing response properties of LC neurons, their response to noxious stimulation was assessed by applying a hemostatic clamp to the tail for 5 s. The clamp produced pain when applied to the finger of the experimenter. It was assumed that those LC neurons that give an excitatory response to noxious pinch are likely to be noradrenergic neurons involved in feedback inhibition of pain (Hirata and Aston-Jones 1994; Viisanen and Pertovaara 2007).
Total duration of the recording session varied from 2 to 4 h. In some of the recordings, it was possible to identify and study in parallel more than one neuron. At the end of the microelectrode recording session, the animal was given a lethal dose of sodium pentobarbital, an electrolytic lesion was made in the recording site, and the brain was removed for histological verification of the recording and injection sites.
Assessment of a spinal nociceptive reflex
Heat-evoked hind limb withdrawal response was used to assess spinal nociception. After induction of anesthesia with sodium pentobarbital (40 mg/kg i.p.), the assessment of limb withdrawal did not start until the level of anesthesia was so low that the animal gave a withdrawal response to noxious pinch of the skin, but did not have spontaneous movements. After that, a low level of anesthesia was maintained by administering sodium pentobarbital at the dose of 15–20 mg/kg/h. For inducing the hind limb withdrawal reflex, noxious heat (54°C) was applied for 10 s with a Peltier device (LTS-3 Stimulator, Thermal Devices Inc., Golden Valley, MN, USA) to the plantar skin of the hind paw. To determine the latency of the heat-induced limb reflex, a piezoceramic movement detector (Siemens Elema Ab, Solna, Sweden) was taped on the skin over a flexor muscle in the hind limb. The signal from the thermostimulator and the movement detector were amplified and sampled with a computer via a CED Micro 1401 interface and Spike 2 software (Cambridge Electronic Design). Latency was determined from the start of the heat stimulus to the first movement of the hind limb.
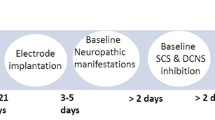
General course of the study
Spinal nerve ligation or sham operation was performed under anesthesia at day 0; i.t. catheter was inserted during the same operation (day 0). Tactile threshold determinations for verification of allodynia were performed in awake animals on day 10–14, and before induction of anesthesia for the terminal experiment. In the terminal experiment, influence of M1 stimulation on the withdrawal threshold or neuronal discharge rates of LC neurons were studied under anesthesia 3–4 weeks following spinal nerve ligation or sham operation. Guide cannulae for intracerebral injections or electrodes for M1 stimulation were inserted during the terminal experiment.
Spinal antinociception induced by electric or chemical stimulation of M1: course of the study
Spinal antinociceptive effect induced by electric stimulation of M1 at varying intensities was assessed in lightly anesthetized animals with spinal nerve ligation (n = 10) or sham operation (n = 6) 4 weeks after spinal nerve ligation. Electric stimulation was administered at the frequency of 300 Hz (duration of each stimulus pulse: 0.1 ms) and at the intensities of 0 (control with no stimulation), 30, 50, 70, 100, 120, and 140 μA. For further details on stimulus production, see section on electric stimulation of M1 (above). Different intensities of cortical electric stimulation were applied first in increasing and then decreasing order (0 μA between). The mean of the values obtained at each stimulus intensity was used in further calculations. Electric stimulation started 5 s before heat stimulation of the hind paw and continued until the end of heat stimulation. The interval between each testing was 2 min. The heat-evoked withdrawal latency was determined in the hind limb ipsilateral to M1 stimulation and ipsilateral to the nerve injury or sham operation. Additionally, in a group of nerve-injured animals (n = 4), the heat-evoked withdrawal latency was determined in the unoperated hind limb contralateral to M1 stimulation. In this group, electric stimulation of M1 was performed at the intensities of 0 (control with no stimulation), 30 and 50 μA (see for further details on the method for reflex measurements the section on assessment of a spinal nociceptive reflex, above).
Spinal antinociceptive effect induced by glutamate in M1 was assessed in a separate group of lightly anesthetized neuropathic animals that had an electrode-cannula guide for cortical microinjections. Saline or glutamate at the dose of 2.5 or 25.0 nmol (in 0.5 μl) was microinjected into M1 in ascending order 2 min prior to heat stimulation of the neuropathic hind paw. The interval between injections was 5–7 min. The mean of the withdrawal latencies evoked by each dose of glutamate or saline for each animal was used in further calculations.
Influence of glutamatergic stimulation of M1 on ongoing neuronal activity in the LC: course of the study
The effect of glutamate administration into M1 on the ongoing activity of LC neurons was studied in nerve-injured (n = 9) and sham-operated animals (n = 7). After characterization of a LC neuron in a lightly anesthetized animal (see for further details section on electrophysiological recordings of LC neurons, above), the effect of M1 stimulation on its ongoing discharge rate was assessed by microinjecting saline or glutamate at the dose of 2.5 nmol or 25.0 nmol (in 0.5 μl) into M1. The discharge rate of the LC neuron was recorded before, during and up to 3 min following each injection. The interval between the injections was 5–7 min. The order of injecting saline or glutamate at different doses was the same in all experimental groups: (1) saline, (2) glutamate at the dose of 2.5 nmol, (3) glutamate at the dose of 25 nmol. The identical procedure of administering various doses of glutamate in all experimental conditions allows comparisons of glutamatergic effects between different experimental groups (nerve-injured vs. sham-operated animals). Since glutamate proved to induce its peak effects during the first minutes following injection, in the final analysis only the discharge rates measured during the first and second minutes following glutamate or saline injection were taken into account. In calculations, the post-injection discharge rate was first compared with the corresponding pre-injection rate by subtracting the pre-injection rate from the post-injection rate. To eliminate potential influence of injection volume per se, the value representing the difference in post-saline and pre-saline activity was subtracted from the value representing the difference in post-glutamate and pre-glutamate activity. Thus, the final value representing the glutamate-induced effect on ongoing discharge rate that is reported in the results was calculated in the following way: [discharge rate after glutamate injection − discharge rate before glutamate injection] − [discharge rate after saline injection − discharge rate before saline injection]. This value, if positive, is expected to represent a true glutamate-induced increase in the ongoing discharge rate of LC neurons, and if negative, a glutamate-induced decrease in the discharge rate.
Modulation of the ongoing discharge rate of LC neurons following administration of a group I metabotropic glutamate receptor agonist, DHPG (10 nmol in 0.5 μl), into M1 was studied in the same sham-operated and nerve-injured animals as the effect of glutamate. Effect of DHPG was studied after the glutamate study was completed. When assessing influence of DHPG, the ongoing activity of the LC neuron was recorded before, during and up to 32 min following saline or DHPG injection into M1. The order of injections was the same in sham-operated and nerve-injured animals: (1) saline and (2) DHPG. Since it proved to take up to 10 min to reach the peak effect of DHPG, discharge rate from the end of injection up to 11th min after injection was taken into account in the data analysis. The ongoing discharge rate of LC neurons was calculated from time point 0–11th min after saline or DHPG injection. After this, the final value representing the DHPG-induced change in the ongoing discharge rate of LC neurons that was reported in the results was calculated by subtracting the value obtained after DHPG injection from the value obtained after saline injection. A positive value represents a true DHPG-induced increase in the ongoing discharge rate and a negative one represents a DHPG-induced decrease in the discharge rate. The interval between testing two different cells with glutamate was at least 30 min, and with DHPG, at least 1 h.
Influence of electric stimulation of M1 on ongoing neuronal activity and on heat-evoked responses of LC neurons: course of the study
The effects of electric stimulation of M1 on the ongoing activity of LC neurons and their heat-evoked responses were studied in a separate group of nerve-injured animals under light pentobarbital anesthesia (n = 5). After searching for and characterizing the response-properties of a LC neuron (for details, see “Electrophysiological recordings of LC neurons”, above), its spontaneous activity and heat-evoked response was studied without and with electric M1 stimulation. Since M1 stimulation produced its strongest antinociceptive effect at the intensity of 30 μA, this study focused on assessing the antinociceptive effect induced by electric M1 stimulation at the intensity of 30 μA and at 0 μA for comparison. Electric stimulation (0.1 ms pulses at 300 Hz) was applied to M1 ipsilateral to LC and nerve injury for 15 s either starting 5 s prior to heat stimulation of the plantar skin in the injured paw (54°C for 10 s; LTS-3 Stimulator, Thermal Devices Inc.) or starting without accompanying heat stimulation, to assess influence of M1 stimulation per se on the neuronal discharge rate. Four to 11 neurons were tested in each animal. In the data analysis, the discharge rate before noxious heat application was compared with the discharge rate determined during noxious heat. When determining the discharge frequency during heat stimulation, a 3-s period beginning 0.5 s before the paw withdrawal was taken in account.
Total duration of the recording session varied from 2 to 3 h and there was no significant difference between responses of the first and last cells examined. At the end of the microelectrode recording session, the animal was given a lethal dose of sodium pentobarbital, an electrolytic lesion was made in the recording site, and the brain was removed for histological verification of the recording and injections sites.
Attempted reversals of the spinal antinociceptive effect of M1 stimulation by pontine or intrathecal drug administrations in neuropathic animals and control animals
Role of descending noradrenergic pathways in M1 stimulation-induced antinociception was assessed by administering intrathecally 5 μg of atipamezole, a selective α2-adrenoceptor antagonist, or physiological saline to the lumbar spinal cord of neuropathic and sham control animals. Eight minutes after its administration, the latency of the heat-induced hind limb reflex was assessed without and with ipsilateral M1 stimulation. Since M1 stimulation produced its strongest antinociceptive effect at the intensity of 30 μA, this study focused on assessing the effect the intensity of 30 μA and at 0 μA for comparison. When attempting to reverse M1-induced spinal antinociception by i.t. treatment with atipamezole, saline condition was tested 10 min before assessing the effect by intrathecal administration of atipamezole.
In a separate experiment, a block of the LC was induced by microinjecting lidocaine (4%/0.5 μl) or saline (control) into the LC to assess its contribution to the M1 stimulation-induced spinal antinociception in neuropathic and control animals. This dose and volume of lidocaine in the brainstem produces up to 30 min an effective block in an area that has a radius of 0.5 mm (Sandkühler and Gebhart 1984). A guide cannula for LC injections was implanted and the injections performed under anesthesia as described above. Five minutes after microinjecting lidocaine or saline into the LC, the latency of the heat-induced limb reflex was determined with and without ipsilateral M1 stimulation as following intrathecal treatments (see above). When assessing effect of lidocaine in the LC, the saline condition was always tested about 10 min before lidocaine treatment.
The results obtained with saline administration into the LC and spinal cord were pooled into one saline control group in the final analysis. After completing the study, the animals were given a lethal dose of pentobarbitone and the brains were removed for histological assessment of the stimulation and injections sites.
Drugs
Glutamate was purchased from Sigma-Aldrich (St. Louis, MO, USA). A group I metabotropic glutamate receptor agonist, 3,5-dihydroxyphenylglycine (DHPG) was purchased from Tocris Bioscience (Bristol, UK). The doses of glutamatergic compounds were chosen based on earlier publications (e.g., Ansah et al. 2009). Atipamezole (OrionPharma, Turku, Finland) was used as a α2-adrenoceptor antagonist. It is noteworthy that atipamezole, unlike some other α2-adrenoceptor antagonists, does not bind to 5-HT1A receptors (Pertovaara et al. 2005). The intrathecal dose of atipamezole was 5 μg, since previous studies indicated that at this dose, intrathecally administered atipamezole has little or no effect on neuropathic hypersensitivity (Pertovaara and Wei 2008). Physiological saline was used as control. Lidocaine was purchased from OrionPharma.
Statistics
Data are presented as mean SEM. Statistical analysis was performed using one- or two-way-analysis of variance (1-w- or 2-w-ANOVA), with repeated measures (rmANOVA) when appropriate. Post hoc testing was performed with Tukey’s test or a t test with a Bonferroni correction. Comparisons between two groups were performed with a t test. P < 0.05 was considered to represent a significant difference.
Results
All spinal nerve-ligated rats in this study developed neuropathic hypersensitivity as indicated by the monofilament-induced limb withdrawal threshold that was always <2 g ipsilateral to the nerve injury. Results obtained with animals born in the Netherlands and their first generation offspring born in Finland were identical and therefore, the data obtained with these two populations of animals were pooled. Only cortical stimulations and injections that were within M1 and injections, and single cell recordings of neurons that were in the LC according to histological analyses were included in this study (Fig. 1).
a A schematic diagram showing cortical sites of glutamate/DHPG/saline injections and electric stimulation. b A schematic diagram showing recording sites and stimulation sites in the LC. c Photographic examples of a microinjection site in M1 and a recording site in the LC. In c, arrows indicate the injection/recording sites. In a and b, filled symbols represent sham control animals and open symbols nerve-injured animals
Spinal antinociception induced by stimulation of M1
Thermal antinociception induced by electric stimulation of M1 ipsilateral to the studied hind limb was assessed by determining the heat-evoked withdrawal reflex latency in ten rats with a nerve injury in the studied limb and in six rats with a sham operation in the studied limb. Moreover, thermal antinociception induced by electric stimulation of M1 contralateral to the studied healthy hind limb was assessed in a separate session in four rats with a nerve injury.
Electric stimulation of M1 produced significant antinociception in the ipsilateral nerve-injured and sham-operated limb that varied with intensity of stimulation (F 6,84 = 4.32 P < 0.001; 2-w-ANOVA). The magnitude of thermal antinociception was increased with an increase in the intensity of M1 stimulation from 0 to 50 μA, while with a further increase of stimulus intensity to 140 μA the magnitude of antinociception was decreased (Fig. 2a). The magnitude of the thermal antinociceptive effect induced by electric stimulation of ipsilateral M1 was not significantly different between sham-operated and nerve-injured animals (F 1,84 = 0.0025; 2-w-ANOVA). In nerve-injured animals, electric stimulation of M1 ipsilateral to injury produced antinociception in the contralateral healthy limb (F 2,3 = 6.749 P < 0.05; 1-w-rmANOVA; Fig. 2a). However, the magnitude of thermal antinociception was smaller in the healthy limb contralateral to M1 stimulation than in the nerve-injured limb ipsilateral to M1 stimulation (F 1,36 = 5.91 P < 0.05; 2-w-ANOVA; Fig. 2a).
a Increase of the heat-evoked hind limb withdrawal latency by electric stimulation of M1 at varying intensities in neuropathic (Neurop) and sham control (Sham) animals. b Heat-evoked hind limb withdrawal latency following administration of glutamate (Glu) or saline (Sal) into M1 of neuropathic animals. Glu 2.5 and Glu 25.0 indicate the dose of glutamate in nmol. Ipsi M1 stimulation ipsilateral to the studied limb and nerve injury or sham operation, Contra M1 stimulation contralateral to the studied limb and nerve injury. §/+ P < 0.05, **/++ P < 0.01 (t-test with a Bonferroni correction; reference: the corresponding latency without electric stimulation = 0 μA). +/++ within the sham group. ** within the neuropathic group (Ipsi). § within the neuropathic group (Contra). Error bars represent SEM (in a, nSham = 6, nNeurop (Ipsi) = 10, and nNeurop (Contra) = 4; in b, n = 14)
Thermal antinociception induced by chemical stimulation of M1 with glutamate was assessed in a separate session in nerve-injured rats only (n = 9). Stimulation of M1 by glutamate, independent of dose (2.5 or 25 nmol), failed to induce a significant prolongation of the heat-evoked hind limb withdrawal latency in the injured limb ipsilateral to M1 stimulation (F 2,13 = 1.418; 1-w-rmANOVA; Fig. 2b).
Discharge rates of LC neurons following glutamate or DHPG administration into M1
Discharge rates of LC neurons following glutamate administration into ipsilateral M1 were studied in nine animals with a nerve injury and seven animals with a sham operation. All LC neurons studied were spontaneously active and gave an excitatory response to noxious pinch of the tail during preliminary characterization of response properties. Before drug injections, the mean discharge rate of LC neurons was 5.4 + 1.3 Hz (n = 20) in the sham-operated group and 6.6 + 1.7 Hz (n = 20) in the neuropathic group. Glutamate administration into M1 produced its maximum effect on on-going discharge rates of LC neurons 1–2 min following its injection and therefore, the discharge rates determined 60–120 s after injection were used in further statistical analyses. In nerve-injured animals, administration of glutamate into M1 produced a slight increase in the on-going discharge rate of LC neurons that was significant at a dose of 25 nmol but not at the dose of 2.5 nmol (paired t test; reference: the corresponding discharge rate 60–120 s after saline injection). In sham-operated animals, glutamate in M1 failed to influence discharge rates of LC neurons, independent of dose (2.5 and 25 nmol; Figs. 3, 4a).
Discharge rates of single LC cells following microinjection of saline and 25 nmol of glutamate (a) or 10 nmol of DHPG (b) into M1 in a sham control and neuropathic animal. In each graph, the line under “I” indicates the duration of microinjection. The order of injecting different compounds or doses was from top to bottom. The vertical calibration bar represents 20 impulses/s (a) or 30 impulses/s (b), and the horizontal calibration bar represents 60 s (a) or 180 s (b). Figure shows that the effects of glutamate or DHPG were minor ones
a Mean changes in the discharge rates of LC cells 1–2 min following injection of 2.5 or 25.0 nmol of glutamate (Glu) into M1. b Mean changes in the discharge rates of LC cells during the first 10 min following injection of 10 nmol of DHPG into M1. Sham sham control animal, Neurop neuropathic animal. In the Y-axis, 0 Hz represents the effect of saline injection into M1, and values >0 Hz indicate that glutamate or DHPG increased the discharge rate of cells. + P < 0.05, ++ P < 0.01 (paired t-test; reference: the corresponding saline group). Error bars represent SEM (in an = 20, in b nSham = 17 and nNeurop = 15)
Effect of cortically administered DHPG, a group I metabotropic glutamate receptor agonist (10 nmol), was studied in seven spinal nerve-ligated and six sham-operated animals. Microinjection of DHPG into M1 produced its maximum effect on neuronal activity in the LC during the first 10 min following its injection and therefore, the effect of DHPG was assessed 0–10 min following its injection. DHPG administration into M1 produced a slight increase in the discharge rates of LC neurons that was significant in the nerve-injured group and short of significance in the sham-operated group (paired t test; reference: the corresponding discharge rate 0–10 min after saline injection into M1; Figs. 3, 4b). During all injections, there was a short-lasting depression of activity that was observed with glutamate, DHPG as well as saline control (Fig. 3).
Discharge rates of LC neurons and heat-evoked responses of LC neurons following electric stimulation of M1
Influence of electric M1 stimulation on spontaneous discharge rates of LC neurons and their heat-evoked responses was separately studied in five spinal nerve-ligated animals. Heat stimulation of the nerve-injured hind paw significantly increased the discharge rate of LC neurons (F 1,26 = 21.07, P = 0.0001; 2-w-rmANOVA; Figs. 5, 6). Moreover, electric stimulation of M1 at an intensity of 30 μA produced a significant increase in the discharge rate of LC neurons (F 1,26 = 9.3, P = 0.0052; 2-w-rmANOVA), independent of heat stimulation (Interaction between heat and electric M1 stimulation: F 1,26 = 0.429).
Responses of one LC cell to heat without (a; 0 μA) and with (b; 30 μA) electric stimulation of M1, and to electric stimulation (30 μA) of M1 alone (c) in a neuropathic animal. In each column, the upper histogram shows the neuronal response and the middle curve shows the temperature of the thermode applied to the hind paw (from the baseline of 35°C to the peak temperature of 54°C). The deflections in the lowest curve show the limb withdrawal response (acceleration) determined with a piezoelectric device. The vertical calibration bars represent 60 impulses/s and the horizontal ones indicate the duration of electric stimulation (15 s). The arrows indicate the onset of the heat-evoked limb withdrawal
Mean baseline discharge rates and heat-evoked responses of LC cells, and their modulation by electric stimulation of the ipsilateral M1 in neuropathic animals. Stimulus intensity 0 μA represents a control condition without M1 stimulation. Error bars represent SEM (n = 27). */+ P < 0.05 (Tukey’s test; reference for *, the corresponding baseline value and for +, the corresponding value with M1 stimulation at the intensity of 0 μA)
Spinal antinociception induced by M1 stimulation following a block of the LC
To assess further whether LC is involved in spinal antinociception induced by electric stimulation of M1, lidocaine (4%, 0.5 μl) was microinjected into the ipsilateral LC, while heat-evoked withdrawal latency was determined in the ipsilateral hind limb. In the neuropathic group, the main effect by lidocaine treatment of LC on M1-induced spinal antinociception was not significant (Table 1; Fig. 7a). Additionally, the interaction between lidocaine treatment and M1 stimulation was not significant indicating that the blockade of the LC by lidocaine failed to attenuate M1-induced spinal antinociceptive effect in neuropathic animals. In the sham-operated group, the main effect by lidocaine treatment of LC and the interaction between lidocaine treatment and M1 stimulation were close to significance (Table 1; Fig. 7a).
Spinal antinociception induced by electric stimulation of M1 and an attempt to attenuate antinociception by administration of lidocaine (Lid; 4%, 0.5 μ) into the LC (a) or atipamezole (Ati; an α2-adrenoceptor antagonist; 5 μg) intrathecally (b) in neuropathic animals (Neurop) and sham control animals (Sham). Sal saline control. Error bars represent SEM (in a, n = 7, and in b, n = 8). */+ P < 0.05 (Tukey’s test; reference for *, the corresponding saline control value with M1 stimulation at the intensity of 0 μA and for +, the corresponding saline control value with M1 stimulation at the intensity of 30 μA). For further statistical analysis of the data, see Table 1
In summary, lidocaine block of the LC failed to produce a significant attenuation of M1-induced spinal antinociception in the neuropathic or the sham-operated group.
Spinal antinociception induced by M1 stimulation following a block of the spinal α2-adrenoceptors
Atipamezole, a α2-adrenoceptor antagonist (5.0 μg), was administered intrathecally to assess further whether descending noradrenergic projections acting on spinal α2-adrenoceptors and originating in the LC are involved in spinal antinociception induced by electric stimulation of M1. In the neuropathic group, neither the main effect of spinal atipamezole treatment on M1-induced spinal antinociception was significant, nor was the interaction between spinal atipamezole treatment and M1 stimulation significant (Table 1; Fig. 7b). In the sham-operated group, the main effect of spinal atipamezole treatment and the interaction between spinal atipamezole treatment and M1 stimulation were not significant (Table 1; Fig. 7b). In summary, blockade of spinal α2-adrenoceptors with atipamezole failed to produce a significant attenuation of M1-induced spinal antinociception in the sham-operated or neuropathic group.
Discussion
The present results indicate that electric stimulation of M1 in the rat produces spinal antinociception in nerve-injured as well as sham-operated control animals. In line with this, earlier studies showed that electric stimulation of M1 in healthy animals attenuates responses of nociceptive neurons in the spinal dorsal horn (Senapati et al. 2005) and spinal withdrawal reflex responses (Fonoff et al. 2009). Moreover, sensory abnormalities were reduced by electric M1 stimulation in animals with a chronic constriction injury of the sciatic nerve or dorsal root rhizotomy, as revealed by assessment of withdrawal reflex responses (Rusina et al. 2005; Vaculin et al. 2008).
While the earlier and present experimental animal studies show top–down antinociception by M1 stimulation, there are also some differences between the present and the earlier findings. In the present study, antinociception was primarily studied and found in the ipsilateral side. Some of the previous animal results indicate that M1 stimulation induces antinociception bilaterally (Senapati et al. 2005), whereas other studies report that M1 stimulation produces antinociception predominantly in the contralateral side (Fonoff et al. 2009; Rusina et al. 2005; Vaculin et al. 2008). Moreover, while M1 stimulation in the present study was equally effective in producing spinal antinociception in nerve-injured as sham-operated control animals, earlier findings suggest that M1 stimulation may suppress withdrawal reflex responses more effectively in nerve-injured than control animals (Vaculin et al. 2008). These differences in results may be explained by differences in the experimental conditions. In the present study, parameters for stimulation of M1 (0.1 ms pulses at 300 Hz for 10–15 s) were adopted from a previous study that reported ipsi- as well as contralateral spinal antinociception (Senapati et al. 2005), as the present study, whereas lower stimulus frequencies (25–60 Hz), longer pulse durations (0.2 ms), and considerably longer stimulation periods (>15 min) were used for cortical stimulation in studies reporting predominantly contralateral effects. It may be proposed that different stimulus parameters activate, at least partly, different pain modulatory mechanisms explaining differences in the results. Furthermore, differences between experimental animal models (spinal nerve-ligation model vs. chronic constriction injury or dorsal root rhizotomy model) and anesthetic conditions (light pentobarbitone anesthesia vs. awake) may contribute to differences between results obtained with neuropathic animals in the present and earlier studies (Rusina et al. 2005; Vaculin et al. 2008).
Role of the LC in descending antinociception induced by M1 stimulation
The noradrenergic LC (or A6), A5, and A7 cell groups in the pons provide noradrenergic innervation to the spinal cord (Kwiat and Basbaum 1992). There is abundant evidence indicating that descending noradrenergic pathways originating in the pons contribute to pain regulation, particularly to feedback inhibition of pain (see for review Pertovaara 2006). At the spinal cord level, the descending noradrenergic inhibition of pain-related responses is predominantly mediated by α2-adrenoceptors, although spinal α1-adrenoceptors may also play a role (Pertovaara 2006). In peripheral neuropathy, however, the role of descending noradrenergic pathways may be more complex. This is suggested by previous findings showing that in nerve-injured animals the noradrenergic system in general or the LC in particular may have not only anti- but also pronociceptive actions (Al-Adawi et al. 2002; Brightwell and Taylor 2009; Li et al. 2002; Viisanen and Pertovaara 2007; Wei and Pertovaara 2006).
A contribution of spinal noradrenergic receptors to the antinociceptive effect of M1 stimulation could be explained by activation of noradrenergic nuclei through direct M1 projections to the pontine region (Keizer et al. 1987) or through structures receiving M1 projections such as the midbrain (Catsman-Berrevoets and Kuypers 1981) and the medial bulboreticular formation (Keizer and Kuypers 1984) that have efferent connections to pontine noradrenergic nuclei (Bajic and Proudfit 1999; Sim and Joseph 1992). Moreover, other cortical areas might be indirectly activated by M1 stimulation (Peyron et al. 2007). For example, the prefrontal cortex has excitatory connections to the noradrenergic locus coeruleus (Jodo et al. 1998) and it could provide a link contributing to the activation of the noradrenergic system.
In the present study, stimulation of M1 increased neuronal discharge rates in the ipsilateral LC cells, particularly in nerve-injured animals. Since an increased discharge rate of LC neurons is expected to reflect enhancement of descending noradrenergic pain inhibition, this finding suggests that descending noradrenergic pathways may contribute to spinal antinociception induced by M1 stimulation. However, a failure to produce a significant attenuation of descending antinociception by lidocaine block of the LC or intrathecal administration of a α2-adrenoceptor antagonist in control or nerve-injured animals suggests that the descending noradrenergic system originating in the LC may not have a critical role in spinal antinociception induced by M1 stimulation. In line with this, while M1 stimulation did increase discharge rates of LC neurons, the increase was so small that it may not have been sufficient to produce a significant antinociceptive effect.
Other pathways potentially relaying antinociception induced by M1 stimulation
While the present results suggests that descending noradrenergic pathways do not have a major role in the M1-induced antinociception, there are several other descending systems that are known to be involved in pain regulation (Millan 2002; Pertovaara and Almeida 2006), that might be activated by M1 stimulation and that might explain descending antinociception in the present study. For example, M1 stimulation has produced release of endogenous opioids in the periaqueductal gray, a structure involved in descending opioidergic inhibition of pain (Maarrawi et al. 2007), and an opioid receptor antagonist has attenuated antinociception induced by M1 stimulation (Fonoff et al. 2009). M1 stimulation is known to induce a release of dopamine in the striatum (Strafella et al. 2003), a structure that contributes to descending control of neuropathic hypersensitivity (Ansah et al. 2007; Pertovaara and Wei 2008). Since electric stimulation of the dopaminergic, A11 cell group in the hypothalamus has produced spinal antinociception both in healthy control and in neuropathic animals (Fleetwood-Walker et al. 1988; Wei et al. 2009), it is among potential alternative relay nuclei contributing to descending antinociception originating in M1. Additionally, among the potential relay nuclei is the rostroventromedial medulla that has a bidirectional role in pain control and that has a major role in brainstem-spinal modulation of pain (Fields et al. 2006; Gebhart 2004). While the present findings still leave open which descending pathways are critical for M1-induced spinal antinociception, the results suggest that repetitive electric stimulation of M1 is a more effective way for activation of corticofugal pathways than administration of a single bolus of glutamate or DHPG into M1.
The present experimental animal study focused on descending control of spinal nociception. It should be noted that in clinical studies, pain alleviation by M1 stimulation may be based not only on spinal but also on supraspinal actions that influence higher processing of nociceptive signals such as emotional appraisal of pain (Garcia-Larrea and Peyron 2007; Ohara et al. 2005).
Conclusions
The results of this study indicate that stimulation of M1 has a spinal antinociceptive effect in neuropathic and control animals. M1 stimulation activates LC neurons, but since local anesthesia of LC and a blockade of spinal α2-adrenoceptors failed to reverse M1-induced spinal antinociception, LC or its descending noradrenergic pathways may not have a major role in the spinal antinociceptive effect induced by stimulation of M1. Due to significant differences in corticofugal pathways between man and rat, one should, however, be cautious when applying these results obtained in the rat to human patients.
Abbreviations
- DHPG:
-
3,5-Dihydroxyphenylglycine
- LC:
-
Locus coeruleus
- M1:
-
Primary motor cortex
- 1-w- or 2-w-rmANOVA:
-
One- or two-way repeated measures analysis of variance
References
Al-Adawi S, Dawe GS, Bonner A, Stephenson JD, Zarei M (2002) Central noradrenergic blockade prevents autotomy in rat: implication for pharmacological prevention of posdenervation syndrome. Brain Res Bull 57:581–586
Ansah OB, Leite-Almeida H, Wei H, Pertovaara A (2007) Striatal dopamine D2 receptors attenuate neuropathic hypersensitivity in the rat. Exp Neurol 205:536–546
Ansah OB, Gonçalves L, Almeida A, Pertovaara A (2009) Enhanced pronociception by amygdaloid group I metabotropic glutamate receptors in nerve-injured animals. Exp Neurol 216:66–74
Bajic D, Proudfit HK (1999) Projections of neurons in the periaqueductal gray to pontine and medullary catecholamine cell groups involved in the modulation of nociception. J Comp Neurol 405:359–379
Basso MA, Evinger C (1996) An explanation for reflex blink hyperexcitability in Parkinson’s disease. II. Nucleus raphe magnus. J Neurosci 16:7318–7330
Basso MA, Powers AS, Evinger C (1996) An explanation for reflex blink hyperexcitability in Parkinson’s disease. I. Superior colliculus. J Neurosci 16:7308–7317
Brightwell JJ, Taylor BK (2009) Noradrenergic neurons in the locus coeruleus contribute to neuropathic pain. Neuroscience 160:174–185
Canedo A (1997) Primary motor cortex influences on the descending and ascending systems. Prog Neurobiol 51:287–335
Catsman-Berrevoets CE, Kuypers HG (1981) A search for corticospinal collaterals to thalamus and mesencephalon by means of multiple retrograde fluorescent tracers in cat and rat. Brain Res 218:15–33
Fields HL, Basbaum AI, Heinricher MM (2006) Central nervous system mechanisms of pain modulation. In: McMahon SB, Koltzenburg M (eds) Wall and Melzack’s textbook of pain, 5th edn. Elsevier, China, pp 125–142
Fleetwood-Walker SM, Hope PJ, Mitchell R (1988) Antinociceptive actions of descending dopaminergic tracts on cat and rat dorsal horn somatosensory neurones. J Physiol (Lond) 399:335–348
Fonoff ET, Dale CS, Pagano RL, Paccola CC, Ballester G, Teixeira MJ, Giorgi R (2009) Antinociception induced by epidural motor cortex stimulation in naive conscious rats is mediated by the opioid system. Behav Brain Res 196:63–70
Garcia-Larrea L, Peyron R (2007) Motor cortex stimulation for neuropathic pain: From phenomenology to mechanisms. Neuroimage 37(Suppl 1):S71–S79
Gebhart GF (2004) Descending modulation of pain. Neurosci Biobehav Rev 27:729–737
Hirata H, Aston-Jones G (1994) A novel long-latency response of locus coeruleus neurons to noxious stimuli: mediation by peripheral C-fibers. J Neurophysiol 71:1752–1761
Hosomi K, Saitoh Y, Kishima H, Oshino S, Hirata M, Tani N, Shimokawa T, Yoshimine T (2008) Electric stimulation of primary motor cortex within the central sulcus for intractable neuropathic pain. Clin Neurophysiol 119:993–1001
Jodo E, Chiang C, Aston-Jones G (1998) Potent excitatory influence of prefrontal cortex activity on noradrenergic locus coeruleus neurons. Neuroscience 83:63–79
Johnson S, Summers J, Pridmore S (2006) Changes in somatosensory detection and pain thresholds following high frequency repetitive TMS of the motor cortex in individuals suffering from chronic pain. Pain 123:187–192
Joosten EA, Schuitman RL, Vermelis ME, Dederen PJ (1992) Postnatal development of the ipsilateral corticospinal component in rat spinal cord: a light and electron microscopic anterograde HRP study. J Comp Neurol 326:133–146
Keizer K, Kuypers HG (1984) Distribution of corticospinal neurons with collaterals to lower brain stem reticular formation in cat. Exp Brain Res 54:107–120
Keizer K, Kuypers HG, Ronday HK (1987) Branching cortical neurons in cat which project to the colliculi and to the pons: a retrograde fluorescent double-labeling study. Exp Brain Res 67:1–15
Kim SH, Chung JM (1992) An experimental model for peripheral neuropathy produced by segmental spinal nerve ligation in the rat. Pain 50:355–363
Kwiat GC, Basbaum AI (1992) The origin of brainstem noradrenergic and serotoninergic projections to the spinal cord dorsal horn in the rat. Somatosens Mot Res 9:157–163
Lazorthes Y, Sol JC, Fowo S, Roux FE, Verdie JC (2007) Motor cortex stimulation for neuropathic pain. Acta Neurochir 97(Suppl):37–44
Lefaucheur JP (2006) The use of repetitive transcranial magnetic stimulation (rTMS) in chronic neuropathic pain. Neurophysiol Clin 36:117–124
Li X, Conklin D, Ma W, Zhu X, Eisenach JC (2002) Spinal noradrenergic activation mediates allodynia reduction from an allosteric adenosine modulator in a rat model of neuropathic pain. Pain 97:117–125
Maarrawi J, Peyron R, Mertens P, Costes N, Magnin M, Sindou M, Laurent B, Garcia-Larrea L (2007) Motor cortex stimulation for pain control induces changes in the endogenous opioid system. Neurology 69:827–834
McGeorge AJ, Faull RL (1989) The organization of the projection from the cerebral cortex to the striatum in the rat. Neuroscience 29:503–537
Millan MJ (2002) Descending control of pain. Prog Neurobiol 66:355–474
Nguyen JP, Lefaucheur JP, Decq P, Uchiyama T, Carpentier A, Fontaine D, Brugieres P, Pollin B, Feve A, Rostaing S, Cesaro P, Keravel Y (1999) Chronic motor cortex stimulation in the treatment of central and neuropathic pain. Correlations between clinical, electrophysiological and anatomical data. Pain 82:245–251
Ohara PT, Vit JP, Jasmin L (2005) Cortical modulation of pain. Cell Mol Life Sci 62:44–52
Paxinos G, Watson C (1998) The rat brain in stereotaxic coordinates. Academic Press, Sydney
Pertovaara A (2006) Noradrenergic pain modulation. Prog Neurobiol 80:53–83
Pertovaara A, Almeida A (2006) Endogenous pain modulation. Descending inhibitory systems. In: Cervero F, Jensen TS (eds) Handbook of clinical neurology, vol 81. Elsevier, Amsterdam, pp 179–192
Pertovaara A, Wei H (2008) Dual influence of the striatum on neuropathic hypersensitivity. Pain 137:50–59
Pertovaara A, Haapalinna A, Sirviö J, Virtanen R (2005) Pharmacological properties, central nervous system effects, and potential therapeutic applications of atipamezole, a selective α2-adrenoceptor antagonist. CNS Drug Rev 11:273–288
Peyron R, Faillenot I, Mertens P, Laurent B, Garcia-Larrea L (2007) Motor cortex stimulation in neuropathic pain. Correlations between analgesic effect and hemodynamic changes in the brain. A PET study. Neuroimage 34:310–321
Rusina R, Vaculin S, Yamamotova A, Barek S, Dvorakova H, Rokyta R (2005) The effect of motor cortex stimulation in deafferentated rats. NeuroEndocrinol Lett 26:283–288
Sandkühler J, Gebhart GF (1984) Relative contributions of the nucleus raphe magnus and adjacent medullary reticular formation to the inhibition by stimulation in the periaqueductal gray of a spinal nociceptive reflex in the pentobarbital-anesthetized rat. Brain Res 305:77–87
Senapati AK, Huntington PJ, Peng YB (2005) Spinal dorsal horn neuron response to mechanical stimuli is decreased by electric stimulation of the primary motor cortex. Brain Res 1036:173–179
Sim LJ, Joseph SA (1992) Efferent projections of the nucleus raphe magnus. Brain Res Bull 28:679–682
Størkson RV, Kjørsvik A, Tjølsen A, Hole K (1996) Lumbar catheterization of the spinal subarachnoid space in the rat. J Neurosci Methods 65:167–172
Strafella AP, Paus T, Fraraccio M, Dagher A (2003) Striatal dopamine release induced by repetitive transcranial magnetic stimulation of the human motor cortex. Brain 126:2609–2615
Summers J, Johnson S, Pridmore S, Oberoi G (2004) Changes to cold detection and pain thresholds following low and high frequency transcranial magnetic stimulation of the motor cortex. Neurosci Lett 368:197–200
Tsubokawa T, Katayama Y, Yamamoto T, Hirayama T, Koyama S (1991) Chronic motor cortex stimulation for the treatment of central pain. Acta Neurochir (Wien) 52(Suppl):137–139
Vaculin S, Franek M, Yamamotova A, Rokyta R (2008) Motor cortex stimulation in rats with chronic constriction injury. Exp Brain Res 185:331–335
Valmunen T, Pertovaara A, Taiminen T, Virtanen A, Parkkola R, Jääskeläinen SK (2009) Modulation of facial sensitivity by navigated rTMS in healthy subjects. Pain 142:149–158
Viisanen H, Pertovaara A (2007) Influence of peripheral nerve injury on response properties of locus coeruleus neurons and coeruleospinal antinociception in the rat. Neuroscience 146:1785–1794
Wei H, Pertovaara A (2006) Spinal and pontine α2-adrenoceptors have opposite effects on pain-related behavior in the neuropathic rat. Eur J Pharmacol 551:41–49
Wei H, Viisanen H, Pertovaara A (2009) Descending modulation of neuropathic hypersensitivity by dopamine D2 receptors in or adjacent to the hypothalamic A11 cell group. Pharmacol Res 59:355–363
Acknowledgments
We wish to thank Dr. H. Wei for her help with surgery. The authors were supported by grants from the Lilly Finland Foundation (HV), the Finnish Cultural Foundation (HV), the Academy of Finland (AP) and the Sigrid Jusélius Foundation (AP), Helsinki, Finland.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Viisanen, H., Pertovaara, A. Antinociception by motor cortex stimulation in the neuropathic rat: does the locus coeruleus play a role?. Exp Brain Res 201, 283–296 (2010). https://doi.org/10.1007/s00221-009-2038-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-009-2038-4