Abstract
Rationale
The rat fear-potentiated startle (FPS) paradigm is a translational model of conditioned fear involving central amygdala pathways of the brain. Hypothalamic orexin neurons have input–output projections to the amygdala; they modulate vigilance and stress-related responses.
Objective
To investigate whether the transient pharmacological blockade of orexin receptors moderates the conditioned fear response.
Methods
F344 rats received acute oral treatment with the dual orexin receptor antagonist almorexant (30–300 mg/kg) or with one of the clinically effective anxiolytics diazepam (1–10 mg/kg), buspirone (10–100 mg/kg), fluoxetine (3–30 mg/kg), and sertraline (10–100 mg/kg). Drug effects on startle responses were assessed in both fear- and non-fear-conditioned rats; on forepaw grip and horizontal wire motor performance, and on elevated plus maze (EPM) behavior.
Results
Diazepam and almorexant both dose-dependently decreased FPS in the presence of the fear-conditioned stimulus (CS; light) more prominently than background startle in absence of the CS (dark). Diazepam induced myorelaxation and reduced startle responses in control non-fear-conditioned rats. Almorexant had no myorelaxant effects and left startle responses under light in non-fear-conditioned rats intact. On the EPM, diazepam showed anxiolytic-like effects, almorexant not. Buspirone demonstrated anxiolytic-like effects on FPS by simultaneously reducing CS-related startle and increasing no-CS-background startle. Fluoxetine did not affect FPS, whereas sertraline showed anxiogenic-like effects.
Conclusions
Almorexant reduced FPS, but did not affect EPM behavior. Almorexant’s overall pattern of effects on FPS was comparable to but less pronounced than that of the anxiolytic benzodiazepine diazepam. The endogenous orexin system actively contributes to fear-conditioned startle reactions in the rat.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acoustic startle is a reflex that is prominently influenced by the emotional and affective states of the individual under test or in natural conditions. It has gained much popularity as a reliable and objective measure of anxiety and fear that can be consistently detected in both humans and animals, thus serving as an important translational research tool (Grillon and Baas 2003). Fear- and anxiety-potentiated startle responses can be evoked in laboratory settings such as in the fear-potentiated startle (FPS) and light-enhanced startle paradigms in both rodents (Brown et al. 1951; Walker and Davis 1997a, b) and humans (Grillon and Baas 2003; Grillon et al. 1997). Acoustic startle responses to adverse emotional stimuli are also exaggerated in anxious rat strains (Steiner et al. 2011a) and in human anxiety patients, including post-traumatic stress disorder (PTSD) and panic disorder patients (Grillon et al. 1994; Grillon and Morgan 1999; Lissek et al. 2008; Morgan et al. 1995; Pole et al. 2003).
The FPS paradigm (Brown et al. 1951) is based on classical conditioning in which subjects are trained to associate a neutral conditioned stimulus (CS) with a noxious unconditioned stimulus (US), such as a mild foot-shock, which is presented in combination with the CS. Once conditioned, subjects that are later exposed to the CS alone show fear responses in expectation of the noxious US (which is actually not delivered this time). The evoked state of fear is objectively measured by comparing the startle responses to loud noise stimuli presented alongside the CS to the startle responses in the absence of the CS. The FPS response is a sensitive measure of conditioned fear of imminent threat, which is an underlying component of several anxiety disorders including panic, specific phobia, and PTSD (Grillon 2008). The predictive validity of the FPS paradigm derives from a number of rodent studies demonstrating the efficacy of anxiolytic benzodiazepines including diazepam, alprazolam, flurazepam, chlordiazepoxide, and midazolam (Berg and Davis 1984; Davis 1979; Hijzen and Slangen 1989; Joordens et al. 1996; Steiner et al. 2011a; Winslow et al. 2007), as well as of atypical anxiolytics, such as the serotonin (5-HT) 1A receptor partial agonist buspirone (Commissaris et al. 2004; Kehne et al. 1988; Mansbach and Geyer 1988; Risbrough et al. 2003). Although selective serotonin reuptake inhibitors (SSRIs) are also frequently employed in the clinics, they have yet to be satisfactorily investigated in the FPS in rodents (Joordens et al. 1996).
The orexin system of the brain, consisting of the orexin-A and orexin-B peptides (OX-A, OX-B) and their respective receptors, orexin receptor type 1 (OXR-1) and orexin receptor type 2 (OXR-2), is functionally implicated in the regulation of wakefulness, vigilance, and arousal (Sakurai 2007). Recent genetic and pharmacological data suggest an additional role for the orexin system in the regulation of mood (Rainero et al. 2011; Scott et al. 2011), anxiety (Johnson et al. 2010; Li et al. 2010; Suzuki et al. 2005), and autonomous and endocrine stress processing (Dun et al. 2000; Kayaba et al. 2003; Shahid et al. 2011; Spinazzi et al. 2006). Anatomically, orexin neurons project from the lateral hypothalamus to key structures involved in the emotional processing of aversive stimuli, such as the amygdala (Bisetti et al. 2006), the bed nucleus of the stria terminalis (Schmitt et al. 2011), and the periaqueductal gray (PAG) (Baldo et al. 2003). Inversely, orexin neurons also receive inputs from the same regions (Sakurai et al. 2005; Yoshida et al. 2006) and thus, being located at the interface of input and output signals, are thought to help coordinate the body’s physiological and behavioral response to anxiety- and fear-evoking stimuli.
Certain dual orexin receptor antagonists, such as almorexant (IC50 of 16 nM for human OXR-1; IC50 of 15 nM for human OXR-2 (Brisbare-Roch et al. 2007)), effectively cross the blood–brain-barrier, and transiently and reversibly, block both orexin receptors at neural projection sites of the orexin wake system in the brain. Single oral administration of almorexant in rats, dogs, and humans decreases wakefulness and increases both non-rapid eye movement and rapid eye movement (REM) sleep time in physiological proportions (Brisbare-Roch et al. 2007).
In addition to enabling sleep, almorexant has been shown to reduce stress-induced sympathetic activation in rats (Furlong et al. 2009) and, when given chronically, to exert antidepressant activity in mice (Nollet et al. 2011). In order to further investigate the role played by the orexin system in modulating fear-conditioned reactions, we tested almorexant in the FPS paradigm in the F344 rat strain (Nicolas and Prinssen 2006; Steiner et al. 2011a) and compared it with the approved anxiolytics diazepam (a benzodiazepine), buspirone (a 5-HT1A receptor partial agonist), and fluoxetine and sertraline (SSRIs). We also investigated drug effects on the startle response in non-fear-conditioned rats, on muscular strength and on spontaneous behavior in the elevated plus maze (EPM).
Methods
Animals
Male F344 rats (for the startle experiments) and Sprague–Dawley rats (for the elevated plus maze experiments) were purchased at 8–10 weeks of age from Harlan (Horst, The Netherlands). They were housed in groups of four in the animal facility under standard housing conditions with ad libitum food and water and under a regular 12:12 h light/dark schedule (lights on at 06:00 h). Following at least 1 week of habituation to the animal facilities, rats weighed between 240 and 260 g at the start of experiments. Experiments were performed during the light phase between 11:00 h and 17:00 h. A total of 60 F344 rats were used for the FPS experiments, with 12 rats per drug tested. A total of 16 rats were used for the non-fear-conditioned control startle experiment and the grip strength and horizontal wire tests. A total of 80 Sprague–Dawley rats were used for the EPM experiment. Experimental procedures were approved by the local Veterinary Office and adhered strictly to Swiss federal regulations on animal experimentation.
Drugs and pharmacology
All drugs were freshly dissolved prior to use in vehicle (polyethylene glycol 400) and administered via oral gavage (p.o.) in a volume of 5 ml/kg body weight. Almorexant ((2R)-2-{(1S)-6,7-dimethoxy-1-[2-(4-trifluoromethylphenyl)-ethyl]-3,4-dihydro-1H-isoquinolin-2-yl}-N-methyl-2-phenyl-acetamide) hydrochloride (Actelion Pharmaceuticals Ltd.) and sertraline hydrochloride (Jinan ShangTai Chemical Technology, Jinan City, China) were administered 1 h before testing. Diazepam (Actelion Pharmaceuticals Ltd.) and buspirone hydrochloride (Sigma, Steinheim, Germany) were administered 30 min before testing. Fluoxetine hydrochloride (Apin Chemicals, Abingdon, UK) was administered 45 min before testing. Doses of all drugs except sertraline were calculated as the free base. Pretreatment times and doses were chosen based on the particular pharmacokinetic/pharmacodynamic profiles of each drug.
Startle apparatus
Startle responses were measured using six individual, ventilated, sound-attenuating startle chambers (32 × 32 × 48 cm; SR-LAB system, San Diego Instruments, San Diego, CA, USA) controlled by SR-LAB software (San Diego Instruments) in parallel. Each chamber contained a stabilimeter device consisting of a clear, plastic, cylindrical animal enclosure (10 cm diameter, 20 cm length) mounted on a plastic base. A wide-band speaker mounted 24 cm above the rat provided the background noise (62 dB) and the startle-eliciting white noise stimuli. Startle responses (movements of a rat within the enclosure) were transduced by a piezoelectric accelerometer mounted below the cylinder and then digitized, rectified, and recorded by an interfacing computer assembly as voltage output samples per millisecond. The average of the first 100 1-ms readings, starting at the onset of each startle-eliciting noise stimulus, was used as the dependent measure. Calibration procedures were performed before each test to ensure consistent levels of loudspeaker performance and stabilimeter sensitivity among the different startle chambers. Electric foot-shocks were delivered through a removable stainless steel grid floor (5 mm diameter stainless steel bars spaced 1 cm apart) within the animal enclosure cylinder via a connected, external, programmable animal shocker (San Diego Instruments).
Fear-condition training
For the training of conditioned fear, F344 rats were placed in the animal enclosures of the startle chambers and were allowed 5 min to acclimate in the dark. Rats were subsequently presented with a CS (light) for 3.7 s that co-terminated in the last 0.5 s with a 0.4 mA electric foot-shock (US). Fifteen CS–US pairings (trials) were presented, using an average inter-trial interval of 30 s. Training sessions (consisting of the 5 min acclimation followed by the 15 trials) were repeated twice a day for either one or two consecutive days (see section below on experiment 1).
Fear-potentiated startle testing
Twenty-four hours after the last fear-condition training, F344 rats were placed in the startle chambers and allowed to acclimatize for 5 min. They were then presented with 10-ms-long startle-eliciting white noise stimuli of 90, 100, or 110 dB intensity. Stimuli were presented 20 times at each noise intensity for a total of 60 test trials per rat, using an average inter-stimulus interval of 30 s (range, 25–35 s). To test for fear-potentiated startle responses, half of the 20 noise stimuli (per intensity) were preceded by a 3.2 s presentation of the CS (light), and the other half were presented in darkness (no-CS trials). Therefore, the 60-trial test session of each rat comprised six types of test trials (presentation of one of three noise intensities in either the absence or presence of the CS). The test sessions were divided into six-trial blocks, in which each trial type was presented at random.
Experiment 1: effects of diazepam, buspirone, fluoxetine, sertraline, and almorexant on FPS
Twelve F344 rats were randomly assigned to each drug (diazepam, buspirone, fluoxetine, sertraline, almorexant) and tested in separate experiments. Each experiment was performed in a Latin-square cross-over design over 4 weeks, with one fear conditioning training, followed 24 h later by the FPS test, per week according to a previously published protocol (Steiner et al. 2011a). During the first week, fear conditioning training to establish fear memory lasted 2 days. Over the following 3 weeks, fear conditioning training to prevent fear memory extinction was given only 1 day per week. Every week, rats received acute drug treatment 30, 45, or 60 min (depending on the pharmacokinetic properties, see above) before each FPS test. Due to the Latin-square cross-over design, each rat received each dose of the assigned drug once. One rat in the diazepam experiment, one rat in the buspirone experiment, and two rats in the sertraline experiment were removed from the statistical analyses because of the electronic failure of certain startle chambers to properly record the responses of one particular startle test.
Experiment 2: effects of high doses of diazepam, buspirone, sertraline, and almorexant on baseline startle reactivity in non-fear-conditioned rats and on forced motor performance
In this control experiment, F344 rats did not undergo fear-condition training, but they were subjected to a startle test session identical to the FPS test session described above in order to investigate drug effects on baseline startle under dark and light conditions. For each drug that had affected background startle responses under no-CS conditions in the FPS paradigm (i.e., almorexant, diazepam, sertraline, buspirone), we selected the most effective dose (strongest effect on no-CS startle) to be additionally tested under the current control conditions. This was the highest dose tested for almorexant, diazepam, and sertraline, but the second highest dose for buspirone. Five treatment types (vehicle, almorexant 300 mg/kg; diazepam 10 mg/kg; sertraline 100 mg/kg; and buspirone 30 mg/kg) were assessed in 16 rats using a 5-week cross-over design (one startle test session per week). At the start of the experiment, rats were randomly assigned to receive vehicle (−60 min) or a particular drug treatment (−30 to −60 min) before startle testing, and the treatment was alternated every week so that in the end each rat had received each drug treatment only once. There was no indication in historical data from our laboratory that alternating pre-treatment time between 30 and 60 min has any influence on startle reactivity. Thus, to reduce animal numbers and to allow direct intra-animal comparisons between the different treatment groups, only one vehicle group (60 min pretreatment time) was included in the experiment.
In order to additionally evaluate potential myorelaxant effects of the selected treatments, which may also have influenced baseline startle reactivity, all F344 rats were subsequently tested in the forepaw grip strength test followed by the horizontal wire test immediately after the termination of each startle test session. The grip strength test used a triangular bar 2 mm in diameter and 5 cm wide connected to a digital strain gauge (BIOSEB, Vitrolles, France) to measure graded changes in the forelimb grip strength of rats. Animals held by the tail grasped the bar and were then gently pulled away from it in a smooth, steady motion, until they released the bar. The strain gauge measured the force [grams] required to break the animal's grip. Three readings were taken for each animal, and the average force required was recorded as the individual grip strength score of that rat. The horizontal wire test used a horizontal wire bar (70 cm long; diameter 0.5 cm) which was fixed at a height of 50 cm above the floor. Rats were gently picked up by the tail and allowed to grasp the wire (close to the middle) with their forepaws. Time spent on the wire was recorded with a cut-off time at 60 s. The performance of the rat on the wire was furthermore evaluated as follows: A score of 0 if the rat was unable to grip the wire or fell off immediately; a score of 1 if the rat gripped the wire, hung on to the wire with its forelimbs, and was able to support its body weight (head below the wire); a score of 2 if the rat was able to support its body weight and, in addition, was able to raise its head above the bar; a score of 3 if the rat was able to place at least one hind paw on the wire; a score of 4 if the rat was able to climb up the wire and to traverse the wire with forepaws and hind paws on the wire. Each rat was placed on the wire three times, and the best value from the three readings (time spent on the wire and rated number score) was recorded as the final test score.
Experiment 3: effects of diazepam and almorexant on behavior in the elevated plus maze (EPM)
Because almorexant showed comparable, but less pronounced, anxiolytic-like effects in the FPS paradigm than diazepam, both drugs were additionally compared in another anxiety paradigm, the EPM. The EPM (Viewpoint, Lyon, France) had runways 11 cm wide and 50 cm long, was made of infrared light translucent plastic, and was placed on an IR-back-lit floor. The EPM was divided in five different areas (two open arms, two closed arms, and one center part). The closed arms had black makrolon plastic walls 15 cm high. Light conditions during testing were 15 lux in the open arms. Upon testing, diazepam- or almorexant-treated Sprague–Dawley rats were placed at the end of an open arm facing the middle of the EPM, and rats were allowed to freely explore the EPM for 5 min. Behavior was recorded via automated video-tracking (Viewpoint, Lyon, France). The tracking system recorded the time spent (seconds), the number of entries in the different arms of the maze and the distance moved (meters). Forty rats were used for the diazepam experiment, another 40 for the almorexant experiment (n = 10 rats per dose group). One rat of the almorexant 100 mg/kg dose group was removed from the analysis because it fell down from the EPM.
Statistical analysis
Startle amplitudes were averaged over the three noise intensities (90, 100, and 110 dB) and over the ten stimuli presented per noise intensity and condition (CS, no-CS, dark, light). For all startle experiments, the main drug effects were analyzed using analyses of variance (ANOVAs) with repeated measures on drug treatment and fear-potentiation (CS and no-CS) or light condition (light and dark) followed by Newman–Keuls post hoc tests where appropriate. In subsequent analyses for the FPS experiment, drug effects were analyzed separately for CS and no-CS conditions by one-way ANOVA with repeated measures on drug treatment followed by Newman–Keuls post hoc tests. Startle reactions in the dark in rats which either had or had not undergone previous fear-condition training were compared with the unpaired Student’s t test. Drug effects on grip strength were analyzed by one-way ANOVA with repeated measures on drug treatment followed by the Newman–Keuls post hoc test. Wire hanging test scores and time spent on the wire were analyzed by the non-parametric Friedman test with repeated measures on drug treatment followed by Dunn’s multiple comparison tests. Drug effects on behavioral measures in the EPM were analyzed by one-way ANOVA followed by the Newman–Keuls post hoc test or planned comparisons where appropriate. Differences were considered statistically significant if p < 0.05. Data are presented as mean ± SEM.
Results
Experiment 1: effects of diazepam, buspirone, fluoxetine, sertraline, and almorexant on FPS
The mean startle amplitudes recorded during FPS testing as a function of increasing doses of diazepam, buspirone, fluoxetine, sertraline, and almorexant are shown in Fig. 1. The corresponding statistical ANOVA results are summarized in Table 1. A main effect for the presentation of the CS was detected for each of the five separately conducted experiments, indicating robust and reliable FPS in F344 rats according to previous observations (Steiner et al. 2011a). Main drug effects were detected for diazepam, buspirone, sertraline, and almorexant, but not for fluoxetine, indicating that four of the five drugs had an overall effect on startle reactivity under CS and no-CS conditions. Furthermore, significant drug × fear-potentiation interactions for diazepam (Fig. 1a) and almorexant (Fig. 1e) indicated more prominent drug effects on reducing CS-induced startle than background startle responses under no-CS conditions, reflecting anxiolytic-like effects. A significant drug × fear-potentiation interaction for buspirone indicated that the drug both decreased CS-induced startle responses and increased background startle responses under no-CS conditions at the same time (Fig. 1b), which also has been interpreted as an anxiolytic-like effect (Kehne et al. 1988; Mansbach and Geyer 1988). A significant drug × fear-potentiation interaction for sertraline, however, indicated that the drug more markedly increased CS-induced startle than background startle responses under no-CS conditions (Fig. 1d), reflecting an anxiogenic-like response. Finally, for fluoxetine no drug × fear-potentiation interaction was found (Fig. 1c).
Effects of diazepam (a), buspirone (b), fluoxetine (c), sertraline (d), and almorexant (e) on the fear-potentiated startle (FPS) response. F344 rats were orally treated acutely before the FPS test with vehicle (0 mg/kg) or increasing doses of the respective drugs. Data are presented as the mean startle amplitudes (±SEM) recorded during the presentation of noise stimuli under no-CS (dark) or CS (light) conditions. n = 10–12 rats per tested drug in a within-subjects cross-over design. *p < 0.05, **p < 0.01, ***p < 0.001 vs. the respective vehicle (0 mg/kg) in presence of the CS; # p < 0.05, ## p < 0.01, ### p < 0.001 vs. the respective vehicle (0 mg/kg) in absence of the CS (no-CS); Newman–Keuls post hoc test following ANOVA. CS conditioned stimulus. Please not the different Y-axis scale for sertraline
More detailed one-way ANOVAs of drug effects (followed by Newman–Keuls post hoc tests), for CS and no-CS conditions separately, revealed the following: Compared with vehicle, diazepam strongly reduced the startle reflex under CS conditions at 3 mg/kg (p < 0.001) and 10 mg/kg (p < 0.001), whereas the startle reflex under no-CS conditions was only reduced at 10 mg/kg (p < 0.001; Fig. 1a). Buspirone significantly reduced the startle reflex under CS conditions at 100 mg/kg (p < 0.01), whereas the startle reflex under no-CS conditions was increased at 10 mg/kg (p < 0.05), 30 mg/kg (p < 0.001), and 100 mg/kg (p < 0.01; Fig. 1b). Fluoxetine did not influence the startle reflex under either CS conditions (p = 0.09) or no-CS conditions (p = 0.26; Fig. 1c). Sertraline significantly increased the startle reflex under both CS and no-CS conditions at 30 mg/kg (p < 0.01) and 100 mg/kg (p < 0.001; Fig. 1d). Almorexant significantly reduced the startle reflex under CS conditions at 100 mg/kg (p < 0.05) and 300 mg/kg (p < 0.01), whereas the startle reflex under no-CS conditions was only reduced at 300 mg/kg (p < 0.001; Fig. 1e).
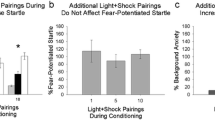
Experiment 2: effects of high doses of diazepam, buspirone, sertraline, and almorexant on baseline startle reactivity in non-fear-conditioned rats and on forced motor performance
The mean startle amplitudes recorded in non-fear-conditioned rats under light and dark conditions in response to almorexant (300 mg/kg), diazepam (10 mg/kg), sertraline (100 mg/kg), and buspirone (30 mg/kg) treatment are shown in Fig. 2a. As expected, the mean startle amplitude in the dark in non-fear-conditioned vehicle-treated rats (27.2 ± 3.7 mV; Fig. 2a) was significantly lower than the mean startle amplitude averaged across all five different vehicle-treated rat cohorts in the FPS paradigm (37.9 ± 1.6 mV; Fig.1) under no-CS (dark) conditions (t 70 = 2.97, p < 0.01). This suggests an additional component of either contextual fear or “background anxiety,” which can be elicited by the intermittent presentation of the fear-evoking CS stimuli during FPS testing that contributed to the startle reactivity in the dark under no-CS conditions in previously fear-conditioned rats, according to earlier observations (Missig et al. 2010; Steiner et al. 2011a).
Effects of acute oral treatment of non-fear-conditioned F344 rats with vehicle, almorexant (300 mg/kg), diazepam (10 mg/kg), sertraline (100 mg/kg), and buspirone (30 mg/kg) on mean startle amplitudes under dark and light conditions (a), on forepaw grip strength (b), and on horizontal wire performance (c). Data are presented as the mean + SEM. n = 16 rats in a within-subjects cross-over design. For a, *p < 0.05 vs. the respective startle response in the dark, # p < 0.05 vs. vehicle tested under dark conditions, + p < 0.05 vs. vehicle tested under light conditions. For b, c, ***p < 0.001 vs. vehicle. Newman–Keuls post hoc test following ANOVA. Dotted lines are placed at the startle amplitude level of vehicle-treated rats under dark and light conditions, respectively, to allow better comparability with the other drug effects
ANOVA of the startle responses in non-fear-conditioned rats revealed a main effect for the presentation of light (F 1,15 = 16.8, p < 0.001). This indicated that startle reflexes in response to noise stimuli which were preceded by short (3.2 s) light presentations were also slightly stronger than startle reflexes in response to noise stimuli received under dark conditions, even if rats had not previously been trained to associate the light with an electric foot-shock. This phenomenon has been described before and is termed “startle-potentiated startle” because it is thought to reflect the rat's conditioning to the short light stimuli preceding the startle-eliciting noise stimuli (Commissaris et al. 2004; Leaton and Cranney 1990).
Main effects for drug (F4,60 = 30.3, p < 0.001) and for the drug × light interaction (F4,60 = 7.48, p < 0.001) indicated that the four tested drugs had different effects on startle reflexes under light and dark conditions in non-fear-conditioned rats. Newman–Keuls post hoc test comparisons revealed the following: In comparison to vehicle, almorexant 300 mg/kg reduced the startle reflex only under dark (p < 0.05) but not light conditions. Diazepam 10 mg/kg reduced the startle reflex under both dark (p < 0.05) and light conditions (p < 0.001), abolishing the dark–light difference. Sertraline 100 mg/kg increased startle reflexes under both dark (p < 0.05) and light conditions (p < 0.001) proportionally, leaving the initial dark–light difference intact. Buspirone 30 mg/kg only increased startle reflexes under dark (p < 0.001) but not light conditions, abolishing the dark–light difference.
In order to exclude potential unspecific effects of the treatments on muscle tonus, which could influence the startle reflex, we also tested almorexant (300 mg/kg), diazepam (10 mg/kg), sertraline (100 mg/kg), and buspirone (30 mg/kg) on the forepaw grip strength and horizontal wire tests (Fig. 2b,c). ANOVA of grip strength revealed a significant main effect for drug treatment (F4,60 = 16.0, p < 0.001), and post hoc analysis revealed that diazepam 10 mg/kg significantly reduced forepaw grip strength (p < 0.001; Fig. 2b). Similarly, Friedman analysis of the horizontal wire test score also revealed a significant main effect for drug (Friedman statistics = 35.7, p < 0.001), and post hoc analysis revealed that diazepam 10 mg/kg significantly reduced the horizontal wire score (p < 0.001; Fig. 2c). Analysis of the horizontal wire test time revealed results (data not shown) similar to those observed for the wire test score.
Experiment 3: effects of diazepam and almorexant on behavior in the elevated plus maze
The different behavioral parameters recorded in the EPM in diazepam- and almorexant-treated rats are shown in Fig. 3. Diazepam treatment dose-dependently increased the time spent on the open arms (F3,44 = 3.04, p < 0.05; Fig. 3a), the number of open arm entries (F3,44 = 8.13, p < 0.001; Fig. 3b), and the ratio between open arm and total arm entries (F3,44 = 6.95, p < 0.001; Fig. 3c), with effective doses of 3 mg/kg (p < 0.05) and 10 mg/kg (p < 0.05). Distance moved was also affected (F3,44 = 3.47, p < 0.05; Fig. 3d) with the 3 mg/kg dose of diazepam increasing locomotion (p < 0.05). Almorexant treatment, however, did not affect any of those parameters (F3,35 < 1.4, p > 0.26; Fig. 3e-h).
Effects of diazepam (a–d) and almorexant (e–h) on behavior in the elevated plus maze (EPM). Sprague–Dawley rats were orally treated acutely before exposure to the EPM test with vehicle (0 mg/kg) or increasing doses of diazepam and almorexant. Data are presented as the mean + SEM. n = 11–12 rats per treatment group. *p < 0.05 vs. the respective vehicle. OA open arm, TA total arm
Discussion
The aim of the present study was to explore the contribution of the orexin system to the modulation of cued fear-conditioned acoustic startle responses by comparing the dual OXR antagonist almorexant to clinically approved anxiolytics of different classes. We found that diazepam, buspirone, and almorexant exerted anxiolytic-like effects. SSRIs had no anxiolytic-like properties after single acute administrations. Interestingly, each drug presented its own particular pattern of activity on startle responses under CS and no-CS conditions in the FPS paradigm and on startle responses under light and dark conditions in non-fear-conditioned rats.
Diazepam strongly reduced CS-induced startle at oral doses of 3 and 10 mg/kg. It also reduced background startle responses under no-CS conditions at 10 mg/kg. This appears to be a FPS profile typical of benzodiazepines (Joordens et al. 1996; Steiner et al. 2011a). Upon further evaluation in non-fear-conditioned rats, 10 mg/kg of diazepam also decreased startle reactivity under both dark and light conditions and, in fact, completely abolished the dark–light difference. Benzodiazepines have both anxiolytic and sedative, muscle-relaxant effects (Tallman et al. 1980), and it is often difficult to separate these characteristics. However, our findings that 10 mg/kg of diazepam effectively reduced forepaw grip strength and the horizontal wire score suggest that the overall reduced startle reactivity at that dose is mainly a consequence of muscle-relaxant effects which probably non-selectively impaired the startle reflex.
Buspirone also reduced CS-induced startle at an oral dose of 100 mg/kg. At the same time, buspirone increased background startle reactivity under no-CS conditions at all doses tested, with the strongest effect achieved with 30 mg/kg. Upon further investigation in non-fear-conditioned rats, we observed that 30 mg/kg of buspirone also increased baseline startle responses under dark conditions which is consistent with previous reports and believed to be a consequence of the partial 5-HT1A receptor agonism of buspirone (Commissaris et al. 2004; Kehne et al. 1988; McQueen et al. 2001). The reduction of the CS-induced startle response which occurred only at high dose is, however, likely the result of a target engagement different from 5-HT1A receptors, such as dopamine D2 receptors or others for which buspirone shows weak affinity (Eison and Temple 1986; McQueen et al. 2001).
Fluoxetine and sertraline had different effects on FPS. Fluoxetine had no significant effects despite an apparent trend towards increasing CS-induced startle responses. Sertraline, however, dose-dependently increased both CS-induced and background startle under no-CS conditions with an overall stronger effect on CS-induced startle, indicating acute anxiogenic potential. The only SSRI that has so far been tested acutely in the rat FPS paradigm is fluvoxamine, which showed no effects (Joordens et al. 1996), similar to our results with fluoxetine. However, SSRIs sometimes exacerbate symptoms of conditioned fear upon acute treatment both in humans (Grillon et al. 2007) and rats (Burghardt et al. 2007), which may explain the observed anxiogenic-like effects of sertraline. In fact, when anxiety patients begin SSRI treatment, the dose is often up-titrated or they are prescribed benzodiazepines concomitantly to avoid initial adverse reactions (Sinclair et al. 2009). The effects of chronic administration of SSRIs in the FPS paradigm await further investigation.
Almorexant decreased CS-induced startle at oral doses of 100 and 300 mg/kg. At the highest dose of 300 mg/kg, almorexant also decreased background startle under no-CS conditions. With this FPS profile, almorexant showed anxiolytic-like properties comparable to diazepam, although it was less effective at reducing CS-induced startle responses at doses which did not simultaneously affect background startle responses under no-CS conditions. With regard to the similarity of the overall pattern of the FPS responses of diazepam and almorexant, it is interesting that reduced c-Fos expression was observed in orexin neurons after mice had been intraperitoneally injected with low and high doses of diazepam (Panhelainen and Korpi 2012). This suggests that some diazepam-mediated effects may involve the suppression of orexin neuron activity. Comparing almorexant and diazepam on the elevated plus maze, however, clearly demonstrated that, in this test, only diazepam showed anxiolytic-like effects. Thus, here, it seems very unlikely that diazepam would rely on inhibiting orexin neuron activity for modulating anxiety-like behavior on the elevated plus maze.
As opposed to diazepam, almorexant left the horizontal wire and grip strength performance unaffected. In contrast to benzodiazepines or other GABAA receptor modulators, when given at high doses, dual OXR antagonists do not impair the ability of rodents to respond naturally in stimulating environmental conditions such as the Morris water maze, tail suspension, or rotarod tasks (Di Fabio et al. 2011; Dietrich and Jenck 2010; Nollet et al. 2011; Steiner et al. 2011b). Thus, we conclude that the effects of almorexant in the FPS paradigm were not confounded by myorelaxant actions. Moreover, in non-fear-conditioned rats, almorexant decreased startle responses in the dark but not in the light, which suggests that the pharmacological OXR blockade did not interfere with neuronal motor circuits of the startle reflex pathway per se. The reduction of startle responses under no-CS conditions induced by almorexant in the FPS paradigm, thus, likely reflects reduced contextual fear or “background anxiety” (Missig et al. 2010). This is in line with recent experiments demonstrating that almorexant treatment reduced cardio-excitatory responses to contextual fear in rats (Furlong et al. 2009). Finally, the finding that almorexant reduced non-fear-conditioned startle responses in the dark corresponds with its vigilance-decreasing effects under low-stimulating (home cage) environmental conditions (Brisbare-Roch et al. 2007).
This is the first study investigating the role of the orexin system in cued fear-conditioned reactions. Previous studies have shown anatomical evidence for orexin fiber and receptor expression in the central amygdala (Cluderay et al. 2002; Peyron et al. 1998), a critical region for the processing of FPS (Fendt and Fanselow 1999; Hitchcock and Davis 1987). Bisetti et al. (2006) have further functionally demonstrated that both OX-A and OX-B excite neurons of the central medial amygdala in ex vivo rat brain slices, and Sakamoto et al. (2004) found that CeA neurons become activated upon intracerebroventricular OX-A injection in the rat. Reciprocally, fibers originating in the CeA also project back to OX neurons in the lateral hypothalamus (Nakamura et al. 2009; Sakurai et al. 2005; Yoshida et al. 2006). While this whole orexin–CeA circuit likely mediates some of the cardiorespiratory responses to stress and fear (Furlong et al. 2009; Johnson et al. 2010; Zhang et al. 2009), our current findings suggest that it may also contribute to cued fear-conditioned startle responses. It is also worth noting that narcoleptic patients, which are often orexin-deficient, have reduced amygdala activity upon aversive conditioning and do not exhibit startle potentiation during unpleasant stimuli (Khatami et al. 2007; Ponz et al. 2010). Further evidence that anxiety-like behavior can be modulated by orexin signaling in the CeA stems from a recent study showing anxiogenic effects of direct intra-CeA administrations of OX-A and OX-B in the elevated-plus maze and light–dark (LD) tests in Syrian golden hamsters (Avolio et al. 2011). OXR-1 and OXR-2 knockout mice, however, did not display altered anxiety-like behavior in the very same tests (Scott et al. 2011), questioning an activation of the endogenous orexin system during EPM or LD exposure. Similarly, almorexant-treated rats did not show altered behavior in the EPM. Yet, it may still be possible that OXR blockade may have revealed anxiolytic-like effects under more aversive conditions (e.g., stressing the animals before EPM exposure or providing higher intensity light during EPM testing). Orexin neuron firing is increased during wakefulness, and it could be hypothesized that orexin neurons become even more activated during emotionally stressful states (Kuwaki et al. 2010). Perhaps, this may explain why almorexant only showed anxiolytic-like effects during the supposedly more aversive conditioned fear testing.
Regarding the effects of almorexant, a dual OXR antagonist, in the FPS paradigm, one may wonder which type of OXR is responsible for regulating the fear-conditioned startle response. From an anatomical point of view, mRNA and protein of both receptors, OXR-1 and OXR-2, have been found co-expressed in the amygdala and in other brain regions influencing FPS such as the ventromedial hypothalamus and PAG (Cluderay et al. 2002; Hervieu et al. 2001; Lu et al. 2000; Marcus et al. 2001; Zhao et al. 2009). Thus, it is difficult to make any prediction without additional functional evidence. It will be up to future pharmacological studies using selective antagonists to decipher the particular role of each of the two OXRs for conditioned fear.
Our present data support the view that the orexin system integrates into the functional brain circuitry responsible for the processing of stressful and aversive events, and we show that endogenous orexin receptor signaling actively contributes to cued fear-conditioned startle reactions in the rat. Whether this has any implication for the clinical use of OXR antagonists remains speculative in light of still only a few rodent studies showing anxiolytic-like potential of such compounds (Furlong et al. 2009; Johnson et al. 2012; Johnson et al. 2010).
References
Avolio E, Alo R, Carelli A, Canonaco M (2011) Amygdalar orexinergic-GABAergic interactions regulate anxiety behaviors of the Syrian golden hamster. Behav Brain Res 218:288–295
Baldo BA, Daniel RA, Berridge CW, Kelley AE (2003) Overlapping distributions of orexin/hypocretin- and dopamine-beta-hydroxylase immunoreactive fibers in rat brain regions mediating arousal, motivation, and stress. J Comp Neurol 464:220–237
Berg WK, Davis M (1984) Diazepam blocks fear-enhanced startle elicited electrically from the brainstem. Physiol Behav 32:333–336
Bisetti A, Cvetkovic V, Serafin M, Bayer L, Machard D, Jones BE, Muhlethaler M (2006) Excitatory action of hypocretin/orexin on neurons of the central medial amygdala. Neuroscience 142:999–1004
Brisbare-Roch C, Dingemanse J, Koberstein R, Hoever P, Aissaoui H, Flores S, Mueller C, Nayler O, van Gerven J, de Haas SL, Hess P, Qiu C, Buchmann S, Scherz M, Weller T, Fischli W, Clozel M, Jenck F (2007) Promotion of sleep by targeting the orexin system in rats, dogs and humans. Nat Med 13:150–155
Brown JS, Kalish HI, Farber IE (1951) Conditioned fear as revealed by magnitude of startle response to an auditory stimulus. J Exp Psychol 41:317–328
Burghardt NS, Bush DE, McEwen BS, LeDoux JE (2007) Acute selective serotonin reuptake inhibitors increase conditioned fear expression: blockade with a 5-HT(2 C) receptor antagonist. Biol Psychiatry 62:1111–1118
Cluderay JE, Harrison DC, Hervieu GJ (2002) Protein distribution of the orexin-2 receptor in the rat central nervous system. Regul Pept 104:131–144
Commissaris RL, Fomum EA, Leavell BJ (2004) Effects of buspirone and alprazolam treatment on the startle-potentiated startle response. Depress Anxiety 19:146–151
Davis M (1979) Diazepam and flurazepam: effects on conditioned fear as measured with the potentiated startle paradigm. Psychopharmacology (Berl) 62:1–7
Di Fabio R, Pellacani A, Faedo S, Roth A, Piccoli L, Gerrard P, Porter RA, Johnson CN, Thewlis K, Donati D, Stasi L, Spada S, Stemp G, Nash D, Branch C, Kindon L, Massagrande M, Poffe A, Braggio S, Chiarparin E, Marchioro C, Ratti E, Corsi M (2011) Discovery process and pharmacological characterization of a novel dual orexin 1 and orexin 2 receptor antagonist useful for treatment of sleep disorders. Bioorg Med Chem Lett 21:5562–5567
Dietrich H, Jenck F (2010) Intact learning and memory in rats following treatment with the dual orexin receptor antagonist almorexant. Psychopharmacology (Berl) 212:145–154
Dun NJ, Le Dun S, Chen CT, Hwang LL, Kwok EH, Chang JK (2000) Orexins: a role in medullary sympathetic outflow. Regul Pept 96:65–70
Eison AS, Temple DL Jr (1986) Buspirone: review of its pharmacology and current perspectives on its mechanism of action. Am J Med 80:1–9
Fendt M, Fanselow MS (1999) The neuroanatomical and neurochemical basis of conditioned fear. Neurosci Biobehav Rev 23:743–760
Furlong TM, Vianna DM, Liu L, Carrive P (2009) Hypocretin/orexin contributes to the expression of some but not all forms of stress and arousal. Eur J Neurosci 30:1603–1614
Grillon C (2008) Models and mechanisms of anxiety: evidence from startle studies. Psychopharmacology (Berl) 199:421–437
Grillon C, Baas J (2003) A review of the modulation of the startle reflex by affective states and its application in psychiatry. Clin Neurophysiol 114:1557–1579
Grillon C, Morgan CA 3rd (1999) Fear-potentiated startle conditioning to explicit and contextual cues in Gulf War veterans with posttraumatic stress disorder. J Abnorm Psychol 108:134–142
Grillon C, Ameli R, Goddard A, Woods SW, Davis M (1994) Baseline and fear-potentiated startle in panic disorder patients. Biol Psychiatry 35:431–439
Grillon C, Pellowski M, Merikangas KR, Davis M (1997) Darkness facilitates the acoustic startle reflex in humans. Biol Psychiatry 42:453–460
Grillon C, Levenson J, Pine DS (2007) A single dose of the selective serotonin reuptake inhibitor citalopram exacerbates anxiety in humans: a fear-potentiated startle study. Neuropsychopharmacology 32:225–231
Hervieu GJ, Cluderay JE, Harrison DC, Roberts JC, Leslie RA (2001) Gene expression and protein distribution of the orexin-1 receptor in the rat brain and spinal cord. Neuroscience 103:777–797
Hijzen TH, Slangen JL (1989) Effects of midazolam, DMCM and lindane on potentiated startle in the rat. Psychopharmacology (Berl) 99:362–365
Hitchcock JM, Davis M (1987) Fear-potentiated startle using an auditory conditioned stimulus: effect of lesions of the amygdala. Physiol Behav 39:403–408
Johnson PL, Truitt W, Fitz SD, Minick PE, Dietrich A, Sanghani S, Traskman-Bendz L, Goddard AW, Brundin L, Shekhar A (2010) A key role for orexin in panic anxiety. Nat Med 16:111–115
Johnson PL, Samuels BC, Fitz SD, Lightman SL, Lowry CA, Shekhar A (2012) Activation of the orexin 1 receptor is a critical component of CO(2)-mediated anxiety and hypertension but not bradycardia. Neuropsychopharmacology doi:10.1038/npp.2012.38
Joordens RJ, Hijzen TH, Peeters BW, Olivier B (1996) Fear-potentiated startle response is remarkably similar in two laboratories. Psychopharmacology (Berl) 126:104–109
Kayaba Y, Nakamura A, Kasuya Y, Ohuchi T, Yanagisawa M, Komuro I, Fukuda Y, Kuwaki T (2003) Attenuated defense response and low basal blood pressure in orexin knockout mice. Am J Physiol Regul Integr Comp Physiol 285:R581–R593
Kehne JH, Cassella JV, Davis M (1988) Anxiolytic effects of buspirone and gepirone in the fear-potentiated startle paradigm. Psychopharmacology (Berl) 94:8–13
Khatami R, Birkmann S, Bassetti CL (2007) Amygdala dysfunction in narcolepsy–cataplexy. J Sleep Res 16:226–229
Kuwaki T, Li A, Nattie E (2010) State-dependent central chemoreception: a role of orexin. Respir Physiol Neurobiol 173:223–229
Leaton RN, Cranney J (1990) Potentiation of the acoustic startle response by a conditioned stimulus paired with acoustic startle stimulus in rats. J Exp Psychol Anim Behav Process 16:279–287
Li Y, Li S, Wei C, Wang H, Sui N, Kirouac GJ (2010) Orexins in the paraventricular nucleus of the thalamus mediate anxiety-like responses in rats. Psychopharmacology (Berl) 212:251–265
Lissek S, Biggs AL, Rabin SJ, Cornwell BR, Alvarez RP, Pine DS, Grillon C (2008) Generalization of conditioned fear-potentiated startle in humans: experimental validation and clinical relevance. Behav Res Ther 46:678–687
Lu XY, Bagnol D, Burke S, Akil H, Watson SJ (2000) Differential distribution and regulation of OX1 and OX2 orexin/hypocretin receptor messenger RNA in the brain upon fasting. Horm Behav 37:335–344
Mansbach RS, Geyer MA (1988) Blockade of potentiated startle responding in rats by 5-hydroxytryptamine1A receptor ligands. Eur J Pharmacol 156:375–383
Marcus JN, Aschkenasi CJ, Lee CE, Chemelli RM, Saper CB, Yanagisawa M, Elmquist JK (2001) Differential expression of orexin receptors 1 and 2 in the rat brain. J Comp Neurol 435:6–25
McQueen DA, Overstreet DH, Ardayfio PA, Commissaris RL (2001) Acoustic startle, conditioned startle potentiation and the effects of 8-OH-DPAT and buspirone in rats selectively bred for differences in 8-OH-DPAT-induced hypothermia. Behav Pharmacol 12:509–516
Missig G, Ayers LW, Schulkin J, Rosen JB (2010) Oxytocin reduces background anxiety in a fear-potentiated startle paradigm. Neuropsychopharmacology 35:2607–2616
Morgan CA 3rd, Grillon C, Southwick SM, Davis M, Charney DS (1995) Fear-potentiated startle in posttraumatic stress disorder. Biol Psychiatry 38:378–385
Nakamura S, Tsumori T, Yokota S, Oka T, Yasui Y (2009) Amygdaloid axons innervate melanin-concentrating hormone- and orexin-containing neurons in the mouse lateral hypothalamus. Brain Res 1278:66–74
Nicolas LB, Prinssen EP (2006) Social approach-avoidance behavior of a high-anxiety strain of rats: effects of benzodiazepine receptor ligands. Psychopharmacology (Berl) 184:65–74
Nollet M, Gaillard P, Minier F, Tanti A, Belzung C, Leman S (2011) Activation of orexin neurons in dorsomedial/perifornical hypothalamus and antidepressant reversal in a rodent model of depression. Neuropharmacology 61:336-346
Panhelainen AE, Korpi ER (2012) Evidence for a role of inhibition of orexinergic neurons in the anxiolytic and sedative effects of diazepam: a c-Fos study. Pharmacol Biochem Behav 101:115–124
Peyron C, Tighe DK, van den Pol AN, de Lecea L, Heller HC, Sutcliffe JG, Kilduff TS (1998) Neurons containing hypocretin (orexin) project to multiple neuronal systems. J Neurosci 18:9996–10015
Pole N, Neylan TC, Best SR, Orr SP, Marmar CR (2003) Fear-potentiated startle and posttraumatic stress symptoms in urban police officers. J Trauma Stress 16:471–479
Ponz A, Khatami R, Poryazova R, Werth E, Boesiger P, Schwartz S, Bassetti CL (2010) Reduced amygdala activity during aversive conditioning in human narcolepsy. Ann Neurol 67:394–398
Rainero I, Ostacoli L, Rubino E, Gallone S, Picci LR, Fenoglio P, Negro E, Rosso C, De Martino P, De Marchi M, Furlan PM, Pinessi L (2011) Association between major mood disorders and the hypocretin receptor 1 gene. J Affect Disord 130:487–491
Risbrough VB, Brodkin JD, Geyer MA (2003) GABA-A and 5-HT1A receptor agonists block expression of fear-potentiated startle in mice. Neuropsychopharmacology 28:654–663
Sakamoto F, Yamada S, Ueta Y (2004) Centrally administered orexin-A activates corticotropin-releasing factor-containing neurons in the hypothalamic paraventricular nucleus and central amygdaloid nucleus of rats: possible involvement of central orexins on stress-activated central CRF neurons. Regul Pept 118:183–91
Sakurai T (2007) The neural circuit of orexin (hypocretin): maintaining sleep and wakefulness. Nat Rev Neurosci 8:171–81
Sakurai T, Nagata R, Yamanaka A, Kawamura H, Tsujino N, Muraki Y, Kageyama H, Kunita S, Takahashi S, Goto K, Koyama Y, Shioda S, Yanagisawa M (2005) Input of orexin/hypocretin neurons revealed by a genetically encoded tracer in mice. Neuron 46:297–308
Schmitt O, Usunoff KG, Lazarov NE, Itzev DE, Eipert P, Rolfs A, Wree A (2011) Orexinergic innervation of the extended amygdala and basal ganglia in the rat. Brain Struct Funct 217:233-256
Scott MM, Marcus JN, Pettersen A, Birnbaum SG, Mochizuki T, Scammell TE, Nestler EJ, Elmquist JK, Lutter M (2011) Hcrtr1 and 2 signaling differentially regulates depression-like behaviors. Behav Brain Res 222:289–294
Shahid IZ, Rahman AA, Pilowsky PM (2011) Orexin A in rat rostral ventrolateral medulla is pressor, sympathoexcitatory, increases barosensitivity and attenuates the somatosympathetic reflex. Br J Pharmacol. doi:10.1111/j.1476-5381.2011.01694.x
Sinclair LI, Christmas DM, Hood SD, Potokar JP, Robertson A, Isaac A, Srivastava S, Nutt DJ, Davies SJ (2009) Antidepressant-induced jitteriness/anxiety syndrome: systematic review. Br J Psychiatry 194:483–490
Spinazzi R, Andreis PG, Rossi GP, Nussdorfer GG (2006) Orexins in the regulation of the hypothalamic-pituitary-adrenal axis. Pharmacol Rev 58:46–57
Steiner MA, Lecourt H, Rakotoariniaina A, Jenck F (2011a) Favoured genetic background for testing anxiolytics in the fear-potentiated and light-enhanced startle paradigms in the rat. Behav Brain Res 221:34–42
Steiner MA, Lecourt H, Strasser DS, Brisbare-Roch C, Jenck F (2011b) Differential effects of the dual orexin receptor antagonist almorexant and the GABA(A)-alpha1 receptor modulator zolpidem, alone or combined with ethanol, on motor performance in the rat. Neuropsychopharmacology 36:848–856
Suzuki M, Beuckmann CT, Shikata K, Ogura H, Sawai T (2005) Orexin-A (hypocretin-1) is possibly involved in generation of anxiety-like behavior. Brain Res 1044:116–121
Tallman JF, Paul SM, Skolnick P, Gallager DW (1980) Receptors for the age of anxiety: pharmacology of the benzodiazepines. Science 207:274–281
Walker DL, Davis M (1997a) Anxiogenic effects of high illumination levels assessed with the acoustic startle response in rats. Biol Psychiatry 42:461–471
Walker DL, Davis M (1997b) Double dissociation between the involvement of the bed nucleus of the stria terminalis and the central nucleus of the amygdala in startle increases produced by conditioned versus unconditioned fear. J Neurosci 17:9375–9383
Winslow JT, Noble PL, Davis M (2007) Modulation of fear-potentiated startle and vocalizations in juvenile rhesus monkeys by morphine, diazepam, and buspirone. Biol Psychiatry 61:389–395
Yoshida K, McCormack S, Espana RA, Crocker A, Scammell TE (2006) Afferents to the orexin neurons of the rat brain. J Comp Neurol 494:845–861
Zhang W, Zhang N, Sakurai T, Kuwaki T (2009) Orexin neurons in the hypothalamus mediate cardiorespiratory responses induced by disinhibition of the amygdala and bed nucleus of the stria terminalis. Brain Res 1262:25–37
Zhao Z, Yang Y, Walker DL, Davis M (2009) Effects of substance P in the amygdala, ventromedial hypothalamus, and periaqueductal gray on fear-potentiated startle. Neuropsychopharmacology 34:331–340
Acknowledgments
We thank Hélène Pierre and Susan Flores (Actelion Pharmaceuticals Ltd.) for careful reading of the manuscript.
Conflict of interest
All authors are employees of Actelion Pharmaceuticals Ltd.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Steiner, M.A., Lecourt, H. & Jenck, F. The brain orexin system and almorexant in fear-conditioned startle reactions in the rat. Psychopharmacology 223, 465–475 (2012). https://doi.org/10.1007/s00213-012-2736-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-012-2736-7