Abstract
Objective
Current pharmacological treatments for depression have a significant treatment-onset-response delay, an insufficient efficacy for many patients and fail to reverse cognitive dysfunction. Erythropoietin (EPO) has neuroprotective and neurotrophic actions and improves cognitive function in animal models of acute and chronic neurodegenerative conditions and in patients with cognitive decline.
Methods
We systematically reviewed the published findings from animal and human studies exploring the potential of EPO to treat depression-related cognitive dysfunction and depression.
Results
We identified five animal studies (two in male rats, two in male mice and one in male rats and mice) and seven human proof-of-concept studies (five in healthy volunteers and two in depressed patients) that investigated the above. All of the reviewed animal studies but one and all human studies demonstrated beneficial effects of EPO on hippocampus-dependent memory and antidepressant-like effects. These effects appear to be mediated through direct neurobiological actions of EPO rather than upregulation of red cell mass.
Conclusions
The reviewed studies demonstrate beneficial effects of EPO on hippocampus-dependent memory function and on depression-relevant behavior, thus highlighting EPO as a candidate agent for future management of cognitive dysfunction and mood symptoms in depression. Larger-scale clinical trials of EPO as a treatment for mood and neurocognitive symptoms in patients with mood disorder are therefore warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Depression is a leading course of disability across the globe owing to its high prevalence, chronic and recurrent nature and comorbidity with other chronic illnesses (Moussavi et al. 2007). Most available antidepressant drug treatments have slow onset of action and insufficient efficacy in 30–40% of patients (Baldessarini 1989; Giacobbe et al. 2009) and fail to reverse neurocognitive dysfunction (Behnken et al. 2010; Hasselbalch et al. 2010; Kessing 1998; Paradiso et al. 1997; Preiss et al. 2009; Reppermund et al. 2007; Smith et al. 2006; Weiland-Fiedler et al. 2004). In particular, there is substantial evidence that memory impairments persist into periods of remission (ibid.), although findings are not unanimous (Biringer et al. 2007). Memory impairment is associated with reduced socio-occupational functioning in patients with affective disorder (Martinez-Aran et al. 2004), which highlights this aspect of cognitive function as a particularly important treatment target.
The discovery of ongoing hippocampal neurogenesis and neuroplasticity in the adult brain has generated enormous interest in depression research over the past decades. Compiling evidence suggests that newborn neurons are essential for hippocampus-dependent memory function (Castilla-Ortega et al. 2011) and for behavioral effects of antidepressant drug treatment (Santarelli et al. 2003). New neurons in their immature stage (from about 1 week) may, in fact, be more important for some aspects of memory formation than mature neurons, given their high degree of plasticity and dependence of environmental modulation (Castilla-Ortega et al. 2011). Computational simulation shows that neurogenesis improves network capacity for new information storage and forgetting of old irrelevant information (Chambers et al. 2004). Hippocampal neurogenesis may hence improve learning and adaptive cognitive and emotional responses to novel challenging contexts, whereas reduced neurogenesis might impair ability to cope with stress and be involved in psychiatric disorders like depression (ibid.). Indeed, it is a prevailing hypothesis that depression is caused by breakdown of neural plasticity arising from ongoing inflammatory processes and an over-active stress-response system (Duman and Monteggia 2006; Miller et al. 2009), which leads to structural and functional abnormalities in a fronto-limbic circuitry (Belmaker and Agam 2008; Berton and Nestler 2006; Manji et al. 2000). In particular, stress-induced elevation of glucocorticoids has been shown to reduce hippocampal neurogenesis and cause hippocampus-dependent memory deficits (Borcel et al. 2008; Kitraki et al. 2004; Yun et al. 2010) and depression-like behavior in animals (Duman et al. 1999). In humans, chronic stress is associated with increased inflammatory response, elevated cortisol levels (Miller et al. 2009) and hippocampus volume reduction paired with hippocampus-dependent memory deficits (Lupien et al. 1998), a hypothesized key pathophysiological mechanism in depression (Campbell and Macqueen 2004). In contrast, increased hippocampal neurogenesis and plasticity and attenuation of inflammatory processes may be central mechanisms underlying improvement of symptoms and cognitive function following long-term antidepressant drug treatment (Berton and Nestler 2006; Duman et al. 1999; Manji et al. 2003), although it should be noted that this hypothesis remains controversial (Herbert 2008). Novel treatment strategies with more rapid and enduring effects on hippocampal neural plasticity and which target hippocampus-dependent memory function may thus impact future management of depression.
Erythropoietin (EPO) is synthesized in the kidney, and it was originally identified for its role in the regulation of the red cell line (Jacobson et al. 1957). More recently, EPO and an EPO receptor (EpoR) system were also demonstrated in the central nervous system of animals and humans (Marti et al. 1996), and they are essential for neurodevelopment and adult neurogenesis and protection (Brines and Cerami 2005). High expression of EPO and EpoR in the hippocampal formation suggests that EPO plays an important role in hippocampal functioning. In high doses (≥500 IU/kg body weight), systemically administered EPO crosses the blood-brain barrier in therapeutic effective concentrations (Brines et al. 2000; Ehrenreich et al. 2004) and exerts neuroprotective and neurotrophic effects in traumatic, hypoxic-ischemic, excitotoxic and inflammatory brain damage (Brines et al. 2000; Morishita et al. 1997; Sakanaka et al. 1998) and neurodegenerative and neuropsychiatric conditions (Agnello et al. 2002; Li et al. 2004; Sattler et al. 2004; Siren et al. 2006). These morphological effects of EPO are accompanied by enhanced cognitive functioning in both acute and chronic neural injury models, including functional inactivation of hippocampus by fimbria-fornix transaction (Mogensen et al. 2004), embolic stroke (Ding et al. 2010; Wang et al. 2004), closed head injury (Yatsiv et al. 2005), neonatal hypoxic-ischemic or hyperoxic insult (Kumral et al. 2003; Yis et al. 2008), functional inactivation of amygdala (Miu et al. 2004), spinal chord injury (Boran et al. 2005) and progressive neurodegenerative conditions (Sargin et al. 2009; Siren et al. 2006). Notably, repeated EPO treatment also enhances cognitive functioning in healthy animals (El-Kordi et al. 2009). These effects highlight EPO as a candidate treatment for neurocognitive dysfunction in patients with neurodegenerative or neuropsychiatric conditions. Indeed, recent translational studies have shown beneficial effects of EPO treatment on cognitive function in patients with multiple sclerosis or chronic schizophrenia (Ehrenreich et al. 2004, 2007a, b) as well as in extremely preterm infants (Bierer et al. 2006; Brown et al. 2009). EPO treatment of preterm infants with intraventricular hemorrhage was associated with increased intelligence at age 10–13 years compared with untreated children (Neubauer et al. 2010), suggesting that the cognitive effects of EPO can be long-lasting. Notably, cognitive improvement in EPO-treated schizophrenic patients was accompanied by decrease in gray matter loss, pointing to an ability of EPO to counteract ongoing neurodegenerative processes in neuropsychiatric disease (Wustenberg et al. 2011).
Several mechanisms mediate the effects of EPO on neuronal plasticity and neuroprotection, including activation of antiapoptotic, antioxidant and anti-inflammatory signaling in neurons, glial and cerebrovascular endothelial cells, promotion of axonal regrowth and dendritic sprouting, and upregulation of hippocampal brain-derived neurotrophic factor (BDNF) and of neurogenesis, as well as neuronal differentiation and migration (Byts and Siren 2009; Girgenti et al. 2009; Leconte et al. 2011; Siren et al. 2009). A key biological mechanism is the enhancement of long-term potentiation (LTP), a cellular correlate of learning processes, in the CA1 region of the hippocampus, which alters short-term synaptic plasticity and synaptic transmission, shifting the balance of excitatory and inhibitory activity (Adamcio et al. 2008; Sargin et al. 2011). Networks of EPO-treated primary hippocampal neurons develop lower overall spiking activity but enhanced bursting in discrete neuronal assemblies. At the level of developing single neurons, EPO treatment reduces the typical increase in excitatory synaptic transmission without changing the number of synaptic boutons, consistent with prolonged functional silencing of synapses (Adamcio et al. 2008). Taken together, EPO improves cognitive function by modulating plasticity, synaptic connectivity and activity in the hippocampus which, in turn, could burst the activity of selected synapses together with persistent silencing of other synapses.
Encouraged by the beneficial modulatory effects of EPO on inflammatory processes and hippocampal neuroplasticity, a new line of research investigates the potential of EPO as a treatment for depressive symptoms and neurocognitive dysfunction in mood disorders such as clinical depression. The current review examines studies of the effects of EPO on hippocampus-dependent memory and anxiety- and depression-relevant behavior in animal models of depression and in human models of antidepressant drug action.
Methods
Searches on the PubMed and PsychInfo databases were performed in May 2011 using the following search profile:
((Erythropoietin) AND (“Mood Disorders”[Mesh] OR “Depression”[Mesh] OR “antidepressive agents”[MeSH Terms] OR “antidepressive agents"[Pharmacological Action])) OR ((Erythropoietin) AND (“amygdala”[MeSH Terms] OR “hippocampus”[MeSH Terms] OR “memory”[MeSH Terms] OR “neuronal plasticity”[MeSH Terms])).
Additional hand searches were carried out to ensure inclusion of all relevant articles. The selection criteria are the following: original investigations with a double-blind placebo-controlled design of the effects of EPO on (1) hippocampus-dependent memory function and depression- and anxiety-relevant behavior in animal models and (1) hippocampus-dependent memory and depression-relevant neurocognitive responses in healthy human volunteers and patients with clinical depression. In addition, observational studies of patients with clinical depression were included.
Results
The systematic search identified 134 articles of which five animal studies and seven human studies met the criteria of this study.
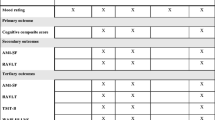
Effects of EPO in animal studies
Of the five identified animal studies, two investigated the effects of EPO on hippocampus-dependent memory function (Adamcio et al. 2008; Mogensen et al. 2004), four investigated the effects of EPO anxiety-relevant behavior (Adamcio et al. 2008; Girgenti et al. 2009; Leconte et al. 2011; Miu et al. 2004) and two explored the effects of EPO on depression-relevant behavior (Girgenti et al. 2009; Leconte et al. 2011). Characteristics of the animals, experimental models, EPO treatment regime and the results of these studies are presented in Table 1.
Effects of EPO on hippocampus-dependent memory
The first study of the effects of EPO on hippocampus-dependent memory function by Mogensen et al. (2004) (Table 1) investigated the effects of a single intraperitoneally (ip.) administrated dose of EPO (5000 IU/kg body weight) vs. saline on place-learning in a Morris water maze after functional inactivation of the hippocampus by fimbria-fornix transection (FF) and in sham-operated rats. The study demonstrated that a single dose of EPO not only improved functional recovery in FF rats but also altered behavior in the intact, sham-operated rats. Although EPO-treated, intact rats did not show improved task performance, they did display a reduction in wall-clinging behavior compared with vehicle-treated rats, suggestive of a decreased stress response (Stratton et al. 1976). In contrast with the absence of memory improvement in the healthy animals after a single dose of EPO (Mogensen et al. 2004), EPO treatment of healthy mice every other day over 3 weeks resulted in enhanced hippocampus-related memory (Adamcio et al. 2008). Repeated EPO administration may thus be required for memory improvement in healthy animals. Interestingly, the memory improvement lasted for up to 3 weeks after treatment cessation (ibid.), at which time point hematocrit levels were comparable in the two groups. Although it cannot be out-ruled that greater hematocrit levels were involved in the immediate memory improvement, this finding indicates that the memory and hematopoietic effects of EPO are not directly related. Indeed, in-vitro analysis demonstrated that the beneficial effect on hippocampus-dependent memory function was associated with enhanced synaptic plasticity and LTP in the hippocampus (ibid). Other evidence for beneficial effects of EPO on hippocampus-dependent memory comes from a study by Leconte et al. (2011) who found that EPO treatment (40 μg/kg corresponding to 5,000 IU/kg) given twice per week for 5–6 weeks improved object recognition performance in healthy mice. This type of memory in the rodent has been related to human episodic memory (ibid.), which could point to a clinical potential of EPO to treat patients remitted from depression with profound deficits in episodic memory performance (Behnken et al. 2010; Hasselbalch et al. 2010; Kessing 1998; Paradiso et al. 1997; Preiss et al. 2009; Reppermund et al. 2007; Smith et al. 2006; Weiland-Fiedler et al. 2004). Notably, beneficial effects on hippocampus-dependent memory were also demonstrated with a non-erythropoietic variant of EPO, carbamoylated EPO (CEPO), suggesting that the hematopoietic action of EPO is not essential for its cognitive effects (Leconte et al. 2011). Further evidence that direct neurotrophic effects may underlie the capacity of EPO to enhance hippocampus-dependent memory comes from a study using a transgenic strategy (Sargin et al. 2011). The study demonstrates that transgenic expression of the EPO receptor system in the hippocampus and cortical regions was associated with enhanced spatial and social memory, an effect opposite to the pronounced emotional memory impairment in a genetic rat model of depression (Eriksson et al. 2011). Together, these studies suggest that EPO reduces stress levels in aversive conditions and improves depression-relevant hippocampus-dependent memory.
Effects of EPO on anxiety-related behavior
Four studies have investigated the possible effects of EPO on anxiety-related behavior in animal models (Adamcio et al. 2008; Girgenti et al. 2009; Leconte et al. 2011; Miu et al. 2004). The first study of the effects of EPO on fear response had a neuroprotective scope, investigating the ability of EPO to protect fear-conditioning performance against functional inactivation of the amygdala in rats (Miu et al. 2004). The study demonstrated that a single EPO infusion (2.5 IU) to the lateral nucleus of the amygdala in addition to an excitotoxic dose of glutamate was capable of preserving normal fear conditioning performance as well as long-term memory of fear response (ibid.). Fear conditioning recruits the same neural circuits implicated in human mood disorders and may arise from pathological activation of amygdala (Drevets 2003; Erickson et al. 2003; McEwen 2005). It has been hypothesized that this amygdala hyper-activity in depression is a result of disrupted top-down control of amygdala by the PFC and hippocampus following excitotoxic effects of prolonged glucocorticoid elevation (ibid.). In light of this, the ability of EPO to preserve fear conditioning after excitotoxic damage to the limbic system could point to EPO as a candidate compound to restore normal amygdala functioning in patients with depression. Evidence for anxiolytic effects of EPO comes from a study by Girgenti et al. (2009), which showed that EPO (500 U/kg body weight) vs. placebo treatment to rats over 4 days resulted in decreased novelty-induced hypophagia (Dulawa and Hen 2005). This anxiolytic effect is usually only apparent with chronic antidepressant drug administration (ibid.) and corresponds to a similar delay necessary to decrease anxiety in clinical populations (Sinclair et al. 2009). Given this time-lag to anxiolytic actions of existing antidepressants, the onset of such effects after only 4 days of EPO administration points to an ability of EPO to rapidly attenuate anxiety symptoms (Girgenti et al. 2009). Results are not uniform, however, with two other studies showing no anxiolytic effects after 3 or 5 weeks EPO administration to mice in the elevated plus maze (Adamcio et al. 2008) or light-dark transition test (Leconte et al. 2011), respectively. In contrast, Leconte and colleagues did reveal modest anxiolytic after 5 weeks of CEPO treatment (2011). The discrepancy between the findings of the studies may reflect differences in the employed anxiety tests and/or treatment schedules (short-term vs. long-term administration). Taken together, there is some evidence for rapid anxiolytic effects of short-term administration of EPO, although these effects may subside with chronic administration.
Effects of EPO on depression-relevant behavior
Two studies have investigated the potential antidepressant properties of EPO in animal models. Girgenti et al. (2009) demonstrated that short-term (4 day) EPO vs. saline administration to rats produced a modest (~35%) decrease in immobility, a display of helplessness in a forced swimming test. This was a specific antidepressant-like effect as there was no change in general locomotor activity between the groups (ibid.). Comparison of long-term EPO and CEPO treatment (biweekly for 5–6 weeks) of healthy mice revealed modest antidepressant-like behavioral effects of CEPO, but not of EPO, as reflected by reduced immobility in CEPO-treated animals in a tail suspension test (Leconte et al. 2011). These divergent findings may be related to differences in species, treatment regimes or behavioral tests.
In summary, there is some evidence for rapid antidepressant-like effects of short-term EPO administration and of long-term CEPO administration in these animal models of depression. Together with the evidence that EPO improves hippocampus-dependent memory and may have early transient effects on fear response, this supports the notion that EPO may have rapid effects on depression and anxiety symptoms in patients with mood disorder.
Effects of EPO in human populations
Since the introduction of human recombinant EPO in the 1980s, EPO has been used to treat millions of patients with anemia, and it is not a new observation that long-term EPO treatment improves cognitive function, mood and well-being in these patients (Jelkmann 1992; Pickett et al. 1999). In contrast, short-term (5 days) EPO vs. placebo treatment of anemic women showed no effect on postpartum blues (Meyer et al. 1995). Until recently, the beneficial effects of EPO on mood and cognition were therefore simply attributed to reversal of patients’ anemic state with long-term EPO treatment (Jelkmann 1992; Pickett et al. 1999). This perception was challenged with the discovery of beneficial neurobiological and neurocognitive effects of EPO in brain-damaged as well as healthy animals. Indeed, translational studies have now demonstrated that long-term EPO treatment produces long-lasting improvement of cognitive function in (non-anemic) patients suffering from neurodegenerative conditions like multiple sclerosis and schizophrenia (Ehrenreich et al. 2007a, b). The interpretation of the cognitive effects as neural in origin was, however, confounded by the concomitant increase in red cell mass in the EPO vs. placebo-treated patients due to the long-term treatment schedule. We therefore performed a series of studies in healthy volunteers using single administration of EPO (40,000 IU; similar to previously used doses (Ehrenreich et al. 2007a, b)), which has no effects on red cell mass, while maintaining an effect on neurocognitive function (Miskowiak et al. 2007a, b, c, 2008a, b).
Effects of EPO on hippocampus-dependent memory in healthy volunteers
The first study of direct neurobiological actions on cognitive function in humans investigated the effects of a single high dose of EPO (40,000 IU) vs. placebo to healthy volunteers on hippocampus-dependent memory 1 week after administration using functional magnetic resonance imaging (fMRI) (Miskowiak et al. 2007b). This interval between EPO administration and testing was chosen because of a similar time-lag for downstream effects of neurotrophic signaling to emerge and for newborn neurons to develop dendrites and begin their functional integration into the hippocampal circuit (Aimone et al. 2006). Indeed, the study revealed enhanced memory-related hippocampus response following EPO vs. placebo administration in the absence of changes in red cell mass, which suggests a direct neurobiological mechanism. See characteristics of the study population, paradigm, treatment regime and results in Table 2. Greater hippocampal response in EPO-treated volunteers is consistent with increased hippocampal BDNF signaling (Hariri et al. 2003; Viviani et al. 2005) and improved recognition memory (Cansino et al. 2002), as well as enhanced hippocampal plasticity and neurogenesis 1 week after EPO administration (Ransome and Turnley 2007). It is important to acknowledge that the fMRI blood-oxygen-level dependent (BOLD) measure is not a specific measure of neural plasticity or neurogenesis per se. It was therefore necessary to make an assumption, which we tested in the second fMRI study. Given the time-lag of several days for functional effects of increased neuroplasticity to emerge (Aimone et al. 2006), a neuroplasticity mechanism of EPO would be associated with no memory-related hippocampus effect at an earlier time point after administration. If, on the other hand, the hippocampal effect of EPO originated from carry-over effects on oxygen availability or neurotransmitter release (Brines and Cerami 2005), this effect would be stronger at an earlier time point. Indeed, we found no effect of EPO vs. placebo on memory-relevant hippocampal response 3 days after administration (Miskowiak et al. 2007a), in support of a neuroplasticity mechanism which emerges with a longer time delay. For the characteristics of the study population, paradigm, treatment regime and results, see Table 2. Given the hypothesized role of hippocampal neuroplasticity in the pathophysiology and treatment of depression, these findings highlight a potential antidepressant action of EPO.
Effects of EPO in healthy volunteer models of antidepressant drug action
Depression is associated with negative bias in attention, interpretation and memory, which correlates positively with illness severity and duration (Bradley et al. 1995). In particular, patients with depression show reduced recognition of positive facial expressions (Lembke and Ketter 2002) and a bias toward interpreting others’ facial expressions as negative, which predicts subsequent relapse (Bouhuys et al. 1999). Antidepressant compounds with different neurochemical actions down-regulate the neural and cognitive processing of negative vs. positive emotional information, whereas drugs devoid of antidepressant effects have no such effects (Harmer et al. 2010; Harmer 2010). Notably, this change in emotional bias occurs early in treatment before any change in mood and has been suggested as an important human biomarker model of antidepressant drug action. In two separate studies (3-day and 7-day studies), we therefore explored the effects of EPO versus saline on neural and behavioral measures of emotional processing using two similar fMRI paradigms probing emotional face processing (Miskowiak et al. 2007c, 2008b). In the first study, we investigated the effects of EPO versus saline on neural and behavioral response to fearful and happy faces 7 days after administration (Miskowiak et al. 2007c) in the same population of healthy volunteers, as implemented in the previously reviewed 7-day study (Miskowiak et al. 2007b) (see Table 2). The study demonstrated that EPO reduced the neural response in occipito-parietal regions to fearful facial expressions and the behavioral recognition of this emotion. This is consistent with decreased attentional processing and perception of threat-relevant stimuli and is similar to effects seen with 7-day administration of serotonergic and noradrenergic drugs to healthy volunteers (Harmer et al. 2004, 2006). Unexpectedly, EPO also produced an acute, transient improvement of mood (Miskowiak et al. 2007c), which is remarkable given the significant time-lag to antidepressant actions of conventional drug treatments of depression. In the second study, we therefore investigated this rapid mood change by assessing the accompanying neuronal and psychological actions on day 3 after EPO (40,000 IU) vs. placebo administration in the same group of volunteers as in the previously reviewed 3-day study (Miskowiak et al. 2008b). At this time point, EPO enhanced the neural response in occipito-parietal regions to facial expressions of happiness and fear consistent with increased vigilance to facial displays of emotion in general (ibid.). These neuronal effects were accompanied by a general improvement in the recognition of emotional facial expressions irrespective of valence after EPO vs. placebo administration. Notably, the effects were independent of the changes in red blood cells, suggesting that they originated from direct neurobiological actions of EPO (ibid.). The enhanced recognition of happiness and fear in EPO-treated volunteers is similar to acute effects of serotonergic antidepressants (Harmer et al. 2003) and in contrast with the decreased neural and behavioral response to fearful faces 1 week after EPO administration (Miskowiak et al. 2007c). This reversal of effects from day 3 to day 7 after EPO administration is strikingly similar to previous findings with SSRI administration to healthy volunteers, where increased fear recognition is seen with acute administration but is reduced after 7 days of treatment relative to matched placebo treatment (Harmer et al. 2003, 2004). This suggests that EPO taps in to emotion processing in ways that resemble conventional antidepressants: early increases in the processing of happy and fearful facial expressions accompanied by a reversal of increased to decreased fear processing over time. Notably, the study replicated the rapid 3-day improvement of mood in EPO-treated volunteers, in further support of a potential antidepressant mechanism (Miskowiak et al. 2008b).
Effects of EPO in biomarker models in patients with depression
The beneficial effects of EPO on memory-relevant hippocampus activity and antidepressant-like actions in healthy volunteers encouraged an investigation of the effects of EPO vs. placebo in a clinically depressed population 3 days after administration (Miskowiak et al. 2009, 2010a). The neuroanatomical underpinnings for the negative bias in depression have often been investigated with affective picture stimuli such as scenes from the International Affective Picture System (IAPS) (Lang et al. 1997) and emotional facial expressions (Britton et al. 2006). We therefore explored the effects of EPO on the neural and cognitive response to emotional IAPS pictures and to facial stimuli. For clarity reasons, the results from these largely overlapping study populations were reported in two separate papers (Miskowiak et al. 2009, 2010a). For the characteristics of the study populations, paradigms, treatment regime and results, see Table 3. The first study revealed that EPO (40,000 IU) reduced neural response in the left hippocampus and in the right-side fronto-parietal regions during encoding of negative compared with positive pictures in acutely depressed patients. This effect of EPO is opposite to the hippocampal over-recruitment during encoding of negative vs. positive or neutral pictures which has been suggested as a neural mechanism of the negative memory bias in depression (Hamilton and Gotlib 2008). The reduced fronto-parietal response during encoding of negative vs. positive pictures following EPO administration is consistent with reduced attentional processing of negative emotional information (Pourtois et al. 2006) and replicates the effects of EPO in healthy volunteers 7 days after administration (Miskowiak et al. 2007c). These effects on neuronal responses were accompanied by greater memory specificity in EPO-treated patients as reflected by fewer memory intrusions or false memories. This suggests that EPO improves memory accuracy in depressed individuals, an effect which could be clinically important given the compromised memory function in this group.
The second task used in this patient study demonstrated that EPO also modulates the neural and cognitive processing of emotional facial expressions in a manner consistent with an antidepressant mechanism 3 days after administration (Miskowiak et al. 2010a). EPO specifically decreased left amygdala-hippocampal and parietal response to fearful faces, which was paired with reduced recognition of fearful facial expressions after the scan. This is similar to effects of conventional antidepressants on neural and behavioral response to emotional faces and to the effects of EPO on face processing in healthy volunteers. The neurocognitive effects in these studies were likely to have a neurobiological mechanism as they occurred in the absence of changes in red cell mass. Interestingly, mood was improved in all patients, perhaps as a result of a large placebo effect, which may have masked any potential subtle effects of EPO on mood (ibid.). Consistent with this interpretation, a recent case study revealed distinct antidepressant effects (~30% decrease in HDRS-scores) after 3 weeks of EPO, but not placebo, injections on a treatment-resistant, severely depressed patient (Sargin et al. 2010). If changes in the processing of emotional information are important in the therapeutic actions of antidepressant drugs as hypothesized (Harmer et al. 2010; Harmer 2010), then EPO may have the ability to improve mood in clinically depressed patients. Together with the known effects on neuroplasticity in animal models, these findings may be important in establishing EPO as a new candidate treatment for affective disorders.
Conclusion and future directions
In conclusion, the findings of the presently reviewed studies highlight EPO as a candidate agent for neuroprotective add-on treatment strategies of depression and other neuropsychiatric conditions marked by progressive neural dysfunction and atrophy. Although evidence is still sparse, the reported findings offer hope that novel agents such as EPO, which directly target neuroplasticity and neurogenesis, represent a new improved generation of antidepressants, which overcome limitations of conventional treatments by addressing the large proportion of patients who so far remain treatment resistant and by targeting pervasive neurocognitive deficits in these patients. If the beneficial effects of EPO on brain function in these pre-clinical and short-term clinical proof-of-concept studies translate into clinical efficacy in treatment of depressive symptoms and cognitive dysfunction in mood disorder, this would have profound impact on patient health and economical burden for society. An ongoing clinical trial with expected completion in 2012 investigates whether these early effects of EPO translate into improvement of mood and neurocognitive function with repeated administration in patients with treatment-resistant depression or bipolar disorder (Miskowiak et al. 2010b). The trial also investigates if any improvement of mood and cognitive function persists at 6 weeks follow-up. Cognitive improvement in multiple sclerosis was maintained for a minimum of 6 months after treatment cessation (Ehrenreich et al. 2007a). It is thus conceivable that any EPO-associated mood and cognitive enhancement in patients with affective disorder could be long-lasting and chronic maintenance treatment therefore may be unnecessary.
Despite the promising evidence for EPO as a new add-on treatment for mood disorder, it is important to acknowledge two major limitations of EPO, which may limit its clinical use. The hematopoietic action of EPO with repeated administration would necessitate close monitoring of hematocrit and thrombocyte levels and, potentially, bloodlettings in these non-anemic patient populations. The reviewed studies demonstrated no change in blood pressure with single or repeated EPO administration (Ehrenreich et al. 2007a, b; Miskowiak et al. 2008b), but regular blood pressure monitoring is warranted with long-term EPO treatment, given a potential risk of developing hypertension as known for patients with chronic renal failure. Studies evaluating the effects of novel EPO derivatives such as CEPO and asialoerythropoietin (asialoEPO) (Erbayraktar et al. 2003; Leist et al. 2004), which exert neuroprotective actions in the absence of hematological effects, are therefore warranted. If the beneficial effects of these compounds were confirmed in healthy and depressed individuals, this could have great clinical value for long-term treatment of mood disorder. The potential risk that EPO promotes malignant tumor growth is still controversial (Jelkmann et al. 2008). Although low-dose EPO is widely used to treat chemotherapy-induced anemia to avoid red blood cell transfusions, EPO is discontinued immediately after chemotherapy completion and is avoided in any non-anemic cancer patients (ibid.). Given this potential risk, a history of cancer was an exclusion criterion in the reviewed human studies and should be a general contraindication for EPO treatment. Another clinical disadvantage is the necessity to administer EPO intravenously or subcutaneously, which is unpleasant and expensive. Evidence of neuroprotective effects of intranasal delivery of EPO in rats (Garcia-Rodriguez and Sosa-Teste 2009; Genc et al. 2011; Yu et al. 2005) therefore deserves to be followed up by investigation of the neurocognitive effects in humans. Intranasal application necessitates significantly smaller doses of EPO for neuroprotection, which would help overcome the problems associated with hematopoietic effects of larger doses. If intranasal delivery of EPO improves neurocognitive function in man, this would highlight intranasal EPO as a simple and non-invasive candidate treatment of neuropsychiatric illness in the future.
References
Adamcio B, Sargin D, Stradomska A, Medrihan L, Gertler C, Theis F et al (2008) Erythropoietin enhances hippocampal long-term potentiation and memory. BMC Biol 6:37
Agnello D, Bigini P, Villa P, Mennini T, Cerami A, Brines ML et al (2002) Erythropoietin exerts an anti-inflammatory effect on the CNS in a model of experimental autoimmune encephalomyelitis. Brain Res 952:128–134
Aimone JB, Wiles J, Gage FH (2006) Potential role for adult neurogenesis in the encoding of time in new memories. Nat Neurosci 9:723–727
Baldessarini RJ (1989) Current status of antidepressants: clinical pharmacology and therapy. J Clin Psychiatry 50:117–126
Behnken A, Schoning S, Gerss J, Konrad C, de Jong-Meyer R, Zwanzger P et al (2010) Persistent non-verbal memory impairment in remitted major depression—caused by encoding deficits? J Affect Disord 122:144–148
Belmaker RH, Agam G (2008) Mechanisms of disease: major depressive disorder. N Engl J Med 358:55–68
Berton O, Nestler EJ (2006) New approaches to antidepressant drug discovery: beyond monoamines. Nat Rev Neurosci 7:137–151
Bierer R, Peceny MC, Hartenberger CH, Ohls RK (2006) Erythropoietin concentrations and neurodevelopmental outcome in preterm infants. Pediatrics 118:e635–e640
Biringer E, Mykletun A, Sundet K, Kroken R, Stordal KI, Lund A (2007) A longitudinal analysis of neurocognitive function in unipolar depression. J Clin Exp Neuropsychol 29:879–891
Boran BO, Colak A, Kutlay M (2005) Erythropoietin enhances neurological recovery after experimental spinal cord injury. Restor Neurol Neurosci 23:341–345
Borcel E, Perez-Alvarez L, Herrero AI, Brionne T, Varea E, Berezin V et al (2008) Chronic stress in adulthood followed by intermittent stress impairs spatial memory and the survival of newborn hippocampal cells in aging animals: prevention by FGL, a peptide mimetic of neural cell adhesion molecule. Behav Pharmacol 19:41–49
Bouhuys AL, Geerts E, Gordijn MC (1999) Depressed patients' perceptions of facial emotions in depressed and remitted states are associated with relapse: a longitudinal study. J Nerv Ment Dis 187:595–602
Bradley BP, Mogg K, Williams R (1995) Implicit and explicit memory for emotion-congruent information in clinical depression and anxiety. Behav Res Ther 33:755–770
Brines M, Cerami A (2005) Emerging biological roles for erythropoietin in the nervous system. Nat Rev Neurosci 6:484–494
Brines ML, Ghezzi P, Keenan S, Agnello D, de Lanerolle NC, Cerami C et al (2000) Erythropoietin crosses the blood-brain barrier to protect against experimental brain injury. Proc Natl Acad Sci U S A 97:10526–10531
Britton JC, Taylor SF, Sudheimer KD, Liberzon I (2006) Facial expressions and complex IAPS pictures: common and differential networks. Neuroimage 31:906–919
Brown MS, Eichorst D, Lala-Black B, Gonzalez R (2009) Higher cumulative doses of erythropoietin and developmental outcomes in preterm infants. Pediatrics 124:e681–e687
Byts N, Siren AL (2009) Erythropoietin: a multimodal neuroprotective agent. Exp Transl Stroke Med 1:4
Campbell S, Macqueen G (2004) The role of the hippocampus in the pathophysiology of major depression. J Psychiatry Neurosci 29:417–426
Cansino S, Maquet P, Dolan RJ, Rugg MD (2002) Brain activity underlying encoding and retrieval of source memory. Cereb Cortex 12:1048–1056
Castilla-Ortega E, Pedraza C, Estivill-Torrus G, Santin LJ (2011) When is adult hippocampal neurogenesis necessary for learning? Evidence from animal research. Rev Neurosci 22:267–283
Chambers RA, Potenza MN, Hoffman RE, Miranker W (2004) Simulated apoptosis/neurogenesis regulates learning and memory capabilities of adaptive neural networks. Neuropsychopharmacology 29:747–758
Ding G, Jiang Q, Li L, Zhang L, Wang Y, Zhang ZG et al (2010) Cerebral tissue repair and atrophy after embolic stroke in rat: a magnetic resonance imaging study of erythropoietin therapy. J Neurosci Res 88:3206–3214
Drevets WC (2003) Neuroimaging abnormalities in the amygdala in mood disorders. Ann N Y Acad Sci 985:420–444
Dulawa SC, Hen R (2005) Recent advances in animal models of chronic antidepressant effects: the novelty-induced hypophagia test. Neurosci Biobehav Rev 29:771–783
Duman RS, Monteggia LM (2006) A neurotrophic model for stress-related mood disorders. Biol Psychiatry 59:1116–1127
Duman RS, Malberg J, Thome J (1999) Neural plasticity to stress and antidepressant treatment. Biol Psychiatry 46:1181–1191
Ehrenreich H, Degner D, Meller J, Brines M, Behe M, Hasselblatt M et al (2004) Erythropoietin: a candidate compound for neuroprotection in schizophrenia. Mol Psychiatry 9:42–54
Ehrenreich H, Fischer B, Norra C, Schellenberger F, Stender N, Stiefel M et al (2007a) Exploring recombinant human erythropoietin in chronic progressive multiple sclerosis. Brain 130:2577–2588
Ehrenreich H, Hinze-Selch D, Stawicki S, Aust C, Knolle-Veentjer S, Wilms S et al (2007b) Improvement of cognitive functions in chronic schizophrenic patients by recombinant human erythropoietin. Mol Psychiatry 12:206–220
El-Kordi A, Radyushkin K, Ehrenreich H (2009) Erythropoietin improves operant conditioning and stability of cognitive performance in mice. BMC Biol 7:37
Erbayraktar S, Grasso G, Sfacteria A, Xie QW, Coleman T, Kreilgaard M et al (2003) Asialoerythropoietin is a nonerythropoietic cytokine with broad neuroprotective activity in vivo. Proc Natl Acad Sci U S A 100:6741–6746
Erickson K, Drevets W, Schulkin J (2003) Glucocorticoid regulation of diverse cognitive functions in normal and pathological emotional states. Neurosci Biobehav Rev 27:233–246
Eriksson TM, Delagrange P, Spedding M, Popoli M, Mathe AA, Ogren SO et al (2011) Emotional memory impairments in a genetic rat model of depression: involvement of 5-HT/MEK/Arc signaling in restoration. Mol Psychiatry
Garcia-Rodriguez JC, Sosa-Teste I (2009) The nasal route as a potential pathway for delivery of erythropoietin in the treatment of acute ischemic stroke in humans. Sci World J 9:970–981
Genc S, Zadeoglulari Z, Oner MG, Genc K, Digicaylioglu M (2011) Intranasal erythropoietin therapy in nervous system disorders. Expert Opin Drug Deliv 8:19–32
Giacobbe P, Mayberg HS, Lozano AM (2009) Treatment resistant depression as a failure of brain homeostatic mechanisms: implications for deep brain stimulation. Exp Neurol 219:44–52
Girgenti MJ, Hunsberger J, Duman CH, Sathyanesan M, Terwilliger R, Newton SS (2009) Erythropoietin induction by electroconvulsive seizure, gene regulation, and antidepressant-like behavioral effects. Biol Psychiatry 66:267–274
Hamilton JP, Gotlib IH (2008) Neural substrates of increased memory sensitivity for negative stimuli in major depression. Biol Psychiatry 63:1155–1162
Hariri AR, Goldberg TE, Mattay VS, Kolachana BS, Callicott JH, Egan MF et al (2003) Brain-derived neurotrophic factor val66met polymorphism affects human memory-related hippocampal activity and predicts memory performance. J Neurosci 23:6690–6694
Harmer CJ (2010) Antidepressant drug action: a neuropsychological perspective. Depress Anxiety 27:231–233
Harmer CJ, Bhagwagar Z, Perrett DI, Vollm BA, Cowen PJ, Goodwin GM (2003) Acute SSRI administration affects the processing of social cues in healthy volunteers. Neuropsychopharmacology 28:148–152
Harmer CJ, Shelley NC, Cowen PJ, Goodwin GM (2004) Increased positive versus negative affective perception and memory in healthy volunteers following selective serotonin and norepinephrine reuptake inhibition. Am J Psychiatry 161:1256–1263
Harmer CJ, Mackay CE, Reid CB, Cowen PJ, Goodwin GM (2006) Antidepressant drug treatment modifies the neural processing of nonconscious threat cues. Biol Psychiatry 59:816–820
Harmer CJ, Cowen PJ, Goodwin GM (2010) Efficacy markers in depression. J Psychopharmacol
Hasselbalch J, Hasselbalch SG, Gade A, Knorr UB, Kessing LV (2010) Cognitive function in the remitted state of unipolar disorder and the association with the course of illness. In.
Herbert J (2008) Neurogenesis and depression: breakthrough or blind alley? J Neuroendocrinol 20:413–414
Jacobson LO, Goldwasser E, Fried W, Plzak LF (1957) Studies on erythropoiesis. VII. The role of the kidney in the production of erythropoietin. In. pp 305–317.
Jelkmann W (1992) Erythropoietin: structure, control of production, and function. Physiol Rev 72:449–489
Jelkmann W, Bohlius J, Hallek M, Sytkowski AJ (2008) The erythropoietin receptor in normal and cancer tissues. Crit Rev Oncol Hematol 67:39–61
Kessing LV (1998) Cognitive impairment in the euthymic phase of affective disorder. Psychol Med 28:1027–1038
Kitraki E, Kremmyda O, Youlatos D, Alexis M, Kittas C (2004) Spatial performance and corticosteroid receptor status in the 21-day restraint stress paradigm. Ann N Y Acad Sci 1018:323–327
Kumral A, Ozer E, Yilmaz O, Akhisaroglu M, Gokmen N, Duman N et al (2003) Neuroprotective effect of erythropoietin on hypoxic-ischemic brain injury in neonatal rats. Biol Neonate 83:224–228
Lang PJ, Bradley MM, Cuthbert BN (1997) International Affective Picture System (IAPS): technical manual and affective ratings. In: NIMH Center for the Study of Emotion and Attention. University of Florida, Gainesville FL
Leconte C, Bihel E, Lepelletier FX, Bouet V, Saulnier R, Petit E et al (2011) Comparison of the effects of erythropoietin and its carbamylated derivative on behaviour and hippocampal neurogenesis in mice. Neuropharmacology 60:354–364
Leist M, Ghezzi P, Grasso G, Bianchi R, Villa P, Fratelli M et al (2004) Derivatives of erythropoietin that are tissue protective but not erythropoietic. Science 305:239–242
Lembke A, Ketter TA (2002) Impaired recognition of facial emotion in mania. Am J Psychiatry 159:302–304
Li W, Maeda Y, Yuan RR, Elkabes S, Cook S, Dowling P (2004) Beneficial effect of erythropoietin on experimental allergic encephalomyelitis. Ann Neurol 56:767–777
Lupien SJ, de LM, de SS, Convit A, Tarshish C, Nair NP et al (1998) Cortisol levels during human aging predict hippocampal atrophy and memory deficits. Nat Neurosci 1:69–73
Manji HK, Moore GJ, Rajkowska G, Chen G (2000) Neuroplasticity and cellular resilience in mood disorders. Mol Psychiatry 5:578–593
Manji HK, Quiroz JA, Sporn J, Payne JL, Denicoff K, A Gray N et al (2003) Enhancing neuronal plasticity and cellular resilience to develop novel, improved therapeutics for difficult-to-treat depression. Biol Psychiatry 53:707–742
Marti HH, Wenger RH, Rivas LA, Straumann U, Digicaylioglu M, Henn V, et al (1996) Erythropoietin gene expression in human, monkey and murine brain. Eur J Neurosci. 8(4):666–676
Martinez-Aran A, Vieta E, Colom F, Torrent C, Sanchez-Moreno J, Reinares M et al (2004) Cognitive impairment in euthymic bipolar patients: implications for clinical and functional outcome. Bipolar Disord 6:224–232
McEwen BS (2005) Glucocorticoids, depression, and mood disorders: structural remodeling in the brain. Metabolism 54:20–23
Meyer JW, Eichhorn KH, Vetter K, Christen S, Schleusner E, Klos A et al (1995) Does recombinant human erythropoietin not only treat anemia but reduce postpartum (emotional) distress as well? J Perinat Med 23:99–109
Miller AH, Maletic V, Raison CL (2009) Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry 65:732–741
Miskowiak K, Inkster B, Selvaraj S, Goodwin G, Harmer C (2007a) Erythropoietin has no effect on hippocampal response during memory retrieval 3 days post-administration. Psychopharmacology (Berl) 195:451–453
Miskowiak K, O’Sullivan U, Harmer CJ (2007b) Erythropoietin enhances hippocampal response during memory retrieval in humans. J Neurosci 27:2788–2792
Miskowiak K, O’Sullivan U, Harmer CJ (2007c) Erythropoietin reduces neural and cognitive processing of fear in human models of antidepressant drug action. Biol Psychiatry 62:1244–1250
Miskowiak K, Inkster B, O’Sullivan U, Selvaraj S, Goodwin GM, Harmer CJ (2008a) Differential effects of erythropoietin on neural and cognitive measures of executive function 3 and 7 days post-administration. Exp Brain Res 184:313–321
Miskowiak K, Inkster B, Selvaraj S, Wise R, Goodwin GM, Harmer CJ (2008b) Erythropoietin improves mood and modulates the cognitive and neural processing of emotion 3 days post administration. Neuropsychopharmacology 33:611–618
Miskowiak KW, Favaron E, Hafizi S, Inkster B, Goodwin GM, Cowen PJ et al (2009) Effects of erythropoietin on emotional processing biases in patients with major depression: an exploratory fMRI study. Psychopharmacology (Berl) 207:133–142
Miskowiak KW, Favaron E, Hafizi S, Inkster B, Goodwin GM, Cowen PJ et al (2010a) Erythropoietin modulates neural and cognitive processing of emotional information in biomarker models of antidepressant drug action in depressed patients. Psychopharmacology (Berl) 210:419–428
Miskowiak KW, Vinberg M, Harmer CJ, Ehrenreich H, Knudsen GM, Macoveanu J et al (2010b) Effects of erythropoietin on depressive symptoms and neurocognitive deficits in depression and bipolar disorder. Trials 11:97
Miu AC, Olteanu AI, Chis I, Heilman RM (2004) Have no fear, erythropoietin is here: erythropoietin protects fear conditioning performances after functional inactivation of the amygdala. Behav Brain Res 155:223–229
Mogensen J, Miskowiak K, Sorensen TA, Lind CT, Olsen NV, Springborg JB et al (2004) Erythropoietin improves place learning in fimbria-fornix-transected rats and modifies the search pattern of normal rats. Pharmacol Biochem Behav 77:381–390
Morishita E, Masuda S, Nagao M, Yasuda Y, Sasaki R (1997) Erythropoietin receptor is expressed in rat hippocampal and cerebral cortical neurons, and erythropoietin prevents in vitro glutamate-induced neuronal death. Neuroscience 76:105–116
Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B (2007) Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 370:851–858
Neubauer AP, Voss W, Wachtendorf M, Jungmann T (2010) Erythropoietin improves neurodevelopmental outcome of extremely preterm infants. Ann Neurol 67:657–666
Paradiso S, Lamberty GJ, Garvey MJ, Robinson RG (1997) Cognitive impairment in the euthymic phase of chronic unipolar depression. J Nerv Ment Dis 185:748–754
Pickett JL, Theberge DC, Brown WS, Schweitzer SU, Nissenson AR (1999) Normalizing hematocrit in dialysis patients improves brain function. Am J Kidney Dis 33:1122–1130
Pourtois G, Schwartz S, Seghier ML, Lazeyras F, Vuilleumier P (2006) Neural systems for orienting attention to the location of threat signals: an event-related fMRI study. Neuroimage 31:920–933
Preiss M, Kucerova H, Lukavsky J, Stepankova H, Sos P, Kawaciukova R (2009) Cognitive deficits in the euthymic phase of unipolar depression. Psychiatry Res 169:235–239
Ransome MI, Turnley AM (2007) Systemically delivered erythropoietin transiently enhances adult hippocampal neurogenesis. J Neurochem 102:1953–1965
Reppermund S, Zihl J, Lucae S, Horstmann S, Kloiber S, Holsboer F et al (2007) Persistent cognitive impairment in depression: the role of psychopathology and altered hypothalamic-pituitary-adrenocortical (HPA) system regulation. Biol Psychiatry 62:400–406
Sakanaka M, Wen TC, Matsuda S, Masuda S, Morishita E, Nagao M et al (1998) In vivo evidence that erythropoietin protects neurons from ischemic damage. Proc Natl Acad Sci U S A 95:4635–4640
Santarelli L, Saxe M, Gross C, Surget A, Battaglia F, Dulawa S et al (2003) Requirement of hippocampal neurogenesis for the behavioral effects of antidepressants. Science 301:805–809
Sargin D, Hassouna I, Sperling S, Siren AL, Ehrenreich H (2009) Uncoupling of neurodegeneration and gliosis in a murine model of juvenile cortical lesion. Glia 57:693–702
Sargin D, Friedrichs H, El-Kordi A, Ehrenreich H (2010) Erythropoietin as neuroprotective and neuroregenerative treatment strategy: comprehensive overview of 12 years of preclinical and clinical research. Best Pract Res Clin Anaesthesiol 24:573–594
Sargin D, El-Kordi A, Agarwal A, Muller M, Wojcik SM, Hassouna I et al (2011) Expression of constitutively active erythropoietin receptor in pyramidal neurons of cortex and hippocampus boosts higher cognitive functions in mice. BMC Biol 9:27
Sattler MB, Merkler D, Maier K, Stadelmann C, Ehrenreich H, Bahr M et al (2004) Neuroprotective effects and intracellular signaling pathways of erythropoietin in a rat model of multiple sclerosis. Cell Death Differ 11(Suppl 2):S181–S192
Sinclair LI, Christmas DM, Hood SD, Potokar JP, Robertson A, Isaac A et al (2009) Antidepressant-induced jitteriness/anxiety syndrome: systematic review. Br J Psychiatry 194:483–490
Siren AL, Radyushkin K, Boretius S, Kammer D, Riechers CC, Natt O et al (2006) Global brain atrophy after unilateral parietal lesion and its prevention by erythropoietin. Brain 129:480–489
Siren AL, Fasshauer T, Bartels C, Ehrenreich H (2009) Therapeutic potential of erythropoietin and its structural or functional variants in the nervous system. Neurotherapeutics 6:108–127
Smith DJ, Muir WJ, Blackwood DH (2006) Neurocognitive impairment in euthymic young adults with bipolar spectrum disorder and recurrent major depressive disorder. Bipolar Disord 8:40–46
Stratton LO, Gibson CA, Kolar KG, Kastin AJ (1976) Neonatal treatment with TRH affects development, learning, and emotionality in the rat. Pharmacol Biochem Behav 5:65–67
Viviani B, Bartesaghi S, Corsini E, Villa P, Ghezzi P, Garau A et al (2005) Erythropoietin protects primary hippocampal neurons increasing the expression of brain-derived neurotrophic factor. J Neurochem 93:412–421
Wang L, Zhang Z, Wang Y, Zhang R, Chopp M (2004) Treatment of stroke with erythropoietin enhances neurogenesis and angiogenesis and improves neurological function in rats. Stroke 35:1732–1737
Weiland-Fiedler P, Erickson K, Waldeck T, Luckenbaugh DA, Pike D, Bonne O et al (2004) Evidence for continuing neuropsychological impairments in depression. J Affect Disord 82:253–258
Wustenberg T, Begemann M, Bartels C, Gefeller O, Stawicki S, Hinze-Selch D et al (2011) Recombinant human erythropoietin delays loss of gray matter in chronic schizophrenia. Mol Psychiatry 16(26–36):1
Yatsiv I, Grigoriadis N, Simeonidou C, Stahel PF, Schmidt OI, Alexandrovitch AG et al (2005) Erythropoietin is neuroprotective, improves functional recovery, and reduces neuronal apoptosis and inflammation in a rodent model of experimental closed head injury. FASEB J 19:1701–1703
Yis U, Kurul SH, Kumral A, Tugyan K, Cilaker S, Yilmaz O et al (2008) Effect of erythropoietin on oxygen-induced brain injury in the newborn rat. Neurosci Lett 448:245–249
Yu YP, Xu QQ, Zhang Q, Zhang WP, Zhang LH, Wei EQ (2005) Intranasal recombinant human erythropoietin protects rats against focal cerebral ischemia. Neurosci Lett 387:5–10
Yun J, Koike H, Ibi D, Toth E, Mizoguchi H, Nitta A et al (2010) Chronic restraint stress impairs neurogenesis and hippocampus-dependent fear memory in mice: possible involvement of a brain-specific transcription factor Npas4. J Neurochem 114:1840–1851
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miskowiak, K.W., Vinberg, M., Harmer, C.J. et al. Erythropoietin: a candidate treatment for mood symptoms and memory dysfunction in depression. Psychopharmacology 219, 687–698 (2012). https://doi.org/10.1007/s00213-011-2511-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-011-2511-1