Abstract
Recently, it was shown that patients have different functional activation patterns within affected primary sensorimotor cortex (SMC) after intensive rehabilitation therapy. This individual difference was supposed to depend on the integrity of the cortico-spinal fibres from the primary motor cortex. In this study, we considered whether patients with different fMRI activation patterns after intensive rehabilitation therapy suffered from different cortico-spinal fibre lesions. To comprehend this circumstance a lesion subtraction analysis was used. To verify these results with the use of transcranial magnetic stimulation motor evoked potentials was also derived. Patients were treated after a modified version of constraint-induced movement therapy (modCIMT; 3 h daily for 4 weeks). Increased and decreased SMC activation showed similar individual patterns as described previously. These activation differences depend on the integrity of the cortico-spinal tract, which was measured via lesion subtraction analysis between patient groups, and was supported by affected motor evoked potentials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Functional imaging methods have been used to understand reorganisation patterns after rehabilitation therapies, e.g., constraint-induced movement therapy (CIMT). Although identical treatment protocols were used, activation patterns in different patients varied in different imaging studies (Schaechter et al. 2002; Johansen-Berg et al. 2002; Wittenberg et al. 2003; Szaflarski et al. 2006; Hamzei et al. 2006; for review see Mark et al. 2006). Until now, a clear concept behind the previously described reorganization patterns due to intensive rehabilitation therapy (CIMT; 6 h daily training for 2 weeks) has been lacking. These divergent findings suggest large interindividual variability or reflect different reorganization mechanisms in different patients. Therefore, the focus on single subjects is important to define interindividual variability. This was done in a previous investigation. Single subject analysis revealed two different activation patterns within the ipsilesional primary sensorimotor cortex (SMC) after CIMT. This difference was presumed to depend on the integrity of the cortico-spinal fibres from the primary motor cortex (Hamzei et al. 2006).
In this study, we investigated whether patients with different SMC activation changes (increase and decrease) after intensive hand motor training within affected hemispheres have different cortico-spinal fibre deficits. Chronic stroke patients were investigated with no further spontaneous motor improvement. Since patients’ hand functions improved after modCIMT (a modified version of CIMT with 3 h daily training for 4 weeks). Dettmers et al. (2005) expected an increased and decreased “blood oxygenation level dependent” (BOLD) signal activity within affected SMC and presume that these two activation changes depend on the integrity of the cortico-spinal fibres. We performed a lesion subtraction analysis depending on the group affinity (patients with increased were compared with those with decreased SMC activation). Furthermore, we investigated motor evoked potentials to verify the results of our lesion subtraction analysis.
Methods
Patients
From 16 patients who were screened (their data are not presented), eight right-handed patients (three females and five males; mean age 57.5 years; range 38–69 years) were included in this study. They were at least two years post-stroke (see Table 1). All patients suffered from an ischemic lesion.
Inclusion criteria consisted of at least active 20° extension of the affected wrist and 10° extension of each finger; onset of stroke more than one year before starting modCIMT; ability to walk without balance problems while wearing a constraint device. Exclusion criteria were hemodynamically relevant intra- or extracranial artery stenosis in Doppler ultrasound, which may alter the BOLD response (Hamzei et al. 2003a); cognitive impairments or aphasia that could compromise the questionnaire’s comprehension, attention deficits, serious uncontrolled medical problems, pace makers, and spasticity (Ashworth scale = 0).
We were interested in the course of motor function tests and fMRI activation changes within the affected SMC (post-therapy vs. pre-therapy, and vice versa comparisons that reveal increase, decrease, or no activation changes). To elucidate SMC activation behaviour after therapy (increase, decrease or no activation changes) a lesion subtraction analysis was performed using structural MRI. Therefore, lesions of patients groups were superimposed and then compared. Motor evoked potentials (MEP) were performed using transcranial magnetic stimulation (TMS) to assess pyramidal tract integrity. These tests will be described in the following.
Clinical assessments
A physical examination was performed to determine patient eligibility for the experiment 4 weeks prior to the study. If subjects were considered for the therapy, they received an explanation of project procedures and signed informed consent was obtained. Motor function tests were applied that have been previously used in clinical CIMT studies (Taub et al. 1993; Wolf et al. 1989, 2006; Miltner et al. 1999; Dettmers et al. 2005; Rijntjes et al. 2005). Before and after modCIMT, a Motor Activity Log (MAL) interview was carried out to determine the Amount of Use (MAL-AoU) and Quality of Movement (MAL-QoM) of the affected arm as rated by the patient (Taub et al. 1993). The physiotherapist performed the Wolf Motor Function Test (WMFT; Wolf et al. 1989; Taub et al. 1993) with Functional Ability (WMFT-FA), and number of seconds needed for these tests (WMFT-sec), as measured with a stop-watch. For the WMFT-sec the time for the subtests was measured and the average of the number of seconds for all subtests was calculated. For the WMFT-FA, video sequences were recorded and presented for evaluation to a second physiotherapist, who was blinded to the time point of recording, as described previously (Dettmers et al. 2005; Rijntjes et al. 2005). The average of all evaluated subtests of WMFT-FA was measured. In order to test clinical efficacy we compared MAL-QoM, MAL-AoU and WMFT (WMFT-FA, WMFT-sec) using a nonparametric Wilcoxon test before (“pre-therapy”) and after (“post-therapy”) modCIMT. Threshold was set at P < 0.05. “Effect sizes” were measured by using the “Cohen’s” d′ (small effect with d′ = 0.14, medium d′ = 0.36, large d′ = 0.57; Cohen 1988, see also Taub et al. 2006a).
Intervention
Patients received intensive daily motor activity training for 3 h a day under physiotherapeutic supervision for 20 consecutive weekdays. To force patients to use the affected hand, the non-affected hand was placed in a splint during the training period and outside the training session (for 90% of waking hours). Treatment was focussed on housekeeping activities (e.g., eating, opening and closing jars and spring-loaded clothespins).
Functional MRI
The following conditions were investigated the day before starting CIMT (“pre-therapy”) and the day after CIMT (“post-therapy”): rest scans with eyes closed served as a low-level baseline condition (REST). Two active conditions included right and left passive wrist joint movements. Passive hand movements have been found to induce almost identical patterns of activation compared to active movements in healthy subjects and stroke patients (Weiller et al. 1996; Lee et al. 1998; Loubinoux et al. 2001; Tombari et al. 2004). Its activation pattern is reliable over a time period of several weeks to months (Tombari et al. 2004; Nelles et al. 2001; Loubinoux et al. 2003; Ward et al. 2006). We chose passive instead of active hand movements, because its performance is identical during follow-up and it is independent of individual performance and clinical improvement. All conditions were presented in a pseudo-randomised order. There were four epochs/cycles, each containing the experimental conditions alternating with rest conditions with no gap between epochs (right hand, Rest, left hand, Rest, left hand, Rest….). Each condition lasted 31 s. Right and left hands were manually moved with an examiner within the scanner room. Dorsal extensions and plantar flexions of the wrist (0–50°) were performed three times (with acoustical signals) for 3.1 s, 30 times within each cycle. The signal for a hand movement was given by an acoustical noise via headphone to the examiner who moved the hand. This acoustical task was controlled by a PC running “Presentation” software (Neurobehavioral System, http://www.neurobehavioralsystems.com). The amplitude of the passive hand movement was limited by the physiological dorsal extension of the hand (50°) in the absence of spasticity (Ashworth scale = 0; for further detail see (Hamzei et al. 2006). The forearm was fixated and only a dorsal extension of the hand was performed. Before scanning, subjects underwent passive hand movements in the MR environment in order to learn to avoid active movements of the hand and movement artefacts of the head. Surface EMG electrodes were positioned on the dorsal interosseus muscle I and on the extensor digitorum communis muscle and the contraction of arm or hand muscles activated an acoustic signal. MRI acquisition was performed when patients were able to relax their arm and hand during the introduction time.
Data acquisition
T2*-weighted functional magnetic resonance images were acquired on a 1.5 Tesla Magnetom VISION whole-body MRI system (Siemens, Erlangen, Germany) equipped with a standard head coil. Contiguous multi-slice echo planar images (TE 60 ms) were obtained in axial orientation. 30 slices (3 mm thickness) were acquired every 3.1 s. Voxel size was 3.28 × 3.28 mm (64 × 64 pixel) and the field of view was 210 × 210 mm. A total of 160 image volumes were acquired over a time period of approximately 9 min.
Data processing and statistics
Data were processed with SPM5 to assess BOLD signal intensity. All volumes were realigned to the first volume (Friston et al. 1995a). Residual motion effects were eliminated by a regression of the time course of each voxel on a periodic function of estimated movement parameters. A mean image was created using realigned volumes. An individual 3-D T1-weighted MRI (1 × 1 × 1 mm voxel size) was coregistered to this mean image. This ensured that functional and structural images were spatially aligned. The functional images and the structural T1-volumes were spatially normalised (Friston et al. 1995b) to templates in a space defined by a template from the Montreal Neurological Institute (Evans et al. 1994), using 12 affine parameters and a set of non-linear basis functions. Since normalization in patients with large lesions might lead to incorrect normalization, we made a mask of the lesion and included it in this procedure. Functional data were smoothed using a 9 mm full-width at half maximum (FWHM) filter in individual subject analyses to compensate for residual variability after spatial normalisation. This also facilitated the application of Gaussian random field theory to provide for corrected statistical inference (Friston et al. 1995a). Data analysis was performed by modelling the different conditions as reference waveforms (i.e., box-car functions convolved with a hemodynamic response function) in the context of the general linear model (Friston et al. 1995b, 1997). A high-pass filter was applied to the data to minimise the effects of aliased physiological noise. We tested for significant effects using voxelwise t statistics assembled into a statistical parametric map. The images of patients with right-sided infarcts were flipped about the mid-sagittal line, such that all subjects were considered to have left-sided infarcts.
To investigate activation changes over time (increase, decreased or no activation changes) the BOLD signal intensity during passive hand movement of each investigation day was calculated as a session mean and compared against each other (“pre-therapy vs. post-therapy” and “post-therapy vs. pre-therapy”) in individual subjects.
We were particularly interested in activation changes in the affected SMC. This region and other motor areas were identified as follows: primary motor cortex as the cortex lying immediately anterior to the central sulcus and primary somatosensory cortex as the cortex lying immediately posterior to the central sulcus and anterior to the postcentral sulcus (Fink et al. 1997; Hamzei et al. 2003b).
To test whether BOLD signal changes between both investigation days are contingent on changes on the REST condition, we also compared the REST condition between both investigation days.
The threshold for group analysis (motor tests and fMRI) was set at P < 0.05, corrected for multiple comparisons. In the case of SMC, we had a regional specific hypothesis (Hamzei et al. 2006); therefore, correction for multiple comparisons in the single subject analysis for the categorical comparisons between investigations days (“pre-therapy vs. post-therapy” and vice versa) was based on the volume of interest (within a sphere of 9 mm). In all single subject analysis cases, the threshold was set at P < 0.05 (corrected for multiple comparisons).
Transcranial magnetic stimulation (TMS)
The integrity of the pyramidal tract from primary motor cortex was investigated with TMS. TMS was performed with a circular coil (Dantec, Germany) to quantify central motor conduction times (CMCT) and maximum motor evoked potential (MEP) amplitudes in all subjects. Electrical stimulation of the median nerve was applied to measure M response latencies, F wave latencies and M response amplitudes. Recordings were obtained with surface electrodes from the abductor pollicis brevis muscle on both sides. The hotspot of the abductor pollicis brevis muscle was stimulated. CMCT was calculated by: total latency − (M-response latency + F-wave latency − 1)/2. The maximal MEP amplitude was expressed as the percentage of the maximal M response amplitude. Before TM stimulation patients were asked for maximal innervations of the APB muscle. Thereafter, they innervated their APB muscle for 10% of the maximal innervations (tonic pre-innervation). TMS was performed with a stimulator intensity 25% above the individual motor threshold during tonic pre-innervation of the target muscle. Recordings were stored on a Viking IV (Nicolet, Kleinostheim, Germany) and analysed off-line. According to normal values from our laboratory the upper normal limit of CMCT was 8.5 ms. This procedure has been described elsewhere (Hamzei et al. 2006).
Lesion subtraction analysis
Previously, lesion localisation has been thought to be responsible for different BOLD signal activation courses after CIMT (Hamzei et al. 2006). Therefore, to acknowledge to SMC activation changes (increase, decrease or no activation changes) patient data were collected as a group. First the lesions of one group are added together, creating an overlap image showing the regions of common involvement. Finally, lesions from another group are subtracted, creating an image that shows regions that are damaged in one group more than in the other group. All lesions were mapped using free MRIcro (http://www.mricro.com) software distribution (Rorden and Brett 2000). The procedure of the lesion subtraction analysis has been described previously (Karnath et al. 2004).
Results
Clinical assessments
Amount of daily use (MAL-AoU; P < 0.017), Quality of movement (MAL-QoM; P < 0.025) and Wolf Motor Function Test with Functional Ability (WMFT-FA; P < 0.012) and number of seconds needed for these tests (WMFT-sec; P < 0.012) improved significantly after modCIMT. The “Effect sizes” were large in all tests (MAL-AoU with Cohen’s d′ = 1.54; MAL-QoM with d′ = 1.1; WMFT-FA d′ = 1.18 and WMFT-sec d′ = 0.61).
Functional MRI
No patient was excluded because of active hand movements during the session time or head movement artefacts (the estimated head movement did not exceed 2 mm). In a group analysis, the BOLD signal intensity within the affected SMC did not differ between both investigation days (P < 0.8).
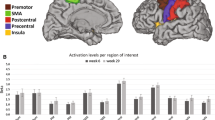
Two groups of patients were identified in a single subject analysis (Fig. 1): subjects with a decreased BOLD signal (or focusing) within the affected SMC (patients 1, 2, 3, and 4; paired-t test: P < 0.034; Groupdec) and patients (numbers 5, 6, 7 and 8) with activation increase (or recruitment; Groupinc) after therapy (P < 0.013; Fig. 1). The number of voxels was also reduced corresponding to activation changes (in case of decreased BOLD signal) and increased (in patients with increasing SMC activation) within ipsilesional SMC after modCIMT. There were no differences of REST conditions between both investigation days within the motor network.
FMRI activation of patients is superimposed on individual T1-weighted MRI. Patients 1, 2, 3 and 4 showed a decreased (focusing) BOLD signal after therapy. This was demonstrated by the categorical comparison between pre-therapy vs. post-therapy time. For patients 3 and 4 activation of each investigation day was superimposed on each other (red for activation before starting therapy, green for activation after therapy and yellow for common area of activation). Patients 5, 6, 7 and 8 showed an increased (recruitment) BOLD signal after motor practice. Post-therapy vs. pre-therapy showed activation within affected SMC (arrow marks the central sulcus in the affected hemisphere). Activation of all investigation days was overlaid on each other for patients 7 and 8 (red for activation before, green for activation after therapy, yellow for common activation)
Lesion subtraction analysis and fMRI
To acknowledge activation changes, lesion localisations of patients within each group (Groupdec and Groupinc) were superimposed, creating an overlap image showing the regions of common involvement. A lesion subtraction analysis between these two groups showed a greater lesion in the affected SMC and internal capsule in Groupinc. Within the internal capsule there was an area more often affected in this group of patients amongst others regions, which is known to contain fibres from the primary motor cortex (Fries et al. 1993; Morecraft et al. 2002) (see Fig. 2).
Individual lesions of patients with increased SMC activation (Groupinc) and those with activation decrease (Groupdec) are superimposed (view of few transversal slices). The lesion subtraction analysis between these two groups demonstrated larger lesions in the affected primary motor cortex and internal capsule in Groupinc
TMS
MEP and CMCT of Groupinc showed extensively delayed MEP and CMCT in comparison to Groupdec with delayed MEP and CMCT to a lesser extent (see Table 1). The two-sample-t test between Groupdec and Groupinc showed a significant difference of MEPs (P < 0.0003) and CMCT (P < 0.0008).
In previous TMS studies, a predictive value of intact MEP has been shown in stroke patients (e.g. Pereon et al. 1995; Wohrle et al. 2004; Escudero et al. 1998; Stinear et al. 2007). Therefore, we tested in a post hoc analysis whether Groupinc and Groupdec (with different MEPs) showed any differences in motor performance first at the time point before starting modCIMT and then in comparison between pre-therapy vs. post-therapy tests. Clinical assessments at the time point “pre-therapy” were compared between these groups to analyse whether there were any clinical differences at inception. Then, the outcome scores (comparison between pre-therapy and post-therapy tests) were also compared to analyse whether the outcomes differed between these two groups. These two post hoc analyses showed statistical differences neither in initial clinical assessments at inception nor in outcome scores.
Discussion
The major finding of this study was that activation changes within the SMC of the lesioned hemisphere in individual subject depend on the integrity of the cortico-spinal tract. Patients (Groupinc) with BOLD signal increases (or “recruitment”) showed more pronounced pyramidal tract lesions in comparison to Groupdec with BOLD signal activity decreases (or “focusing”).
SMC activation changes after modCIMT are very similar those observed after classical CIMT (Hamzei et al. 2006). This might suggest that the cortical reorganization strategy is rather independent of daily training time, when the total amount of training duration is similar (modCIMT with reduced daily training was extent across a longer time period). This conclusion does not rule out the possibility that there might be activation differences in direct comparisons between modCIMT and CIMT (in analogue to functional difference; Sterr et al. 2002). Probably, there is a critical threshold of training duration (less than 3 h or more than 6 h) which affects SMC activation and functional improvement in a different manner as presented here and elsewhere (Sterr et al. 2002; Dettmers et al. 2005; Rijntjes et al. 2005; Hamzei et al. 2006).
We suggest that the integrity of pyramidal tract is the strongest predictor for recruitment or focusing of activation within affected SMC. This observation confirmed the hypothesis of Ward and colleagues that the integrity of the pyramidal tract influences activation patterns within the ipsilesional SMC (Ward et al. 2006). Ward’s study referred to subacute stroke patients and the present data are only partially comparable, because our patients are in a chronic stable phase. But comparable findings support the idea of a “reorganization-model”, that the integrity of the pyramidal tract determines activation patterns within ipsilesional SMC (Fig. 3).
In this context a further aspect should be considered: until now, it was generally suggested that reorganization patterns depend on whether fibres (“subcortical”) or neurons (“cortical”) are damaged after a stroke. For example, most studies with lesions within internal capsules were generally collected as “subcortical infarct”, irrespective whether pyramidal tracts from the premotor cortex (lateral and medial) or primary motor cortex were affected. Fries et al. (1993) and Morecraft et al. (2002) in humans and in non-human primates showed that fibres from the primary motor cortex pass through the middle third of the posterior limb of the internal capsule. As described above, we believe that the integrity of the pyramidal tract from the primary motor cortex (irrespective of whether fibres or cortex are damaged) influences reorganization patterns within the ipsilesional SMC. This aspect was also previously demonstrated with the use of diffusion-weighted imaging and probabilistic tractography after stroke. Disruption of cortico-spinal fibres influenced functional activation patterns in three patients with subcortical strokes (Newton et al. 2006). Therefore, similar findings would be expected after a cortical lesion.
To consider interindividual variability the number of patients within subgroup analyses decreases, therefore future investigations are necessary to replicate the present results. One further limiting factor of this view could be the fact, that the observed interhemispheric inhibition with different impairment depends on cortical or subcortical strokes (Niehaus et al. 2003; Murase et al. 2004; Liepert et al. 2000). We did not investigate the effect of the interhemispheric inhibition. Therefore, additional mechanisms might affect reorganization. However, this should be addressed in future investigations. Also of interest could be an investigation of long term patient outcomes to find out whether the motor improvements seen in patients with activation recruitment (and more pronounced pyramidal tract lesions) persists for a long time period, as previously described in clinical CIMT studies (Taub et al. 2006b; Wolf et al. 2006).
Abbreviations
- BOLD:
-
Blood oxygenation level dependent
- CIMT:
-
Constraint-induced movement therapy
- CMCT:
-
Central motor conduction times
- fMRI:
-
Functional magnetic resonance imaging
- MAL-AoU:
-
Motor activity log with amount of use
- MAL-QoM:
-
Motor activity log with quality of movement
- MEP:
-
Motor evoked potentials
- modCIMT:
-
Modified version of constraint-induced movement therapy
- SMC:
-
Primary sensorimotor cortex
- TMS:
-
Transcranial magnetic stimulation
- WMFT-FA:
-
Wolf motor function test with functional ability
- WMFT-sec:
-
Wolf motor function test with number of seconds
References
Cohen J (1988) Statistical power analysis for the behavioral science. Lawerance Erlbaum Associates, Hillsdale
Dettmers C, Teske U, Hamzei F, Uswatte G, Taub E, Weiller C (2005) Distributed form of constraint-induced movement therapy improves functional outcome and quality of life after stroke. Arch Phys Med Rehabil 86:204–209
Escudero JV, Sancho J, Bautista D, Escudero M, Lopez-Trigo J (1998) Prognostic value of motor evoked potential obtained by transcranial magnetic brain stimulation in motor function recovery in patients with acute ischemic stroke. Stroke 29:1854–1859
Evans AC, Kamber M, Collins DL, Macdonald D (1994) An MRI-based probabilistic atlas of neuroanatomy. In: Shorvon S, Fish D, Andermann F, Bydder GM, Stefan H (eds) Magnetic resonance scanning and epilepsy. Plenum, New York, pp 263–274
Fink GR, Frackowiak RS, Pietrzyk U, Passingham RE (1997) Multiple nonprimary motor areas in the human cortex. J Neurophysiol 77:2164–2174
Fries W, Danek A, Scheidtmann K, Hamburger C (1993) Motor recovery following capsular stroke. Role of descending pathways from multiple motor areas. Brain 116:369–382
Friston KJ, Ashburner J, Frith CD, Poline J-B, Heather JD, Frackowiak RS (1995a) Spatial registration and normalization of images. Hum Brain Map 2:1–25
Friston KJ, Holmes AP, Worsley KJ, Poline JB, Frith CD, Frackowiak RS (1995b) Statistical parametric maps in functional imaging: a general linear approach. Hum Brain Map 2:189–210
Friston KJ, Ashburner J, Poline JB, Frith CD, Heather JD, Frackowiak RS (1997) Spatial realignment and normalization of images. Hum Brain Map 2:165–189
Hamzei F, Knab R, Weiller C, Rother J (2003a) The influence of extra- and intracranial artery disease on the BOLD signal in FMRI. Neuroimage 20:1393–1399
Hamzei F, Rijntjes M, Dettmers C, Glauche V, Weiller C, Büchel C (2003b) The human action recognition system and its relationship to Broca’s area: an fMRI study. Neuroimage 19:637–644
Hamzei F, Liepert J, Dettmers C, Weiller C, Rijntjes M (2006) Two different reorganization patterns after rehabilitative therapy: an exploratory study with fMRI and TMS. Neuroimage 31:710–720
Johansen-Berg H, Dawes H, Guy C, Smith SM, Wade DT, Matthews PM (2002) Correlation between motor improvements and altered fMRI activity after rehabilitative therapy. Brain 125:2731–2742
Karnath HO, Fruhmann Berger M, Kuker W, Rorden C (2004) The anatomy of spatial neglect based on voxelwise statistical analysis: a study of 140 patients. Cereb Cortex 14:1164–1172
Lee CC, Jack CR Jr, Riederer SJ (1998) Mapping of the central sulcus with functional MR: active versus passive activation tasks. AJNR 19:847–852
Liepert J, Storch P, Fritsch A, Weiller C (2000) Motor cortex disinhibition in acute stroke. Clin Neurophysiol 111:671–676
Loubinoux I, Carel C, Alary F, Boulanouar K, Viallard G, Manelfe C, Rascol O, Chollet F (2001) Within-session and between session reproducibility of cerebral sensorimotor activation: a test–retest effect evidenced with functional magnetic resonance imaging. J Cereb Blood Flow Meta 21:592–607
Loubinoux I, Carel C, Pariente J, Dechaumont S, Albucher JF, Marque P, Manelfe C, Chollet F (2003) Correlation between cerebral reorganization and motor recovery after subcortical infarcts. NeuroImage 20:2166–2180
Mark VW, Taub E, Morris DM (2006) Neuroplasticity and constraint-induced movement therapy. Eura Medicophys 42:269–284
Miltner WH, Bauder H, Sommer M, Dettmers C, Taub E (1999) Effects of constraint-induced movement therapy on patients with chronic motor deficits after stroke: a replication. Stroke 30:586–592
Morecraft RJ, Herrick JL, Stilwell-Morecraft KS, Louie JL, Schroeder CM, Ottenbacher JG, Schoolfield MW (2002) Localization of arm representation in the corona radiata and internal capsule in the non-human primate. Brain 125:176–198
Murase N, Duque J, Mazzocchio R, Cohen LG (2004) Influence of interhemispheric interactions on motor function in chronic stroke. Ann Neurol 55:400–409
Nelles G, Jentzen W, Jueptner M, Muller S, Diener HC (2001) Arm training induced brain plasticity in stroke studied with serial positron emission tomography. Neuroimage 13:1146–1154
Newton JM, Ward NS, Parker GJ, Deichmann R, Alexander DC, Friston KJ, Frackowiak RS (2006) Non-invasive mapping of corticofugal fibres from multiple motor areas—relevance to stroke recovery. Brain 129:1844–1858
Niehaus L, Bajbouj M, Meyer BU (2003) Impact of interhemispheric inhibition on excitability of the non-lesioned motor cortex after acute stroke. Suppl Clin Neurophysiol 56:181–186
Pereon Y, Aubertin P, Guiheneuc P (1995) Prognostic significance of electrophysiological investigations in stroke patients: somatosensory and motor evoked potentials and sympathetic skin response. Neurophysiol Clin 25:146–157
Rijntjes M, Hobbeling V, Hamzei F, Dohse S, Ketels G, Liepert J, Weiller C (2005) Individual factors in constraint-induced movement therapy after stroke. Neurorehabil Neural Repair 19:238–249
Rorden C, Brett M (2000) Stereotaxic display of brain lesions. Behav Neurol 12:191–200
Schaechter JD, Kraft E, Hilliard TS, Dijkhuizen RM, Benner T, Finklestein SP, Rosen BR, Cramer SC (2002) Motor recovery and cortical reorganization after constraint-induced movement therapy in stroke patients: a preliminary study. Neurorehabil Neural Repair 16:326–338
Sterr A, Elbert T, Berthold I, Kolbel S, Rockstroh B, Taub E (2002) Longer versus shorter daily constraint-induced movement therapy of chronic hemiparesis: an exploratory study. Arch Phys Med Rehabil 83:1374–1377
Stinear CM, Barber PA, Smale PR, Coxon JP, Fleming MK, Byblow WD (2007) Functional potential in chronic stroke patients depends on corticospinal tract integrity. Brain 130:170–180
Szaflarski JP, Page SJ, Kissela BM, Lee JH, Levine P, Strakowski SM (2006) Cortical reorganization following modified constraint-induced movement therapy: a study of 4 patients with chronic stroke. Arch Phys Med Rehabil 87:1052–1058
Taub E, Miller NE, Novack TA, Cook EW III, Fleming WC, Nepomuceno CS, Connell JS, Crgo JE (1993) Technique to improve chronic motor deficits after stroke. Arch Phys Med Rehabil 74:347–354
Taub E, Uswatte G, Mark VW, Morris DM (2006a) The learned nonuse phenomenon: implications for rehabilitation. Eura Medicophys 42:241–256
Taub E, Uswatte G, King DK, Morris D, Crago JE, Chatterjee A (2006b) A placebo-controlled trial of constraint-induced movement therapy for upper extremity after stroke. Stroke 37:1045–1049
Tombari D, Loubinoux I, Parinete J, Gerdelat A, Albucher J-F, Tardy J, Cassol E, Chollet F (2004) A longitudinal fMRI study: in recovering and then in clinically stable sub-cotical stroke patients. NeuroImage 23:827–839
Ward NS, Brown MM, Thompson AJ, Frackowiak RS (2006) Longitudinal changes in cerebral response to proprioceptive input in individual patients after stroke: an FMRI study. Neurorehabil Neural Repair 20:398–405
Weiller C, Jueptner M, Fellows S, Rijntjes M, Leonhardt G, Kiebel S, Muller S, Diener HC, Thilmann AF (1996) Brain representation of active and passive movements. Neuroimage 4:105–110
Wittenberg GF, Chen R, Ishii K, Bushara KO, Eckloff S, Croarkin E, Taub E, Gerber LH, Hallett M, Cohen LG (2003) Constraint-induced therapy in stroke: magnetic-stimulation motor maps and cerebral activation. Neurorehabil Neural Repair 17:48–57
Wohrle JC, Behrens S, Mielke O, Hennerici MG (2004) Early motor evoked potentials in acute stroke: adjunctive measure to MRI for assessment of prognosis in acute stroke within 6 hours. Cerebrovasc Dis 18:130–134
Wolf SL, Lecrew DE, Barton LA, Jann BB (1989) Forced use of hemiplegic upper extremities to reverse the effect of learned nonuse among chronic stroke and head-injured patients. Exp Neurol 104:125–132
Wolf SL, Winstein CJ, Miller JP, Taub E, Uswatte G, Morris D, Giuliani C, Light KE, Nichols-Larsen D (2006) Effect of constraint-induced movement therapy on upper extremity function 3 to 9 months after stroke: the EXCITE randomized clinical trial. JAMA 296:2095–2104
Acknowledgments
We are grateful to P.T. Alleyne-Dettmers, Ph.D. for editing the text. We thank C. Büchel for his comments during preparation of the study’s design and an early version of the manuscript and Thomas Wolbers and Volkmar Glauche for his statistical support. We are grateful to all individuals who participated in this study, particularly to Ulrike Teske how performed the training sessions. CW was supported by DFG, BMBF (GFGO 0 123 7301—01GO 0105; DFG: WE 1352/13-1), EU (QLK6 CT 1999 02140) and by the Competence network stroke (01GI9917).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hamzei, F., Dettmers, C., Rijntjes, M. et al. The effect of cortico-spinal tract damage on primary sensorimotor cortex activation after rehabilitation therapy. Exp Brain Res 190, 329–336 (2008). https://doi.org/10.1007/s00221-008-1474-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-008-1474-x