Abstract
Rationale
While the relationship between inflammation and depression is well-established, the molecular mechanisms mediating this relationship remain unclear. RNA sequencing analysis comparing brains of vehicle- and lipopolysaccharide-treated mice revealed LCN2 among the most dysregulated genes. As LCN2 is known to be an important regulator of the immune response to bacterial infection, we investigated its role in the behavioral response to lipopolysaccharide.
Objective
To explore the role of LCN2 in modulating behavior following lipopolysaccharide administration using wild type (WT) and lcn2−/− mice.
Methods
Using a within-subjects design, mice were treated with 0.33 mg/kg liposaccharide (LPS) and vehicle. Primary outcome measures included body weight, food consumption, voluntary wheel running, sucrose preference, and the tail suspension test. To evaluate the inflammatory response, 1 week later, mice were re-administered either vehicle or LPS and terminated at 6 h.
Results
While lcn2−/− mice had increased baseline food consumption and body weight, they showed a pattern of reduced food consumption and weight loss similar to WT mice in response to LPS. WT and lcn2−/− mice both recovered voluntary activity on the fourth day following LPS. LPS induced equivalent reductions in sucrose preference and TST immobility in the WT and lcn2−/− mice. Finally, there were no significant effects of genotype on inflammatory markers.
Conclusions
Our data demonstrate that lcn2 is dispensable for sterile inflammation-induced sickness and depression-like behavior. Specifically, lcn2−/− mice displayed sickness and immobility in the tail suspension test comparable to that of WT mice both in terms of intensity and duration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
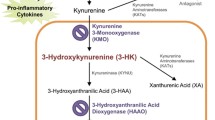
The possibility of a causal relationship between inflammation and depression stems from a number of preclinical and clinical data. In laboratory rodent models, both acute inflammation (e.g., administration of cytokine inducers such as lipopolysaccharide (LPS)) and chronic inflammation (e.g., inoculation of Bacillus Calmette-Guerin) result in the development of depression-like behavior (Frenois et al. 2007; Moreau et al. 2008; Moreau et al. 2005; O’Connor et al. 2009). At the clinical level, symptoms of depression are associated with elevated levels of biomarkers of inflammation (Dowlati et al. 2010; Goldsmith et al. 2016; Haapakoski et al. 2015; Leighton et al. 2018; Smith et al. 2018; Valkanova et al. 2013). Furthermore, administration of endotoxin to volunteers has been shown to induce depressed mood (Eisenberger et al. 2010; Reichenberg et al. 2001) while administration of anti-cytokine treatment alleviates symptoms of depression in patients with chronic inflammatory diseases as well as in psychiatric patients with elevated biomarkers of inflammation (Kappelmann et al. 2018; Raison et al. 2013). The mechanisms of these effects are under intense study. Inflammatory cytokines act on the brain by various pathways that all converge on dopaminergic, glutamatergic, and serotoninergic neurotransmission (Dunn et al. 1999; Miller et al. 2013; Schaefer et al. 2003). One aspect that is still obscure is the way that these effects are regulated at the molecular level.
In an attempt to identify possible novel mechanisms of inflammation-induced depression, we conducted an unbiased RNA sequencing study in which we compared mice treated with vehicle or the inflammatory inducer LPS. For this study, we focused on the parietal cortex. The parietal cortex is an important region for attention and sensorimotor integration and is the projection site of whisker sensory information in rodents (Colby and Goldberg 1999; Mohan et al. 2018; Teixeira et al. 2014). There is growing awareness of the importance of sensory and motor systems in mental health. Further, prior research has demonstrated that depression is often associated with reduced activity within the parietal cortex and particularly within the frontoparietal circuit. For example, it has shown that depression was associated with decreased glucose metabolism within the parietal cortex (Biver et al. 1994). Further, Vasic and colleagues demonstrated that the prefrontoparietal network showed reduced connectivity in patients with MDD (Vasic et al. 2009). These findings are supported by a study demonstrating reduced resting state connectivity within frontoparietal network using a meta-analysis comprising data from over 1000 individuals (Kaiser et al. 2015). The targets that showed the greatest change in response to LPS were evaluated in the context of the literature. One of the identified targets was lipocalin-2 (LCN2).
LCN2, also known as neutrophil gelatinase-associated lipocalin (NGAL), is the product of the lcn2 gene. This glycoprotein plays an important role in the regulation of the innate immune response to bacterial infection (Goetz et al. 2002) and it is associated with a variety of inflammatory conditions (Gouweleeuw et al. 2015; Marijnissen et al. 2014; Mommersteeg et al. 2016; Naude et al. 2012, 2014, 2015). In a recent report, bone-derived LCN2 was reported to suppress appetite by acting at the melanocortin 4 receptor in the hypothalamus (Mosialou et al. 2017). This observation led to the speculation that LCN2 could be involved in inflammation-induced anorexia (Palmiter 2017). However, the literature is unclear concerning its role in regulating inflammation-induced behavioral alterations. As we observed a high level of expression of brain lcn2 at the time at which we usually observe depression-like behavior in LPS-treated mice, we decided to explore its possible role in LPS-induced sickness (including reduced food consumption and voluntary activity) and in pharmacological tests of anti-depressant activity (tail suspension test and sucrose preference) by comparing wild type to lcn2 genetically deficient mice. The present experiments show that lcn2-deficient mice did not differ from wild-type mice in their behavioral response to LPS.
Methods
Animals and drugs
Experiments were conducted in adult wild-type C57BL/6J mice and lcn2−/− (stock number 024630) mice purchased from Jackson Laboratories (Bar Harbor, ME). The mice were housed in a temperature- and humidity-controlled environment on a 12-h light:dark cycle with food and water available ad libitum. Mice were treated with LPS (L-3129, serotype 012:B8, Sigma-Aldrich) and/or sterile saline vehicle by intraperitoneal injection (IP). All protocols were approved by the University of Texas MD Anderson Cancer Center Institutional Animal Care and Use Committee.
Behavioral testing
Mice were single housed with wireless low profile running wheels (Med Associates, Fairfax, VT). Wheel access was provided approximately 2 weeks prior to the start of drug treatment and continued throughout the experiment.
Depression-like behavior was assessed in two pharmacological tests sensitive to anti-depressant drugs, sucrose preference and tail suspension test. In both cases, the use of the depression-like behavior terminology does not imply that the behavioral performance of mice in these tests reflects any form of “depressed” mood. Sucrose preference was assessed by providing single-housed mice access to two identical water bottles, one containing normal drinking water and the other containing a 1% sucrose solution. As anticipated, mice rapidly developed a preference for the sweetened solution as measured by weighing the bottles (percent sucrose preference = [sucrose consumed]/[total sucrose + water consumed]*100). Preference was established prior to the start of drug treatments. Sucrose preference was evaluated 24 and 48 h post-treatment. Within the first 24 h, alterations can be attributed to the sickness phase, while deficits after 24 h are generally interpreted to be an indication of depression-like behavior. The tail suspension test was performed 24 h post-treatment and immobility during the 6-min test was scored by an experimenter blind to experimental condition (Can et al. 2012). This test has been shown to be responsive to inflammation-induced depression and is a sensitive indicator anti-depressant activity (Castagne et al. 2011; O’Connor et al. 2009).
Tissue processing
At the completion of experimental procedures, mice were euthanized and tissue was collected after intracardiac perfusion of PBS, snap frozen in liquid nitrogen, and stored at − 80C until analyzed. RNA was extracted using E.Z.N.A. Total RNA Isolation kit (Omega Bio-Tek, Norcross, GA). RNA sequencing was performed at the UCLA Neuroscience Genomics Core, with cDNA synthesis using the Illumina TruSeq Stranded RNA system with RiboZero Gold reduction of globin and ribosomal RNAs. Sequencing was performed on an Illumina HiSeq 4000 instrument, acquiring an average of 11.8 million single-stranded 65 bp reads per sample. Reads were mapped to the Mus musculus transcriptome (GRCm38.89) using hisat2, and mRNA abundance was quantified as transcripts per million and log2-transformed for analysis by linear statistical models with false discovery rate correction for multiple testing. Endpoint quality control metrics (alignment rate and mean profile correlation with other samples) identified one aberrant sample from a mouse in the LPS-treated group, which was excluded from further analyses.
For qRT-PCR following the behavioral experiment, liver and brain RNA was reverse transcribed using a High Capacity cDNA Revers Transcription Kit (Applied Biosystems, Thermo Fisher Scientific, Waltham, MA) and analyzed by real-time PR-PCR using TaqMan Gene expression assays. Il-1β (Mm.PT.58.17212823), Il-6 (Mm.PT.58.13354106), Tnf-α (Mm.PT.56a.12575861), and Gapdh (Mm.PT.39a.1) were purchased from IDT (Coralville, IA), and Itgam (Mm01271259) was from Applied Biosystems (Waltham, MA). Plasma was evaluated for IL-6 levels (BioLegend Mouse IL-6 ELISA MAX, catalog number 431304).
Experimental protocols
Experiment 1: Mice were treated with vehicle or 0.5 mg/kg LPS and were euthanized 24 h after treatment (n = 6 mice/group). Cortical tissue (particularly at the area of the parietal cortex) was collected and RNA sequencing was performed as described above.
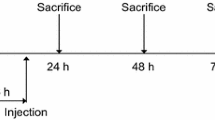
Experiment 2: Using a within-subjects counterbalanced design, all mice were treated with 0.33 mg/kg LPS and vehicle. Treatment occurred within 30 min of the onset of the dark cycle. The treatments were separated by an interval of 1 week. Body weight and food consumption was assessed at 12, 24, 36, 48, and 72 h post-treatment. Voluntary wheel running, sucrose preference, and TST were performed as described above. To evaluate the inflammatory response to LPS, 1 week after, the second treatment mice were re-administered either vehicle or LPS and terminated 6 h later. Given that the response LPS is blunted with repeated injections, a dose of 1.0 mg/kg was selected for the second injection.
Statistical analysis
Data from the behavioral study were analyzed using one-way or two-way ANOVAs with repeated measures on the time factor followed by Tukey post hoc analyses when significant interactions were identified. Each animal was treated as its own control. Data are presented as mean ± standard error of the mean (SEM).
Results
RNA sequencing implicated Lcn2 in LPS-induced neuroinflammation
The RNA sequencing analysis, corrected for multiple comparisons, revealed 128 genes that were significantly dysregulated in response to LPS treatment (Vichaya et al., in preparation). We present the 4 targets that showed the greatest change in response to LPS in Table 1 (> 50-fold change compared to control). From this analysis, we focused on the third most dysregulated gene, lcn2, based on the published findings pointing to its possible role in regulation of inflammation (Gouweleeuw et al. 2015; Marijnissen et al. 2014; Mommersteeg et al. 2016; Naude et al. 2012, 2014, 2015).
Lcn2 deficiency did not influence LPS-induced sickness behavior
Administration of LPS induces a sickness episode that peaks during the first 3–15 h after injection. This sickness episode is characterized by body weight loss, decreased food and water consumption, and reduced locomotion (Henry et al. 2008; O’Connor et al. 2009). Sickness gradually wanes with time and depression-like behavior persists (Dantzer et al. 2008). Depression-like behavior can be measured at 24 h post-LPS by behavioral tests such as the forced swim test, tail suspension test, and sucrose preference test (Frenois et al. 2007; O’Connor et al. 2009). To explore the role of LCN2 in inflammation-induced sickness and depression, we treated WT and Lcn2−/− mice with LPS. Both genotypes showed a similar pattern of weight loss (Fig. 1a), with a significant main effect of treatment, F(1,28) = 6.7, p < 0.05, and a time by treatment interaction, F(5,140) = 63.2, p < 0.001. There was also a main effect of genotype, indicating that lcn2−/− mice had higher body weight in general, as has been previously reported (Guo et al. 2010; Mosialou et al. 2017). Both genotypes returned to their baseline body weight approximately 72 h post-treatment. LPS also altered food consumption patterns in both genotypes (time by treatment interaction, F(1,28) = 103.0, p < 0.001). During the first two nights after treatment (0–12 h and 24–36 h post-LPS), mice showed a reduction in food consumption followed by increased eating between 36 and 72 h post-LPS (Fig. 1b). In line with the body weight data, untreated lcn2−/− mice displayed increased average daily food consumption compared to WT mice (p < 0.05). Another highly sensitivity measure of sickness is voluntary wheel running. As would be expected, LPS induced a significant reduction in nightly wheel running (main effect of treatment, F(1,28) = 21.1, p < 0.001, and a treatment by time interaction, F(4,112) = 44.3, p < 0.001)). This effect remained significant through the third night after treatment (48–60 h post-LPS; Fig. 1c), and there was no significant interaction with genotype. There were no baseline differences in voluntary wheel running activity between the two genotypes.
Lcn2−/− mice display a similar sickness behavior in response to LPS. In response to LPS, both WT and lcn2−/− mice showed a significant loss of body weight (a) and a corresponding reduction in food consumption between 0–12 h and 24–36 h post-LPS (b). They did display a slight compensatory increase in food consumption at 36–48 h. LPS treatment also reduced wheel running for 3 days following treatment equally in both genotypes (c). Dark bars on panel a indicate light/dark cycle. * Post hoc analyses indicate a significant difference between vehicle- and LPS-treated mice, p < 0.05
Lcn2 deficiency did not modify LPS-induced depression-like behavior
To evaluate depression-like behavior, we measured sucrose preference and conducted the tail suspension test at 24 h post-LPS. Sucrose preference was significantly reduced by LPS and returned relatively rapidly (time by treatment interaction, F(2,56) = 10.5, p < 0.001). Post hoc analyses revealed recovery after the first day of treatment in both WT and lcn2−/− mice (Fig. 2a). Immobility in the tail suspension test showed a significant LPS effect (F(1,14) = 24.5, p < 0.001), but no effect of genotype nor genotype by treatment interaction (Fig. 2b).
Lcn2−/− mice display a similar immobility in the tail suspension task in response to LPS. WT and lcn2−/− mice displayed a reduction in sucrose preference during the first 24 h following LPS treatment; however, this deficit did not persist beyond the phase of acute sickness (a). Both genotypes displayed significantly increased immobility time in the TST following LPS (b). * p < 0.05
Lcn2 deficiency did not impact the LPS-induced inflammatory response
When mice were re-injected with a higher dose of LPS and euthanized 6 h later, the predicted LPS-induced systemic and brain inflammatory response was observed with no difference between genotypes. LPS increased serum IL-6 (F(1,11) = 14.9, p < 0.005) (Fig. 3a) and liver mRNA expression of Il-1β (F(1,11) = 6.3, p < 0.05), Tnf-α (F(1,11) = 12.7, p < 0.005), and Itgam (F(1,11) = 6.8, p < 0.05) with a trend for Il-6 (p < 0.10) (Fig. 3b). LPS also increased brain expression of Il-1β (F(1,11) = 17.2, p < 0.005) and Tnf-α (F(1,11) = 23.5, p < 0.005) (Fig. 3c). There were no significant effects of genotype nor genotype by treatment interactions on these inflammatory markers.
Lcn2−/− mice display a similar peripheral and inflammatory response to LPS. Mice were euthanized 6 h after a second dose of vehicle or 1.0 mg/kg LPS and tissue was collected. At this time, both WT and lcn2−/− mice displayed a significant elevation in circulating IL-6 (a), increased Il-1β, Tnf-α, and Itgam in the liver (trend for increase IL-6) (b), and increased Il-1β and Tnf-α in the brain (c). There were no significant differences between the genotypes on any of the inflammatory markers assessed. * p < 0.05
Discussion
The lack of differences between lcn2−/− and wild-type mice in their behavioral and inflammatory response to LPS can be interpreted to indicate that despite its high responsiveness to LPS at the level of brain mRNA expression, lcn2 is dispensable for acute inflammation-induced behavioral changes. This indicates that while brain lcn2 may be an important biomarker of neuroinflammation, it is likely a poor candidate as a therapeutic target for inflammation-induced depression.
The lack of modulatory function of lcn2 in our model was unanticipated based on the high LPS-induced mRNA expression levels and the previous reports of a modulatory function of LCN2 during other LPS challenges. For example, Kang et al. (2018) recently reported that LCN2 serves a protective function in the context of an LPS challenge, as lcn2−/− mice displayed a more severe neuroinflammatory and behavioral response. In the same vein, Zhang et al. (2008) reported that RAW264.7 macrophages treated in vitro with LCN2 displayed a suppression in LPS-induced cytokine production. However, this favorable picture of LCN2 as a negative regulator of inflammation is blurred by other reports showing that LCN2 enhances neuroinflammation and behavioral deficits by polarizing microglia and astrocytes toward a more inflammatory phenotype (Jang et al. 2013a, b).
A noteworthy difference between our approach and that of Kang et al. is the dose of LPS selected. They used a high dose of 2 mg/kg that is likely to be disruptive of blood-brain barrier (BBB) integrity (Zhao et al. 2014). A disruption of the BBB will result a more severe inflammatory response with infiltration of immune cells and inflammatory mediators. The dose of LPS we used has no such effect and produces systemic inflammation that propagates to the brain via other communication pathways (Dantzer et al. 2000). Similarly, it is likely that the in vitro culture system reported by Zhang et al. based on addition of 1 ng/mL of LPS for 4 h to RAW 264.7 macrophages mimics a much more severe inflammatory condition than the relatively low level of inflammation induced in vivo with our dosing regimen. Therefore, a provisional interpretation of the data would be that although we did not observe a significant modulatory function for LCN2 in inflammation-induced sickness or depression, LCN2 could still have a role in more severe inflammatory conditions.
Another notable finding from this study is that lcn2 expression appears to be dispensable to LPS-induced anorexia. By increasing or decreasing the expression of lcn2 specifically in osteoblasts, a tissue with high constitutive expression of this gene, Mosialou and colleagues reported that bone-derived LCN2 suppresses appetite (Mosialou et al. 2017). LCN2 was further shown to cross the blood-brain barrier and activates a melanocortin-4 receptor-dependent anorexigenic pathway. Our baseline data aligns with previous data demonstrating that lcn2 deficiency is associated with increased body weight possibly because of increased food intake, although others have reported no effect of lcn2 deficiency on body weight or appetite (Law et al. 2010). In any case, the observation that lcn2-deficient mice displayed the same reduced food consumption as wild-type mice in response to LPS does not support the hypothesis that LCN2 is a therapeutic target for inflammation-induced anorexia. Several other mediators have been proposed for this effect including activation of neural afferents from the gut at the periphery (Griton and Konsman, Clin Auton Res 2018) and mobilization of neuropeptide Y and pro-opiomelanocortin in the hypothalamus (Dwarkasing et al. 2016).
Considering the primary mechanism by which LCN2 is activated by infectious stimuli may explain why it is exceptionally responsive to this regimen of LPS without having a modulatory role. In response to bacterial infection, toll like receptors (TLRs) on immune, parenchymal, and epithelial cells are activated which induce the synthesis and secretion of LCN2 (Cleaver et al. 2014; Layoun et al. 2012; Ostvik et al. 2013; Sunil et al. 2007). As such, there are reduced levels of LCN2 in mice with nonfunctional TLR4 (Sunil et al. 2007). The primary function of LCN2 appears to be the sequestration of iron, preventing its acquisition by micro-organisms and minimizing bacterial growth. However, LPS activates TLR4 but does not mimic active infection. There is therefore no benefit derived from sequestering iron. In other words, a possible role of LCN2 in modulating the behavioral response to inflammation would have to be investigated in the context of an active infection induced for instance by Salmonella or Escherichia coli rather than in response to pathogen-associated molecular patterns.
In summary, while LCN-2 may be a good inflammatory biomarker, it is not required for the development of inflammation-induced sickness and depression-like behavior. Even if there are likely contexts in which LCN2 modulates inflammation by impacting bacterial growth, it does not appear to be a viable therapeutic target for treating sterile inflammation-induced depression.
References
Biver F, Goldman S, Delvenne V, Luxen A, De Maertelaer V, Hubain P, Mendlewicz J, Lotstra F (1994) Frontal and parietal metabolic disturbances in unipolar depression. Biol Psychiatry 36:381–388
Can A, Dao DT, Terrillion CE, Piantadosi SC, Bhat S, Gould TD (2012) The tail suspension test. J Vis Exp (59):e3769. https://doi.org/10.3791/3769(2012)
Castagne V, Moser P, Roux S, Porsolt RD (2011) Rodent models of depression: forced swim and tail suspension behavioral despair tests in rats and mice. Curr Protoc Neurosci Chapter 8:Unit 8.10A
Cleaver JO, You D, Michaud DR, Guzmán Pruneda FA, Leiva Juarez MM, Zhang J, Weill PM, Adachi R, Gong L, Moghaddam S, Poynter ME, Tuvim MJ, Evans SE (2014) Lung epithelial cells are essential effectors of inducible resistance to pneumonia. Mucosal Immunol 7:78–88. https://doi.org/10.1038/mi.2013.26
Colby CL, Goldberg ME (1999) Space and attention in parietal cortex. Annu Rev Neurosci 22:319–349
Dantzer R, Konsman JP, Bluthe RM, Kelley KW (2000) Neural and humoral pathways of communication from the immune system to the brain: parallel or convergent? Auton Neurosci 85:60–65
Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW (2008) From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci 9:46–56
Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, Lanctot KL (2010) A meta-analysis of cytokines in major depression. Biol Psychiatry 67:446–457
Dunn AJ, Wang J, Ando T (1999) Effects of cytokines on cerebral neurotransmission. Comparison with the effects of stress. Adv Exp Med Biol 461:117–127
Dwarkasing JT, Marks DL, Witkamp RF, van Norren K (2016) Hypothalamic inflammation and food intake regulation during chronic illness. Peptides 77:60–66
Eisenberger NI, Berkman ET, Inagaki TK, Rameson LT, Mashal NM, Irwin MR (2010) Inflammation-induced anhedonia: endotoxin reduces ventral striatum responses to reward. Biol Psychiatry 68:748–754
Frenois F, Moreau M, O’Connor J, Lawson M, Micon C, Lestage J, Kelley KW, Dantzer R, Castanon N (2007) Lipopolysaccharide induces delayed FosB/DeltaFosB immunostaining within the mouse extended amygdala, hippocampus and hypothalamus, that parallel the expression of depressive-like behavior. Psychoneuroendocrinology 32:516–531
Goetz DH, Holmes MA, Borregaard N, Bluhm ME, Raymond KN, Strong RK (2002) The neutrophil lipocalin NGAL is a bacteriostatic agent that interferes with siderophore-mediated iron acquisition. Mol Cell 10:1033–1043
Goldsmith DR, Rapaport MH, Miller BJ (2016) A meta-analysis of blood cytokine network alterations in psychiatric patients: comparisons between schizophrenia, bipolar disorder and depression. Mol Psychiatry 21:1696–1709
Gouweleeuw L, Naude PJ, Rots M, DeJongste MJ, Eisel UL, Schoemaker RG (2015) The role of neutrophil gelatinase associated lipocalin (NGAL) as biological constituent linking depression and cardiovascular disease. Brain Behav Immun 46:23–32
Guo H, Jin D, Zhang Y, Wright W, Bazuine M, Brockman DA, Bernlohr DA, Chen X (2010) Lipocalin-2 deficiency impairs thermogenesis and potentiates diet-induced insulin resistance in mice. Diabetes 59:1376–1385
Haapakoski R, Mathieu J, Ebmeier KP, Alenius H, Kivimaki M (2015) Cumulative meta-analysis of interleukins 6 and 1beta, tumour necrosis factor alpha and C-reactive protein in patients with major depressive disorder. Brain Behav Immun 49:206–215
Henry CJ, Huang Y, Wynne A, Hanke M, Himler J, Bailey MT, Sheridan JF, Godbout JP (2008) Minocycline attenuates lipopolysaccharide (LPS)-induced neuroinflammation, sickness behavior, and anhedonia. J Neuroinflammation 5:15
Jang E, Kim JH, Lee S, Kim JH, Seo JW, Jin M, Lee MG, Jang IS, Lee WH, Suk K (2013a) Phenotypic polarization of activated astrocytes: the critical role of lipocalin-2 in the classical inflammatory activation of astrocytes. J Immunol 1950(191):5204–5219
Jang E, Lee S, Kim JH, Kim JH, Seo JW, Lee WH, Mori K, Nakao K, Suk K (2013b) Secreted protein lipocalin-2 promotes microglial M1 polarization. FASEB J 27:1176–1190
Kaiser RH, Andrews-Hanna JR, Wager TD, Pizzagalli DA (2015) Large-scale network dysfunction in major depressive disorder: a meta-analysis of resting-state functional connectivity. JAMA Psychiat 72:603–611
Kang SS, Ren Y, Liu CC, Kurti A, Baker KE, Bu G, Asmann Y, Fryer JD (2018) Lipocalin-2 protects the brain during inflammatory conditions. Mol Psychiatry 23:344–350
Kappelmann N, Lewis G, Dantzer R, Jones PB, Khandaker GM (2018) Antidepressant activity of anti-cytokine treatment: a systematic review and meta-analysis of clinical trials of chronic inflammatory conditions. Mol Psychiatry 23:335–343
Law IK, Xu A, Lam KS, Berger T, Mak TW, Vanhoutte PM, Liu JT, Sweeney G, Zhou M, Yang B, Wang Y (2010) Lipocalin-2 deficiency attenuates insulin resistance associated with aging and obesity. Diabetes 59:872–882
Layoun A, Huang H, Calve A, Santos MM (2012) Toll-like receptor signal adaptor protein MyD88 is required for sustained endotoxin-induced acute hypoferremic response in mice. Am J Pathol 180:2340–2350
Leighton SP, Nerurkar L, Krishnadas R, Johnman C, Graham GJ, Cavanagh J (2018) Chemokines in depression in health and in inflammatory illness: a systematic review and meta-analysis. Mol Psychiatry 23:48–58
Marijnissen RM, Naude PJ, Comijs HC, Schoevers RA, Oude Voshaar RC (2014) Waist circumference and neutrophil gelatinase-associated lipocalin in late-life depression. Brain Behav Immun 37:231–239
Miller AH, Haroon E, Raison CL, Felger JC (2013) Cytokine targets in the brain: impact on neurotransmitters and neurocircuits. Depress Anxiety 30:297–306
Mohan H, de Haan R, Mansvelder HD, de Kock CPJ (2018) The posterior parietal cortex as integrative hub for whisker sensorimotor information. Neuroscience 368:240–245
Mommersteeg PMC, Schoemaker RG, Naude PJW, Eisel ULM, Garrelds IM, Schalkwijk CG, Westerhuis B, Kop WJ, Denollet J (2016) Depression and markers of inflammation as predictors of all-cause mortality in heart failure. Brain Behav Immun 57:144–150
Moreau M, Lestage J, Verrier D, Mormede C, Kelley KW, Dantzer R, Castanon N (2005) Bacille Calmette-Guerin inoculation induces chronic activation of peripheral and brain indoleamine 2,3-dioxygenase in mice. J Infect Dis 192:537–544
Moreau M, Andre C, O’Connor JC, Dumich SA, Woods JA, Kelley KW, Dantzer R, Lestage J, Castanon N (2008) Inoculation of Bacillus Calmette-Guerin to mice induces an acute episode of sickness behavior followed by chronic depressive-like behavior. Brain Behav Immun 22:1087–1095
Mosialou I, Shikhel S, Liu JM, Maurizi A, Luo N, He Z, Huang Y, Zong H, Friedman RA, Barasch J, Lanzano P, Deng L, Leibel RL, Rubin M, Nickolas T, Chung W, Zeltser LM, Williams KW, Pessin JE, Kousteni S (2017) MC4R-dependent suppression of appetite by bone-derived lipocalin 2. Nature 543:385–390
Naude PJ, Nyakas C, Eiden LE, Ait-Ali D, van der Heide R, Engelborghs S, Luiten PG, De Deyn PP, den Boer JA, Eisel UL (2012) Lipocalin 2: novel component of proinflammatory signaling in Alzheimer’s disease. FASEB J 26:2811–2823
Naude PJ, Mommersteeg PM, Zijlstra WP, Gouweleeuw L, Kupper N, Eisel UL, Kop WJ, Schoemaker RG (2014) Neutrophil gelatinase-associated lipocalin and depression in patients with chronic heart failure. Brain Behav Immun 38:59–65
Naude PJ, Mommersteeg PM, Gouweleeuw L, Eisel UL, Denollet J, Westerhuis LW, Schoemaker RG (2015) NGAL and other markers of inflammation as competitive or complementary markers for depressive symptom dimensions in heart failure. World J Biol Psychiatry 16:536–541
O’Connor JC, Lawson MA, Andre C, Moreau M, Lestage J, Castanon N, Kelley KW, Dantzer R (2009) Lipopolysaccharide-induced depressive-like behavior is mediated by indoleamine 2,3-dioxygenase activation in mice. Mol Psychiatry 14:511–522
Ostvik AE, Granlund AV, Torp SH, Flatberg A, Beisvag V, Waldum HL, Flo TH, Espevik T, Damas JK, Sandvik AK (2013) Expression of Toll-like receptor-3 is enhanced in active inflammatory bowel disease and mediates the excessive release of lipocalin 2. Clin Exp Immunol 173:502–511
Palmiter RD (2017) Physiology: bone-derived hormone suppresses appetite. Nature 543:320–322
Raison CL, Rutherford RE, Woolwine BJ, Shuo C, Schettler P, Drake DF, Haroon E, Miller AH (2013) A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression: the role of baseline inflammatory biomarkers. JAMA Psychiatry 70:31–41
Reichenberg A, Yirmiya R, Schuld A, Kraus T, Haack M, Morag A, Pollmacher T (2001) Cytokine-associated emotional and cognitive disturbances in humans. Arch Gen Psychiatry 58:445–452
Schaefer M, Schwaiger M, Pich M, Lieb K, Heinz A (2003) Neurotransmitter changes by interferon-alpha and therapeutic implications. Pharmacopsychiatry 36(Suppl 3):S203–S206
Smith KJ, Au B, Ollis L, Schmitz N (2018) The association between C-reactive protein, Interleukin-6 and depression among older adults in the community: a systematic review and meta-analysis. Exp Gerontol 102:109–132
Sunil VR, Patel KJ, Nilsen-Hamilton M, Heck DE, Laskin JD, Laskin DL (2007) Acute endotoxemia is associated with upregulation of lipocalin 24p3/Lcn2 in lung and liver. Exp Mol Pathol 83:177–187
Teixeira S, Machado S, Velasques B, Sanfim A, Minc D, Peressutti C, Bittencourt J, Budde H, Cagy M, Anghinah R, Basile LF, Piedade R, Ribeiro P, Diniz C, Cartier C, Gongora M, Silva F, Manaia F, Silva JG (2014) Integrative parietal cortex processes: neurological and psychiatric aspects. J Neurol Sci 338:12–22
Valkanova V, Ebmeier KP, Allan CL (2013) CRP, IL-6 and depression: a systematic review and meta-analysis of longitudinal studies. J Affect Disord 150:736–744
Vasic N, Walter H, Sambataro F, Wolf RC (2009) Aberrant functional connectivity of dorsolateral prefrontal and cingulate networks in patients with major depression during working memory processing. Psychol Med 39:977–987
Zhang J, Wu Y, Zhang Y, Leroith D, Bernlohr DA, Chen X (2008) The role of lipocalin 2 in the regulation of inflammation in adipocytes and macrophages. Mol Endocrinol 22:1416–1426
Zhao P, Elks CM, Stephens JM (2014) The induction of lipocalin-2 protein expression in vivo and in vitro. J Biol Chem 289:5960–5969
Funding
This research was supported by the National Institutes of Health (R01 CA193522 and R21 MH104694 to R.D., R01 NS073939 to A.K., R.D., and C.J.H., and an MD Anderson Cancer Center Support Grant (P30 CA016672)).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All protocols were approved by the University of Texas MD Anderson Cancer Center Institutional Animal Care and Use Committee.
Conflict of interest
Robert Dantzer has received honoraria from Danone Nutricia Research and Pfizer that are unrelated to the present study. All remaining authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article belongs to a Special Issue on Neuroimmune Signaling in Psychiatric Disease
Rights and permissions
About this article
Cite this article
Vichaya, E.G., Gross, P.S., Estrada, D.J. et al. Lipocalin-2 is dispensable in inflammation-induced sickness and depression-like behavior. Psychopharmacology 236, 2975–2982 (2019). https://doi.org/10.1007/s00213-019-05190-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-019-05190-7