Abstract
Sedative agents are used to facilitate sexual assault due to their ability to render the victim passive, submissive and unable to resist. The primary pharmacological effect of the benzodiazepine tetrazepam is muscle relaxation, whereas the benzodiazepine diazepam acts on the central nervous system (CNS) exerting mainly sedation effects. Therefore, contrary to tetrazepam, diazepam is an often-abused drug, which can potentially be used as a date-rape drug. In this study, we describe the detection of low amounts of diazepam in Myolastan® (Sanofi–Synthelabo S.A., Brussels, Belgium) and Epsipam® (Will-Pharma, Wavre, Belgium) 50mg tablet preparations by LC-MS-MS, GC-FID and HPLC-DAD. Considering the important forensic implication of this finding, a study was conducted with volunteers receiving a single or repeated dosage of Myolastan®. Urine, hair and preserved oral fluid samples were analysed using a previously described sensitive and specific LC-MS-MS detection method allowing for the simultaneous quantification of tetrazepam, diazepam, nordiazepam, oxazepam and temazepam. This study demonstrates that diazepam can be observed in urine samples even after a single dose of Myolastan®. In addition, maintaining therapy for 1 week results in the detection of both diazepam and nordiazepam in urine samples and of diazepam in the first hair segment. Importantly, comparing urine and hair samples after a single intake of diazepam versus the single and 1 week administration of Myolastan® shows that the possible metabolic conversion of tetrazepam to diazepam is a more plausible explanation for the detection of diazepam in biological samples after the intake of Myolastan®. As such, these results reveal that the presence of diazepam and/or nordiazepam in biological samples from alleged drug-facilitated assault cases should be interpreted with care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
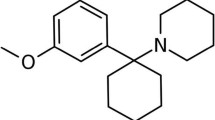
In the past few years, an increase in the number of scientific publications on so-called date-rape drugs, drug-facilitated sexual assault (DFSA) and drug-facilitated crimes (DFC) has been observed [1–8]. The most renowned drug associated with sexual assault is Rohypnol® (flunitrazepam) [9]. However, many other drugs have been implicated in these crimes, including other benzodiazepines, GHB (γ-hydroxybutyric acid) and ketamine. These drugs are all characterized by having depressant effects on their users, resulting in confusion, drowsiness, impaired memory and reduced inhibition. In addition, they induce amnesia, presumably the principal reason for their selection as date-rape drugs. During a 3-year surveillance in the UK, the toxicology results from 1,014 cases of claimed DFSA showed a relatively high number of cases which contained benzodiazepines (9%), with diazepam being the most prevalent benzodiazepine [10].
However, several difficulties in the diagnosis of DFC are apparent. These crimes are often difficult to prove due to factors such as the low concentrations of drugs used or their rapid clearance from the body. In addition, many victims of DFC do not report an incident until several days later, often due to the amnesia caused by the drug. Hence, conventional specimens from alleged victims such as blood or urine may have limited value. Recently, hair samples have been successfully used to document cases of DFC [4, 8, 11–14]. Kintz and co-workers concluded that due to the extremely low concentrations of drugs typically encountered in hair analysis (in the lower ranges of picograms per milligram) the “sensitivity of LC-MS-MS appears to be a pre-requisite to document any case involving drug-facilitated sexual assault” [4]. However, they also added the caveat that hair analysis should not simply be considered as an alternative to blood and urine testing but as a complementary technique where possible.
Furthermore, the use of preserved oral fluid samples to document DFC has recently been reported [15–17]. Indeed, preserved oral fluid offers a series of advantages over traditional specimens since it is non-invasive, with an easy collection protocol and can be considered as an additional source of information. It has been suggested that the concentrations of many drugs in oral fluid correlate well with their concentrations in blood, which suggests that the analysis of the former matrix may show value in the determination of the current degree of exposure to a particular drug at the time of sampling [18].
Recently, we presented a validated and highly sensitive LC-ESI-MS-MS method for the quantification of 26 commonly encountered benzodiazepines and their metabolites, zolpidem and zopiclone in three different biological matrices, i.e. blood, urine and hair [13]. During the routine application of this method on a hair sample from a regular Myolastan® user, diazepam and traces of nordiazepam were also detected in several segments (concentrations ranging from 1.0 to 8.2 pg mg−1 for diazepam). Myolastan® is a pharmaceutical specialty available on the Belgian market (Sanofi–Synthelabo, Brussels) which contains the benzodiazepine tetrazepam. Whereas tetrazepam is only used for its muscle-relaxant properties, diazepam (and its metabolite nordiazepam) also exerts strong hypnotic and sedative activities. As such, diazepam also appears on the list of alleged date-rape drugs [9]. In view of the possible erratic conclusions regarding DFC in victims taking therapeutic doses of Myolastan®, we evaluated the diazepam and tetrazepam concentrations in urine, hair and preserved oral fluid after the intake of a single or sustained therapeutic dose of Myolastan® and compared these results with those obtained after a single administration of diazepam (Valium®, Roche, Brussels).
Experimental
Specimens
Six healthy subjects (4 females and 2 males, aged 27–38 years, with a body weight varying between 64 and 93 kg) received either 50 mg tetrazepam in the form of one tablet of Myolastan® (Sanofi–Synthelabo S.A., Brussels, Belgium) or 10 mg diazepam in the form of one tablet of Valium® (Roche, Brussels, Belgium) along with 100 mL of water. In addition, one healthy female (aged 27 years, 64 kg) received a single dose of 25 mg tetrazepam in the form of half a tablet of Myolastan® each day, during a 1-week therapy. Subjects participated in the experimental part of the study through written informed consent. Urine was collected over 280 h in plastic tubes, without any preservative, and frozen at −20 °C until analysis (performed within 15 days). Preserved oral fluid was collected at regular time intervals during 600 min following administration, using the Intercept® device (OraSure Technologies, Bethlehem, PA) according to the manufacturer’s instructions. The device collects an average of 0.38 ± 0.19 mL of oral fluid and a dilution factor of 1 in 3 is arbitrarily accepted [19]. All devices were weighed before and after collection. An average weight of 0.86 ± 0.14 g of oral fluid was collected. The tubes were centrifuged and the preserved oral fluid was stored at −20 °C prior to analysis (within 15 days). Blank preserved oral fluid, used for the preparation of negative controls, calibrators and quality control (QC) samples, was obtained from healthy volunteers (also collected with the Intercept®). The data are expressed as nanograms per milliliter of diluted specimen.
A lock of hair the size of the diameter of a pencil (about 100 mg) was collected from the posterior vertex of the head 3 weeks after the last dose of Myolastan®/Valium®. Hair was clipped as close to the scalp as possible and stored at room temperature. Hair strands were aligned to keep root ends together.
Chemicals
Individual ampoules of 7-aminoclonazepam, 7-aminoflunitrazepam, bromazepam, clonazepam, flunitrazepam, clobazam, desmethylflunitrazepam, estazolam, nitrazepam, alprazolam, temazepam, desalkylflurazepam, oxazepam, nordiazepam, triazolam, lormetazepam, lorazepam, prazepam, tetrazepam, diazepam and flurazepam (at a concentration of 1 mg mL−1 in methanol) and 7-aminoclonazepam-d4, 7-aminoflunitrazepam-d7, clonazepam-d4, flunitrazepam-d7, alprazolam-d5, temazepam-d5, desalkylflurazepam-d4, oxazepam-d5, nordiazepam-d5, triazolam-d4, lorazepam-d4, prazepam-d5 and diazepam-d5 (0.1 mg mL−1 in methanol) were purchased from LGC Promochem (Molsheim, France). Brotizolam, clotiazepam, chlornordiazepam, loprazolam, cloxazolam, zolpidem and zopiclone were a gift from Dr. V. Maes (VUB, Brussels) (pure standards obtained from respective manufacturers).
Methanol (Biosolve, Valkenswaard, The Netherlands), water (Biosolve), dicholoromethane (Merck, Darmstadt, Germany) and 1-chlorobutane (Merck) were HPLC grade. Acetic acid (glacial) 100% anhydrous (Merck) and NaOH (Fluka, Buchs, Germany) were used for the preparation of the acetate buffer 3 M, pH 4.6. For the saturated ammonium chloride buffer pH 9.2, ammonium chloride from Fluka and ammonia solution 32% from Merck were used. β-Glucuronidase, Type HP-2 from Helix pomatia (111,480 units mL−1) was obtained from Sigma (Steinheim, Germany). For the mobile phase of the HPLC-DAD method, phosphoric acid, 85% wt % solution in water (Aldrich, Steinheim, Germany) and potassium dihydrogen phosphate (Merck) were used.
Preparation of standard solutions
An internal standard (IS) working solution of the deuterated analytes was prepared (0.4 μg mL−1 in methanol), which was further diluted with methanol to yield appropriate concentrations to add to samples, calibrators and QC samples.
A benzodiazepine working solution of all analytes was prepared (4 μg mL−1 in methanol) and further diluted with methanol to yield working solutions at appropriate concentrations to add to calibrators and QC samples. Separate stock solutions of tetrazepam, diazepam, nordiazepam, oxazepam and temazepam were prepared (4 μg mL−1 in methanol) and further diluted with methanol for the stability and ion suppression experiments.
Working solutions were prepared monthly and stored at 4 °C.
Sample preparation and extraction for LC-MS-MS analysis
Sample preparation
Urine and hair samples were analysed by LC-MS-MS for 26 benzodiazepines and metabolites, zolpidem and zopiclone according to a published validated procedure [13]. Briefly, urine samples (250 μL) mixed with 50 μL of the IS stock solution were buffered to pH 4.6 with 200 μL acetate buffer (3 M) and then incubated for 1 h at 56 °C with 25 μL of β-glucuronidase.
Hair samples were decontaminated, dried and cut in segments of 1–3 cm each. Approximately 20 mg was powdered in a ball mill which allowed simultaneous pulverization of 48 segments (Precellys 48, Bertin Technologies, Montigny-Le-Bretonneux, France) and then 50 μL of a 1:20 dilution of the IS stock solution was added. After incubation of the pulverized samples with 1 mL of methanol at 45 °C for 2 h with orbital shaking, samples were centrifuged. The supernatants were subsequently transferred to 10-mL disposable screw top vials and concentrated under nitrogen to 100–200 μL.
Preserved oral fluid samples (500 μL) were mixed with 50 μL of a 1:20 dilution of the IS stock solution.
Extraction
Following sample preparation, samples were extracted with 4 mL of 1-chlorobutane after the addition of a saturated ammonium chloride buffer (pH 9.2); 500 μL was used for urine and preserved oral fluid samples and 1 mL was used for the pulverized hair samples. After mechanical shaking (10 min) and centrifugation (10 min at 3,000 g), the organic phase was transferred to a 5-mL disposable screw top vial and then evaporated to dryness at 40 °C in a vacuum centrifuge. For the extracted urine samples, the residue was reconstituted in 100 μL of 0.1% formic acid in water/methanol (70:30, v/v) and 10 μL was injected into the LC-MS-MS system. The residue of the preserved oral fluid and hair samples was reconstituted in 80 μL of 0.1% formic acid in water/methanol (70:30, v/v) and 20 μL was injected into the LC-MS/MS system. The limit of quantification (LOQ) in urine was 25 ng mL−1 for tetrazepam and 10 ng mL−1 for diazepam, nordiazepam, oxazepam and temazepam. For hair samples, the LOQ was established at 10 pg mg−1 for tetrazepam and 1 pg mg−1 for diazepam, nordiazepam, oxazepam and temazepam.
LC-MS-MS
Chromatography
LC was performed using a Waters Alliance 2690 separation module (Waters, Milford, MA, USA). Analytes were separated on a Gemini C18 column (150 × 2.0 mm, 3.5 μm) (Phenomenex, Torrance, CA), using a gradient elution with 0.1% formic acid (A) and methanol (B), at a flow rate of 0.2 mL min−1. A gradient was applied starting from 10% B, and increased to 50% over the first 5 min. From 5 min to 20 min, B was linearly increased to 70% before returning to the initial conditions within 0.1 min and equilibrating for 14.9 min, which resulted in a total run time of 35 min.
Mass spectrometry
A Quattro Premier tandem mass spectrometer (Waters) was used for all analyses. Ionization was achieved using electrospray in positive mode (ESI+). The optimum conditions were capillary voltage, 1.0 kV; source block temperature, 120 °C; desolvation gas (nitrogen) heated to 270 °C and delivered at a flow rate of 700 L h−1.
The collision gas (argon) pressure was maintained at 0.35 Pa (3.5 × 10−3 mbar) and the collision energy (eV) adjusted to optimize the signal for the most abundant product ions, which were subsequently used for MRM analysis. Quantification and a confirmation transition were selected for each compound, except for the deuterated analogs, for which only one transition was chosen. The optimized MRM transitions for diazepam, nordiazepam, oxazepam, temazepam, tetrazepam and the internal standards, diazepam-d5, nordiazepam-d5, oxazepam-d5 and temazepam-d5, are presented in Table 1. All aspects of data acquisition were controlled using MassLynx NT 4.1 software with automated data processing using the TargetLynx program (Waters).
LC-MS-MS assay validation for preserved oral fluid samples
Linearity, LOQ, precision, accuracy and recovery
The method was validated for the detection of diazepam, nordiazepam, oxazepam, temazepam and tetrazepam in preserved oral fluid samples. Selectivity was evaluated by analysing preserved oral fluid samples from eight healthy volunteers who did not take any of the targeted compounds for several days before preserved oral fluid sampling and checked for the absence of the compounds of interest by analysing the samples with the present technique before using them as blanks. Assay linearity was investigated by constructing calibration curves (n = 5) using blank preserved oral fluid spiked with the analytes at concentrations of 0.05, 0.1, 0.25, 0.5, 1, 2, 5, 10, 20 and 40 ng mL−1. Quantification was achieved by integration of the area under the specific MRM chromatograms in reference to the integrated area of the deuterated analogues. Standard response curves were generated daily using a weighted (1/x) least-squares linear regression model.
The LOQ was defined as the concentration of the lowest calibrator which was calculated to be within ±20% of the nominal value and with a RSD (relative standard deviation) less than 20% [20, 21].
QCs were prepared for every run in blank matrix at a concentration of 0.75 ng mL−1 (low), 4 ng mL−1 (medium) and 15 ng mL−1 (high). Intra-assay precision was evaluated by analysis of five replicates of each QC in one run. Inter-assay precision was evaluated by replicate analysis of one set of QC samples in several experiments performed on five different days. The precision was expressed as the %RSD. A comparison of the calculated concentrations of the QC samples to their respective nominal values was used to assess the accuracy (bias) of the method.
Relative recoveries were estimated by comparing the ratio of the peak area of the low, medium and high QC samples when the non-deuterated compounds were added before extraction (n = 3) divided by the peak area of the internal standards with the ratio of the peak area obtained when the non-deuterated analytes were added after the extraction (n = 3) divided by the peak area of the IS. The deuterated standards were added before the extraction in all experiments.
Stability of unprepared and prepared samples
Stability of tetrazepam, diazepam, nordiazepam, oxazepam and temazepam was monitored in non-extracted preserved oral fluid samples spiked at the initial concentrations of 0.75 and 15 ng mL−1. Concentrations of the drugs in the samples were either determined (each in triplicate) immediately (control samples) or following incubation at room temperature for 24 h or at 4 °C for a period of 24 h, 48 h and 72 h after preparation. In addition, the stability of the same preserved oral fluid samples was evaluated after 2 weeks of incubation at −20 °C. Stability at each time point was tested against a lower acceptance limit corresponding to 90% of the mean of control samples by a one-sided t-test (P < 0.05).
The stability of tetrazepam, diazepam, nordiazepam, oxazepam and temazepam in the extracted sample (preserved oral fluid initially spiked at 0.75 ng mL−1 and 15 ng mL−1) was investigated by repeated injections of a mixture of six extracted samples (maintained in the autosampler at 4 °C) over a period of 24 h. Absolute peak areas were plotted as a function of injection time and the stability of the processed samples tested by regression analysis. Instability of the processed samples would be indicated by a slope that was significantly different from zero (P < 0.05).
Assessment of matrix effects
To assess any potential suppression or enhancement of ionization from components present in the extracted biological matrix, a continuous post-column infusion was performed using a separate solution of tetrazepam, diazepam, nordiazepam, oxazepam and temazepam (10 ng mL−1 at a flow rate of 10 μL min−1) to produce a constant elevated response in both MRM channels. The interference of this constant response was monitored following the injection of extracted samples and compared to the response following the injection of mobile phase only.
Quantification of creatinine
The concentration of creatinine in urine was determined using a Vitros 5,1 FS Chemistry System (Ortho-Clinical Diagnostics, Beerse, Belgium) and corresponding reagents according to the manufacturer’s recommendations.
GC-FID
One tablet of Myolastan® was pulverized, weighed and dissolved in 10 mL of methanol. Tribenzylamine was added as internal standard at a concentration of 0.5 mg mL−1. Samples were sonicated for 15 min and filtered using a Puradisc™ 25 NYL filter (0.45-μm pore size) (Whatman, Clifton, NJ), after which a 1-μL aliquot was injected into the chromatographic system for analysis. A Hewlett–Packard 6890 Series GC System was used furnished with a HP5-MS column (25 m, 0.32-mm i.d, 0.52-μm film thickness) (J&W Scientific, Folsom, CA) and a flame ionization detector at 300 °C. The injector was operated at 250 °C in the split mode, using a split ratio of 25:1. Helium was used as the carrier gas. The oven temperature programme was as follows: 150 °C (hold 1 min), 15 °C min−1 ramp to 300 °C (hold 3 min). The total running time was 14 min. For quantification, calibration curves with eight calibrators of diazepam and tetrazepam were prepared for each batch ranging from 2.88 μg mL−1 to 1.36 mg mL−1. Internal QC samples were analysed with each batch of samples.
HPLC-DAD
One tablet of Myolastan® was dissolved in 10 mL of methanol. After addition of the internal standard (clobazam) and 500 μL of a saturated ammonium chloride buffer (pH 9.2), a 500-μL aliquot of this solution was extracted with 4 mL of 1-chlorobutane. Analyses were performed using a Hewlett–Packard HP 1100 Series HPLC (Agilent Technologies). Analytes were separated on a Lichrospher RP8ec column (250 × 4.0 mm, 5 μm) (Merck, Darmstadt, Germany), eluted isocratically with 100 mM phosphate buffer pH 2.3/acetonitrile (63:37, v/v), delivered at a flow rate of 1 mL min−1 with a run time of 30 min. Systematic toxicological analysis was performed using a UV spectra library [22]. Wavelength calibration and accuracy checks of the DAD were performed regularly.
Results
Validation of the analytical method for preserved oral fluid samples
The selectivity of the method was acceptable in terms of absence of interferences in the blank preserved oral fluid samples analyzed. The combination of retention time and two transitions (and their relative abundances) provided high specificity for all of the compounds [13]. The deuterated IS selected for each compound is shown in Table 2. No cross-talk interference with the deuterated IS was observed.
Calibration curves for all compounds tested were prepared in blank preserved oral fluid for each batch and ranged from the LOQ to 40 ng mL−1. Linearity, LOQ, intra-assay and inter-assay precision and bias are summarized in Tables 2 and 3. The observed LOQ, ranging from 0.05 to 0.2 ng mL−1, is consistent with previous reports [23, 24]. %RSD at the low (0.75 ng mL−1), medium (4 ng mL−1) and high (15 ng mL−1) QC level were consistently below 15%. The extraction recovery of the analytes is presented in Table 4.
The stability of non-extracted spiked samples (0.75 and 15 ng mL−1) was monitored at room temperature for 24 h or at 4 °C for a period of 24 h, 48 h and 72 h. No statistically significant differences could be observed for the two different concentrations under both conditions. Also no statistical differences could be noted for the stability of non-extracted spiked samples (0.75 and 15 ng mL−1) during 2 weeks at −20 °C.
The potential for instability of the processed samples was also tested. To this end, the stability of the compounds was monitored by means of repeated injections of extracted samples (0.75 ng mL−1 and 15 ng mL−1) over a period of 24 h, and by plotting the absolute peak areas as a function of time. The results indicated no significant instability over the course of the experiment.
Post-column infusion experiments (based on the method described by Bonfiglio et al. [25]) indicated no significant ion suppression or enhancement during the chromatographic run.
Analysis of the pharmaceutical specialty Myolastan®
To assess the origin of the diazepam and nordiazepam present in hair samples from a regular Myolastan® user, it was decided to initially analyse one tablet of the pharmaceutical specialty Myolastan® (50 mg tetrazepam). The presence of diazepam in this tablet was confirmed in two different lots by various techniques (LC-MS-MS, HPLC-DAD and GC-FID). Quantification with GC-FID showed a relative concentration of around 0.068% and 0.061% of the active ingredient for two different lots of Myolastan®.
Since tetrazepam is available as Myolastan® or Epsipam® 50 mg (Will–Pharma, Wavre, Belgium) tablets, an analysis of the latter was also performed. Diazepam was also present in this preparation at a relative concentration of 0.37% of the active ingredient.
Analysis of urine samples after the controlled administration of Myolastan® and Valium®
Urine samples were analyzed according to a previously published procedure [13]. In this report, a reduced stability for tetrazepam was observed during the enzymatic hydrolysis of the urine samples. Indeed, an experiment with spiked urine samples (n = 3) showed a reduction of 94.3 ± 0.3% and 96.8 ± 0.2% for QCs at 150 ng mL−1 and 600 ng mL−1 respectively, when incubated at 56 °C for 1 h. However, no statistically significant difference was noted for diazepam, nordiazepam, oxazepam and temazepam under these conditions. Therefore, we decided to analyze all urine samples twice: once without enzymatic hydrolysis in order to have the optimal conditions for tetrazepam detection, and once using the described protocol for the quantification of diazepam, nordiazepam, oxazepam and temazepam. A limited validation including linearity, LOQ, precision and accuracy was performed (n = 5). The obtained r 2 was in all cases >0.998 with an LOQ of 10 ng mL−1. The %RSD and bias were evaluated at 40, 150 and 600 ng mL−1 and were consistently <15%.
After oral administration of a single tablet of Myolastan® (50 mg tetrazepam) to three subjects, 17 consecutive specimens of urine were collected over 280 h (Fig. 1a). Benzodiazepine concentrations of all urine samples were interpreted with respect to the creatinine content to compensate for the diuretical state. Tetrazepam was present in all urine samples, with the highest concentration on average after 12 h. After 280 h, urine samples were still positive for tetrazepam at a LOQ of 10 ng mL−1. In addition, diazepam could be detected in the first sample of two persons and was observed up to 36 h after intake. However, no metabolites of diazepam were noted in these samples. In order to rule out a possible formation of diazepam during the extraction process, blank urine samples, spiked with 600 ng mL−1 tetrazepam were analyzed following the described method. No diazepam was detected in these samples.
A typical therapy with tetrazepam includes a daily administration of 25–150 mg for 1 week. Therefore, half a tablet of Myolastan® (25 mg tetrazepam) was administered to one subject during 1 week. Urine specimens were collected for 280 h after the first intake and quantified with respect to creatinine concentrations in these samples (Fig. 1b). Diazepam was detected in these samples up to 210 h and a peak concentration was seen after 114 h. Furthermore, nordiazepam was additionally detected between 66 and 138 h. Further metabolites of diazepam could not be detected.
The concentrations detected in urine samples after single and repeated administration of Myolastan® were compared with those obtained after a single dose of Valium® (10 mg diazepam) to three persons (Fig. 1c). Traces of diazepam could only be detected in the first urine sample (8 h after intake) from one person. In the following samples from this person and all of the samples of the two other persons, only the metabolites of diazepam, i.e. nordiazepam, oxazepam and temazepam, were detected. Mean urine concentrations showed a large variation throughout the whole collection period. Whereas temazepam and oxazepam were alternately detected as the most abundant metabolite, nordiazepam was the minor metabolite in all urine samples analyzed.
Analysis of preserved oral fluid samples after the controlled administration of Myolastan® and Valium®
After administration of one tablet of Myolastan® (50 mg tetrazepam) to three volunteers, 20 specimens of oral fluid were collected from each subject with the Intercept® collection device (Fig. 2a). Tetrazepam was detectable 15 min after intake in all volunteers. Peak concentrations of tetrazepam were obtained after 105 min. Samples were still positive after 600 min. However, no diazepam or metabolites were detected in these samples.
The same study was conducted including three persons receiving one tablet of Valium® (10 mg diazepam) (Fig. 2b). Peak concentrations were noted in all subjects after 15 min, rapidly decreasing at the second time point (30 min), indicating a possible contamination of the oral cavity. A second peak was observed after 120 min. Oral fluid samples tested positive for diazepam over 600 min. The metabolites of diazepam could not be detected in these samples.
Analysis of hair samples after the controlled administration of Myolastan® and Valium®
The corresponding hair samples after the administration of a single dose or 1-week therapy with Myolastan® and a single dose of Valium® were collected 3 weeks after the last intake. After segmentation, the first three proximal segments were analyzed. Following a single dose of Myolastan®, the first segments of the three volunteers were positive for tetrazepam (17.3–59.7 pg mg−1). No diazepam or metabolites could be detected in any of the segments tested. After 1 week of therapy with the same drug, tetrazepam was detected in the first (454.0 pg mg−1) and second (13.0 pg mg−1) segment (Fig. 3). In addition, the first segment of this person was also positive for diazepam (10.7 pg mg−1). No nordiazepam was observed in any of the segments. After a single dose of Valium®, the first and second segments were positive for diazepam (2.3–6.0 pg mg−1) and nordiazepam (traces–5.4 pg mg−1). The third segment of all volunteers was negative for all drugs tested.
MRM chromatogram obtained after the analysis of the first hair segment following a 1-week therapy with Myolastan® (25 mg tetrazepam). The figure shows the response (quantifier and qualifier) for diazepam (a, b) and tetrazepam (c, d). Diazepam-d5 (e) was used as internal standard. Peak intensity is shown in the top right-hand corner of each trace
Discussion
Whereas tetrazepam is a medication with primarily muscle-relaxant effects and is commonly prescribed for the treatment of muscle spasms, diazepam acts on the CNS with mainly sedation effects. Therefore, diazepam belongs to the class of abused drugs and shows a potential to be used as a date-rape drug [10]. The detection of the latter in all hair segments from a regular Myolastan® user, who denied the consumption of diazepam at any time in her life, led us to analyze the presence of diazepam in the pharmaceutical specialty Myolastan®. Confirmation of the presence of low quantities of diazepam in different lots of this preparation was obtained through GC-FID, LC-MS-MS and HPLC-DAD. Owing to the important forensic implication of this finding, a small-scale study with single and/or repeated administration of Myolastan® and Valium® was designed. Urine and hair samples were analyzed according to a previously published method [13]. In the present paper, the same liquid–liquid extraction protocol and LC-MS-MS method have been applied for the detection of diazepam, nordiazepam, oxazepam and tetrazepam in oral fluid samples, collected with the Intercept® device. The method was fully validated and the high sensitivity of the method permits the detection of very low concentrations of drugs in these samples.
Due to the instability of tetrazepam in urine samples during the enzymatic hydrolyzation process, we decided to analyze the urine specimens with and without a hydrolysis step. Indeed, whereas diazepam is extensively metabolized to oxazepam glucuronide, conjugated nordiazepam and conjugated temazepam, it appears that tetrazepam is not excreted in the glucuronidated form [26]. Thus, a hydrolysis step would not yield a higher concentration for tetrazepam.
After the administration of a single dose of one tablet of Myolastan® (3 subjects), the presence of diazepam in urine was observed for up to 36 h after the intake. Following a 1-week therapy with half a tablet of this preparation, both diazepam and nordiazepam were present at 8–210 h and 66–138 h, respectively, after the ingestion of the first dose. These results were compared with those obtained after a single dose of Valium®. However, in this case, only the metabolites of the parent drug, i.e. nordiazepam, oxazepam and temazepam, could be detected in these urine samples, indicating a complete metabolization of diazepam.
In contrast to an earlier report [27], diazepam could be detected in oral fluid samples throughout the whole collection period after the administration of a single dose of Valium®. However, the analysis of the preserved oral fluid samples showed the presence of only the parent benzodiazepines after a single dose of Myolastan® or Valium®. Similar concentrations of tetrazepam in oral fluid were observed in a previous study [15], taking into account a 1:3 dilution due to the use of the Intercept® collector. Peak concentrations were obtained after 105 min and 120 min for tetrazepam and diazepam, respectively, which is approximately the time of peak plasma concentration [26]. The absence of nordiazepam in the preserved oral fluid samples after the intake of Valium® can be explained by the fact that average peak concentrations of nordiazepam in blood are only reached 24 h following a single oral dose of 10 mg diazepam. In addition, approximately 97% of the nordiazepam in plasma is bound to proteins [26], consequently the concentrations in the preserved oral fluid samples are probably below the LOQ during the collection period. This is also likely to be the cause of the absence of diazepam in these samples after the administration of Myolastan®.
Finally, hair samples were also collected and analyzed. These results indicated that after a single dose of Myolastan®, no diazepam could be observed; however, the 1-week therapy resulted in a positive first segment for this compound. In addition, the observed concentration was higher than that observed following a single dose of Valium®. Under the latter condition, nordiazepam could also be detected. However, it is not clear why diazepam and nordiazepam could also be detected in the second segment of all persons after the intake of a single dose of Valium®. Hair strands were collected after 3 weeks of delay, in order for the region of drug incorporation to emerge above the scalp. Therefore, with an average growth of 1 cm month−1, the administered drug should be present in the proximal segment, and not in the following segments. One possible interpretation is the variability in the incorporation of this drug into the hair shaft and axial migration after incorporation, leading to a further distribution, an observation already reported for bromazepam [7] and cocaine [28]. However, a decreased concentration would be expected in the second segment. Therefore, more research has to be done to study the incorporation of diazepam and nordiazepam in hair after controlled administration.
Another question remains as to whether or not the diazepam observed in the urine and hair samples after administration of Myolastan® is the result of the diazepam present in the pharmaceutical preparation. If this were true, diazepam should also experience complete metabolic conversion to nordiazepam, oxazepam and temazepam, as was observed after a single dose of Valium®. The presence of nordiazepam was however only noted after a repeated administration of Myolastan® with diazepam remaining the primary drug detected and the absence of other metabolites. In addition, after repeated administration of Myolastan®, only diazepam was detected in the first hair segment of this person, whereas after a single dose of Valium®, nordiazepam was also observed although lower concentrations of diazepam were present in comparison with the latter. Therefore, the results of this study may indicate that there is a metabolic conversion of tetrazepam to diazepam in the human body. In 1987, Maurer and Pfleger described the presence of the hydrolysis product of diazepam in urine samples collected after the ingestion of tetrazepam following acid hydrolysis [29]. Only one other recent report mentions the possibility of this metabolic conversion process [30]. In this report, plasma and urine were collected for 11 h and 72 h, respectively, after administration of 50 mg of tetrazepam. Nordiazepam was not detected in any of the plasma samples and diazepam could be found in only one sample. In all cases, diazepam was also detected in the first sample. In contrast to our observations, these authors also detected nordiazepam between 4 and 26 h after a single tetrazepam intake. However, no other matrices were analyzed and no correlation has been made after a single diazepam intake. Benzodiazepines are metabolized in the liver by enzymes of the cytochrome P-450 family of oxido-reductases. Therefore, the metabolic conversion of tetrazepam could be explained by a double hydroxylation of the unsaturated tetrazepam ring followed by subsequent elimination of two water molecules and the formation of the stable aromatic ring, and hence diazepam. However, further research is needed to elucidate the complete conversion process of tetrazepam.
In conclusion, detection of the presence of diazepam and nordiazepam in biological samples from suspected DFSA cases could lead to erratic conclusions. However, this study showed that, following the intake of diazepam, only diazepam metabolites were observed in urine, whereas the single or repeated administration of Myolastan® led mainly to diazepam in these samples.
Conclusions
Sedative agents are used to facilitate sexual assault due to their ability to render the victim passive, submissive and unable to resist. Most of these substances possess anterograde amnesic properties and can rapidly impair an individual. Benzodiazepines and related hypnotics are frequently observed in these cases. Diazepam is regarded as having a significant potential as a date-rape drug, whereas tetrazepam has only a low sedative effect and is commonly prescribed as a muscle relaxant. Tetrazepam is available as Myolastan® and Epsipam® 50 mg tablets in Belgium. However, the presence of low doses of diazepam in these preparations, as confirmed by LC-MS-MS, GC-FID and HPLC-DAD, could be the reason for the presence of diazepam and nordiazepam in the hair sample from a regular Myolastan® user. In the present paper, a sensitive, specific and reproducible method for the detection and quantification of tetrazepam, diazepam, nordiazepam, oxazepam and temazepam in preserved oral fluid samples is described and applied to a study involving the administration of Myolastan® and Valium®.
Our study shows that diazepam can be observed in urine samples even after a single dose. In addition, a 1-week therapy resulted in the detection of both diazepam and nordiazepam in urine samples and of diazepam in the first hair segment. However, a comparison with urine and hair samples after a single diazepam dose showed that the possible metabolic conversion of tetrazepam to diazepam is a more plausible explanation for the detection of diazepam in biological samples after the intake of Myolastan®. Due to the high protein binding property of diazepam, however, this compound was not observed in preserved oral fluid samples. These results have an important forensic implication and, therefore, the presence of diazepam and/or nordiazepam in biological samples from alleged DFSA cases should be interpreted with care.
References
Cheze M, Villain M, Pepin G (2004) Forensic Sci Int 145:123–130
ElSohly MA, Gul W, ElSohly KM, Avula B, Khan IA (2006) J Anal Toxicol 30:524–538
Hurley M, Parker H, Wells DL (2006) J Clin Forensic Med 13:181–185
Kintz P, Villain M, Dumestre-Toulet V, Ludes B (2005) J Clin Forensic Med 12:36–41
Ohshima T (2006) J Clin Forensic Med 13:44–45
Scott-Ham M, Burton FC (2006) J Clin Forensic Med 13:107–111
Villain M, Cheze M, Dumestre V, Ludes B, Kintz P (2004) J Anal Toxicol 28:516–519
Villain M, Cheze M, Tracqui A, Ludes B, Kintz P (2004) Forensic Sci Int 143:157–161
Negrusz A, Gaensslen RE (2003) Anal Bioanal Chem 376:1192–1197
Scott-Ham M, Burton FC (2005) J Clin Forensic Med 12:175–186
Kintz P, Villain M, Cheze M, Pepin G (2005) Forensic Sci Int 153:222–226
Kintz P, Villain M, Dumestre-Toulet V, Capolaghi B, Cirimele V (2005) Ther Drug Monit 27:741–743
Laloup M, Ramirez Fernandez MM, De Boeck G, Wood M, Maes V, Samyn N (2005) J Anal Toxicol 29:616–626
Kintz P, Villain M, Ludes B (2004) Ther Drug Monit 26:211–214
Concheiro M, Villain M, Bouchet S, Ludes B, Lopez-Rivadulla M, Kintz P (2005) Ther Drug Monit 27:565–570
Kintz P, Villain M, Cirimele V, Pepin G, Ludes B (2004) Forensic Sci Int 145:131–135
Kintz P, Villain M, Ludes B (2004) J Chromatogr B Anal Technol Biomed Life Sci 811:59–63
Samyn N, Verstraete A, van Haeren C, Kintz P (1999) Forensic Sci Rev 11:1–19
Cone EJ, Presley L, Lehrer M, Seiter W, Smith M, Kardos KW, Fritch D, Salamone S, Niedbala RS (2002) J Anal Toxicol 26:541–546
Shah VP, Midha KK, Dighe S, McGilveray IJ, Skelly JP, Yacobi A, Layloff T, Viswanathan CT, Cook CE (1991) Eur J Drug Metab Pharmacokinet 16:249–255
Shah VP, Midha KK, Findlay JW, Hill HM, Hulse JD, McGilveray IJ, McKay G, Miller KJ, Patnaik RN, Powell ML, Tonelli A, Viswanathan CT, Yacobi A (2000) Pharm Res 17:1551–1557
Herzler M, Herre S, Pragst F (2003) J Anal Toxicol 27:233–242
Kintz P, Villain M, Concheiro M, Cirimele V (2005) Forensic Sci Int 150:213–220
Quintela O, Cruz A, Castro A, Concheiro M, Lopez-Rivadulla M (2005) J Chromatogr B Anal Technol Biomed Life Sci 825:63–71
Bonfiglio R, King RC, Olah TV, Merkle K (1999) Rapid Commun Mass Spectrom 13:1175–1185
Moffat AC, Osselton MD, Widdop B (2004) (eds) Clarke’s analysis of drugs and poisons. Phramaceutical Press, London
Sharp ME, Wallace SM, Hindmarsh KW, Peel HW (1983) J Anal Toxicol 7:11–14
Henderson GL, Harkey MR, Zhou C, Jones RT, Jacob P III (1996) J Anal Toxicol 20:1–12
Maurer H, Pfleger K (1987) J Chromatogr 422:85–101
Pavlic M, Libiseller K, Grubwieser P, Schubert H, Rabl W (2006) Int J Legal Med (in press)
Acknowledgements
The authors would like to thank Dr. Frank Peters and Dr. Jochen Beyer for their valuable discussions and suggestions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Laloup, M., Ramirez Fernandez, M.d.M., Wood, M. et al. Detection of diazepam in urine, hair and preserved oral fluid samples with LC-MS-MS after single and repeated administration of Myolastan® and Valium®. Anal Bioanal Chem 388, 1545–1556 (2007). https://doi.org/10.1007/s00216-007-1297-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-007-1297-9