Abstract
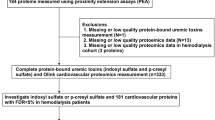
Cardiovascular disease (CVD) is prevalent in patients with chronic kidney disease (CKD). In hemodialysis (HD) patients, some protein-bound uremic toxins are considered to be associated with CVD. However, it is not yet known which uremic toxins are important in terms of endothelial toxicity. Serum samples were obtained from 45 HD patients before and after HD. Total and free serum concentrations of indoxyl sulfate, indoxyl glucuronide, indoleacetic acid, p-cresyl sulfate, p-cresyl glucuronide, phenyl sulfate, phenyl glucuronide, phenylacetic acid, phenylacetyl glutamine, hippuric acid, 4-ethylphenyl sulfate, and 3-carboxy-4-methyl-5-propyl-2-furanpropionic acid (CMPF) were simultaneously measured by liquid chromatography/electrospray ionization–mass spectrometry/mass spectrometry (LC/ESI-MS/MS). The effects of these solutes at their pre-HD mean and maximum serum concentrations on reactive oxygen species (ROS) production in human umbilical vein endothelial cells (HUVEC) were measured with a ROS probe. Serum levels of 11 of the solutes (all except 4-ethylphenyl sulfate) were significantly increased in HD patients compared to healthy subjects. All 12 solutes showed changes in their protein-binding ratios. In particular, indoxyl sulfate, p-cresyl sulfate, CMPF, and 4-ethylphenyl sulfate showed high protein-binding ratios (>95 %) and low reduction rates by HD (<35 %). Indoxyl sulfate at its mean and maximum pre-HD serum concentrations—even with 4 % albumin—stimulated ROS production in HUVEC most intensely, followed by CMPF. In conclusion, the serum levels of 11 protein-bound uremic toxins were increased in HD patients. Indoxyl sulfate, p-cresyl sulfate, and CMPF could not be removed efficiently by HD due to their high protein-binding ratios. Indoxyl sulfate most intensely induced endothelial ROS production, followed by CMPF.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Uremic toxins are involved in a variety of symptoms in patients with stage 5 chronic kidney disease (CKD). More than ninety compounds have been considered uremic toxins [1–4]. Uremic toxins include free water-soluble low-molecular-weight solutes, protein-bound solutes, and middle molecules [1]. Protein-bound uremic toxins have been identified as the main toxins involved in cardiovascular lesions of CKD patients. Notably, protein-bound uremic toxins such as indoxyl sulfate and p-cresyl sulfate have emerged as important targets of therapeutic removal.
In earlier investigations, we applied metabolomics analysis of comprehensive small-molecular metabolites with liquid chromatography/electrospray ionization–tandem mass spectrometry (LC/ESI-MS/MS) and principal component analysis to identify uremic toxins that had accumulated in the serum of CKD rats. Indoxyl sulfate was the first principal serum metabolite to be shown to differentiate CKD from normal, followed by phenyl sulfate, hippuric acid, and p-cresyl sulfate [5]. Further, we applied the metabolomic approach to search for uremic toxins as possible indicators of the effect of an oral sorbent, AST-120, which absorbs uremic toxins or their precursors in the intestines. Indoxyl sulfate was also the first principal serum metabolite to be shown to differentiate CKD from both normal and AST-120-administered CKD rats, followed by hippuric acid, phenyl sulfate, and 4-ethylphenyl sulfate [6].
Endothelial dysfunction is a critical precursor of cardiovascular disease (CVD), which is the most important cause of morbidity and mortality in CKD patients. CKD patients show impaired endothelium-dependent vasodilatation, elevated biomarkers of endothelial dysfunction, and increased oxidative stress, and also present an imbalance between circulating endothelial populations reflecting endothelial injury and repair [7, 8]. Thus, endothelial dysfunction is a hallmark of CKD. Several uremic toxins including indoxyl sulfate and p-cresyl sulfate exhibit endothelial toxicity. Recent studies have demonstrated that indoxyl sulfate stimulates reactive oxygen species (ROS) production in human umbilical vein endothelial cells (HUVEC) [9–11].
As a result of our earlier metabolomics analysis, we identified 12 metabolites, including indoxyl sulfate and p-cresyl sulfate, that present higher serum concentrations in CKD rats than in normal rats. However, indoxylacetyl glycine and phenylacetyl glycine could not be detected in human serum, although they were detected in rat serum. On the other hand, phenyacetyl glutamine and 3-carboxy-4-methyl-5-propyl-2-furanpropionic acid (CMPF) were included in the analysis because they were detected in human serum but not in rat serum.
This study aimed to determine the serum levels of these metabolites as well as their reduction rates and protein-binding ratios in hemodialysis (HD) patients with LC/ESI-MS/MS, and to compare their effects on ROS production in HUVEC.
Materials and methods
Reagents
Indoxyl sulfate potassium salt was purchased from Avocado (Alfa Aesar, Ward Hills, MA, USA), indoxyl-β-D-glucuronide cyclohexylammonium salt and p-tolyl-β-D-glucuronide (p-cresyl glucuronide) were from Sigma (St. Louis, MO, USA), phenyl-β-D-glucuronide hydrate was from Acros (Geel, Belgium), 3-indoleacetic acid potassium salt and hippuric acid were from Tokyo Chemical Industry (Tokyo, Japan), phenylacetic acid was from Wako Pure Chemical Industries, Ltd. (Osaka, Japan), phenylacetyl glutamine was from Bachem AG (Bubendorf, Switzerland), CMPF was from Cayman Chemical (Ann Arbor, MI, USA), indole-2,4,5,6,7-d5-3-acetic acid and N-benzoyl-d5-glycine (hippuric acid-d5) were purchased from C/D/N Isotopes Inc. (Pointe-Claire, QC, Canada), and phenyl-d5-acetic acid was purchased from Euriso-Top (Saint Aubin Cedex, France). p-Cresyl sulfate sodium salt and indoxyl-4,5,6,7-d4 sulfate potassium salt were synthesized by Eiweiss Chemical Co. (Shizuoka, Japan). Phenyl sulfate sodium salt and 4-ethylphenyl sulfate sodium salt were synthesized in Kureha (Tokyo, Japan). Methanol, acetonitrile, and distilled water of high–performance liquid chromatography (HPLC) grade were purchased from Kishida Chemical Industry (Osaka, Japan). Ammonium acetate of mass spectrometry grade was purchased from Fluka (Sigma, St. Louis, MO, USA). Human serum (pooled) was purchased from Cosmo Bio., Ltd. (Tokyo, Japan).
HUVEC and cell culture medium were purchased from DS Pharma Biomedical (Osaka, Japan). Hanks’ balanced salt solution (HBSS) (Ca+, Mg+) and 5-(and-6)-chloromethyl-2′,7′-dichlorodihydrofluorescein diacetate, acetyl ester (CM-H2DCFDA) as a ROS probe were obtained from Invitrogen (Carlsbad, CA, USA). Human serum albumin (HSA) was purchased from Sigma. All other chemicals used were of analytical grade.
Patients
Serum samples were obtained from 45 patients on hemodialysis (HD) [20 males and 25 females, age: 62.3 ± 0.7 (mean ± SE) years old ranging from 50 to 69, dialysis vintage: 6.11 ± 0.70 years, Kt/V: 1.40 ± 0.03, PCR: 0.97 ± 0.02 g/kg/day] from a single dialysis unit (Meiyo Clinic, Toyohashi, Aichi, Japan), and 8 healthy male subjects (age: 59.9 ± 1.1 years old, ranging from 57 to 65). The etiology of end-stage renal disease in the patients included chronic glomerulonephritis (n = 17), diabetes mellitus (n = 16), nephrosclerosis (n = 7), polycystic kidney disease (n = 2), bilateral nephrolithiasis followed by bilateral nephrectomy (n = 1), chronic glomerulonephritis after right renal cancer nephrectomy (n = 1), and left hypoplasia with right nephrosclerosis (n = 1). No specific criteria were used to obtain a representative population of HD patients. HD procedures (4 h) were performed three times per week. The serum samples from the HD patients were obtained just before and after HD. The samples were kept at −80 °C prior to analysis. Written informed consent was obtained from all subjects, and the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 1983. Subject enrollment was approved by the Ethics Committee of Nagoya University School of Medicine.
Microscale ultracentrifugation for measurement of protein-binding ratios
This experiment was conducted on the serum samples of 19 HD patients (pre-HD) and 5 healthy volunteers who showed triglyceride levels of <100 mg/dL, because it is difficult to separate layers in serum with a high triglyceride level using an ultracentrifugation method.
We used a microscale and rapid ultracentrifugation method with a table-top ultracentrifuge (Optima MAX Ultracentrifuge, Beckman Coulter, Inc., Brea, CA, USA) to measure the protein-binding ratios of 12 endogenous metabolites (indoxyl sulfate, indoxyl glucuronide, indoleacetic acid, p-cresyl sulfate, p-cresyl glucuronide, phenyl sulfate, phenyl glucuronide, phenylacetic acid, phenylacetyl glutamine, hippuric acid, 4-ethylphenyl sulfate, and CMPF) [12]. A 200 μL serum sample in a centrifuge tube (polycarbonate, 7 × 20 mm, Beckman Coulter, Inc., Brea, CA, USA) was ultracentrifuged at 100,000 rpm (436,000×g) for 140 min at 4 °C. After ultracentrifugation, the serum was separated into three layers according to the density of the substances in the serum. The tube was cut about 6 mm below the top to discard about 30 μL of the upper layer, which contained chylomicrons and very low-density lipoproteins. A 25 μL aliquot of the upper part of the middle layer, which did not contain serum protein (less than 1 % serum protein), was subjected to LC/ESI-MS/MS analysis for the free fraction of metabolites in serum.
Liquid chromatography/electrospray ionization–mass spectrometry/mass spectrometry (LC/ESI-MS/MS)
Quantitative analysis of 12 metabolites (indoxyl sulfate, indoxyl glucuronide, indoleacetic acid, p-cresyl sulfate, p-cresyl glucuronide, phenyl sulfate, phenyl glucuronide, phenylacetic acid, phenylacetyl glutamine, hippuric acid, 4-ethylphenyl sulfate, and CMPF) was performed by selected reaction monitoring (SRM) of LC/ESI-MS/MS [6]. Chemical structures for the uremic solutes are shown in Fig. 1.
Chemical structure of uremic solutes: A indoxyl sulfate, B indoxyl glucuronide, C indoleacetic acid, D p-cresyl sulfate, E p-cresyl glucuronide, F phenyl sulfate, G phenyl glucuronide, H phenylacetic acid, I phenylacetylglutamine, J hippuric acid, K 4-ethylphenyl sulfate, L 3-carboxy-4-methyl-5-propyl-2-furanpropionic acid (CMPF). GlcUA conjugate of glucuronic acid
HPLC analysis of a sample (10 μL) was performed using gradient elution with a LC-10Avp LC system (Shimadzu, Kyoto, Japan) on an Atlantis dC18 column (2.1 mm × 50 mm, 3 μm) (Waters, Milford, MA, USA) at 0.2 mL/min with the column maintained at 40 °C and an autosampler maintained at 10 °C. The gradient solution consisted of solvent A (5 mmol/L ammonium acetate solution) and solvent B (methanol). For the negative ion (NI) mode, the elution solution was 20 % B (A:B; 80:20, by volume) for 2 min followed by a linear gradient up to 60 % B for the next 2 min and up to 95 % for the next 3 min, before it was returned to 20 % B for 5 min. For the positive ion (PI) mode, the elution solution was 20 % B (A:B; 80:20, by volume) for 2 min, 95 % B for the next 5 min, and then 20 % B for 5 min.
The SRM method of LC/ESI-MS/MS was carried out using a triple quadrupole mass spectrometer (API4000, AB SCIEX, Carlsbad, CA, USA) equipped with an ESI source. Table 1 shows MS/MS parameters for the quantification of uremic solutes. MS/MS operating conditions were as follows; curtain gas: 10 psi for NI mode and 10 psi for PI mode; ion source gas 1: 60 psi for NI and 80 psi for PI; ion source gas 2: 80 psi for NI and 85 psi for PI; collision gas: 4 for NI and 5 for PI; ESI: -4 kV for NI and 5 kV for PI; ion source temperature: 700 °C for NI and 525 °C for PI; interface heater: on for NI and PI. Data acquisition and processing were carried out using the software package Analyst 1.5.1.
To measure the total serum concentration, a 20 μL serum sample obtained from each of 45 HD patients before and after HD and 8 healthy male volunteers was diluted with 40 μL of distilled water. A 50 μL aliquot of serum was added to acetonitrile (200 μL) containing internal standard (stable-isotope-labeled compounds; indoxyl-d4 sulfate 100 ng/mL; indole-d5-3-acetic acid, 200 ng/mL; phenyl-d5-acetic acid, 100 ng/mL; hippuric acid-d5, 100 ng/mL) in a Sirocco 96-well protein precipitation plate (Waters, Milford, MA, USA), and the mixture was thoroughly mixed. The solution was filtered by applying a vacuum to remove protein precipitation, and eluents (40 μL) were diluted with 5 mmol/L ammonium acetate solution (120 μL) before LC/ESI-MS/MS analysis. To calibrate the total serum concentration, a 40 μL aliquot of 12 endogenous metabolites of known concentrations in distilled water (nine concentrations of each metabolite were used for calibration) was spiked into a 20 μL aliquot of the commercial human serum, which was preprocessed in active carbon (2.5 g/50 mL serum) to remove internal metabolites. The subsequent steps were the same as described previously [5, 6]. Calibration curve ranges and correlation coefficients for the measurement of total serum concentration are shown in Table 2. The calibration curves showed almost linear correlation coefficients in the range between the minimum and maximum concentrations. Samples with concentrations beyond the maximum concentrations of the calibration curves were diluted with distilled water and then processed for LC/ESI-MS/MS analysis.
To measure free-form concentrations, the protein-free fraction (25 μL) was added to 25 μL of acetonitrile containing internal standards (stable-isotope-labeled compounds) in a test tube, and the mixture was thoroughly mixed. The solution was centrifuged at 20,600×g for 10 min at 4 °C, and upper layer was diluted with 5 mmol/L ammonium acetate solution (75 μL) before LC/ESI-MS/MS analysis. To calibrate the free-form concentrations, a 25 μL aliquot of 12 endogenous metabolites of known concentrations in distilled water (ten concentrations of each metabolite were used for calibration) was spiked into 25 μL of acetonitrile containing internal standards. Subsequent steps were the same as described previously. Calibration curve ranges and correlation coefficients for the measurement of free-form concentrations are shown in Table 2.
Calculation of the protein-binding ratio and reduction rate
The protein-binding ratio, B (%), was calculated according to the following equation:
where Cs and Cf are the total serum concentration and the free-form concentration as measured by LC/MS/MS, respectively. The results are expressed as the mean±SE.
The reduction rate, R (%), was calculated according to the following equation:
where Cpre and Cpost are the total serum concentrations before and after HD, respectively.
Cell culture and measurement of ROS in HUVEC
HUVEC (104 cells/well) were pre-incubated in 96-well plates for 24 h at 37 °C in culture medium. The HUVEC were then incubated with 10 μM CM-H2DCFDA for 30 min at 37 °C in HBSS (Ca+, Mg+). After incubation, the cells were washed with HBSS (Ca+, Mg+), and uremic solutes at their mean and maximum serum concentrations in CKD patients (Table 3) with or without 4 % HSA in HBSS were added to the cells and incubated overnight at 37 °C. The cells were processed with or without 4 % HSA because serum contains 4 % HSA and the uremic solutes are bound to HSA in serum.
The fluorescence intensity was measured at 494 nm excitation and 530 nm emission using a fluorescence microplate reader (Spectra Max Gemini XS, Molecular Devices, Sunnyvale, CA, USA). The mean fluorescence intensity ratio is presented after subtraction of the background fluorescence.
Statistical analysis
The results are expressed as the mean±SE. The Tukey–Kramer HSD test was performed for multiple comparisons in JMP 8.0.1 (SAS Institute, Cary, NC, USA). A value of p < 0.05 was considered to be statistically significant.
Results
Serum concentrations and reduction rates of uremic solutes in HD patients
Figure 2 shows representative SRM chromatograms for the quantification of 12 uremic solutes. Table 3 shows the serum concentrations of the uremic solutes in addition to BUN and creatinine in HD patients and healthy subjects. Serum levels of 11 solutes (all except 4-ethylphenyl sulfate) were significantly increased in HD patients compared to healthy subjects. Serum concentrations of indoxyl sulfate, p-cresyl sulfate, phenyl sulfate, phenylacetyl glutamine, hippuric acid, and CMPF were relatively high (more than 1 mg/dL). Indoxyl sulfate, p-cresyl sulfate, 4-ethylphenyl sulfate, and CMPF could not be efficiently removed by HD, as evidenced by their relatively low reduction rates (less than 35 %); indeed, CMPF actually increased in concentration after HD. Phenylacetyl glutamine, hippuric acid, indoxyl glucuronide, p-cresyl glucuronide, phenyl sulfate, and phenyl glucuronide were removed efficiently by HD because their reduction rates were more than 60 %, comparable to those of BUN and creatinine.
SRM chromatograms from LC/ESI-MS/MS for the quantification of uremic solutes. IS indoxyl sulfate, IG indoxyl glucuronide, IAA indoleacetic acid, PCS p-cresyl sulfate, PCG p-cresyl glucuronide, PhS phenyl sulfate, PhG phenyl glucuronide, PAA phenylacetic acid, PAGln phenylacetylglutamine, HA hippuric acid, EtPhS 4-ethylphenyl sulfate, CMPF 3-carboxy-4-methyl-5-propyl-2-furanpropionic acid
Protein-binding ratios of uremic solutes in HD patients
Table 4 shows the pre-HD serum concentrations of the total and free forms of the 12 uremic solutes in HD patients. A high-protein binding ratio was defined as >95 %, and a low reduction rate was defined as <35 %. Indoxyl sulfate, p-cresyl sulfate, 4-ethylphenyl sulfate, and CMPF showed high protein binding ratios (>95 %). Figure 3 shows the relationship between reduction rate and protein-binding ratio. CMPF, 4-ethylphenyl sulfate, indoxyl sulfate, and p-cresyl sulfate showed high protein-binding ratios (>95 %) and low reduction rates (<35 %).
Relationship between the protein-binding ratios of uremic solutes and their reduction rates by HD. IS indoxyl sulfate, IG indoxyl glucuronide, IAA indoleacetic acid, PCS p-cresyl sulfate, PCG p-cresyl glucuronide, PhS phenyl sulfate, PhG phenyl glucuronide, PAA phenylacetic acid, PAGln phenylacetylglutamine, HA hippuric acid, EtPhS 4-ethylphenyl sulfate, CMPF 3-carboxy-4-methyl-5-propyl-2-furanpropionic acid
Although phenylacetic acid presented a protein-binding ratio of 60.5 %, its reduction rate was low as 35.0 %. The serum levels of phenylacetic acid in 17 of the 45 HD patients were within normal levels. When the reduction rate of was calculated only for the HD patients (n = 28) who showed elevated serum levels of it, the reduction rate of phenylacetic acid was found to be 52.5 ± 9.3 %. Thus, phenylacetic acid can be removed relatively efficiently by HD in patients with elevated serum levels of phenylacetic acid.
Effects of uremic solutes on ROS production by HUVEC
Figure 4 shows ROS production by HUVEC in the presence (A, C) or absence (B, D) of 4 % HSA by uremic solutes at their mean (A, B) and maximum (C, D) pre-HD serum concentrations in HD patients. At their mean serum concentrations and in the absence of 4 % HSA (Fig. 4B), indoxyl sulfate showed the most intense ROS production in HUVEC, followed by indoxyl glucuronide. At their mean serum concentrations, and even in the presence of 4 % HSA (Fig. 4A), indoxyl sulfate induced ROS production in HUVEC most intensely, followed by CMPF. However, p-cresyl sulfate did not induce any ROS production in HUVEC.
ROS production by HUVEC in the presence (A, C) or absence (B, D) of 4 % human serum albumin (HSA) by uremic solutes at their mean (A, B) and maximum (C, D) serum concentrations in HD patients. Data are expressed as the mean ± SE (n = 3). *p < 0.05 vs control. A and B: IS indoxyl sulfate (2.99 mg/dL), IG indoxyl glucuronide (0.25 mg/dL), IAA indoleacetic acid (0.12 mg/dL), PCS p-cresyl sulfate (3.71 mg/dL), PCG p-cresyl glucuronide (0.58 mg/dL), PhS phenyl sulfate (1.35 mg/dL), PhG phenyl glucuronide (0.06 mg/dL), PAA phenylacetic acid (0.05 mg/dL), PAGln phenylacetylglutamine (4.15 mg/dL), HA hippuric acid (4.43 mg/dL), EtPhS 4-ethylphenyl sulfate (0.0242 mg/dL), CMPF 3-carboxy-4-methyl-5-propyl-2-furanpropionic acid (2.11 mg/dL). C and D: IS indoxyl sulfate (5.72 mg/dL), IG indoxyl glucuronide (0.92 mg/dL), IAA indoleacetic acid (0.32 mg/dL), PCS p-cresyl sulfate (10.91 mg/dL), PCG p-cresyl glucuronide (2.31 mg/dL), PhS phenyl sulfate (4.52 mg/dL), PhG phenyl glucuronide (0.23 mg/dL), PAA phenylacetic acid (0.26 mg/dL), PAGln phenylacetylglutamine (10.91 mg/dL), HA hippuric acid (14.48 mg/dL), EtPhS 4-ethylphenyl sulfate (0.156 mg/dL), CMPF 3-carboxy-4-methyl-5-propyl-2-furanpropionic acid (4.70 mg/dL)
At their maximum serum concentrations, and in the absence of 4 % HSA (Fig. 4D), indoxyl sulfate showed the most intense ROS production in HUVEC, followed by indoxyl glucuronide. At their maximum serum concentrations, and even in the presence of 4 % HSA (Fig. 4C), indoxyl sulfate induced ROS production in HUVEC most intensely, followed by CMPF.
Discussion
The present study describes a newly developed method involving the simultaneous LC/ESI-MS/MS measurement of 12 uremic solutes in HD patients, and is the first to demonstrate the protein binding of indoxyl glucuronide, p-cresyl glucuronide, phenyl sulfate, phenyl glucuronide, and 4-ethylphenyl sulfate in uremic serum. The other solutes investigated, such as indoxyl sulfate, indoleacetic acid, p-cresyl sulfate, phenylacetic acid, hippuric acid, and CMPF, have already been reported to be protein-bound [1, 4]. Furthermore, the present study is the first to demonstrate that CMPF and indoxyl glucuronide induce endothelial ROS production, although indoxyl sulfate is well known to induce endothelial ROS production [9, 10].
The present study revealed that serum levels of 11 solutes were significantly increased in HD patients. In particular, indoxyl sulfate, p-cresyl sulfate, and CMPF could not be removed efficiently by HD (reduction rates were <35 %) due to their high protein-binding ratios (>95 %). More notably, indoxyl sulfate at its mean serum concentration induced endothelial ROS production most intensely, even in the presence of 4 % HSA.
CMPF showed significant ROS production in HUVEC in the presence of 4 % HSA, although CMPF did not show any significant ROS production in the absence of HSA. This might be due to its poor solubility in water in the absence of HSA, and it might be soluble in the presence of HSA due to its strong albumin-binding property.
By measuring serum levels in HD patients with or without colon, Aronov et al. [13] demonstrated that indoxyl sulfate, indoxyl glucuronide, p-cresyl sulfate, and phenyacetyl glutamine were derived exclusively from colon. It was also suggested that p-cresyl glucuronide was derived from colon. However, hippuric acid, phenyl glucuronide, and indoleacetic acid were not significantly derived from colon. By comparing serum levels in germ-free and conventional mice, Wikoff et al. [14] found that indoxyl sulfate, p-cresyl sulfate, and phenyl sulfate were produced only in conventional mice, not in germ-free mice, demonstrating a critical role of intestinal bacteria in their production.
Indoxyl sulfate is derived from indole, which is produced in the intestine from tryptophan by intestinal bacteria. Indole is oxidized to indoxyl and subsequently sulfated to produce indoxyl sulfate in the liver. Indoxyl sulfate is a nephrovascular toxin involved in the progression of not only CKD [15–18] but also CVD [19, 20]. p-Cresyl sulfate is derived from p-cresol, which is produced in the intestine from tyrosine by intestinal bacteria. p-Cresol is sulfated to produce p-cresyl sulfate in the intestinal wall [21]. Indoxyl sulfate and p-cresyl sulfate share the same albumin-binding site, for which they are competitive binding inhibitors [22]. It was recently reported that indoxyl sulfate and p-cresyl sulfate may have a multicompartmental distribution, which may affect reduction ratios [23]. Phenyl sulfate is produced in the intestine from tyrosine. Although phenyl sulfate exhibits a high protein-binding ratio (90.7 %), it can be removed efficiently by HD (it has a relatively high reduction rate of 65.2 %). This might be due to its weak affinity for albumin. Hippuric acid is derived from polyphenols in plant foods and added to processed foods as a preservative. Phenylacetyl glutamine is produced by microbial decarboxylation of phenylalanine to phenylethylamine with subsequent conjugation.
Jankowski et al. [24] reported that phenylacetic acid was increased in HD patients, presenting a concentration of 3.49 mmol/L (47.5 mg/dL), and that it was below the detection limit in healthy subjects. Surprisingly, the serum concentration of phenylacetic acid in HD patients reported by them was 950 times higher than the corresponding value found in the present study (0.05 mg/dL). This discrepancy in the serum concentration of phenylacetic acid may be due to the use of different measuring methods in the two studies. Jankowski et al. used nuclear magnetic resonance (NMR) spectroscopy, which is not appropriate for measuring uremic solutes due to its low sensitivity. LC/ESI-MS/MS is sensitive and specific, and can quantify minor uremic solutes such as phenylacetic acid.
HD cannot efficiently remove highly protein-bound uremic toxins such as indoxyl sulfate, p-cresyl sulfate, and CMPF because of their high albumin-binding properties. Novel dialysis techniques should be developed to efficiently remove these protein-bound uremic toxins in order to prevent uremic complications such as CVD. Adding a sorbent to the dialysate removes indoxyl sulfate and p-cresyl sulfate more efficiently [25]. Alternatively, AST-120 reduces the serum levels of indoxyl sulfate and p-cresyl sulfate [6, 26].
References
Vanholder R, De Smet R, Glorieux G, Argilés A, Baurmeister U, Brunet P, Clark W, Cohen G, De Deyn PP, Deppisch R, Descamps-Latscha B, Henle T, Jörres A, Lemke HD, Massy ZA, Passlick-Deetjen J, Rodriguez M, Stegmayr B, Stenvinkel P, Tetta C, Wanner C, Zidek W, European Uremic Toxin Work Group (EUTox) (2003) Review on uremic toxins: classification, concentration, and interindividual variability. Kidney Int 63:1934–1943
Yavuz A, Tetta C, Ersoy FF, D'intini V, Ratanarat R, De Cal M, Bonello M, Bordoni V, Salvatori G, Andrikos E, Yakupoglu G, Levin NW, Ronco C (2005) Uremic toxins: a new focus on an old subject. Semin Dial 18:203–211
Niwa T (2011) Update of uremic toxin research by mass spectrometry. Mass Spectrom Rev 30:510–521
Jourde-Chiche N, Dou L, Cerini C, Dignat-George F, Vanholder R, Brunet P (2009) Protein-bound toxins—update 2009. Semin Dial 22:334–339
Kikuchi K, Itoh Y, Tateoka R, Ezawa A, Murakami K, Niwa T (2010) Metabolomic analysis of uremic toxins by liquid chromatography/electrospray ionization-tandem mass spectrometry. J Chromatogr B 878:1662–1668
Kikuchi K, Itoh Y, Tateoka R, Ezawa A, Murakami K, Niwa T (2010) Metabolomic search for uremic toxins as indicators of the effect of an oral sorbent AST-120 by liquid chromatography/tandem mass spectrometry. J Chromatogr B 878:2997–3002
Jourde-Chiche N, Dou L, Cerini C, Dignat-George F, Brunet P (2011) Vascular incompetence in dialysis patients—protein-bound uremic toxins and endothelial dysfunction. Semin Dial 24:327–337
Annuk M, Zilmer M, Lind L, Linde T, Fellström B (2001) Oxidative stress and endothelial function in chronic renal failure. J Am Soc Nephrol 12:2747–2752
Dou L, Jourde-Chiche N, Faure V, Cerini C, Berland Y, Dignat-George F, Brunet P (2007) The uremic solute indoxyl sulphate induces oxidative stress in endothelial cells. J Thromb Haemost 5:1302–1308
Tumur Z, Niwa T (2009) Indoxyl sulfate inhibits nitric oxide production and cell viability by inducing oxidative stress in vascular endothelial cells. Am J Nephrol 29:551–557
Tumur Z, Shimizu H, Enomoto A, Miyazaki H, Niwa T (2010) Indoxyl sulfate upregulates expression of ICAM-1 and MCP-1 by oxidative stress-induced NF-kB activation. Am J Nephrol 31:435–441
Nakai D, Kumamoto K, Sakikawa C, Kosaka T, Tokui T (2004) Evaluation of the protein binding ratio of drugs by a micro-scale ultracentrifugation method. J Pharm Sci 93:847–854
Aronov PA, Luo FJ, Plummer NS, Quan Z, Holmes S, Hostetter TH, Meyer TW (2011) Colonic contribution to uremic solutes. J Am Soc Nephrol 22:1769–1776
Wikoff WR, Anfora AT, Liu J, Schultz PG, Lesley SA, Peters EC, Siuzdak G (2009) Metabolomics analysis reveals large effects of gut microflora on mammalian blood metabolites. Proc Natl Acad Sci USA 106:3698–3703
Niwa T, Ise M (1994) Indoxyl sulfate, a circulating uremic toxin, stimulates the progression of glomerular sclerosis. J Lab Clin Med 124:96–104
Niwa T, Ise M, Miyazaki T (1994) Progression of glomerular sclerosis in experimental uremic rats by administration of indole, a precursor of indoxyl sulfate. Am J Nephrol 14:207–212
Miyazaki T, Ise M, Seo H, Niwa T (1997) Indoxyl sulfate increases the gene expressions of TGF-β1, TIMP-1 and pro-α1(I) collagen in uremic rat kidneys. Kidney Int 52(S62):S15–S22
Enomoto A, Takeda M, Tojo A, Sekine T, Cha SH, Khamdang S, Takayama F, Aoyama I, Nakamura S, Endou H, Niwa T (2002) Role of organic anion transporters in the tubular transport of indoxyl sulfate and the induction of its nephrotoxicity. J Am Soc Nephrol 13:1711–1720
Adijiang A, Goto S, Uramoto S, Nishijima F, Niwa T (2008) Indoxyl sulphate promotes aortic calcification with expression of osteoblast-specific proteins in hypertensive rats. Nephrol Dial Transplant 23:1892–1901
Niwa T (2010) Indoxyl sulfate is a nephro-vascular toxin. J Ren Nutr 20(Suppl 1):S2–S6
Schepers E, Glorieux G, Vanholder R (2010) The gut: the forgotten organ in uremia? Blood Purif 29:130–136
Meijers BK, De Loor H, Bammens B, Verbeke K, Vanrenterghem Y, Evenepoel P (2009) p-Cresyl sulfate and indoxyl sulfate in hemodialysis patients. Clin J Am Soc Nephrol 4:1932–1938
Meijers B, Toussaint ND, Meyer T, Bammens B, Verbeke K, Vanrenterghem Y, Kerr PG, Evenepoel P (2011) Reduction in protein-bound solutes unacceptable as marker of dialysis efficacy during alternate-night nocturnal hemodialysis. Am J Nephrol 34:226–232
Jankowski J, van der Giet M, Jankowski V, Schmidt S, Hemeier M, Mahn B, Giebing G, Tolle M, Luftmann H, Schluter H, Zidek W, Tepel M (2003) Increased plasma phenylacetic acid in patients with end-stage renal failure inhibits iNOS expression. J Clin Invest 112:256–264
Meyer TW, Peattie JW, Miller JD, Dinh DC, Recht NS, Walther JL, Hostetter TH (2007) Increasing the clearance of protein-bound solutes by addition of a sorbent to the dialysate. J Am Soc Nephrol 18:868–874
Niwa T, Nomura T, Sugiyama S, Miyazaki T, Tsukushi S, Tsutsui S (1997) The protein metabolite hypothesis, a model for the progression of renal failure: an oral sorbent lowers indoxyl sulfate levels in undialyzed uremic patients. Kidney Int 52(Suppl 62):S23–S28
Conflict of interest
Y.I., A.E., and K.K. are employed by Kureha Corporation. The other authors declare no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Published in the special paper collection Biomedical Mass Spectrometry with guest editors Toyofumi Nakanishi and Mitsutoshi Setou.
Rights and permissions
About this article
Cite this article
Itoh, Y., Ezawa, A., Kikuchi, K. et al. Protein-bound uremic toxins in hemodialysis patients measured by liquid chromatography/tandem mass spectrometry and their effects on endothelial ROS production. Anal Bioanal Chem 403, 1841–1850 (2012). https://doi.org/10.1007/s00216-012-5929-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-012-5929-3