Abstract
Visceral leishmaniasis (VL) is a zoonotic infectious disease with a severe impact on humans and animals. Infection is transmitted by phlebotomine sand flies, and several domestic and wild mammals act as reservoirs for the infection, so the prompt detection of infected hosts is crucial to preventing and controlling the spread of the disease and its transmission to humans. A rapid and portable tool for VL diagnosis based on the lateral flow immunoassay (LFIA) technology is described herein. The device exploits a highly specific chimeric recombinant antigen as the recognition element for capturing anti-leishmanial antibodies, and protein A labelled with gold nanoparticles as the signal reporter. The LFIA shows excellent diagnostic sensitivity (98.4%), specificity (98.9%), and agreement with serological reference methods for diagnosing canine VL. The long-term stability of the LFIA device was confirmed based on six months of storage at room temperature or 4 °C, and the qualitative response of the device was not affected by limited thermal stress. The use of the broadly specific protein A means that the LFIA can be readily adapted to diagnose VL in dogs (the main reservoir for human infection) and other mammals, thus further assisting efforts to control the spread of VL.

A rapid and portable diagnostic tool for visceral leishmaniasis (VL) based on lateral flow immunoassay (LFIA) technology. The presence of anti-leishmanial antibodies is revealed through the binding of these antibodies to a highly specific chimeric antigen. Employing a broadly specific signal reporter (protein A labelled with gold nanoparticles) enables the LFIA to be easily adapted to diagnose VL in different animals
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Visceral leishmaniasis (VL) is a zoonotic disease caused by the protozoan parasite Leishmania infantum, which is transmitted to vertebrate hosts through the bites of infected female phlebotomine sand flies that are endemic to many countries throughout Latin America and Asia [1]. It is ranked second in mortality and fourth in morbidity among tropical diseases, and is considered one of the world’s most neglected diseases by the WHO (World Health Organization) [2]. In European countries, the incidence of VL is still relatively low, although the disease is spreading to regions in which it was previously considered nonendemic, probably because of climate change and population movements [3, 4]. The impact of VL on human health is severe and characterised by fever, weight loss, splenomegaly, hepatomegaly and anaemia [1]. It is estimated that there are more than 700,000 new cases of human VL (HVL) and about 20,000–30,000 deaths due to HVL annually worldwide [5]. Although Leishmania amastigotes infect more than 70 vertebrate hosts, domestic dogs are considered the main reservoir for human infection [1,2,3]. Infected dogs have highly variable clinical manifestations that range from apparently healthy to severely diseased. Many infected dogs never exhibit clinical signs of VL, thus making it difficult to detect canine visceral leishmaniasis (CVL) early [6]. Nevertheless, both symptomatic and asymptomatic dogs are able to transmit the parasite to other dogs and humans [3]. Therefore, early detection and prompt treatment of infected animals help to reduce transmission and represent an important part of the strategy for preventing and controlling VL in humans.
CVL can be diagnosed by combining clinical and epidemiological parameters with parasitological, serological or molecular methods [1]. According to the World Organisation for Animal Health [7], serology is the preferred diagnostic method for CVL. In particular, the detection of anti-leishmanial antibodies is commonly realized by three techniques: the immunofluorescent antibody test (IFAT), the enzyme-linked immunosorbent assay (ELISA), and the lateral-flow immunoassay (LFIA). The IFAT is considered the reference method for anti-leishmanial serology in dogs, and is used as the reference test when validating new diagnostic methods, though data on its diagnostic sensitivity and specificity are controversial [3]. Furthermore, IFAT suffers from operator-dependent variability. The ELISA is also very sensitive and specific, with the advantage of easier standardisation [8]. Both IFAT and ELISA provide quantitative results, defined as the antibody titre (the last twofold serial dilution of the sample that provided a positive result). However, the rapid and cost-effective detection of infected dogs is key to controlling VL infection and transmission. LFIA, also known as immunochromatographic assay (ICA) and the immunochromatographic strip test (ICST), is the most popular diagnostic tool for rapid onsite assays. A major advantage of LFIA is that it fulfils all of the ASSURED criteria required for point-of-care testing (affordable, sensitive, specific, user-friendly, rapid/robust, equipment-free and deliverable to end users) [9], which explains its rapid spread and huge commercial success. Nevertheless, LFIA only provides qualitative results (i.e. the subject is healthy/sick), which need to be complemented by quantitative information to ensure that the disease is managed correctly. Several commercial LFIA devices are available [10,11,12,13] that differ in their simplicity of use, rapidity and sensitivity [6]. The specificity of these tests is generally high, while the diagnostic sensitivity is usually low (30–70%) and largely dependent on leishmaniasis stage [6, 8]. A limited sensitivity strongly reduces the effectiveness of infection transmission control, frustrating attempts to prevent the spread of the disease in humans.
In addition to inadequate sensitivity, existing LFIA kits for diagnosing leishmaniasis are designed to detect only CVL and HVL. Although dogs are considered the most important domestic reservoir of L. infantum, several species of wild mammals are known to be hosts and potential reservoirs of Leishmania parasites [14]. In addition, domestic mammals (sheep, goats, cattle and donkeys) have been proposed as the reservoir hosts responsible for a HVL outbreak in 2008–2009 in China [15]. Therefore, versatile diagnostic tools that can be adapted for VL diagnosis in mammals other than dogs are also needed.
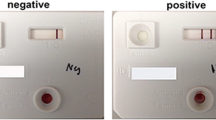
In this work, we describe the design of a rapid diagnostic tool for detecting anti-leishmanial antibodies that shows high diagnostic sensitivity and versatility, as it can be adapted for use with other mammals besides dogs and humans. This rapid test for diagnosing VL is a lateral flow immunoassay based on the one-site immunometric assay format. The specific recognition element is a recombinant chimeric antigen (rCAg) comprising three Leishmania antigens, which has been shown to be highly specific for VL [16, 17]. The signal reporter is staphylococcal protein A (pA) labelled with gold nanoparticles (GNPs), which are used as coloured probes that permit visual interpretation of the qualitative result. Anti-leishmanial antibodies present in the sample bind to the chimeric antigen forming the so-called test line, and the rate of formation of the complex is measured by reaction with the labelled protein A. The protein A, which is also used for the control line, captures any excess immunoglobulins, regardless of their specificity for the leishmanial antigen. Again, the captured immunoglobulins are revealed by protein A labelled with GNPs. Therefore, two coloured lines form if anti-leishmanial antibodies are present in the sample, due to the accumulation of GNP-pA at both the test and control zones. Only the control line is visible if the sample does not contain any anti-leishmanial antibodies (Fig. 1).
Scheme of the LFIA device used for the rapid diagnosis of VL. The strip is composed of an analytical membrane onto which a recombinant chimeric antigen (rCAg) and protein A (pA) are coated to form the test and control lines, respectively. The signal reporter consists of pA labelled with gold nanoparticles that are coloured red due to a surface resonance band at 525 nm. GNP-pA is included in the device in dried form by pre-impregnating the probe pad. The device also includes a sample pad that adsorbs the sample and distributes it homogeneously to the membrane, and an adsorbent pad that decreases the background colour by increasing the volume of the flowing sample. A single visible line (Ctrl) is expected for a canine serum that does not contain any anti-leishmanial antibodies (negative sample) due to the interaction of generic immunoglobulins with the labelled pA and with the pA immobilised on the membrane. The presence of specific anti-leishmanial antibodies is revealed by the specific binding of these antibodies to the rCAg, which generates a second red line (Test)
The use of protein A as a generic recognition element that confers versatility to the assay, due to the ability of pA to bind immunoglobulins from various animal species, has been reported for ELISA methods [18,19,20]. Some LFIAs have also employed protein A/G as the labelled probe in combination with immunoglobulins as the capture reagent at the control line [21]. However, VL is commonly associated with hypergammaglobulinemia [22], and high levels of gamma globulins can saturate the binding capacity of the pA-GNP probe, thus preventing it from reacting with the immunoglobulins forming the control line. The effect of this is an unacceptably high probability of an invalid result (control line not visible, Fig. 2). To overcome this limitation, we also used pA as the capture reagent on the control line. This allows the LFIA for diagnosing VL to be modified to detect anti-leishmanial antibodies belonging to different mammalian species while also assuring the validity of the test, even for subjects showing abnormal levels of immunoglobulins.
Typical results provided by the LFIA for detecting anti-leishmanial antibodies when exposed to positive and negative canine sera. Negativity is represented by the presence of a single red line (the control line, Ctrl), while positivity is observed as the presence of two red lines (the Test and Ctrl lines) after running the sample. The strip is enclosed in a plastic cassette that provides a sample well and a reading window. The test is invalid when only the test line is visibly coloured
Materials and methods
Immunoreagents, chemicals and materials
Gold (III) chloride trihydrate (ACS reagent), protein A (pA), bovine serum albumin (BSA), rabbit immunoglobulins, swine immunoglobulins and polyvinyl alcohol (PVA) were obtained from Sigma–Aldrich (St. Louis, MO, USA). Triton X-100 and other chemicals were purchased from VWR International (Milan, Italy). Anti-dog IgG was purchased from Sigma–Aldrich.
Nitrocellulose membranes (HF180 plus card), cellulose adsorbent pads and glass fibre conjugate pads were obtained from Merck Millipore (Billerica, MA, USA). Standard 14 glass fibre pads from Whatman (Little Chalfont, UK) were used as sample pads.
K9-K39-K26 recombinant chimeric antigen (rCAg) was prepared as described in [17].
Statistical calculations were carried out with SigmaPlot 11.0 software.
Preparation of GNPs and GNP–protein A conjugates (GNP-pA)
GNPs with a SPR band at 525 nm and a mean diameter of ca. 30 nm were prepared by tetrachloroauric acid reduction with sodium citrate [23]. Briefly, 1 mL of 1% w/v sodium citrate was added to 0.01% of boiling tetrachloroauric acid under vigorous stirring. The colour of the solution changed gradually from light yellow to red, indicating the successful formation of gold nanoparticles. Signal reporters used in the LFIA were prepared by adsorbing protein A onto GNPs. In detail, 8 μg of pA and 1 ml of borate buffer (pH 7.4) were mixed with 10 ml of GNPs and incubated for 30 min at 37 °C. Next, 1 ml of BSA (1% in borate buffer) was added and reacted for 10 min at 37 °C to saturate the free GNP surface. GNP-pA conjugates were recovered by centrifugation (14,000 rpm, 15 min) and washed twice with borate buffer supplemented with 0.1% BSA. Finally, the GNP-pA was resuspended in GNP storage buffer (borate buffer with 1% BSA, 0.25% Tween 20, 2% sucrose and 0.02% sodium azide) and stored at 4 °C until use.
Fabrication of the LFIA device
The recombinant chimeric antigen [17] was applied to the nitrocellulose (NC) membrane to form the test line (0.5 mg/ml). Protein A (0.2 mg/ml) was used as the capture reagent at the control line. Reagents were dotted at 1 μL cm−1 by means of a XYZ3050 platform (Biodot, Irvine, CA, USA) equipped with a BioJet Quanti™ 3000 line dispenser for noncontact dispensing, keeping a distance of 4 mm between the lines. The signal reporters (GNP-pA conjugates) were adsorbed onto the glass fibre conjugate pad that had previously been saturated with GNP storage buffer. The pad was dipped into GNP-pA solution (optical density 1) and dried for 3 h at room temperature. NC membranes were dried at 37 °C for 60 min under vacuum, layered with sample, conjugate and adsorbent pads (Fig. 1), cut into strips (4.2 mm width) by means of a CM4000 guillotine (Biodot), and inserted into plastic cassettes (Kinbio, Shanghai, China) to fabricate the ready-to-use LFIA device. Cassettes were stored in the dark in plastic bags containing silica at room temperature until use.
The lateral flow immunoassay for diagnosing canine leishmaniasis
Assays to detect anti-leishmanial antibodies were carried out at room temperature by applying 70 μl of diluted serum to the sample well. For the analysis, the samples were thawed at room temperature, carefully mixed and then diluted 1:20 using the running buffer (phosphate buffer 20 mM, pH 7.4, 50 mM NaCl, 1% BSA, 0.5% PVA, 0.1% Triton X-100).
Qualitative results were judged by the naked eye after 15 min (Fig. 2). Samples were analysed in duplicate and results were observed by three operators. Images of LFIA devices were also acquired by a portable scanner (OpticSlim 550 scanner, Plustek Technology GmbH, Norderstedt, Germany), and the area of the coloured lines was quantified by means of QuantiScan 3.0 software (Biosoft, Cambridge, UK).
Serum samples
A total of 167 canine sera were used in the study; 37 serum samples were collected in a region in which VL is endemic (West Liguria, Italy), while 130 samples were obtained in a region in which VL is nonendemic (Piemonte and Valle d’Aosta, Italy). Most canine sera were characterised by analysing them using more than one reference method: IFAT titration was carried out on 157 samples, PCR and western blot (WB) were carried out on 120 samples, and 141 canine sera were analysed by a previously validated ELISA (enzyme-linked immunosorbent assay) that was based on the same recombinant chimeric antigen employed in the LFIA [20]. Samples belonging to the region in which VL is nonendemic were characterised by IFAT, PCR and WB. In order to classify canine sera, the IFAT cutoff was set at 1/80 [3, 6, 8, 20], while PCR and WB were carried out according to the protocols described in Ferroglio et al. [24].
In detail, 70 samples showed IFAT titres of <1/40 and were also negative according to the PCR and WB methods; 40 samples showed IFAT titres of >1/80 and were also positive according to the PCR and WB methods; 10 samples were analysed using WB and PCR and were found to be positive. Those samples were also analysed by the ELISA, which classified 5 samples as positive and 5 as negative.
Samples belonging to the region in which VL was nonendemic were classified according to either IFAT titre or ELISA score; in particular, 7 samples that were inconclusively classified (IFAT = 1/80) were analysed by the ELISA method. A further 102 samples were randomly chosen from among those already characterised by other reference methods and were submitted to ELISA qualification too.
To evaluate the potential applicability of the assay to different animal species, 2 red fox sera (1 IFAT positive and 1 negative) and 9 cat sera were also analysed. The cat sera were characterised by PCR and WB; however, the results were ambiguous and were considered inconclusive. The fox and cat samples were analysed by the versatile LFIA and by the reference ELISA (which also employed protein A as the probe, although conjugated to horseradish peroxidase).
Validation of the LFIA device for detecting leishmaniasis in canine serum
The impact of the serum matrix on the assay was studied by variably diluting a pool of positive and a pool of negative canine sera with phosphate buffer supplemented with various additives. In order to limit matrix interference, the following chemicals were considered: proteins (BSA, casein), surfactants (Tween 20, Triton X-100), polymers (polyvinyl alcohol) and salts (NaCl). Each additive was added to phosphate buffer at three different levels and used to dilute pooled sera 1:10 before LFIA analysis. In addition, the same compounds were also used to impregnate the sample pad, as an alternative to sample dilution.
The accuracy of the assay was calculated as the proportion of the results for the canine sera that agreed with those provided by the reference methods (IFAT and ELISA). Cohen’s κ parameter was calculated to evaluate the concordance of the new LFIA with serological reference methods.
The imprecision of the LFIA was considered to be the sum of three components: the within- and between-day variations due to the assay, and the biological variability. Accordingly, overall imprecision was estimated using an experimental design approach first proposed by Lattanzio et al. [25, 26], although we made minor modifications to this approach due to the availability of biological samples [27]. The study was conducted by analysing 11 sets of canine serum, of which 7 were positive and 4 negative. The samples were analysed on two days. On each day, the samples were analysed in triplicate. Negative samples and positive samples were used to calculate the proportions of false positives (n = 24) and false negatives (n = 42), respectively.
Robustness, in terms of the reliability of the assay response over time, was also studied. For that purpose, 10 serum samples (5 positive and 5 negative) were analysed in duplicate and the results were observed 10, 20 and 60 min after sample application. The false-positive (n = 10) and false-negative (n = 10) rates were calculated at each observation time.
Stability of the LFIA device
In order to evaluate the shelf-life of the LFIA device, real-time stability and accelerated ageing experiments were carried out as follows [27, 28]. For the accelerated ageing experiment, LFIA cassettes were kept at 37 °C for 7 days and tested on days 0, 1, 3 and 7. For the real-time stability experiment, LFIA cassettes were stored at room temperature and 4 °C for 6 months and tested in weeks 0, 1, 2, 4, 8, 12 and 24. For each experiment, a pool of positive samples and a pool of negative samples were analysed in duplicate. For all experiments, LFIA devices were stored in the dark and with desiccant added.
Results and discussion
Optimization of the LFIA device
The LFIA device was designed to be a versatile tool for diagnosing leishmaniasis in various animal species. Hence, protein A was used as a broadly selective recognition element and was labelled with gold nanoparticles to fabricate the signal reporter (Fig. 1). The same protein was also used as the capture reagent in the control line. Attempts were made to use immunoglobulins from other animal species that are known to bind pA (rabbit and swine) as the C-line capture reagent, according to the strategy proposed by Intaramat et al. [21]. However, the rate of invalid test results (i.e. where the control line was not visible) was unacceptably high due to the inability of the GNP-pA probe to bind to the immunoglobulins immobilised at the C-line. Subjects infected with VL also show hypergammaglobulinemia [22], which saturates the binding capacity of the labelled pA. Using an anti-canine antibody partially solved the problem, but at the expense of assay versatility. Therefore, we opted to use the same pA as the C-line reagent. In this way, the LFIA is putatively able to reveal immunoglobulins from any animal species that are bound by pA.
The specificity of the LFIA is connected to the recognition element deposited on the test line, which is a recombinant chimeric antigen (rCAg) from the amastigote form of the Leishmania parasite [17]. In detail, the rCAg comprises three antigenic domains (K9, K39 and K26) from L. infantum [11], and has been shown to allow the highly sensitive and specific detection of anti-leishmanial antibodies by ELISA [20]. Most importantly, the rCAg is representative of the form of the leishmanial amastigote antigens that are expressed in vertebrates, enabling infected subjects to be discriminated from those who just came into contact with the phlebotomine vector. This is particularly relevant when attempting to correctly identify infected subjects in VL-endemic areas, where the probability of accidental contact with the vector is high but such contact does not necessarily lead to the development of VL [29].
We set up the LFIA and tuned its parameters in order to produce a rapid, sensitive and easy-to-handle device using a checkerboard strategy in which the concentrations of the signal reporter (GNP-pA), the recognition element for the test line (rCAg) and the capture reagent (pA) for the control line were varied. Pooled positive and negative canine sera were used during the optimisation to mitigate the influence of biological variability. The experimental conditions for the optimal conjugation of pA with gold nanoparticles were identified beforehand. The optimal pH and pA concentration were established by finding the best compromise between stable GNP-pA conjugates [30] and high VL detectability of the device [31].
The protocol for executing the assay includes the dilution of serum with a running buffer. This additional step makes it more difficult for untrained personnel to use the device, and for it to be applied in low-resource settings. However, this step is required for two main reasons. On the one hand, serum is a viscous liquid that barely flows across the LFIA membrane. As a consequence, the application of an undiluted sample lengthens the analysis time and increases the rate of irreproducible results. Most importantly, the false-negative rate was unacceptably high due to the hook effect associated with the hypergammaglobulinemia of subjects infected with VL [22]. The minimum degree of sample dilution required to obtain a clearly visible signal at the test line for most positive samples in a reasonable time (15 min) was found to be 1:20. Lower dilution factors (e.g. 1:10) permitted acceptable diagnostic sensitivity at the expense of rapidity (accurate results were observed >60 min after sample application). Commercial LFIA kits also dilute the serum, typically by adding a larger volume of a diluent immediately following the application of a limited volume of the sample [10,11,12,13].
The composition of the running buffer was optimised with the aim of guaranteeing rapidity, high detectability and reduced sample-to-sample result variation. For this purpose, several modifiers were added to the phosphate buffer, such as BSA, PVA, NaCl and Triton X-100. PVA was found to be especially useful for rapidly and completely redissolving the dried GNP-pA, while NaCl efficiently abated nonspecific binding of the GNP-pA to the rCAg at the test line, thus dramatically reducing the false-positive rate.
Analytical parameters of the LFIA for the qualitative detection of anti-leishmanial antibodies in canine serum
The precision of the LFIA device was investigated using an approach that was first proposed by Lattanzio et al. [25] and has since been widely applied to assess qualitative LFIA performance [26, 27]. This strategy involves designing a set of experiments that include three factors which potentially contribute to the overall precision of the assay, namely the within-day, between-day and biological variability. Therefore, tests of seven positive and four negative serum samples were performed and replicated on the same day and on two distinct days. Positive samples included sera with high and low IFAT titres. No false-positive (n = 42) nor false-negative (n = 24) results were registered during the assessment, indicating that the LFIA is precise enough to permit the reproducible detection of anti-leishmanial antibodies in canine serum. The mean coefficients of variation were calculated for the positive canine sera by digitalizing images of the cassettes and converting them into quantitative data [23]. The area under the test line (“AreaT”) was measured and used as the quantitative parameter when determining the repeatability and reproducibility. The mean coefficients of variation were calculated as 14.6% (n = 12) and 15.5% (n = 6) for the within- and between-day experiments, respectively (Fig. 3a). The mean values of AreaT for the two days were compared by one-way analysis of variance (ANOVA). The observed difference between the results obtained on the two days was not statistically significant (P = 0.145), although the power of the test was found to be below the desired value (0.199 with alpha = 0.050).
In-house validation of the LFIA for detecting anti-leishmanial antibodies. a Within- and between-day variability of the LFIA response; bars represent standard deviations based on the three replicates performed each day in the between-day experiment. b Stability of the LFIA response over time for six positive samples. c Shelf-life of the LFIA device as measured at 4 °C (circles) and room temperature (squares). d Thermal stability of the LFIA device at 37 °C. Bars in b–d represent the standard deviations based on two replicates
High variability was observed among the canine samples, but this was expected as the samples were expressly chosen for their wide range of IFAT titres. Even though the LFIA is not able to provide quantitative results, variations in the content of anti-leishmanial antibodies in the samples were reflected in differently coloured test lines—the higher the content of antibodies, the more strongly coloured the test line, and vice versa.
A frequent issue with LFIAs for serological application is changes in the visual result over time. In particular, negative results (i.e. an assay in which only the control line is visibly coloured) have the tendency to become positive (the test line becomes coloured too). In order to define the minimum time required for the LFIA to produce a reliable response, and to verify the robustness of this response over time, the LFIA was used to detect anti-leishmanial antibodies in ten canine sera, and the results were observed at 10, 20 and 60 min after sample application. Four negative and six positive samples were analysed. Among the positive samples, three were characterised by high IFAT titres (≥1/640) and three by low IFAT titres (<1/640). Each sample was tested in duplicate and results were observed with the naked eye. Colour at the test line indicating positivity was detectable after ten minutes for all positive samples; this colour increased over the following 10 min and then stabilised (Fig. 3b). As a precaution, we set 15 min as the time needed to obtain a reliable response for samples characterised by low IFAT titres. Most interestingly, no colour was visible at the test line after 60 min for negative samples, and this was the case for all negative samples analysed during LFIA validation. Therefore, the LFIA demonstrated a very stable response over time.
Validation of the LFIA as a rapid tool for the serological diagnosis of canine leishmaniasis
The ability of the LFIA to correctly identify subjects infected with CVL was studied by analysing sera from a total of 167 dogs from both CVL-endemic (37 subjects) and CVL-nonendemic (130 subjects) areas.
Considering that there is no gold-standard reference method for diagnosing VL and that all of the analytical methods that are commonly employed show some limitations [1, 3, 8, 32,33,34,35], we opted to classify canine serum based on IFAT and ELISA responses. Indeed, the IFAT is commonly regarded as the reference when validating new diagnostic tools [1,2,3]. On the other hand, the ELISA used in the study was based on the same capture antigen used in the LFIA device. Thus, we considered that any discordance between the two methods would be attributable to the functioning of the LFIA itself and not to the specificity of the capture reagent. For the same reason, we only interpreted the LFIA result qualitatively (i.e. whether or not colour was present at the test line); we did not attempt to quantitatively correlate the LFIA output with the IFAT titre.
Most samples were characterised by the serological reference method and were classified as positive/negative based on the general assumption that IFAT titres above 1/160 and below 1/40 are considered unequivocally positive and negative, respectively. IFAT titres in the range between 1/40 and 1/80 are considered controversial [6, 33], although the 1/80 level is commonly considered the threshold level [3, 6, 8]. The sensitive and specific ELISA was used to confirm the classification of samples with ambiguous titres and to assign samples without IFAT titres. Another 102 sera were also analysed by the ELISA. Most of the results obtained using the ELISA were in agreement with those provided by the IFAT. However, 11 samples gave conflicting results for the two reference methods. These samples belonged to a CVL-nonendemic area and were classified as positive by the IFAT and negative by the ELISA. The difference between the results of the two methods can be explained by noting that the two reference techniques utilize different antigens. In particular, the ELISA employed the same chimeric antigen as the LFIA and was therefore more specific for antibodies against Leishmania amastigotes, while IFAT employs an antigen relating to Leishmania promastigotes. Thus, samples were classified as true negatives if they had an IFAT titre below the cutoff titre (1/80) and a negative ELISA score [20]. Positivity was assigned to samples with an IFAT titre above the cutoff titre (1/80) and a positive ELISA score. Sera with an IFAT titre at the cutoff level (1/80) or with no IFAT titre were classified based on the ELISA score only. Accordingly, 93 true-negative samples, 63 true-positive samples, and 11 ambiguous samples (positive according to IFAT, negative according to ELISA) were analysed by the LFIA during the study.
Samples were blindly analysed using the LFIA in duplicate and were judged positive based on the presence of two visible lines. The visual result of each test was assessed by three different operators, who observed the LFIA devices with the naked eye 15 min after the application of the sample. Agreement was obtained among replicate measurements and among the observations of the three operators for all canine sera.
From these results, we obtained the figures of merit used to validate the qualitative LFIA (Table 1). In particular, we calculated the diagnostic sensitivity (Se) of the test, defined as the rate of true-positive results, and we calculated the diagnostic specificity (Sp) of the test, defined as the rate of true-negative results [36]. The LFIA furnished one false-negative result for a canine serum sample obtained in the CVL-endemic region. This sample had an IFAT titre of 1/80, which is considered controversial and, especially for animals living in the CVL-endemic area, can be related to an initial phase of the infection. A false-positive result was observed for a sample belonging to the CVL-nonendemic area; this sample was classified as negative by both reference methods. Nevertheless, the LFIA demonstrated very high diagnostic sensitivity (98.4%, 95% confidence interval 91.47–99.96%) and specificity (98.9%, 95% confidence interval 94.15–99.97%), thus confirming its applicability for the accurate diagnosis of CVL. The sensitivity achieved was higher than those of other rapid test kits, especially considering that the LFIA was also able to correctly discriminate samples with very low IFAT titres (1/40 and 1/80) whereas previously reported assays failed to classify such samples. Low IFAT titres can be associated with the early stage of infection, so the proposed LFIA is an effective tool for preventing and controlling CVL infection transmission as it enables early diagnosis.
Canine sera that yielded conflicting results with the reference methods were not considered when calculating the diagnostic sensitivity and specificity of the LFIA. They were, however, included in the comparison of the LFIA with the reference methods (Table 2) in terms of accuracy. For this purpose, the samples were classified in accordance with the response of each individual reference method considered. The LFIA provided 8 positive and 3 negative results for the ambiguous samples, meaning that it was in closer agreement with the IFAT reference results than the ELISA results, despite the fact that the ELISA method used the same antigen specific for Leishmania amastigotes as employed in the LFIA. The accuracy of the test, defined as the proportion of the samples that were correctly classified, was ca. 97% or 93% when the IFAT or the ELISA method was used as the reference, respectively.
The concordance of the LFIA with the two reference methods was estimated via Cohen’s κ [36]. Excellent concordance with both reference methods was observed. Moreover, upon comparing the LFIA to the IFAT, which is generally considered the gold standard reference method for leishmaniasis diagnosis, the κ value exceeded 0.9, indicating very high concordance.
Shelf-life study
Long-term and thermal stability are crucial attributes for LFIA devices because they are intended for use in the field. However, most materials and bioreagents included in the device are intrinsically sensitive to environmental conditions.
The long-term stability of the LFIA device stored at 4 °C and at room temperature was investigated over a period of six months. LFIA cassettes were packed individually, protected from the light, and placed in the presence of a desiccant. A positive and a negative control were correctly attributed, based on visual observation of the colour at the test line. Quantification of the coloured area confirmed the visual observations (Fig. 3c). Although we observed a slight decrease in the test line colour starting from day 7 compared to that measured at day 0 at both temperatures, we found that the LFIA was acceptably stable during the six-month period and did not require a specific storage temperature.
In addition, accelerated ageing of the LFIA was carried out by maintaining the LFIA device at 37 °C for one week. This experiment led us to conclude that the LFIA device is insensitive to the limited increases in temperature (Fig. 3d) that typically occur in the field (i.e. temperature fluctuations during the summer season, storage in an unconditioned environment for short periods), and is therefore robust enough for usage in the field.
Application of the LFIA for the diagnosis of VL in other animal species
Although dogs are considered the main reservoir for VL, other mammalian reservoirs have been reported and implicated in the transmission of the infection to humans [14, 15]. Companion animals such as cats can be infected by L. infantum and transmit the infection to sand flies [37], and several species of wild animals have been found to be infected in Europe [38]. In the past, wild species were considered secondary reservoirs or occasional hosts; however, the recent focus on the >600 human cases in Madrid highlights the risk of VL spreading from wildlife to humans [38]. One major barrier to a better understanding of the dynamics of the interactions between VL hosts and reservoirs is the lack of availability of diagnostic methods for animals other than dogs. Most serological methods use probes that are specific for canine immunoglobulins; those protocols must be modified significantly to allow the detection of anti-leishmanial antibodies from other mammals. That said, a broadly specific serological assay for VL diagnosis in dogs and humans in the ELISA format has also been developed by the present research group [20], based on a similar strategy to that used by the LFIA. Protein A labelled with an enzyme was exploited as a versatile probe that is capable of revealing both human and canine anti-leishmanial antibodies. To demonstrate the versatility of the LFIA and its ability to be adapted to detect anti-leishmanial antibodies produced by diverse animal species, two sera from red foxes and nine from cats were analysed by the protocol optimised for CVL diagnosis. The red fox sera were characterised by IFAT titration; one was found to be positive and the other negative. PCR and WB analyses provided somewhat conflicting classifications of the feline sera, so they were analysed by the reference ELISA. The ELISA provided a positive response for the red fox sample classified as positive by IFAT, and for three feline samples. The observed disagreement between the results of the molecular and serological techniques has also been noted previously for cats [37], and it appears to be due to significant differences between the immune responses of cats and dogs, as the low number of clinical cases of VL in cats demonstrates.
LFIA analysis was conducted with two replicates. No invalid tests were observed, which means that the GNP-pA probe is suitable for adapting the LFIA to allow it to diagnose VL in cat and red fox sera. Furthermore, the LFIA results for the red fox sera matched those obtained by both reference methods (ELISA and IFAT). Regarding feline sera, three samples were classified as positive and six as negative (Fig. 4), leading to excellent concordance with the reference ELISA. The observed discordance with PCR was attributed to the variability of the results from molecular and serological diagnostic methods, which is often mentioned in the rather scarce literature in this research area [37]. More interestingly, the strategy used to develop the LFIA, based on the broadly specific GNP-pA probe, enabled the detection of immunoglobulins from different mammals (dogs, cats and red foxes), and the recombinant chimeric antigen was able to capture anti-leishmanial antibodies from other carnivores.
Conclusions
Tests available on the Brazilian market for the rapid diagnosis of CVL have had their performance reviewed by Woyame-Pinto et al. [6]. Although validation studies were heterogeneous in sample size and in regard to the reference methods used to classify the samples (IFAT, ELISA, PCR), some conclusions can be drawn. Ignoring the Rapidtest assay, which was validated about ten years earlier than the others, the diagnostic specificities of existing point-of-care tests for CVL ranged from 90.6% (for the SNAP Leishmania Test [10]) to 100% (for the Kalazar Detect assay [11]). Sensitivity ranged from 32.6% (Kalazar Detect) to 98% (Dual Path Platform, dpp®) [12], with strong variability depending on the phase of the disease. In particular, asymptomatic dogs were only rarely considered to be sick by most of the rapid tests reviewed (sensitivity: 32.6–94.7%), while symptomatic animals were more easily identified as infected (sensitivity: 77–98%). The highest sensitivity was provided by the dpp® test (98%). Another LFIA kit for CVL diagnosis, the Speed Leish K test [13], was validated in a study by Ferroglio et al. [35]. Its sensitivity and specificity were found to be 96.3% and 100%, respectively, when calculated for canine sera with high IFAT titres (>1/160), which likely correspond to animals with clinical signs of infection or in which the disease is at an advanced stage [35]. Otranto et al. validated a LFIA for CVL based on a recombinant K39 antigen that provided 97.06% sensitivity and 100% specificity [36].
The LFIA for detecting canine anti-leishmanial antibodies developed in this study has a higher sensitivity (98.4%) than other LFIAs, and the validation also included subjects with low IFAT titres. Therefore, it has been shown to be a reliable tool for the accurate early detection of CVL. The specificity of the present LFIA is comparable to the mean specificity of the LFIA kits for leishmaniasis diagnosis that are currently on the market. The present LFIA device is also robust, as the visual output was found to remain stable over time and to be unaffected by occasional increases in temperature. It showed long-term stability (up to six months) without requiring refrigeration. In conclusion, it is suitable for use in the field by untrained personnel and in low-resource settings.
Furthermore, due to the design of the assay, it can easily be modified to allow it to diagnose VL in other companion animals and wild carnivores that are known to play a role in VL transmission. This versatility should aid attempts to control VL transmission in a timely and efficient way.
The LFIA provides a qualitative yes/no response, meaning that it can be used as an initial screening test. When the LFIA gives a positive result, a quantitative serology method (ELISA or IFAT) can then be performed to better determine the stage of infection and the most appropriate treatment.
References
Solca MDS, Bastos LA, Guedes CES, Bordoni M, Borja LS, et al. Evaluating the accuracy of molecular diagnostic testing for canine visceral leishmaniasis using latent class analysis. PLoS ONE. 2014;9(7):e103635. https://doi.org/10.1371/journal.pone.0103635.
Adams E, Hasker E, Cunningham J. Visceral leishmaniasis rapid diagnostic test performance. Diagnostic evaluation series no. 4. Geneva: World Health Organization; 2011.
Adel A, Berkvens D, Abatih E, Soukehal A, Bianchini J, Saegerman C. Evaluation of immunofluorescence antibody test used for the diagnosis of canine leishmaniasis in the Mediterranean Basin: a systematic review and meta-analysis. PLoS One. 2016;11(8):e0161051. https://doi.org/10.1371/journal.pone.0161051.
Ferroglio E, Maroli M, Gastaldo S, Mignone M, Rossi L. Canine leishmaniosis in Italy. Emerg Infect Dis. 2005;11:1618–20.
World Health Organization. Media centre: Leishmaniasis.http://www.who.int/mediacentre/factsheets/fs375/en/. Accessed 23 Jan 2018.
Woyames Pinto AJ, Ribeiro VM, Tafuri WL. The immunochromatography use in canine visceral leishmaniasis in Brazil: a “quick solution” of a complex diagnostic? Rapid test in dogs with leishmaniasis. Ann Clin Cytol Pathol. 2016;2(4):1033.
The World Organization for Animal Health. Leishmaniasis. http://www.oie.int/fileadmin/Home/eng/Health_standards/tahm/2.01.08_LEISHMANIOSIS.pdf. Accessed 22 Jan 18.
Paltrinieri S, Gradoni L, Roura X, Zatelli A, Zini E. Laboratory tests for diagnosing and monitoring canine leishmaniasis. Vet Clin Pathol. 2016;45:552–78.
St John A, Price CP. Existing and emerging technologies for point-of-care testing. Clin Biochem Rev. 2014;35:155–67.
IDEXX Laboratories. SNAP Leishmania Test.https://www.idexx.eu/en/products-and-solutions/SNAP-and-Pet-Side-Tests/snap-leishmania-test/. Accessed 23 Jan 2018.
InBios International, Inc. Kalazar Detect™ Rapid Test for Visceral Leishmaniasis.http://www.inbios.com/kalazar-detecttm-rapid-test-for-visceral-leishmaniasis-intl/ Accessed 23 Jan 2018.
Chembio Diagnostic Systems, Inc. Dual Path Platform.http://chembio.com/innovation/platforms/dual-path-platform/. Accessed 23 Jan 2018.
Virbac BVT. Speed Leish K. https://bvt.virbac.com/en/home/diagnostic-solutions/pour-le-veterinaire-praticien/vector-borne-and-parasitic-disea/main/produits/speed-leish-k.html. Accessed 23 Jan 2018.
Martins Cardoso R, Silva Lociks de Araújo NN, Sierra Romero GA, Castro Minuzzi Souza TT, Dietrich AG, Donizette Mendes J, et al. Expanding the knowledge about Leishmania species in wild mammals and dogs in the Brazilian savannah. Parasit Vectors. 2015;8:171. https://doi.org/10.1186/s13071-015-0780-y.
Gao C-H, Wang J-Y, Zhang S, Yang Y-T, Wang Y. Survey of wild and domestic mammals for infection with Leishmania infantum following an outbreak of desert zoonotic visceral leishmaniasis in Jiashi, People's Republic of China. PLoS One. 2015;10(7):e0132493. https://doi.org/10.1371/journal.pone.0132493.
Rosati S, Ortoffi M, Profiti M, Mannelli A, Mignone W, Bollo E, et al. Prokaryotic expression and antigenic characterization of three recombinant Leishmania antigens for serological diagnosis of canine leishmaniasis. Clin Diagn Lab Immunol. 2003;10:1153–6. https://doi.org/10.1128/CDLI.10.6.1153-1156.2003.
Boarino A, Scalone A, Gradoni L, Ferroglio E, Vitale F, Zanatta R, et al. Development of recombinant chimeric antigen expressing immunodominant B epitopes of Leishmania infantum for serodiagnosis of visceral leishmaniasis. Diag Lab Immunol. 2005;5:647–53.
Stobel K, Schonberg A, Staak C. A new non-species dependent ELISA for detection of antibodies to Borrelia burgdorferi s. I. in zoo animals. Int J Med Microbiol. 2002;291(33):88–99.
Al-Adhami BH, Gajadhar AA. A new multi-host species indirect ELISA using protein A/G conjugate for detection of anti-Toxoplasma gondii IgG antibodies with comparison to ELISA-IgG, agglutination assay and Western blot. Vet Parasitol. 2014;200:66–73. https://doi.org/10.1016/j.vetpar.2013.11.004.
Scalone DF, Mignone W, Ferroglio E, Mannelli A, Biglino A, Zanatta R, et al. Validation of a recombinant based antibody ELISA for diagnosis of human and canine leishmaniasis. J Immun Immunochem. 2008;29:244–56. https://doi.org/10.1080/15321810802116006.
Intaramat A, Sornprachum T, Chantrathonkul B, Chaisuriya P, Lohnoo T, Yingyong W, et al. Protein A/G-based immunochromatographic test for serodiagnosis of pythiosis in human and animal subjects from Asia and Americas. Med Mycol Open Access. 2016;54:641–7. https://doi.org/10.1093/mmy/myw018.
Omachi S, Matsumoto Y, Goto Y. Immunoglobulins in the pathophysiology of visceral leishmaniasis. In: Noiri E, Jha T, editors. Kala azar in South Asia. Cham: Springer; 2016.
Anfossi L, Calderara M, Baggiani C, Giovannoli C, Arletti E, Giraudi G. Development and application of a quantitative lateral flow immunoassay for fumonisins in maize. Anal Chim Acta. 2010;682:104–9. https://doi.org/10.1016/j.aca.2010.09.045.
Ferroglio E, Zanet S, Mignone W, Poggi M, Trisciuoglio A, Bianciardi P. Evaluation of a rapid device for serological diagnosis of Leishmania infantum infection in dog, compared to immunofluorescence assay and western blot. Clin Vaccine Immunol. 2013;20:657–9.
Lattanzio VMT, von Holst C, Visconti A. Experimental design for in-house validation of a screening immunoassay kit. The case of a multiplex dipstick for Fusarium mycotoxins in cereals. Anal Bioanal Chem. 2013;405:7773–82.
Lattanzio VMT, Guarducci N, Powers S, Ciasca B, Pascale M, von Holst C. Validation of a lateral flow immunoassay for the rapid determination of aflatoxins in maize by solvent free extraction. Anal Methods. 2018;10:123–30. https://doi.org/10.1039/C7AY02249B.
Di Nardo F, Anfossi L, Ozella L, Saccani A, Giovannoli C, Spano G, et al. Validation of a qualitative immunochromatographic test for the noninvasive assessment of stress in dogs. J Chromatog B. 2016;1028:192–8. https://doi.org/10.1016/j.jchromb.2016.06.019.
Kaplan LA, Pesce AJ. Clinical chemistry. Theory, analysis, correlation. 5th ed. Maryland Heights, MO: Mosby Elsevier Inc.; 2010.
Da Silva ES, Van der Meide WF, Schoone GJ, Gontijo CMF, Schallig HDFH, Brazil RP. Diagnosis of canine leishmaniasis in the endemic area of Belo Horizonte, Minas Gerais, Brazil by parasite, antibody and DNA detection assays. Vet Res Comm. 2006;30:637–43. https://doi.org/10.1007/s11259-006-3324-2.
Chun P. Colloidal gold and other labels for lateral flow immunoassays. In: Wong RC, Tse HY, editors. Lateral flow immunoassay. 1st ed. New York: Humana Press; 2009. p. 75–93.
Byzova NA, Safenkova IV, Slutskaya ES, Zherdev AV, Dzantiev BB. Less is more: a comparison of antibody-gold nanoparticle conjugates of different ratios. Bioconjug Chem. 2017;28:2737–46. https://doi.org/10.1021/acs.bioconjchem.7b00489.
Solano-Gallego L, Villanueva-Saz S, Carbonell M, Trotta M, Furlanello T, Natale A. Serological diagnosis of canine leishmaniosis: comparison of three commercial ELISA tests (Leiscan®, ID Screen® and Leishmania 96®), a rapid test (Speed Leish K®) and an in-house IFAT. Parasit Vectors. 2014;7:111. https://doi.org/10.1186/1756-3305-7-111.
Moreira OC, Yadon ZE, Cupolillo E. The applicability of real-time PCR in the diagnostic of cutaneous leishmaniasis and parasite quantification for clinical management: current status and perspectives. Acta Trop. 2017, in press; https://doi.org/10.1016/j.actatropica.2017.09.020.
Pomares C, Despierres L, Del Giudice P, Delaunay P, Michel G, Ferrua B, et al. Western blot analysis as an aid for the diagnosis of cutaneous leishmaniasis due to Leishmania major. Trans R Soc Trop Med Hyg. 2012;106:452–4. https://doi.org/10.1016/j.trstmh.2012.03.001.
Ferroglio E, Centaro E, Mignone W, Trisciuoglio A. Evaluation of an ELISA rapid device for the serological diagnosis of Leishmania infantum infection in dog as compared with immunofluorescence assay and western blot. Vet Parasitol. 2007;144:162–6.
Otranto D, Paradies P, Sasanelli M, Leone N, De Caprariis D, Chirico J, et al. Recombinant K39 dipstick immunochromatographic test: a new tool for the serodiagnosis of canine leishmaniasis. J Vet Diagn Investig. 2005;17:32–7.
Pennisi MG. Leishmaniosis of companion animals in Europe: an update vet. Parasitology. 2015;208:35–47.
Millán J, Ferroglio E, Solano-Gallego L. Role of wildlife in the epidemiology of Leishmania infantum infection in Europe. Parasitol Res. 2014;113:2005–14.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure of potential conflicts of interest
The author Chiara Nogarol works at the company In3Diagnostic (L.go P. Braccini 2, Grugliasco (TO), Italy), which may commercialise the LFIA device. However, this does not alter the authors’ adherence to the principles of good scientific practice and to relevant policies on sharing data and materials. The authors declare that they have no other competing interests.
Research involving animal participants
Blood samples were obtained during routine activities at the Veterinary Teaching Hospital of the Department of Veterinary Science or by veterinary practitioners. The study utilized samples from dogs at a private kennel/small-animal veterinary clinics, and informed consent was obtained from the owner of each dog. The consent was provided in oral form. No additional permission was required. All procedures were conducted in accordance with EU Directive 2010/63/EU for animal experiments, as well as with the informed consent of the owner of the animal.
Rights and permissions
About this article
Cite this article
Anfossi, L., Di Nardo, F., Profiti, M. et al. A versatile and sensitive lateral flow immunoassay for the rapid diagnosis of visceral leishmaniasis. Anal Bioanal Chem 410, 4123–4134 (2018). https://doi.org/10.1007/s00216-018-1067-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-018-1067-x