Abstract
Rationale
Previous research has shown limited efficacy of nicotine replacement therapy (NRT) among adolescents and generally low compliance rates. As higher compliance rates are associated with improved abstinence rates, the present study examined predictors of NRT compliance.
Objectives
This study aims to test whether different NRT compliance trajectories can be distinguished among adolescents, to test whether these trajectories can be predicted by demographic, smoking-related, and personality factors, and to examine abstinence rates for each trajectory.
Methods
Data were used from a randomized controlled trial that tested the efficacy of nicotine patches versus placebo patches among 265 Dutch adolescents. During NRT treatment, adolescents filled out six online questionnaires in which they reported on the number of days they used the patches. Predictors (i.e., demographic and smoking-related factors and personality characteristics) and end-of-treatment abstinence were also administered through these self-reports. Latent class growth analysis (LCGA) was used to analyze compliance data by classifying individuals into similar growth trajectories.
Results
Three compliance trajectories were found (i.e., “compliers” (n = 89), “moderate decreasers” (n = 41), and “strong decreasers” (n = 127)). The compliers can be characterized by higher levels of conscientiousness and agreeableness and lower levels of extraversion compared with the strong decreasers, and by higher levels of conscientiousness and education compared with the moderate decreasers. Among the compliers, a substantially higher percentage of adolescents achieved abstinence at end-of-treatment (10 %) compared with the moderate decreasers (3 %) and the strong decreasers (6 %).
Conclusions
These findings could be the starting point for person-tailored interventions that aim to enhance NRT compliance rates among adolescents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although a decline in smoking prevalence among Dutch adolescents has been observed over the past 10 years, still 11 % of adolescents aged 10 to 19 years are daily smokers (STIVORO 2012). This decline in prevalence rates has also been seen in the USA, although there the percentage of daily smokers is slightly lower (ranging from 2 % at age 14 to 9 % at age 18; Johnston et al. 2010). The majority of adolescent smokers have tried to quit smoking at least once (61 % of high school students) but only 12 % actually succeeded (Centers for Disease Control and Prevention 2009). An important factor that obstructs successful smoking cessation is the occurrence of nicotine-dependence symptoms (Kleinjan et al. 2009) such as withdrawal symptoms and cravings (Bagot et al. 2007; van Zundert et al. 2009). Young adolescent smokers may already experience these symptoms (DiFranza et al. 2002), even after smoking for only a short period (DiFranza et al. 2000; DiFranza et al. 2002; O’Loughlin et al. 2003). Therefore, when it comes to achieving (more) sustainable abstinence, adolescents might benefit from nicotine replacement therapy (NRT), as this approach aims to reduce relapse by relieving withdrawal symptoms and cravings (Stead et al. 2008).
Recently, a meta-analysis (Kim et al. 2011) and a review (Bailey et al. 2012) reported on the effectiveness of pharmacological therapies (i.e., NRT and bupropion) in adolescent smokers. The review yielded some evidence for the efficacy of pharmacological therapies on smoking cessation immediately after the end of treatment. However, the meta-analysis concluded that pharmacological therapy among adolescent smokers did not result in a significant increase of short- and mid-term abstinence cessation rates. One reason that may explain the small or nonsignificant effects could be low compliance rates in most studies, though this factor varies largely across studies (32.5–91.8 %; Kim et al. 2011).
Recently, a randomized controlled trial (RCT) was conducted to test the short-term efficacy of NRT in adolescents and investigate whether the efficacy of NRT depends on medication compliance (Scherphof et al. 2014). Results showed that the efficacy of NRT on smoking cessation depends on the level of compliance. That is, nicotine patches increase the chance of achieving abstinence but among higher compliant adolescents only. This emphasizes the relevance of NRT compliance to achieve smoking cessation among adolescents.
Adults generally show a decline in compliance with NRT. For example, Stapleton et al. (1995) found a decline in active patch use over a 12-week patch treatment period from 92 % in week 1 to 61 % in week 12. In adolescents, such a clear decline was not demonstrated, but compliance rates have been shown to be low; Killen et al. (2004) demonstrated that only 41 % of the adolescents receiving patch therapy used all their patches during only two of eight treatment weeks or even less. To improve compliance rates among adolescents, more insight is needed concerning the individual-level factors that determine compliance to NRT.
Previous studies have investigated predictors of compliance with pharmacotherapy conducted among adults; as far as we know, such research has not been conducted among adolescents. Most of these studies focused on demographic and smoking-related factors. With regard to demographic factors, higher compliance was associated with higher levels of education, older age, and being female (Hays et al. 2010; Lam et al. 2005). Secondly, smoking (cessation)-related factors that have been linked to high compliance with pharmacotherapy include (a) smoking fewer cigarettes per day (CPD) at the onset of treatment, (b) a larger number of previous quit attempts, and (c) a higher level of motivation to quit smoking (Alterman et al. 1999; Hays et al. 2010; Lam et al. 2005; Okuyemi et al. 2010). Moreover, the substantial number of Dutch adolescents using cannabis (8 % in 2009; Verdurmen et al. 2012) and the frequently reported co-occurrence of smoking and cannabis use (Agrawal and Lynskey 2009), indicates the relevance of taking cannabis use into account as one of the smoking-related predictors. In addition to demographic and smoking-related factors, personality characteristics can be expected to predict compliance to NRT because these characteristics have emerged as potentially useful determinants of several health-related behaviors (Raynor 2004) including medication adherence (Jerant et al. 2011). Moreover, these characteristics may be important for the improvement of compliance rates because previous studies indicate that personality-targeted interventions generally yield larger effect sizes than do universal programs (Conrod et al. 2008; Gottfredson and Wilson 2003). Hence, personality factors may be a good starting point for predicting and ultimately increasing compliance rates. Previous studies found that several personality factors were related to medication compliance for different (chronic) diseases in young people. For example, (facets of) conscientiousness, openness and agreeableness have been associated with compliance to asthma medication and with compliance behaviors in adolescent hypertensive patients (Axelsson et al. 2009; Zugelj et al. 2010). However, to our knowledge only one study has addressed personality characteristics as potential predictors of compliance to pharmacological treatment for smoking cessation (Raynor 2004). This study found that higher levels of conscientiousness and openness were associated with higher medication compliance while adjusting for demographics, smoking-related factors, and other personality characteristics. It must be noted that this study was conducted among weight-concerned women receiving group behavior therapy with either bupropion or placebo, which may subvert the external validity of the findings.
To conclude, efforts to increase NRT compliance, with the ultimate aim to develop individualized tailored interventions to improve compliance rates (Okuyemi et al. 2010), seem warranted to improve cessation rates among adolescents. As compliance is a dynamic process, instead of merely examining predictors of compliance, the present study aimed to identify compliance trajectories of adolescents who displayed unique patterns of compliance behavior. Relevant individual factors were included to predict these trajectories. Based on previous findings concerning NRT compliance in adults, we studied the predictive role of demographic factors (age, gender, and education level), smoking (cessation)-related factors (number of previous quit attempts, CPD, motivation to quit, and cannabis use), and personality factors (the five dimensions of the Big Five (McCrae and John 1987): openness, extraversion, agreeableness, conscientiousness, and neuroticism). In addition, as compliance to treatment has been associated with improved health outcomes (i.e., successful smoking cessation) (Alterman et al. 1999; Killen et al. 1999), we also examined whether the odds of achieving abstinence differed across the different trajectories. We expected to find the highest percentage of quitters in the trajectory with the most compliant adolescents.
Methods
Design
For this randomized, double-blind placebo-controlled clinical trial, adolescents were randomized according to a computer-generated randomization list by the pharmacy of the University Medical Center Utrecht into either (1) an active study medication group (nicotine patch) or (2) an identical appearing placebo group (placebo patch). Participants were recruited from September to November 2010. Treatment started in the period between February and May 2011. The present study is part of a long-term follow-up study registered at TrialRegister.nl (NTR3031), which was approved by the Medical Ethical Committee of the Utrecht Medical Center.
Participants
After an Internet search, 66 public secondary schools and 8 higher vocational training schools in the Netherlands were randomly selected and invited to participate in the study, upon which 33 schools agreed to participate. For participant recruitment, research assistants visited the schools during lunch breaks, handed out flyers, and pinned up posters at notice boards. In addition, banners were placed on Hyves, a popular network site on the Internet. Students who were interested in participating were required to fill out an online screening questionnaire for eligibility. Participants were allowed to participate if (1) they were 12 years up to and including 18 years old, (2) they were not having major physical health problems (cardiovascular disease, diabetes, and/or skin disease), (3) they smoked at least seven cigarettes a day, (4) the parents were aware of their smoking behavior, and (5) they were motivated to quit smoking (score 2 or 3 on the question: “How eagerly do you want to be a nonsmoker?” using a scale from 0 (Not at all) to 3 (Very much)). Individuals (1) who were currently using NRT or other smoking cessation medication, (2) who were pregnant or lactating, or (3) who reported being allergic to patches in general or to any ingredients in the patches, were excluded from participation. Signed informed consent was obtained from both participants and parents (or legal guardians) if participants were 17 years or younger and from only participants if they were 18 years old.
A total of 585 adolescents filled out the online screening questionnaire, of which 362 were eligible to participate. The others did not meet the inclusion criteria or failed to complete the online questionnaire. Of the 362 adolescents who were invited to join an information meeting (see below), 265 were actually present at the meeting. Eight participants were excluded from all analyses due to contradictory answers, quitting study participation, or filling out fewer than two online questionnaires. The final randomized sample consisted of 257 participants (see Fig. 1 for a flowchart).
The sample was characterized by an average age of 16.6 (SD = 1.13) at baseline and consisted of 52.9 % girls and 60.3 % in higher education (high school and higher vocational education). At baseline, the nicotine patch group contained significantly more females than the placebo patch group (χ 2 (1, 257) = 4.59, p = 0.03). For all other covariates (i.e., age, education level, number of previous quit attempts, cigarettes per day, motivation to quit, cannabis use, openness, extraversion, agreeableness, conscientiousness, and neuroticism), no differences between conditions were found.
Intervention
All 257 participants first attended a 75-min information meeting. This meeting, chaired by a trained research assistant, consisted of three parts. First, a pretreatment questionnaire was filled out that contained important background information of the participant. Second, participants received (a) information about the study, (b) a short behavioral intervention aimed at quitting smoking (e.g., preparations and expectations), and (c) instructions for the use of NRT (e.g., the importance of adherence). Finally, the placebo and nicotine patches were handed out, whereby both participants and research assistants were blind to treatment allocation.
Participants were instructed to start the treatment period and quit smoking on the Monday after the meeting. Adolescents who were smoking >20 cigarettes a day received a higher patch dose and continued use for 9 weeks (3 weeks at 21 mg/day, 3 weeks at 14 mg/day, and 3 weeks 7 mg/day), whereas adolescents smoking ≤20 cigarettes a day used a lower dose for a period of 6 weeks (3 weeks at 14 mg/day and 3 weeks at 7 mg/day). During the treatment period, six online questionnaires were filled out: on the first quit day (T1), the third day (T2), the fifth day (T3), the eighth day (T4), the 15th day (T5), and for the last time on the day after finishing treatment (T6). At every measurement occasion, respondents received an e-mail including an individualized URL that would lead them to the questionnaire. Participants were compensated with €20 for attending the meeting and €25 for filling out six online questionnaires (with €5 reduction for each questionnaire that was missing).
Measures
Compliance was measured in all six online questionnaires. Respondents were asked how many days since the previous online questionnaire they had used the patches. Example answers were as follows: “I used patches at 0 days/1 day/2 days/3 days since the previous questionnaire” (T1–T4), “I used patches at 0 days/1–2 days/3–4 days/5–6 days/every day since the previous questionnaire” (T5), and “I used patches at 0 days/1–2 days/3–4 days/5–6 days/7 days/week since the previous questionnaire” (T6). To take into account the different time spans between measurements, the number of days patches were used in between measurements was divided by the total number of days between measurements. This resulted in percentile scores between 0 and 1. Self-report measures are very efficient and cost-effective methods of assessing medication compliance (Thompson et al. 2000), and a moderate to high concordance with nonself-report measures has been shown (Garber et al. 2004).
Smoking cessation was defined as a 30-day point prevalence abstinence at 6-month follow-up (T7). Participants were asked to report which of the following statements suited them best: “In the period between the previous questionnaire until now (1) I have not smoked at all; (2) I have smoked, but now I quit; (3) I quit for a while, but now I smoke again; or (4) I have smoked the whole period.” Respondents who answered (1) or (2) were presented with the following question: “How long ago did you smoke your last cigarette?” Answers for this question ranged from 1 (today) to 8 (4 weeks ago or longer). Participants who answered “4 weeks ago or longer” to the latter question were considered to be abstinent.
The pretreatment questionnaire (T0) contained questions on smoking characteristics, personality, and demographic variables. Smoking characteristics included number of previous quit attempts, number of CPD, cannabis use in the past year, and motivation to quit smoking.
Personality traits were measured by the Quick Big Five (QBF) Inventory (Vermulst and Gerris 2005; Gerris et al. 1998). The QBF Inventory consists of 30 items that are divided into 5 scales (of six items each): Openness (item example: “imaginative”), Extraversion (item example: “talkative”), Agreeableness (item example: “pleasant”), Conscientiousness (item example: “tidy”), and Neuroticism (item example: “irritable”). Participants were asked to rate the degree to which each personality characteristic applied to them. Answers ranged from 0 (“not at all applicable”) to 6 (“completely applicable”). Cronbach’s alphas were 0.76, 0.78, 0.77, 0.84, and 0.81, respectively.
Demographic characteristics included age, gender, and educational level (higher education (i.e., high school and pre-university) versus lower education (i.e., vocational training)). Finally, we included condition as a predictor (i.e., nicotine patch versus placebo patch).
Data analyses
Latent class growth analysis (LCGA), conducted in Mplus version 7.0, was used to analyze compliance data collected six times during NRT treatment by classifying individuals into groups based on similarities in growth trajectories (i.e., intercepts and slopes) (King et al. 2012; Muthén and Muthén 2000). In LCGA, all elements of the within-class covariance matrix of the growth factors are constrained to zero (i.e., each trajectory is assumed identical for all individuals within the class) (Muthén and Muthén 2000; St Pourcain et al. 2011). We modelled linear growth in compliance rates. Missing data on the compliance variables were handled by the Full Information Maximum Likelihood (FIML) procedure, which uses all the available information without imputing missing values. Other missing data were imputed by the Expectation-Maximization algorithm (Schafer 1999) in SPSS version 20.0 (IBM Corp. 2011)..
To determine the optimal number of latent compliance trajectories, we compared models with one to four trajectories on the Bayesian Information Criterion (BIC), the Bootstrapped Likelihood Ratio Test (BLRT), and the Entropy. Lower BIC values indicate a better fit of the model to the data, while significant BLRT results indicate that adding an extra trajectory significantly improves the model (Nylund et al. 2007). To determine how accurately each model places participants into trajectories, we examined Entropy values, whereby values of 0.8 or higher indicated a good classification (Celeux and Soromenho 1996). To increase the quality of the classifications, latent classes in all models were regressed on a set of covariates via a multinomial logistic regression model in which latent classes served as the dependent variable (Olino et al. 2010). To adjust for the effect of any smoking behavior during the treatment period on compliance, we included smoking as a time-varying variable in additional analyses, whereby the same effect was assumed for all trajectories. We checked for and found no multicollinearity between the predictors. The strongest correlations was found between agreeableness and openness (r = 0.46, p < 0.01).
Finally, we determined the propensity to quit smoking after the treatment for each trajectory using a three-step method in which smoking cessation was regressed on the latent class trajectories (Asparouhov and Muthén 2012). Smoking cessation was treated here as a distal outcome with unequal means and equal variances. We performed an intent-to-treat analysis and included all participants randomized; participants who did not fill out one or more of the questionnaires were assumed to have been smoking.
Results
Identifying compliance trajectories
Results indicated that the three-class model was a better fit than the two-class model. When comparing the three- and four-class models, the four-class model fit slightly better than did the three-class model according to the BIC; however, the BLRT was not significant, which indicates that adding a fourth trajectory did not significantly improve the model. As the fourth class was very similar to the class of “compliers” in the three-class solution, the three-class model was chosen as the optimal model (Table 1). Entropy in the three-class model was high. Means of the predictors for each trajectory are depicted in Table 2.
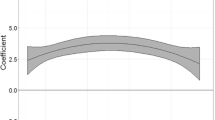
In the three-class model shown in Fig. 2, the first latent class contained 34.6 % of the sample (N = 89). This class was characterized by high compliance rates at T1 (intercept = 1.004) and a small, but significant, decrease in compliance rates during treatment (slope = −0.002, p < 0.001). We called this class the compliers. The second latent class contained 16.0 % of the sample (N = 41). This class demonstrated the same compliance rates at T1 (intercept = 1.009), but a somewhat steeper decrease compared with that of class 1 (slope = −0.012, p < 0.001). Therefore, we called this group the “moderate decreasers.” The third latent class contained 49.4 % of the sample (N = 127). This class demonstrated similar compliance rates at T1 (intercept = 0.999) and the steepest decrease compared with groups 1 and 2 (slope = −0.022, p < 0.001). This class was named the “strong decreasers.”
Predictors of compliance trajectories
The coefficients (odds) in Table 3 depict how much lower or higher participants in the strong decreasers and moderate decreasers trajectories scored on the predictor variables compared with the compliers trajectory (reference category). Adolescents in the strong decreasers trajectory were less conscientious (p = 0.001), more extravert (p = 0.004), and more agreeable (p = 0.047) than were adolescents in the compliers trajectory. Adolescents in the moderate decreasers trajectory were less conscientious (p = 0.002) and lower educated (p = 0.049) than were adolescents in the compliers trajectory. Adolescents in both the strong decreasers and moderate decreasers had undertaken fewer previous quit attempts than adolescents in the compliers trajectory, but differences were not significant (p = 0.092 and p = 0.056, respectively). Finally, we found that condition (i.e., active patch versus placebo patch use) did not differentiate between the different trajectories, suggesting that compliance was not dependent on whether adolescents used the nicotine patch or the placebo patch.
The time-varying effects of smoking on compliance at each measurement are depicted in Table 4. All coefficients are negative, and significant effects were found at T3, T4, and T5. This means that if one started smoking at time T, compliance at the same T was lower than the compliance as predicted by the trajectory. As compliance is a 0/1 variable, the coefficients can be interpreted in percentages. For example, smoking at T3 means that compliance is 6 % lower than the predicted compliance by the trajectory. The effect is especially strong at T5 (14 % lower) and seems to increase over time (from T1 to T5). Only at T6, the effect is smaller, probably because the time interval between T5 and T6 was much larger than the previous time intervals.
Reasons for noncompliance
At T7, all participants who reported not having used the patches every day until the end of treatment (n = 206) were asked why they did not use the patches during the total treatment period (multiple answers possible, n = 19 missing cases). Of the 187 participants who answered this question, the reported reasons for noncompliance were returning to smoking (18.7 %), having the feeling that the patches had no effect (38.0 %), forgetfulness (37.4 %), experiencing side effects (19.3 %), and quitting smoking (10.2 %).
Abstinence rates
With regard to the probability of achieving abstinence for the different trajectories, we found that the compliers had the highest chances of quitting smoking at 6-month follow-up (T7; 10.4 %) compared with the moderate decreasers (3.1 %) and the strong decreasers (6.1 %). Abstinence rates, however, did not differ significantly between the three trajectories (overall equality test, χ 2 (2, 257) = 3.612, p = 0.164).
Discussion
There is increasing interest in NRT to promote smoking cessation among adolescents, although the effectiveness of this treatment is not yet fully established (Bailey et al. 2012; Kim et al. 2011). These unconvincing results may be explained by the low compliance rates in these studies, which raises the need to investigate developmental trajectories and predictors of compliance. Our findings revealed that three compliance trajectories can be identified (compliers, moderate decreasers, and strong decreasers), who all started at the same high initial levels of compliance but differed in the degree of decline over time. The differences in the development of these trajectories were explained by one smoking-cessation-related variable and three personality characteristics. The compliers were higher educated compared with the moderate decreasers, confirming previous research (Lam et al. 2005). The compliers are also characterized by higher levels of conscientiousness and agreeableness and lower levels of extraversion compared with the strong decreasers, and by higher levels of conscientiousness compared with the moderate decreasers. Although most of the adolescents who achieved abstinence at 6-month follow-up were found in the compliers trajectory (10 %), this percentage did not significantly differ from the other two trajectories (3 and 6 % among the moderate and strong decreasers, respectively).
The results of our study are in line with those of previous studies among adult samples that show compliance to patch therapy declines over time (e.g., Stapleton et al. 1995). However, our study extends that finding by determining three different trajectories of compliance and their characteristics. The compliers reported higher levels of conscientiousness compared with the moderate and strong decreasers. This finding confirms results from studies among adults in which conscientiousness was established as a fairly constant factor related to (smoking cessation) medication compliance (Axelsson et al. 2011; Jerant et al. 2011; Raynor 2004). Young people with lower conscientiousness levels, that is, those who are less self-disciplined, responsible, and reliable, are less likely to use the patches as described.
In addition, we found that the compliers were less extravert compared with the strong decreasers. Higher levels of extraversion are associated with sociability, excitement seeking, and activity (Cohen et al. 2004), which are characteristics that have been related to adolescent smoking (onset) (Harakeh et al. 2006; Otten et al. 2008). It can be assumed that extravert adolescents, because of their higher sociability and excitement seeking tendencies, will be more tempted to smoke and will be “too busy or too engaged to remember taking medication” (Cohen et al. 2004, p. 111). Furthermore, we also found higher levels of agreeableness among the compliers compared with the strong decreasers. Individuals with higher levels of agreeableness are less predisposed to being skeptical, reluctant, and more cooperative (Axelsson et al. 2009, 2013). Therefore, it is likely that more compliant adolescents are less assertive (less prone to do things their own way) and more cooperative with the study protocol (i.e., using the patches daily).
Thus, conscientiousness, extraversion, and agreeableness appeared to be the personality factors associated with compliance. The other two personality domains of the Big Five, i.e., neuroticism and openness) did not differ between compliance trajectories. Future studies should investigate the complex relationships between such personality factors, compliance, and abstinence of smoking, in the context of mediation modeling, to shed further light on the role of personality in the success of smoking abstinence therapies.
Furthermore, our results suggest the relevance of being compliant to medication, as we showed that higher percentages (although not significant) of successful smoking cessation was found in the most compliant trajectory. This is consistent with results of previous research that has demonstrated a positive relation between NRT compliance and smoking cessation (Alterman et al. 1999; Killen et al. 1999. The nonsignificant results might be due to the long time span between treatment period and follow-up.
Limitations
There are several potential limitations. First, NRT compliance was assessed by means of six online self-report measures, which may have elicited socially desirable answering tendencies. However, we decided to use these self-report measures because a previous study showed that a more objective measures of compliance (i.e., collecting used and unused patches), was unreliable because participants often failed to return their patches (Hanson et al. 2003). With regard to the reliability of this self-report measure, we would like to note that we put substantial effort in emphasizing the importance of being honest (“there are no good or bad answers”) and that the high compliant group indeed showed substantially more quitters than the group of moderate and strong decreasers. Second, due to the use of adolescents’ self-reports of their smoking status, without biochemical validation, under- or over-reporting may have occurred (Patrick et al. 1994). Conversely, several studies among adolescents have concluded that self-reported smoking and quitting behavior are as valid and reliable as a more objective method such as biochemical verification (Dolcini et al. 1996). Moreover, although biochemical measures are recommended for special subgroups (e.g., adolescents), in some situations the added precision gained by biochemical verification is not required and may not be desirable, such as studies with limited face-to-face contact and studies where the optimal data collection methods are through the mail, telephone, or Internet (Society for Research on Nicotine and Tobacco (SRNT) Subcommittee on Biochemical Verification 2002). Related to this, in the self-report question about their smoking status, we did not explicitly distinguish between smoking cigarettes and cannabis, and therefore we cannot be sure that respondents reported about their cigarette smoking behavior only. However, during the information meeting we did emphasize that smoking cannabis was (in principle) not allowed during their smoking cessation attempt, and in some of the intermittent questionnaires we did separately ask about their cannabis smoking behavior. In addition, as we did not specify the time exact period in which participants had to report on their smoking behavior, underreporting of the number of cigarettes per day might have occurred if participants already had cut down their smoking behavior by the time of filling out the pretreatment questionnaire. Third, as we asked how many days, on average, they used the patches per week during the last 4 weeks of the treatment period, we assumed that the decrease in patch compliance followed a linear trend. Considering the longer timespan between T5 and T6, the estimation of compliance during these 4 weeks might not have been linear, rather mainly focused on first days after T5. Given the way we asked about compliance, we cannot check this. Moreover, a slight nonlinear trend between T5 and T6 alone, could not affect the general growth pattern in compliance over the entire study. Fourth, the pharmacotherapy used in this study was 6/9 weeks 21/14/7 mg nicotine patch. Therefore, the present findings may not generalize to other treatment durations, other dosages of the patch, or other smoking cessation pharmacotherapy. Finally, since the aim of the present paper was to get more insight into personality factors related to compliance behavior in the general adolescent population, we included the Big-Five personality characteristics as predictor variables. However, psychiatric illness may be related to decreased medication compliance rates as well. Therefore, it would be interesting to include measures of psychiatric illnesses (e.g., depression and attention deficit hyperactivity disorder) in future research as well.
Implications
Insight into adolescent smokers’ characteristics that predict the use of NRT might help in the development of interventions tailored to their particular needs for assistance with quitting (Botello-Harbaum et al. 2010). As adolescents’ levels of conscientiousness, agreeableness, and extraversion were predictors of the different compliance trajectories, treatment to enhance compliance to NRT should dilate on these factors. Previous studies have shown that providing personality-targeted interventions can reduce substance abuse in (early) adolescence (Conrod et al. 2008, 2010; O'Leary-Barret et al. 2010). In these selective interventions, elevated levels of personality risk factors for substance abuse were examined and subsequently targeted by means of psycho-education, motivational interviewing, and behavioral cognitive therapy. These techniques of targeting the risk factors could also be applied to enhance compliance rates. For instance, youth scoring low on conscientiousness might benefit from interventions aimed at support and assistance by peers, parents or a professional, whereas those who score high on extraversion might benefit from interventions aimed at resisting peer pressure and developing systematic daily patch use schedules, and those scoring low on agreeableness might be helped with interventions aimed at increasing cooperative behavior. Such a tailored intervention that aims at enhancing compliance in adolescents can be integrated into currently used smoking-cessation interventions for adolescents.
References
Agrawal A, Lynskey MT (2009) Tobacco and cannabis co-occurrence: does route of administration matter? Drug Alcohol Depend 99:240–247
Alterman AI, Gariti P, Cook TG, Cnaan A (1999) Nicodermal patch adherence and its correlates. Drug Alcohol Depend 53:159–165
Asparouhov T, Muthén B (2012) Auxiliary variables in mixture modeling: a 3-step approach using Mplus. Mplus Webnote 15
Axelsson M, Emilsson M, Brink E, Lundgren J, Torén K, Lotvall J (2009) Personality, adherence, asthma control and health-related quality of life in young adult asthmatics. Respir Med 103:1033–1040
Axelsson M, Brink E, Lundgren J, Lötvall J (2011) The influence of personality traits on reported adherence to medication in individuals with chronic disease: an epidemiological study in West Sweden. PLoS ONE 6:e18241
Axelsson M, Cliffordson C, Lundback B, Lotvall J (2013) The function of medication beliefs as mediators between personality traits and adherence behavior in people with asthma. Patient Prefer Adherence 7:1101–1109
Bagot KS, Heishman SJ, Moolchan ET (2007) Tobacco craving predicts lapse to smoking among adolescent smokers in cessation treatment. Nicotine Tob Res 9:647–652
Bailey SR, Crew EE, Riske EC, Ammerman S, Robinson TN, Killen JD (2012) Efficacy and tolerability of pharmacotherapies to aid smoking cessation in adolescents. Pediatr Drugs 14:91–108
Botello-Harbaum M, Schroeder JR, Collins CC, Moolchan ET (2010) Nicotine replacement therapy use among adolescent smokers seeking cessation treatment. Ethn Dis 20:180–184
Celeux G, Soromenho G (1996) An entropy criterion for assessing the number of clusters in a mixture model. J Classif 13:195–212
Centers for Disease Control and Prevention (2009) High school students who tried to quit smoking cigarettes—United States, 2007. Morb Morb Weekly Report 58:428–431
Cohen NL, Ross EC, Bagby RM, Farvolden P, Kennedy SH (2004) The 5-factor model of personality and anti-depressant medication compliance. Can J Psychiatry 49:106–113
Conrod PJ, Castellanos N, Mackie C (2008) Personality-targeted interventions delay the growth of adolescent drinking and binge drinking. J Child Psychol Psychiatry 49:181–190
Conrod PJ, Castellanos-Ryan N, Strang J (2010) Brief, personality-targeted coping skills interventions and survival as a non-drug user over a 2-year period during adolescence. Arch Gen Psychiatr 67:85–93
DiFranza JR, Rigotti NA, McNeill AD, Ockene JK, Savageau JA, St Cyr D et al (2000) Initial symptoms of nicotine dependence in adolescents. Tob Control 9:313–319
DiFranza JR, Savageau JA, Rigotti NA, Fletcher K, Ockene JK, McNeill AD et al (2002) Development of symptoms of tobacco dependence in youths: 30 month follow up data from the DANDY study. Tob Control 11:228–235
Dolcini MM, Adler NE, Ginsberg D (1996) Factors influencing agreement between self-reports and biological measures of smoking among adolescents. J Res Adolesc 6:515–542
Garber MC, Nau DP, Erickson SR, Aikens JE, Lawrence JB (2004) The concordance of self-report with other measures of mediation adherence. Med Care 42:649–652
Gerris JRM, Houtmans MJM, Kwaaitaal-Roosen EMG, De Schipper JC, Vermulst AA, Janssens JMAM (1998) Parents, adolescents and young adults in Dutch families: a longitudinal study. Nijmegen, the Netherlands: Institute of Family Studies
Gottfredson DC, Wilson DB (2003) Characteristics of effective school-based substance abuse prevention. Prev Sci 4:27–38
Hanson K, Allen S, Jensen S, Hatsukami D (2003) Treatment of adolescent smokers with the nicotine patch. Nicotine Tob Res 5:515–526
Harakeh Z, Scholte RHJ, de Vries H, Engels RCME (2006) Association between personality and adolescent smoking. Addict Behav 31:232–245
Hays JT, Leischow SJ, Lawrence D, Lee TC (2010) Adherence to treatment for tobacco dependence: associations with smoking abstinence and predictors of adherence. Nicotine Tob Res 12:574–581
IBM Corp (2011) IBM SPSS Statistics for Windows, Version 20.0. IBM Corp, Armonk, NY
Jerant A, Chapman B, Duberstein P, Robins J, Franks P (2011) Personality and medication non-adherence among older adults enrolled in a six-year trial. Br J Health Psychol 16:151–169
Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE (2010) Monitoring the future national survey results on drug use, 1975–2009. Volume I: secondary school students. National Institute on Drug Abuse, Bethesda, MD
Killen JD, Fortmann SP, Davis L, Strausberg L, Varady A (1999) Do heavy smokers benefit from higher dose nicotine patch therapy? Exp Clin Psychopharmacol 3:226–233
Killen JD, Robinson TN, Ammerman S, Hayward C, Rogers J, Stone C et al (2004) Randomized clinical trial of the efficacy of bupropion combined with nicotine patch in the treatment of adolescent smokers. J Consult Clin Psychol 72:729–735
Kim Y, Myung SK, Jeon YJ, Lee EH, Park CH, Seo HG, Huh BY (2011) Effectiveness of pharmacologic therapy for smoking cessation in adolescent smokers: meta-analysis of randomized controlled trials. Am J Health Syst Pharm 68:219–226
King PS, Berg CA, Butner J, Drew LM, Foster C, Donaldson D et al (2012) Longitudinal trajectories of metabolic control across adolescence: associations with parental involvement, adolescents’ psychosocial maturity, and health care utilization. J Adolesc Health 50:491–496
Kleinjan M, van den Eijnden RJJM, Engels RCME (2009) Adolescents’ Rationalizations to continue smoking: the role of disengagement beliefs and nicotine dependence in smoking cessation. Addict Behav 34:440–445
Lam TH, Abdullah ASM, Chan SSC, Hedley AJ (2005) Adherence to nicotine replacement therapy versus quitting smoking among Chinese smokers: a preliminary investigation. Psychopharmacol 177:400–408
McCrae RR, John OP (1987) An introduction of the five-factor model and its applications. J Pers 60:175–215
Muthén B, Muthén LK (2000) Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res 24:882–891
Nylund KL, Asparouhov T, Muthén BO (2007) Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Model 14:535–569
O’Loughlin J, DiFranza J, Tyndale RF, Meshefedjian G, McMillan-Davey E, Clarke PBS et al (2003) Nicotine-dependence symptoms are associated with smoking frequency in adolescents. Am J Prev Med 25:219–225
Okuyemi KS, Zheng H, Guo H, Ahluwalia JS (2010) Predictors of adherence to nicotine gum and counseling among African–American light smokers. J Gen Intern Med 25:969–976
O'Leary-Barret M, Mackie CJ, Castellanos-Ryan N, Al-Khudhairy N, Conrod PJ (2010) Personality-targeted interventions delay uptake of drinking and decrease risk of alcohol-related problems when delivered by teachers. J Am Acad Child Adolesc Psychiatry 49:954–963
Olino TM, Klein DN, Lewinsohn PM, Rohde P, Seeley JR (2010) Latent trajectory classes of depressive and anxiety disorders from adolescence to adulthood: descriptions of classes and associations with risk factors. Compr Psychiatry 51:224–235
Otten R, Engels RCME, van den Eijnden RJJM (2008) Smoking behavior in asthmatic and non-asthmatic adolescents: the role of smoking models and personality. Subst Use Misuse 43:341–360
Patrick DL, Cheadle A, Thompson DC, Diehr P, Koepsell T, Kinne S (1994) The validity of self-reported smoking: a review and meta-analysis. Am J Public Health 84:1086–1093
Raynor DA (2004) Adherence to pharmacological smoking cessation treatment among weight-concerned women. PhD dissertation, University of Pittsburgh
Schafer JL (1999) Multiple imputation: a primer. Stat Methods Med Res 8:3–15
Scherphof CS, van den Eijnden RJJM, Engels RCME, Vollebergh WAM (2014) Short-term efficacy of nicotine replacement therapy for smoking cessation in adolescents: a randomized controlled trial. J Subst Abuse Treat 46:120–127
St Pourcain B, Mandy WP, Heron J, Golding J, Smith GD, Skuse DH (2011) Links between co-occurring social-communication and hyperactive-inattentive trait trajectories. J Am Acad Child Adolesc Psychiatry 50:892–902
Stapleton JA, Russell MA, Feyerabend C, Wiseman SM, Gustavsson G, Sawe U, Wiseman D (1995) Dose effects and predictors of outcome in randomized trial of transdermal nicotine patches in general practice. Addiction 90:31–42
Stead LF, Perera R, Bullen C, Mant D, Lancaster T (2008) Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev Issue 1. Art. No.: CD000146
STIVORO (2012) Roken, de harde feiten: jeugd 2012 [Smoking, the harsh facts: youth 2013]. STIVORO-voor een rookvrije toekomst, The Hague
Thompson K, Kulkarni J, Sergejew AA (2000) Reliability and validity of a new Medication Adherence Rating Scale (MARS) for the psychoses. Schizophr Res 42:241–247
Van Zundert RMP, Boogerd EA, Vermulst AA, Engels RCME (2009) Nicotine withdrawal symptoms following a quit attempt: an ecological momentary assessment study among adolescents. Nicotine Tob Res 11:722–729
Verdurmen J, Monshouwer K, van Dorsselaar S, Lokman S, Vermeulen-Smit E, Vollebergh W (2012) Jeugd en riskant gedrag 2011. Kerngegevens uit het peilstationsonderzoek scholieren. Trimbos-Instituut, Utrecht
Vermulst AA, Gerris JRM (2005) Quick Big Five Persoonlijkheidsvragenlijst. Handleiding [Quick Big Five Personality Questionnaire. Manual]. LDC, Leeuwarden
Zugelj U, Zupancic M, Komidar L, Kenda R, Varda NM, Gregoric A (2010) Self-reported adherence behavior in adolescent hypertensive patients: the role of illness representations and personality. J Pediatr Psychol 35:1049–1060
Conflict of interest
No conflicts of interest were reported by the authors of this paper.
Funding
This study is funded by the Netherlands Organization for Health Research and Development (ZonMw).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Scherphof, C.S., van den Eijnden, R.J.J.M., Lugtig, P. et al. Adolescents’ use of nicotine replacement therapy for smoking cessation: predictors of compliance trajectories. Psychopharmacology 231, 1743–1752 (2014). https://doi.org/10.1007/s00213-014-3511-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-014-3511-8