Abstract
In the present report, we extend our previous observations on corticomotor facilitation associated with covert (action observed or imagined) and overt (action imitated) action execution in old adults (Leonard and Tremblay in Exp Brain Res 117:167–175, 2007) to investigate the impact of Parkinson’s disease (PD). Participants consisted of 22 older adults (age range 58–76 years) of whom 11 were medicated patients diagnosed with PD (patient group) and 11 were age-matched healthy controls (healthy group). Corticomotor facilitation was assessed by monitoring the changes in the amplitude of motor evoked potentials (MEP) in muscles of the right hand (first dorsal interosseous: FDI; and abductor digiti minimi: ADM) in response to transcranial magnetic stimulation of the left motor cortex. In each group, corticomotor facilitation was assessed with participants seated in front of a computer screen under four testing conditions: (1) REST: eyes closed and instructions to relax for 10 s, (2) OBS: observe action, (3) IMAG: imagine action and (4) IMIT: imitate action. The action depicted in the video displayed the hand of a male subject cutting a piece of material with scissors. Comparison of variations in MEP amplitude revealed a significant interaction between groups and conditions. In the healthy group, the OBS and IMAG conditions were both associated with significant facilitation in the FDI and ADM, whereas the same conditions failed to produce facilitation in the PD group. In both groups, the IMIT condition produced the largest facilitation in hand muscles. Further planned comparisons revealed a significant difference between groups in the FDI for the OBS condition. From these findings, we conclude that, even when properly medicated, old adults with PD may experience major difficulties in engaging the motor system for covert actions, particularly when asked to observe another person’s action. This failure of corticomotor facilitation for covert actions appears to be linked with the deficit in motor activation associated with basal ganglia dysfunction in PD and in line with the difficulty experienced in general by patients “to energize” the motor system in preparation for action.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is known to lead to deficits in motor activation, which translate clinically into cardinal symptoms associated with slowing of motor executions (bradykinesia) and difficulties in action initiation (akinesia) (DeLong 2000). Impaired motor activation in PD is thought to reflect the dysfunction of the basal ganglia loop as a result of the degeneration of the nigrostriatal pathway. The deactivation of the motor cortical network in PD is particularly apparent early in the disease, where patients typically exhibit lower activation levels than controls in areas such as the supplementary motor area (SMA, particularly the rostral part) and the primary motor cortex, during performance of motor tasks (Playford et al. 1992; Rascol et al. 1992; Buhmann et al. 2003). With disease progression, the pattern of hypoactivation tends to be replaced by a pattern of hyper activation in certain areas such as the lateral premotor cortex and the primary motor cortex (Samuel et al. 1997; Sabatini et al. 2000). Such hyperactivity is thought to reflect a compensatory cortical reorganization secondary to drug-induced reafferentation of the deficient subcortical motor system to overcome the functional deficit affecting the SMA (Rothwell and Huang 2003).
In general, neurophysiological studies have been consistent with findings from neuroimaging studies in pointing to abnormalities in the cortical network subserving movement preparation and movement execution. For instance, PD patients typically exhibit reduction in surface cortical potentials (e.g., Bereishaftpotential, Contingent Negative Variation) that are normally associated with movement preparation and thought to originate from SMA (Dick et al. 1989; Cunnington et al. 1997). More specific abnormalities at the motor cortical level have also been described in the context of studies with transcranial magnetic stimulation (TMS). For example, when tested at rest, patients with PD tend to show lower motor thresholds and larger amplitude motor evoked potentials (MEPs) than controls, suggesting an increased excitability of the corticomotor output in the resting state (Valls-Sole et al. 1994; Chen et al. 2001; Tremblay and Tremblay 2002). However, when tested in the active state, patients often fail to show the large facilitation that is normally seen when TMS is delivered during contraction of the target muscle (Valls-Sole et al. 1994; Chen et al. 2001; Tremblay and Tremblay 2002). Such a failure of volitional facilitation of MEP responses has been linked with impaired motor activation and bradykinesia (Ellaway et al. 1995).
Deficits in motor activation associated with voluntary movements are also apparent when patients attempt to simulate actions mentally. For example, Dominey et al. (1995) showed that PD patients with unilateral impairments experienced more difficulties in performing imagined movements with their most affected hand in the context of a finger-sequencing task. Such observations have been paralleled by findings from neuroimaging studies showing decreased activation in several of the cortical areas that are normally active when healthy persons perform motor imagery tasks (e.g. dorsolateral frontal cortex, SMA, inferior parietal cortex and precuneus) (Cunnington et al. 2001; Samuel et al. 2001). Interestingly, the pattern of cortical activation associated with movement execution and motor imagery was largely restored in patients in the presence of subthalamic nucleus stimulation; suggesting a direct link between impaired motor activation and dysfunction of the frontal–striatal loop in patients (Thobois et al. (2002).
The fact that patients with PD exhibit parallel deficits during both real and imagined movement is consistent with the notion that actions executed and actions simulated are functionally equivalent. This notion of functional equivalence between simulated and real actions has been strengthened by observations from neuroimaging studies showing striking similarities in the parieto-frontal network activated when people observed, imagined or executed motor actions (Grezes and Decety 2001). Further support for the notion of equivalence between executed and simulated actions comes from TMS studies showing selective corticomotor facilitation in hand muscles in the context of action observation and motor imagery (Fadiga et al. 1995; Clark et al. 2004). Such findings led to the proposal by Jeannerod (2001) that both action observation and motor imagery correspond to covert states, where actions are being simulated but not overtly executed; the two processes engaging the motor system at the subliminal level for internal simulation. In that sense, observing or mentally simulating an action would be equivalent to performing it without actually doing the action. In a recent companion paper (Leonard and Tremblay 2007), we investigated, using TMS, whether normal aging would affect the ability of old persons to engage the motor system when observing or imagining motor actions. Our results showed that the capacity of healthy older adults to produce such corticomotor facilitation in hand muscles was largely preserved, although with a loss of selectivity with regards to the muscle involved in the task when compared to young persons. In the present report, we extend these observations to a group of older patients diagnosed with PD. Our goal was to determine whether deficient motor generation mechanisms would affect the ability of PD patients to produce corticomotor facilitation when observing, imagining or imitating a simple tool-oriented gesture.
Methods
Participants
Eleven patients with mild PD and bilateral impairments (six males; mean age ± SD, 68.6 ± 5.8 years) and eleven age-matched healthy controls (three males; 66.2 ± 4.9 years) participated in the study. The age-matched controls consisted of a subset of older adults that were tested in the context of a study conducted in parallel to investigate age differences in corticomotor facilitation (Leonard and Tremblay 2007). All participants were right-handed, as determined by The Edinburgh Handedness Inventory (Oldfield 1971). Prior to the experimental session, participants completed a medical questionnaire to ensure that there were no contra-indications for TMS. Patients were also screened with the Mini-mental state examination test (MMSE) for possible cognitive impairments (i.e., score <24/30, (Tombaugh and McIntyre 1992). The characteristics of patients are detailed in Table 1. At the time of assessment, all patients were on their regular medication schedule. The local Institutional Ethics Committee approved the study’s procedures and each participant provided informed consent before participation.
TMS and EMG recording
The procedures for TMS applications and for recordings of evoked potentials (MEPs) have been described in details in the companion paper (Leonard and Tremblay 2007). Briefly, TMS was administered using a Magstim 200 (Magstim Co. Dyfed, UK) connected to a figure-eight coil (70-mm diameter loop) with participants seated in a recording chair. Motor evoked potentials (MEPs) were obtained from the first dorsal interosseous (FDI) and abductor digiti minimi (ADM) muscles of the right hand by recording electromyographic (EMG) signals (100 μV/div; bandwidth filter, 10 Hz–1 kHz) with a polygraph amplifier (RMP-6004, Nihon-Kohden Corp.). For one patient, recordings of MEPs were obtained from the left non-dominant side because the presence of tremor on the right side precluded recordings at rest. For each trial, 300 ms epochs were recorded with a 50 ms delay preceding stimulus onset. EMG signals were digitized at a 2 kHz sampling rate using custom software on a PC running under Microsoft® Windows® XP equipped with a digital/analogue acquisition card (BNC-2090, National Instrument Corp.).
To facilitate coil positioning, participants were fitted with a Lycra swimming cap with marking grids traced onto it. The optimal site on the scalp to evoke MEPs in both contralateral hand muscles was marked with a red dot to ensure consistency during the recordings. In most cases, the coil was held firmly in place using a mechanical custom coil holder. In some participants, however, the utilization of the coil holder was not possible. In these instances, the coil was held in place manually by one of the experimenter. In all instances, the experimenter frequently reassessed the coil position to ensure that it remained over the optimal stimulation site throughout the experiment. The relaxed motor threshold was determined using the method advocated by Mills and Nithi (1997), which consists of determining a lower (0 MEPs/10 TMS pulses) and upper threshold (10 MEPs of ∼50 μV/10 pulses) and then taking the median between these two extremes as the threshold intensity. In all participants, the stimulation intensity used to assess corticomotor excitability corresponded to 110% of the pre-determined motor threshold.
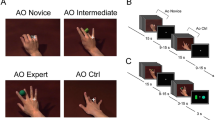
Recording of MEPs during video presentations
The experimental paradigm to assess corticomotor excitability during video presentation is described in the companion paper (Leonard and Tremblay 2007). Briefly, participants were presented with four digital video sequences, which were displayed on a 42.5-cm LCD monitor placed in front of the participants (1.3 m viewing distance). Each of the four digitized video sequences lasted 10 s and consisted of a 3 s sequence of preset instructions followed by either a dark screen or an action sequence lasting 7 s. The first video (REST) instructed participants to relax with eyes closed for the duration of a tone signal (350 Hz). The second video (OBS) displayed instruction for participants to observe attentively the coming sequence depicting a model performing a scissoring action. In the third video (IMAG), the participants were asked to close their eyes and to mentally simulate the scissoring action. The fourth video (IMIT) instructed participants to imitate the action, i.e., they had to reproduce the actual scissoring actions by cutting in the air using a pair of scissors held in their hand. In the OBS and IMIT conditions, participants both saw and heard the scissors in action, whereas in the IMAG condition only the sound could be heard, the computer screen being filled with a dark background. During all the presentations, participants held a pair of small scissors in their right (n = 21) or left (n = 1) hand in order to perform the IMIT condition. To minimize tonic EMG activity in the hand muscles for conditions where relaxation was required (i.e., REST, OBS, IMAG), the hand was positioned on the armrest so that the scissors could be held passively between the thumb and index fingers, thereby virtually eliminating muscle contraction. The four videos were presented 10× each following a pre-set random sequence for a total of 40 presentations. The order of presentation was the same for all participants. In each presentation, MEPs were recorded form the FDI and ADM by delivering TMS at a pre-determined delay (7 s) in the video sequence, which corresponded with the closing phase of the scissors action, where the FDI is most active. Custom software, which allowed triggering on a frame-by-frame basis, was used to set the trigger for TMS to the desired time-frame. In sequences wherein the scissors action was not shown (i.e., REST and IMAG), TMS was set to trigger at the same 7 s delay. EMG activity was constantly monitored in the OBS and IMAG conditions to make sure that participants did not attempt to contract their muscles. Trials where EMG silence could not be obtained were rejected and additional trials were performed if necessary. This problem occurred only in few instances (6/22 participants, four PD patients) and concerned <10% of the trials (i.e., 3–4/40 trials). At the end of the session, participants were also asked to rate how easy it was to imagine the action depicted in the video. These ratings were obtained using a visual analog scale (VAS) consisting of a 10-cm ruler with a sliding marker moving along the scale with word descriptors on the blank side ranging from “Very easy” to “Very difficult”.
Data analysis and statistics
The peak-to-peak amplitude and latency of MEPs recorded in each condition and for each participant were measured off-line and averaged to derive individual mean values. MEP amplitude data were transformed into natural logarithm (Nielsen 1996) to obtain a normal distribution. Latency measurements were normally distributed and required no transformation. The individual mean log-amplitudes and latencies computed in each group were then entered into a two-way repeated-measures analysis of variance (ANOVA) with “Condition” (REST, OBS, IMAG, IMIT) and “Muscle” (FDI, ADM) as within-subject factors and “Group” (Healthy, PD) as a between-subjects factor. Upon detection of significant main effects or interactions, post-tests comparisons were performed using the Dunnett’s test to assess differences between conditions with the REST condition serving as “Control”. Other planned comparisons were performed using independent t-tests to assess differences between groups. All tests were performed using statistical software packages (SPSS software version 13.0 for Windows® Chicago, IL, USA; GraphPad Software, San Diego California USA, http://www.graphpad.com). The level of significance was set at P < 0.05 for all tests. All values are reported as mean ± 1 SD.
Results
General observations
The stimulation intensity used to assess corticomotor excitability was similar in the two groups (PD, 43.2 ± 7%; healthy, 46.8 ± 7%; respectively, t 20 = 1.20, P = 0.24). In general, participants in both groups had no difficulty in complying with the protocol, especially with regard to the capacity to relax hand muscles when required. As noted earlier, the presence of resting tremor in the right hand proved to be problematic in only one patient (male 74 years), forcing testing of the left hand (see Methods). Inspection of imagery ratings obtained at the end of the session indicated that patients in general had no more difficulty than healthy controls in imagining the scissoring action, as judged by their VAS scores (PD, 6.5 ± 0.7 cm; controls 7.1 ± 0.6 cm, t 20 = 0.68, P = 0.50). However, two patients in the PD group (female 69 years; male 74 years) and one healthy participant (female 70 years) produced very low ratings (i.e., <4/10-cm); indicating that they might have experienced more difficulty in simulating the action mentally than the other participants. In the case of the two patients, this difficulty was not related however to lower scores on the MMSE (28 and 30/30, respectively) nor with exceptionally low MEP values when tested under the IMAG condition.
Variations in MEP amplitude
Comparison of MEP amplitude variations measured across conditions revealed a different pattern in the two groups. In healthy older adults, there was a clear tendency for MEPs to be facilitated either when observing or imagining the action. In contrast, in the PD group, the same conditions often failed to produce facilitation in hand muscles. In the two groups, the largest facilitation was seen for the IMIT condition for both muscles. Individual examples of typical variations seen in MEP amplitude in healthy controls and PD patients are shown in Fig. 1. The ANOVA confirmed the large effect of “Condition” on MEP amplitude (F 3,18 = 55.2, P < 0.001), while the main effect of “Muscle” was only marginally significant (F 1,20 = 4.4, P = 0.049). No “Muscle × Condition” interaction was detected. The ANOVA also revealed a significant “Group × Condition” interaction (F 3,18 = 4.2, P = 0.02); confirming that MEP variations recorded across conditions were influenced by the group’s status.
Typical examples of MEP facilitation elicited under the OBS (action observed) and IMAG (action imaged mentally) conditions with respect to REST (baseline condition) in a healthy (a) participant and a PD (b) patient. The imitation condition is not shown here for clarity. Each trace is an average of 10 evoked responses recorded in the FDI and ADM muscles. Note the absence of facilitation relative to REST for the OBS and IMAG conditions in the PD patient
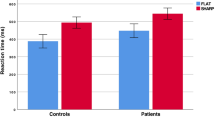
Figure 2 compares the mean variations in the size of MEPs computed in the two groups across the different conditions for the two muscles and the results of the post-test comparisons. It can be seen in Fig. 2a that the large effect of “Condition” on MEP amplitude was largely attributable to the facilitation observed in the healthy group for the FDI under the OBS, IMAG and IMIT conditions, which were all highly significantly different from REST (mean diff. of 0.7, 0.8 and 1.5 log-amplitude μV, respectively, P < 0.01). In the PD group, only the IMIT condition was associated with significant amplitude facilitation (mean diff., 1.9, P < 0.01). As shown in Fig. 2b, the same comparisons for the ADM muscle revealed a slightly different pattern of facilitation with significant differences being observed for the IMAG (mean diff., 0.6, P < 0.05) and IMIT (mean diff., 1.7, P < 0.01) conditions in the healthy group, whereas only IMIT (mean diff., 1.3, P < 0.01) was significantly different from REST in the PD group. Further planned comparisons of the differences observed between the two groups for the FDI revealed a significant difference for the OBS condition (mean diff., 0.96, t 20 = 2.25, P = 0.036) but not for the IMAG and the IMIT conditions (mean diff. of 0.55 and 0.34, respectively, P > 0.05). Similar planned comparisons of conditions between groups were also performed for the ADM and revealed no significant differences.
Comparison of the mean variations measured in MEP amplitude in the two groups across the different conditions. Each column represents an average of the MEP log-amplitude computed under each condition in each group for the two muscles investigated (a FDI, first dorsal interosseous; b ADM, adductor digiti minimi). The thick line and asterisks denote significant differences observed between conditions relative to REST after comparisons with the Dunnett’s post-test. In a, the dotted line and the asterisk denote a significant difference for the OBS condition between the two groups. *P < 0.05, **P < 0.01
Variations in MEP latency
As for amplitude data, variations in MEP latency were mostly affected by “Condition”, this factor alone accounting for >75% of the variance observed (F 3,18 = 21.0, P < 0.001). Apart from a significant “Muscle × Condition” interaction (F3,18 = 5.5, P = 0.007), no other interactions were detected. As shown in Fig. 3, the latter interaction reflected the differences observed between the FDI and ADM muscles across conditions. In the FDI (Fig. 3a), post-test comparisons revealed a significant reduction from REST only for the IMIT condition and this, for both groups (mean diff., Healthy, 1.9 ms; PD, 2.4 ms, P < 0.01). In the ADM (Fig. 3b), significant reductions were observed only in the healthy group for the IMIT and IMAG conditions (mean diff. of 2.2 and 1.6 ms, respectively, P < 0.01). In the PD group, no such differences were detected in the post- test comparisons, in spite of the reductions observed (Fig. 3b).
Comparison of the mean variations measured in MEP latency in the two groups across the different conditions. Representations and symbols as in Fig. 2
Discussion
In the present study, we compared corticomotor facilitation elicited in hand muscles in two groups of old participants under conditions involving observation, imagery or imitation of a tool-oriented action. In a companion paper (Leonard and Tremblay 2007), we showed that the ability to produce corticomotor facilitation under such conditions (i.e., action observed, imaged or imitated) was largely preserved in healthy old adults, in spite of a loss in muscle selectivity when compared to young adults. The present study confirms these findings in the case of healthy older adults and extend these observations to show that in a group of age-matched medicated patients treated for PD, corticomotor facilitation in hand muscles was notably reduced or absent when patients either observed or imagined the action. On the other hand, when asked to actively imitate, the level of facilitation was comparable to that seen in healthy controls; indicating a preserved capacity to normalize corticomotor excitability when executing a manual action. Thus, our observations in PD patients are indicative of a failure to engage the motor system more at the covert than at the overt stage of action execution.
Before considering the reasons as to why facilitation with action observations and imagery failed in the patient group, three possible confounding issues must be addressed. The first issue concerns the fact that our patients were tested “on” medication, as this factor is known to affect patterns of cortical activation and motor symptoms. The second pertains to reports from neuroimaging and TMS studies indicating that PD patients often exhibit hyperactivity in the primary motor cortex at rest. The final issue concerns the presence of potential cognitive impairments that might have affected the ability of patients to perform the task. With regards to the effect of dopaminergic medication, Cunnington et al. (2001) have examined this issue carefully using fMRI in the context of a motor imagery task involving thumb–index finger opposition. Although their results confirm that dopaminergic stimulation tended to normalize activation levels in the cortical network associated with motor imagery, they noted that certain areas like the SMA proper and the inferior parietal cortex were unaffected by the medication. In fact, both regions showed normal activation levels in patients both “on” and “off” medication. Thobois et al. (2000) reported similar results, finding a preserved activation of SMA and posterior parietal cortex in patients in the “off-state” performing a motor imagery tasks with their akinetic hand, without activation of the primary motor cortex. Interestingly, the pattern was reversed when the movement was simulated using the less affected hand with activation of the motor cortex and deactivation of the SMA being detected. Thus, one cannot simply assume that patterns of cortical activation will be “normal” just because patients are tested “on” medication. Even if it were the case on the neuroimaging side, deficits in performance may still be detected at the behavioral level, as revealed in chronometric studies of real or mentally simulated actions (Dominey et al. 1995; Cunnington et al. 1997; Amick et al. 2006). In the present study, we elected to test patients in their “on” period to make sure they were able to go through the protocol without having to deal with disturbing motor symptoms and so that they can be at their best when performing the task conditions.
As for the issue of hyperactivity in the motor cortex at rest, which could have limited the ability of patients to produce facilitation, we did not find evidence of increased corticomotor excitability in our group of patients. In fact, MEPs measured for the REST condition in both the FDI and the ADM in patients (mean, 244 and 211 μV, respectively) were comparable to those measured in the healthy group (mean, 392 and 311 μV, respectively). In addition, the fact that the patients were able to produce normal facilitation levels when actively imitating the action provides another argument against the possibility that “hyperactivity” in the motor cortex was a limiting factor preventing MEP facilitation under the OBS or IMAG conditions.
Finally, the possibility that MEP facilitation failed simply because patients were unable to attend to the task at hand when asked to observe or to imagine the action, appears unlikely for several reasons. First, as stated before, all patients were alert and cooperative during testing and none showed signs of cognitive impairments, as judged by scores on the MMSE (see Table 1). Second, during the recording session, we deliberately provided participants with the sound coming from the snipping actions so that they can stay alert and focus while observing or imagining the action. In fact, just listening to the sound of actions appears to be sufficient in itself to produce corticomotor facilitation in hand muscles (Aziz-Zadeh et al. 2004). Accordingly, we believe that our conditions were more than optimal to elicit motor facilitation (i.e., sounds and/or image) in hand muscles. Third, subjective ratings of patients with regards to the ability to imagine the action were not different from those obtained in healthy controls; indicating that the majority did attend to the task at hand when asked to simulate the action mentally.
Why, then, if patients were medicated, cognitively alert and not limited by an “overactive” motor cortex at rest, corticomotor facilitation failed with action observation and imagery while the same conditions elicited clear MEP facilitation in healthy controls. As stated earlier, the fact that facilitation was mostly impaired when the action had to be internally simulated rather than physically performed, points to a deficit in action representation (i.e., covert stage). According to motor simulation theory, both action observation and motor imagery are thought to lead to subliminal activation of the motor system allowing one to prepare for subsequent actions in the absence of execution. A failure to produce such subliminal activation in the group of patients thus appears to be at the basis of the present observation. It is tempting to suggest that the facilitation failed because patients were unable to properly engage certain critical areas, such as the inferior parietal cortex or the SMA, while observing or imagining the action, even though they were tested on therapy, which should help normalize movement-related activity. It is worth noting again that dopa therapy only partially restores patterns of cortical activity associated with motor execution and motor preparation and that deficits remain apparent even when patients are tested “on” medication (Dominey et al. 1995; Amick et al. 2006). Interestingly, Amick et al. (2006), in their recent report, revealed asymmetries in the quality of the central representation deficit in patients with PD. Their results showed that patients with right side onset, and presumably greater left hemispheric dysfunction, were more severely affected in a task involving motor imagery (i.e., mental rotation of hands), as compared to those with left-side onset (right hemispheric dysfunction), who were more impaired in tasks involving visual imagery. Although we did not specifically address this issue in the present study, it is interesting to note that the failure of corticomotor facilitation we observed in our group of patients was localized on the right side in response to TMS of the left motor cortex; a finding congruent with the predominant role ascribed to left the hemisphere in action representation (Decety et al. 1997; Della Sala et al. 2006; Lewis 2006).
Given the existence of dense interconnections between non primary motor areas and the motor cortex (Rizzolatti et al. 1998), any deficient activation in those areas could certainly affect the level of corticomotor excitability detected in PD patients. One cannot exclude, however, the possibility that the primary failure was in the motor cortex itself. While neuroimaging studies have produced mixed results with regards to the involvement of the primary motor cortex during mental simulation of actions, recent works by Dechent et al. (2004) showed that this activation was real but weak and very brief in time; making it difficult to detect in neuroimaging paradigms. In patients with PD, some reports indicate that activation of the motor cortex might be lacking when patients imagined movements (Thobois et al. 2002), but these reports have been inconsistent and their interpretation remains blurred by factors like “medication” and by the presence of compensatory activations in other cortical areas. In normal controls, recording techniques with high temporal resolution such as magneto-encephalography (Hari et al. 1998) and TMS (Fadiga et al. 1995; Maeda et al. 2002; Clark et al. 2004) have produced far more consistent results with regard to the involvement of the motor cortex in mentally simulated actions. In sum, it seems reasonable to conclude that the lack of facilitation we observed in our group of patients for conditions associated with motor simulation without overt execution (i.e., OBS and IMAG) likely reflected a deficit in motor activation affecting critical nodes in the motor cortical network normally engaged when actions are prepared.
One intriguing finding of the present study is that the most significant difference between the two groups was found for the OBS condition. In fact, under this condition, MEP facilitation was virtually absent in the PD group (see Fig. 2). This finding was somewhat unexpected given the well-known clinical observation that motor performance in PD patients can be improved by visual cues (Stern et al. 1980; Dunne et al. 1987; Suteerawattananon et al. 2004). In fact, one would have expected that patients should have more difficulty in facilitating the corticomotor system during motor imagery, when participants had to internally generate the motor image from memory, rather than when they observed the actual action being performed on screen (eyes open, visual cues). In addition, the presence of background sounds coupled with video images should have provided the best conditions to elicit corticomotor facilitation in hand muscles, as we stated earlier; but this was not the case. One possible explanation for this finding may reside in the difference between motor imagery and action observation as modes of motor simulation. In fact, while the two modes are thought to be largely equivalent at the neural level, they differ in the fact that “action observation” is considered to be a more implicit process in nature as compared to motor imagery, which by virtue of the instructions given to participants (e.g., see yourself raising your arm) is considered a more explicit process leading to conscious representation (Jeannerod and Frak 1999). In the present study, the IMAG condition contained specific instructions for participants to imagine the task. To some extent, these explicit instructions may have assisted, at least in some cases, in drawing the patient’s attention on the task at hand and helped in producing corticomotor facilitation. Without explicit instructions under the OBS condition, patients might have been simply unable to overcome the deficit in motor activation and thus facilitation largely failed under this condition. In this respect, our findings appears consistent with those of Cunnington et al. (1999), who showed that, when given explicit instructions to concentrate on internally timed responses, PD patients actually exhibited faster reaction times than when given no specific instructions. The large failure of “implicit motor imagery” in our group of patients is also in line with a large body of evidence indicating that deficits in implicit procedural learning is indeed a preeminent feature in PD, as demonstrated by serial reaction time tasks (Siegert et al. 2006).
In conclusion, the present results confirm that healthy older adults have a preserved capacity to activate the corticomotor system during implicit motor imagery when observing an action, as well as during explicit imagery of the same action. However, the ability of older adults affected with PD to engage the motor system under similar conditions was notably impaired and this, even if they were properly medicated to control for their motor symptoms. Such a deficit could reflect their impaired capacity to energize the motor system in preparation for action, a deficit that is only partially restored by dopaminergic therapy.
References
Amick MM, Schendan HE, Ganis G, Cronin-Golomb A (2006) Frontostriatal circuits are necessary for visuomotor transformation: mental rotation in Parkinson’s disease. Neuropsychologia 44:339–349
Aziz-Zadeh L, Iacoboni M, Zaidel E, Wilson S, Mazziotta J (2004) Left hemisphere motor facilitation in response to manual action sounds. Eur J Neurosci 19:2609–2612
Buhmann C, Glauche V, Sturenburg HJ, Oechsner M, Weiller C, Buchel C (2003) Pharmacologically modulated fMRI—cortical responsiveness to levodopa in drug-naive hemiparkinsonian patients. Brain 126:451–461
Chen R, Kumar S, Garg RR, Lang AE (2001) Impairment of motor cortex activation and deactivation in Parkinson’s disease. Clin Neurophysiol 112:600–607
Clark S, Tremblay F, Ste-Marie D (2004) Differential modulation of corticospinal excitability during observation, mental imagery and imitation of hand actions. Neuropsychologia 42:105–112
Cunnington R, Iansek R, Johnson KA, Bradshaw JL (1997) Movement-related potentials in Parkinson’s disease. Motor imagery and movement preparation. Brain 120:1339–1353
Cunnington R, Iansek R, Bradshaw JL (1999) Movement-related potentials in Parkinson’s disease: external cues and attentional strategies. Mov Disord 14:63–68
Cunnington R, Egan GF, O’Sullivan JD, Hughes AJ, Bradshaw JL, Colebatch JG (2001) Motor imagery in Parkinson’s disease: a PET study. Mov Disord 16:849–857
Decety J, Grezes J, Costes N, Perani D, Jeannerod M, Procyk E, Grassi F, Fazio F (1997) Brain activity during observation of actions. Influence of action content and subject’s strategy. Brain 120:1763–1777
Dechent P, Merboldt KD, Frahm J (2004) Is the human primary motor cortex involved in motor imagery? Cogn Brain Res 19:138–144
Della Sala S, Faglioni P, Motto C, Spinnler H (2006) Hemisphere asymmetry for imitation of hand and finger movements, Goldenberg’s hypothesis reworked. Neuropsychologia 44:1496–1500
DeLong M (2000) The basal ganglia. In: Kandel E, Schwartz J, Jessel T (eds) Principles of neural science. McGraw-Hill, Montréal, pp 851–867
Dick JP, Rothwell JC, Day BL, Cantello R, Buruma O, Gioux M, Benecke R, Berardelli A, Thompson PD, Marsden CD (1989) The Bereitschaftspotential is abnormal in Parkinson’s disease. Brain 112:233–244
Dominey P, Decety J, Broussolle E, Chazot G, Jeannerod M (1995) Motor imagery of a lateralized sequential task is asymmetrically slowed in hemi-Parkinson’s patients. Neuropsychologia 33:727–741
Dunne JW, Hankey GJ, Edis RH (1987) Parkinsonism: upturned walking stick as an aid to locomotion. Arch Phys Med Rehabil 68:380–381
Ellaway PH, Davey NJ, Maskill DW, Dick JP (1995) The relation between bradykinesia and excitability of the motor cortex assessed using transcranial magnetic stimulation in normal and parkinsonian subjects. Electroencephalogr Clin Neurophysiol 97:169–178
Fadiga L, Fogassi L, Pavesi G, Rizzolatti G (1995) Motor facilitation during action observation: a magnetic stimulation study. J Neurophysiol 73:2608–2611
Fahn S, Elton R, Committee UD (1987) Unified Parkinson’s disease rating scale. In: Fahn S, Marsden CD, Calne DB, Goldstein M (eds) Recent developments in Parkinson’s disease, vol 2. Macmillan Healthcare Information, Florham Park, pp 153–163
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Hari R, Forss N, Avikainen S, Kirveskari E, Salenius S, Rizzolatti G (1998) Activation of human primary motor cortex during action observation: a neuromagnetic study. Proc Natl Acad Sci USA 95:15061–15065
Jeannerod M (2001) Neural simulation of action: a unifying mechanism for motor cognition. Neuroimage 14:S103–S109
Jeannerod M, Frak V (1999) Mental imaging of motor activity in humans. Curr Opin Neurobiol 9:735–739
Leonard G, Tremblay F (2007) Corticomotor facilitation associated with observation, imagery and imitation of hand actions: a comparative study in young and old adults. Exp Brain Res 177:167–175
Lewis JW (2006) Cortical networks related to human use of tools. Neuroscientist 12:211–231
Maeda F, Kleiner-Fisman G, Pascual-Leone A (2002) Motor facilitation while observing hand actions: specificity of the effect and role of observer’s orientation. J Neurophysiol 87:1329–1335
Mills KR, Nithi KA (1997) Corticomotor threshold to magnetic stimulation: normal values and repeatability. Muscle Nerve 20:570–576
Nielsen JF (1996) Logarithmic distribution of amplitudes of compound muscle action potentials evoked by transcranial magnetic stimulation. J Clin Neurophysiol 13:423–434
Oldfield RC (1971) The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia 9:97–113
Playford ED, Jenkins IH, Passingham RE, Nutt J, Frackowiak RS, Brooks DJ (1992) Impaired mesial frontal and putamen activation in Parkinson’s disease: a positron emission tomography study. Ann Neurol 32:151–161
Rascol O, Sabatini U, Chollet F, Celsis P, Montastruc JL, Marc-Vergnes JP, Rascol A (1992) Supplementary and primary sensory motor area activity in Parkinson’s disease. Regional cerebral blood flow changes during finger movements and effects of apomorphine. Arch Neurol 49:144–148
Rizzolatti G, Luppino G, Matelli M (1998) The organization of the cortical motor system: new concepts. Electroencephalogr Clin Neurophysiol 106:283–296
Rothwell JC, Huang YZ (2003) Systems-level studies of movement disorders in dystonia and Parkinson’s disease. Curr Opin Neurobiol 13:691–695
Sabatini U, Boulanouar K, Fabre N, Martin F, Carel C, Colonnese C, Bozzao L, Berry I, Montastruc JL, Chollet F, Rascol O (2000) Cortical motor reorganization in akinetic patients with Parkinson’s disease: a functional MRI study. Brain 123:394–403
Samuel M, Ceballos-Baumann AO, Blin J, Uema T, Boecker H, Passingham RE, Brooks DJ (1997) Evidence for lateral premotor and parietal overactivity in Parkinson’s disease during sequential and bimanual movements. A PET study. Brain 120:963–976
Samuel M, Ceballos-Baumann AO, Boecker H, Brooks DJ (2001) Motor imagery in normal subjects and Parkinson’s disease patients: an H215O PET study. Neuroreport 12:821–828
Siegert RJ, Taylor KD, Weatherall M, Abernethy DA (2006) Is implicit sequence learning impaired in Parkinson’s disease? A meta-analysis. Neuropsychology 20:490–495
Stern GM, Lander CM, Lees AJ (1980) Akinetic freezing and trick movements in Parkinson’s disease. J Neural Transm Suppl 16:137–141
Suteerawattananon M, Morris GS, Etnyre BR, Jankovic J, Protas EJ (2004) Effects of visual and auditory cues on gait in individuals with Parkinson’s disease. J Neurol Sci 219:63–69
Thobois S, Dominey PF, Decety PJ, Pollak PP, Gregoire MC, Le Bars PD, Broussolle E (2000) Motor imagery in normal subjects and in asymmetrical Parkinson’s disease: a PET study. Neurology 55:996–1002
Thobois S, Dominey P, Fraix V, Mertens P, Guenot M, Zimmer L, Pollak P, Benabid AL, Broussolle E (2002) Effects of subthalamic nucleus stimulation on actual and imagined movement in Parkinson’s disease: a PET study. J Neurol 249:1689–1698
Tombaugh TN, McIntyre NJ (1992) The mini-mental state examination: a comprehensive review. J Am Geriatr Soc 40:922–935
Tremblay F, Tremblay LE (2002) Cortico-motor excitability of the lower limb motor representation: a comparative study in Parkinson’s disease and healthy controls. Clin Neurophysiol 113:2006–2012
Valls-Sole J, Pascual-Leone A, Brasil-Neto JP, Cammarota A, McShane L, Hallett M (1994) Abnormal facilitation of the response to transcranial magnetic stimulation in patients with Parkinson’s disease. Neurology 44:735–741
Acknowledgments
The authors wish to thank all participants for their time and patience during testing. Part of this work served as a partial fulfillment of Masters’ degree in Human Kinetics by Guillaume Leonard. Guillaume Leonard received a CIHR (Canada) postgraduate scholarship towards the completion of this project and an Ontario Graduate Scholarship. Francois Tremblay is supported by Natural Sciences & Engineering Research Council of Canada.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tremblay, F., Léonard, G. & Tremblay, L. Corticomotor facilitation associated with observation and imagery of hand actions is impaired in Parkinson’s disease. Exp Brain Res 185, 249–257 (2008). https://doi.org/10.1007/s00221-007-1150-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-007-1150-6