Abstract
Rationale
Nesfatin-1, derived from the protein NEFA/nucleobindin2 (NUCB2), is a newly identified peptide that acts as a potent satiety agent. It has been reported that peptides involved in the regulation of ingestive behavior are also involved in the regulation of the stress response. However, the relation between nesfatin-1 and stressor-related behaviors like anxiety and/or fear has not yet been investigated.
Objective
The effects of intracerebroventricular (ICV) injection of nesfatin-1 (0, 5, and 25 pmol/3 μl) were assessed in several paradigms that are thought to reflect anxiety and/or fear in rats.
Results
Consistent with an anxiogenic effect, nesfatin-1 dose-dependently decreased the percentage of time spent on the open arms of the elevated plus maze, increased latency to approach, and decreased consumption of a palatable snack in an anxiogenic (unfamiliar) environment. Moreover, ICV nesfatin-1 increased the fear-potentiated startle response and the time spent freezing to both context and conditioned cues in a conditioned emotional response test.
Conclusions
These findings suggest that in addition to its role as a satiety peptide, nesfatin-1 may also be involved in the mediation of anxiety- and/or fear-related responses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nesfatin-1 is a newly identified 82 amino acid peptide derived from the larger precursor protein, NEFA/nucleobindin2 (NUCB2) (Oh et al. 2006). This peptide, which is highly conserved from mice to man, is abundantly expressed in several hypothalamic regions, including the paraventricular nucleus (PVN), supraoptic nucleus, arcuate nucleus, lateral nucleus, and the zona incerta (Oh et al. 2006; Brailoiu et al. 2007). Beyond the hypothalamus, nesfatin-1 has also been identified in several other brain regions, including the Edinger–Westphal nucleus, central nucleus of the amygdala (CeA), nucleus of the solitary tract, caudal raphé nucleus, locus coeruleus, periaqueductal gray matter, and the dorsal motor nucleus of the vagus (Brailoiu et al. 2007; Fort et al. 2007). Nesfatin-1 has been proposed as a novel satiety agent, stemming, in part, from its widespread distribution in hypothalamic regions involved in appetite and metabolic regulation (Oh et al. 2006; Brailoiu et al. 2007). Moreover, central administration of nesfatin-1 dose-dependently suppressed food intake, whereas intracerebroventricular (ICV) administration of antibodies directed against the peptide increased food intake (Oh et al. 2006).
It addition to its role in the regulation of feeding behavior, it is likely that this peptidergic system has functional consequences involving other physiological processes. In this regard, it has been suggested that, as behaviors associated with feeding are incompatible with defensive behaviors, those systems associated with reductions in consummatory behavior should be linked directly or indirectly to those subserving stressor reactivity (Akana et al. 1994; Dallman et al. 1995; Merali et al. 1998; Pecoraro et al. 2004). In support of this contention, it is not only well-documented that stressor exposure alters food intake (Levine and Morley 1981; Morley et al. 1983; Marti et al. 1994; Valles et al. 2000; Tamashiro et al. 2007), but that appetitive stimuli influence the stress response including the secretion of glucocorticoids (Follenius et al. 1982; Al-Damluji et al. 1987; Karbonits et al. 1996; Piazza and Le Moal 1997; Merali et al. 1998). Moreover, several investigators have reported that the state of hunger (fasting vs. satiated) as well as the type of meal consumed (high vs. low fat content) influences the responsiveness of the hypothalamic–pituitary–adrenal axis to stressor exposure (Shiraishi et al. 1984; Schwartz et al. 1995; Dallman et al. 1995; Leal and Moreira 1997; Tannenbaum et al. 1997). It is also noteworthy that many of the peptides involved in the central regulation of food intake also mediate or moderate the stress response. These peptides include (but are not limited to) corticotropin-releasing hormone (CRH), gastrin-releasing peptide, leptin, ghrelin, orexin, neuropeptide Y, and cholecystokinin (Crawley and Corwin 1994; Dallman et al. 1995; Hanson and Dallman 1995; Merali et al. 1998; Koob and Heinrichs 1999; Ahima and Flier 2000; Ueta et al. 2003; Spinazzi et al. 2006; Anisman et al. 2008).
In light of these observations, the primary objective of the present investigation was to assess the effects of central nesfatin-1 administration on stressor-related behaviors reflecting anxiety and/or fear. To this end, animals were centrally injected with one of two doses of nesfatin-1 (5 or 25 pmol; similar to the doses employed by Oh et al. 2006) and were assessed in several behavioral paradigms including those that measure innate (unlearned) anxiety responses (elevated plus maze [EPM] and novelty-induced suppression of food intake), and conditioned (learned) fear responses (fear-potentiated startle [FPS] and conditioned emotional response [CER]).
Materials and methods
Subjects
Male Sprague–Dawley rats from Charles River Laboratories (Saint-Constant, Quebec), weighing 275–300 g upon arrival, were doubly housed in standard plastic cages (45 × 25 × 20 cm) until surgery. In the housing/testing room, lighting was maintained on a 12-h light/dark cycle (lights on at 0700 hours) and the temperature (22°C) and humidity (63%) were kept constant. Throughout the study, including an initial 1-week period of acclimatization to the laboratory, animals had free access to food and water. All experiments were conducted in accordance with the Guide for the Care and Use of Laboratory Animals as well as with the guidelines established by the Canadian Council on Animal Care. All experiments were approved by the Animal Care Committee of the University of Ottawa.
Surgery
Animals were anesthetized with halothane (2.5%) and stereotaxically implanted with a 22-gauge stainless steel guide cannula (Plastics One, Roanoke, VA, USA) aimed at the third ventricle. For pain control, the rats received oral Tylenol (100–200 mg/kg) for 3 days prior to and 3 days following surgery. In addition, they received rectal Tylenol (50 mg/kg) on the day of surgery and for 3 days post surgery. The placement coordinates (obtained from Paxinos and Watson 1986) were 4.4 mm posterior to bregma, 0 mm lateral, and 4.4 mm below the skull surface. The cannula was anchored to the skull with three stainless steel screws and dental cement. A stainless steel obturator (Plastics One, Roanoke, VA, USA) was inserted into the guide cannula and was kept patent by daily manipulation, which consisted of gently wrapping the rat in a cloth and rotating the obturator. Following surgery, animals were individually housed and allowed a 7-day recovery period prior to behavioral testing.
Drugs and injections
Nesfatin-1 (Phoenix Pharmaceuticals, Burlingame, CA, USA) was dissolved in Krebs–Ringer buffered saline solution (KRB) consisting of (in nmol): 2.7 K+, 145 Na+, 1.35 Ca2+, 1.0 Mg2+, 150 Cl−, 0.05 ascorbate, pH 7.4 (Moghaddam and Bunney 1989). The control animals received an equivalent volume of KRB alone (vehicle). Nesfatin-1 or vehicle was microinjected into the third ventricle in a 3-μl volume, infused over 60 s, via an injection cannula (0.5 mm longer than the guide cannula) connected to an infusion pump with polyethylene tubing (Harvard Apparatus, Holliston, MA, USA). Following drug infusion, the injector was left in place for an additional 60 s to ensure drug diffusion.
Behavioral testing
Naïve animals were used in all experiments with the exception of the CER paradigm where the same rats were used for both contextual and cued testing with 1 week intervening between contextual and cued tests. All testing was conducted under low illumination (30–40 lx) between 9:00 a.m. and 12:00 p.m. daily.
Elevated plus maze
The EPM, consisting of two open arms (50 × 10 cm) and two perpendicularly situated arms enclosed by 40 cm high walls, is commonly used to assess anxiety-like behavior in laboratory rodents (Pellow et al. 1985; File 1992). The EPM was elevated approximately 50 cm above the floor. A black curtain surrounded the chamber to limit the influence of spatial cues and other extraneous stimuli. A video camera was mounted above the arena to permit remote monitoring and recording.
Rats (n = 8/group) were individually placed in the testing room for 1 h acclimatization and were then injected ICV with either vehicle (KRB solution) or nesfatin-1 (5 or 25 pmol) 15 min prior to testing. Each rat was then placed onto the open central platform of the EPM (facing a closed arm). The rats’ behavior was monitored for 5 min and scored as follows: (1) frequency of entries into the open arms (all four paws on an open arm), (2) percentage of time spent on the open arms (time open/300 × 100), (3) frequency of entries in the closed arms, and (4) risk assessment behavior (unprotected head dips; head protruding over the edge of an open arm and down toward the floor). Between tests, the EPM was cleaned with 70% ethanol. The percent of time in the open arms, frequency of open arm entries, and unprotected head dips are all validated measures of anxiety-like behavior on the EPM (Pellow et al. 1985; File 1992; Griebel et al. 1997; Carobrez and Bertoglio 2005). Increases in these measures are indicative of reduced anxiety, whereas decreases suggest increased anxiety (File 1992). In contrast, the frequency of closed arm entries is an index of general activity (Cruz et al. 1994).
Approach to a palatable snack in a novel environment
When presented with a familiar snack in a novel (anxiogenic) environment, rodents are reluctant to approach and consume the treat. Anxiolytic agents have been shown to attenuate the reluctance to approach the snack and increase the amount of snack consumed, thus validating this model as a test of anxiety (Merali et al. 2003; Merali et al. 2004). Rats were habituated to a novel, highly palatable snack (Christie HoneyMaid© Graham Crumbs) presented in their home cage (15 min snack access) for eight consecutive days. The snack was presented in a 6 cm diameter ceramic dish placed in the center of the cage. During the last 3 days of this habituation period, when the approach and consumption parameters had stabilized (intake varied by less than ± 0.5 g), baseline measures of the latency to initiate consumption as well as the amount consumed were recorded. On the test day, rats received either ICV nesfatin-1 (5 or 25 pmol; n = 8/group) or vehicle (KRB; n = 10) and were then returned to their home cage. Fifteen minutes later, the rats were presented with the same (now familiar) palatable snack. The latency to initiate snack consumption and the amount consumed (over 15 min) were monitored. For the next 2 days, rats were again presented with the snack in their home cages in the absence of drug treatment. This served as a drug washout period and also ensured that a stable baseline was maintained and that no preexisting group differences were present prior to novel cage testing. On the following day, rats received either nesfatin-1 (5 or 25 pmol) or vehicle and were then returned to their home cage. Fifteen minutes following treatment, rats were transferred to a novel cage (freshly cleaned clear Plexiglas test cage without bedding) and presented with the familiar palatable snack. The latency to initiate snack consumption and the amount consumed (over 15 min) were monitored.
Fear-potentiated startle
The startle apparatus (Coulbourn Instruments, Whitehall, PA, USA) consisted of a sound attenuated chamber containing two calibrated platforms (18 × 10 cm) designed to measure the animal’s startle response. Animals were placed in a Teflon cage (18.5 × 11 cm) positioned atop the platforms. The cage floor consisted of stainless steel rods (4 mm diameter spaced 1.8 cm apart) connected to shock generators (Coulbourn Instruments; H13–16). Force changes produced by the rats’ startle response were measured by the startle sensor platform. The resultant voltage output from the platform transducer was digitized by an analog-to-digital converter card, interfaced with the computer, and recorded using data acquisition software (Coulbourn AASS v3.02). Startle amplitude was defined as the maximum peak to peak voltage that occurred during the first 200 ms after onset of the auditory startle stimulus. A high-frequency speaker, mounted (24 cm) above the platforms, generated white noise, while tones (startle stimulus) were generated by a Sonalert model tone generator (75 kHz; Coulbourn Instruments).
The training and testing for FPS spanned 4 days. On day 1, rats (n = 8–11/group) were placed inside the startle chamber and exposed to random bursts of white noise (95, 110, and 115 db) for acclimatization and establishment of individual baseline startle amplitudes. On day 2, animals received a conditioning session where a tone (conditioning stimulus; CS) was paired with a shock (unconditioned stimulus; US). Specifically, a 1.0-mA, 0.5 s foot shock (US) was administered during the last 500 ms of the CS (a 4 s tone; 75 KHz). There were seven CS–US trials with an average of 1 min (randomized) intertrial intervals (ITI). Forty-eight hours later (day 4), rats received either ICV vehicle or nesfatin-1 (5 or 25 pmol) 15 min before testing for fear potentiation. Twenty trials of 110 db white noise bursts (random 1 min ITI) were followed by five trials of tones paired with noise bursts, and finally, five noise-alone trials. Cages were cleaned with 70% ethanol between testing of each animal. Rats that have learned to associate the CS (tone) with the US (foot shock) typically display a greater startle amplitude in the presence of the CS (Davis et al. 1993; Davis 1993). Administration of anxiolytic compounds decrease the FPS response in rodents (Davis 1993).
Conditioned emotional response
The conditioning chamber (Coulbourn Instruments, Whitehall, PA, USA) measured 31 × 25 × 30 cm. The front and back walls were made of clear Plexiglas and the two side walls were made of stainless steel panels. The floor comprised 16 stainless steel rods (2 mm diameter, 3 cm apart), connected to a constant current shock generator (Coulbourn Instruments; model H13–16). A Sonalert tone generator (Coulbourn Instruments; 75 kHz, low setting) was situated in the top rear panel and provided the conditioning auditory cue.
All subjects completed 1 day of training followed by a day of testing 24 h later. Training for contextual fear occurred 1 week after surgery, whereas cued fear training followed 2 weeks from surgery. During the contextual training phase, subjects were placed in the conditioning chamber where they received six foot shocks (1.0 mA; 1 s in duration) on a random schedule with an average ITI of 1 min. Cued fear training consisted of the delivery of six pairings of a 20 s tone with a 1.0-mA (1 s) foot shock in the conditioning chamber. The shock was delivered during the final second of the 20 s tone. Again, each trial was delivered at an average ITI of 1 min.
On the test days, rats (n = 7–9/group) received ICV injections of vehicle or nesfatin-1 (5 or 25 pmol) 15 min before testing. Contextual fear was assessed over an 8 min period by placing rats in the conditioning chamber where they had previously been shocked. Freezing behavior, which was used as an index of conditioned fear, was timed using the software program ODlog (Macropod Software). Freezing was defined as the absence of movement excluding involuntary respiratory movements (Blanchard and Blanchard 1969). Trained experimenters blind to the drug condition conducted evaluations of freezing responses. To assess the CER in the cued condition, rats were transferred to a novel environment of similar dimensions, but visually and textually distinct from the training chamber. Specifically, black laminate covered the walls, and the floor was smooth (instead of a grid bar floor) and covered with bedding chips. Animals were allowed a 1 min exploration period and were then presented with the conditioned cue (the tone that had previously been paired with foot shock). A total of eight tones (each 20 s in duration) were presented at 1 min intervals (20 s tone + 40 s ITI). Freezing was scored as described in the contextual test. Chambers were cleaned with 70% ethanol between each training and testing session.
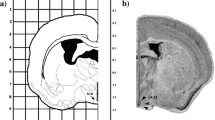
Histology
Following completion of the experimental procedures, rats received an overdose of pentobarbital and 25% India ink (1 μl) was delivered through the injection cannula. Animals were then killed, and their brains were removed and frozen. The location of the cannula was verified histologically following thionin staining of the sections. With the exception of two cannulae, all others were correctly positioned.
Statistics
Data obtained from the EPM was analyzed using one-way analysis of variance (ANOVA) for each of the behavioral measures with treatment condition (vehicle, nesfatin-1 5 or 25 pmol) as the between-group factor. Data from approach to a snack in a novel environment experiment was analyzed using a mixed measures ANOVA with treatment condition (vehicle, nesfatin-1 5 and 25 pmol) as the between-group factor and test condition (home vs. novel cage) as the within-group factor. For the FPS experiment, to obtain an operational measure of fear, data was converted to percent change scores (mean startle amplitude on CS + noise trails − mean startle amplitude on noise-alone trials/mean startle amplitude on noise-alone trials × 100) (see Walker and Davis 2002). The potentiated startle data was then analyzed using a one-way ANOVA with treatment condition as the between-group factor. For the CER data, raw freezing scores were transformed into a percentage of time spent freezing within each 1-min bin. These percentage scores were then averaged across the 8-min contextual and cued tests and analyzed using a one-way ANOVA with treatment condition as the between-group factor. In all experiments, follow-up analyses were conducted using t tests with a Bonferroni correction to protect the α at 0.05.
Results
Analyses of the EPM behaviors indicated that nesfatin-1 affected the percentage of time spent on the open arms (F 2, 21 = 11.87; p < 0.0003), the number of open arm entries (F 2, 21 = 5.07; p < 0.015), and the number of unprotected head dips (F 2, 21 = 5.76; p < 0.01)(see Fig. 1a–c). The follow-up tests revealed that rats that received nesfatin-1 spent significantly less time on the open arms (25 pmol), initiated significantly fewer open arm entries and unprotected head dips (25 pmol) relative to vehicle-treated rats. In contrast, nesfatin-1 administration had no effect on the number of closed arm entries (see Fig. 1d).
Mean±SEM for several behaviors on the EPM among rats treated ICV with either vehicle (open columns), the low dose (5 pmol) of nesfatin-1 (hatched columns), or the high dose (25 pmol) of nesfatin-1 (solid columns). a Percent time (±SEM) animals spent on the open arms of the EPM, b the mean number of unprotected head dips (±SEM), c the mean number of times (±SEM) animals entered onto the open arms of the EPM, and d the mean number of times (±SEM) animals entered onto the closed arms of the EPM. *p < 0.05; significantly different from vehicle condition
Figure 2a and b depict the effects of nesfatin-1 on the latency to approach the snack and the amount of a palatable snack consumed in both the home and novel cages. Mixed-measures ANOVA of the amount of snack consumed revealed a significant test condition (home vs. novel cage) × drug treatment (vehicle, nesfatin-1 5 or 25 pmol) interaction (F 2, 22 = 3.76; p < 0.039). Follow-up tests of the simple effects comprising this interaction indicated that, in the home cage, there were no significant differences in the amount of snack consumed. However, a marked reduction in the amount of snack consumed was evident in the novel cage, which was significantly more pronounced following nesfatin-1 (5 or 25 pmol) administration. Similarly, analysis of the latency to consume the snack revealed a significant test condition (home vs. novel cage) × drug treatment (vehicle, nesfatin-1 5 or 25 pmol) interaction (F 2, 22 = 4.76; p < 0.019). Follow-up tests again revealed that this interaction was attributable to a novelty-induced increase in latency to eat in the vehicle-treated animals tested in the novel cage and an even greater increase of the latency in animals treated with nesfatin-1 (5 and 25 pmol).
Effect of nesfatin-1 on a snack consumption (in grams) and b on the latency to approach the snack (in seconds) in the home cage and novel cage conditions. Each column depicts snack consumption (mean±SEM over 15 min) or approach latency (mean±SEM) in the home cage or the novel cage conditions following ICV injection of vehicle (open columns), low-dose (5 pmol) nesfatin-1 (hatched columns), or high-dose (25 pmol) nesfatin-1 (solid columns). *p < 0.05; significantly different from respective home cage baselines; †p < 0.05; significantly different from condition matched control
As depicted in Fig. 3, nesfatin-1 dose-dependently increased the expression of FPS (F 2, 26 = 4.01; p < 0.03) without affecting the baseline startle amplitude (noise-alone trails; F 2, 26 = 1.19; p < 0.32) (data not shown). The follow-up comparisons revealed that rats treated with the high dose of nesfatin-1 (25 pmol) displayed significantly greater startle potentiation than did the vehicle control group.
The effects of nesfatin-1 administration on freezing behavior in the contextual and cued CER tests are depicted in Fig. 4a and b. ANOVA revealed that, in both instances, percentage freezing varied as a function of the treatment condition (F 2, 20 = 3.42 and 3.99, ps < 0.05). Follow-up comparisons indicated that, in both the contextual and cued tests, rats treated with the high dose of nesfatin-1 (25 pmol) exhibited more freezing behavior compared to vehicle-treated rats.
Percentage of time engaged in freezing (mean±SEM) in the a contextual task and b in response to the fear cue applied in a different environment, following ICV administration of vehicle (open columns), the low dose (5 pmol) of nesfatin-1 (hatched columns), or the high dose (25 pmol) of nesfatin-1 (solid columns). *p < 0.05; significantly different from vehicle condition
Discussion
In addition to its role in the regulation of feeding, the data of the present investigation suggest that nesfatin-1 is also involved in the mediation of anxiety- and/or fear-type behaviors. The EPM and novelty-induced suppression of food intake both measure behaviors reflecting unconditioned responses, and thus innate anxiety in rodents (Rodgers and Dalvi 1997; Merali et al. 2003). In the EPM, ICV administration of nesfatin-1 produced an anxiogenic effect reflected by significantly less time spent on the open arms of the maze and significantly fewer open arm entries and unprotected head dips (an index of risk assessment behavior). Importantly, the anxiogenic effects of nesfatin-1 on the EPM were not accompanied by nonspecific effects (changes of general locomotor activity) reflected by closed arm entries (File 1992; Cruz et al. 1994).
Central administration of nesfatin-1 also produced an anxiogenic effect in the approach to a snack in a novel environment paradigm. Typically, when a familiar snack is presented to a rat in a familiar environment, it will readily approach and consume the snack. When the same snack is then presented in a novel environment, the latency to consume the snack is markedly increased and the amount of snack consumed is reduced, and these effects are antagonized by benzodiazepine administration (Merali et al. 2003; Merali et al. 2004). In the novel cage, central administration of nesfatin-1 at both doses (5 and 25 pmol) significantly increased the approach latency to the snack and decreased the amount of snack consumed relative to the vehicle-treated rats. In contrast, in the home cage, nesfatin-1 was without effect on either of these behavioral measures. This observation is interesting in light of the finding that central nesfatin-1 injection (4 and 20 pmol) suppresses food intake (Oh et al. 2006). Based on this finding, it might be tempting to speculate that, rather than playing a direct physiological role in appetite suppression, nesfatin-1 decreases food intake indirectly as a consequence of enhanced fear/anxiety. While this remains a possibility, it is important to consider that the effects of peptides on anxiety and satiety need not be mutually exclusive. In fact, as discussed earlier, many so-called satiety peptides also affect anxiety-like states. However, the fact that ICV infusion of either antiserum directed against nesfatin-1 or antisense oligonucleotide (which downregulated the mRNA for NUCB2) increased food intake and body weight gain suggests a physiological role of this peptide in food intake (Oh et al. 2006). This position is further supported by the observation that NUCB2 mRNA expression at regions known to be important in the regulation of food intake (PVN and supraoptic nucleus) is affected by the state of hunger (Oh et al. 2006; Kohno et al. 2008). Possible reasons why a decrease in food intake was not observed in the home cage may be attributable to differences in the paradigms employed. Specifically, rats in the Oh et al. study were fed normal rat chow as opposed to a palatable snack. Consistent with our present findings, we previously reported that central administration of CRH, a peptide that also has anxiogenic and anorectic properties, did not affect palatable snack consumption in the home cage (Merali et al. 2004). In contrast, however, central injection of another satiety peptide, gastrin-releasing peptide, reduced palatable snack consumption in the home cage (Merali et al. 2004). Although the neuronal mechanisms mediating these differences of peptide effects are not known, it appears that, at the doses used, the effect of nesfatin-1 was more aligned with the actions of CRH.
The effects of nesfatin-1 were also assessed in two models that measure learned (classically conditioned) fear responses, namely, the FPS and the CER paradigms (Davis 1990). In both models, central nesfatin-1 administration enhanced the fear response. In the FPS paradigm, rats treated with the high dose of nesfatin-1 (25 pmol) displayed an increased FPS response compared to vehicle-treated rats. This effect was apparent in the absence of any differences in startle reactivity in the noise-alone trials. Similarly, in both the contextual and cued components of the CER test, rats treated with nesfatin-1 (25 pmol) displayed significantly higher levels of freezing compared to vehicle-treated rats.
Taken together, these findings suggest a generalized role for nesfatin-1 in the mediation of anxiety- and fear-related behaviors, as the effects of the compound are evident across a variety of different anxiety- and fear-provoking situations. At present, the neuronal mechanism(s) mediating these effects are unknown. Based on recent findings, however, some speculations are possible. One obvious candidate might be through interactions with CRH. Indeed, the distribution patterns of these peptidergic systems, both abundantly found in hypothalamic regions as well as in extrahypothalamic sites such as the CeA (recognized as a key structure in the mediation of anxiety- and/or fear-related behaviors) (Davis 1992; Schulkin 2006), are in keeping with the contention that CRH and nesfatin-1 act in a collaborative or serial manner (Swanson et al. 1983; Oh et al. 2006; Brailoiu et al. 2007; Fort et al. 2007). In this regard, it has been reported that a subpopulation of nesfatin-1 neurons in the PVN coexpress CRH (Kohno et al. 2008; Price et al. 2008). It will be recalled that CRH is as a key mediator of the stress response, and like nesfatin-1, produces anxiogenic and fear-enhancing effects in several animal models of anxiety and/or fear (Kalin and Takahashi 1990; Heinrichs et al. 1995; Koob and Heinrichs 1999). In addition, CRH has clear anorectic properties, demonstrated by the ability of central CRH administration to suppress food intake (Morley and Levine 1982; Gosnell et al. 1983; Richard et al. 2002).
Other than CRH, another potential candidate through which nesfatin-1 may be mediating its anxiogenic effects is the melanocortin system. Supporting this contention, ICV administration of α-MSH (a melanocortin agonist) enhanced the expression of the gene encoding NUCB2 in the PVN (Oh et al. 2006), whereas administration of the melanocortin receptor antagonist, SHU9119, attenuated nesfatin-1-induced satiety (Oh et al. 2006). The melanocortin system appears to be involved in the mediation of anxiety-related behaviors, as administration of α-MSH reduced time spent on the open arms of the EPM as well as the number of licks in the Vogel test (Rao et al. 2003; Chaki et al. 2003). Moreover, pretreatment with SHU9119 dose-dependently attenuated stressor-induced anxiogenic behaviors (measured on the EPM) (Liu et al. 2007). There is also substantial evidence that the melanocortin system plays a role in feeding-related processes. For example, central administration of melanocortin agonists such as α-MSH or MTII reduce food intake (Rossi et al. 1998; Vergoni and Bertolini 2000). Interestingly, this effect was attenuated by blockade of CRH receptors suggesting a functional link between the CRH and central melanocortin systems (Dhillo et al. 2002; Lu et al. 2003). Taken together, these findings suggest that the relationship between nesfatin-1 and CRH and/or the melanocortin system might be interrelated. Of course, this suggestion is highly speculative, and further analyses will be needed to determine what role, if any, these systems play in the mediation of nesfatin-1-induced anxiogenic effects.
In summary, the present set of experiments demonstrates that central nesfatin-1 administration produces anxiogenic and fear-enhancing effects in several animal models that assess anxiety and/or fear. Like many other peptides that are involved in both the regulation of feeding behavior and stress-related responses, nesfatin-1 also appears to play a dual role in these physiological processes. Although the significance of this finding is not known, we previously suggested that peptidergic responses may be activated to draw attention to external events or cues of biological significance, irrespective of whether they involve food availability or a threat to survival (Merali et al. 1998).
References
Ahima RS, Flier JS (2000) Leptin. Annu Rev Physiol 62:413–437
Akana SF, Strack AM, Hanson ES, Dallman MF (1994) Regulation of activity in the hypothalamic–pituitary–adrenal axis is integral to a larger hypothalamic system that determines caloric flow. Endocrinology 135:1125–1134
Al-Damluji S, Iverson T, Thomas JM, Pendlebury DJ, Rees LH, Besser GM (1987) Food-induced cortisol secretion is mediated by central alpha-1 adrenoceptor modulation of pituitary ACTH secretion. Clin Endocrinol 26:629–636
Anisman H, Merali Z, Hayley S (2008) Neurotransmitter, peptides and cytokine processes in relation to depressive disorder: comorbidity between depression and neurodegenerative disorders. Prog Neurobiol 85:1–74
Blanchard RJ, Blanchard DC (1969) Crouching as an index of fear. J Comp Physiol Psychol 67:370–375
Brailoiu GC, Dun SL, Brailoiu E, Inan S, Yang J, Chang JK, Dun NJ (2007) Nesfatin-1: distribution and interaction with a G protein-coupled receptor in the rat brain. Endocrinology 148:5088–5094
Carobrez AP, Bertoglio LJ (2005) Ethological and temporal analyses of anxiety-like behavior: the elevated plus-maze model 20 years on. Neurosci Biobehav Rev 29:1193–1205
Chaki S, Ogawa S, Toda Y, Funakoshi T, Okuyama S (2003) Involvement of the melanocortin MC4 receptor in stress-related behavior in rodents. Eur J Pharmacol 474:95–101
Crawley JN, Corwin RL (1994) Biological actions of cholecystokinin. Peptides 15:731–755
Cruz APM, Frei F, Graeff FG (1994) Ethopharmacological analysis of rat behavior on the elevated plus-maze. Pharmacol Biochem Behav 49:171–176
Dallman MF, Akana SF, Strack AM, Hanson S, Sebastian RJ (1995) The neural network that regulates energy balance is responsive to glucocorticoids and insulin and also regulates HPA axis responsivity at sites proximal to CRF neurons. Ann NY Acad Sci 771:730–742
Davis M (1990) Animal models of anxiety based on classical conditioning: the conditioned emotional response (CER) and the fear-potentiated startle effect. Pharmacol Ther 47:147–165
Davis M (1992) The role of the amygdala in fear and anxiety. Annu Rev Neurosci 15:353–375
Davis M (1993) Pharmacological analysis of fear-potentiated startle. Braz J Med Biol Res 26:235–260
Davis M, Falls WA, Campeau S, Kim M (1993) Fear-potentiated startle: a neural and pharmacological analysis. Behav Brain Res 58:175–198
Dhillo WS, Small CJ, Seal LJ, Kim MS, Stanley SA, Murphy KG, Ghatei MA, Bloom SR (2002) The hypothalamic melanocortin system stimulates the hypothalamo-pituitary-adrenal axis in vitro and in vivo in male rats. Neuroendocrinology 75:209–216
File SE (1992) Behavioural detection of anxiolytic action. In: Elliot JM, Heal DJ, Marsden CA (eds) Experimental approaches to anxiety and depression. Wiley, Chichester, pp 25–44
Follenius M, Brandenberger G, Hietter B (1982) Diurnal cortisol peaks and their relationships to meals. J Clin Endocrinol Metab 55:757–761
Fort P, Butaud C, Salvert D, Shimizu H, Hashimoto K, Mori M, Luppi PH (2007) The satiety molecule nesfatin-1 is co-localized with MCH in hypothalamic neurons expressing Fos during paradoxical sleep in rats. Société des Neuroscience (8e Colloque Montpellier) Abstract:B.13
Gosnell BA, Morley JE, Levine AS (1983) A comparison of the effects of corticotropin releasing factor and sauvagine on food intake. Pharmacol Biochem Behav 19:771–775
Griebel G, Rodgers RJ, Perrault G, Sanger DJ (1997) Risk assessment behaviour: evaluation of utility in the study of 5-HT-related drugs in the rat elevated plus-maze test. Pharmacol Biochem Behav 57:817–827
Hanson ES, Dallman MF (1995) Neuropeptide Y (NPY) may integrate responses of hypothalamic feeding systems and the hypothalamic–pituitary–adrenal axis. J Neuroendocrinol 7:273–279
Heinrichs SC, Menzaghi F, Pich EM, Britton KT, Koob GF (1995) The role of CRF in behavioral aspects of stress. Ann NY Acad Sci 771:92–104
Kalin NH, Takahashi LK (1990) Fear-motivated behavior induced by prior shock experience is mediated by corticotropin-releasing hormone systems. Brain Res 509:80–84
Karbonits M, Trainer PJ, Nelson ML, Howse I, Kopelman PG, Besser GM, Grossman AB, Svec F (1996) Differential stimulation of cortisol and dehydroepiandrosterone levels by food in obese and normal subjects: relation to body fat distribution. Clin Endocrinol 45:699–706
Kohno D, Nakata M, Maejima Y, Shimizu H, Sedbazar U, Yoshida N, Dezaki K, Onaka T, Mori M, Yada T (2008) Nesfatin-1 neurons in paraventricular and supraoptic nuclei of the rat hypothalamus coexpress oxytocin and vasopressin and are activated by refeeding. Endocrinology 149:1295–1301
Koob GF, Heinrichs SC (1999) A role for corticotropin releasing factor and urocortin in behavioral responses to stressors. Brain Res 848:141–152
Leal AM, Moreira AC (1997) Food and the circadian activity of the hypothalamic–pituitary–adrenal axis. Braz J Med Biol Res 30:1391–1405
Levine AS, Morley JE (1981) Stress-induced eating in rats. Am J Physiol 241:R72–R76
Liu J, Garza JC, Truong HV, Henschel J, Zhang W, Lu XY (2007) The melanocortinergic pathway is rapidly recruited by emotional stress and contributes to stress-induced anorexia and anxiety-like behavior. Endocrinology 148:5531–5540
Lu XY, Barsh GS, Akil H, Watson SJ (2003) Interaction between alpha-melanocyte-stimulating hormone and corticotropin-releasing hormone in the regulation of feeding and hypothalamo-pituitary-adrenal responses. J Neurosci 23:7863–7872
Marti O, Marti J, Armario A (1994) Effects of chronic stress on food intake in rats: influence of stressor intensity and duration of daily exposure. Physiol Behav 55:747–753
Merali Z, McIntosh J, Kent P, Michaud D, Anisman H (1998) Aversive and appetitive events evoke the release of corticotropin-releasing hormone and bombesin-like peptides at the central nucleus of the amygdala. J Neurosci 18:4758–4766
Merali Z, Levac C, Anisman H (2003) Validation of a simple, ethologically relevant paradigm for assessing anxiety in mice. Biol Psychiatry 54:552–565
Merali Z, Khan S, Michaud DS, Shippy SA, Anisman H (2004) Does amygdaloid corticotropin-releasing hormone (CRH) mediate anxiety-like behaviors? Dissociation of anxiogenic effects and CRH release. Eur J Neurosci 20:229–239
Moghaddam B, Bunney BS (1989) Ionic composition of microdialysis perfusing solution alters the pharmacological responsiveness and basal outflow of striatal dopamine. J Neurochem 53:652–654
Morley JE, Levine AS (1982) Corticotropin-releasing factor, grooming and ingestive behavior. Life Sci 31:1459–1464
Morley JE, Levine AS, Rowland NE (1983) Minireview. Stress induced eating. Life Sci 32:2169–2182
Oh I, Shimizu H, Satoh T, Okada S, Adachi S, Inoue K, Eguchi H, Yamamoto M, Imaki T, Hashimoto K, Tsuchiya T, Monden T, Horiguchi K, Yamada M, Mori M (2006) Identification of nesfatin-1 as a satiety molecule in the hypothalamus. Nature 443:709–712
Paxinos G, Watson C (1986) The rat brain in stereotaxic coordinates. Academic Press, New York
Pecoraro N, Reyes F, Gomez F, Bhargava A, Dallman MF (2004) Chronic stress promotes palatable feeding, which reduces signs of stress: feedforward and feedback effects of chronic stress. Endocrinology 145:3754–3762
Pellow S, Chopin P, File SE, Briley M (1985) Validation of open:closed arm entries in an elevated plus-maze as a measure of anxiety in the rat. J Neurosci Methods 14:149–167
Piazza PV, Le Moal M (1997) Glucocorticoids as a biological substrate of reward: physiological and pathophysiological implications. Brain Res Rev 25:359–372
Price CJ, Hoyda TD, Samson WK, Ferguson AV (2008) Nesfatin-1 influences the excitability of paraventricular nucleus neurons. J Neuroendocrinol 20:245–250
Rao TL, Kokare DM, Sarkar S, Khisti RT, Chopde CT, Subhedar N (2003) GABAergic agents prevent alpha-melanocyte stimulating hormone induced anxiety and anorexia in rats. Pharmacol Biochem Behav 76:417–423
Richard D, Lin Q, Timofeeva E (2002) The corticotropin-releasing factor family of peptides and CRF receptors: their roles in the regulation of energy balance. Eur J Pharmacol 440:189–197
Rodgers RJ, Dalvi A (1997) Anxiety, defense and the elevated plus-maze. Neurosci Biobehav Rev 21:801–810
Rossi M, Kim MS, Morgan DG, Small CJ, Edwards CM, Sunter D, Abusnana S, Goldstone AP, Russell SH, Stanley SA, Smith DM, Yagaloff K, Ghatei MA, Bloom SR (1998) A C-terminal fragment of Agouti-related protein increases feeding and antagonizes the effect of alpha-melanocyte stimulating hormone in vivo. Endocrinology 139:4428–4431
Schulkin J (2006) Angst and the amygdala. Dialogues in Clinical Neuroscience 8:407–416
Schwartz MW, Dallman MF, Woods SC (1995) Hypothalamic response to starvation: implications for the study of wasting disorders. Am J Physiol 269:R949–R957
Shiraishi I, Honma K, Honma S, Hiroshige T (1984) Ethosecretogram: relation of behavior to plasma corticosterone in freely moving rats. Am J Physiol 247:R40–R45
Spinazzi R, Andreis PG, Rossi GP, Nussdorfer GG (2006) Orexins in the regulation of the hypothalamic–pituitary–adrenal axis. Pharmacol Rev 58:46–57
Swanson LW, Sawchenko PE, Rivier J, Vale WW (1983) Organization of ovine corticotropin-releasing factor (CRF)-immunoreactive cells and fibers in the rat brain: an immunohistochemical study. Neuroendocrinology 36:165–186
Tamashiro KL, Hegeman MA, Nguyen MM, Melhorn SJ, Ma LY, Woods SC, Sakai RR (2007) Dynamic body weight and body composition changes in response to subordination stress. Physiol Behav 91:440–448
Tannenbaum BM, Brindley DN, Tannenbaum GS, Dallman MF, McArthur MD, Meaney MJ (1997) High-fat feeding alters both basal and stress-induced hypothalamic–pituitary–adrenal activity in the rat. Am J Physiol 273:E1168–E1177
Ueta Y, Ozaki Y, Saito J, Onaka T (2003) Involvement of novel feeding-related peptides in neuroendocrine response to stress. Exp Biol Med 228:1168–1174
Valles A, Marti O, Garcia A, Armario A (2000) Single exposure to stressors causes long-lasting, stress-dependent reduction of food intake in rats. Am J Physiol 279:R1138–R1144
Vergoni AV, Bertolini A (2000) Role of melanocortins in the central control of feeding. Eur J Pharmacol 405:25–32
Walker DL, Davis M (2002) Quantifying fear potentiated startle using absolute versus proportional increase scoring methods: implications for the neurocircuitry of fear and anxiety. Psychopharmacology 164:318–328
Acknowledgements
This study was supported by funds from the Canadian Institutes of Health Research (CIHR) and the Natural Science and Engineering Research Council of Canada (NSERC). HA is a Canadian Research Chair in Neuroscience. All experiments were conducted in accordance with the current laws of Canada. None of the authors have any direct or indirect conflicts of interests of a financial nature relevant to the present work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Merali, Z., Cayer, C., Kent, P. et al. Nesfatin-1 increases anxiety- and fear-related behaviors in the rat. Psychopharmacology 201, 115–123 (2008). https://doi.org/10.1007/s00213-008-1252-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-008-1252-2