Abstract
Rationale
The available treatments for alcoholism are only modestly effective, and patients vary widely in their treatment response. Quetiapine, an atypical antipsychotic medication with antagonist activity at D1 and D2, 5-HT1A and 5-HT2A, H1, and α1 and α2 receptors was shown to promote abstinence, reduce drinking days, and reduce heavy drinking days in a 12-week double-blind placebo-controlled trial.
Objective
Although quetiapine represents one of the promising pharmacotherapies for the treatment of alcoholism, its mechanisms of action are poorly understood. The objective of this study is to elucidate the biobehavioral mechanisms of action of quetiapine for alcoholism, by examining its effects on subjective intoxication and craving.
Method
A total of 20 non-treatment-seeking alcohol-dependent individuals were randomized to one of the following conditions in a double-blind, placebo-controlled design: (1) quetiapine (400 mg/day); or (2) matched placebo. Participants were on the target medication dose (or matched placebo) for 4 weeks during which they completed weekly assessments of drinking, sleep, mood, and anxiety. Participants completed two counterbalanced intravenous placebo-alcohol administration sessions as well as cue-reactivity assessments.
Results
Analyses revealed a significant effect of quetiapine in reducing craving during the alcohol administration, the alcohol cue-exposure, and the weekly reports of alcohol craving. Quetiapine was also found to reduce subjective intoxication and alcohol-induced sedation during the alcohol administration paradigm.
Conclusions
This study contributes critical new information about mechanisms of response to quetiapine for alcoholism, which, in turn, can inform larger-scale studies and ultimately, clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Quetiapine is a multiple receptor antagonist at 5-HT1A and 5-HT2A, dopamine D1 and D2, histamine H1, and adrenergic α1 and α2 receptors. In particular, 5-HT2A and D2 antagonism on the mesolimbic dopaminergic pathway into the nucleus accumbens is thought to decrease dopaminergic output in those areas, as 5-HT2A antagonism modulates the activity of dopaminergic neurons differentially in the mesocortical areas (Horacek et al. 2006). Nucleus accumbens dopamine is also thought to play a role in attentional and executive processes, including impulsivity, as it modulates cortico-limbic inputs from the prefrontal cortex (Besson et al. 2010; Pezze et al. 2007). Medications that effectively block dopamine output in the brain’s reward pathway could reduce alcohol consumption by blunting the reinforcing effects of alcohol and dampening alcohol craving. Such medications might also affect inhibitory control processes and reduce impulsive decision making (Van den Eynde et al. 2008).
Initial support for quetiapine as a pharmacotherapy for alcoholism came from a retrospective chart review suggesting that quetiapine-treated patients reported a significantly higher number of abstinent days and fewer hospitalizations, as compared with non-quetiapine-treated patients (Monnelly et al. 2004). An additional chart review of nine patients admitted to a residential rehabilitation program suggested that quetiapine was well tolerated and associated with significant decreases in anxiety, improvements in sleep, and lower craving for alcohol (Sattar et al. 2004). Published single-case (Lindberg et al. 2006) and observational studies (Croissant et al. 2006) suggested that quetiapine was well tolerated and may be effective in treating alcoholism. An open-label study of quetiapine in patients with comorbid schizophrenia-spectrum and substance use disorders suggested that the severity of substance abuse decreased over the course of a 12-week trial of quetiapine, as indicated by reduced number of substance use days and money spent on alcohol/drugs (Potvin et al. 2006). Likewise, an open-label study found that quetiapine reduced alcohol consumption and craving among dually diagnosed patients with alcoholism (Martinotti et al. 2008). Although these studies lack random assignment, which precludes causal inferences, they suggest that quetiapine may be effective for alcoholism.
The first placebo-controlled trial of quetiapine for alcoholism found that quetiapine treatment was associated with significantly higher abstinence rates. Medication effects were found by stratifying the sample into type A and type B alcohol-dependent patients. Consistent with Babor’s alcoholism typology, type A alcoholism is characterized by fewer childhood risk factors, later onset of alcohol problems, less severe dependence, and less psychopathology, whereas type B alcoholism is characterized by more childhood risk factors, early onset of alcohol problems, greater severity of dependence, and greater psychopathology (Babor et al. 1992). Quetiapine was associated with fewer drinking days, fewer days of heavy drinking, and blunted alcohol craving among patients classified as type B alcoholics (Kampman et al. 2007), but not among type A patients. More recently, a placebo-controlled study of quetiapine as adjunct therapy with lithium or divalproex for patients with bipolar I disorder and co-existing alcohol dependence did not find support for its efficacy with regard to alcohol use measures in this comorbid sample (Stedman et al. 2010). Likewise, a study combining naltrexone and quetiapine did not demonstrate a benefit of the combination over naltrexone alone (Guardia et al. 2011). While the efficacy of quetiapine for alcoholism has not been definitively demonstrated in the literature to date, understanding the mechanisms of action of this pharmacotherapy may be useful in identifying responders as no one pharmacotherapy is likely to be effective for all patients with alcohol dependence, a complex and heterogeneous disorder.
Although reports from clinical observation, case studies, and retrospective chart reviews have suggested that quetiapine may reach its clinical effects for alcoholism by reducing alcohol craving (Croissant et al. 2006), improving sleep (Lindberg et al. 2006; Monnelly et al. 2004), and increasing sedation/decreasing anxiety (Sattar et al. 2004), no experimental studies to date have examined the mechanisms of action of this pharmacotherapy. As recently reviewed, knowledge of the mechanisms of action of quetiapine may improve the available treatments for alcoholism by: (1) informing targeted interventions that are guided by the pharmacotherapy’s mechanisms and assessment of the patient’s needs; (2) elucidating the underlying pathophysiology of alcohol dependence itself; and (3) informing efforts to combine pharmacotherapies on the basis of their neurobiological and biobehavioral effects (Ray et al. 2010a).
To that end, the present study represents a pilot, phase II, human laboratory investigation of the effects of quetiapine on alcohol craving and subjective intoxication. Non-treatment-seeking alcohol-dependent individuals (n = 20) were randomized in a double-blind fashion to either quetiapine (target dose = 400 mg/day) or matched placebo for a period of 6 weeks, including 1-week lead-in, 4 weeks on the target dose, and 1 week of dose-reduction. Participants came to the laboratory on a weekly basis to complete assessments of alcohol use, mood, anxiety, sleep, alcohol craving, medication compliance, and side effects. While on the target dose, participants completed a single blind, placebo-controlled intravenous alcohol administration to assess subjective responses to alcohol and a cue-exposure session, to assess cue-induced alcohol craving. Based on previous findings of uncontrolled studies, it was hypothesized that quetiapine would reduce subjective intoxication and urge to drink. In addition, secondary analyses will examine the effects of quetiapine on measures of sleep, anxiety, depression, and alcohol use. Although preliminary in nature, this study seeks to elucidate the biobehavioral mechanisms of action of quetiapine for alcoholism.
Method
Participants
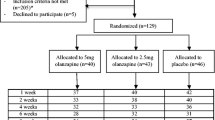
A total of 20 non-treatment-seeking alcohol-dependent individuals were randomized to one of the two medication conditions: quetiapine (400 mg/day) or matched placebo. Inclusion criteria were as follows: (1) age range between 21 and 65 years; and (2) meet the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) diagnostic criteria for alcohol dependence. Exclusion criteria were: (1) current treatment for alcohol problems or a history of treatment 30 days before enrollment or are treatment seeking; (2) a current (last 12 months) DSM-IV diagnosis of dependence on any psychoactive substances other than alcohol and nicotine; (3) a lifetime DSM-IV diagnosis of schizophrenia, bipolar disorder, or any psychotic disorder; (4) current use of a psychoactive drug, other than marijuana, as determined by a positive toxicology screen covering the following substances: cocaine, methamphetamine, amphetamine, marijuana, opiods, methadone, barbiturates, benzodiazepines, and PCP; (5) serious alcohol withdrawal symptoms as indicated by a score > 10 on the Clinical Institute Withdrawal Assessment for Alcohol-Revised (CIWA); (6) clinically significant physical abnormalities as indicated by physical examination, hematological assessment, bilirubin concentration, or urinalysis; (7) history of epilepsy, seizures, or severe head trauma; (8) history of alcohol intoxication delirium, alcohol withdrawal delirium or seizures, alcohol-induced persisting dementia, or alcohol-induced psychosis; (9) treatment with any of the following medications within the last 30 days prior to randomization: antidepressants, anti-convulsants, hypnotics, antipsychotics, psychomotor stimulants, or anti-anxiety agents; (10) history of tardive dyskinesia, movement disorder, tic or Tourette’s disorder, and Parkinson’s disease; (11) current sleep disorder other than primary insomnia, including narcolepsy, restless leg syndrome, and sleep apnea; (12) previous treatment with quetiapine discontinued due to an adverse event; (13) diabetes or a fasting blood glucose level indicating impaired glucose tolerance; and (14) currently taking or expected to take any medications that could interact adversely with quetiapine, such as sedating antihistamines, beta blockers, alpha adrenergic agents, and oral antifungal agents; (15) if female: pregnancy, nursing, or refusal to use reliable barrier method of birth control. Sample characteristics are presented in Table 1.
Screening and experimental design
Initial assessment of the eligibility criteria was conducted through a telephone interview. Eligible participants were invited to the laboratory for an additional screening session. Upon arrival at the laboratory, participants read and signed an informed consent form, completed a series of individual differences measures, as well as the Structured Diagnostic Interview for DSM-IV (SCID-IV; First et al. 1995). The diagnostic interview was used to ensure eligibility based on current alcohol dependence criteria and exclusion for psychiatric disorders (i.e., lifetime DSM-IV diagnosis of schizophrenia, bipolar disorder, other psychotic disorder, or current drug dependence). Participants deemed eligible after the in-person screening visit were invited to complete a physical examination and laboratory exams at the UCLA General Clinical Research Center. The medical visit was designed to assess medical eligibility to receive the study medication and to participate in the ethanol infusion procedure. The study physician (K.M.) conducted the physical exams and reviewed laboratory test results to determine medical eligibility for the study.
Eligible participants were then randomized to receive either quetiapine (400 mg/day) or matched placebo for a total of 6 weeks. A total of 20 participants were randomized to receive medication, with ten participants in each medication group. The first week consisted of a titration period to the target dose, followed by 4 weeks on the target dose, and the last (sixth) week consisted of a titration down period. Participants came to the laboratory weekly to complete assessments of alcohol use, mood, anxiety, sleep, and alcohol craving. Weekly assessments also consisted of medication compliance verification, assessment of side effects, and medication pick up for the next 7 days. During weeks 2 and 4 on the target dose of the medication, or matched placebo, participants completed a randomized, placebo-controlled, single blind, alcohol infusion session. During the active alcohol session, participants received intravenous doses of alcohol (described in detail below) and during the control alcohol session, participants received a matched saline infusion. Each infusion session was immediately followed by a cue-exposure paradigm, by which participants were systematically presented with their preferred alcoholic beverage and urge to drink was assessed. Participants returned to the laboratory 1 month after the completion of the study for a check-up on any residual side effects and received an individual session of Motivational Interviewing (MI), delivered by a licensed clinical psychologist (L.R.) or a PhD student under the supervision of the licensed clinician. Participants were required to have a verified Breath Alcohol Concentration (BrAC) of 0.000 g/dl prior to starting each study visit. The institutional review board for Human Research at the University of California Los Angeles approved all study procedures and documents. All participants provided an initial written informed consent after receiving a full explanation of the study, and written informed consent for the physical exam, alcohol infusion, and medication component of the study were obtained by the study physician (K.M.).
Alcohol administration cue-exposure
In order to effectively control blood alcohol levels, the alcohol administration paradigm used in this study consisted of delivering doses of ethanol intravenously. The ethanol and saline infusion sessions took place at the UCLA General Clinical Research Center and were performed by registered nurses under the direct supervision of the study physician (K.M.). The alcohol infusion was performed using a 5% ethanol IV solution. An infusion nomogram was developed, taking into account participant’s gender and weight. The formulas for determining target infusion rates were 0.166-ml/min × weight, in kilograms, for males, and 0.126-ml/min × weight, for females. Participants started the intravenous administration at their target rate, and BrAC was monitored every 3 to 5 min. Target BrACs were 0.02, 0.04, and 0.06. Upon reaching each of the target levels of intoxication, participants’ infusion rates were reduced to half their target rate, in order to maintain stable BrAC levels during the testing procedures. Assessments were administered immediately upon reaching target BrAC levels, and participants were held at each level for as long as was required to complete the assessments (approximately 5–7 min each). During the control condition, participants received a matched saline infusion and were breathalized every 3 to 5 min, and assessments were administered at 18, 43, and 75 min into the session, in order to mirror the average timing to each target BrAC on the alcohol infusion. Ordering of placebo and alcohol infusions were counterbalanced between subjects, as every participant underwent one alcohol infusion and one placebo infusion. Details on the infusion procedures are provided in previous reports (Ray and Hutchison 2004; Ray et al. 2007).
Each infusion session (alcohol and saline) was followed by a standardized alcohol cue-exposure (CE; Monti et al. 1987, 2001). During CE, participants were systematically exposed to water and alcohol beverages and guided through a process of systematically experiencing each beverage’s smell and sight while imagining what it would be like to consume that beverage. Order of alcohol and water stimuli was not counterbalanced because of carryover effects that are known to occur (Monti et al. 1987). Direct observation of these procedures by the research team was used to ensure compliance.
Medication procedures
Medication was a randomized, double-blinded, between-subjects condition. Participants were randomly assigned to receive either quetiapine (400 mg/day) or matched placebo. Participants followed a dosage schedule in order to minimize any side effects while reaching the target dose, similar to that implemented by Kampman et al. (2007). The dosage schedule consisted of a dose escalation during week 1 (50 mg for days 1–2, 100 mg for day 3, 200 mg for days 4–5, and 300 mg for days 6–7), target dosage for weeks 2–5 (at 400 mg/day), and a dose decrease during week 6 (300 mg for days 36–37, 200 mg for days 38–39, 100 mg for days 40–41, and 0 mg for day 42). Study medication was provided in 7-day supplies during weekly laboratory visits. While maintaining the blind, the study physician was allowed to make dose adjustments for patients who could not tolerate the study medication/placebo. One participant underwent a dose-reduction to 200 mg/day, and after the blind was broken, it was determined that this individual was in the active quetiapine group. Medication was delivered in blister packs, and all pills (active and placebo) were compounded with 50 mg of riboflavin, for the purpose of monitoring medication compliance. Urine samples were collected weekly for analysis under a UV light, a procedure that makes riboflavin content detectable through fluorescence (Del Boca et al. 1996). In addition, participants returned their used blister packs at each weekly visit, and pill count data were collected as an added compliance measure.
Measures
During the in-person screening session, participants completed a battery of individual difference measures that included demographics, alcohol use and problems, family history of alcohol problems, and DSM-IV alcohol abuse and dependence symptoms. During each of the weekly visits, participants reported on alcohol use, mood, anxiety, sleep, side effects, and medication compliance for that week. During the alcohol administration and cue-exposure sessions, measures of subjective responses to alcohol and alcohol craving were administered at baseline and at each target BrAC (i.e., 0.02, 0.04, and 0.06 g/dl) or matched time points (i.e., 18, 43, and 75 min) during the saline infusion. Measures administered during baseline screening, weekly assessments, and the human laboratory procedures are described below:
Alcohol administration and cue-exposure measures
(1) The Subjective High Assessment Scale (SHAS) was used to assess subjective feelings of alcohol intoxication. The SHAS has been adapted by Schuckit and has since been used extensively in alcohol administration studies (Schuckit 1984); (2) The Biphasic Alcohol Effects Scale (BAES) captures feelings of alcohol-induced stimulation and sedation, with each subscale consisting of seven items rated on a Likert scale, ranging from 0 to 10. The BAES is a reliable and valid measure of subjective intoxication (Erblich and Earleywine 1995; Martin et al. 1993); and (3) The Alcohol Urge Questionnaire (AUQ) which is composed of eight items related to urge to drink alcohol. Each item is rated on a seven-point Likert scale anchored by “Strongly Disagree” and “Strongly Agree.” The AUQ has demonstrated high reliability in experimental studies of state levels of urge to drink (Bohn et al. 1995; MacKillop 2006).
Baseline and weekly visit measures
(1) The Systematic Assessment for Treatment Emergent Events (SAFTEE) consists of 24 common drug adverse effects and has been recommended for use in clinical and experimental psychopharmacology studies (SAFTEE; Jacobson et al. 1986; Levine and Schooler 1986); (2) The Timeline Follow Back (TLFB; Sobell and Sobell 1980) is a calendar-assisted interview developed for in-depth retrospective assessment of alcohol use. Primary measures derived from the TLFB were total drinks per week and total drinking days per week; (3) The Pittsburgh Sleep Quality Index (PSQI; Buysse et al. 1989) was used to assess subjective sleep quality and components of disturbed sleep; (4) The Beck Depression Inventory (BDI-II) assessed severity of depressive symptomatology; (5) The Beck Anxiety Inventory (BAI; Beck et al. 1988) measured severity of anxiety symptoms; (6) The Penn Alcohol Craving Scale (PACS; Flannery et al. 1999) and the Obsessive Compulsive Drinking Scale (OCDS; Anton et al. 1995; Anton et al. 1996) were administered to capture weekly levels of alcohol craving.
Statistical analysis
A series of mixed-design repeated-measures analysis of variance (ANOVAs) were conducted to test the study hypotheses. Specifically, ANOVAs using the general linear model (PROC GLM) were used to examine the effects of Medication, which was a two-level between-subjects factor (quetiapine vs. placebo), the effects of Alcohol, which was a two-level within-subjects factor (alcohol vs. saline), the effects of Trial, which was a three-level within-subjects factor (i.e., BrAC = 0.02, 0.04, and 0.06 in the alcohol session and 18, 43, and 75 min in the saline control), and their interactions. Post hoc comparisons of medication group differences at each assessment point were conducted using a series of t tests. The dependent variables were measures of subjective responses to alcohol (i.e., SHAS and BAES) and alcohol craving (AUQ). Analyses of secondary outcomes focused on the weekly assessments during target dosing of the study medication or placebo (weeks 2–5) in the study design. In order to reduce the number of parameters in the model (i.e., increase degrees of freedom) due to the small sample size, baseline assessments were only included when medication groups were found to differ on the dependent measure of interest at baseline, or when baseline levels represented significant model covariates. Lastly, given that this is a proof-of-concept study with small sample size, effect size estimates are provided in order to inform power analyses for future studies. Specifically, partial η 2 are provided for the main analyses below and can be interpreted as R 2 estimates, since they index the proportion of the variance in the dependent variable explained by a given predictor variable.
Results
Baseline comparisons
Of the 20 individuals randomized, 15 completed the study, nine in the placebo group and six in the quetiapine group, suggesting a trend towards differential retention as a function of medication condition, χ 2 (1) = 2.40, p = 0.12. Of the four dropouts in the quetiapine condition, only one participant reported an inability to tolerate quetiapine. A total of 12 out of the 15 completers returned to the laboratory for the 1-month follow-up and MI session. Analysis of drinking data (30-day TLFB) from follow-up completers suggested a trend towards higher drinking at baseline (Mean = 144.48, SD = 87.32) than at 1-month follow-up (Mean = 102.04, SD = 60.52); F (1,11) = 2.95, p = 0.11. As shown in Table 1, the completers in both medication groups were comparable across a range of demographic and alcohol use variables.
Two participants could not complete both alcohol/saline infusion sessions, one in each medication condition, given that the infusion procedures resulted in elevations in blood pressure and heart rate parameters requiring the infusion to be stopped by the study physician. There were no significant differences in weekly drinking as a function of saline/alcohol infusion.
There was no effect of medication on the baseline measures of subjective intoxication or craving, which are the primary dependent measures in this study. Thus, the analyses presented herein will focus on the comparison of the alcohol intoxication at the three levels of alcohol/saline administration (i.e., BrAC = 0.02, 0.04, and 0.06 in the alcohol session and 18, 43, and 75 min in the saline session). Consistent with the highly controlled alcohol administration procedure (Ray et al. 2007), the target BrACs were reliably reached, and observed BrACs were as follows: 0.0204 (SD = 0.0015), 0.0405 (SD = 0.0013), and 0.0601 (SD = 0.0013). There were no group differences in BrAC at any target level, ps > 0.55.
Analyses of the secondary outcomes, obtained during the weekly visits, compared the medication groups across the 4 weeks of assessments on the target medication dose, weeks 2, 3, 4, and 5 in the experimental protocol.
Medication effects on subjective intoxication
Analyses of subjective intoxication, measured by the SHAS, indicated a significant alcohol × medication × trial interaction (F(2,24) = 3.63, p < 0.05, partial η 2 = 0.23) suggesting that placebo-treated individuals reported higher subjective intoxication on the alcohol versus saline conditions whereas quetiapine-treated individuals did not. A similar pattern of results emerged for the sedation subscale of the BAES, such that there was a significant alcohol × medication (F(1,12) = 6.79, p < 0.05, partial η 2 = 0.36). As shown in Fig. 1, placebo-treated individuals reported feelings of sedation during the alcohol administration but not on saline while quetiapine-treated participants did not distinguish alcohol from saline in terms of sedative effects. Analyses of the stimulation subscale of the BAES did not detect significant alcohol × medication interaction (F(1,12) = 0.09, p = 0.77, partial η 2 = 0.01) or alcohol × medication × trial interaction (F(2,24) = 1.30, p = 0.29, partial η 2 = 0.10). Post hoc comparisons revealed no significant group differences at specific assessment time points beyond the effects reported above, ps > 0.10.
Mean scores on the Sedation Subscale of the Biphasic Alcohol Effects Scale (BAES) and standard error of the mean across assessment points in the placebo (i.e., time 1, time 2, and time 3) and alcohol (i.e., target BrAC = 0.02, 0.04, and 0.06) infusion sessions for both placebo (n = 8) and quetiapine (n = 5) medication groups; *p < 0.05
Medication effects on alcohol craving
Analyses of alcohol craving during the alcohol and saline sessions revealed a significant alcohol × medication interaction (F(1,12) = 8.73, p < 0.05, partial η 2 = 0.42) as well as an alcohol × medication × trial interaction (F(2,24) = 4.12, p < 0.05, partial η 2 = 0.26). As seen in Fig. 2, these results suggest that quetiapine-treated individuals reported lower alcohol craving during the alcohol administration session as compared with the saline infusion session and compared with placebo-treated participants. Post hoc comparisons revealed a significant group difference at BrAC = 0.04 g/dl such that quetiapine-treated individuals reported lower alcohol craving, t(13) = 2.18, p < 0.05.
Mean scores on the Alcohol Urge Questionnaire (AUQ) and standard error of the mean across assessment points in the placebo (i.e., time 1, time 2, and time 3) and alcohol (i.e., target BrAC = 0.02, 0.04, and 0.06) infusion sessions for both placebo (n = 8) and quetiapine (n = 5) medication groups; *p < 0.05
Further analyses examined the effects of medication on cue-induced alcohol craving. Results revealed a significant alcohol × medication interaction (F(1,12) = 5.03, p < 0.05, partial η 2 = 0.30) such that quetiapine reduced cue-induced alcohol craving following the alcohol administration session, but not saline control, and as compared with placebo (see Fig. 3). Post hoc comparisons revealed no significant group differences at specific assessment time points beyond the effects reported above, ps > 0.10.
Analyses of weekly reports of alcohol craving, measured by the OCDS and PACS, were performed to extend the experimental findings. Results revealed a significant effect of medication (F(1,13) = 13.29, p < 0.01, partial η 2 = 0.51) on craving measured by the PACS, such that quetiapine-treated individuals reported lower alcohol craving than placebo-treated participants (see Fig. 4). Post hoc comparisons indicated significant group differences during assessment weeks 2, 4, and 5 with t values of 2.68 (p < 0.05), 3.32 (p < 0.01), and 3.57 (p < 0.01), respectively. In addition, there was a significant medication × trial interaction (F(3,39) = 3.11, p < 0.05, partial η 2 = 0.19) with regard to OCDS scores, suggesting that quetiapine reduced alcohol craving across trial, as compared with placebo. A similar pattern of medication × trial interaction was confirmed by analyses of the OCDS subscales (Roberts et al. 1999), such that there was a significant interaction for the obsession subscale (F(3,39) = 3.38, p < 0.05, partial η 2 = 0.24), a marginally significant effect for the resistance/control impairment subscale (F(3,39) = 2.68, p = 0.06, partial η 2 = 0.22), and no significant effect for the interference subscale (F(3,39) = 0.75, p = 0.53, partial η 2 = 0.03). Together, these results provide initial evidence that quetiapine reduces alcohol craving across a range of experimental paradigms, including alcohol administration, cue-exposure, and weekly self-reports.
Medication effects on sleep, anxiety, depression, and alcohol use
Secondary analyses examined the effects of quetiapine, versus placebo, on weekly assessments of sleep, anxiety, depression, and alcohol use. Results revealed no significant main effect of quetiapine on sleep quality, assessed by the PSQI, Global Scale (F(1,13) = 2.06, p = 0.18, partial η 2 = 0.16). Likewise, there was no medication main effect on measures of anxiety (BAI; F(1,13) = 0.55, p = 0.47, partial η 2 = 0.04) or depression (BDI-II; F(1,13) = 0.90, p = 0.36, partial η 2 = 0.07). There was no significant medication effect on measures of alcohol use, captured by weekly assessments while on the target dose (TLFB). Quetiapine did not significantly reduce number of drinks per week (F(1,13) = 1.80, p = 0.21, partial η 2 = 0.14) or drinks per drinking day (F(1,13) = 0.13, p = 0.73, partial η 2 = 0.01, after controlling for baseline drinking levels. For descriptive purposes, drinking data during the trial are provided in Table 2.
Adverse effects and compliance
All urine samples provided by the 15 study completers tested positive for riboflavin, suggesting that individuals were compliant with the medication immediately prior to each appointment. In addition, participants were asked to bring back their pill-minders (i.e., blister packs) at each weekly visit. Analysis of the pill minder data suggested 91.3% compliance for the 15 completers, and there were no significant differences in compliance across medication conditions. Regarding the integrity of the medication blind, out of the nine completers in the placebo condition, two guessed they were on the placebo group, and the remaining seven guessed that they were receiving the active medication. Conversely, in the quetiapine condition, all six completers guessed correctly that they were receiving the active medication. There was no significant difference in correct guesses as a function of medication, χ 2(1) = 1.54, p = 0.22. Regarding the alcohol/saline blind, of the 14 completers on each session, 11 correctly guessed receiving alcohol and ten correctly guessed receiving placebo, χ 2(1) = 0.04, p = 0.84.
A series of Fisher’s exact tests, a non-parametric test appropriate for small cell sizes, were conducted comparing the medication vs. placebo on each of the 24 items from the side effects checklist (SAFTEE). Results revealed that the following side effects were significantly (Fisher’s Exact Test, p < 0.05) more common in the quetiapine group, compared with the placebo-treated group across trial: (1) increased desire for sex; (2) difficulty staying awake; and (3) mental confusion. In addition, there were trend-level medication effects on the following adverse events: (1) nervousness (p = 0.06); (2) blurred vision (p = 0.06); and (3) joint or muscle pain (p = 0.06). At the 1-month follow-up, no significant differences in side effects persisted between placebo and quetiapine groups (Fisher’s exact test, p > 0.20).
Discussion
This study provides initial controlled evidence that quetiapine reduces alcohol craving across a range of experimental paradigms, such as alcohol administration, cue-exposure, and weekly self-reports. Quetiapine was also found to attenuate subjective intoxication and alcohol-induced sedation, as compared with placebo, suggesting that disruptions in subjective intoxication and reductions in alcohol craving may play a role in the biobehavioral mechanisms of action of this pharmacotherapy for alcoholism. These findings extend the clinical literature suggesting that quetiapine may be effective for the treatment of alcohol dependence. These results are consistent with previous reports of quetiapine-induced blunting of alcohol craving, both in open-label studies (Croissant et al. 2006; Martinotti et al. 2008; Sattar et al. 2004) and in a placebo-controlled trial (Kampman et al. 2007). While the results for alcohol craving are clearly supportive of the potential clinical utility of quetiapine for alcoholism treatment, the findings for subjective intoxication and sedation lend themselves to alternative explanations. Specifically, individuals seeking the sedative effects of alcohol may in fact drink more while on quetiapine in order to reach those desired effects. Research with heavy drinkers has found that sedative effects of alcohol may be protective against alcohol use and distinct from the negative reinforcing effects of alcohol (Ray et al. 2009; Wiers 2008); however, there is the potential for the sedative effects of alcohol to serve as negative reinforcers, particularly in alcohol-dependent drinkers (Stritzke et al. 1995). Of note, in the present study, the association between self-reports of sedation and self-reports of alcohol craving during the active alcohol administration was positive and non-significant (r = 0.23 to 0.38), and a similar pattern was found for subjective intoxication (SHAS; r = 0.27 to 0.49). Therefore, it is plausible that reductions in subjective intoxication and sedation in this sample of non-treatment seekers may be indicative of a clinically useful mechanism of action.
Interestingly, the cue-exposure paradigm conducted after the saline/alcohol administration provides a useful framework for dissociating exteroceptive cues (cue-exposure paradigm) from interoceptive ones (intravenous doses of alcohol). Participants in the quetiapine condition maintained lower levels of alcohol craving post-cue, as compared with the saline condition and to placebo-treated individuals. These findings suggest that the quetiapine-induced reduction in craving observed during the alcohol administration is maintained during cue-exposure at BrAC = 0.06 g/dl. Consistent with these methods, the paradigm is more relevant to relapse models of craving than those of drinking initiation and suggest a benefit of quetiapine over placebo in dampening cue-induced craving once alcohol is onboard. In short, these results extend previous findings by employing well-validated experimental psychopharmacology paradigms, such as alcohol administration and alcohol cue-exposure. In brief, investigation demonstrates the utility of human laboratory paradigms for pharmacotherapy development in alcoholism (Ray et al. 2010b).
These results stand in contrast to recent studies suggesting no benefit of quetiapine as an adjunct therapy for patients with bipolar I disorder and alcohol dependence (Stedman et al. 2010) or when used in combination with naltrexone (Guardia et al. 2011). A number of methodological issues preclude direct comparisons across such studies. For example, the Stedman et al. (2010) study examined the effects of quetiapine as an adjunct pharmacotherapy and among dually diagnosed individuals. The Guardia et al. (2011) study, in turn, had much lower target doses of quetiapine (25 to 200 mg/day) and tested the combination of quetiapine and naltrexone to naltrexone alone. Together, these recent studies of quetiapine for alcoholism highlight several key issues in understanding the clinical utility of this pharmacotherapy. The first issue is whether quetiapine is effective in treating dually diagnosed individuals versus patients with a primary alcohol use disorder. Second, it is unclear whether quetiapine may be most effective as a monotherapy or in combination with other pharmacotherapies. Third, dose-response studies have not been conducted to date, and the optimal dosage of quetiapine, either as a monotherapy or as an adjunct therapy, remains unknown.
The present study provides relevant data on some of these important issues by examining the biobehavioral mechanisms of quetiapine, used as a monotherapy, in a sample of alcohol-dependent individuals. From an experimental psychopharmacology viewpoint, it appears that initial characterization of the effects of quetiapine as a monotherapy and among individuals with a primary alcoholism diagnosis represents an ideal first step towards ascertaining its efficacy, mechanisms, and dose-response. Although studies of dually diagnosed samples are rather appealing, given the current FDA indications of quetiapine, these efforts may obscure the direct effects of this medication on alcohol use outcomes.
In the present study, individuals who met criteria for bipolar disorder, schizophrenia, or any psychotic disorder were excluded. Although anxiety and other mood disorders were not exclusionary, participants in this sample did not report clinical levels of depression or anxiety, which precludes a proper examination of medication effects on these parameters. Sleep disturbance was lower on quetiapine versus placebo, although these effects did not reach statistical significance. Likewise, there was no medication effect on alcohol use per se, though a trend towards reduction in alcohol intake was observed. Many factors may explain these findings. Specifically, the small sample size and the non-treatment-seeking nature of the sample may account for the null effects on drinking outcomes since participants were not actively trying to reduce their drinking while in the study. It is also possible that these medication effects may be overcome, or may increase, at higher blood alcohol levels. Additionally, there was a strong placebo effect in this study with the majority of placebo-treated individuals incorrectly guessing their medication status and reporting clinical benefits. Larger studies examining these secondary mechanisms in treatment-seeking samples and over longer periods of time are warranted in order to more fully evaluate medication effects on sleep, mood, anxiety, and alcohol use.
An important issue is that of differential attrition as evidenced by the fact that four of the five dropouts were in the active medication condition. While only one participant reported dropout due to side effects, this remains an important issue in clinical practice with atypical antipsychotics. The statistically significant adverse events observed included increased desire for sex, difficulty staying awake, and mental confusion. In addition, there were trend-level medication effects on nervousness, blurred vision, and joint or muscle pain. Overall, these adverse events are consistent with quetiapine’s pharmacology, perhaps with the exception of increased desire for sex. While studies have found antipsychotics, including quetiapine, to typically decrease libido (Atmaca et al. 2005; Novick et al. 2009), case reports of increased libido have also been found in the clinical literature (Menon et al. 2006). In short, while quetiapine was generally well tolerated in this study (only one dose-reduction requested), identifying an optimal dose that can maximize both tolerability and efficacy remains a priority.
These findings must be interpreted in light of the study’s strengths and limitations. Strengths include the double-blind randomized medication design in combination with experimental psychopharmacology paradigms (i.e., alcohol administration and cue-exposure). The sample was comprised of alcohol-dependent individuals who were maintained on the target dose of the medication for an adequate period of time in order to ensure stable dosing at the time of experimental assessments. High levels of medication compliance and overall adequate retention (15 out of 20 completers) of non-treatment seekers also constitute strengths of this investigation. Limitations include the small sample size and the use of a single dose of quetiapine. In addition, the differential retention for quetiapine and placebo conditions limits the study results. Although the study did not exclude participants based on comorbid psychopathology (other than bipolar disorder and psychosis), the sample did not report high levels of mood or anxiety symptomatology, which may limit the findings to individuals without significant psychiatric comorbidity. Although riboflavin is a useful tracer of medication compliance (Del Boca et al. 1996), the use of frequent dosages may reduce its reliability (Babiker et al. 1989) such that additional compliance measures are warranted in future studies. Limitations notwithstanding, this study provides a proof-of-concept regarding the effects of quetiapine on subjective intoxication and alcohol craving. Specifically, it suggests that to the extent to which efficacious medications for alcoholism may reach their effects by altering subjective intoxication and reducing alcohol craving, then quetiapine represents a useful pharmacotherapy for alcoholism. This study demonstrates the utility of these human laboratory paradigms in pharmacotherapy development for alcoholism (Ray et al. 2010b).
In conclusion, this study was primarily designed to examine the biobehavioral effects of quetiapine on subjective intoxication and alcohol craving. To that end, saline-controlled alcohol administration and alcohol cue-exposure paradigms were conducted in double-blind, randomized, and cross-over fashion. These methods afforded greater statistical power to detect medication effects through the use of controlled laboratory procedures and within-subjects methodology. Results revealed quetiapine-induced disruption in subjective intoxication and reductions in alcohol craving during alcohol administration, cue-exposure, and weekly self-reports. Together, these findings suggest that future studies employing similar experimental psychopharmacology designs with larger sample sizes and varying medication doses may be useful in elucidating the biobehavioral mechanisms of action of quetiapine for alcoholism. These mechanistic insights, in turn, may inform clinical practice regarding the optimal use of quetiapine for alcoholism. Future studies examining moderators of clinical response to quetiapine, including pharmacogenetics, also seem warranted.
References
Anton RF, Moak DH, Latham P (1995) The obsessive compulsive drinking scale: a self-rated instrument for the quantification of thoughts about alcohol and drinking behavior. Alcohol Clin Exp Res 19:92–99
Anton RF, Moak DH, Latham PK (1996) The obsessive compulsive drinking scale: a new method of assessing outcome in alcoholism treatment studies. Arch Gen Psychiatry 53:225–231
Atmaca M, Kuloglu M, Tezcan E (2005) A new atypical antipsychotic: quetiapine-induced sexual dysfunctions. Int J Impot Res 17:201–203
Babiker IE, Cooke PR, Gillett MG (1989) How useful is riboflavin as a tracer of medication compliance? J Behav Med 12:25–38
Babor TF, Hofmann M, DelBoca FK, Hesselbrock V, Meyer RE, Dolinsky ZS, Rounsaville B (1992) Types of alcoholics. I. Evidence for an empirically derived typology based on indicators of vulnerability and severity. Arch Gen Psychiatry 49:599–608
Beck AT, Epstein N, Brown G, Steer RA (1988) An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 56:893–897
Besson M, Belin D, McNamara R, Theobald DE, Castel A, Beckett VL, Crittenden BM, Newman AH, Everitt BJ, Robbins TW, Dalley JW (2010) Dissociable control of impulsivity in rats by dopamine d2/3 receptors in the core and shell subregions of the nucleus accumbens. Neuropsychopharmacology 35:560–569
Bohn MJ, Krahn DD, Staehler BA (1995) Development and initial validation of a measure of drinking urges in abstinent alcoholics. Alcohol Clin Exp Res 19:600–606
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213
Croissant B, Klein O, Gehrlein L, Kniest A, Hermann D, Diehl A, Mann K (2006) Quetiapine in relapse prevention in alcoholics suffering from craving and affective symptoms: a case series. Eur Psychiatry 21:570–573
Del Boca FK, Kranzler HR, Brown J, Korner PF (1996) Assessment of medication compliance in alcoholics through UV light detection of a riboflavin tracer. Alcohol Clin Exp Res 20:1412–1417
Erblich J, Earleywine M (1995) Distraction does not impair memory during intoxication: support for the attention-allocation model. J Stud Alcohol 56:444–448
First MB, Spitzer RL, Gibbon M, Williams JBW (1995) Structured Clinical Interview for DSM-IV Axis I Disorders - Patient edition (SCID-I/P, version 2.0). . Biometrics Research Department, New York State Psychiatric Institute., Biometrics Research Department, New York State Psychiatric Institute
Flannery BA, Volpicelli JR, Pettinati HM (1999) Psychometric properties of the Penn Alcohol Craving Scale. Alcohol Clin Exp Res 23:1289–1295
Guardia J, Roncero C, Galan J et al. (2011) A double-blind, placebo-controlled, randomized pilot study comparing quetiapine with placebo, associated to naltrexone, in the treatment of alcohol-dependent patients. Addict Behav
Horacek J, Bubenikova-Valesova V, Kopecek M, Palenicek T, Dockery C, Mohr P, Hoschl C (2006) Mechanism of action of atypical antipsychotic drugs and the neurobiology of schizophrenia. CNS Drugs 20:389–409
Jacobson AF, Goldstein BJ, Dominguez RA, Steinbook RM (1986) Interrater agreement and intraclass reliability measures of SAFTEE in psychopharmacologic clinical trials. Psychopharmacol Bull 22:382–388
Kampman KM, Pettinati HM, Lynch KG, Whittingham T, Macfadden W, Dackis C, Tirado C, Oslin DW, Sparkman T, O'Brien CP (2007) A double-blind, placebo-controlled pilot trial of quetiapine for the treatment of Type A and Type B alcoholism. J Clin Psychopharmacol 27:344–351
Levine J, Schooler NR (1986) SAFTEE: a technique for the systematic assessment of side effects in clinical trials. Psychopharmacol Bull 22:343–381
Lindberg N, Tani P, Takala P, Sailas E, Putkonen H, Eronen M, Virkkunen M (2006) Increased deep sleep in a medication-free, detoxified female offender with schizophrenia, alcoholism and a history of attempted homicide: effect of concomitant administration of quetiapine and citalopram. Crim Behav Ment Health 16:60–66
MacKillop J (2006) Factor structure of the alcohol urge questionnaire under neutral conditions and during a cue-elicited urge state. Alcohol Clin Exp Res 30:1315–1321
Martin CS, Earleywine M, Musty RE, Perrine MW, Swift RM (1993) Development and validation of the Biphasic Alcohol Effects Scale. Alcohol Clin Exp Res 17:140–146
Martinotti G, Andreoli S, Di Nicola M, Di Giannantonio M, Sarchiapone M, Janiri L (2008) Quetiapine decreases alcohol consumption, craving, and psychiatric symptoms in dually diagnosed alcoholics. Hum Psychopharmacol 23:417–424
Menon A, Williams RH, Watson S (2006) Increased libido associated with quetiapine. J Psychopharmacol 20:125–127
Monnelly EP, Ciraulo DA, Knapp C, LoCastro J, Sepulveda I (2004) Quetiapine for treatment of alcohol dependence. J Clin Psychopharmacol 24:532–535
Monti PM, Binkoff JA, Abrams DB, Zwick WR, Nirenberg TD, Liepman MR (1987) Reactivity of alcoholics and nonalcoholics to drinking cues. J Abnorm Psychol 96:122–126
Monti PM, Rohsenow DJ, Swift RM, Gulliver SB, Colby SM, Mueller TI, Brown RA, Gordon A, Abrams DB, Niaura RS, Asher MK (2001) Naltrexone and cue exposure with coping and communication skills training for alcoholics: treatment process and 1-year outcomes. Alcohol Clin Exp Res 25:1634–1647
Novick D, Haro JM, Perrin E, Suarez D, Texeira JM (2009) Tolerability of outpatient antipsychotic treatment: 36-month results from the European Schizophrenia Outpatient Health Outcomes (SOHO) study. Eur Neuropsychopharmacol 19:542–550
Pezze MA, Dalley JW, Robbins TW (2007) Differential roles of dopamine D1 and D2 receptors in the nucleus accumbens in attentional performance on the five-choice serial reaction time task. Neuropsychopharmacology 32:273–283
Potvin S, Stip E, Lipp O, Elie R, Mancini-Marie A, Demers MF, Roy MA, Bouchard RH, Gendron A (2006) Quetiapine in patients with comorbid schizophrenia-spectrum and substance use disorders: an open-label trial. Curr Med Res Opin 22:1277–1285
Ray LA, Hutchison KE (2004) A polymorphism of the mu-opioid receptor gene (OPRM1) and sensitivity to the effects of alcohol in humans. Alcohol Clin Exp Res 28:1789–1795
Ray LA, Meskew-Stacer S, Hutchison KE (2007) The relationship between prospective self-rating of alcohol sensitivity and craving and experimental results from two alcohol challenge studies. J Stud Alcohol Drugs 68:379–384
Ray LA, MacKillop J, Leventhal A, Hutchison KE (2009) Catching the alcohol buzz: an examination of the latent factor structure of subjective intoxication. Alcohol Clin Exp Res 33:2154–2161
Ray LA, Heydari A, Zorick T (2010a) Quetiapine for the treatment of alcoholism: scientific rationale and review of the literature. Drug Alcohol Rev 29:568–575
Ray LA, Hutchison KE, Tartter M (2010b) Application of human laboratory models to pharmacotherapy development for alcohol dependence. Curr Pharm Des 16:2149–2158
Roberts JS, Anton RF, Latham PK, Moak DH (1999) Factor structure and predictive validity of the Obsessive Compulsive Drinking Scale. Alcohol Clin Exp Res 23:1484–1491
Sattar SP, Bhatia SC, Petty F (2004) Potential benefits of quetiapine in the treatment of substance dependence disorders. J Psychiatry Neurosci 29:452–457
Schuckit MA (1984) Subjective responses to alcohol in sons of alcoholics and control subjects. Arch Gen Psychiatry 41:879–884
Sobell LC, Sobell MB (1980) Convergent validity: an approach to increasing confidence in treatment outcome conclusions with alcohol and drug abusers. In: Sobell LC, Sobell MB, Ward E (eds) Evaluating Alcohol and Drug Abuse Treatment Effectiveness: Recent Advances. Pergamon Press, Elmsford, pp 177–183
Stedman M, Pettinati HM, Brown ES, Kotz M, Calabrese JR, Raines S (2010) A double-blind, placebo-controlled study with quetiapine as adjunct therapy with lithium or divalproex in bipolar I patients with coexisting alcohol dependence. Alcohol Clin Exp Res 34:1822–1831
Stritzke WG, Patrick CJ, Lang AR (1995) Alcohol and human emotion: a multidimensional analysis incorporating startle-probe methodology. J Abnorm Psychol 104:114–122
Van den Eynde F, Senturk V, Naudts K, Vogels C, Bernagie K, Thas O, van Heeringen C, Audenaert K (2008) Efficacy of quetiapine for impulsivity and affective symptoms in borderline personality disorder. J Clin Psychopharmacol 28:147–155
Wiers RW (2008) Alcohol and drug expectancies as anticipated changes in affect: negative reinforcement is not sedation. Subst Use Misuse 43:429–444
Acknowledgments
This study was supported by seed funds from the Department of Psychology at the University of California Los Angeles (UCLA) and by NIH/NCRR grant number M01-RR00865. The authors wish to thank Ryan Arellano, Ellen Chang, Belinda De La Torre, Ana Heydari, and Spencer Bujarski for their contribution to data collection and data management for this project.
Conflict of interest
None of the authors have any conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ray, L.A., Chin, P.F., Heydari, A. et al. A human laboratory study of the effects of quetiapine on subjective intoxication and alcohol craving. Psychopharmacology 217, 341–351 (2011). https://doi.org/10.1007/s00213-011-2287-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-011-2287-3