Abstract
Rationale
Available neurochemical probes that lower brain dopamine (DA) levels in man are limited by their tolerability and efficacy. For instance, the acute lowering of brain tyrosine is well tolerated, but only modestly lowers brain DA levels. Modification of tyrosine depletion to robustly lower DA levels would provide a superior research probe.
Objectives
The objective of this study was to determine whether the subthreshold stimulation of presynaptic DA receptors would potentiate tyrosine depletion-induced effects on extracellular DA levels in the medial prefrontal cortex (MPFC) and striatum of the rat.
Methods
We administered quinpirole, a predominantly DA type 2 (D2R) receptor agonist, into the MPFC and striatum by reverse dialysis. A tyrosine- and phenylalanine-free neutral amino acid mixture [NAA(−)] IP was used to lower brain tyrosine levels. DA levels in the microdialysate were measured by HPLC with electrochemical detection.
Results
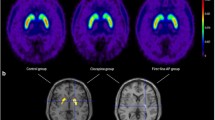
Quinpirole dose-dependently lowered DA levels in MPFC as well as in the striatum. NAA(−) alone transiently lowered DA levels (80 % baseline) in the striatum, but had no effect in MPFC. The co-administration of NAA(−) and a subthreshold concentration of quinpirole (6.25 nM) lowered DA levels (50 % baseline) in both the MPFC and striatum. This effect was blocked by the mixed D2R/D3R antagonist haloperidol at IP doses that on their own did not affect DA levels (10.0 nmol/kg in the MPFC and 0.10 nmol/kg in the striatum).
Conclusions
Pharmacological stimulation of inhibitory D2R receptors during tyrosine depletion markedly lowers the extracellular DA levels in the MPFC and striatum. The data suggest that combining tyrosine depletion with a low dose of a DA agonist should robustly lower brain regional DA levels in man.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The function of brain dopamine (DA) systems in man can be probed experimentally by transiently lowering brain regional DA levels. Each of the currently available methods, however, is limited by issues of efficacy or tolerability. The tyrosine hydroxylase (TH) inhibitor α-methyl-para-tyrosine robustly lowers catecholamine levels throughout the body (Engelman et al. 1968), but induces significant sedation, orthostasis, and bradykinesia (Abi-Dargham et al. 2000; Miller et al. 1996). The direct DA agonist apomorphine also lowers brain regional DA levels, but the effective dose (03–0.6 mg/kg SC; de La Fuente-Fernandez et al. 2001) overlaps with the threshold (0.4–0.5 mg/kg SC) for inducing emesis (Angrist et al. 1980). Such side effects can confound cognitive and other assessments.
The acute lowering of brain tyrosine (TYR) levels lowers brain DA turnover and/or efflux in the rat (Biggio et al. 1976; Fernstrom and Fernstrom 1995; Jaskiw et al. 2005; McTavish et al. 1999a; Wurtman et al. 1974) as well as in non-human primates (Palmour et al. 1998). In man, TYR depletion is generally well tolerated; its central anti-dopaminergic actions include the attenuation of manic symptoms, (McTavish et al. 2001), amphetamine antagonism (McTavish et al. 1999b), elevation of prolactin, and changes in DA-mediated indices of cognition and emotion (Gijsman et al. 2002; Harmer et al. 2001; Harrison et al. 2004). However, in vivo imaging shows that TYR depletion produces a rather modest (∼20 %) decline in extracellular DA levels in man (Montgomery et al. 2003). This may account for reports in which the lowering of TYR levels did not produce the expected effects (Ellis et al. 2007; Lythe et al. 2005; Mehta et al. 2005). The research utility of TYR depletion would be enhanced if associated changes in brain DA levels were larger and more consistent. We now report on one such strategy in the rat.
TYR availability can affect the rate of TYR hydroxylation, the rate-limiting step in DA synthesis (Ikeda et al. 1966). The enzyme tyrosine hydroxylase (TH) is normally thought to be close to full saturation with its TYR substrate (Kaufman and Kaufman 1985). Hence, an acute lowering of TYR levels lowers TYR hydroxylation (Bongiovanni et al. 2008, 2012; Fernstrom and Fernstrom 1995; McTavish et al. 1999a; Wurtman et al. 1974). This, given the usually rapid and efficient decarboxylation of DOPA (Neff et al. 2006; Waymire and Haycock 2002), results in a lower rate of DA synthesis and a reduction in the size of the releasable vesicular DA pool (Pothos et al. 1996). Since TYR depletion does not usually affect baseline extracellular DA levels (Bongiovanni et al. 2008; Jaskiw et al. 2005, 2006, 2008b), however, other homeostatic mechanisms must be involved.
In the striatum, DA receptors belonging to the type 2 family (D2R) and located on DA terminals as well as on non-DA neurons participate in the regulation of DA synthesis, release, and uptake (Anzalone et al. 2012; Wolf and Roth 1990; Wu et al. 2002; Zhang and Sulzer 2012). DA terminals in the medial prefrontal cortex possess only release-modulating autoreceptors, also from the D2R family (Bannon et al. 1982; Fadda et al. 1984; Galloway et al. 1986). We previously postulated that release-modulating terminal D2R receptors mediate the maintenance of stable extracellular DA levels in the face of acutely lowered DA synthesis (Bongiovanni et al. 2008). If this hypothesis were true, then TYR depletion concomitant with appropriate stimulation of these D2R receptors should result in a marked lowering of extracellular DA levels.
(−)-Quinpirole (QUI) is a direct agonist for D2R and D3R receptors (Flietstra and Levant 1998; Gehlert et al. 1992). The administration of QUI by reverse dialysis lowers in vivo DA levels in the medial prefrontal cortex (MPFC; Santiago et al. 1993b) and striatum (Imperato and Di Chiara 1988; Mao et al. 1996; Santiago et al. 1993a; Westerink and De Vries 2001). At a subthreshold concentration, namely, the maximal concentration that does not affect extracellular DA levels, QUI should provide stimulation to inhibitory D2R receptors comparable to that provided by endogenous DA. Under continuous pharmacological stimulation, these inhibitory receptors could no longer mediate compensatory processes normally triggered by a decline in extracellular DA levels. Thus, we postulated that TYR depletion during the administration of QUI by reverse dialysis would result in a marked lowering of extracellular DA levels in the MPFC and striatum.
Given the variability in the reported relationship between perfusate QUI concentrations and the DA response (Devoto et al. 2001; Freeman and Tallarida 1994; Imperato and Di Chiara 1988; Kurata and Shibata 1990; Mao et al. 1996; Santiago et al. 1993a, b; Tanaka et al. 1992; Westerink and De Vries 2001; You et al. 1994), we first determined a dose–response curve under our own laboratory conditions. Then, while perfusing the MPFC or the striatum with a subthreshold concentration of QUI, we systemically administered a TYR- and phenylalanine-free neutral amino acid solution [NAA(−)] that lowers brain TYR levels (Jaskiw et al. 2005, 2008a; McTavish et al. 1999a). Finally, to confirm that the action of QUI was DA receptor-mediated, we examined TYR depletion during the administration of QUI along with IP administration of the mixed D2R/D3R antagonist haloperidol at a dose that on its own does not affect DA levels (Westerink et al. 2001).
Materials and methods
Procedures were conducted in accordance with the NIH Guide for the Care and Use of Laboratory Animals (1996) and were approved by the LSC-VAMC Animal Care Committee. Male Sprague–Dawley rats (Harlan, 250–330 g) were housed three to a plastic cage (61 × 30 cm.) with sawdust bedding and maintained on a standard 12-h on/off light cycle with food and water ad libitum in an AALAC-accredited facility.
There were several modifications to our previous (Bongiovanni et al. 2008) microdialysis procedures. Anesthesia was administered in a gas chamber with 4.5 % isoflurane (Baxter) flushed with 2.0 L/min O2 at 1.0 bar. Anesthetized rats were removed, weighed, shaved, and placed in a stereotaxic frame (Kopf) with the incisor bar set at 7 mm. Anesthesia was then maintained through a nosecone perfused with 3 % isoflurane. A guide cannula and a microdialysis probe (PAN. 30 kDa, MWCO, 320-μm OD, 4-mm active membrane; Bioanalytical Science) were surgically implanted either in the MPFC (probe terminating: M/L ± 0.70 mm, A/P + 3.20 mm, V/D − 7.00 mm, relative to bregma) or in the striatum (probe terminating: M/L ± 3.20 mm, A/P + 1.00 mm, D/V − 7.00 mm). Only one probe was implanted in each animal with the side (i.e., L vs. R) alternating between rats. The probe was connected to polyethylene tubing (0.965-mm OD, 0.58-mm ID; length, 2 m) to a swivel and perfusion pump. Each rat was then placed singly in a 30 × 30 × 35-cm Plexiglas enclosure with hardwood shavings and food and water ad libitum.
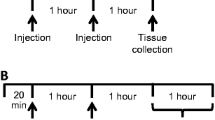
On the following morning (18–22 h after implantation), perfusion began with Dulbecco’s phosphate-buffered saline containing (in milliequivalents): 137 NaCl, 2.7 KCl, 0.5 MgCl2, 1.5 KH2PO4, 8.1 Na2HPO4, 1.2 CaCl2, and 5 % glucose (final pH 7.4). A perfusion rate of 1 μL/min was maintained using a syringe pump (Harvard Apparatus). The perfusate could be changed by switching the perfusion tubing directly at the probe inflow. Given the length of the probe outflow tubing (13.7 cm), there was a lag time of 36.2 min between a change in perfusate and the time at which the new perfusate entered the collection vial. Samples were collected every 30 min until a stable baseline was reached. At that point (t = 0 h), one of the following protocols was followed. In experiment 1, the vehicle perfusate was switched to one containing QUI (0–100 nM, free base). In experiment 2, one group was switched to a perfusate containing the subthreshold concentration of QUI (6.25 nM) while two groups continued to receive the standard perfusate vehicle (VEH). Then, at t = 1 h and t = 2 h, all animals received two identical IP injections of either NAA(−) or a saline VEH (1 ml/280 g). The administration of NAA(−) in two doses at separate time points 60 min apart has been demonstrated to induce a greater degree of TYR depletion than a single administration (McTavish et al. 1999a). The three groups in experiment 2 were: VEH/VEH, VEH/NAA(−), and QUI/NAA(−). Experiment 3 followed the same sequence as experiment 2, except that an additional IP injection of haloperidol (2 ml/kg) was administered at t = 1.5 h. The two groups in experiment 3 were: VEH/VEH/HAL and QUI/NAA(−)/HAL. Data were collected from a single microdialysis session in each rat.
A stock solution of QUI was made by dissolving (−)-quinpirole hydrochloride (Tocris Biosciences) 1 ng/μL (hydrochloride) in vehicle, pipetting it into aliquots and storing at −80 °C. On the morning of use, an aliquot was thawed and used to make a solution of QUI (6.25–100 nM as the free base) in PBS. The pH of the PBS was not significantly affected. The NAA(−) (total, 1 g/kg IP) was prepared as previously described (Bongiovanni et al. 2008; McTavish et al. 1999a) and administered in two equal volumes 1 h apart. A stock solution of haloperidol was prepared by adding 100 μL 1.0 M tartaric acid and 2.0 mg haloperidol (Sigma-Aldrich) to 1.73 mL H2O, sonicating until fully dissolved, and then adding 100 μL of 1 N NaOH. This stock solution was stored at 4 °C. On the morning of use, the stock solution was diluted with vehicle and brought to a pH ∼ 7.3. The dose of administered haloperidol was 10.0 nmol/kg = 3.76 μg/kg for MPFC and 0.10 nmol/kg = 0.0376 μg/kg for the striatum (Westerink et al. 2001).
At the end of the experiment, the animals were euthanized (IP Euthasol, Virbac Animal Health), decapitated, and their brains removed. Brains were stored at −40 °C until they were cut on a cryostat at 50-μm intervals for probe placement verification. Data from rats in which the probe extended beyond the region of interest were discarded.
The microdialysate (10 μL) was analyzed by HPLC coupled with electrochemical detection. Separation was achieved on a 100 × 4.6-mm reversed-phase C18 column with 3-μm particles (Agilent Technologies Microsorb-MV). The mobile phase consisted of 12.5 mM citrate, 20.0 mM acetate, and 0.1 mM EDTA, with 5 % (v/v) methanol adjusted to pH 4.5 with sodium hydroxide and 0–3.0 mM octylsulfonic acid adjusted as a modifier. The mobile phase was pumped at a rate of 0.5 mL/min. DA was measured using an electrochemical detector with a glassy carbon electrode and maintained at a relative potential of 0.50 V to an Ag/AgCl reference electrode (model LC-4; Bioanalytical Systems, IN, USA). The detection limit for DA was 50 fg/10 μL at a 3:1 signal-to-noise ratio.
Data expressed as the percentage of baseline were analyzed (GraphPad Prism) using ANOVA with time as the repeated factor. If the overall ANOVA was significant, it was followed by Bonferroni’s post hoc t tests. Data are expressed as the mean ± SEM.
Results
Basal levels
The basal values of DA in microdialysate were 0.51 ± 0.04 nM in the MPFC and 3.66 ± 0.36 nM in striatum.
QUI lowers DA levels
For the MPFC, the two-way ANOVA showed significant effects of treatment [F(5,233) = 46.12, p < 0.0001], time [F(11,233) = 18.16, p < 0.0001], and a treatment × time interaction [F(55,233) = 1.98, p < 0.0003] (Fig. 1). Post hoc tests showed that QUI concentrations ≥25 nM significantly lowered DA levels relative to vehicle. For the striatum, the two-way ANOVA showed significant effects of treatment [F(5,233) = 57.40, p < 0.0001], time [F(11,233) = 16.95, p < 0.0001], and treatment × time interaction [F(55,233) = 3.91, p < 0.0001] (Fig. 1). Post hoc tests showed that QUI concentrations ≥12.5 nM significantly lowered DA levels relative to vehicle. QUI 6.25 nM was then selected as the subthreshold concentration for lowering DA levels in the MPFC and striatum.
Effect of quinpirole (QUI) or vehicle (VEH) administered by reverse dialysis into the medial prefrontal cortex or the striatum on dopamine (DA) levels in a microdialysate. Results are expressed as percent baseline or percent vehicle, with error bars for ±SEM. The graph on the left shows the time course of changes. The heavy black line denotes the duration of QUI perfusion. The graph on the right shows the maximal change for a given concentration of QUI relative to vehicle (n = 4–6/group). Significant differences for each concentration relative to vehicle at any time point are denoted: *p < 0.05, ***p < 0.001 (ANOVA followed by Bonferroni t test)
TYR depletion and a subthreshold dose of QUI lower DA levels
For the MPFC, the two-way ANOVA showed effects of treatment [F(2,128) = 35.75, p < 0.0001], time [F(11,128) = 3.88, p < 0.0001] and a time × treatment interaction [F(22,128) = 2.29, p < 0.002]. Post hoc tests showed that while there were no significant differences between the VEH/VEH and the VEH/NAA(−) groups, after t = 3.0 h, the DA levels in the QUI/NAA(−) group were significantly lower than those in the VEH/VEH group (p < 0.05–0.001; Fig. 2). For the striatum, the two-way ANOVA showed effects of treatment [F(2,137) = 43.64, p < 0.0001], time [F(11,137) = 5.42, p < 0.0001] and time × treatment interaction [F(22,137) = 5.80, p < 0.0001]. Post hoc tests showed that DA levels in the VEH/NAA(−) compared to the VEH/VEH group were significantly lower at t = 2.5 h (p < 0.01) and t = 3.0 h (p < 0.05). DA levels in the QUI/NAA(−) group were significantly lower compared to the VEH/VEH group at t ≥ 2.5 h (p < 0.001) and compared to the VEH/NAA(−) group at t ≥ 3.5 h (p < 0.001; Fig. 2).
Effect of vehicle (VEH) or quinpirole (QUI) ± a tyrosine- and phenylalanine-free neutral amino acid solution [NAA(−)] on dopamine (DA) levels in a microdialysate. QUI 6.25 nM was administered by reverse dialysis (heavy black line denotes the duration of perfusion) to one of three groups. NAA(−) or VEH was administered IP at the times indicated by the arrows. Results are expressed as percent baseline, with error bars for ±SEM (n = 5/group). Significant differences from vehicle are denoted: *p < 0.05, **p < 0.01, ***p < 0.001 (ANOVA followed by Bonferroni t test comparison to VEH)
Haloperidol blocks the QUI effect
For the MPFC, the two-way ANOVA showed no significant effects of treatment [F(1,68) = 2.04, p < 0.2], time [F(11,68) = 0.72, p < 0.7] or treatment × time interaction [F(11,68) = 0.52, p < 0.9]. In addition, post hoc tests showed that there were no significant differences between the VEH/VEH group (Fig. 2a) and either the VEH/VEH/ HAL group or the QUI/NAA(−)/HAL group (Fig. 3a). For the striatum, the two-way ANOVA showed a significant effect of treatment [F(1,66) = 5.94, p < 0.02], but not of time [F(11,66) = 1.18, p < 0.3] or treatment × time interaction [F(11,66) = 0.72, p < 0.7]. In addition, post hoc tests showed that there were no significant differences between the VEH/VEH group (Fig. 2b) and either the VEH/VEH/HAL group or the QUI/NAA(−)/HAL group (Fig. 3b).
Effect of vehicle (VEH) or quinpirole (QUI) ± a tyrosine- and phenylalanine-free neutral amino acid solution [NAA(−)] and haloperidol (HAL) on dopamine (DA) levels in a microdialysate. QUI 6.25 nM was administered by reverse dialysis (heavy black line denotes the duration of perfusion) to one of two groups. NAA(−) or VEH was administered IP at the times indicated by the arrows. Haloperidol (10.0 nmol/kg for MPFC and 0.10 nmol/kg for the striatum; Westerink et al. 2001) was administered IP at the time denoted by the arrow (n = 4/group). There were no significant differences between the groups
Discussion
QUI effects on DA levels
DA was dose-dependently lowered to 40 % of baseline levels by QUI ≥25 nM in the MPFC and QUI ≥12.5 nM in the striatum (Fig. 1). The literature provides limited data on QUI effects in the MPFC. One group did not find any effect of QUI 1–100 μM on frontal cortex DA levels, but used a trans-cerebral probe and collected microdialysate from regions outside of the MPFC (Devoto et al. 2001). Another group found that QUI 10 μM lowered MPFC DA to 65 % of baseline levels when the monoamine uptake blocker nomifensine was included in the perfusate (Santiago et al. 1993b). In the striatum, there are several reports that reverse dialysis of QUI 1–100 μM lowers DA (Freeman and Tallarida 1994; Imperato and Di Chiara 1988; Kurata and Shibata 1990; Mao et al. 1996; Santiago et al. 1993a; Sarre et al. 1996; Tanaka et al. 1992; Westerink and De Vries 2001; You et al. 1994), whereas QUI 100 nM has little, if any, effect (Imperato and Di Chiara 1988; Westerink and De Vries 2001). One group did find that QUI ∼50 nM lowered striatal DA levels (Freeman and Tallarida 1994). While our effective QUI concentrations are lower than most reported in the literature, such differences are not unusual given the sensitivity of microdialysis data to methodological variables (de Lange et al. 2000).
NAA(−) effects on the DA levels
We used a NAA(−) mixture known to lower brain tissue and extracellular TYR levels by 40–60 % (Bongiovanni et al. 2008; Jaskiw et al. 2008a; Jaskiw and Bongiovanni 2004; McTavish et al. 1999a). As in our earlier studies (Jaskiw et al. 2005, 2006), NAA(−) did not significantly affect DA levels in the MPFC (Fig. 2). We were surprised, however, that NAA(−) lowered DA levels in the striatum, albeit modestly (Fig. 2). Another group had not found any NAA(−) effects on in vivo striatal DA levels in anesthetized rats (McTavish et al. 1999a). Although we had previously shown that NAA(−) blunts haloperidol- or high potassium-induced elevations of striatal DA (Jaskiw et al. 2008b; Jaskiw and Bongiovanni 2004), this is the first time that we examined the effects of NAA(−) alone on striatal DA levels.
NAA(−) + QUI
During reverse dialysis with QUI 6.25 nM, TYR depletion produced a sustained lowering of DA levels in the MPFC to approximately 50 % the baseline (Fig. 2). In the striatum, the levels in the NAA(−) and the NAA(−) + QUI groups declined in parallel to 80 % of the baseline by t = 3 h. After that, DA levels in the NAA(−) group returned to baseline levels, whereas those in the NAA(−) + QUI continued to decline to 50 % of the baseline and remained significantly lower than those for NAA(−) alone for the duration of the experiment (Fig. 2). Thus, TYR depletion concurrent with local administration of a subthreshold dose of QUI resulted in a marked and sustained lowering of extracellular DA levels in both regions.
Reversal of effects by haloperidol
As reported by others (Westerink et al. 2001), haloperidol 10 and 0.01 nmol/kg IP alone did not affect DA levels in the MPFC or striatum, respectively (Fig. 3). However, haloperidol pretreatment completely prevented the effects of QUI + NAA(−) in the MPFC as well as striatum (Fig. 3).
Receptor specificity
QUI shows greater affinity for D2R than for D3R (Gehlert et al. 1992; Levant et al. 1995; Stanwood et al. 2000). Haloperidol has comparable antagonist potency at D2R and D3R (Levant et al. 1995). While we did not pharmacologically distinguish these receptor subtypes, the relative paucity of D3R in the MPFC and the dorsal striatum (Diaz et al. 2000; Levesque et al. 1992; Stanwood et al. 2000) suggests that D2R stimulation accounted for the lowering of the DA levels in the QUI + NAA(−) group. This is also in keeping with the functional nature of the QUI effects.
Receptors inhibiting DA efflux
Observations that opposite responses could be elicited by low doses as opposed to high doses of DA agonists led to the pharmacological characterization of inhibitory D2R receptors that were present on neuronal soma as well as on terminals, had a higher affinity for DA than conventional receptors, and were involved in the presynaptic modulation of DA release (Favard et al. 1990; Meller et al. 1987; Roth 1984; Starke et al. 1989). Autoreceptors tonically inhibiting both DA synthesis and release were identified on mesolimbic and nigrostriatal DA neurons; DA terminals innervating the MPFC possessed only release-modulating autoreceptors (Bannon et al. 1981b; Chiodo et al. 1984; Galloway et al. 1986; Wolf and Roth 1990). Later studies demonstrated D2R autoreceptors involved in the regulation of both DA uptake and release (Wu et al. 2002). D2R that tonically inhibit local DA efflux have also been identified on non-DAergic neurons of the dorsal striatum (Anzalone et al. 2012). Thus, the actions of QUI (Figs. 1 and 2) were likely D2R-mediated.
We were able to block QUI effects in the striatum at a dose of haloperidol (0.01 nmol/kg) well below the threshold (90 nmol/kg) for affecting striatal DA synthesis (Bardo et al. 1990). Compared to the striatum, DA synthesis in the MPFC is less responsive to D2R antagonism (Bannon et al. 1981b). These data suggest that QUI-induced subthreshold stimulation of tonically inhibitory release-modulating D2R receptors in the MPFC and striatum permitted DA levels to fall after TYR depletion.
NAA(−) and TYR hydroxylation
NAA(−)-induced TYR depletion lowers tissue DOPA accumulation across multiple brain regions, including the striatum and the frontal cortex (Fernstrom and Fernstrom 1995; McTavish et al. 1999a). While we did not measure DOPA levels in the current study, we previously found that NAA(−) lowers MPFC DOPA levels in vivo (Bongiovanni et al. 2008). Under the heuristic assumption that TYR is homogeneously distributed in the intracellular water of all cell types, cytosolic TYR levels in the brain have been estimated to be in the range 110–150 μM, well above the affinity of TH for TYR (∼10–20 μM; Kaufman and Kaufman 1985). This has suggested that TH is usually close to full saturation (Kaufman and Kaufman 1985) or perhaps even under the inhibitory influence of TYR (Best et al. 2009). Experimentally, a lowering of brain TYR availability lowers the rate of brain regional TYR hydroxylation (Bongiovanni et al. 2012; Fernstrom and Fernstrom 1995; Jaskiw et al. 2005, 2008a; McTavish et al. 1999a; Tam et al. 1990). On the other hand, the assumption that TYR is homogeneously distributed within a given cell is violated in at least some models (Menniti and Diliberto 1989). Several studies suggest partial compartmentalization of the TYR destined for monoamine synthesis (Delanoy et al. 1982; Kapatos and Zigmond 1977). In addition, brain cytosol contains both soluble and membrane-bound forms of TH that may have different regulatory properties (Cartier et al. 2010; Kuczenski and Mandell 1972). A mitochondrial form of TH has also been identified (Wang et al. 2009). Thus, the ultrastructural localization and kinetics of the TH that accounts for our current results remain to be fully characterized.
MPFC vs. striatum
We were surprised to find that NAA(−) lowered extracellular DA levels, albeit transiently and modestly, in the striatum but not in the MPFC (Fig. 2). DA terminals in the MPFC are characterized by a high fraction of activated TH (Iuvone and Dunn 1986), a greater dependence of DA synthesis on TYR levels (Bradberry et al. 1989; Tam et al. 1990), rapid DA turnover (Bannon et al. 1981a), tight coupling between DA synthesis and efflux (Galloway et al. 1986), and a high rate of DA efflux per terminal (Cass and Gerhardt 1995; Garris and Wightman 1994). These features have been taken to suggest that of all DA terminal fields, the MPFC should be the most sensitive to TYR availability (Tam et al. 1990). There are, however, additional considerations. The striatum/MPFC ratio is ∼10:1 with respect to the rate of tissue DOPA accumulation (Argiolas et al. 1979; Bradberry et al. 1989; Galloway et al. 1986; Kilts et al. 1987; Tam et al. 1990; Tyler and Galloway 1992), but ∼100:1 for tissue DA levels (Bannon et al. 1981a; Jaskiw et al. 1990, 2008a; Kilts et al. 1987). Assuming comparable DA content per DA terminal, the rate of TYR hydroxylation per DA terminal would be higher in the MPFC. On the other hand, the density of DA terminals is greater in the striatum. Furthermore, the regulation of extracellular DA levels in the MPFC and striatum differs considerably (Budygin et al. 1999; Ciliax et al. 1995; Kaenmaki et al. 2010; Masana et al. 2011). These differences notwithstanding, QUI + NAA(−) comparably lowered DA levels in both regions by about 50 % (Fig. 2).
Clinical research implications
The use of an amino acid mixture to lower the indices of brain DA turnover was originally demonstrated in the rat (Biggio et al. 1976), confirmed in non-human primates (Palmour et al. 1998), and then adapted for clinical research. The ability of NAA(−) to attenuate manic symptoms (McTavish et al. 2001) counteract certain amphetamine effects (McTavish et al. 1999b), elevate prolactin levels, and affect processes involving cognition, emotion, and reward (Gijsman et al. 2002; Harmer et al. 2001; Harrison et al. 2004) is consistent with anti-dopaminergic actions. In vivo imaging data confirmed that NAA(−) lowers striatal DA levels in man by around 20 % (Montgomery et al. 2003). However, a number of negative reports (Ellis et al. 2007; Lythe et al. 2005; Mehta et al. 2005) suggest that the decline in DA levels may be too modest or transient for NAA(−) to constitute a reliable probe. We posit that this shortcoming could be resolved by combining NAA(−) with a presynaptic DA agonist.
Apomorphine is a clinically available (LeWitt et al. 2009) direct DA agonist that at low doses stimulates inhibitory receptors and lowers extracellular brain regional DA levels in the rat (Adachi et al. 2000; Bean et al. 1990; Rodenhuis et al. 2000) as well as in man (de La Fuente-Fernandez et al. 2001). However, the dose of apomorphine that effectively lowers extracellular DA brain levels in man (03–0.6 mg/kg SC; de La Fuente-Fernandez et al. 2001) overlaps with the threshold (0.4–0.5 mg/kg SC) for inducing emesis (Angrist et al. 1980). Our data suggest that administering NAA(−) in combination with a dose of apomorphine subthreshold both for lowering the DA levels and inducing emesis would lower extracellular brain DA levels by about 50 % (Fig. 2). This level of DA depletion should provide a reliable and valuable probe of human brain regional DA systems without inducing extrapyramidal (Nord and Farde 2011) and other side effects.
References
Abi-Dargham A, Rodenhiser J, Printz D, Zea-Ponce Y, Gil R, Kegeles LS, Weiss R, Cooper TB, Mann JJ, Van Heertum RL, Gorman JM, Laruelle M (2000) Increased baseline occupancy of D2 receptors by dopamine in schizophrenia. Proc Natl Acad Sci U S A 97:8104–8109
Adachi Y, Uchihashi Y, Watanabe K, Satoh T (2000) Halothane anesthesia decreases the extracellular level of dopamine in rat striatum: a microdialysis study in vivo. J Anesth 14:82–90
Angrist B, Rotrosen J, Gershon S (1980) Responses to apomorphine, amphetamine, and neuroleptics in schizophrenic subjects. Psychopharmacology (Berlin) 67:31–38
Anzalone A, Lizardi-Ortiz JE, Ramos M, De MC, Hopf FW, Iaccarino C, Halbout B, Jacobsen J, Kinoshita C, Welter M, Caron MG, Bonci A, Sulzer D, Borrelli E (2012) Dual control of dopamine synthesis and release by presynaptic and postsynaptic dopamine D2 receptors. J Neurosci 32:9023–9034
Argiolas A, Fadda F, Melis MR, Serra G, Gessa GL (1979) Chronic haloperidol causes persistent increase in 3,4-dihydroxyphenylacetic acid (DOPAC) concentration in the substantia nigra but not in the ventral tegmental area. Brain Res 175:178–182
Bannon MJ, Bunney EB, Roth RH (1981a) Mesocortical dopamine neurons: rapid transmitter turnover compared to other brain catecholamine systems. Brain Res 218:376–382
Bannon MJ, Michaud RL, Roth RH (1981b) Mesocortical dopamine neurons: lack of autoreceptors modulating dopamine synthesis. Mol Pharmacol 19:270–275
Bannon MJ, Reinhard JF Jr, Bunney EB, Roth RH (1982) Unique response to antipsychotic drugs is due to absence of terminal autoreceptors in mesocortical dopamine neurones. Nature 296:444–446
Bardo MT, Bowling SL, Pierce RC (1990) Changes in locomotion and dopamine neurotransmission following amphetamine, haloperidol, and exposure to novel environmental stimuli. Psychopharmacology (Berlin) 101:338–343
Bean AJ, During MJ, Roth RH (1990) Effects of dopamine autoreceptor stimulation on the release of colocalized transmitters: in vivo release of dopamine and neurotensin from rat prefrontal cortex. Neurosci Lett 108:143–148
Best JA, Nijhout HF, Reed MC (2009) Homeostatic mechanisms in dopamine synthesis and release: a mathematical model. Theor Biol Med Model 6:21
Biggio G, Porceddu ML, Gessa GL (1976) Decrease of homovanillic, dihydroxyphenylacetic acid and cyclic-adenosine-3′,5′-monophosphate content in the rat caudate nucleus induced by the acute administration of an aminoacid mixture lacking tyrosine and phenylalanine. J Neurochem 26:1253–1255
Bongiovanni R, Kyser AN, Jaskiw GE (2012) Tyrosine depletion lowers in vivo DOPA synthesis in ventral hippocampus. Eur J Pharmacol 696:70–76
Bongiovanni R, Newbould E, Jaskiw GE (2008) Tyrosine depletion lowers dopamine synthesis and desipramine-induced prefrontal cortex catecholamine levels. Brain Res 1190:39–48
Bradberry CW, Karasic DH, Deutch AY, Roth RH (1989) Regionally-specific alterations in mesotelencephalic dopamine synthesis in diabetic rats: association with precursor tyrosine. J Neural Transm 78:221–229
Budygin EA, Gainetdinov RR, Kilpatrick MR, Rayevsky KS, Mannisto PT, Wightman RM (1999) Effect of tolcapone, a catechol-O-methyltransferase inhibitor, on striatal dopaminergic transmission during blockade of dopamine uptake. Eur J Pharmacol 370:125–131
Cartier EA, Parra LA, Baust TB, Quiroz M, Salazar G, Faundez V, Egana L, Torres GE (2010) A biochemical and functional protein complex involving dopamine synthesis and transport into synaptic vesicles. J Biol Chem 285:1957–1966
Cass WA, Gerhardt GA (1995) In vivo assessment of dopamine uptake in rat medial prefrontal cortex: comparison with dorsal striatum and nucleus accumbens. J Neurochem 65:201–207
Chiodo LA, Bannon MJ, Grace AA, Roth RH, Bunney BS (1984) Evidence for the absence of impulse-regulating somatodendritic and synthesis-modulating nerve terminal autoreceptors on subpopulations of mesocortical dopamine neurons. Neuroscience 12:1–16
Ciliax BJ, Heilman C, Demchyshyn LL, Pristupa ZB, Ince E, Hersch SM, Niznik HB, Levey AI (1995) The dopamine transporter: immunochemical characterization and localization in brain. J Neurosci 15:1714–1723
de La Fuente-Fernandez, Lim AS, Sossi V, Holden JE, Calne DB, Ruth TJ, Stoessl AJ (2001) Apomorphine-induced changes in synaptic dopamine levels: positron emission tomography evidence for presynaptic inhibition. J Cereb Blood Flow Metab 21:1151–1159
de Lange EC, de Boer AG, Breimer DD (2000) Methodological issues in microdialysis sampling for pharmacokinetic studies. Adv Drug Deliv Rev 45:125–148
Delanoy RL, Hunter GD, Dunn AJ (1982) Catecholamine metabolism in brain slices. Determination of relevant precursor pool and the effects of elevated K+. Biochem Pharmacol 31:3289–3296
Devoto P, Flore G, Pani L, Gessa GL (2001) Evidence for co-release of noradrenaline and dopamine from noradrenergic neurons in the cerebral cortex. Mol Psychiatry 6:657–664
Diaz J, Pilon C, Le Foll B, Gros C, Triller A, Schwartz JC, Sokoloff P (2000) Dopamine D3 receptors expressed by all mesencephalic dopamine neurons. J Neurosci 20:8677–8684
Ellis KA, Mehta MA, Naga Venkatesha Murthy PJ, McTavish SF, Nathan PJ, Grasby PM (2007) Tyrosine depletion alters cortical and limbic blood flow but does not modulate spatial working memory performance or task-related blood flow in humans. Hum Brain Mapp 28:1136–1149
Engelman K, Horwitz D, Jequier E, Sjoerdsma A (1968) Biochemical and pharmacologic effects of alpha-methyltyrosine in man. J Clin Invest 47:577–594
Fadda F, Gessa GL, Marcou M, Mosca E, Rossetti Z (1984) Evidence for dopamine autoreceptors in mesocortical dopamine neurons. Brain Res 293:67–72
Favard C, Simon A, Vigny A, Nguyen-Legros J (1990) Ultrastructural evidence for a close relationship between dopamine cell processes and blood capillary walls in Macaca monkey and rat retina. Brain Res 523:127–133
Fernstrom MH, Fernstrom JD (1995) Acute tyrosine depletion reduces tyrosine hydroxylation rate in rat central nervous system. Life Sci 57:97–102
Flietstra RJ, Levant B (1998) Comparison of D2 and D3 dopamine receptor affinity of dopaminergic compounds in rat brain. Life Sci 62:1825–1831
Freeman KA, Tallarida RJ (1994) A quantitative study of dopamine control in the rat striatum. J Pharmacol Exp Ther 268:629–638
Galloway MP, Wolf ME, Roth RH (1986) Regulation of dopamine synthesis in the medial prefrontal cortex is mediated by release modulating autoreceptors: studies in vivo. J Pharmacol Exp Ther 236:689–698
Garris PA, Wightman RM (1994) Different kinetics govern dopaminergic transmission in the amygdala, prefrontal cortex, and striatum: an in vivo voltammetric study. J Neurosci 14:442–450
Gehlert DR, Gackenheimer SL, Seeman P, Schaus J (1992) Autoradiographic localization of [3H]quinpirole binding to dopamine D2 and D3 receptors in rat brain. Eur J Pharmacol 211:189–194
Gijsman HJ, Scarna A, Harmer CJ, McTavish SB, Odontiadis J, Cowen PJ, Goodwin GM (2002) A dose-finding study on the effects of branch chain amino acids on surrogate markers of brain dopamine function. Psychopharmacology (Berlin) 160:192–197
Harmer CJ, McTavish SF, Clark L, Goodwin GM, Cowen PJ (2001) Tyrosine depletion attenuates dopamine function in healthy volunteers. Psychopharmacology (Berlin) 154:105–111
Harrison BJ, Olver JS, Norman TR, Burrows GD, Wesnes KA, Nathan PJ (2004) Selective effects of acute serotonin and catecholamine depletion on memory in healthy women. J Psychopharmacol 18:32–40
Ikeda M, Fahien LA, Udenfriend S (1966) A kinetic study of bovine adrenal tyrosine hydroxylase. J Biol Chem 241:4452–4456
Imperato A, Di Chiara G (1988) Effects of locally applied D-1 and D-2 receptor agonists and antagonists studied with brain dialysis. Eur J Pharmacol 156:385–393
Iuvone PM, Dunn AJ (1986) Tyrosine hydroxylase activation in mesocortical 3,4-dihydroxyphenylethylamine neurons following footshock. J Neurochem 47:837–844
Jaskiw GE, Bongiovanni R (2004) Brain tyrosine depletion attenuates haloperidol-induced striatal dopamine release in vivo and augments haloperidol-induced catalepsy in the rat. Psychopharmacology (Berlin) 172:100–107
Jaskiw GE, Karoum F, Freed WJ, Phillips I, Kleinman JE, Weinberger DR (1990) Effect of ibotenic acid lesions of the medial prefrontal cortex on amphetamine-induced locomotion and regional brain catecholamine concentrations in the rat. Brain Res 534:263–272
Jaskiw GE, Kirkbride B, Bongiovanni R (2006) In rats chronically treated with clozapine, tyrosine depletion attenuates the clozapine-induced in vivo increase in prefrontal cortex dopamine and norepinephrine levels. Psychopharmacology (Berlin) 185:416–422
Jaskiw GE, Kirkbride B, Newbould E, Young D, Durkalski V, Bongiovanni R (2005) Clozapine-induced dopamine release in the medial prefrontal cortex is augmented by a moderate concentration of locally administered tyrosine but attenuated by high tyrosine concentrations or by tyrosine depletion. Psychopharmacology (Berlin) 179:713–724
Jaskiw GE, Newbould E, Bongiovanni R (2008a) Gamma-butyrolactone-induced dopamine accumulation in prefrontal cortex is affected by tyrosine availability. Eur J Pharmacol 589:106–109
Jaskiw GE, Newbould E, Bongiovanni R (2008b) Tyrosine availability modulates potassium-induced striatal catecholamine efflux in vivo. Brain Res 1209:74–84
Kaenmaki M, Tammimaki A, Myohanen T, Pakarinen K, Amberg C, Karayiorgou M, Gogos JA, Mannisto PT (2010) Quantitative role of COMT in dopamine clearance in the prefrontal cortex of freely moving mice. J Neurochem 114:1745–1755
Kapatos G, Zigmond M (1977) Dopamine biosynthesis from l-tyrosine and l-phenylalanine in rat brain synaptosomes: preferential use of newly accumulated precursors. J Neurochem 28:1109–1119
Kaufman S, Kaufman EE (1985) Tyrosine Hydroxylase. In: Blakley RL, Benkovic SJ (eds) Chemistry and biochemistry of the pterins. Wiley, New York, pp 251–352
Kilts CD, Anderson CM, Ely TD, Nishita JK (1987) Absence of synthesis-modulating nerve terminal autoreceptors on mesoamygdaloid and other mesolimbic dopamine neuronal populations. J Neurosci 7:3961–3975
Kuczenski RT, Mandell AJ (1972) Regulatory properties of soluble and particulate rat brain tyrosine hydroxylase. J Biol Chem 247:3114–3122
Kurata K, Shibata R (1990) Biphasic effect of locally applied apomorphine and 2,3,4,5-tetrahydro-7,8-dihydroxy-1-phenyl-1H-3-benzazepine on the release of striatal dopamine investigated by means of brain dialysis. Neurosci Lett 117:264–268
Levant B, Grigoriadis DE, De Souza EB (1995) Relative affinities of dopaminergic drugs at dopamine D2 and D3 receptors. Eur J Pharmacol 278:243–247
Levesque D, Diaz J, Pilon C, Martres MP, Giros B, Souil E, Schott D, Morgat JL, Schwartz JC, Sokoloff P (1992) Identification, characterization, and localization of the dopamine D3 receptor in rat brain using 7-[3H]hydroxy-N,N-di-n-propyl-2-aminotetralin. Proc Natl Acad Sci U S A 89:8155–8159
LeWitt PA, Ondo WG, Van LB, Bottini PB (2009) Open-label study assessment of safety and adverse effects of subcutaneous apomorphine injections in treating “off” episodes in advanced Parkinson disease. Clin Neuropharmacol 32:89–93
Lythe KE, Anderson IM, Deakin JF, Elliott R, Strickland PL (2005) Lack of behavioural effects after acute tyrosine depletion in healthy volunteers. J Psychopharmacol 19:5–11
Mao A, Freeman KA, Tallarida RJ (1996) Transient loss of dopamine autoreceptor control in the presence of highly potent dopamine agonists. Life Sci 59:L317–L324
Masana M, Bortolozzi A, Artigas F (2011) Selective enhancement of mesocortical dopaminergic transmission by noradrenergic drugs: therapeutic opportunities in schizophrenia. Int J Neuropsychopharmacol 14:53–68
McTavish SF, Cowen PJ, Sharp T (1999a) Effect of a tyrosine-free amino acid mixture on regional brain catecholamine synthesis and release. Psychopharmacology (Berlin) 141:182–188
McTavish SF, McPherson MH, Harmer CJ, Clark L, Sharp T, Goodwin GM, Cowen PJ (2001) Antidopaminergic effects of dietary tyrosine depletion in healthy subjects and patients with manic illness. Br J Psychiatry 179:356–360
McTavish SF, McPherson MH, Sharp T, Cowen PJ (1999b) Attenuation of some subjective effects of amphetamine following tyrosine depletion. J Psychopharmacol 13:144–147
Mehta MA, Gumaste D, Montgomery AJ, McTavish SF, Grasby PM (2005) The effects of acute tyrosine and phenylalanine depletion on spatial working memory and planning in healthy volunteers are predicted by changes in striatal dopamine levels. Psychopharmacology (Berlin) 180:654–663
Meller E, Bohmaker K, Namba Y, Friedhoff AJ, Goldstein M (1987) Relationship between receptor occupancy and response at striatal dopamine autoreceptors. Mol Pharmacol 31:592–598
Menniti FS, Diliberto EJ Jr (1989) Newly synthesized dopamine as the precursor for norepinephrine synthesis in bovine adrenomedullary chromaffin cells. J Neurochem 53:890–897
Miller HL, Delgado PL, Salomon RM, Berman R, Krystal JH, Heninger GR, Charney DS (1996) Clinical and biochemical effects of catecholamine depletion on antidepressant-induced remission of depression. Arch Gen Psychiatry 53:117–128
Montgomery AJ, McTavish SF, Cowen PJ, Grasby PM (2003) Reduction of brain dopamine concentration with dietary tyrosine plus phenylalanine depletion: an [11C]raclopride PET study. Am J Psychiatry 160:1887–1889
Neff NH, Wemlinger TA, Duchemin AM, Hadjiconstantinou M (2006) Clozapine modulates aromatic l-amino acid decarboxylase activity in mouse striatum. J Pharmacol Exp Ther 317:480–487
Nord M, Farde L (2011) Antipsychotic occupancy of dopamine receptors in schizophrenia. CNS Neurosci Ther 17:97–103
Palmour RM, Ervin FR, Baker GB, Young SN (1998) An amino acid mixture deficient in phenylalanine and tyrosine reduces cerebrospinal fluid catecholamine metabolites and alcohol consumption in vervet monkeys. Psychopharmacology (Berlin) 136:1–7
Pothos E, Desmond M, Sulzer D (1996) L-3,4-dihydroxyphenylalanine increases the quantal size of exocytotic dopamine release in vitro. J Neurochem 66:629–636
Rodenhuis N, Dijkstra D, de BP, Vermeulen ES, Timmerman W, Wikstrom HV (2000) Dopamine D(2) activity of R-(−)-apomorphine and selected analogs: a microdialysis study. Eur J Pharmacol 387:39–45
Roth RH (1984) CNS dopamine autoreceptors: distribution, pharmacology, and function. Ann N Y Acad Sci 430:27–53
Santiago M, Machado A, Cano J (1993a) Effects of age and dopamine agonists and antagonists on striatal dopamine release in the rat: an in vivo microdialysis study. Mech Ageing Dev 67:261–267
Santiago M, Machado A, Cano J (1993b) Regulation of prefrontal cortical dopamine release by dopamine receptor agonists and antagonists. Eur J Pharmacol 239:83–91
Sarre S, Ebinger G, Michotte Y (1996) Levodopa biotransformation in hemi-Parkinson rats: effect of dopamine receptor agonists and antagonists. Eur J Pharmacol 296:247–260
Stanwood GD, Artymyshyn RP, Kung MP, Kung HF, Lucki I, McGonigle P (2000) Quantitative autoradiographic mapping of rat brain dopamine D3 binding with [(125)I]7-OH-PIPAT: evidence for the presence of D3 receptors on dopaminergic and nondopaminergic cell bodies and terminals. J Pharmacol Exp Ther 295:1223–1231
Starke K, Gothert M, Kilbinger H (1989) Modulation of neurotransmitter release by presynaptic autoreceptors. Physiol Rev 69:864–989
Tam SY, Elsworth JD, Bradberry CW, Roth RH (1990) Mesocortical dopamine neurons: high basal firing rate frequency predicts tyrosine dependence of dopamine synthesis. J Neural Transm 81:97–110
Tanaka T, Vincent SR, Nomikos GG, Fibiger HC (1992) Effect of quinine on autoreceptor-regulated dopamine release in the rat striatum. J Neurochem 59:1640–1645
Tyler CB, Galloway MP (1992) Acute administration of amphetamine: differential regulation of dopamine synthesis in dopamine projection fields. J Pharmacol Exp Ther 261:567–573
Wang J, Lou H, Pedersen CJ, Smith AD, Perez RG (2009) 14-3-3zeta contributes to tyrosine hydroxylase activity in MN9D cells: localization of dopamine regulatory proteins to mitochondria. J Biol Chem 284:14011–14019
Waymire JC, Haycock JW (2002) Lack of regulation of aromatic l-amino acid decarboxylase in intact bovine chromaffin cells. J Neurochem 81:589–593
Westerink BH, De Vries JB (2001) A method to evaluate the diffusion rate of drugs from a microdialysis probe through brain tissue. J Neurosci Methods 109:53–58
Westerink BH, Kawahara Y, De Boer P, Geels C, De Vries JB, Wikstrom HV, Van Kalkeren A, Van Vliet B, Kruse CG, Long SK (2001) Antipsychotic drugs classified by their effects on the release of dopamine and noradrenaline in the prefrontal cortex and striatum. Eur J Pharmacol 412:127–138
Wolf ME, Roth RH (1990) Autoreceptor regulation of dopamine synthesis. Ann N Y Acad Sci 604:323–343, 323–343
Wu Q, Reith ME, Walker QD, Kuhn CM, Carroll FI, Garris PA (2002) Concurrent autoreceptor-mediated control of dopamine release and uptake during neurotransmission: an in vivo voltammetric study. J Neurosci 22:6272–6281
Wurtman RJ, Larin F, Mostafapour S, Fernstrom JD (1974) Brain catechol synthesis: control by brain tyrosine concentration. Science 185:183–184
You ZB, Herrera-Marschitz M, Nylander I, Goiny M, O’Connor WT, Ungerstedt U, Terenius L (1994) The striatonigral dynorphin pathway of the rat studied with in vivo microdialysis—II. Effects of dopamine D1 and D2 receptor agonists. Neuroscience 63:427–434
Zhang H, Sulzer D (2012) Regulation of striatal dopamine release by presynaptic auto- and heteroreceptors. Basal Ganglia 2:5–13
Acknowledgments
This work was funded by MERIT award 1 I01 BX000381-01 from the Medical Research Service of the Department of Veterans Affairs. There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brodnik, Z., Double, M. & Jaskiw, G.E. Presynaptic regulation of extracellular dopamine levels in the medial prefrontal cortex and striatum during tyrosine depletion. Psychopharmacology 227, 363–371 (2013). https://doi.org/10.1007/s00213-013-2977-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-013-2977-0