Abstract
Rationale
Cannabidiol is a non-psychoactive phytocannabinoid with great therapeutic potential in diverse psychiatric disorders; however, its antidepressant potential has been mainly ascertained in adult rats.
Objectives
To compare the antidepressant-like response induced by cannabidiol in adolescent and adult rats and the possible parallel modulation of hippocampal neurogenesis.
Methods
Male Sprague-Dawley rats were repeatedly treated with cannabidiol (3, 10, and 30 mg/kg) or vehicle (1 mL/kg) during adolescence (postnatal days, PND 27-33) or adulthood (PND 141-147) and exposed to 3 consecutive tests (forced swim, open field, two-bottle choice) that quantified behavioral despair, anxiety, and sucrose intake respectively.
Results
Cannabidiol induced differential effects depending on the age and dose administered, with a decreased sensitivity observed in adolescent rats: (1) cannabidiol (30 mg/kg) decreased body weight only in adult rats; (2) cannabidiol ameliorated behavioral despair in adolescent and adult rats, but with a different dose sensitivity (10 vs. 30 mg/kg), and with a different extent (2 vs. 21 days post-treatment); (3) cannabidiol did not modulate anxiety-like behavior at any dose tested in adolescent or adult rats; and (4) cannabidiol increased sucrose intake in adult rats.
Conclusions
Our findings support the notion that cannabidiol exerts antidepressant- and anorexigenic-like effects in adult rats and demonstrate a decreased potential when administered in adolescent rats. Moreover, since cannabidiol did not modulate hippocampal neurogenesis (cell proliferation and early neuronal survival) in adolescent or adult rats, the results revealed potential antidepressant-like effects induced by cannabidiol without the need of regulating hippocampal neurogenesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescence is a vulnerable period for the onset of depression (Burke et al. 1990), while there are similarities in the clinical presentation of adolescent and adult depression, there are differences in the biological correlates (Toenders et al. 2019) and in the responses to pharmacological treatment (Kaufman et al. 2001). Several studies have proven the effectiveness of different classes of antidepressant drugs in the treatment of depression in adults (e.g., Charney et al. 1998; Cipriani et al. 2016), but the efficacy of antidepressants during adolescence is controversial (see a network meta-analysis comparing the efficacy and safety of different types of antidepressants in children and adolescents; Cipriani et al. 2016). For example, selective serotonin reuptake inhibitor-type antidepressants are efficacious, but tricyclic antidepressants have no or limited efficacy in treating adolescent patients (see Cipriani et al. 2016). This is an important issue because treatment with antidepressants that have marginal efficacy can lead to serious consequences (i.e., increased risk of suicidal thinking and behavior in some children and adolescent with major depressive disorder), as labeled with a black box warning in all antidepressants’ prescriptions (see details in Cipriani et al. 2016). Therefore, given the limited options for a safe treatment of major depressive disorder in children and adolescents, and since antidepressants are not well studied in this population, further research on putative new targets and/or interventions is needed.
In this context, the possible role of cannabis and/or cannabinoid system in improving or worsening the symptoms associated with psychiatric pathologies has been a topic of several studies (e.g., Haney and Evins 2016). In fact, adolescence is a period of great sensitivity during brain development in which changes in the normal functioning of the endocannabinoid system signaling could potentially lead to altered developmental trajectories of neural circuits’ governing emotional behaviors (Meyer et al. 2018). One drug that seems to play an important neuroprotective role in neuropsychiatric disorders by modulating endocannabinoids is cannabidiol, a fitocannabinoid non-psychomimetic found in Cannabis sativa (see revision at Campos et al. 2017). Prior studies in rodents have proven a beneficial role for cannabidiol on ameliorating negative affect, such as ameliorating behavioral despair as measured in the forced swim test (see revision in Silote et al. 2019), inducing anxiolytic-like effects, normally observed in rodents exposed to a prior stressor (see revision in de Mello Schier et al. 2014), or producing prohedonic-like responses (Shoval et al. 2016; Linge et al. 2016). However, these studies have been mainly centered in adult rodents and it is not currently known whether cannabidiol would produce differential antidepressant-like responses in adolescent rats. Therefore, the first part of the study aimed at comparing cannabidiol potential antidepressant-like effects in adolescent and adult rats. This is of great relevance given the FDA approval of cannabidiol (Epidiolex, pure cannabidiol) for the treatment of infantile epileptic encephalopathies and further studies on its effects in adolescence are needed.
The mechanism of action by which cannabidiol exerts its effects involves multiple targets (recently revised in Silote et al. 2019). For instance, although it shows low affinity for CB1 and CB2 receptors, cannabidiol could act as an antagonist on CB1 (Thomas et al. 2007), probably ascribed to its capacity to act as a negative allosteric modulator at these receptors (Laprairie et al. 2015; Martínez-Pinilla et al. 2017). Moreover, since cannabidiol inhibits the enzymatic degradation and uptake of anandamide (Bisogno et al. 2001), it indirectly increases anandamide levels, which facilitates endocannabinoid signaling through CB1 and CB2 receptors (Pertwee 2008). In addition to the modulation of the endocannabinoid system, cannabidiol can regulate the serotoninergic system by directly binding to 5-HT1A receptors (Russo et al. 2005) and other transmitter systems and targets (see Silote et al. 2019). For example, one such neuroplasticity target could be adult hippocampal neurogenesis, which is regulated by antidepressant drugs (Dranovsky and Hen 2006) and cannabinoids in general (Prenderville et al. 2015), and by cannabidiol in particular (Wolf et al. 2010). In this context, this study evaluated cannabidiol regulation of adult hippocampal neurogenesis in adolescent and adult rats.
Materials and methods
Animals
A total of 110 male Sprague-Dawley rats bred in the animal facility at the University of the Balearic Islands were used in this study. Depending on the age and/or weight, rats were initially housed in groups of 2 to 4. The housing used standard cages in precise environmental conditions (22 °C, 70% humidity, and 12-h light/dark cycle, lights on at 8:00 AM) with ad libitum access to a standard diet and tap water. All animal experiments complied with the ARRIVE guidelines (McGrath and Lilley 2015) and were carried out in accordance with the EU Directive 2010/63/EU of the European Parliament and of the Council. Following the Spanish Royal Decree 53/2013, the Local Bioethical Committee (University of the Balearic Islands) and the regional Government (Conselleria Medi Ambient, Agricultura i Pesca, Direcció General Agricultura i Ramaderia, Govern de les Illes Balears) approved all experimental procedures. All efforts were made to minimize the number of rats used and their suffering. All procedures were performed during the light period.
Cannabidiol treatment
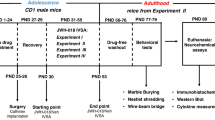
For this study, a total of 75 adolescent (PND 26 at the beginning of the experiment) or 35 adult (around PND 140 at the beginning of the experiment) male rats were used in two separate sets of experiments per age for evaluating; on the one hand, the effects of cannabidiol as a potential antidepressant agent (44 adolescent and 21 adult rats in total, see Fig. 1a and c), and on the other hand, the possible parallel regulation of hippocampal neurogenesis when behavior was altered (31 adolescent and 14 adult rats in total, see Fig. 1b and d). Notably, hippocampal neurogenesis was also evaluated in rats exposed to behavior (PND 48 or PND 175, see Fig. 1a and c). All rats were handled for 1 day (PND 26 or PND 140) prior to any drug treatment. Rats were exposed to a daily dose of cannabidiol (3, 10, or 30 mg/kg, i.p.) (purity ≥ 98%; THC Pharm, Germany) for 7 days (PND 27 to 33 or PND 141 to 147) or vehicle (1 mL/kg of a mixture of saline, 0.9% NaCl, and DMSO, 1:1 proportion or 1 mL/kg of DMSO; control groups). The doses of cannabidiol were selected based on prior studies performed in rodents (e.g., Silote et al. 2019). Rats were weighted daily throughout drug treatment.
Behavioral tests
Cannabidiol potential antidepressant-like properties were evaluated by 3 consecutive experimental tests (i.e., forced swim test, open field, sucrose preference) that measure changes in behavioral despair, anxiety-like behavior, and hedonic-like responses respectively in a subgroup of adolescent or adult rats (see Fig. 1a and c). The forced swim test, which is a widely accepted experimental tool used to screen drugs for antidepressant activity in a stress situation, consisted of a 15 min pre-test on PND 34 or PND 148 and a 5-min test on PND 35 or PND 149 (this session was videotaped). Each rat was placed in an individual tank (41 cm high × 32 cm diameter), with water to a depth of 25 cm, and at 25 ± 1 °C (see for further details García-Cabrerizo et al. 2015). Videos were then analyzed (blind to the experimental groups) to evaluate the potential antidepressant-like effects (i.e., changes in the time spent immobile) of cannabidiol administration in adolescent or adult rats (Behavioral Tracker software, CA, USA). In an attempt to evaluate the temporal course of the effects observed, a modified approach to the forced swim test was then followed (i.e., re-exposure to the test on PND 47 or PND 161, 168, and 174), until improvements on behavior in comparison with their respective control groups were vanished (see Fig. 1a and c; see similar procedures followed in García-Cabrerizo and García-Fuster 2019a). Although repetition of the same test might induce a learning dimension and/or lead to the development of tolerance to the test performance, the same conditions were followed for all rats (i.e., to compare the progression of treated rats vs. their respective controls).
Then, on PND 37 or PND 151, rats were placed for 5 min in an open field, a wall-enclosed square arena (60 × 60 cm and 40 cm of height) to evaluate potential effects on anxiety-like behavior (i.e., changes in exploratory behavior, Hernández-Hernández et al. 2018). At the beginning of the session, rats were placed in the center of the arena and left undisturbed to freely move and explore the field. The test sessions were performed and recorded under housing illumination conditions. Videos were then analyzed (blind to the experimental groups) using a digital video tracking system (Smart Video Tracking software, Version 3.0.03, Panlab SL, Barcelona, Spain) to calculate exploratory time (i.e., time spent active), distance traveled, time spent inactive, latency to center, and time spent in center (see García-Cabrerizo and García-Fuster 2019a).
Right after the open-field test, rats were single housed (PND 37 or PND 151, Fig. 1a and c) in order to evaluate their individual amount of sucrose intake in a two-bottle choice test (PND 40-41 or PND 154-155) (see further details in García-Cabrerizo and García-Fuster 2019b). To avoid bias towards any side of the cage, bottles were placed in alternate positions each day and were weighted daily to evaluate sucrose intake (g) during 48 h (PND 40 and PND 41 or PND 154 and PND 155).
Tissue collection
Rat were sacrificed at the indicated times (PND 35 or 149 for rats with no behavioral testing and PND 48 or PND 175 for rats exposed to behavioral testing, see Fig. 1) and their brains removed. For each animal, the left half-brain was quickly frozen in − 30 °C isopentane and stored at − 80 °C until 30-μm sections were cryostat cut and slide mounted throughout the entire hippocampal extent (− 1.72 to − 6.80 mm from Bregma). Hippocampal sections were stored at − 80 °C until the content of cell genesis markers (i.e., Ki-67 for cell proliferation and NeuroD for early neuronal survival; García-Fuster et al. 2010, 2011) were evaluated by immunohistochemical analysis.
Immunohistochemical analysis
Hippocampal recent cell proliferation (all diving cells within a cell cycle) was labeled with Ki-67 (Cameron and McKay 2001) and early neuronal survival was labeled with NeuroD (Lee 1997). As previously described in detail (e.g., García-Fuster et al. 2010, 2011), each cell genesis labeling was performed on 3 slides per animal containing 8 hippocampal tissue sections (24 sections total; every 8th section throughout the entire extent of the hippocampus). Sections were post-fixed in 4% paraformaldehyde followed by several steps such as antigen retrieval, blocking in peroxidase solution and BSA (with 1% serum and 0.05% Triton X-100), overnight incubation with rabbit polyclonal anti-Ki-67 (1:40,000; kindly provided by Drs. Huda Akil and Stanley J. Watson, University of Michigan) or goat polyclonal anti-NeuroD (1:25,000; Santa Cruz Biotechnology), and 1-h incubation with biotinylated anti-rabbit or anti-goat secondary antibody 1:1000 (Vector Laboratories). An Avidin/Biotin complex (Vectastain Elite ABC kit; Vectors Laboratories) and the chromogen 3,3′-diaminobenzidine (DAB) (with nickel chloride for NeuroD) were used for visualization of the antibody bound. Finally, tissue was counterstained with cresyl violet (only for Ki-67 detection), dehydrated in graded alcohols, immersed in xylene, and cover-slipped with Permount®. The number of immunostained positive cells in the dentate gyrus was quantified (by a blind experimenter to the treatment groups) with a Leica DMR light microscope (63× objective lens) in all sections following a modified unbiased stereological procedure (see García-Fuster et al. 2010, 2011). To correct for possible different areas of analysis among different treatment groups (Amrein et al. 2011; García-Cabrerizo et al. 2015; García-Cabrerizo and García-Fuster 2016), the overall number of Ki-67+ or NeuroD+ cells counted for each animal was divided by the hippocampal area quantified (mm2, as measured in a densitometer, GS-800 Imaging Calibrated Densitometer, BioRad).
Statistical analyses
Data were analyzed with GraphPad Prism, Version 6 (GraphPad Software, Inc.). Results are expressed as mean values ± standard error of the mean (SEM). Changes in body weight (g) or in behavioral despair (i.e., time spent immobile in the forced swim test) were evaluated by two-way repeated measures ANOVAs followed by a multiple comparison tests when appropriate (e.g., Sidak’s), in which treatment (vehicle vs. cannabidiol) and age (PND; as indicated in Fig. 1) were used as independent variables. Changes in anxiety-like behavior, sucrose intake, and brain markers (i.e., Ki-67, NeuroD) were evaluated at the indicated times (see Fig. 1) by one-way ANOVAs followed by Sidak’s multiple comparison tests (i.e., experimental procedures with C and 3 and 10 mg/kg of cannabidiol in adolescent rats or C and 10 and 30 mg/kg of cannabidiol in adult rats) or Student’s t test (i.e., experimental procedures with C and 30 mg/kg of cannabidiol in adolescent rats, see Fig. 1a and b). The level of significance was set at p ≤ 0.05.
Results
Cannabidiol effects on body weight in adolescent and adult rats
Rat’s weight gain did not vary throughout the duration of cannabidiol treatment in adolescence (PND 27-33): doses 3 and 10 mg/kg (no effect of treatment: F2,46 = 0.397, p = 0.675, and no treatment × PND interaction: F12,276 = 0.510, p = 0.908; Fig. 2a) and dose 30 mg/kg (no effect of treatment: F1,24 = 0.001, p = 0.991, but a significant treatment × PND interaction: F6,144 = 22.62, p < 0.001, although no post hoc comparisons rendered significant) (Fig. 2b).
Cannabidiol effects on body weight in adolescent a, b or adult c rats: an anorexigenic-like effect observed in adult rats. Doses tested: 3, 10, and 30 mg/kg of cannabidiol, i.p., 7 days. Data represents mean ± SEM of body weight (g). Two-way repeated measures ANOVAs followed by Sidak’s multiple comparison tests: *p < 0.05 when compared with control rats. CBD, cannabidiol; PND, postnatal day
When cannabidiol was administered in adult rats, although no overall effect of treatment was observed (F2,28 = 2.360, p = 0.113), there was a significant treatment × PND interaction (F12,168 = 5.075, p < 0.001), and multiple post hoc comparisons revealed a smaller body weight following 30 mg/kg of cannabidiol as observed on PND 146 and 147 (*p < 0.05 vs. control-treated rats; see Fig. 2c).
Cannabidiol effects on behavioral despair in adolescent and adult rats
The effects of cannabidiol (lower doses tested of 3 and 10 mg/kg) on the time spent immobile (s) in the forced swim test in adolescent rats (expressed as percent change vs. the respective control group) were analyzed by a two-way ANOVA-repeated measures as follows: effect of PND (35 vs. 47: F1,25 = 4.46, p = 0.045), effect of treatment (C vs. CBD: F2,25 = 3.05, p = 0.065), and treatment × PND interaction (F2,25 = 1.48, p = 0.248). When evaluating the effects of treatment at each time window of adolescence (PND 35 and PND 47), Sidak’s multiple comparison tests revealed that the dose of 10 mg/kg of cannabidiol decreased immobility on PND 35 (− 25 ± 9%, *p < 0.05 vs. C), suggesting a potential antidepressant-like effect for cannabidiol (dose of 10 mg/kg) when administered repeatedly in adolescent rats as observed 2 days post-treatment under the stress of a forced swim test (see Fig. 3a). The decreased immobility paralleled an increase in the time spent climbing (data not shown). The effects of a higher dose of cannabidiol (30 mg/kg) on immobility were assessed in a different experiment performed in adolescent rats (see Fig. 3b). A two-way ANOVA-repeated measures revealed no effect of PND (PND 35 vs. 47: F1,14 = 0.05, p = 0.830), treatment (C vs. CBD: F1,14 = 0.80, p = 0.387) nor a treatment × PND interaction (F1,14 = 0.06, p = 0.803).
Cannabidiol antidepressant-like effects in a, b adolescent or c adult rats as measured under the stress of the forced swim test. Doses tested: 3, 10, and 30 mg/kg of cannabidiol, i.p., 7 days. Data represent mean ± SEM of the time (s) spent immobile and is expressed as % change vs. control rats. Two-way repeated measures ANOVAs followed by Sidak’s multiple comparison tests: ***p < 0.001, **p < 0.01, or *p < 0.05 when compared with control rats. CBD, cannabidiol; PND, postnatal day
In adult rats, the effects of cannabidiol (doses tested of 10 and 30 mg/kg) on immobility in the forced swim test were analyzed by a two-way ANOVA-repeated measures, which revealed an effect of PND (F3,51 = 4.80, p = 0.005), an effect of treatment (F2,17 = 6.60, p = 0.008), but no treatment × PND interaction (F6,51 = 1.66, p = 0.151). When evaluating the effects of treatment at each time window tested (PND 149, 161, 168, and 174), Sidak’s multiple comparison tests revealed that 30 mg/kg of cannabidiol significantly decreased immobility up to 21 days post-treatment (PND 149: − 24 ± 6%, ***p < 0.001; PND 161: − 19 ± 6%, *p < 0.05; PND 168: − 20 ± 6%, **p < 0.01) when compared with control-treated rats, suggesting a sustained antidepressant-like effect when administered repeatedly in adult rats exposed to the stress of a forced swim test (see Fig. 3c).
Cannabidiol effects on anxiety-like behavior in adolescent and adult rats
When evaluating the effects of adolescent cannabidiol treatment (lower doses tested of 3 and 10 mg/kg) on anxiety-like behavior (PND 37), as measured in the open field, no significant results were observed by one-way ANOVAs for any of the parameters analyzed (see Fig. 4a; data expressed as percent change vs. the respective control group): overall distance traveled (F2,25 = 0.26, p = 0.772), time spent inactive (F2,25 = 0.17, p = 0.848), or time spent in center (F2,23 = 1.35, p = 0.875). Similarly, the dose of 30 mg/kg of cannabidiol did not alter any of the parameters analyzed in the open-field test in adolescent rats (see Fig. 4b): overall distance traveled (t = 0.14, df = 14, p = 0.893), time spent inactive (t = 0.53, df = 14, p = 0.606), or time spent in center (t = 1.35, df = 14, p = 0.199).`
Cannabidiol did not induce changes in anxiety-like behavior in a, b adolescent or c adult rats as measured in the open-field test (PND 37 or PND 151 respectively). Doses tested: 3, 10, and 30 mg/kg of cannabidiol, i.p., 7 days. Data represents mean ± SEM of the distance traveled (cm), the time spent inactive (s), and the time spent in center (s) and is expressed as % change vs. control rats. Two-way ANOVAs did not detect any significant effects. CBD, cannabidiol; PND, postnatal day
Comparably, in adult rats, cannabidiol (doses of 10 and 30 mg/kg) did not modulate anxiety-like behavior in the open-field test (see Fig. 4c) as measured by overall distance traveled (F2,17 = 0.47, p = 0.631), time spent inactive (F2,18 = 0.17, p = 0.847), or time spent in center (F2,18 = 0.81, p = 0.459).
Cannabidiol effects on sucrose intake in adolescent and adult rats
Adolescent cannabidiol treatment did not modify the amount of sucrose consumed (g) during 48 h (PND 40-41; data expressed as percent change vs. the respective control group): doses of 3 and 10 mg/kg (F2,24 = 1.02, p = 0.377, see Fig. 5a), and dose of 30 mg/kg (t = 0.98, df = 13, p = 0.346, see Fig. 5b). Conversely, cannabidiol increased the amount of sucrose intake following repeated cannabidiol administration in adult rats (F2,18 = 4.05, p = 0.035, Fig. 5c). Sidak’s multiple comparison tests revealed that cannabidiol significantly increased sucrose consumption when administered at the highest dose tested (30 mg/kg: + 52 ± 20%, *p < 0.05) when compared with control rats, and as observed 7 to 8 days post-treatment (see Fig. 5c).
Cannabidiol effects on the two-bottle choice test in adolescent a, b or adult c rats as measured by 1% sucrose intake (PND 40-41 or 154-155 respectively). Doses tested: 3, 10, and 30 mg/kg of cannabidiol, i.p., 7 days. Data represents mean ± SEM of the amount of 1% sucrose consumed (g) during the length of the two-bottle choice test (48 h) and is expressed as % change vs. control rats. One-way ANOVAs followed by Sidak’s multiple comparison tests a, c or Student’s t test b: *p < 0.05 when compared with age-matched control rats
Cannabidiol effects on hippocampal neurogenesis in adolescent and adult rats
When evaluating the effects of adolescent (PND 27-33) cannabidiol administration (doses of 3 and 10 mg/kg) on hippocampal neurogenesis markers, the results (data expressed as percent change vs. control group) revealed no significant changes on cell proliferation (Ki-67+ cells/area; F2,18 = 0.45, p = 0.648; see Fig. 6a, c) or early neuronal survival (NeuroD+ cells/area; F2,18 = 1.76, p = 0.200; see Fig. 6e, g) as measured 2 days post-treatment on PND 35 (when the antidepressant-like effect was observed, see Fig. 3) and compared with control rats. When adolescent rats were treated with a higher dose of cannabidiol (30 mg/kg), the results showed no changes on Ki-67+ (t = 0.23, df = 8, p = 0.821) or NeuroD+ (t = 1.44, df = 8, p = 0.189) cells/area on PND 35 (see Fig. 6a, c, e, and g). Moreover, 15 days post-treatment (PND 48), no changes were observed in Ki-67 (t = 0.36, df = 16, p = 0.722; Fig. 6a, c) or NeuroD (t = 1.57, df = 16, p = 0.136; Fig. 6e, g) for rats treated with the dose of 10 mg/kg of cannabidiol (i.e., dose that induced the antidepressant-like effects in adolescence).
Cannabidiol did not modulate cell proliferation a–d or early neuronal survival e–h in the hippocampus of adolescent (PND 35 or PND 48 a, c and e, g) or adult (PND 149 or PND 175 b, d and f, h) rats. Doses tested: 3, 10, and 30 mg/kg of cannabidiol, i.p., 7 days. a, b Quantitative analysis (mean ± SEM) of Ki-67+ cells per area (mm2) in the left dentate gyrus and expressed as % change vs. control rats. c, d Representative images of Ki-67+ (brown labeling in the blue granular layer, DAB) taken with a light microscope using a 63× objective lens to identify individual cells. Scale bar = 30 μm. e–f Quantitative analysis (mean ± SEM) of NeuroD+ cells per area (mm2) in the left dentate gyrus and expressed as % change vs. control rats. g, h Representative images of NeuroD (dark blue labeling in the blue granular layer, DAB + nickel chloride) taken with a light microscope using a 63× objective lens to identify individual cells. Scale bar = 30 μm. One-way ANOVAs or Student’s t test did not detect any significant effects
Similarly, when evaluating the effects of adult cannabidiol administration (PND 141-147) on hippocampal neurogenesis markers, the results revealed no significant changes on cell proliferation (Ki-67+ cells/area; F2,11 = 0.27, p = 0.766; see Fig. 6b, d) or early neuronal survival (NeuroD+ cells/area; F2,11 = 0.13, p = 0.877; see Fig. 6f, h) as measured 2 days post-treatment on PND 149 (when the antidepressant-like effect observed was more robust, see Fig. 3) and compared with control rats. Moreover, 28 days post-treatment (PND 175), no changes were observed in Ki-67 (t = 0.42, df = 12, p = 0.423; Fig. 6b, d) or NeuroD (t = 1.47, df = 12, p = 0.166; Fig. 6f, h) for rats treated with the dose of 30 mg/kg of cannabidiol (i.e., dose that induced the antidepressant-like effects in adulthood).
Discussion
The main results presented in this study suggest that cannabidiol has the potential to induce differential behavioral effects depending on the age and dose administered, with a decreased sensitivity observed in adolescent rats. For instance, cannabidiol (30 mg/kg) decreased body weight, an effect only observed for adult rats and that emerged following 6 days of treatment. While cannabidiol decreased immobility in the forced swim test both in adolescent and adult rats, it did so with a different dose sensitivity, 10 vs. 30 mg/kg, and with a different extent (effects observed up to 2 vs. 21 days post-treatment). Moreover, cannabidiol did not modulate anxiety-like behavior, as measured in the open field, at any dose tested in adolescent or adult rats, but increased sucrose intake exclusively in adult rats. Lastly, cannabidiol did not modulate hippocampal neurogenesis (i.e., cell proliferation and early neuronal survival) in adolescent or adult rats.
Acute cannabidiol did not affect body weight in adolescent or adult rats. However, the effects of repeated administration of cannabidiol observed on body weight were age dependent, while no effects were observed in adolescent rats, it reduced body weight in adult rats. In this context, a recent study showed that repeated cannabidiol administration during adolescence (0.5, 1, or 5 mg/kg from PND 30-60) did not alter body weight and did not promote motor or metabolic side effects in rodents (Peres et al. 2018), in line with the present results, and suggesting cannabidiol, both acutely and/or repeatedly seems to be well tolerated during adolescence. Moreover, cannabidiol (15 and 30 mg/kg, oral administration during 34 days, PND 21-55) did not alter body weight in mice (Carvalho et al. 2018). Interestingly, when revising the current literature exploring the effects of cannabidiol in adult rats, some prior studies suggested that while acute cannabidiol did not affect body weight (de Morais et al. 2018), its repeated treatment decreased body weight in rodents (e.g., Ignatowska-Jankowska et al. 2011; Santiago et al. 2019), an effect that was prevented by a CB2 receptor antagonist (Ignatowska-Jankowska et al. 2011). There is a broad literature suggesting a potential role for endocannabinoids in controlling body weight by regulating circuits that coordinate energy homeostasis (e.g., Di Marzo et al. 2001; Di Marzo and Matias 2005; Horn et al. 2018), mainly through drugs that function as an antagonist or inverse agonist over CB1 receptors (e.g., rimonabant; Horn et al. 2018). In addition to modulating the endocannabinoid system, cannabidiol also signals through other type of receptors, for example, 5-HT1A (Campos and Guimarães 2008), associated with the control of body weight (Scopinho et al. 2011). These results support the existing literature regarding the anorexigenic-like effects of cannabidiol in adult rats, and extend it, by demonstrating a reduced sensitivity to these effects in adolescent rats.
The potential expected beneficial effects of cannabidiol on regulating different aspects of emotional-like behavior were evaluated by several consecutive tests that induce distress to the animals (i.e., forced swim test, open-field test) or assess preference for sucrose intake (two-bottle choice test) and quantify behavioral despair, anxiety-like behavior, and anhedonia respectively. The results showed that cannabidiol improved behavioral despair in rats at both ages evaluated but with a different dose sensitivity (10 vs. 30 mg/kg), and with a different duration (effects observed up to 2 vs. 21 days post-treatment) for adolescent and adult rats respectively. Prior studies in regard to this topic, mainly centered in adult rodents, have proven a role for cannabidiol on ameliorating behavioral despair when animals are exposed to the stressor of the forced swim test. The first study evaluated the effects induced by acute systemic cannabidiol administration in mice (Zanelati et al. 2010) and was followed by several others (e.g., El-Alfy et al. 2010; Réus et al. 2011; Schiavon et al. 2016) that have established that both acute and/or chronic cannabidiol treatment is an effective antidepressant, at the range of doses of 3–30 mg/kg in mice and 30–60 mg/kg in rats (see revision in Silote et al. 2019). To our knowledge, this is the first study to compare the antidepressant-like potential of cannabidiol in rats at different ages during development, proving a decreased response in adolescent rats. This adds up to the existing literature suggesting a lack of efficacy of certain antidepressants when given to children or adolescents (Cipriani et al. 2016) and could be caused by age-related variations in the maturation rates of brain neurotransmitters systems involved in the response (i.e., the serotonergic nervous system matures earlier than the noradrenergic system, see Kozisek et al. 2008 for differential antidepressant-like response in adolescence; the endocannabinoid system has a crucial role during the brain development, see Viveros et al. 2012) or in the elimination rates of the drug (i.e., lower doses of the antidepressant desipramine were needed in adolescent rats to obtain the same brain desipramine concentrations as adults due to slower elimination rates, see Kozisek et al. 2007). In this context, the present results denoted different dosing regimens (10 mg/kg vs. 30 mg/kg) in adolescent vs. adult rats to achieve an antidepressant-like effect in the forced swim test 2 days post-treatment. Moreover, the present results showed that cannabidiol beneficial effects lasted up to 21 days post-treatment in adult rats, suggesting a long-term and sustained antidepressant-like effect. While most of the prior studies have been centered in proving the fast-acting antidepressant-like effects induced by cannabidiol (e.g., Linge et al. 2016, see revision in Silote et al. 2019), a recent study also showed that the effects of cannabidiol lasted for up to a week after a single injection, both in mice and rats (Sales et al. 2019), that together with the current data support a promising therapeutic profile for cannabidiol as a long-lasting antidepressant when administered in adulthood.
Additionally, cannabidiol has been shown to induce anxiolytic-like effects in rodents (see revision in de Mello Schier et al. 2014), among multiple examples from the literature, following sleep disruption (Hsiao et al. 2012), a prior foot shock (Rock et al. 2017) or the induction of neuropathic pain (de Gregorio et al. 2019). Therefore, the lack of cannabidiol significant effects on modulating anxiety-like behavior, as measured by different features in the open-field test, in adolescent or adult rats, could be explained by the fact that cannabidiol might require the presence of a specific stressor to induce anxiolytic-like effects or that other behavioral tests more specific to measure changes in anxiety-like behavior (i.e., elevated plus maze, novelty-suppressed feeding) are needed to capture cannabidiol anxiolytic-like effects. Alternatively, the regimen of cannabidiol used in this study may have led to the development of tolerance to the anxiolytic effects of the drug, thus inducing a decreased sensitivity observed as a lack of effects in the open field. Finally, the fact that the open-field test was performed 4 days after the last treatment dose administered, and/or that rats were previously exposed to 2 sessions in the forced swim test in 2 consecutive days, might justify the present negative outcome, in disagreement with some prior literature supporting an anxiolytic-like role for cannabidiol.
Finally, the results of the sucrose preference test revealed a potential prohedonic-like effect induced by cannabidiol when administered repeatedly (30 mg/kg) in adult rats and observed up to 7 and 8 days post-treatment. Similarly, 30 mg/kg of cannabidiol (oral administration by food pellet), but not the dose of 15 or 45 mg/kg, induced a prohedonic-like effect in adult Wistar-Kyoto rats in the sucrose preference test (Shoval et al. 2016). Comparably, repeated, but not acute, cannabidiol (50 mg/kg, 7 d, i.p.) induced a prohedonic effect in male C57BL6 mice (with an olfactory bulbectomy), in the sucrose preference test (Linge et al. 2016). The observed increase in sucrose consumption might be a way to balance energy homeostasis (i.e., decreased body weight observed in adult rats following repeated intake of 30 mg/kg). Thus far, the behavioral results suggest a great potential for cannabidiol as a long-lasting antidepressant when administered in adulthood while prove a decreased effect in adolescence, in line with the expected differences observed for other pharmacological treatments in adolescents (Kaufman et al. 2001; Cipriani et al. 2016).
Given the accepted regulation of adult hippocampal neurogenesis by antidepressant drugs (Dranovsky and Hen 2006) and by cannabinoids (Prenderville et al. 2015), this study evaluated whether there was a parallel regulation between the antidepressant-like effect observed 2 days post-treatment in rats and hippocampal neurogenesis regulation. Surprisingly, the results showed that cannabidiol did not modulate hippocampal neurogenesis, as evaluated by a marker of recent cell proliferation (Ki-67) and a marker of early neuronal survival (NeuroD) in adolescent or adult rats. Most of the literature supports a role for cannabidiol on inducing hippocampal neurogenesis (Wolf et al. 2010), in a dose-dependent fashion (Luján et al. 2018). However, one study suggested a negative impact of cannabidiol on neurogenesis at high doses (i.e., increased neurogenesis following 3 mg/kg but decreased with 30 mg/kg, see Cheng et al. 2014). In summary, most of the experiments relied on murine models exposed to a prior stress and were performed during adulthood (see revision in Campos et al. 2017). For example, cannabidiol induced an anxiolytic-like effect in chronically stresses mice in association with the regulation of hippocampal neurogenesis (Fogaça et al. 2018). In support of the present results, a recent study showed a dissociation between the regulation of emotional behavior and the proliferative effects induced by repeated cannabidiol (Schiavon et al. 2016), suggesting, together with the present results that the antidepressant-like effects of cannabidiol might occur independently of adult neurogenesis in naïve animals. Thus, the potential mechanism by which cannabidiol induced its antidepressant- and/or prohedonic-like effects might involve increases of anandamide levels through the inhibition of its uptake or metabolism (Gorzalka and Hill 2011; Micale et al. 2013) and/or the activation of 5-HT1A receptors (Carr and Lucki 2011; Linge et al. 2016) and deserves further studies.
To conclude, our findings support the notion that cannabidiol exerts antidepressant- and anorexigenic-like effects in adult rats and prove a decreased potential when administered in adolescent rats. Moreover, the results reveal that the potential antidepressant-like effects induced by cannabidiol are observed without the need of regulating hippocampal neurogenesis. These results indicate clear differences in the effects cannabidiol exert in adolescent vs. adult rats suggesting the need for further studies to elucidate the mechanisms behind the observed decreased sensitivity in adolescence.
References
Amrein I, Isler K, Lipp HP (2011) Comparing adult hippocampal neurogenesis in mammalian species and orders: influence of chronological age and life history stage. Eur J Neurosci 34:978–987
Bisogno T, Hanus L, De Petrocellis L, Tchilibon S, Ponde DE, Brandi I, Moriello AS, Davis JB, Mechoulam R, Di Marzo V (2001) Molecular targets for cannabidiol and its synthetic analogues: effect on vanilloid VR1 receptors and on the cellular uptake and enzymatic hydrolysis of anandamide. Br J Pharmacol 134:845–852
Burke KC, Burke JD Jr, Regier DA, Rae DS (1990) Age at onset of selected mental disorders in five community populations. Arch Gen Psychiatry 47:511–518
Cameron HA, McKay RD (2001) Adult neurogenesis produces a large pool of new granule cells in the dentate gyrus. J Comp Neurol 435:406–417
Campos AC, Guimarães FS (2008) Involvement of 5HT1A receptors in the anxiolytic-like effects of cannabidiol injected into the dorsolateral periaqueductal gray of rats. Psychopharmacology 199:223–230
Campos AC, Fogaça MV, Scarante FF, Joca SRL, Sales AJ, Gomes FV, Sonego AB, Rodrigues NS, Galve-Roperh I, Guimarães FS (2017) Plastic and neuroprotective mechanisms involved in the therapeutic effects of cannabidiol in psychiatric disorders. Front Pharmacol 8:269
Carr GV, Lucki I (2011) The role of serotonin receptor subtypes in treating depression: a review of animal studies. Psychopharmacology 213:265–287
Carvalho RK, Souza MR, Santos ML, Guimarães FS, Pobbe RLH, Andersen ML, Mazaro-Costa R (2018) Chronic cannabidiol exposure promotes functional impairment in sexual behavior and fertility of male mice. Reprod Toxicol 81:34–40
Charney DS, Berman RM, Miller H (1998) Treatment of depression. In: Schatzberg AF, Nemeroff CB (eds) The American psychiatric press textbook of psychopharmacology. American Psychiatric Press, Washington, D.C., pp 705–731
Cheng D, Low JK, Logge W, Garner B, Karl T (2014) Chronic cannabidiol treatment improves social and object recognition in double transgenic APPswe/PS1∆E9 mice. Psychopharmacology 231:3009–3017
Cipriani A, Zhou X, Del Giovane C, Hetrick SE, Qin B, Whittington C, Coghill D, Zhang Y, Hazell P, Leucht S, Cuijpers P, Pu J, Cohen D, Ravindran AV, Liu Y, Michael KD, Yang L, Liu L, Xie P (2016) Comparative efficacy and tolerability of antidepressants for major depressive disorder in children and adolescents: a network meta-analysis. Lancet 388:881–890
de Gregorio D, McLaughlin RJ, Posa L, Ochoa-Sanchez R, Enns J, Lopez-Canul M, Aboud M, Maione S, Comai S, Gobbi G (2019) Cannabidiol modulates serotonergic transmission and reverses both allodynia and anxiety-like behavior in a model of neuropathic pain. Pain 160:136–150
de Mello Schier AR, de Oliveira Ribeiro NP, Coutinho DS, Machado S, Arias-Carrión O, Crippa JA, Zuardi AW, Nardi AE, Silva AC (2014) Antidepressant-like and anxiolytic-like effects of cannabidiol: a chemical compound of Cannabis sativa. CNS Neurol Disord Drug Targets 13:953–960
de Morais H, Chaves YC, Waltrick APF, Jesus CHA, Genaro K, Crippa JA, da Cunha JM, Zanoveli JM (2018) Sub-chronic treatment with cannabidiol but not with URB597 induced a mild antidepressant-like effect in diabetic rats. Neurosci Lett 682:62–68
Di Marzo V, Matias I (2005) Endocannabinoid control of food intake and energy balance. Nat Neurosci 8:585–589
Di Marzo V, Goparaju SK, Wang L et al (2001) Leptin-regulated endocannabinoids are involved in maintaining food in- take. Nature 410:822–825
Dranovsky A, Hen R (2006) Hippocampal neurogenesis: regulation by stress and antidepressants. Biol Psychiatry 59:1136–1143
El-Alfy AT, Ivey K, Robinson K, Ahmed S, Radwan M, Slade D, Khan I, ElSohly M, Ross S (2010) Antidepressant-like effect of delta9-tetrahydrocannabinol and other cannabinoids isolated from Cannabis sativa L. Pharmacol Biochem Behav 95:434–442
Fogaça MV, Campos AC, Coelho LD, Duman RS, Guimarães FS (2018) The anxiolytic effects of cannabidiol in chronically stressed mice are mediated by the endocannabinoid system: role of neurogenesis and dendritic remodeling. Neuropharmacology 135:22–33
García-Cabrerizo R, García-Fuster MJ (2016) Comparative effects of amphetamine-like psychostimulants on rat hippocampal cell genesis at different developmental ages. Neurotoxicology 56:29–39
García-Cabrerizo R, García-Fuster MJ (2019a) Adolescent cocaine exposure enhanced negative affect following drug re-exposure in adult rats: attenuation of c-Fos activation. J Psychopharmacol 33:154–162
García-Cabrerizo R, García-Fuster MJ (2019b) Methamphetamine binge administration dose-dependently enhanced negative affect and voluntary drug consumption in rats following prolonged withdrawal: role of hippocampal FADD. Addict Biol 24:239–250
García-Cabrerizo R, Keller B, García-Fuster MJ (2015) Hippocampal cell fate regulation by chronic cocaine during periods of adolescent vulnerability: consequences of cocaine exposure during adolescence on behavioral despair in adulthood. Neuroscience 304:302–315
García-Fuster MJ, Perez JA, Clinton SM, Watson SJ, Akil H (2010) Impact of cocaine on adult hippocampal neurogenesis in an animal model of differential propensity to drug abuse. Eur J Neurosci 31:79–89
García-Fuster MJ, Flagel SB, Mahmood ST, Mayo LM, Thompson RC, Watson SJ, Akil H (2011) Decreased proliferation of adult hippocampal stem cells during cocaine withdrawal: possible role of the cell fate regulator FADD. Neuropsychopharmacology 36:2303–2317
Gorzalka BB, Hill MN (2011) Putative role of endocannabinoid signaling in the etiology of depression and actions of antidepressants. Prog Neuro-Psychopharmacol Biol Psychiatry 35:1575–1585
Haney M, Evins AE (2016) Does cannabis cause, exacerbate or ameliorate psychiatric disorders? An oversimplified debate discussed. Neuropsychopharmacology 41:393–401
Hernández-Hernández E, Miralles A, Esteban S, García-Fuster MJ (2018) Improved age-related deficits in cognitive performance and affective-like behavior following acute, but not repeated, 8-OH-DPAT treatments in rats: regulation of hippocampal FADD. Neurobiol Aging 71:115–126
Horn H, Böhme B, Dietrich L, Koch M (2018) Endocannabinoids in body weight control. Pharmaceuticals (Basel) 11:E55. https://doi.org/10.3390/ph11020055
Hsiao YT, Yi PL, Li CL, Chang FC (2012) Effect of cannabidiol on sleep disruption induced by the repeated combination tests consisting of open field and elevated plus-maze in rats. Neuropharmacology 62:373–384
Ignatowska-Jankowska B, Jankowski MM, Swiergiel AH (2011) Cannabidiol decreases body weight gain in rats: involvement of CB2 receptors. Neurosci Lett 490:82–84
Kaufman J, Martin A, King RA, Charney D (2001) Are child-, adolescent-, and adult-onset depression one and the same disorder? Biol Psychiatry 49:980–1001
Kozisek ME, Deupree JD, Burke WJ, Bylund DB (2007) Appropriate dosing regimens for treating juvenile rats with desipramine for neuropharmacological and behavioral studies. J Neurosci Methods 163:83–91
Kozisek ME, Middlemas D, Bylund DB (2008) The differential regulation of BDNF and TrkB levels in juvenile rats after four days of escitalopram and desipramine treatment. Neuropharmacology 54:251–257
Laprairie RB, Bagher AM, Kelly ME, Denovan-Wright EM (2015) Cannabidiol is a negative allosteric modulator of the cannabinoid CB1 receptor. Br J Pharmacol 172:4790–4805
Lee JE (1997) NeuroD and neurogenesis. Dev Neurosci 19:27–32
Linge R, Jiménez-Sánchez L, Campa L, Pilar-Cuéllar F, Vidal R, Pazos A, Adell A, Díaz Á (2016) Cannabidiol induces rapid-acting antidepressant-like effects and enhances cortical 5-HT/glutamate neurotransmission: role of 5-HT1A receptors. Neuropharmacology 103:16–26
Luján MÁ, Castro-Zavala A, Alegre-Zurano L, Valverde O (2018) Repeated Cannabidiol treatment reduces cocaine intake and modulates neural proliferation and CB1R expression in the mouse hippocampus. Neuropharmacology 143:163–175
Martínez-Pinilla E, Varani K, Reyes-Resina I, Angelats E, Vincenzi F, Ferreiro-Vera C, Oyarzabal J, Canela EI, Lanciego JL, Nadal X, Navarro G, Borea PA, Franco R (2017) Binding and signaling studies disclose a potential allosteric site for cannabidiol in cannabinoid CB2 receptors. Front Pharmacol 8:744
McGrath JC, Lilley E (2015) Implementing guidelines on reporting research using animals (ARRIVE etc.): new requirements for publication in BJP. Br J Pharmacol 172:3189–3193
Meyer HC, Lee FS, Gee DG (2018) The role of the endocannabinoid system and genetic variation in adolescent brain development. Neuropsychopharmacology 43:21–33
Micale V, Di Marzo V, Sulcova A, Wotjak CT, Drago F (2013) Endocannabinoid system and mood disorders: priming a target for new therapies. Pharmacol Ther 138:18–37
Peres FF, Diana MC, Levin R, Suiama MA, Almeida V, Vendramini AM, Santos CM, Zuardi AW, Hallak JEC, Crippa JA, Abílio VC (2018) Cannabidiol administered during peri-adolescence prevents behavioral abnormalities in an animal model of schizophrenia. Front Pharmacol 9:901
Pertwee RG (2008) The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: delta9-tetrahydrocannabinol, cannabidiol and delta9-tetrahydrocannabivarin. Br J Pharmacol 153:199–215
Prenderville JA, Kelly ÁM, Downer EJ (2015) The role of cannabinoids in adult neurogenesis. Br J Pharmacol 172:3950–3963
Réus GZ, Stringari RB, Ribeiro KF, Luft T, Abelaira HM, Fries GR, Aguiar BW, Kapczinski F, Hallak JE, Zuardi AW, Crippa JA, Quevedo J (2011) Administration of cannabidiol and imipramine induces antidepressant-like effects in the forced swimming test and increases brain-derived neurotrophic factor levels in the rat amygdala. Acta Neuropsychiatr 23:241–248
Rock EM, Limebeer CL, Petrie GN, Williams LA, Mechoulam R, Parker LA (2017) Effect of prior foot shock stress and Δ9-tetrahydrocannabinol, cannabidiolic acid, and cannabidiol on anxiety-like responding in the light-dark emergence test in rats. Psychopharmacology 234:2207–2217
Russo EB, Burnett A, Hall B, Parker KK (2005) Agonistic properties of cannabidiol at 5-HT1a receptors. Neurochem Res 30:1037–1043
Sales AJ, Fogaça MV, Sartim AG, Pereira VS, Wegener G, Guimaraes FS, Joca SRL (2019) Cannabidiol induces rapid and sustained antidepressant-like effects through increased BDNF signaling and synaptogenesis in the prefrontal cortex. Mol Neurobiol 56:1070–1081
Santiago AN, Mori MA, Guimarães FS, Milani H, Weffort de Oliveira RM (2019) Effects of cannabidiol on diabetes outcomes and chronic cerebral hypoperfusion comorbidities in middle-aged rats. Neurotox Res 35:463–474
Schiavon AP, Bonato JM, Milani H, Guimarães FS, Weffort de Oliveira RM (2016) Influence of single and repeated cannabidiol administration on emotional behavior and markers of cell proliferation and neurogenesis in non-stressed mice. Prog Neuro-Psychopharmacol Biol Psychiatry 64:27–34
Scopinho AA, Guimarães FS, Corrêa FM, Resstel LB (2011) Cannabidiol inhibits the hyperphagia induced by cannabinoid-1 or serotonin-1A receptor agonists. Pharmacol Biochem Behav 98:268–272
Shoval G, Shbiro L, Hershkovitz L, Hazut N, Zalsman G, Mechoulam R, Weller A (2016) Prohedonic effects of cannabidiol in a rat model of depression. Neuropsychology 73:123–129
Silote GP, Sartim A, Sales A, Eskelund A, Guimarães FS, Wegener G, Joca S (2019) Emerging evidence for the antidepressant effect of cannabidiol and the underlying molecular mechanisms. J Chem Neuroanat 98:104–116
Thomas A, Baillie GL, Phillips AM, Razdan RK, Ross RA, Pertwee RG (2007) Cannabidiol displays unexpectedly high potency as an antagonist of CB1 and CB2 receptor agonists in vitro. Br J Pharmacol 150:613–623
Toenders YJ, van Velzen LS, Heideman IZ, Harrison BJ, Davey CG, Schmaal L (2019) Neuroimaging predictors of onset and course of depression in childhood and adolescence: a systematic review of longitudinal studies. Dev Cogn Neurosci 39:100700
Viveros MP, Llorente R, Suarez J, Llorente-Berzal A, López-Gallardo M, de Fonseca FR (2012) The endocannabinoid system in critical neurodevelopmental periods: sex differences and neuropsychiatric implications. J Psychopharmacol 26:164–176
Wolf SA, Bick-Sander A, Fabel K, Leal-Galicia P, Tauber S, Ramirez-Rodriguez G, Müller A, Melnik A, Waltinger TP, Ullrich O, Kempermann G (2010) Cannabinoid receptor CB1 mediates baseline and activity-induced survival of new neurons in adult hippocampal neurogenesis. Cell Commun Signal 8:12
Zanelati TV, Biojone C, Moreira FA, Guimarães FS, Joca SR (2010) Antidepressant-like effects of cannabidiol in mice: possible involvement of 5-HT1A receptors. Br J Pharmacol 159:122–128
Acknowledgments
We would like to thank Drs. Huda Akil and Stanley J. Watson (University of Michigan, Ann Arbor, MI, USA) who kindly provided Ki-67 antibody.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article. This study was funded by Delegación del Gobierno para el Plan Nacional sobre Drogas (grant 2016/002, Ministerio de Sanidad, Servicios Sociales e Igualdad, Spain) and by Fundación Alicia Koplowitz to MJG-F. MJG-F is a member of RETICS-RTA (RD16/0017/0010; Instituto de Salud Carlos III, MINECO/FEDER). The program “TECH” from project “TALENT PLUS Construint Salut, Generant Valor” (IdISBa, GOIB) supports CB-H’s salary.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bis-Humbert, C., García-Cabrerizo, R. & García-Fuster, M.J. Decreased sensitivity in adolescent versus adult rats to the antidepressant-like effects of cannabidiol. Psychopharmacology 237, 1621–1631 (2020). https://doi.org/10.1007/s00213-020-05481-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-020-05481-4