Abstract
While GABAB receptors are thought to have an important role in mediating long interval intracortical inhibition (LICI) in the human motor cortex, the effect of a selective GABAB receptor agonist on this measure has not been directly tested. Nine healthy volunteers ingested either 50 mg baclofen (BAC) or placebo (PBO) in a randomized, double blind crossover design, with the second session one week later. We used transcranial magnetic stimulation to assess motor threshold, motor evoked potential (MEP) amplitude, cortical silent period (CSP) duration, short interval intracortical inhibition (SICI) and LICI before and 90 min following drug intake. There was no specific effect of drug on motor threshold, MEP amplitude or CSP duration. BAC resulted in a significant increase in LICI (P=0.002) and a significant decrease in SICI (P=0.046) while PBO had no effect. Our findings demonstrate that the enhanced GABAB receptor activation results in differential effects on these two measures of intracortical inhibition in the human motor cortex. The increase in LICI is likely to be a result of increased GABAB receptor mediated inhibitory post-synaptic potentials, while the reduction in SICI may relate to the activation of pre-synaptic GABAB receptors reducing GABA release.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inhibitory synaptic transmission in the brain is predominantly mediated by gamma-aminobutyric acid (GABA), a neurotransmitter that is present in all layers of the cortex (Jones 1993). Of the three types of GABA receptors, GABAA and GABAB receptors are more widely distributed within the CNS (Watanabe et al. 2002) and have been more extensively targeted for research and therapeutic uses. This includes studies in the human motor cortex of measures of corticospinal and intracortical excitability, as assessed by transcranial magnetic stimulation (TMS). Using this technique, the role of GABAA receptors in mediating short interval intracortical inhibition (SICI), a measure that is obtained in a paired-pulse TMS protocol (Kujirai et al. 1993; Ziemann et al. 1996c), has been well established (Ziemann et al. 1996a; Di Lazzaro et al. 2000, 2005a, b; Ilic et al. 2002).
In contrast, the role of GABAB receptors in TMS measures of cortical excitability is less clear. It was shown that administration of the selective GABAB receptor agonist baclofen (BAC) has no effect on the amplitude of the motor evoked potential (MEP) (Inghilleri et al. 1996). The effects of pharmacological modulation of GABAB receptors on the cortical silent period (CSP), a putative measure of long-lasting motor cortical inhibition (Hallett 1995), are contradictory. It was suggested that the CSP is mediated by GABAB receptors (Werhahn et al. 1999), and this was supported by one study examining the effect of intrathecal BAC (Siebner et al. 1998). In contrast, intravenous or oral administration of BAC reportedly had no effect on CSP duration (Inghilleri et al. 1996; Ziemann et al. 1996b).
Preventing cellular re-uptake of GABA from the synaptic cleft by the anticonvulsant tiagabine revealed differential modulation of intracortical inhibitory processes (Werhahn et al. 1999). Tiagabine increased CSP duration and long interval intracortical inhibition (LICI), another measure obtained by paired-pulse TMS (Valls-Sole et al. 1992; Nakamura et al. 1997; Chen et al. 1999). In contrast, tiagabine decreased SICI. The proposed mechanisms for these effects are through GABAB receptor mediated increased long-lasting inhibitory post-synaptic potentials (IPSPB) in motor cortex output neurons, and through activation of pre-synaptic GABAB receptors on inhibitory interneurons, reducing the release of GABA, respectively. Whether these effects were truly mediated through GABAB receptors is, however, unknown because increased GABA in the synaptic cleft activates both GABAA and GABAB receptors.
To clarify this issue, we investigated here the effects of a single dose of the specific GABAB receptor agonist BAC on measures of cortical excitability, in particular LICI and SICI. If, according to the proposed mechanisms, our experiments showed that BAC increases LICI and decreases SICI then this would indicate, for the first time, a specific role of GABAB receptors in controlling various forms of inhibition in the human motor cortex.
Materials and methods
Subjects
Nine healthy right-handed subjects (21–41 years old, 5 females) were recruited for the study after giving written informed consent. None of the subjects had a history of neurological disease or was on medication at the time of the experiments. All testing was done in accordance with the Declaration of Helsinki, with approval from the Ethics Committee of the J.W. Goethe University of Frankfurt, Germany.
Study design
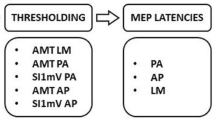
The study employed a randomized, placebo (PBO)-controlled, double-blinded crossover design. All subjects participated in two sessions at least 1 week apart, investigating the effect of drug on motor threshold, MEP amplitude, CSP, SICI and LICI. Following the baseline measures of cortical excitability, subjects were given either a PBO or 50 mg BAC (Lioresal®, Novartis Pharma). BAC is the beta-p-chlorophenyl derivative of GABA and a selective agonist at the GABAB receptor (Hill and Bowery 1981; Bowery 1993). The order of drug allocation was randomized and balanced across subjects. Measures of cortical excitability were repeated, starting 90 min following drug intake; the peak plasma concentration of BAC is reached, according to the prescribed information provided by Novartis Pharma, at 2.1±0.7 h, but the time of the peak concentration in the brain or CSF is not known. Therefore, late BAC effects may have been missed in the present study, but this is unlikely as we adopted the timing of the post-drug measurements from a previous study that showed significant BAC effects on motor cortical excitability at 2 and 5 h, but not 24 h, after drug intake (Ziemann et al. 1996b).
Stimulation and recording procedures
EMG recordings
Subjects were seated in a comfortable chair while the following procedures were undertaken. Surface electromyograms (EMG) were recorded from the abductor pollicis brevis (APB) muscle of the right hand using surface electrodes in a belly-tendon montage. Signals were amplified and filtered (0.05–2 kHz), digitized (analog-to-digital rate 5 kHz, CED Micro 1401, Cambridge Electronic Design, Cambridge, UK) and fed into a computer for online visual display and off-line analysis.
Transcranial magnetic stimulation
TMS was applied over the hand area of the left motor cortex with a figure-of-eight coil (outer diameter of each wing, 90 mm) connected to two Magstim 200 magnetic stimulators (Magstim Co., Whitland, UK) via a BiStim module throughout all measurements, and placed flat on the skull at the optimal stimulation site with the handle pointing backwards and oriented 45° from the midline. The optimal position of the coil for eliciting MEPs in the APB was marked on the scalp with a soft-tipped pen to ensure accurate positioning of the coil. Resting motor threshold (RMT) was determined to the nearest 1% of the maximum stimulator output and defined as the minimum stimulus intensity to elicit MEPs >50 μV in peak-to-peak amplitude in at least five out of ten consecutive trials (Rossini et al. 1994). Motor thresholds will be given in percentage of maximum stimulator output. Stimulus intensity was then adjusted to produce peak-to-peak MEP amplitudes of ~1 mV (MEP1 mV) and 20 MEPs were recorded (random intertrial intervals of 7.5–12.5 s to reduce anticipation). MEP amplitude was calculated as the mean from the single-trial peak-to-peak amplitudes.
Active motor threshold (AMT) was obtained during a slight isometric contraction (5–10% of maximum voluntary contraction, monitored by visual and auditory feedback of the EMG raw signal) and was defined as the lowest stimulus intensity to elicit a MEP of >100 μV averaged across five consecutive trials. The CSP was then elicited while subjects maintained a maximal voluntary contraction, using a TMS intensity of 150% AMT. Ten trials were obtained, single-trial rectified and averaged. The duration of the CSP was calculated with a graphical method as previously described (Garvey et al. 2001) and is defined as the period from the onset of EMG suppression until the resumption of sustained post-stimulus EMG activity.
SICI was recorded as previously described with an interstimulus interval of 3.0 ms in order to produce clear inhibition of the test response (Kujirai et al. 1993; Ziemann et al. 1996c; Hanajima et al. 2003). This particular interval was selected because we sought to isolate GABAA receptor mediated motor cortical inhibition. SICI occurs in two phases at intervals around 1 and 2.5–4 ms but only the later phase is thought to measure true GABAA receptor mediated synaptic inhibition while refractoriness contributes to the early phase (Fisher et al. 2002; Hanajima et al. 2003). Furthermore, short interval intracortical facilitation may contaminate SICI, but this facilitation occurs only at discrete intervals that typically spare the interstimulus interval of 3.0 ms (Tokimura et al. 1996; Ziemann et al. 1998). The intensity of the conditioning stimulus (CS3) was set at approximately 70% RMT and the test stimulus intensity was set to produce MEP1 mV when given alone. The intensity of CS3 was then adjusted, if necessary, to produce approximately 50% inhibition of the test MEP in order to provide the largest possible modification range for both increases and decreases of SICI. The final intensity of CS3 used for the measurements was always, except for one subject in the PBO condition, below AMT. This ensures that the inhibitory effect of CS3 on the test MEP occurs at the level of motor cortex and not at the level of spinal cord (Kujirai et al. 1993; Di Lazzaro et al. 1998). Blocks consisted of ten trials each of the test stimulus alone and the CS3-test stimulus pair, delivered in random order and at intertrial intervals of 5–7 s. To calculate SICI, the mean MEP elicited by the CS3-test stimulus pair was expressed as a percentage of the mean MEP elicited by the test stimulus alone.
LICI was tested by using a suprathreshold (approximately 120% RMT) conditioning stimulus that was delivered 100 ms prior (CS100) to the test stimulus, which was set to MEP1 mV (Valls-Sole et al. 1992). The interstimulus interval of 100 ms was chosen because epidural recordings from the cervical spinal cord show that LICI at this interval occurs at a supraspinal level, most likely within circuits of the motor cortex (Nakamura et al. 1997; Chen et al. 1999) while spinal inhibition is no longer prevalent at this interval when explored with H reflex testing (Fuhr et al. 1991). The intensity of CS100 was adjusted, if necessary, to produce approximately 50% inhibition of the test MEP to provide the largest possible modification range. Blocks consisted of ten trials each of the test stimulus alone and CS100-test stimulus pair, delivered in random order and at intertrial intervals of 5–7 s. To calculate LICI, the mean MEP elicited by the CS100-test stimulus pair was expressed as a percentage of the mean MEP elicited by the test stimulus alone.
RMT, MEP amplitude, SICI and LICI were measured during complete voluntary relaxation. This was monitored by high gain EMG (50 μV/div). Trials contaminated by voluntary EMG activity were discarded from further analysis.
Ninety minutes following drug administration, the RMT, AMT and intensity required to produce MEP1 mV were determined again. If these measures deviated from those at baseline then conditioning and test stimulus intensities were adjusted in the post-drug paired-pulse tests. In this way, the test stimulus intensity was able to maintain MEP1 mV (MEP amplitude elicited by the test pulse alone). Further, if there was a change in RMT, the intensities of CS3 and CS100 were adjusted to maintain the same relationship to RMT compared with pre-drug measures. Any changes in SICI and LICI in the post-drug compared to pre-drug measures are then most likely attributable to a specific drug effect. Stimulus intensity in the CSP measurements was also adjusted in the case of changes in AMT such that intensity remained at 150% AMT. Finally, stimulus intensity for the single-pulse MEP amplitude recordings remained identical to the pre-drug value.
Data analysis and statistics
Two-way analysis of variance (ANOVA) was used to determine the effects of drug administration on RMT, AMT, MEP amplitude and CSP with drug (PBO, BAC) and time (pre, post) as within-subject factors. Post hoc Student’s paired two-tailed t tests were conducted if one of the main effects or their interaction was significant. In all tests, results were considered significant at a level of P<0.05. Data are expressed as mean±SD unless otherwise stated.
Results
All subjects reported mild adverse effects after the administration of BAC, most commonly tiredness and light-headedness. These effects did not interfere with the ability of subjects to comply with all requirements of the study.
Resting and active motor threshold
Following drug administration, there was a slight but significant increase in RMT, as demonstrated by a significant effect of time (F 1,8=20.2, P=0.002). Post hoc paired Student’s t tests showed that this was explained by a slight increase of RMT after administration of both drugs (BAC: P=0.035; PBO: P=0.003, Table 1). There was no difference in RMT between BAC and PBO sessions at baseline (P=1.000). There was no significant difference in AMT due to drug, time or the interaction between drug and time (Table 1 )
MEP amplitude
The stimulus intensity used to produce MEP1 mV at baseline was similar in the BAC and PBO groups (51.7±11.2% of maximum stimulator output vs. 51.1±10.9%, P=0.633). There was no change in MEP amplitude following administration of either drug (Fig. 1a, Table 1).
a EMG recordings from a single subject illustrating the effect of BAC on MEPs evoked from single pulse TMS (top traces), SICI at an interval between conditioning pulse (CS) and test pulse of 3 ms (middle traces) and LICI at an interval of 100 ms (bottom traces). The dotted line in the lower two rows indicates the test MEP and the conditioned MEP is represented as a solid line. Solid arrows indicate the timing of the CS and test stimulus. All traces are averages of ten trials. Percentages indicate the values of SICI and LICI (conditioned MEP/unconditioned MEP×100%). Note that BAC resulted in a marked decrease of SICI and a marked increase in LICI in this subject. b SICI (left diagrams) and LICI data (right diagrams) from all individuals (each symbol denotes one subject) before and after BAC (top row) or PBO (bottom row). Gray circles and error bars are means±SD. BAC led to a significant decrease in SICI (*P=0.046) and an increase in LICI (**P=0.002). In contrast, there was no consistent change in SICI or LICI following PBO (P>0.05)
Cortical silent period
There was no significant effect of drug, time or the interaction between drug and time on CSP duration (Table 1).
Short interval intracortical inhibition
Small changes in RMT and the intensity required to produce MEP1 mV necessitated alteration of the conditioning and test stimulus intensities for both groups following drug administration. Despite this, there was no significant effect of drug, time or the interaction between drug and time on the absolute intensity of CS3 in% of maximum stimulator output (BAC: 28.1±6.4%→28.6±6.1%; PBO: 27.0±5.6%→27.0±5.4%), or on CS3 intensity expressed as a percentage of RMT (BAC: 65.5±11.2%→64.6±11.1%; PBO: 62.7±8.8%→61.0±9.7%), or on the absolute intensity of the test stimulus in% of maximum stimulator output (BAC: 55.0±11.6% → 55.8±12.0%; PBO: 54.4±11.3% → 55.1±12.2%). Therefore, there were no changes in absolute or relative intensity of CS3 or the test stimulus that could have accounted for the significant drug effects on SICI. In addition, there was no change in the amplitude of the MEP elicited by the test stimulus alone (BAC: 1.05±0.21 mV→1.19±0.30 mV; PBO: 1.30±0.43 mV→1.14±0.37 mV) that could have been responsible for the drug effects on SICI.
In the BAC group, SICI decreased in seven of the nine subjects, while there was no consistent change in SICI in the PBO group (Fig. 1b), resulting in a significant interaction of drug and time (F 1,8=9.18, P=0.016, Fig. 1). Post hoc Student’s paired t tests showed that this was explained by a significant decrease of SICI under BAC while there was no significant change of SICI under PBO (BAC: P=0.046; PBO: P=0.477, Table 1). SICI at baseline was not significantly different between the BAC and PBO sessions (P=0.100). The magnitude of SICI at baseline had no significant effect on the change of SICI produced by BAC, as indicated by a linear regression analysis with SICI at baseline as independent variable and the ratio SICI (post/pre) as dependent variable (r=-0.23, P=0.555). This indicates that the effect of BAC on SICI was not confounded by the level of SICI at baseline. Finally, the intensity of CS3, normalized to RMT (range across subjects, 0.41–0.80), did not correlate with the change of SICI produced by BAC (r=−0.063, P=0.873), suggesting that the exact point on the typically U-shaped SICI intensity curve where a given subject was tested did not systematically influence the decreasing effect of BAC on SICI.
Long interval intracortical inhibition
As with SICI, there was no significant effect of drug, time or the interaction between drug and time on the absolute intensity of CS100 in% of maximum stimulator output (BAC: 49.9±14.3%→50.1±13.7%; PBO: 46.8±12.1%→46.9±12.1%), or on CS100 intensity expressed as a percentage of RMT (BAC: 114.3±20.0%→111.3±19.0%; PBO: 107.2±16.5%→104.1±15.0%), or on the absolute intensity of the test stimulus in% of maximum stimulator output (BAC: 56.3±13.2%→56.6±12.6%; PBO: 55.3±12.2%→56.1±12.9%). Therefore, there were no changes in absolute or relative intensity of CS100 or the test stimulus that could have accounted for the significant drug effects on LICI. In addition, there was no change in the amplitude of the MEP elicited by the test stimulus alone (BAC: 1.23±0.35 mV→1.15±0.21 mV; PBO: 1.33±0.22 mV→1.15±0.34 mV) that could have been responsible for the drug effects on LICI.
There was a marked increase in LICI in all subjects in the BAC group, but in only two subjects in the PBO group, resulting in a significant interaction of drug and time (F 1,8=38.11, P<0.001, Fig. 1). Post hoc Student’s paired t tests showed that this was explained by a significant increase of LICI under BAC while there was no significant change of LICI under PBO (BAC: P=0.002; PBO: P=0.053, Table 1). LICI at baseline was not significantly different between the BAC and PBO sessions (P=0.162). The magnitude of LICI at baseline had no significant effect on the change of LICI produced by BAC, as indicated by a linear regression analysis with LICI at baseline as independent variable and the ratio of LICI (post/pre) as dependent variable (r=0.53, P=0.148). The positive but non-significant correlation coefficient strongly indicates that the effect of BAC on LICI was not confounded by the level of LICI at baseline.
In summary, BAC decreased SICI and increased LICI, while PBO produced no significant change. The changes of SICI and LICI under BAC were not correlated with each other (linear regression, r=−0.02, P=0.963).
Discussion
This study is the first to provide a direct evidence of the role of post-synaptic GABAB receptors in the mechanism of LICI. A single dose of the specific GABAB receptor agonist BAC increased LICI in healthy subjects, when tested with a standardized conditioning-test pulse protocol with an interstimulus interval of 100 ms (Valls-Sole et al. 1992; Nakamura et al. 1997; Chen et al. 1999). In addition, BAC resulted in a concomitant reduction in SICI, as tested with another standardized conditioning-test pulse protocol at an ISI of 3 ms (Kujirai et al. 1993; Ziemann et al. 1996c; Hanajima et al. 2003). There was no specific effect of BAC on RMT, AMT, MEP amplitude or CSP duration. The increase in RMT that occurred under both BAC and PBO was very minor (on average about 1% of maximum stimulator output). Therefore, it is not regarded as important in explaining the drug specific effects of BAC on LICI and SICI. There were also non-significant trends for MEP amplitude to decrease under both BAC and PBO and for LICI to weaken under PBO (Table 1). The reason for these slight changes are unclear but may be explained by a slightly reduced level of alertness during the course of the long experiment. The trend in LICI under PBO is not problematic because it strengthens, if anything, the validity of the LICI increase under BAC.
It is likely that, at the dose used in the present experiments, BAC alters spinal excitability. Intravenous infusion of 0.6 mg/kg BAC resulted in a depression of the H reflex/M wave ratio (Inghilleri et al. 1996). Other measures of spinal and neuromuscular excitability (peripheral silent period duration, amplitude of the maximum M wave) remained unchanged (Inghilleri et al. 1996). However, the measures of interest in the present study, SICI and LICI, test excitability of inhibitory neural circuits specifically at the level of motor cortex. Solid evidence supporting this view comes from epidural recordings from the cervical spinal cord (Nakamura et al. 1997; Di Lazzaro et al. 1998). These studies show a decrease in the number and amplitude of the multiple descending corticospinal discharges (in particular, late I-waves) with both protocols, pointing to the intracortical origin of both forms of inhibition. Even if a change in spinal excitability had contributed to the present findings, it would not explain the observed dissociation (decrease of SICI, increase of LICI). Therefore, it is safe to conclude that, even in the absence of measures on spinal excitability, the site of modulation of SICI and LICI by BAC is, not necessarily exclusively but to a significant extent, at the level of inhibitory circuits in the motor cortex.
The increase of LICI is most plausibly explained by facilitation of GABAB receptor mediated IPSPB in corticomotoneuronal neurons. Intracellular recordings from cortical neurons show that, in contrast to GABAA receptor mediated IPSPs (IPSPA), IPSPB typically last several hundreds of milliseconds (Connors et al. 1988; McCormick 1989; Avoli et al. 1997) and can be mimicked by application of BAC (McCormick 1989). Therefore, it is likely that, in the present experiments, facilitation of IPSPB by BAC led to stronger hyperpolarization of the corticomotoneuronal cells 100 ms after the conditioning pulse, and that this was associated with stronger inhibition of the conditioned MEP.
It was proposed that the CSP duration also reflects GABAB receptor mediated motor cortical inhibition (Siebner et al. 1998; Werhahn et al. 1999). The lack of effect of BAC on CSP duration in this and previous studies (Inghilleri et al. 1996; Ziemann et al. 1996b) does not disprove this view. However, this dissociation indicates that LICI and CSP durations are not identical processes. While LICI measures excitability of corticomotoneuronal cells to a second synchronized input elicited by the magnetic test pulse, CSP duration probes interruption of voluntary motor drive by a single pulse (Tergau et al. 1999). Consequently, LICI at a single interstimulus interval measures magnitude of inhibition while CSP measures duration of inhibition. The present results contrast with the finding that intrathecal administration of BAC resulted in a dose-dependent increase in CSP duration in a single patient with generalized dystonia (Siebner et al. 1998). However, since spinal inhibition contributes to the CSP (Ziemann et al. 1993) and measures of spinal inhibition were not investigated in that study, it remained unclear whether the lengthening of CSP duration was caused by enhancement of GABAB receptor mediated inhibition at the level of cortex or spinal cord, or both.
The mechanism for SICI has been established previously as a GABAA receptor mediated inhibition of motor cortex output cells (Ziemann et al. 1996a; Di Lazzaro et al. 2000, 2005a, b; Ilic et al. 2002). SICI has duration of approximately 20 ms (Hanajima et al. 1998) similar to IPSPA (Connors et al. 1988; McCormick 1989; Avoli et al. 1997), and is enhanced by benzodiazepines which are allosteric positive modulators of the GABAA receptor (Ziemann et al. 1996a; Di Lazzaro et al. 2000, 2005a, b; Ilic et al. 2002). SICI is reduced in the presence of LICI (Sanger et al. 2001). This finding supports the idea that SICI is controlled by pre-synaptic GABAB receptor mediated auto-inhibition on inhibitory interneurons, similar to pre-synaptic auto-inhibition revealed by paired intracellular recordings in slices of rat and human motor cortex (Deisz 1999a, b). Our findings confirm results from one previous report that showed a decrease of SICI under the GABA re-uptake inhibitor tiagabine (Werhahn et al. 1999). Those authors speculated already that this finding was most likely to be explained by GABAB receptor mediated pre-synaptic auto-inhibition of inhibitory interneurons but were unable to provide specific evidence because tiagabine increases the availability of GABA in the synaptic cleft and therefore increases, at the same time, neurotransmission through both GABAA and GABAB receptors. Our results now verify the specific role of GABAB receptors in controlling GABA release from inhibitory interneurons.
It should be noted that the SICI protocol (Kujirai et al. 1993; Ziemann et al. 1996c) does not, in contrast to protocols in slice experiments that measure paired-pulse IPSPA depression by means of intracellular recordings (see Deisz 1999a), specifically test pre-synaptic auto-inhibition of inhibitory interneurons but rather the effective magnitude of the IPSPA in motor cortex output neurons. The observed decrease of SICI after BAC intake compared to baseline is best explained by the assumption that pre-synaptic auto-inhibition of inhibitory interneurons is always active due to a certain level of sustained extracellular GABA and specifically facilitated by agonists of the GABAB receptor.
The results of this study are at variance with those of a previous report that showed a non-significant increase of SICI under BAC at an interstimulus interval of 3 ms (Ziemann et al. 1996b). The reasons for this discrepancy are not clear since the experimental protocols and the SICI baseline data in both studies are similar. The present study shows that the decrease of SICI under BAC is relatively weak and not present in all subjects. Therefore, one possibility to explain the discrepancy is genetic polymorphism of the GABAB receptor that may also play a role in drug addiction and certain forms of epilepsy (Sander et al. 1999). Certainly, future studies in larger samples of subjects are necessary to address this point.
We did not find a significant correlation between the individual increase in LICI and decrease in SICI. This strongly suggests that these two GABAB receptor controlled processes are different. This is supported by slice recordings in rat motor cortex that showed, for instance, that pre-synaptic auto-inhibition of inhibitory interneurons is unaffected by barium ions, despite the abolition of the IPSPB, indicating that the physiology of GABAB receptors differs between the pre-synaptic and post-synaptic effects (Deisz et al. 1997).
In conclusion, we have shown that GABAB receptors have a crucial role in intracortical inhibition, most likely through the activation of post-synaptic receptors mediating LICI and pre-synaptic auto-inhibition of inhibitory interneurons resulting in reduction of SICI. These findings are potentially important for future TMS research, for instance to assess patients with certain forms of epilepsy in which GABAB receptors may play a pathogenic role (Caddick and Hosford 1996).
References
Avoli M, Hwa G, Louvel J, Kurcewicz I, Pumain R, Lacaille JC (1997) Functional and pharmacological properties of GABA-mediated inhibition in the human neocortex. Can J Physiol Pharmacol 75:526–534
Bowery NG (1993) GABAB receptor pharmacology. Annu Rev Pharmacol Toxicol 33:109–147
Caddick SJ, Hosford DA (1996) The role of GABAB mechanisms in animal models of absence seizures. Mol Neurobiol 13:23–32
Chen R, Lozano AM, Ashby P (1999) Mechanism of the silent period following transcranial magnetic stimulation. Exp Brain Res 128:539–542
Connors BW, Malenka RC, Silva LR (1988) Two inhibitory postsynaptic potentials, and GABAA and GABAB receptor- mediated responses in neocortex of rat and cat. J Physiol (Lond) 406:443–468
Deisz RA (1999a) The GABA(B) receptor antagonist CGP 55845A reduces presynaptic GABA(B) actions in neocortical neurons of the rat in vitro. Neuroscience 93:1241–1249
Deisz RA (1999b) GABA(B) receptor-mediated effects in human and rat neocortical neurones in vitro. Neuropharmacology 38:1755–1766
Deisz RA, Billard JM, Zieglgansberger W (1997) Presynaptic and postsynaptic GABAB receptors of neocortical neurons of the rat in vitro: differences in pharmacology and ionic mechanisms. Synapse 25:62–72
Di Lazzaro V, Restuccia D, Oliviero A, Profice P, Ferrara L, Insola A, Mazzone P, Tonali P, Rothwell JC (1998) Magnetic transcranial stimulation at intensities below active motor threshold activates intracortical inhibitory circuits. Exp Brain Res 119:265–268
Di Lazzaro V, Oliviero A, Meglio M, Cioni B, Tamburrini G, Tonali P, Rothwell JC (2000) Direct demonstration of the effect of lorazepam on the excitability of the human motor cortex. Clin Neurophysiol 111:794–799
Di Lazzaro V, Oliviero A, Saturno E, Dileone M, Pilato F, Nardone R, Ranieri F, Musumeci G, Fiorilla T, Tonali PA (2005a) Effects of lorazepam on short latency afferent inhibition and short latency intracortical inhibition in humans. J Physiol 564:661–668
Di Lazzaro V, Pilato F, Dileone M, Tonali PA, Ziemann U (2005b) Dissociated effects of diazepam and lorazepam on short latency afferent inhibition. J Physiol 569:315–323
Fisher RJ, Nakamura Y, Bestmann S, Rothwell JC, Bostock H (2002) Two phases of intracortical inhibition revealed by transcranial magnetic threshold tracking. Exp Brain Res 143:240–248
Fuhr P, Agostino R, Hallett M (1991) Spinal motor neuron excitability during the silent period after cortical stimulation. Electroencephalogr Clin Neurophysiol 81:257–262
Garvey MA, Ziemann U, Becker DA, Barker CA, Bartko JJ (2001) New graphical method to measure silent periods evoked by transcranial magnetic stimulation. Clin Neurophysiol 112: 1451–1460
Hallett M (1995) Transcranial magnetic stimulation. Negative effects. Adv Neurol 67:107–113
Hanajima R, Ugawa Y, Terao Y, Sakai K, Furubayashi T, Machii K, Kanazawa I (1998) Paired-pulse magnetic stimulation of the human motor cortex: differences among I waves. J Physiol 509: 607–618
Hanajima R, Furubayashi T, Iwata NK, Shiio Y, Okabe S, Kanazawa I, Ugawa Y (2003) Further evidence to support different mechanisms underlying intracortical inhibition of the motor cortex. Exp Brain Res 151:427–434
Hill DR, Bowery NG (1981) 3H-baclofen and 3H-GABA bind to bicuculline-insensitive GABA B sites in rat brain. Nature 290:149–152
Ilic TV, Meintzschel F, Cleff U, Ruge D, Kessler KR, Ziemann U (2002) Short-interval paired-pulse inhibition and facilitation of human motor cortex: the dimension of stimulus intensity. J Physiol 545.1:153–167
Inghilleri M, Berardelli A, Marchetti P, Manfredi M (1996) Effects of diazepam, baclofen and thiopental on the silent period evoked by transcranial magnetic stimulation in humans. Exp Brain Res 109:467–472
Jones EG (1993) GABAergic neurons and their role in cortical plasticity in primates. Cereb Cortex 3:361–372
Kujirai T, Caramia MD, Rothwell JC, Day BL, Thompson PD, Ferbert A, Wroe S, Asselman P, Marsden CD (1993) Corticocortical inhibition in human motor cortex. J Physiol (Lond) 471:501–519
McCormick DA (1989) GABA as an inhibitory neurotransmitter in human cerebral cortex. J Neurophysiol 62:1018–1027
Nakamura H, Kitagawa H, Kawaguchi Y, Tsuji H (1997) Intracortical facilitation and inhibition after transcranial magnetic stimulation in conscious humans. J Physiol (Lond) 498:817–823
Rossini PM, Barker AT, Berardelli A, Caramia MD, Caruso G, Cracco RQ, Dimitrijevic MR, Hallett M, Katayama Y, Lücking CH, Maertens de Noordhout A, Marsden CD, Murray NMF, Rothwell JC, Swash M, Tomberg C (1994) Non-invasive electrical and magnetic stimulation of the brain, spinal cord and roots: basic principles and procedures for routine clinical application. Report of an IFCN committee. Electroencephalogr Clin Neurophysiol 91:79–92
Sander T, Samochowiec J, Ladehoff M, Smolka M, Peters C, Riess O, Rommelspacher H, Schmidt LG (1999) Association analysis of exonic variants of the gene encoding the GABAB receptor and alcohol dependence. Psychiatr Genet 9:69–73
Sanger TD, Garg RR, Chen R (2001) Interactions between two different inhibitory systems in the human motor cortex. J Physiol 530.2:307–317
Siebner HR, Dressnandt J, Auer C, Conrad B (1998) Continuous intrathecal baclofen infusions induced a marked increase of the transcranially evoked silent period in a patient with generalized dystonia. Muscle Nerve 21:1209–1212
Tergau F, Becher V, Canelo M, Wischer S, Wassermann EW, Ziemann U, Paulus W (1999) Complete suppression of voluntary motor drive during the silent period after transcranial magnetic stimulation. Exp Brain Res 124:447–454
Tokimura H, Ridding MC, Tokimura Y, Amassian VE, Rothwell JC (1996) Short latency facilitation between pairs of threshold magnetic stimuli applied to human motor cortex. Electroencephalogr Clin Neurophysiol 101:263–272
Valls-Sole J, Pascual-Leone A, Wassermann EM, Hallett M (1992) Human motor evoked responses to paired transcranial magnetic stimuli. Electroencephalogr Clin Neurophysiol 85:355–364
Watanabe M, Maemura K, Kanbara K, Tamayama T, Hayasaki H (2002) GABA and GABA receptors in the central nervous system and other organs. Int Rev Cytol 213:1–47
Werhahn KJ, Kunesch E, Noachtar S, Benecke R, Classen J (1999) Differential effects on motorcortical inhibition induced by blockade of GABA uptake in humans. J Physiol (Lond) 517:591–597
Ziemann U, Netz J, Szelenyi A, Hömberg V (1993) Spinal and supraspinal mechanisms contribute to the silent period in the contracting soleus muscle after transcranial magnetic stimulation of human motor cortex. Neurosci Lett 156:167–171
Ziemann U, Lönnecker S, Steinhoff BJ, Paulus W (1996a) The effect of lorazepam on the motor cortical excitability in man. Exp Brain Res 109:127–135
Ziemann U, Lönnecker S, Steinhoff BJ, Paulus W (1996b) Effects of antiepileptic drugs on motor cortex excitability in humans: a transcranial magnetic stimulation study. Ann Neurol 40:367–378
Ziemann U, Rothwell JC, Ridding MC (1996c) Interaction between intracortical inhibition and facilitation in human motor cortex. J Physiol (Lond) 496:873–881
Ziemann U, Tergau F, Wassermann EM, Wischer S, Hildebrandt J, Paulus W (1998) Demonstration of facilitatory I-wave interaction in the human motor cortex by paired transcranial magnetic stimulation. J Physiol (Lond) 511:181–190
Acknowledgements
MM and YO were supported by fellowships awarded by the German Academic Exchange Service (DAAD).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McDonnell, M.N., Orekhov, Y. & Ziemann, U. The role of GABAB receptors in intracortical inhibition in the human motor cortex. Exp Brain Res 173, 86–93 (2006). https://doi.org/10.1007/s00221-006-0365-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-006-0365-2