Abstract
Rationale
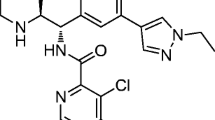
The α-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid (AMPA) receptor positive allosteric modulators (AMPA-PAMs), Org 24448 and Org 26576, and the glycine transporter-1 (GlyT-1) inhibitor Org 25935 are developed for treatment of schizophrenia.
Objectives
Here we examined experimentally the ability of co-administration of these AMPA-PAMs or the GlyT-1 inhibitor to augment the antipsychotic activity and effect on cortical N-methyl-d-aspartate (NMDA) receptor-mediated transmission of risperidone, olanzapine, or haloperidol.
Methods
We examined antipsychotic efficacy using the conditioned avoidance response (CAR) test, extrapyramidal side effect liability using a catalepsy test, and cortical NMDA receptor-mediated glutamatergic transmission using intracellular electrophysiological recording technique in vitro.
Results
Both AMPA-PAMs enhanced the suppression of CAR induced by risperidone or olanzapine, and Org 24448 also enhanced the effect of haloperidol. In contrast, the GlyT-1 inhibitor did not cause any behaviorally significant effect in the CAR test. However, the GlyT-1 inhibitor, but not the AMPA-PAMs, produced a large facilitation of NMDA-induced currents. All three drugs potentiated the effect of risperidone but not haloperidol on these currents. The GlyT-1 inhibitor also facilitated the effect of olanzapine. All drugs potentiated the effect of risperidone on electrically stimulated excitatory postsynaptic potentials (EPSP) in cortical pyramidal cells, whereas only the GlyT inhibitor facilitated the effect of olanzapine.
Conclusions
Our results suggest that the AMPA-PAMs, when compared to the GlyT-1 inhibitor, show differential effects in terms of augmentation of antipsychotic efficacy, particularly when combined with risperidone or olanzapine. Both AMPA-PAMs and the GlyT-1 inhibitor may also improve negative symptoms and cognitive impairments in schizophrenia, in particular when combined with risperidone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The glutamate hypothesis of schizophrenia postulates that an aberrant glutamatergic neurotransmission, particularly N-methyl-d-aspartate (NMDA) receptor hypofunction, contributes to both cognitive and other psychiatric manifestations of the disorder, including negative symptoms (Deutsch et al. 1989; Olney and Farber 1995). This is strongly supported by the ability of the noncompetitive NMDA receptor antagonist phencyclidine (PCP) to induce a psychosis in healthy volunteers, which may be indistinguishable from schizophrenia (see Javitt 2010; Javitt and Zukin 1991; Luby et al. 1959; Svensson 2000). In addition, postmortem studies have revealed that the prefrontal cortex (PFC) of schizophrenic patients exhibit alterations in the expression of NR2 subunit mRNA, which indicate an impaired NMDA receptor-mediated neurotransmission that accompanies functional hypoactivity of the frontal lobe (Akbarian et al. 1996), as well as abnormal expression of NR1 and NR2A subunits relative to NR2B expression in the dorsolateral PFC (see Dracheva et al. 2001; Beneyto and Meador-Woodruff 2008). Accordingly, several pharmacological strategies aiming at potentiating NMDA receptor function are of considerable interest for the treatment of schizophrenia.
Direct enhancement of NMDA receptor function can be achieved by different types of agonists at the strychnine-insensitive glycine-B site on the NMDA receptor or by blocking glycine reuptake through the glycine transporter 1 (GlyT-1). Another indirect approach to enhance NMDA receptor-mediated transmission can be achieved by activation of the α-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid (AMPA) receptor through the use of AMPA receptor positive allosteric modulators (AMPA-PAMs). Activation of AMPA receptors leads to neuronal depolarization, which in turn removes the magnesium block from the NMDA receptor and enables an enhanced ion flux of Na+ and Ca2+ through the receptor channel.
Indeed, several clinical studies have reported improvement of negative symptoms in schizophrenic patients treated with agonists (e.g., glycine, d-serine, and d-cycloserine) when combined with both typical (Goff et al. 1999b; Heresco-Levy et al. 1996) and some atypical antipsychotic drugs (APDs), e.g., risperidone (Heresco-Levy et al. 2004, 2005). However, when used as adjunct treatment in patients treated with clozapine, no improvement was reported (Evins et al. 2000; Potkin et al. 1999; Tsai et al. 1999), and negative symptom may even be exacerbated in patients receiving a combination of clozapine and d-cycloserine (see Goff et al. 1999a). Similar results have been found with the GlyT-1 inhibitor sarcosine, which also has shown beneficial effects in patients treated with several APDs, including risperidone (Lane et al. 2010; Tsai et al. 2004) but not clozapine (Lane et al. 2006). These clinical observations are consistent with previous experimental results in the rat, showing that the GlyT-1 inhibitor N-[3-(4′-fluorophenyl)-3-(4′-phenylphenoxy)propyl]sarcosine (NFPS) significantly potentiates the effect of risperidone but not clozapine on NMDA-induced currents in pyramidal cells of the medial PFC (mPFC; Konradsson et al. 2006). It is of note that facilitation of NMDA receptor-mediated transmission in pyramidal cells of the rat mPFC has previously been demonstrated following administration of several atypical APDs, in particular clozapine, but not typical APDs, e.g., haloperidol (Arvanov et al. 1997; Jardemark et al. 2002; Ninan et al. 2003b), an effect which thus may contribute to the improvement of certain aspects of cognitive dysfunction as well as negative symptoms in schizophrenia that may be achieved with clozapine but not haloperidol.
Two clinical studies using adjunct treatment with AMPA-PAMs in schizophrenic patients have shown inconsistent results. In the first (Goff et al. 2001), the prototypic AMPA-PAM CX-516 produced improved attention and memory in patients treated with clozapine, effects that, however, were not reproduced in an add-on trial of this compound with risperidone, olanzapine, or clozapine (Goff et al. 2008). Irrespective of these clinical observations, CX-516 has been shown to enhance the effect of subthreshold doses of both typical and atypical APDs in rodent models that are considered to predict clinical antipsychotic effect, yet without increasing catalepsy which predicts extrapyramidal side effect (EPS) liability (Johnson et al. 1999; Olsen et al. 2006). Moreover, a recent study demonstrated that CX-516 as well as another related compound, CX-546, both reversed PCP-induced cognitive deficits, using the novel object recognition task in rats (Damgaard et al. 2010). These findings thus suggest that positive modulators of the AMPA receptor may well provide a useful adjunctive treatment in schizophrenic patients maintained on antipsychotic medication, both as regards positive and negative symptoms as well as certain aspects of cognitive impairment.
Here we have examined in rats the antipsychotic-like effects of two AMPA-PAMs, Org 24448 and Org 26576, and one GlyT-1 inhibitor, Org 25935, both when given alone and in combination with the atypical APDs risperidone and olanzapine, and the typical APD haloperidol, using the conditioned avoidance response (CAR) test, as well as the associated EPS liability using a catalepsy test. Although previous clinical studies indicate a preferential action of GlyT-1 inhibitors on negative symptoms, we here also studied the putative antipsychotic potential of a new GlyT-I inhibitor, Org 25935, in the same behavioral paradigm. In addition, we analyzed the effects of these drugs and drugs combinations on cortical NMDA receptor-mediated transmission using intracellular electrophysiological recording in pyramidal cells of the mPFC in vitro, both as regards their ability to enhance NMDA-induced currents in the neurons and their capacity to enhance electrically stimulated excitatory postsynaptic potentials (EPSPs) in the cells.
Materials and methods
Biological materials
Male Wistar rats (B & K Universal, Sollentuna, Sweden and Charles River Laboratories, Sulzfeld, Germany), with an average weight of 200–250 g upon arrival, were used for the behavioral experiments, whereas male Sprague-Dawley rats (B & K Universal, Sollentuna, Sweden and Charles River Laboratories, Sulzfeld, Germany), with an average weight of approximately 70 g upon arrival, were used for in vitro electrophysiological experiments. The animals were housed four to five per cage (Makrolon® IV, BK Universal AS, Nittedal, Norway) under standard laboratory conditions with a temperature of 21.0 ± 0.4°C and relative humidity of 55–65%. Food (R34, Ewos, Södertälje, Sweden) and tap water were available ad libitum. For the behavioral tests, animals were maintained on a reversed 12:12-h light/dark cycle (lights off at 6:00 AM), whereas for the electrophysiological experiments, the animals were kept on a 12:12-h light/dark cycle (lights on at 6:00 AM). The animals were acclimatized for at least 5 days prior to experiments. All experiments were performed between 8:00 AM and 6:00 PM. All experiments were approved by and conducted in accordance with the local Animal Ethics Committee, Stockholm North and the Karolinska Institutet, Sweden.
Equipment and methods
Conditioned avoidance response
Rats were trained in conventional shuttle boxes (530 × 250 × 225 mm), divided into two compartments of equal size by a partition with an opening (Salmi et al. 1994). The apparatus was equipped with photocells, automatically registering the position of the rat in relation to the opening, and a grid floor connected to a high resistance power supply. Upon presentation of the 80-dB white noise (white noise generator; Lafayette Instruments, Lafayette, IN, USA) conditioned stimulus (CS), the rats had 10 s to move from one compartment of the shuttle box into the other. If the rat remained in the same compartment for more than 10 s, an intermittent electric shock (intershock interval 2.5 s, shock duration 0.5 s) of approximately 0.4 mA, i.e., the unconditioned stimulus (UCS), was presented to the grid floor until an escape was performed. If the rat did not respond within 50 s, the trial was terminated, i.e., escape failure. After three consecutive escape failures, the session was terminated. The position of the rat was automatically transferred to the computer, and the following behavioral variables were recorded: (1) avoidance (response to CS within 10 s), (2) escape (response to CS + UCS), (3) escape failure (failure to respond within 50 s), and (4) inter-trial crosses (movement between compartments between trials). The animals were transferred from the animal quarters to the laboratory 1 h before behavioral experiments were started and were housed in a ventilated cabinet between observations. The animals were trained for five consecutive days, each session lasting 15 min per animal and day. Only animals reliably performing >85% avoidance were included in the study. Experimental manipulations were always preceded by a pretest, and experiment sessions, lasting 10 min, were conducted 20, 90, and 240 min after injection of the drug or vehicle. If the animal was not back to baseline performance, an additional session was performed at 360 or 480 min. Experimental days were always separated by at least two non-experimental days. The animals were tested in a counterbalanced change-over design serving as their own controls (Li 1964).
Catalepsy
Catalepsy was observed in a dimly lit room by placing the animals on an inclined grid (60°) for a maximum of 3 min. The animals were allowed 30 s of adaptation on the grid before observations started. The catalepsy was scored from 0 to 5, according to the time (square root transformation) the rat remained immobile (min): 0 = 0.00–0.08, 1 = 0.09–0.35, 2 = 0.36–0.80, 3 = 0.81–1.42, 4 = 1.43–2.24, and 5 ≥ 2.25, i.e., if the rat remained immobile for 0.08 min, it was scored as 0, etc. (Ahlenius and Hillegaart 1986). The animals were transferred from the animal quarters to the laboratory 1 h before behavioral experiments were started and were housed in a ventilated cabinet between observations. Observations were performed 30, 60, and 120 min after the last drug or vehicle injection. The different treatments were unknown to the observer. Each animal received only one treatment.
Intracellular recording of pyramidal cells in the mPFC
The procedures for the preparation of the rat brain slice have been described elsewhere (Arvanov and Wang 1998; Arvanov et al. 1997). Briefly, the rats were decapitated under halothane anesthesia (AstraZeneca AB, Södertälje, Sweden). The brains were then rapidly removed and cooled in ice-cold Ringer’s solution (in mM: 126 NaCl, 2.5 KCl, 2.4 CaCl2, 1.3 MgCl2, 1.2 NaH2PO4, 10 d-glucose, 18 NaHCO3, pH 7.4) aerated by 95% O2/5% CO2. The brains were then cut coronally to produce 450-μm slices. The brain slices were removed from the Vibroslice (Campden model MA 752, World Precision Instruments, Sarasota, FL, USA) and kept submerged in aerated Ringer’s solution at room temperature for at least 1 h to allow for recovery. A single slice containing mPFC, approximately anterioposterior +3.2 mm from bregma (Paxinos and Watson 2007), was then transferred to a recording chamber (32°C), in which it was held submerged between two nylon nets during the electrophysiological recordings. The chamber was continuously perfused by aerated Ringer’s solution at a flow rate of ∼2 ml/min.
Standard intracellular recording was used to record pyramidal cells in layers V and VI of the mPFC in slice preparations (Arvanov and Wang 1998; Arvanov et al. 1997). Electrodes were pulled from borosilicate glass capillaries (Clark Electromedical Instruments, Pangbourne, UK) by using a horizontal electrode puller (Model P-87, Sutter Instruments, San Rafael, CA, USA). Recording electrodes were filled with 2 M KAc (the resistance of the recording electrodes was between 60 and 120 MΩ) and used for recording the mPFC neurons with an Axoclamp 2A amplifier (Axon Instruments, Foster City, CA, USA).
Single electrode voltage-clamp (holding potential −60 mV) was performed in the discontinuous mode with a sampling rate of 5–6.2 kHz. The voltage recordings are acquired using digital/analog sampling and acquisition software (Clampex version 9.2, Axon Instruments). During the voltage-clamp recordings of NMDA-evoked currents, tetrodotoxin (0.5 μM, to block the action potentials), glycine (1 μM, to enhance the NMDA-induced responses), and bicuculline (5 μM, to block the GABAA responses) were routinely included in the aerated Ringer’s solution. All drugs used were diluted in Ringer’s solution and administered via bath application by perfusion via a three-way tap system. The concentrations of risperidone, haloperidol, and olanzapine are those which produced maximal effects on the NMDA-induced currents. NMDA (7.5–15 μM) was also applied via bath perfusion, to induce inward currents. The effect of the drug on the NMDA-induced current was calculated by dividing the NMDA-induced current 30 min after the bath application of the drug with the control NMDA-induced current.
The procedures for eliciting EPSPs by electrical stimulation of the forceps minor (white matter) have been described (Arvanov et al. 1997; Chen and Yang 2002; Jardemark et al. 2005). Briefly, the EPSPs, recorded in the current clamp mode, were elicited by passing rectangular current pulses (0.3 ms duration, 6–40 V) between the tips of a bipolar stainless steel electrode placed in the medial part of the forceps minor close to the recording electrode (filled with 2 M KAc). Electrical pulses were delivered before and after 5, 15, and 25 min of drug application for evaluation of the drug’s effects on the EPSPs. Bicuculline (2 μM; to block GABAA receptor-mediated inhibitory postsynaptic potentials) was included in the bath (Ringer’s) solution throughout the recordings. All drugs were administered via bath perfusion.
Drugs
For in vivo experiments, the dose selections of the compounds are generally consistent with previously published data (Jordan et al. 2005; Molander et al. 2007; Hamlyn et al. 2009; Su et al. 2009; Lidö et al. 2009; Vengeliene et al. 2010; Kalinichev et al. 2010). Org 24448 was dissolved in 50% dimethyl sulfoxide (DMSO) in 0.9% NaCl (except for the CAR experiment Org 24448 3 mg/kg + risperidone 0.25 and 0.3 mg/kg, where the drug was dissolved in 10% DMSO in 0.9% NaCl), and Org 25935 was dissolved in 25% DMSO in 0.9% NaCl. Org 26576, risperidone, haloperidol, and olanzapine were dissolved in a minimal amount (∼1%) of acetic acid with a 5.5% glucose solution added to volume. Control animals received injections with the respective vehicle. Systemic administration was performed by subcutaneous (s.c.) or intraperitoneal (i.p.) injections at a volume of 2.0 ml/kg.
For in vitro electrophysiology experiments, Org 24448, Org 26576, Org 25935, risperidone, olanzapine, and haloperidol were first dissolved in DMSO and then brought to stock concentration by the addition of purified water. The concentrations of stock solutions were prepared 1,000-fold higher than that of final target solution. Previous tests have shown that artificial cerebral spinal fluid containing DMSO has, without drugs, no effect on the recorded responses (Jardemark et al. 2000). The concentrations of DMSO in the present and previous (Jardemark et al. 2000) perfusion solutions were <0.1%.
Data compilations and processing
The data from behavioral experiments are not normally distributed and accordingly non-parametric tests are used. Thus, for the CAR data, the Friedman two-way analysis of variance (ANOVA), followed by Wilcoxon matched-pairs signed-ranks test, and for the catalepsy data, the Kruskal–Wallis one-way ANOVA, followed by Mann–Whitney U test, were used (Siegel and Castellan 1988). The statistical evaluations were performed by using Statistica version 9.1 (Statsoft).
Statistical evaluation of the intracellular recording data was performed with the software GraphPad Prism version 4.0 (GraphPad Software Inc., San Diego, CA, USA) using a paired t-test, measuring significant difference from the control NMDA-induced currents, and a Student’s t-test, measuring significant difference between treatment groups. In all statistical measures, a p value less than 0.05 (p < 0.05) was considered significant.
Results
Effects of the AMPA-PAM Org 24448 on CAR behavior
First, a dose–response relationship for the antipsychotic-like effect of Org 24448 (3, 10, and 30 mg/kg, s.c.) was established (Fig. 1a). At both 20 and 90 min, 30 mg/kg produced a significant suppression of CAR (p < 0.05–0.01). Escape failures were recorded in three rats, i.e., at 10 mg/kg (one rat) and at 30 mg/kg (three rats). For our subsequent studies, 20 mg/kg of Org 24448 was used, since this dose was expected to generate a suppressant effect on CAR combined with a low risk of escape failure.
Effects of the AMPA-PAM Org 24448 on CAR behavior in rats. a Effects of Org 24448 (3, 10, and 30 mg/kg, s.c.) at 0 to 240 min after administration. Statistical evaluation of suppression of CAR was performed [20 min: χ 2(3) = 12.44, p < 0.01; 90 min: χ 2(3) = 19.48, p < 0.001; 240 min: χ 2(3) = 8.21, p < 0.05; n = 10]. All animals were back to normal performance at 480 min after drug administration. b, c Effects of Org 24448 (20 mg/kg s.c.) alone and in combination with haloperidol 0.025 mg/kg i.p. [20 min: χ 2(3) = 13.48, p < 0.01; 90 min: χ 2(3) = 21.49, p < 0.001; 240 min: χ 2(3) = 2.00, p = 0.57; n = 9]. All animals were back to normal performance at 240 min. d, e Effects of Org 24448 20 mg/kg s.c. alone and in combination with risperidone 0.25 mg/kg i.p. or olanzapine 1.25 mg/kg i.p. [20 min: χ 2(5) = 30.00, p < 0.001; 90 min: χ 2(5) = 25.68, p < 0.001; 240 min: χ 2(5) = 3.56, p = 0.614; n = 11]. Animals were back to normal performance at 480 min. Results are presented as median (avoidance %) ± semi-interquartile range. Animals are serving as their own controls in a change-over design. *p < 0.05; **p < 0.001 vs. vehicle-treated animals; #p < 0.05; ##p < 0.01 vs. Org 24448-treated animals; +p < 0.05; ++p < 0.01 as indicated in the figure
In a second set of animals (Fig. 1b, c), Org 24448 (20 mg/kg) was added to a dose of haloperidol that, when given alone, does not produce a suppression of CAR sufficient to indicate an antipsychotic effect, i.e., 0.025 mg/kg (Wadenberg et al. 2007). Org 24448 significantly enhanced the haloperidol-induced suppression of CAR (20 min, p < 0.05 and 90 min, p < 0.01). Escape failure was recorded in one animal for both Org 24448 alone and the combination Org 24448 and haloperidol.
In a third set of animals (Fig. 1d, e), Org 24448 (20 mg/kg) was added to doses of risperidone or olanzapine that by themselves did not produce a suppression of CAR sufficient to indicate an antipsychotic effect, i.e., 0.25 and 1.25 mg/kg, respectively (Marcus et al. 2010; Wadenberg et al. 2007). Org 24448 significantly enhanced the risperidone-induced suppression of CAR (20 and 90 min, p < 0.05), as well as the olanzapine-induced suppression of CAR (90 min, p < 0.05), although only to a small extent. In these tests, escape failure was recorded in three animals, i.e., Org 24448 and risperidone (one rat) and Org 24448 and olanzapine (two rats).
Effects of the AMPA-PAM Org 26576 on CAR behavior
First, a dose–response relationship for Org 26576 (3, 10, and 30 mg/kg s.c.) was established (Fig. 2a). Both 10 and 30 mg/kg produced a small but statistically significant suppression of CAR (10 mg/kg at 90 min, p < 0.05, and 30 mg/kg at 20 min, p < 0.05). Escape failures were recorded in five rats, i.e., 10 (two rat) and 30 mg/kg (four rats). For further studies, 10 mg/kg Org 26576 was used, as this dose still produced suppression of CAR, but a reduced risk of escape failure.
Effects of the AMPA-PAM Org 26576 on CAR behavior in rats. a Effects of Org 26576 (3, 10, and 30 mg/kg, s.c.) at 0 to 240 min after administration [20 min: χ 2(3) = 11.67, p < 0.01; 90 min: χ 2(3) = 8.76, p < 0.05; 240 min: χ 2(3) = 10.83, p < 0.05, n = 11]. Animals were back to normal performance at 480 min after drug administration. b Effects of Org 26576 10 mg/kg s.c. alone and in combination with haloperidol 0.025 mg/kg i.p. or olanzapine 1.25 mg/kg i.p. [20 min: χ 2(5) = 35.46, p < 0.001; 90 min: χ 2(5) = 10.91, p = 0.053; 240 min: χ 2(5) = 8.94, p = 0.111; n = 12]. Animals were back to normal performance at 360 min. c Effects of Org 26576 10 mg/kg s.c. alone and in combination with risperidone 0.25 mg/kg i.p. [20 min: χ 2(3) = 25.53, p < 0.001; 90 min: χ 2(3) = 9.57, p < 0.05; 240 min: χ 2(3) = 0.45, p = 0.929; n = 12]. Animal was back to normal performance at 240 min. Results are presented as median (avoidance %) ± semi-interquartile range. Rats are serving as their own controls in a change-over design. *p < 0.05; **p < 0.01 vs. vehicle-treated animals; ###p < 0.001 vs. Org 26576-treated animals; ++p < 0.01 as indicated in the figure
In a second set of animals (Fig. 2b), Org 26576 (10 mg/kg) was added to haloperidol (0.025 mg/kg) or olanzapine (1.25 mg/kg). Org 26576 significantly enhanced the olanzapine-induced suppression of CAR (20 min, p < 0.01), but had no effect when combined with haloperidol. Here, escape failures were recorded in three rats, i.e., olanzapine (one rat) and Org 26576 and olanzapine (two rats).
In a third set of animals, Org 26576 (10 mg/kg) was added to risperidone (0.25 mg/kg; Fig. 2c). Org 26576 apparently enhanced the risperidone-induced suppression of CAR, but this effect did not reach statistical significance (p = 0.06). No escape failures were recorded.
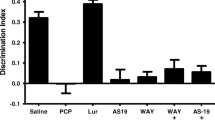
Effects of the GlyT-1 inhibitor Org 25935 on CAR behavior
First, the dose–response relationship for Org 25935 (1, 3, and 6 mg/kg s.c.) was established (Fig. 3a). A very small but statistically significant suppression of CAR was produced by 6 mg/kg Org 25935 (90 min, p < 0.01). No escape failures were recorded.
Effects of the GlyT-1 inhibitor Org 25935 on CAR behavior in rats. a Effects of Org 25935 (1, 3, and 6 mg/kg s.c.) at 0 to 240 min after drug administration [20 min: χ 2(3) = 2.31, p = 0.51; 90 min: χ 2(3) = 18.43, p < 0.001; 240 min: χ 2(3) = 6.69, p = 0.082; n = 11]. All animals were back to normal performance at 240 min after drug administration. b, c Effects of Org 25935 6 mg/kg s.c. alone and in combination with haloperidol 0.025 mg/kg i.p. and olanzapine 1.25 mg/kg i.p. [20 min: χ 2(5) = 37.17, p < 0.001; 90 min: χ 2(5) = 26.80, p < 0.001; 240 min: χ 2(5) = 10.99, p = 0.051; n = 11]. Animals were back to normal performance at 240 min (one animal back at 360 min). d, e Effects of Org 25935 6 mg/kg s.c. alone and in combination with risperidone 0.25 mg/kg i.p. [20 min: χ 2(3) = 24.26, p < 0.001; 90 min: χ 2(3) = 11.21, p < 0.05; 240 min: χ 2(3) = 4.47, p = 0.215; n = 12]. Animals were back to normal performance at 240 min. Results are presented as median (avoidance %) ± semi-interquartile range. Animals are serving as their own controls in a change-over design. *p < 0.05; **p < 0.001 vs. vehicle-treated animals; ##p < 0.01; ###p < 0.001 vs. Org 25935-treated animals; +p < 0.05 as indicated in the figure
In a second set of animals, Org 25935 (6 mg/kg) was added to haloperidol (0.025 mg/kg) or olanzapine (1.25 mg/kg; Fig. 3b, c). Org 25935 caused a very small, but statistically significantly enhancement of the haloperidol-induced suppression of CAR (90 min, p < 0.05), but did not significantly enhance the olanzapine-induced suppression of CAR. Escape failure was recorded in one animal.
In a third set of animals, Org 25935 (6 mg/kg) was added to risperidone (0.25 mg/kg; Fig. 3d, e). Addition of Org 25935 did not significantly enhance the risperidone-induced suppression of CAR. No escape failures were recorded.
Effects of the AMPA-PAMs Org 24448 and ORG 26576 and GlyT-1 inhibitor Org 25935 on catalepsy
Org 24448 20 mg/kg alone, and in combination with olanzapine 1.25 mg/kg, risperidone 0.25 mg/kg, and haloperidol 0.025 mg/kg, was tested in the catalepsy test. Statistical evaluation revealed statistical significant effect [30 min: H(7) = 11.74, p = 0.1095; 60 min: H(7) = 15.28, p < 0.05; 120 min: H(7) = 13.84, p = 0.0541; n = 7–8; Table 1]. Compared to control, risperidone, Org 24448, the combinations of Org 24448 and olanzapine, and Org 24448 and haloperidol showed statistical significant effect (60 min; p < 0.05–0.001). Addition of Org 24448 to haloperidol enhanced the catalepsy score (60 min; p < 0.05). According to previous studies, an animal is considered cataleptic with a score ≥ 2 (Wadenberg et al. 2001). The maximal score in this test is 5, indicating that score of 2, which was recorded here, is in the low range of catalepsy.
Org 26576 (10 mg/kg) alone, or in combinations with either olanzapine 1.25 mg/kg, risperidone 0.25 mg/kg, or haloperidol 0.025 mg/kg, did not reveal any statistical significant effect in the catalepsy test [30 min: H(7) = 6.27, p = 0.5084; 60 min: H(7) = 12.71, p = 0.0795; 120 min: H(7) = 10.2253, p = 0.1762; n = 8; Table 2]. Also Org 25935 6 mg/kg alone, or in combinations with olanzapine 1.25 mg/kg, risperidone 0.25 mg/kg, or haloperidol 0.025 mg/kg, did not reveal any statistical significant effect [30 min: H(7) = 12.38, p = 0.0888; 60 min: H(7) = 7.26, p = 0.4021; 120 min: H(7) = 11.13, p = 0.1329; Table 3].
Effects of the AMPA-PAM Org 24448 on NMDA-induced currents in pyramidal cells of the rat mPFC
Intracellular voltage-clamp recordings of NMDA-induced currents were performed in pyramidal cells in layer V and VI of the rat mPFC in slice preparations. The electrophysiological criteria for distinguishing pyramidal from non-pyramidal neurons have been described previously (Arvanov and Wang 1998; Arvanov et al. 1997; Konradsson et al. 2006). Briefly, the presumed pyramidal cells of the mPFC have relatively long spike duration (1–3 ms at half-maximum spike amplitude) and show a pronounced spike-frequency adaptation in response to constant-current depolarization pulses.
A concentration–response curve for Org 24448 showed that it had no effect on the NMDA-induced currents when given alone (Fig. 4a). The mean effects, expressed as percent of control NMDA-induced current, of Org 24448 on the NMDA-induced currents were 88 ± 8% (1 μM, n = 3), 112 ± 16% (10 μM, n = 3), and 96 ± 15% (50 μM, n = 3).
Effects of the AMPA-PAM Org 24448 on NMDA-induced currents in pyramidal cells of the rat mPFC. a The concentration–response relationship of the effect of Org 24448 on the NMDA-induced currents. b–d Histograms illustrating the effects of Org 24448 (10 μM) in combination with risperidone (20 nM), haloperidol (100 nM), or olanzapine (5 nM) on the NMDA-induced currents. Each bar represents the mean ± SEM percent of control. The holding potential was −60 mV. For comparison, the maximal effect of clozapine (100 nM) is included in the bar graphs. *p < 0.05 (Student’s t-test)
The effects on NMDA-induced currents of Org 24448 in combinations with haloperidol, risperidone, or olanzapine were examined. Org 24448 (10 μM) did not facilitate the effect of haloperidol (100 nM) on the NMDA-induced currents (104 ± 25%; n = 3; Fig. 4b). On the other hand, Org 24448 (10 μM) was able to potentiate the effect of a maximal concentration of risperidone (20 nM; 258 ± 52%; Students t-test, p < 0.05; n = 3; Fig. 4c). As with haloperidol, Org 24448 (10 μM) was unable to facilitate the effect of a maximal concentration of olanzapine (5 nM) on the NMDA-induced currents in pyramidal cells of the mPFC (169 ± 19% of baseline; n = 3; Fig. 4d).
Effects of the AMPA-PAM Org 26576 on NMDA-induced currents in pyramidal cells of the rat mPFC
Bath perfusion with Org 26576 significantly potentiated the NMDA-induced currents (see Fig. 5a; paired t-test, p < 0.05). The mean effects, expressed as percent of control NMDA-induced current, of this AMPA-PAM on NMDA-induced currents were 105 ± 15% (1 μM, n = 3 cells), 117 ± 7% (10 μM, n = 6), 117 ± 22% (30 μM, n = 7), and 75 ± 21% (50 μM, n = 3).
Effects of the AMPA-PAM Org 26576 on NMDA-induced currents in pyramidal cells of the rat mPFC. a A histogram illustrating the concentration–response relationship of the effect of Org 26576 on the NMDA-induced currents. b–d Bar graphs showing the effects of Org 26576 (10 μM) in combination with risperidone (20 nM), haloperidol (100 nM), or olanzapine (5 nM) on the NMDA-induced currents. Each bar represents the mean ± SEM percent of control. The holding potential was −60 mV. For comparison, the maximal effect of clozapine (100 nM) is included in the bar graphs. +p < 0.05 (paired t-test); *p < 0.05 (Student’s t-test)
Org 26576 (10 μM) did not facilitate the effect of haloperidol (100 nM) on the NMDA-induced currents (109 ± 9%; n = 3; Fig. 5b). In contrast, Org 26576 (10 μM) significantly facilitated the effect of risperidone (20 nM) on the NMDA-induced currents (214 ± 24%; n = 5; Student’s t-test, p < 0.05; Fig. 5c). Org 26576 (10 μM) was also able to facilitate the effect of olanzapine (5 nM) on the NMDA-induced currents (199 ± 4%; n = 4; Student’s t-test, p < 0.05; Fig. 5d).
Effects of the GlyT-1 inhibitor Org 25935 on NMDA-induced currents in pyramidal cells of the rat mPFC
Bath perfusion with Org 25935 significantly potentiated the NMDA-induced currents (see Fig. 6a; paired t-test, p < 0.05). The mean effects, expressed as percent of control NMDA-induced current, of this GlyT-1 inhibitor on the NMDA-induced currents were 120 ± 8% (1 μM, n = 3 cells), 153 ± 9% (10 μM, n = 3), and 192 ± 13% (50 μM, n = 3).
Effects of the GlyT-1 inhibitor Org 25935 on NMDA-induced currents in pyramidal cells of the rat mPFC. a A histogram illustrating the concentration–response relationship of the effect of Org 25935 on the NMDA-induced currents, when given alone. b–d Histograms illustrating the effects of Org 25935 (1 μM) in combination with risperidone (20 nM), haloperidol (100 nM), or olanzapine (5 nM) on the NMDA-induced currents. Each bar represents the mean ± SEM percent of control. The holding potential was −60 mV. For comparison, the maximal effect of clozapine (100 nM) is included in the bar graphs. +p < 0.05 (paired t-test); *p < 0.05 (Student’s t-test)
Org 25935 (1 μM) did not facilitate the effect of haloperidol (100 nM) on the NMDA-induced currents (Fig. 6b). The effects on NMDA-induced current were haloperidol (100 nM) 116 ± 19% (n = 5) and Org 25935 (1 μM) + haloperidol (100 nM) 102 ± 20% (n = 3). However, Org 25935 (1 μM) was able to potentiate the effect of a maximal concentration of risperidone (20 nM; Fig. 6c; Students t-test, p < 0.05). The effects of risperidone (20 nM) alone and the combination Org 25935 (1 μM) + risperidone (20 nM) on the NMDA-induced currents were 147 ± 26% (n = 6) and 249 ± 55% (n = 3), respectively. As with haloperidol, Org 25935 (1 μM) did not facilitate the effect of a maximal concentration of olanzapine (5 nM) on the NMDA-induced currents in pyramidal cells of the mPFC (see Fig. 6d). The effects on NMDA-induced current were olanzapine (100 nM) 170 ± 13% (n = 3) and the combination of Org 25935 (1 μM) + olanzapine (5 nM) 171 ± 23% (n = 3).
Effects of the AMPA-PAMs Org 24448 and Org 26576 and the GlyT-1 inhibitor Org 25935 on electrically stimulated EPSPs in pyramidal cells of the rat mPFC
Here we examined the effects of Org 24448, Org 26576, and Org 25935, as well as combinations of these drugs with risperidone or olanzapine, on electrically stimulated EPSPs in pyramidal cells of the rat mPFC. In these experiments, the concentration of each drug was submaximal and chosen based on concentration–response curves for the effects of these drugs on the NMDA-induced currents (see above). For comparison, the effect of clozapine (1 μM) is included in Fig. 7. The submaximal concentrations of risperidone (10 nM, n = 3) and olanzapine (3 nM, n = 3) did not produce any effects on the EPSPs (Fig. 7b, c).
Effects of the AMPA-PAMs, Org 24448 and Org 26576, and the GlyT-1 inhibitor Org 25935, alone and in combination with various APDs on electrically stimulated EPSPs in pyramidal cells of the mPFC. a For comparison, the effect of clozapine 1 μM is included in the figure. b, c Effects of submaximal concentrations of risperidone (10 nM) and olanzapine (3 nM) on the EPSPs. d–l Effects of Org 24448 (1 μM) and Org 26576 (1 μM) and Org 25935 (0.5 μM), when given alone and in combinations with either risperidone (10 nM) or olanzapine (3 nM), on the EPSPs
When given alone, the submaximal concentrations of the AMPA-PAM Org 24448 (1 μM, n = 3) or Org 26576 (1 μM, n = 3) and the GlyT-1 inhibitor Org 25935 (0.5 μM, n = 3) did not potentiate the EPSPs (Fig. 7d–f). However, these drugs were all able to potentiate the effect of risperidone (10 nM, Fig. 7g–i, n = 3) on these responses.
Finally, Org 25935 (0.5 μM), but not Org 24448 (1 μM) or Org 26576 (1 μM), facilitated the effect of olanzapine (3 nM) on the EPSPs in the mPFC (Fig. 7j–l; n = 3 in each combination). However, this effect was small compared to the effect produced by the GlyT-1 inhibitor Org 25935 in combination with risperidone.
Discussion
The present study demonstrates that both the AMPA-PAMs tested, Org 24448 and Org 26576, enhanced the suppression of CAR induced by risperidone or olanzapine, whereas only Org 24448 enhanced the effect of haloperidol. In contrast, the GlyT-1 inhibitor Org 25935 did not cause any significant effect in the CAR test, whether given alone or in combination with various APDs. However, the GlyT-1 inhibitor, but not the AMPA-PAMs used, produced a large facilitation of NMDA-induced currents when given alone. Interestingly, all three drugs potentiated the effect of risperidone, but not haloperidol, on these currents. The AMPA-PAM Org 26576 showed a slightly different profile as it also facilitated the effect of olanzapine on cortical NMDA receptor-mediated transmission. Furthermore, all three drugs were effective in potentiating the effect of a submaximal concentration of risperidone on electrically stimulated EPSP in pyramidal cells of the mPFC, whereas only the GlyT-1 inhibitor Org 25935 facilitated the effect of a submaximal concentration of olanzapine on these responses.
The CAR paradigm is a behavioral test which examines antipsychotic activity, i.e., effect on psychotic/positive symptoms in schizophrenia, by measuring the suppression of avoidance response to a conditioning stimulus. The test has shown high predictive validity, since suppression of CAR is a characteristic effect of all clinically used antipsychotic drugs (see Wadenberg and Hicks 1999; Wadenberg 2010). The dose range within which an antipsychotic drug exerts suppression of CAR in rats without concomitant escape failure or motor disturbance such as catalepsy has been found to roughly correspond to the concomitant striatal D2 receptor occupancy, which in turn resembles the D2 occupancy seen in patients treated with the same antipsychotic drug (Wadenberg et al. 2001). However, the CAR test is not only a measurement of D2 occupancy, since different receptor ligands, e.g., 5-HT2A and α2 antagonists, have been found to enhance the inhibition of CAR without increasing the D2 receptor occupancy (see Wadenberg 2010). The fact that the GlyT-1 inhibitor Org 25935 did not produce any behaviorally significant effect in this behavioral model is clearly not surprising, since when GlyT-1 inhibitors have been tried clinically as adjuvant treatment in schizophrenia, the main effect has been obtained on negative and not on positive symptoms (c.f. “Introduction”). In contrast, both AMPA-PAMs tested, even when given alone, produced some suppression of CAR in rats in doses that did not generate a high risk of EPS, as assessed by the catalepsy test. According to previous studies, a 70–80% suppression of CAR is needed for prediction of a clinically relevant antipsychotic effect in patients (Wadenberg et al. 2001), indicating that the AMPA-PAMs used in the current study would not produce a sufficient antipsychotic effect if used as monotherapy in schizophrenia. When used as adjunctive treatment in rats, Org 24448 significantly enhanced the suppression of CAR by low doses of risperidone, olanzapine, and haloperidol, whereas Org 26576 enhanced the suppression of CAR by low doses of olanzapine and to some extent risperidone (p = 0.06), but not haloperidol. Thus, our data overall suggest that both the AMPA-PAMs might serve to enhance the antipsychotic effect of several APDs without increasing their EPS liability. A comparison between the two compounds tested suggests that, if anything, Org 24448 may appear slightly more useful in this regard.
In similarity with the GlyT-1 inhibitor NFPS (Chen et al. 2003; Konradsson et al. 2006), the GlyT-1 inhibitor Org 25935 produced a significant potentiation of the NMDA-induced currents in the mPFC, both when given alone and in combination with a maximal concentration of risperidone. These data suggest that adjunctive use of Org 25935 may enhance the effect of risperidone on negative and cognitive symptoms, since these symptoms may indeed be related to impaired NMDA receptor-mediated transmission, inter alia in the PFC of schizophrenic patients (c.f. “Introduction”). Previous studies have reported that two other GlyT-1 inhibitors, sarcosine and RG1678, were effective in ameliorating negative symptoms in patients who were maintained on stable antipsychotic medication, including risperidone (Lane et al. 2005, 2010; Tsai et al. 2004; www.roche.com, available at http://www.roche.com/investors/ir_update/inv-update-2009-11-10.htm, accessed 25 May 2011). It appears likely that also sarcosine and RG1678 may exert their action at least partly in the PFC, since previous findings suggest that extracellular glycine is efficiently regulated by GlyT-1, which is expressed in astrocytes adjacent to the glutamatergic synapses in the forebrain (Borowsky et al. 1993; Smith et al. 1992). Moreover, mutant mice with 30% reduction of GlyT-1 expression in the forebrain showed an enhanced cognitive performance in the novel object recognition test (see Möhler et al. 2011), which has shown predictive validity as an animal model for certain aspects of cognitive dysfunction in schizophrenia (Neill et al. 2010). Thus, the present experimental results provide novel support for the notion that inhibition of GlyT-1 may serve as an effective add-on therapy to risperidone for the treatment of negative and cognitive symptoms in schizophrenia and, in addition, delineates a mechanism that may underlie this effect in the brain.
In comparison with clozapine and other atypical APDs (Ninan et al. 2003b), as well as NFPS and the GlyT-1 inhibitor Org 25935, both of the AMPA-PAMs tested, Org 24448 and Org 26576, produced only minor effects on NMDA-induced currents in pyramidal cells of the mPFC. The small effects obtained may be explained by the fact that the major part of these currents are mediated by postsynaptic NMDA receptors and only to a minor extent by non-NMDA receptors (e.g., AMPA receptors), which are activated via a NMDA-evoked release of glutamate in the mPFC (see Arvanov et al. 1997). In contrast, the GlyT-1 inhibitors NFPS and Org 25935 probably increase the synaptic levels of glycine, an obligatory coagonist for the NMDA receptor (Johnson and Ascher 1987), which may contribute to the facilitation of NMDA-induced currents by these compounds. Also atypical APDs may facilitate the NMDA receptor activity by several mechanisms. For example, the large enhancement of NMDA-induced currents in the mPFC that is produced by clozapine seems to be mediated by dopamine and executed via dopamine D1 receptors that are in turn coupled to NMDA receptors (Chen and Yang 2002; Ninan and Wang 2003; Chen et al. 2004). Moreover, our previous data indicate that this effect of clozapine is largely related to its highly potent, presynaptic α2-adrenoceptor antagonistic action, an effect that is essentially unique among both typical and atypical APDs (see Marcus et al. 2005). A similar mechanism for potentiation of NMDA activity was recently reported for the new antipsychotic agent asenapine (Jardemark et al. 2010), which also possesses a potent α2-adrenoceptor effect (Shahid et al. 2009). At any rate, our present electrophysiological data suggest that direct modulation of AMPA receptors by Org 24448 or Org 26576, when given alone, is not sufficient to effectively facilitate NMDA receptor-mediated transmission in the mPFC.
When considering the abilities of the GlyT-1 inhibitor, as well as the two AMPA-PAMs tested, to enhance the effects of different APDs on cortical NMDA receptor-mediated transmission, both the GlyT-1 inhibitor and the two AMPA-PAMs seem to be more useful in conjunction with risperidone than with olanzapine or haloperidol. These results suggest indirectly that risperidone and olanzapine both qualitatively and quantitatively may differ in their effects on NMDA receptor-mediated transmission in the mPFC. Previous studies have demonstrated that olanzapine alone is more potent than risperidone to enhance NMDA receptor-mediated transmission in these models (see Ninan et al. 2003a). Thus, the possibility for improvement is per se smaller in the case of olanzapine. The mechanism underlying the facilitating effects of risperidone in combination with either of the two AMPA-PAMs on the NMDA-induced currents may involve several actions on postsynaptic glutamate receptors. For example, risperidone may like clozapine (Arvanov et al. 1997) induce an increase of presynaptic NMDA receptor-mediated glutamate release in the mPFC. The released glutamate may in turn activate postsynaptic AMPA receptors, which are potentiated by Org 24448 and Org 26576. In principle, the ability of both Org 24448 and Org 26576 to enhance the effect of risperidone on the NMDA-induced currents suggests that these compounds, like GlyT-inhibitors, may help improve negative and cognitive symptoms in patients treated with risperidone.
Our present results also demonstrate that combinations of the GlyT-1 inhibitor as well as the two AMPA-PAMs, with risperidone, can mimic the effect of clozapine (Chen and Yang 2002; Jardemark et al. 2009) in evoking spikes riding over the EPSPs. This effect, which is specifically mediated via activation of NMDA receptors (Chen and Yang 2002; Jardemark et al. 2005), has been suggested to be related to an increased excitability of interconnected pyramidal cells in the mPFC. Excitation of these connections is thought to represent one of the critical mechanisms underlying the generation of persistent neuronal activity in the PFC, which is required for the neuronal representation of information in working memory (Camperi and Wang 1998; Durstewitz et al. 2000; Shu et al. 2003; Wang 1999). Therefore, our results propose that the combined treatment with the two AMPA-PAMs and risperidone, in analogy with clozapine, can facilitate NMDA receptor-mediated interactions between pyramidal cells in the mPFC, providing a neurobiological underpinning for a procognitve action of the two AMPA-PAMs.
Although the initial pilot study of the AMPA-PAM CX516 as add-on treatment in schizophrenia by Goff et al. was, in principle, positive, their second, larger RCT study produced a negative outcome. There may be several reasons for this, as discussed in detail by the authors. However, an additional, major difference between the negative clinical results, especially concerning the effect of add-on CX516 on positive symptoms in schizophrenia, and our results, using a similar add-on treatment in the CAR model which essentially predicts the clinical effect on positive symptoms, is that we used lower than optimal doses of the antipsychotic drugs, i.e., doses that did not produce a sufficient antipsychotic-like effect when given alone. Therefore, our data suggest that by combining suboptimal doses of antipsychotic drugs with AMPA-PAMs may allow for an effective antipsychotic clinical action, yet at a lower D2 occupancy in brain than otherwise would have been needed. In fact, some previous preclinical data support this notion, since CX516 was found to potentiate attenuation of methamphetamine-induced rearing when combined with low-dose antipsychotics (Johnson et al. 1999).
In summary, when comparing the two AMPA-PAMs with the GlyT-1 inhibitor tested, a slightly different clinical utility for the two types of compounds is indicated. Thus, the AMPA-PAMs may appear more useful than the GlyT-1 inhibitor as adjunct treatment to atypical APDs in order to enhance their antipsychotic efficacy, i.e., against positive symptoms in schizophrenia. On the other hand, both the AMPA-PAMs as well as the GlyT-1 inhibitor may be suitable as adjunct treatment for improving negative symptoms and cognitive impairments in this disease.
References
Ahlenius S, Hillegaart V (1986) Involvement of extrapyramidal motor mechanisms in the suppression of locomotor activity by antipsychotic drugs: a comparison between the effects produced by pre- and post-synaptic inhibition of dopaminergic neurotransmission. Pharmacol Biochem Behav 24:1409–1415
Akbarian S, Sucher NJ, Bradley D, Tafazzoli A, Trinh D, Hetrick WP, Potkin SG, Sandman CA, Bunney WE Jr, Jones EG (1996) Selective alterations in gene expression for NMDA receptor subunits in prefrontal cortex of schizophrenics. J Neurosci 16:19–30
Arvanov VL, Liang X, Schwartz J, Grossman S, Wang RY (1997) Clozapine and haloperidol modulate N-methyl-D-aspartate- and non-N-methyl-D-aspartate receptor-mediated neurotransmission in rat prefrontal cortical neurons in vitro. J Pharmacol Exp Ther 283:226–234
Arvanov VL, Wang RY (1998) M100907, a selective 5-HT2A receptor antagonist and a potential antipsychotic drug, facilitates N-methyl-D-aspartate-receptor mediated neurotransmission in the rat medial prefrontal cortical neurons in vitro. Neuropsychopharmacology 18:197–209
Beneyto M, Meador-Woodruff JH (2008) Lamina-specific abnormalities of NMDA receptor-associated postsynaptic protein transcripts in the prefrontal cortex in schizophrenia and bipolar disorder. Neuropsychopharmacology 33:2175–2186
Borowsky B, Mezey E, Hoffman BJ (1993) Two glycine transporter variants with distinct localization in the CNS and peripheral tissues are encoded by a common gene. Neuron 10:851–863
Camperi M, Wang XJ (1998) A model of visuospatial working memory in prefrontal cortex: recurrent network and cellular bistability. J Comput Neurosci 5:383–405
Chen G, Greengard P, Yan Z (2004) Potentiation of NMDA receptor currents by dopamine D1 receptors in prefrontal cortex. Proc Natl Acad Sci U S A 101:2596–2600
Chen L, Muhlhauser M, Yang CR (2003) Glycine transporter-1 blockade potentiates NMDA-mediated responses in rat prefrontal cortical neurons in vitro and in vivo. J Neurophysiol 89:691–703
Chen L, Yang CR (2002) Interaction of dopamine D1 and NMDA receptors mediates acute clozapine potentiation of glutamate EPSPs in rat prefrontal cortex. J Neurophysiol 87:2324–2336
Damgaard T, Larsen DB, Hansen SL, Grayson B, Neill JC, Plath N (2010) Positive modulation of alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors reverses sub-chronic PCP-induced deficits in the novel object recognition task in rats. Behav Brain Res 207:144–150
Deutsch SI, Mastropaolo J, Schwartz BL, Rosse RB, Morihisa JM (1989) A “glutamatergic hypothesis” of schizophrenia. Rationale for pharmacotherapy with glycine. Clin Neuropharmacol 12:1–13
Dracheva S, Marras SA, Elhakem SL, Kramer FR, Davis KL, Haroutunian V (2001) N-Methyl-D-aspartic acid receptor expression in the dorsolateral prefrontal cortex of elderly patients with schizophrenia. Am J Psychiatry 158:1400–1410
Durstewitz D, Seamans JK, Sejnowski TJ (2000) Neurocomputational models of working memory. Nat Neurosci 3(Suppl):1184–1191
Evins AE, Fitzgerald SM, Wine L, Rosselli R, Goff DC (2000) Placebo-controlled trial of glycine added to clozapine in schizophrenia. Am J Psychiatry 157:826–828
Goff DC, Henderson DC, Evins AE, Amico E (1999a) A placebo-controlled crossover trial of D-cycloserine added to clozapine in patients with schizophrenia. Biol Psychiatry 45:512–514
Goff DC, Lamberti JS, Leon AC, Green MF, Miller AL, Patel J, Manschreck T, Freudenreich O, Johnson SA (2008) A placebo-controlled add-on trial of the ampakine, CX516, for cognitive deficits in schizophrenia. Neuropsychopharmacology 33:465–472
Goff DC, Leahy L, Berman I, Posever T, Herz L, Leon AC, Johnson SA, Lynch G (2001) A placebo-controlled pilot study of the ampakine CX516 added to clozapine in schizophrenia. J Clin Psychopharmacol 21:484–487
Goff DC, Tsai G, Levitt J, Amico E, Manoach D, Schoenfeld DA, Hayden DL, McCarley R, Coyle JT (1999b) A placebo-controlled trial of D-cycloserine added to conventional neuroleptics in patients with schizophrenia. Arch Gen Psychiatry 56:21–27
Hamlyn E, Brand L, Shahid M, Harvey BH (2009) The ampakine, Org 26576, bolsters early spatial reference learning and retrieval in the Morris water maze: a subchronic, dose-ranging study in rats. Behav Pharmacol 20(7):662–667
Heresco-Levy U, Ermilov M, Lichtenberg P, Bar G, Javitt DC (2004) High-dose glycine added to olanzapine and risperidone for the treatment of schizophrenia. Biol Psychiatry 55:165–171
Heresco-Levy U, Javitt DC, Ebstein R, Vass A, Lichtenberg P, Bar G, Catinari S, Ermilov M (2005) D-Serine efficacy as add-on pharmacotherapy to risperidone and olanzapine for treatment-refractory schizophrenia. Biol Psychiatry 57:577–585
Heresco-Levy U, Javitt DC, Ermilov M, Mordel C, Horowitz A, Kelly D (1996) Double-blind, placebo-controlled, crossover trial of glycine adjuvant therapy for treatment-resistant schizophrenia. Br J Psychiatry 169:610–617
Jardemark K, Marcus MM, Konradsson A, Svensson TH (2005) The combination of nicotine with the D2 antagonist raclopride or the weak D4 antagonist L-745,870 generates a clozapine-like facilitation of NMDA receptor-mediated neurotransmission in pyramidal cells of the rat medial prefrontal cortex. Int J Neuropsychopharmacol 8:157–162
Jardemark K, Marcus MM, Shahid M, Svensson TH (2010) Effects of asenapine on prefrontal N-methyl-D-aspartate receptor-mediated transmission: involvement of dopamine D1 receptors. Synapse 64(11):870–874
Jardemark K, Ninan I, Svensson TH, Wang RY (2002) Differential effects of atypical and typical antipsychotic drugs on NMDA-receptor-mediated neurotransmission in pyramidal cells of the rat medial prefrontal cortex. Nord J Psychiatry 56:20
Jardemark KE, Konradsson A, Schilstrom B, Marcus MM, Svensson TH (2009) Differential effects of topiramate on prefrontal glutamatergic transmission when combined with raclopride or clozapine. Synapse 63:913–920
Jardemark KE, Liang X, Arvano V, Wang RY (2000) Subchronic treatment with either clozapine, olanzapine or haloperidol produces a hyposensitive response of the rat cortical cells to N-methyl-D-aspartate. Neuroscience 100:1–9
Javitt DC (2010) Glutamatergic theories of schizophrenia. Isr J Psychiatry Relat Sci 47:4–16
Javitt DC, Zukin SR (1991) Recent advances in the phencyclidine model of schizophrenia [see comments]. Am J Psychiatry 148:1301–1308
Johnson JW, Ascher P (1987) Glycine potentiates the NMDA response in cultured mouse brain neurons. Nature 325:529–531
Johnson SA, Luu NT, Herbst TA, Knapp R, Lutz D, Arai A, Rogers GA, Lynch G (1999) Synergistic interactions between ampakines and antipsychotic drugs. J Pharmacol Exp Ther 289:392–397
Jordan GR, McCulloch J, Shahid M, Hill DR, Henry B, Horsburgh K (2005) Regionally selective and dose-dependent effects of the ampakines Org 26576 and Org 24448 on local cerebral glucose utilisation in the mouse as assessed by 14C-2-deoxyglucose autoradiography. Neuropharmacology 49(2):254–264
Kalinichev M, Starr KR, Teague S, Bradford AM, Porter RA, Herdon HJ (2010) Glycine transporter 1 (GlyT1) inhibitors exhibit anticonvulsant properties in the rat maximal electroshock threshold (MEST) test. Brain Res 1331:105–113
Konradsson A, Marcus MM, Hertel P, Svensson TH, Jardemark KE (2006) Inhibition of the glycine transporter GlyT-1 potentiates the effect of risperidone, but not clozapine, on glutamatergic transmission in the rat medial prefrontal cortex. Synapse 60:102–108
Lane HY, Chang YC, Liu YC, Chiu CC, Tsai GE (2005) Sarcosine or D-serine add-on treatment for acute exacerbation of schizophrenia: a randomized, double-blind, placebo-controlled study. Arch Gen Psychiatry 62:1196–1204
Lane HY, Huang CL, Wu PL, Liu YC, Chang YC, Lin PY, Chen PW, Tsai G (2006) Glycine transporter I inhibitor, N-methylglycine (sarcosine), added to clozapine for the treatment of schizophrenia. Biol Psychiatry 60:645–649
Lane HY, Lin CH, Huang YJ, Liao CH, Chang YC, Tsai GE (2010) A randomized, double-blind, placebo-controlled comparison study of sarcosine (N-methylglycine) and D-serine add-on treatment for schizophrenia. Int J Neuropsychopharmacol 13:451–460
Li CC (1964) Change-over design. Introduction to experimental statistics. McGraw-Hill, New York, pp 207–226
Lidö HH, Stomberg R, Fagerberg A, Ericson M, Söderpalm B (2009) The glycine reuptake inhibitor org 25935 interacts with basal and ethanol-induced dopamine release in rat nucleus accumbens. Alcohol Clin Exp Res 33(7):1151–1157
Luby ED, Cohen BD, Rosenbaum G, Gottlieb JS, Kelley R (1959) Study of a new schizophrenomimetic drug; sernyl. AMA Arch Neurol Psychiatry 81:363–369
Marcus MM, Jardemark KE, Wadenberg ML, Langlois X, Hertel P, Svensson TH (2005) Combined alpha2 and D2/3 receptor blockade enhances cortical glutamatergic transmission and reverses cognitive impairment in the rat. Int J Neuropsychopharmacol 8:315–327
Marcus MM, Wiker C, Franberg O, Konradsson-Geuken A, Langlois X, Jardemark K, Svensson TH (2010) Adjunctive alpha2-adrenoceptor blockade enhances the antipsychotic-like effect of risperidone and facilitates cortical dopaminergic and glutamatergic, NMDA receptor-mediated transmission. Int J Neuropsychopharmacol 13:891–903
Molander A, Lidö HH, Löf E, Ericson M, Söderpalm B (2007) The glycine reuptake inhibitor Org 25935 decreases ethanol intake and preference in male Wistar rats. Alcohol Alcohol 42(1):11–18
Möhler H, Boison D, Singer P, Feldon J, Pauly-Evers M, Yee BK (2011) Glycine transporter 1 as a potential therapeutic target for schizophrenia-related symptoms: evidence from genetically modified mouse models and pharmacological inhibition. Biochem Pharmacol 81:1065–1077
Neill JC, Barnes S, Cook S, Grayson B, Idris NF, McLean SL, Snigdha S, Rajagopal L, Harte MK (2010) Animal models of cognitive dysfunction and negative symptoms of schizophrenia: focus on NMDA receptor antagonism. Pharmacol Ther 128:419–432
Ninan I, Jardemark KE, Wang RY (2003a) Olanzapine and clozapine but not haloperidol reverse subchronic phencyclidine-induced functional hyperactivity of N-methyl-D-aspartate receptors in pyramidal cells of the rat medial prefrontal cortex. Neuropharmacology 44:462–472
Ninan I, Jardemark KE, Wang RY (2003b) Differential effects of atypical and typical antipsychotic drugs on N-methyl-D-aspartate- and electrically evoked responses in the pyramidal cells of the rat medial prefrontal cortex. Synapse 48:66–79
Ninan I, Wang RY (2003) Modulation of the ability of clozapine to facilitate NMDA- and electrically evoked responses in pyramidal cells of the rat medial prefrontal cortex by dopamine: pharmacological evidence. Eur J Neurosci 17:1306–1312
Olney JW, Farber NB (1995) Glutamate receptor dysfunction and schizophrenia. Arch Gen Psychiatry 52:998–1007
Olsen CK, Kreilgaard M, Didriksen M (2006) Positive modulation of glutamatergic receptors potentiates the suppressive effects of antipsychotics on conditioned avoidance responding in rats. Pharmacol Biochem Behav 84:259–265
Paxinos G, Watson C (2007) The rat brain in sterotaxic coordinates, 6th edn. Academic, London
Potkin SG, Jin Y, Bunney BG, Costa J, Gulasekaram B (1999) Effect of clozapine and adjunctive high-dose glycine in treatment-resistant schizophrenia. Am J Psychiatry 156:145–147
Salmi P, Samuelsson J, Ahlenius S (1994) A new computer-assisted two-way avoidance conditioning equipment for rats: behavioral and pharmacological validation. J Pharmacol Toxicol Methods 32:155–159
Shahid M, Walker GB, Zorn SH, Wong EH (2009) Asenapine: a novel psychopharmacologic agent with a unique human receptor signature. J Psychopharmacol 23(1):65–73
Shu Y, Hasenstaub A, McCormick DA (2003) Turning on and off recurrent balanced cortical activity. Nature 423:288–293
Siegel S, Castellan NJ Jr (1988) Nonparametric statistics for the behavioral sciences. McGraw-Hill, New York
Smith KE, Borden LA, Hartig PR, Branchek T, Weinshank RL (1992) Cloning and expression of a glycine transporter reveal colocalization with NMDA receptors. Neuron 8:927–935
Su XW, Li XY, Banasr M, Koo JW, Shahid M, Henry B, Duman RS (2009) Chronic treatment with AMPA receptor potentiator Org 26576 increases neuronal cell proliferation and survival in adult rodent hippocampus. Psychopharmacology (Berl) 206(2):215–222
Svensson TH (2000) Dysfunctional brain dopamine systems induced by psychotomimetic NMDA-receptor antagonists and the effects of antipsychotic drugs. Brain Res Brain Res Rev 31:320–329
Tsai G, Lane HY, Yang P, Chong MY, Lange N (2004) Glycine transporter I inhibitor, N-methylglycine (sarcosine), added to antipsychotics for the treatment of schizophrenia. Biol Psychiatry 55:452–456
Tsai GE, Yang P, Chung LC, Tsai IC, Tsai CW, Coyle JT (1999) D-Serine added to clozapine for the treatment of schizophrenia. Am J Psychiatry 156:1822–1825
Vengeliene V, Leonardi-Essmann F, Sommer WH, Marston HM, Spanagel R (2010) Glycine transporter-1 blockade leads to persistently reduced relapse-like alcohol drinking in rats. Biol Psychiatry 68(8):704–711
Wadenberg ML (2010) Conditioned avoidance response in the development of new antipsychotics. Curr Pharm Des 16:358–370
Wadenberg ML, Hicks PB (1999) The conditioned avoidance response test re-evaluated: is it a sensitive test for the detection of potentially atypical antipsychotics? Neurosci Biobehav Rev 23:851–862
Wadenberg ML, Wiker C, Svensson TH (2007) Enhanced efficacy of both typical and atypical antipsychotic drugs by adjunctive alpha2 adrenoceptor blockade: experimental evidence. Int J Neuropsychopharmacol 10:191–202
Wadenberg M-LG, Soliman A, VanderSpek SC, Kapur S (2001) Dopamine d(2) receptor occupancy is a common mechanism underlying animal models of antipsychotics and their clinical effects. Neuropsychopharmacology 25:633–641
Wang XJ (1999) Synaptic basis of cortical persistent activity: the importance of NMDA receptors to working memory. J Neurosci 19:9587–9603
Acknowledgements
This work was supported by the Swedish Research Council grant nos. 4747 and 15049, the Karolinska Institutet, and a research grant from Department of Molecular Pharmacology, MSD, Newhouse, UK.
Conflict of interest
Apart from the grant received from MSD, there is no conflict of interest. Kent Jardemark is employee at the Karolinska Institutet and Chalmers University of Technology. Torgny H. Svensson, Monica M. Marcus, and Anna Malmerfelt are employees at the Karolinska Institutet, and Mohammed Shahid is a previous employee at Department of Molecular Pharmacology, MSD, Newhouse, UK. All experiments were approved by and conducted in accordance with the local Animal Ethics Committee, Stockholm North and the Karolinska Institutet, Sweden.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jardemark, K., Marcus, M.M., Malmerfelt, A. et al. Differential effects of AMPA receptor potentiators and glycine reuptake inhibitors on antipsychotic efficacy and prefrontal glutamatergic transmission. Psychopharmacology 221, 115–131 (2012). https://doi.org/10.1007/s00213-011-2554-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-011-2554-3