Abstract
Background
Despite evidence supporting the benefits of cannabinoids for symptom control across a wide range of medical conditions, concerns have been raised regarding the potential misuse and/or problematic use of cannabinoids (CBs).
Objective
The first objective of this study was to examine the incidence of problematic prescription cannabinoid use (PPCBU) over a 12-month period among patients initiating cannabinoid therapy. The second objective was to examine the factors associated with PPCBU. A total of 265 patients who were prescribed oral cannabinoid therapy as part of usual medical practice were enrolled into this prospective observational study. Patients first completed a series of baseline questionnaires assessing demographic, clinical, and substance use variables. Three measures designed to assess PPCBU were then administered at 3, 6, and 12 months after initiation of cannabinoid therapy.
Results
At each of the follow-up assessment time points, a significantly greater number of patients scored below (vs above) cutoff scores on the three main PPCBU outcomes (all p’s < .001). At any follow-up time point, a maximum of roughly 25% of patients demonstrated PPCBU. Heightened odds of PPCBU were observed among patients with a history of psychiatric problems, tobacco smokers, and recreational cannabis users (all p’s < .05). Results indicated that past-year substance abuse, assessed using the DAST-20, was the strongest predictor of PPCBU (p < .005).
Conclusion
Findings from the present study could have implications for clinicians considering the use of cannabinoids for the management of patients with medical conditions. Although results indicated that the majority of patients included in this study did not reach cutoff scores on the three main PPCBU outcomes, our findings suggest that PPCBU should be routinely assessed and monitored over the course of cannabinoid therapy, particularly among patients with a history of psychiatric or substance use problems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cannabinoids (CBs) are natural or synthetic drugs that bind to cannabinoid receptors or demonstrate endogenous cannabinoid system activity (Aggarwal 2013). Randomized, controlled trials of natural and synthetic CBs are showing efficacy for symptom control across a wide range of conditions, including chronic pain (Narang et al. 2008; Toth et al. 2012; Ware et al. 2010), cancer (Johnson et al. 2010; Portenoy et al. 2012), human immunodeficiency virus (Abrams et al. 2007; Haney et al. 2005, 2007), and multiple sclerosis (Collin et al. 2010; Notcutt et al. 2012). Consequently, an increasing number of physicians are considering the therapeutic use of cannabinoids for symptom control among patients with these conditions (Carliner et al. 2017; Compton et al. 2017; Corroon et al. 2017; Hasin et al. 2016).
Despite the potential benefits of cannabinoids for symptom control across a wide range of medical conditions, concerns have been raised regarding the potential misuse and/or problematic use of prescription cannabinoids (Kahan and Srivastava 2007; Kalant 2004; Savage et al. 2016). In research and clinical settings, the term “problematic prescription drug use” has been commonly used to describe any problematic drug-related behaviors that arise over the course of therapy (Savage 2008; Smith and Passik 2008). Although problematic prescription drug use may simply take the form of transient “aberrant” drug use behaviors (e.g., hoarding or losing prescription drugs), it may also reflect more serious problems such as prescription drug misuse, addiction, or diversion (Savage 2008; Smith and Passik 2008).
While considerable research has been conducted among recreational cannabis users (Compton et al. 2004; Kalant 2004), research on problematic prescription cannabinoid use (PPCBU) among medical users has considerably lagged behind. To date, the bulk of studies that have been conducted among medical users have focused on potential adverse side effects of herbal cannabis or other prescription cannabinoids, with non-serious side effects such as dizziness, somnolence, and dry mouth being among the most commonly reported (Savage et al. 2016; Ware et al. 2015). A handful of studies have specifically examined the incidence of problematic cannabinoid use (e.g., cannabinoid overuse), but these studies were either short-term (≤ 12 weeks) randomized controlled trials (Collin et al. 2010) or trials in which “high-risk” patients (e.g., those with psychiatric issues or past history of substance use problems) were excluded (Wade et al. 2004; Wade et al. 2006). Longer-term prospective studies conducted with more representative populations of patients are needed to further explore the incidence of problematic prescription cannabinoid use.
Additional research is also needed to further explore the factors that may contribute to problematic prescription cannabinoid use. For instance, in previous studies conducted among patients using other types of prescription drugs, heightened rates of prescription drug misuse have been observed among younger males (Michna et al. 2004; Wasan et al. 2007) as well as among patients with a history of substance use problems (Boscarino et al. 2010; Nielsen et al. 2015; Saunders et al. 2012). Heightened rates of prescription drug misuse have also consistently been observed among patients experiencing high levels of psychological distress such as anxiety (Schieffer et al. 2005; Wasan et al. 2007) or depression (Grattan et al. 2012; Martel et al. 2014). Research has yet to systematically investigate whether these factors also contribute to the problematic use of cannabinoids among patients who are prescribed cannabinoid therapy.
The first objective of this prospective observational study was to examine the incidence of problematic prescription cannabinoid use (PPCBU) over a 12-month period among patients initiating oral cannabinoid therapy. The second objective was to examine the factors associated with PPCBU.
Methods
Study design and participants
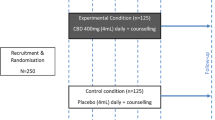
A total of 265 patients who were prescribed CBs as part of usual medical practice were enrolled from 12 Canadian outpatient clinics from July 2009 to July 2011 into a prospective, non-interventional, observational, multicenter study. Eligible participants were males or females aged ≥ 18 years, initiating cannabinoid therapy (i.e., having started cannabinoid therapy within the previous 14 days), and prescribed any CB medication during the course of normal clinical practice at a pain, MS, HIV, physical rehabilitation, or other clinic (see Supplementary Table 6). Participants excluded were those who had previously been prescribed CBs, and those with a medical condition or reason that could interfere with study participation or protocol adherence. Substance abuse history alone was not grounds for exclusion.
Procedures and measures
Patients underwent baseline assessment (see Baseline assessment visit) in one of the outpatient clinics and were then followed over a 12-month period during the course of usual care. Each of the clinics had sole discretion for patient assignment to cannabinoid therapy and the subsequent management of patients throughout the study period. In-clinic follow-up assessments were conducted at 3, 6, and 12 months after initiation of cannabinoid therapy (see Follow-up assessment visits). In this study, all data collection procedures were based on a standardized protocol, and one visit at each study (i.e., clinic) site was conducted over the course of the study to monitor data collection and to ensure the quality of study data.
Baseline assessment visit
At baseline, patients were asked to complete a questionnaire assessing demographic and clinical variables. Demographic variables included age, sex, race, marital status, income, and education. Clinical variables included patients’ histories of medical and psychiatric problems. Patients’ histories of medical and psychiatric problems were assessed based on self-reports. Patients’ reports of medical and psychiatric histories involved any “past” or “current” problems. During the baseline visit, patients were also asked to report on their daily use of alcohol, tobacco, and herbal cannabis, and to complete the Drug Abuse Screening Test (DAST-20; (Skinner 1982)), a self-report questionnaire designed to assess past-year substance abuse problems involving illicit drugs. The DAST was chosen given that it is a well-accepted screening tool that can be easily and rapidly administered in clinic settings in order to screen for past-year substance use problems.
Follow-up assessment visits
At each of the follow-up visits (i.e., 3, 6, and 12 months), three measures designed to assess problematic prescription cannabinoid use were administered. All these measures were originally developed and worded for use in patient populations prescribed opioids, but these measures were adapted for the purposes of the present study by changing the opioid-specific wording to a cannabinoid-specific wording. As can be seen in Supplementary Tables 1, 2, and 3, all scales remained identical to the original versions that were developed and validated, with the exception of the opioid wording. Modified versions of the following measures were administered to patients at baseline:
The Current Opioid Misuse Measure
(COMM; (Butler et al. 2007)), a 17-item self-report questionnaire designed to identify patients exhibiting aberrant and/or problematic medication-related behaviors. COMM items are scored on a 5-point scale (0 = never, 4 = very often) and are designed to assess a variety of behaviors that are indicative of problematic use (e.g., How often have you taken more medication than prescribed? How often have you taken your medications differently from how they were prescribed?). A cutoff score of ≥ 9 on the COMM is considered indicative of problematic medication use (Butler et al. 2007, 2010).
The Addiction Behavior Checklist
(ABC; (Wu et al. 2006)), a 20-item clinician-administered instrument designed to assess problematic medication use. ABC items are rated as “yes” or “no” and focus on observable behaviors exhibited by patients either during or between clinic visits (e.g., Patient ran out of medications early; Patient appears sedated or confused). A score of ≥ 3 on the ABC is considered indicative of problematic medication use (Wu et al. 2006).
The Chabal Prescription Opioid Abuse Checklist
(CPAC; (Chabal et al. 1997)), a 5-item clinician-administered instrument designed to assess problematic medication use. CPAC items are rated as “yes” or “no” and evaluate behaviors such as early refills, dose escalations, and aberrant behaviors such as phone calls or clinic visits to request more medications. A score of ≥ 3 on the CPAC is considered indicative of problematic medication use (Chabal et al. 1997).
During each of the follow-up assessment visits, measures designed to evaluate the severity of patients’ medical condition as well as cannabinoid therapy efficacy were also administered. These measures, which were developed and validated to be used with patients with any type of medical condition, included the following:
The Clinical Global Impression
(CGI; (Guy 1976)), a standardized instrument designed to be used by clinicians in order to assess the severity of patients’ medical condition (CGI-severity range 1 = normal; 7 = extremely ill). Items on the CGI are also designed to assess clinicians’ judgments of treatment efficacy (CGI-efficacy). The CGI is one of the most commonly used measures in pharmacological treatment studies and has been used among patients with a wide range of medical conditions (Spearing et al. 1997).
The Patient Global Impression of Change
(PGIC; (Hurst and Bolton 2004)), a single-item self-report measure designed to assess patients’ perceptions of changes in condition severity as a result of treatment. The PGIC is rated on a 7-point scale ranging from very much worse to very much improved.
Data reduction and analysis
In order to examine the incidence of problematic prescription cannabinoid use (PPCBU), we first conducted frequency analyses to determine the number of patients reaching cutoff scores on the three main PPCBU outcomes (i.e., COMM, ABC, CPAC), separately for the 3-, 6-, and 12-month follow-up assessment visits. Frequency distributions for each of the PPCBU outcomes were tabulated as counts and percentages.
In order to examine the factors associated with PPCBU, a series of univariate analyses were first conducted to examine the influence of patient demographics, medication use, psychological/psychiatric characteristics, and substance use history on PPCBU. Analyses were also conducted to examine the influence of patients’ condition severity and cannabinoid therapy efficacy on PPBCU. For these analyses, scores on measures of condition severity (PGIC, CGI-severity) and cannabinoid therapy efficacy (CGI-efficacy) were aggregated across follow-up visits. In order to minimize the number of analyses being conducted and the likelihood of family-wise (i.e., type-1) errors, data from each PPCBU outcome (i.e., COMM, ABC, CPAC) were pooled across study visits and used as outcome variables. Outcome variables were coded as “1” if patients scored above the PPCBU cutoff during at least one of the follow-up visits, and coded as “0” if patients scored below the cutoff across all the follow-up visits.
Results
Descriptive statistics
Descriptive statistics on patient demographics are presented in Table 1. Of the 265 enrolled participants, 69.7% were female, 87.9% were Caucasian, and the mean age was 49.2 years (SD = 11.9). As can be seen from Supplementary Table 4, early termination was most frequently due to adverse events (AEs) (n = 76; 49.4%), discontinuation of cannabinoid therapy (n = 51; 33.1%), and loss to follow-up (n = 15; 9.7%). The AEs that were reported by patients over the course of the study are listed in Supplementary Table 5. Cannabinoid therapy discontinuation primarily resulted from lack of efficacy and/or financial considerations. Study completion was not significantly associated with participant age, gender, race, marital status, education, income, or clinical characteristics (all p’s > .05).
The most frequent reasons for which cannabinoids were prescribed included pain (93.6%), sleep (18.5%), and spasticity (6%). Other reasons (2.6%) included anxiety and nausea. The specific types of cannabinoid medications that were used by study participants included nabilone (89.7%) and Sativex (9.2%). A small percentage (1.1%) of patients used Sativex in addition to nabilone.
Incidence of problematic prescription cannabinoid use
As can be seen from Table 2, frequency analyses were conducted to determine the number of patients reaching cutoff scores on the three main PPCBU outcomes (i.e., COMM, ABC, CPAC), separately for the 3-, 6-, and 12-month follow-up assessment visits. At each of the follow-up visits, results from chi-square analyses indicated that a significantly greater proportion of participants scored below the cutoff threshold (vs cutoff or higher) on all PPCBU measures (i.e., COMM, ABC, CPAC) (all p’s < .001). Across all visits, an average of 26.5% of participants reached the COMM cutoff for PPCBU (visits 2, 3, and 4; 28.4, 22.1, and 28.9%, respectively), while an average of 9.4% reached the ABC cutoff (visits 2, 3, and 4; 9.2, 12.3, and 6.8%, respectively). None of the participants met the CPAC cutoff threshold across all follow-up visits.
Subsequent analyses were conducted to examine, for each follow-up visit, the number of “new” patients reaching cutoff scores on PPCBU outcomes. These analyses were done separately for measures of PPCBU derived from the ABC and COMM. Analyses were not conducted based on the CPAC given that none of the participants reached the CPAC cutoff for any of the follow-up visits. Results indicated that 13.3% of patients who scored below the COMM cutoff at the first follow-up (i.e., 3-month) visit reached the COMM cutoff for PPCBU at the 6-month visit. Results also indicated that 15.8% of patients who scored below the COMM cutoff at the second follow-up (i.e., 6-month) visit reached the COMM cutoff for PPCBU at the 12-month visit. For the ABC, results indicated that 4% of patients who scored below the ABC cutoff at the first follow-up (i.e., 3-month) visit reached the ABC cutoff for PPCBU at the 6-month visit. Results also indicated that 1.9% of patients who scored below the ABC cutoff at the second follow-up (i.e., 6-month) visit reached the ABC cutoff for PPCBU at the 12-month visit.
Influence of patients’ demographic and psychological characteristics on PPCBU
Analyses were conducted to examine the influence of patients’ demographic and clinical characteristics on PPCBU. Results indicated that none of the demographic variables or were significantly associated with the COMM or ABC cutoff (all p’s > .05). The use of other prescription drugs in addition to cannabinoids (i.e., opioids, antidepressants, anticonvulsants, or anxiolytics/sedatives) was also not significantly associated with the COMM or ABC cutoff (all p’s > .05). Psychiatric history, however, was significantly associated with PPCBU, as a greater proportion of participants with a psychiatric history reached cutoffs on the COMM (p < .001) and ABC (p < .05) compared to participants without a psychiatric history (see Table 3). In the present study, the most frequent psychiatric problems were depression (51.2%), anxiety (23.8%), and insomnia (11.6%). Post hoc examination of data indicated that the likelihood of reaching cutoff scores on the COMM and ABC was greater among patients with depression than those with other type of psychiatric problems, but these effects did not reach significance (both p’s > .05).
Influence of substance use on PPCBU
Analyses were conducted to examine whether daily use of alcohol, tobacco, or herbal cannabis, assessed at baseline, was associated with PPCBU. Daily alcohol use was not significantly associated with PPCBU. Results, however, indicated that tobacco use was significantly associated with PPCBU (p < .05), as daily tobacco smokers were more likely to reach the ABC cutoff than non-smokers. A significant association between daily herbal cannabis use and PPCBU was also found (p < .05), as recreational herbal cannabis users were more likely to reach the ABC cutoff than non-users (see Table 4). Results also indicated that higher DAST-20 scores were associated with a greater likelihood of reaching the ABC cutoff (point-biserial r = .29, p < .001). In the present sample, 3% of patients had scores on the DAST-20 suggestive of a past-year substance use disorder based on the DAST scoring criteria. A subsequent direct logistic regression analysis indicated that the DAST-20 was the strongest predictor of PPCBU (p < .05). None of the substance use variables were associated with the COMM cutoff (all p’s > .05).
Influence of condition severity and cannabinoid therapy efficacy on PPCBU
Analyses were conducted to examine the influence of patients’ condition severity and cannabinoid therapy efficacy on PPBCU. Results indicated that patients’ reports of condition severity on the PGIC were neither associated with the COMM nor the ABC (both p’s > .05). Clinicians’ ratings of condition severity (CGI-severity) and cannabinoid therapy efficacy (CGI-efficacy) were also not significantly associated with the COMM or ABC (both p’s > .05).
Discussion
The present study examined the incidence of problematic prescription cannabinoid use (PPCBU) over a 12-month period among patients initiating cannabinoid therapy. Overall, results indicated that the majority of patients included in this study did not reach cutoff scores on the three main PPCBU outcomes (i.e., COMM, ABC, CPAC) at the 3-, 6-, and 12-month follow-up assessment visits. Across all the study visits, an average of roughly 25% of participants reached the COMM cutoff, and an average of 9.4% reached the ABC cutoff. None of the patients demonstrated problematic behaviors on the CPAC. On the COMM and ABC, results indicated that the majority of PPCBU behaviors occurred within the first 3 months after initiation of cannabinoid therapy. Incidences of PPCBU behaviors, however, were also observed later over the course of therapy.
Although some of the patients included in the present study may have exhibited behaviors indicative of clinically significant problems associated with cannabinoid use, it is worth noting that PPCBU behaviors are not necessarily indicative of a cannabis use disorder. In recent nationally representative studies examining prevalence rates of cannabis use disorders among adults (Hasin et al. 2015, 2016), the lifetime and 12-month prevalence rates were found to be roughly 6% and 2.5%, respectively. These prevalence estimates were derived based on the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) and DSM-5 criteria for cannabis use disorder. In our study, the incidence of cannabis use disorders was not assessed. However, it is not surprising to find that rates of PPBCU in our study were higher than rates of cannabis use disorders observed among recreational cannabis users. The COMM and ABC, two of the instruments used in our study to assess PPCBU, include items designed to assess “aberrant” drug use behaviors such as having “discussions focused on medication,” “expressing worries” about how medications are being handled, and having trouble “thinking clearly.” Although some of these behaviors and symptoms may require clinical attention, they are arguably less severe than those characterizing patients with a cannabis use disorder. Additional studies will be needed to assess rates of cannabis use disorders among patients prescribed cannabinoid therapy.
In addition to examining the incidence of problematic prescription cannabinoid use, the present study also examined the factors associated with PPBCU. We found that patients with a history of psychiatric problems, particularly depression, were more likely to exhibit problematic prescription cannabinoid use. This finding is consistent with previous studies that have found heightened rates of prescription drug misuse among patients with psychiatric problems who are prescribed opioids (Boscarino et al. 2010; Edlund et al. 2013; Grattan et al. 2012) or sedatives (Kouyanou et al. 1997; Liebschutz et al. 2010). It has been suggested that these patients might engage in problematic medication use behaviors (e.g., medication overuse) as a way to cope with psychological distress and/or to alleviate (i.e., self-medicate) distressing symptoms (Kirsh et al. 2007; Passik and Lowery 2011). There is also evidence indicating that patients with histories of psychiatric problems tend to self-medicate using cannabis (Corroon et al. 2017; Hasin 2017; Osborn et al. 2015).
Analyses were also conducted to examine the influence of patients substance use history on PPCBU. We found that daily tobacco smokers were more likely to exhibit PPCBU than non-smokers, and a similar pattern of findings was observed for herbal cannabis users. A subsequent regression analysis, however, revealed that past-year substance abuse, assessed using the DAST-20, was the strongest predictor of PPCBU. In previous studies conducted among patients prescribed other types of prescription drugs, heightened rates of prescription drug misuse have been observed among patients with a history of substance use and/or addiction (Edlund et al. 2007; Ives et al. 2006; Michna et al. 2004), similar to what was found here. In our study, it is worth noting that the association between substance use history and PPCBU was not observed based on COMM scores, but only based on the ABC, a clinician-based measure of problematic medication use.
In the present study, we found that the severity of patients’ condition, either reported by the patients or evaluated by clinicians, was not associated with PPCBU. The efficacy of cannabinoid therapy, assessed at multiple times across the 12-month period, was also unrelated to PPBCU. Interestingly, this set of findings parallels results from studies among pain patients that failed to find an association between patients’ reports of clinical pain severity and problematic opioid use behaviors (Garland et al. 2016; Martel et al. 2014, 2016). It has been argued that some patients, in an attempt to seek symptom relief, may exhibit aberrant and/or problematic medication use behaviors, a phenomenon known as pseudo-addiction (Ballantyne and LaForge 2007; Jamison et al. 2011). Findings from the present study, however, suggest that pseudo-addiction is not likely to have contributed to problematic cannabinoid use given that patients’ condition severity and measures of cannabinoid therapy efficacy were unrelated to PPBCU.
Findings from the present study could have implications for clinicians considering the use of cannabinoids for the management of patients with medical conditions. As noted earlier, rates of problematic cannabinoid use behaviors appear to be relatively low, but our findings nevertheless suggest that PPCBU should be routinely assessed and monitored over the course of cannabinoid therapy. Our findings suggest that monitoring PPCBU among patients with histories of psychiatric and substance use problems might be particularly important. Given that these patients appear to be at heightened risk of PPCBU, the use of a patient risk assessment and stratification approach in CB prescribing should be considered, similar to the current recommended approach for the use of long-term opioid therapy among patients with chronic pain (Chou et al. 2009; Furlan et al. 2010). Opioid-specific tools have been developed and validated for monitoring opioid users (e.g., COMM, ABC), and our findings suggest that these tools could also have some clinical utility for monitoring patients prescribed cannabinoid therapy.
There are limitations to the present study that must be considered when interpreting our findings. First, given that the study sample was restricted to patients prescribed oral cannabinoids, our findings on problematic cannabinoid use cannot be generalized to medical users of inhaled cannabis. Second, our measures of PPCBU were originally developed, validated, and worded for use among patients prescribed opioid analgesics. They were adapted for the purposes of the present study by changing opioid-specific wording to a cannabinoid-specific wording, but none of these measures has been validated in patient populations prescribed cannabinoids. Although tools used in the present study arguably possess high face and content validity by being virtually identical to previously validated opioid tools, further efforts will be needed to support the psychometric properties of the CB-specific tools used in our study. As noted earlier, additional studies relying on structured interviews will also be needed to assess rates of cannabis use disorders among patients prescribed cannabinoid therapy. Finally, as in most longitudinal studies, the possibility that drop-out rates might have influenced study findings must be considered. However, patients lost to follow-up did not differ significantly from patients who completed the study in terms of demographic variables, clinical characteristics, or PPCBU behaviors. This should attenuate potential concerns regarding the influence of attrition bias on the present findings.
In spite of these limitations, findings from the present study provide valuable new insights into the incidence of problematic cannabinoid use among patients prescribed cannabinoid therapy. With previous clinical trials primarily comprised of short-term studies of CB efficacy, issues related to problematic cannabinoid use had not been fully addressed in the literature and contributed to physician reluctance in prescribing CBs (Kahan and Srivastava 2007; Kalant 2004). While a few studies have examined PPCBU associated with smoked or vaporized cannabinoids (Collin et al. 2007, 2010), this is, to our knowledge, the first study to systematically examine PPCBU among patients prescribed oral cannabinoids. Numerous confounding factors prohibit generalization of findings across cannabinoid medications, including THC content, quantity, and pharmacokinetic profiles associated with different routes of administration. Unlike oral administration of CBs containing Δ9-tetrahydrocannabinol (THC) or its analogs, inhaled (e.g., smoked or vaporized) marijuana involves a substantially more rapid pulmonary absorption, plasma distribution, CNS penetration, and mesolimbic cannabinoid receptor binding and activation of THC at CB receptors. Inhalation produces the most rapid onset of therapeutic effects, and the most rapid surge in mesolimbic dopamine release and onset of psychoactivity, a rewarding and reinforcing effect that may, over time, contribute to repeated problematic cannabinoid use or addiction. Theoretically, rates of problematic cannabinoid use associated with orally administered prescribed CBs are thus expected to be lower than those associated with inhaled prescribed marijuana.
In addition to its novelty and clinical relevance, one of the key strengths of this study was to systematically examine the incidence and correlates of PPCBU using a prospective longitudinal study design. Other strengths include multicenter enrolment, the combination of self-report and clinician-based measures of PPCBU, and the inclusion of patients with a past history of substance abuse. Additional studies will be needed to compare rates of PPBCU among patients prescribed different types of cannabinoids. Further efforts are also needed to develop and/or refine risk screening and monitoring tools that could be used among patients prescribed cannabinoids. Advances in this domain would have direct implications for clinicians involved in the management of patients using cannabinoids and might ultimately contribute to preventing problematic prescription cannabinoid use.
References
Abrams DI, Jay CA, Shade SB, Vizoso H, Reda H, Press S, Kelly ME, Rowbotham MC, Petersen KL (2007) Cannabis in painful HIV-associated sensory neuropathy: a randomized placebo-controlled trial. Neurology 68(7):515–521. https://doi.org/10.1212/01.wnl.0000253187.66183.9c
Aggarwal SK (2013) Cannabinergic pain medicine: a concise clinical primer and survey of randomized-controlled trial results. Clin J Pain 29(2):162–171. https://doi.org/10.1097/AJP.0b013e31824c5e4c
Ballantyne JC, LaForge KS (2007) Opioid dependence and addiction during opioid treatment of chronic pain. Pain 129(3):235–255. https://doi.org/10.1016/j.pain.2007.03.028
Boscarino JA, Rukstalis M, Hoffman SN, Han JJ, Erlich PM, Gerhard GS, Stewart WF (2010) Risk factors for drug dependence among out-patients on opioid therapy in a large US health-care system. Addiction 105(10):1776–1782. https://doi.org/10.1111/j.1360-0443.2010.03052.x
Butler SF, Budman SH, Fernandez KC, Houle B, Benoit C, Katz N, Jamison RN (2007) Development and validation of the Current Opioid Misuse Measure. Pain 130(1):144–156. https://doi.org/10.1016/j.pain.2007.01.014
Butler SF, Budman SH, Fanciullo GJ, Jamison RN (2010) Cross validation of the current opioid misuse measure to monitor chronic pain patients on opioid therapy. Clin J Pain 26(9):770–776. https://doi.org/10.1097/AJP.0b013e3181f195ba
Carliner H, Brown QL, Sarvet AL, Hasin DS (2017) Cannabis use, attitudes, and legal status in the U.S.: a review. Prev Med. https://doi.org/10.1016/j.ypmed.2017.07.008
Chabal C, Erjavec MK, Jacobson L, Mariano A, Chaney E (1997) Prescription opiate abuse in chronic pain patients: clinical criteria, incidence, and predictors. Clin J Pain 13(2):150–155. https://doi.org/10.1097/00002508-199706000-00009
Chou R, Fanciullo GJ, Fine PG, Adler JA, Ballantyne JC, Davies P, Donovan MI, Fishbain DA, Foley KM, Fudin J, Gilson AM, Kelter A, Mauskop A, O'Connor PG, Passik SD, Pasternak GW, Portenoy RK, Rich BA, Roberts RG, Todd KH, Miaskowski C (2009) Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain 10(2):113–130. https://doi.org/10.1016/j.jpain.2008.10.008
Collin C, Davies P, Mutiboko IK, Ratcliffe S (2007) Randomized controlled trial of cannabis-based medicine in spasticity caused by multiple sclerosis. Eur J Neurol 14(3):290–296. https://doi.org/10.1111/j.1468-1331.2006.01639.x
Collin C, Ehler E, Waberzinek G, Alsindi Z, Davies P, Powell K, Notcutt W, O’Leary C, Ratcliffe S, Novakova I, Zapletalova O, Pikova J, Ambler Z (2010) A double-blind, randomized, placebo-controlled, parallel-group study of Sativex, in subjects with symptoms of spasticity due to multiple sclerosis. Neurol Res 32(5):451–459. https://doi.org/10.1179/016164109X12590518685660
Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS (2004) Prevalence of marijuana use disorders in the United States: 1991–1992 and 2001–2002. JAMA 291(17):2114–2121. https://doi.org/10.1001/jama.291.17.2114
Compton WM, Han B, Hughes A, Jones CM, Blanco C (2017) Use of marijuana for medical purposes among adults in the United States. JAMA 317(2):209–211. https://doi.org/10.1001/jama.2016.18900
Corroon JM Jr, Mischley LK, Sexton M (2017) Cannabis as a substitute for prescription drugs—a cross-sectional study. J Pain Res 10:989–998. https://doi.org/10.2147/JPR.S134330
Edlund MJ, Steffick D, Hudson T, Harris KM, Sullivan M (2007) Risk factors for clinically recognized opioid abuse and dependence among veterans using opioids for chronic non-cancer pain. Pain 129(3):355–362. https://doi.org/10.1016/j.pain.2007.02.014
Edlund MJ, Sullivan MD, Han X, Booth BM (2013) Days with pain and substance use disorders: is there an association? Clin J Pain 29(8):689–695. https://doi.org/10.1097/AJP.0b013e318270fa77
Furlan AD, Reardon R, Weppler C (2010) Opioids for chronic noncancer pain: a new Canadian practice guideline. CMAJ 182(9):923–930. https://doi.org/10.1503/cmaj.100187
Garland EL, Brown SM, Howard MO (2016) Thought suppression as a mediator of the association between depressed mood and prescription opioid craving among chronic pain patients. J Behav Med 39(1):128–138. https://doi.org/10.1007/s10865-015-9675-9
Grattan A, Sullivan MD, Saunders KW, Campbell CI, Von Korff MR (2012) Depression and prescription opioid misuse among chronic opioid therapy recipients with no history of substance abuse. Ann Fam Med 10(4):304–311. https://doi.org/10.1370/afm.1371
Guy W (1976) Assessment manual for psychopharmacology—revised. Department of Health, Education, and Welfare Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, NIMH Psychopharmacology Research Branch, Division of Extramural Research Programs, Rockville, MD, pp 218–222
Haney M, Rabkin J, Gunderson E, Foltin RW (2005) Dronabinol and marijuana in HIV(+) marijuana smokers: acute effects on caloric intake and mood. Psychopharmacology 181(1):170–178. https://doi.org/10.1007/s00213-005-2242-2
Haney M, Gunderson EW, Rabkin J, Hart CL, Vosburg SK, Comer SD, Foltin RW (2007) Dronabinol and marijuana in HIV-positive marijuana smokers. Caloric intake, mood, and sleep. J Acquir Immune Defic Syndr (1999) 45(5):545–554. https://doi.org/10.1097/QAI.0b013e31811ed205
Hasin DS (2017) US Epidemiology of Cannabis Use and Associated Problems. Neuropsychopharmacology 43(1):195-212
Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, Jung J, Pickering RP, Ruan WJ, Smith SM, Huang B, Grant BF (2015) Prevalence of marijuana use disorders in the United States between 2001–2002 and 2012–2013. JAMA Psychiatry 72(12):1235–1242. https://doi.org/10.1001/jamapsychiatry.2015.1858
Hasin DS, Kerridge BT, Saha TD, Huang B, Pickering R, Smith SM, Jung J, Zhang H, Grant BF (2016) Prevalence and correlates of DSM-5 cannabis use disorder, 2012-2013: findings from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Am J Psychiatry 173(6):588–599. https://doi.org/10.1176/appi.ajp.2015.15070907
Hurst H, Bolton J (2004) Assessing the clinical significance of change scores recorded on subjective outcome measures. J Manip Physiol Ther 27(1):26–35. https://doi.org/10.1016/j.jmpt.2003.11.003
Ives TJ, Chelminski PR, Hammett-Stabler CA, Malone RM, Perhac JS, Potisek NM, Shilliday BB, DeWalt DA, Pignone MP (2006) Predictors of opioid misuse in patients with chronic pain: a prospective cohort study. BMC Health Serv Res 6(1):46. https://doi.org/10.1186/1472-6963-6-46
Jamison RN, Serraillier J, Michna E (2011) Assessment and treatment of abuse risk in opioid prescribing for chronic pain. Pain Res Treat 2011:941808
Johnson JR, Burnell-Nugent M, Lossignol D, Ganae-Motan ED, Potts R, Fallon MT (2010) Multicenter, double-blind, randomized, placebo-controlled, parallel-group study of the efficacy, safety, and tolerability of THC:CBD extract and THC extract in patients with intractable cancer-related pain. J Pain Symptom Manag 39(2):167–179. https://doi.org/10.1016/j.jpainsymman.2009.06.008
Kahan M, Srivastava A (2007) Is there a role for marijuana in medical practice? No. Can Fam Physician Medecin de famille canadien 53(1):22–25
Kalant H (2004) Adverse effects of cannabis on health: an update of the literature since 1996. Prog Neuro-Psychopharmacol Biol Psychiatry 28(5):849–863. https://doi.org/10.1016/j.pnpbp.2004.05.027
Kirsh KL, Jass C, Bennett DS, Hagen JE, Passik SD (2007) Initial development of a survey tool to detect issues of chemical coping in chronic pain patients. Palliat Support Care 5(3):219–226
Kouyanou K, Pither CE, Wessely S (1997) Medication misuse, abuse and dependence in chronic pain patients. J Psychosom Res 43(5):497–504. https://doi.org/10.1016/S0022-3999(97)00171-2
Liebschutz JM, Saitz R, Weiss RD, Averbuch T, Schwartz S, Meltzer EC, Claggett-Borne E, Cabral H, Samet JH (2010) Clinical factors associated with prescription drug use disorder in urban primary care patients with chronic pain. J Pain 11(11):1047–1055. https://doi.org/10.1016/j.jpain.2009.10.012
Martel MO, Dolman AJ, Edwards RR, Jamison RN, Wasan AD (2014) The association between negative affect and prescription opioid misuse in patients with chronic pain: the mediating role of opioid craving. J Pain 15(1):90–100. https://doi.org/10.1016/j.jpain.2013.09.014
Martel MO, Finan PH, McHugh RK, Issa M, Edwards RR, Jamison RN, Wasan AD (2016) Day-to-day pain symptoms are only weakly associated with opioid craving among patients with chronic pain prescribed opioid therapy. Drug Alcohol Depend 162:130–136. https://doi.org/10.1016/j.drugalcdep.2016.02.047
Michna E, Ross EL, Hynes WL, Nedeljkovic SS, Soumekh S, Janfaza D, Palombi D, Jamison RN (2004) Predicting aberrant drug behavior in patients treated for chronic pain: importance of abuse history. J Pain Symptom Manag 28(3):250–258. https://doi.org/10.1016/j.jpainsymman.2004.04.007
Narang S, Gibson D, Wasan AD, Ross EL, Michna E, Nedeljkovic SS, Jamison RN (2008) Efficacy of dronabinol as an adjuvant treatment for chronic pain patients on opioid therapy. J Pain 9(3):254–264. https://doi.org/10.1016/j.jpain.2007.10.018
Nielsen S, Lintzeris N, Bruno R, Campbell G, Larance B, Hall W, Hoban B, Cohen ML, Degenhardt L (2015) Benzodiazepine use among chronic pain patients prescribed opioids: associations with pain, physical and mental health, and health service utilization. Pain Med (Malden, Mass) 16(2):356–366. https://doi.org/10.1111/pme.12594
Notcutt W, Langford R, Davies P, Ratcliffe S, Potts R (2012) A placebo-controlled, parallel-group, randomized withdrawal study of subjects with symptoms of spasticity due to multiple sclerosis who are receiving long-term Sativex(R) (nabiximols). Mult Scler (Houndmills, Basingstoke, England) 18(2):219–228. https://doi.org/10.1177/1352458511419700
Osborn LA, Lauritsen KJ, Cross N, Davis AK, Rosenberg H, Bonadio F, Lang B (2015) Self-medication of somatic and psychiatric conditions using botanical marijuana. J Psychoactive Drugs 47(5):345–350. https://doi.org/10.1080/02791072.2015.1096433
Passik SD, Lowery A (2011) Psychological variables potentially implicated in opioid-related mortality as observed in clinical practice. Pain Med (Malden, Mass) 12(Suppl 2):S36–S42. https://doi.org/10.1111/j.1526-4637.2011.01130.x
Portenoy RK, Ganae-Motan ED, Allende S, Yanagihara R, Shaiova L, Weinstein S, McQuade R, Wright S, Fallon MT (2012) Nabiximols for opioid-treated cancer patients with poorly-controlled chronic pain: a randomized, placebo-controlled, graded-dose trial. J Pain 13(5):438–449. https://doi.org/10.1016/j.jpain.2012.01.003
Saunders KW, Von Korff M, Campbell CI, Banta-Green CJ, Sullivan MD, Merrill JO, Weisner C (2012) Concurrent use of alcohol and sedatives among persons prescribed chronic opioid therapy: prevalence and risk factors. J Pain 13(3):266–275. https://doi.org/10.1016/j.jpain.2011.11.004
Savage SR (2008) The language of pain and addiction. In: Smith HS, Passik SD (eds) Pain and chemical dependency. Oxford, pp 9–13
Savage SR, Romero-Sandoval A, Schatman M, Wallace M, Fanciullo G, McCarberg B, Ware M (2016) Cannabis in pain treatment: clinical and research considerations. J Pain 17(6):654–668. https://doi.org/10.1016/j.jpain.2016.02.007
Schieffer BM, Pham Q, Labus J, Baria A, Van Vort W, Davis P, Davis F, Naliboff BD (2005) Pain medication beliefs and medication misuse in chronic pain. J Pain 6(9):620–629. https://doi.org/10.1016/j.jpain.2005.04.004
Skinner HA (1982) The drug abuse screening test. Addict Behav 7(4):363–371. https://doi.org/10.1016/0306-4603(82)90005-3
Smith HS, Passik SD (2008) Pain and chemical dependency. Oxford University Press, New York
Spearing MK, Post RM, Leverich GS, Brandt D, Nolen W (1997) Modification of the Clinical Global Impressions (CGI) Scale for use in bipolar illness (BP): the CGI-BP. Psychiatry Res 73(3):159–171. https://doi.org/10.1016/S0165-1781(97)00123-6
Toth C, Mawani S, Brady S, Chan C, Liu C, Mehina E, Garven A, Bestard J, Korngut L (2012) An enriched-enrolment, randomized withdrawal, flexible-dose, double-blind, placebo-controlled, parallel assignment efficacy study of nabilone as adjuvant in the treatment of diabetic peripheral neuropathic pain. Pain 153(10):2073–2082. https://doi.org/10.1016/j.pain.2012.06.024
Wade DT, Makela P, Robson P, House H, Bateman C (2004) Do cannabis-based medicinal extracts have general or specific effects on symptoms in multiple sclerosis? A double-blind, randomized, placebo-controlled study on 160 patients. Mult Scler (Houndmills, Basingstoke, England) 10(4):434–441. https://doi.org/10.1191/1352458504ms1082oa
Wade DT, Makela PM, House H, Bateman C, Robson P (2006) Long-term use of a cannabis-based medicine in the treatment of spasticity and other symptoms in multiple sclerosis. Mult Scler (Houndmills, Basingstoke, England) 12(5):639–645. https://doi.org/10.1177/1352458505070618
Ware MA, Fitzcharles MA, Joseph L, Shir Y (2010) The effects of nabilone on sleep in fibromyalgia: results of a randomized controlled trial. Anesth Analg 110(2):604–610. https://doi.org/10.1213/ANE.0b013e3181c76f70
Ware MA, Wang T, Shapiro S, Collet JP (2015) Cannabis for the management of pain: assessment of safety study (COMPASS). J Pain 16(12):1233–1242. https://doi.org/10.1016/j.jpain.2015.07.014
Wasan AD, Butler SF, Budman SH, Benoit C, Fernandez K, Jamison RN (2007) Psychiatric history and psychologic adjustment as risk factors for aberrant drug-related behavior among patients with chronic pain. Clin J Pain 23(4):307–315. https://doi.org/10.1097/AJP.0b013e3180330dc5
Wu SA, Compton P, Bolus R, Schieffer B, Pham Q, Baria A, Van Vort W, Davis F, Shekelle P, Naliboff BD (2006) The addiction behaviors checklist: validation of a new clinician-based measure of inappropriate opioid use in chronic pain. J Pain Symptom Manag 32:342–351
Acknowledgements
The authors wish to acknowledge all the additional clinical site investigators who enrolled subjects for the study, including Dr. Gordon Ko, Dr. Peter Blecher, Dr. Aline Boulanger, and Dr. May Ong-Lam. We also wish to acknowledge the advice of Dr. Kenneth Kirsch, the study management team at AXON for study coordination and data management, and medical writer Mark E. Rose, MA, for putting together the early draft of the paper.
Funding
The study was supported by an unrestricted educational grant from Valeant Pharmaceuticals (Canada). Valeant markets nabilone under the brand name Cesamet®.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MAW discloses the following relationships: CanniMed, Green Sky Labs (grant to institution), CHI Inc., Zynerba, and CannaRoyalty (consultant). RJ discloses the following relationships: Astra Zeneca, Knight, Paladin, and Purdue Pharma (speakers’ bureau, consultant). MM and JS declare that they have no conflict of interest.
Electronic supplementary material
Supplementary Table 1
(DOCX 17 kb)
Supplementary Table 2
(DOCX 16 kb)
Supplementary Table 3
(DOCX 17 kb)
Supplementary Table 4
(DOCX 14 kb)
Supplementary Table 5
(DOCX 12 kb)
Supplementary Table 6
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Ware, M.A., Martel, M.O., Jovey, R. et al. A prospective observational study of problematic oral cannabinoid use. Psychopharmacology 235, 409–417 (2018). https://doi.org/10.1007/s00213-017-4811-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-017-4811-6