Abstract
New biomarkers of cardiovascular disease are needed to augment the information obtained from traditional indicators and to illuminate disease mechanisms. One of the approaches used in metabolomics/metabonomics for that purpose is metabolic fingerprinting aiming to profile large numbers of chemically diverse metabolites in an essentially nonselective way. In this study, gas chromatography-mass spectrometry was employed to evaluate the major metabolic changes in low molecular weight plasma metabolites of patients with acute coronary syndrome (n = 9) and with stable atherosclerosis (n = 10) vs healthy subjects without significant differences in age and sex (n = 10). Reproducible differences between cases and controls were obtained with pattern recognition techniques, and metabolites accounting for higher weight in the classification have been identified through their mass spectra. On this basis, it seems inherently plausible that even a simple metabolite profile might be able to offer improved clinical diagnosis and prognosis, but in addition, specific markers are being identified.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite considerable advances in the treatment of atherothrombosis, it remains the leading cause of death in developed countries. The assessment of classic cardiovascular risk factors—including high blood pressure, dyslipidemia, diabetes, and smoking—has a central role in disease prevention. However, the presence of these risk factors is not enough to predict accurately what persons are at risk of suffering an acute ischemic event, which is caused by the occlusion of an artery due to the formation of a thrombus on the atherosclerotic plaques. Identifying individuals at risk of developing these events is critical in order to direct available therapeutic resources efficiently. Thus, complementary approaches are needed to improve our ability to predict the appearance of these events. The possibility that abnormal plasma levels of one or more molecules may predict the appearance of new vascular events has gained acceptance in the last years. However, no biomarker has shown consistent results to be used in the clinical practice [1, 2].
Application of large-scale technologies to the study of cardiovascular diseases has resulted in outstanding advances in the last years. These include improvements in our understanding of molecular mechanisms of pathophysiological processes, identification of diagnostic/prognostic biomarkers for cardiovascular disease, and identification of novel therapeutic targets [3]. In this respect, metabolite fingerprinting is an example of a new type of diagnostic test that shows considerable promise. Metabolites are the small molecular products of enzyme-catalyzed reactions. Metabolite levels are determined by protein activities, so a comprehensive understanding of biological systems is not possible without measuring and modeling these small molecules and integrating the information with data from other large-scale molecular analyses. Nuclear magnetic resonance spectroscopy or chromatographic separations can be used to generate a “molecular fingerprint” of a serum sample, and cutting-edge pattern recognition techniques can then be applied to identify molecular signatures associated with the presence of occlusive atherosclerotic lesions [4]. The aim is the collection of profiles (containing as many metabolites as possible) and search within those profiles for signatures that predict future cardiovascular events with high sensitivity and specificity through mathematical modeling tools. Afterward, target biomarkers would be identified with the use of standardized technology platforms, followed by validation of the assays, statistical evaluation of biomarker distributions in reference samples and in those with disease, and assessment of the correlation between biomarker levels (or expression patterns of biomarkers) and clinical measurements that define disease status [5].
Recent studies have reported the use of multivariate analysis of 1H NMR spectroscopy of serum and plasma samples to predict the presence and severity of angiographically defined coronary artery disease and of hypertension [6, 7]. Nevertheless, different authors argued that the analysis depended mainly on the major lipid regions of the spectra, but many variables, including gender and drug treatment, affect lipid composition and are potential confounders [8]. Recently, an application of metabolomics to acute myocardial ischemia has been reported, in which novel biomarkers have been identified. Plasma samples were fractionated by liquid chromatography, and profiling of analytes was performed with a high-sensitivity electrospray triple–quadrupole mass spectrometer under selected reaction monitoring conditions. Changes in six metabolites, including citric acid, differentiated cases from controls with a high degree of accuracy (P < 0.0001; cross-validated c statistic = 0.83) [9].
Gas chromatography-mass spectrometry (GC-MS) has been one of the techniques commonly used for metabolomic analysis due to technical advantages, including separation capability, larger spectrum libraries, robustness, and sensitivity. Our final aim will be the employment of as many analytical platforms as possible in order to gather the broadest possible information, and GC-MS has been the technique of choice to get the fingerprint of low molecular weight metabolites in plasma. GC-MS metabolomics, however, requires derivatization of the original sample, with the corresponding decrease in sample throughput. Therefore, its use is not intended for routine clinical work, but to find the markers for which later will be developed a specific and simple analysis.
Perhaps the greatest strength of these metabolic profiling methods, however, comes from their ability to identify previously unknown correlations between unexpected metabolic partners, either in disease or in response to chemical perturbation.
In a previous study, Moritz et al. [10] developed and optimized an extraction and derivatization protocol for analyzing human blood plasma metaboloma by GC/MS. The method was validated for 32 compounds out of 500 resolved peaks in the profile.
The aim of our work was to generate the GC-MS fingerprint of low molecular weight metabolites in the plasma of patients with a non-ST-elevation acute coronary syndrome (NSTEACS). Afterward, without identifying any specific metabolites in the profile, but merely reproducible differences between cases and controls, pattern recognition techniques have been successfully applied. Finally, metabolites accounting for higher weight in the classification have been identified through their mass spectra as well as those that significantly correlate with them.
Materials and methods
Chemicals
The reference compounds were purchased from Sigma (St. Louis, MO, USA) and Aldrich (Steinhein, Germany). The compounds and reagents were all of analytical grade except where stated otherwise. N,O-Bis(trimethylsilyl)trifluoroacetamide (BSTFA) plus 1% trimethylchlorosilane (TMCS) were purchased from Pierce Chemical Co (Rockford, IL, USA). O-Methoxyamine hydrochloride, pyridine (silylation grade), and heptane (analytical grade) were obtained from Sigma. Methanol, acetone, and acetonitrile (HPLC grade) were from Supelco (Bellefonte, PA, USA). Ultrapure water was produced by a Milli-Q Reagent Water System (Millipore, MA, USA).
Stock solutions of the reference compounds were prepared either in Milli-Q water or in methanol at the same concentration 25 mM. These solutions were kept at −80 °C. Before the analysis, the solutions were thawed and diluted (1/100) with methanol.
Samples
Plasma of patients with NSTEACS (n = 9), withdrawn the fourth day of hospital stay, patients with stable carotid atherosclerosis (n = 10), and healthy subjects (n = 10) without significant differences in age and sex have been studied. All subjects were in fasting state, and the extraction was performed in the morning (between 8 a.m. and 11 a.m.).
All NSTEACS and carotid atherosclerosis patients were under low-cholesterol diet. In 33% of NSTEACS patients, the diet was also low salt containing; in 44%, low salt and low carbohydrate; and in 11%, low carbohydrate diet. Sixty percent of patients with carotid atherosclerosis received a diet that was also low salt containing, 20% a low carbohydrate and low salt diet, and 10% a low carbohydrate diet. Healthy subjects did not have dietary restrictions. All patients with NSTEACS were under enoxaparin, aspirin, and statins; 89% received clopidogrel and nitroglycerin, 78% omeprazol and angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, 67% beta blockers, 44% lorazepam, 33% oral antidiabetic drugs, 22% furosemide, and 11% tirofiban, insulin, alprazolam, sucralfate, alopurinol, and trimetazidine. Sixty percent of patients with carotid atherosclerosis received statins, aspirin, and angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, 20% oral antidiabetic drugs and clopidogrel, and 10% insulin.
In addition, for quality control, a pool was prepared of samples from healthy people, and all the plasma samples were stored in aliquots at −80 °C.
Fresh EDTA anticoagulated blood was centrifuged at 1,000×g (Heraeus Instruments, Landgeselbold) for 10 min at 4 °C. Plasma was thawed, vortex-mixed, and filtered through a 0.22-μm filter (Millipore) before use.
Sample treatment
Plasma (50 μL) or standard was vortex-mixed with 50 μL of acetonitrile, let stand for 5 min, and centrifuged at 15,400×g (Hettich, Tuttlingen) for 10 min at 4 °C. Upper-phase (50 μL) was transferred to a GC vial and evaporated to dryness in a Speedvac Concentrator (Thermo Fisher Scientific, Waltham, MA, USA). Ten microliters of O-methoxyamine hydrochloride (15 mg/mL) in pyridine was added to each GC vial, and the resultant mixture was vigorously vortex-mixed for 5 min. Methoxymation was carried out at room temperature for 16 h. The solution was then vortex-mixed again for 5 min after adding 10 μL of BSTFA with 1% TMCS as catalyst. After silylation for 1 h at 70 °C in an oven, 100 μL of heptane with 10 ppm of C16:0 methyl ester (IS) was added to each GC vial and vortex-mixed for 2 min before GC analysis.
GC-MS method
Derivatized samples (1 μL) were analyzed by GC-MS with a Varian instrument 3900 Series GC. Helium was used as carrier gas at a constant flow rate of 1 mL min−1 through the column. The injector temperature was 250 °C and split ratio 1:10.
The initial oven temperature of the column (Factor four capillary column, VF-5 ms 30 m × 0.25 mm ID DF = 0.25, VARIAN, USA) was 50 °C; 1 min after injection, the temperature was raised at the rate of 3.3 °C/min to reach a final temperature of 340 °C.
Detection conditions: mass spectrometer detector Saturn 2110 T with ionic trap. The transfer line temperature was set at 280 °C and the trap temperature at 200 °C, and the manifold temperature was set at 60 °C. Ions were generated by a 70 eV. The mass spectrometer was operated in full-scan mode only (scanning from m/z 50 to m/z 650) at a rate of five spectra per second.
Quality control
The analytical method is based on two methods previously described and validated [10, 11], optimized for the low volume of sample available. For that reason and because the aim is not quantification, only repeatability was tested with six real samples from a pool submitted individually to the whole method described above. RSDs of the areas in different compounds identified along the chromatogram were studied.
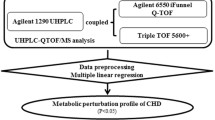
Data alignment and treatment
Multialignment of the electropherograms was performed with an in-house program developed in Matlab® 7.0, using the correlation optimized warping (COW) method previously described [12]. Subsequently, data were analyzed with SIMCA P+ 11.5 (Umetrics, Sweden). Another in-house program developed in Matlab makes a complete study of correlations among the selected variable and all the others by using Pearson correlation coefficient. It also calculates the statistical significance of the correlations [13].
Results and discussion
The median (interquartile range) age was 79 (58–84) years in NSTEACS patients, 67 (58–74) in stable atherosclerosis, and 64 (63–64) in healthy subjects (p = 0.073). The proportion of male/females was 66.6/33.4%, 70/30%, and 70/30%, respectively (p = 0.984).
GC-MS was selected as the first approach in this study because, although the drawbacks related with exhaustive sample treatment are well known, the efficiency in the separation of very small molecules and the ability to identify them through libraries are important values.
As in previous works [14, 15], the whole signal in the profile in total ion mode was employed to compare the fingerprints that avoids deciding the threshold for peak detection, which is always cumbersome, and permitted us to use the existing software for data pre-treatment. The first treatment applied to each profile was baseline correction that could not be as necessary for GC data as it is for other techniques such as capillary electrophoresis. However, it is part of the routine developed in Matlab and always poses an improvement in the raw signal. The treatment consisted of dividing the electropherogram in p regions (p is a value to be optimized). Then, the minimum value in each region is calculated, and all the minimums are interpolated by means of a polynomial function to obtain the baseline. The second step was the multialignment of the profiles. Again, shifts in GC profiles are quite smaller than in other separation techniques, and probably the alignment would not be very important for sample classification as it affects randomly to all the samples and only in a small number of peaks, but it improves marker identification, which was the final aim of the study. We have been working with the COW algorithm with very good results, and again, after data alignment, the situation was perfect to apply pattern recognition tools. Previously, samples were normalized with the internal standard to avoid solvent evaporation effects and autoscaled.
Principal component analysis was firstly used as multivariate nontarget analysis of the patterns to reduce the dimensionality of a multidimensional dataset while retaining the characteristics of the dataset that contributes most to its variance. In humans, a great number of sources of variation exist, and therefore, a target multivariate analysis was necessary.
After applying partial least square discriminant analysis (PLS-DA), samples were perfectly classified both controls vs NSTEACS patients (Fig. 1) and controls vs patients with stable atherosclerosis (Fig. 2). The classification error was 0% in both groups, while after making the cross-validation by leaving one out applied to all the individuals, it was 10% in control vs NSTEACS and 22% in controls vs stable atherosclerosis, which is quite sensible considering the type of samples. In both cases, variability explained in Y (classes) was over 90%. When testing the three groups together (Fig. 3), classification error was 5.3% in NSTEACS and 0% in controls and stable atherosclerosis.
Looking for disease markers, the loading plot in the assays by pairs was used because the classification was better. The loading plot informs about variables responsible for sample grouping by giving the number of the variable. Taking the number of the variable to the profile, peaks were identified. As identification of metabolites responsible for differences in the profiles was one of the aims in the study, a set of 85 individual standards was previously analyzed. Figure 4a and b shows the chromatographic profile, and all the metabolites were identified by retention time and fragmentation pattern as compared with the corresponding standard and with the MS (NIST) library.
a and b Chromatographic profile of the derivatized plasma. a From 0 to 43 min. Peaks: 1 lactate I, 2 lactate II, 3 oxalacetate, 4 valine, 5 alanine I, 6 unknown, 7 glycine I, 8 2-hydroxybutyric, 9 oxalate I, 10 oxalate II, 11 3-hydroxypropionate, 12 unknown, 13 unknown, 14 3-hydroxybutyrate, 15 siloxane, 16 2-Aminobutyrate, 17 unknown, 18 valine II, 19 urea, 20 leucine, 21 isoleucine, 22 threonine I + proline, 23 glycine II, 24 succinate, 25 glycerate, 26 serine, 27 nonanoate (not injected), 28 threonine II, 29 unknown, 30 aminomalonate (not injected), 31 malate, 32 unknown, 33 2,3,4-trihydroxybutanal aldehyde (not injected), 34 methyonine + piroglutamate + glutamine, 35 4-hydroxyproline, 36 aspartate, 37 2,3,4-trihydroxybutyrate (not injected), 38 phenylalanine I, 39 creatinine, 40, 41, 42 unknown, 43 glutamate + phenylalanine II, 44 and 45 unknown, 46 laurate, 47 asparagine, 48 and 49 unknown, 50 xylitol (not injected), 51 ornitine, 52 dehydrated citric (not injected), 53 galactopyranose (not injected), 54 9-H-purine (not injected), 55 citric, 56 galactofuranose (not injected), 57 deoxyglucose (not injected). b From 40 to 75 min. Peaks: 53 galactopyranose (not injected), 54 9-H-purine (not injected), 55 citric, 56 galactofuranose (not injected), 57 deoxyglucose (not injected), 58 myristic, 59 fructose, 60 gluconate, 61 and 62 glucose, 63 glucitol, 64 unknown, 65 tyrosine, 66 unknown, 67 and 68 disaccharide glucose derivate (not injected), 69 unknown, 70 inositol (not injected), 71 glucose, 72 palmitate, 73 myo-inositol, 74 urate, 75 methyl estearate (IS), 76 unknown, 77 tryptophan + 5-hydroxy-3-indolacetate, 78 linoleate, 79 oleate, 80 estearate, 81 EDTA, 82 phthalate, 83–86 unknown, 87 cholesterol
In order to assure repeatability of the results, six quality control plasma samples were analyzed, and RSDs of the areas of different peaks along the profile were calculated and are shown in Table 1. Values ranged from 4.5% to 19.6% and can be considered adequate for this type of analysis.
From the loading plot, citric acid, 4-hydroxyproline, aspartic acid, and fructose were decreased and lactate, urea, glucose, and valine were increased in NSTEACS patients vs healthy people.
Citric acid was previously described as decreased in acute myocardial ischemia [16] as expected, as it is related to aerobic metabolism. Aspartic acid is quite unspecific. Nevertheless, increased expression of cysteine and aspartic proteases were found during progression of atherosclerosis in apolipoprotein E-deficient mice, suggesting that these proteases may participate in the remodeling of extracellular matrix associated with the atherosclerotic process [17]. Fructose could have different origins, including the diet. Therefore, we were especially interested in 4-hydroxyproline.
Hydroxyproline is a highly specific component of collagen. It is also found in minor proportion in other proteins, such as elastin, the C1q component of the complement system and acetylcholinesterase [18]. Trieu et al. [19] reported that lipoprotein(a) binds to l-proline and hydroxyproline [20]. Circulating hydroxyproline could prevent the binding of LDL to lipoprotein(a) already deposited in the vascular wall and, by the same mechanism, release already deposited LDL from the atherosclerotic lesions. Elderly Okinawans, with high levels of hydroxyproline, have coronary arteries virtually free of atherosclerotic plaques [21]. Moreover, collagen confers stability to the atherosclerotic plaque, avoiding its rupture as a consequence of the hemodynamic forces [22]. Macrophages have been shown to degrade collagen into hydroxyproline [23]. This favors the rupture of the fibrous cap of the atherosclerotic plaques, allowing the blood to contact with the lipid core, which is highly thrombogenic [24], triggering thrombosis. The decrease in plasma hydroxyproline levels in our patients may reflect a status of low collagen synthesis and turnover in NSTEACS, although these findings deserve further study.
Conclusion
In a preliminary assay, GC-MS has been applied to plasma samples for disease diagnosis (without identifying any specific metabolites in the profile, but merely reproducible differences between cases and controls) with pattern recognition techniques. Samples coming from patients with acute coronary syndrome, as compared to healthy subjects and patients with stable atherosclerosis, have been successfully classified. Furthermore, identification of variables accounting for the classification through spectral libraries and the corresponding standards has led us to a list of markers. Among them, 4-hydroxyproline appears as an interesting compound for further studies.
References
Wang TJ, Gona P, Larson MG, Tofler GH, Levy D, Newton-Cheh C, Jacques PF, Rifai N, Selhub J, Robins SJ, Benjamin EJ, D’Agostino RB, Vasan RS (2006) N Engl J Med 355:2631–2639
Gerszten RE, Wang TJ (2008) Nature 451:949–952
Arab S, Gramolini AO, Ping P, Kislinger T, Stanley B, van Eyk J, Ouzounian M, MacLennan DH, Emili A, Liu PP (2006) J Am Coll Cardiol 48:1733–1741
Grainger DJ (2006) Heart Metab 32:22–25
Vasan RS (2006) Circulation 113:2335–2362
Brindle JT, Nicholson JK, Schofield PM, Grainger DJ, Holmes E (2003) Analyst 128:32–36
Brindle JT, Antti H, Holmes E, Tranter G, Nicholson JK, Bethell HW, Clarke S, Schofield PM, McKilligin E, Mosedale DE, Grainger DJ (2002) Nat Med 8(12):1439–1444
Kirschenlohr HL, Griffin JL, Clarke SC, Rhydwen R, Grace AA, Schofield PM, Brindle KM, Metcalfe JC (2006) Nat Med 12(6):705–710
Sabatine MS, Liu E, Morrow DA, Heller E, McCarroll R, Wiegand R, Berriz GF, Roth FP, Gerszten RE (2005) Circulation 112:3868–3875
Jiye A, Trygg J, Gullberg J, Johansson AI, Jonsson P, Antti H, Marklund SL, Moritz T (2005) Anal Chem 77:8086–8094
Daykin CA, Foxall PJD, Connor SC, Lindon JC, Nicholson JK (2002) Anal Biochem 304(2):220–230
Nielsen NP, Carstensen JM, Smedsgaard J (1998) J Chromatogr A 805:17–35
Angulo S, García-Pérez I, Legido-Quigley C, Barbas C (2008) Electrophoresis (in press)
Barbas C, Vallejo M, Garcia A, Barlow D, Hanna-Brown A (2008) J Pharm Biomed Anal 47:388–398
Vallejo M, Angulo S, Garcia-Martinez D, Garcia A, Barbas C (2008) J Chromatogr A 1187:267–274
Sabatine MS, Liu E, Morrow DA, Heller E, McCarroll R, Wiegand R, Berriz GF, Roth FP, Gerszten RE (2005) Circulation 112:3868–3875
Jormsjo S, Wuttge DM, Sirsjo A, Whatling C, Hamsten A, Stemme S, Eriksson P (2002) AM J Pathol 161:939–945
Berg RA (1982) Methods Enzymol 82:372–378
Trieu VN, Zioncheck TF, Lawn RM, McConathy WJ (1991) J Biol Chem 266:5480–5485
Rath M (1992) J Orthomol Med 7:153–162
Bernstein AM, Willcox BJ, Tamaki H, Kunishima N, Suzuki M, Willcox DC, Yoo JS, Perls TT (2004) J Gerontol (A Biol Sci Med Sci) 59:1195–1199
Davies MJ (1996) Circulation 94(8):2013–2020
Shah PK, Falk E, Badimon JJ, Fernandez-Ortiz A, Mailhac A, Villareal-Levy G, Fallon JT, Regnstrom J, Fuster V (1995) Circulation 92(6):1565–1569
Toschi V, Gallo R, Lettino M, Fallon JT, Gertz SD, Fernández-Ortiz A, Chesebro JH, Badimon L, Nemerson Y, Fuster V, Badimon JJ (1997) Circulation 95(3):594–599
Acknowledgments
This work has been supported by the Comunidad Autónoma de Madrid (S2006/GEN-0247), Spanish Ministery of Sciences and Technology CTQ2008-03779, Fundación Ramón Areces, FIS (PI050451), and Sociedad Española de Arteriosclerosis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vallejo, M., García, A., Tuñón, J. et al. Plasma fingerprinting with GC-MS in acute coronary syndrome. Anal Bioanal Chem 394, 1517–1524 (2009). https://doi.org/10.1007/s00216-009-2610-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-009-2610-6