Abstract
Rationale
Impulsivity is related to greater risk of nicotine dependence, perhaps by enhancing sensitivity to nicotine’s reinforcing and rewarding effects during initial smoking experiences.
Objective
We examined the influence of impulsivity characteristics on acute sensitivity to nicotine reward, reinforcement, and other effects in 131 young adult nonsmokers.
Materials and methods
Participants engaged in four sessions: the first three to assess dose–response effects of nasal spray nicotine (0, 5, 10 μg/kg) on reward, as well as mood, physiological, and performance effects, and the fourth to assess nicotine reinforcement using a choice procedure. Five impulsivity factors, derived from factor analysis of self-report (e.g., Barratt Impulsivity Scale, Sensation-Seeking Scale, Novelty seeking) and computer (stop–go, delay discounting, probability discounting) measures of impulsivity, were labeled “novelty seeking”, “response disinhibition”, “extraversion”, “inhibition”, and “probability/delay discounting”.
Results
The associations of novelty seeking with nicotine reinforcement and reward tended to move in opposite directions by sex, generally being directly related in men but inversely or unrelated in women. Similarly, response disinhibition was associated with reward and some mood responses to nicotine that differed by sex. Extraversion was inversely associated with nicotine reinforcement. Characteristics loading on to the other impulsivity factors had little association with nicotine sensitivity.
Conclusions
These results are preliminary, but they suggest that characteristics broadly related to impulsivity, especially novelty seeking and response disinhibition, are associated with initial sensitivity to some effects of acute nicotine, including reinforcement and reward, and may do so differentially between men and women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fewer than half of all teens who experiment with tobacco become nicotine dependent (Anthony et al. 1994). Factors that may explain differential vulnerability to dependence among those ever exposed to tobacco are numerous and a major focus of research aimed at understanding and preventing dependence (e.g., Audrain-McGovern et al. 2008). One of the most studied characteristics associated with risk of dependence on nicotine, as well as other drugs, is impulsivity and associated traits such as inattention, novelty seeking, and disinhibition (e.g., Lane and Cherek 2001; deWit and Richards 2004; Kreek et al. 2005).
Smoking status and nicotine dependence severity are related to impulsivity in cross-sectional studies. For example, Reynolds et al. (2007) found that adolescent smokers appear more impulsive than adolescent nonsmokers on some measures, such as the self-report Barratt Impulsivity Scale (BIS) and a behavioral delay discounting task (i.e., degree to which smaller but immediate rewards are preferred over larger but delayed rewards) but not on other measures (probability discounting, stop–go task). Smoking status among adults is also related to delay discounting and other impulsivity measures (e.g., Bickel et al. 1999; Mitchell 1999). Moreover, within smokers, some measures of impulsivity are higher among those who relapse more quickly after a quit attempt, both in adolescents (Krishnan-Sarin et al. 2007) and in adults (Doran et al. 2004), suggesting that impulsivity contributes to greater persistence of dependence. Similarly, adult smokers with current or past history of attention deficit hyperactivity disorder (ADHD), marked by impulsivity and inattention, show more severe withdrawal symptoms on some measures when attempting to quit (Pomerleau et al. 2003; McClernon et al. 2008).
While some theories propose that smoking exposure can foster impulsivity (deBry and Tiffany 2008), other research suggests that impulsivity may be causally related to onset of regular smoking. Characteristics related to impulsivity, such as inattention (Burke et al. 2001), risk-taking (Burt et al. 2000), extraversion (Harakeh et al. 2006), novelty seeking (Masse and Tremblay 1997), and ADHD itself (Milberger et al., 1997), are prospectively associated with onset of smoking in adolescents. Similarly, in preclinical findings with rodents, impulsivity predicts enhanced acquisition of nicotine self-administration (Diergaarde et al. 2008).
One mechanism to explain this link is that nicotine may have greater positively and/or negatively reinforcing effects in impulsive individuals, perhaps due to its dopaminergic actions. Although reduced central serotonergic activity is believed to be critical to impulsivity, effects of stimulant medications such as methylphenidate in relieving symptoms of impulsive disorders suggest that dopaminergic transmission also has important but complex influences on impulsivity, particularly in prefrontal cortex and basal ganglia (Dalley et al. 2008; Pattij and Vandenschuren 2008). Thus, because of their dopaminergic actions, other stimulants, including nicotine, may elicit greater negative reinforcement (e.g., alleviation of discomfort or cognitive deficits) in those who are more impulsive. Several observations support this notion. Nicotine via patch acutely alleviates difficulty concentrating and ADHD symptoms in adult smokers with ADHD who briefly abstain from smoking, similar to effects of ADHD medication (Gehricke et al. 2006). Nicotine via patch also improves cognitive performance (recognition memory) and decreases impulsive performance (stop–go task) in adolescent nonsmokers with ADHD (Potter and Newhouse 2004, 2008), indicating that nicotine’s effects may be a true pharmacological influence and not due simply to relief of tobacco withdrawal symptoms (Hughes 1991).
Aside from nicotine having greater negatively reinforcing effects in those with the disorder of ADHD, acute nicotine may have greater positively reinforcing effects (e.g., pleasure or reward) in such individuals. These effects may also be seen in those with impulsive personality characteristics that are not pathological but within normal levels. For example, novelty seeking may be characterized by heightened reactivity to novel stimuli, and drug exposure in a naïve individual may be viewed as presenting novel interoceptive stimuli (see Kreek et al. 2005). Consistent with this idea, we found greater subjective stimulation in response to acute nicotine administration as a function of higher scores on the disinhibition and experience-seeking subscales of the Sensation-Seeking Scale (SSS; see Zuckerman 1994) but only in young adult nonsmokers and not in smokers (Perkins et al. 2000). Therefore, characteristics related to impulsivity may influence sensitivity to nicotine upon early exposure, but not after chronic exposure and the onset of dependence and tolerance to nicotine’s effects. Impulsivity in humans increases risk of other drug use (Kreek et al. 2005) and may similarly influence initial sensitivity to other drugs as higher scores on several SSS subscales are associated with greater mood responses to amphetamine in healthy non-drug-abusing adults (Hutchison et al. 1999; Kelly et al. 2006).
Other research promotes the view that impulsivity may increase risk of dependence by enhancing “initial” sensitivity to nicotine, i.e., upon early exposure. The “sensitivity” model of Pomerleau (1995) proposes that individuals at higher risk for nicotine dependence experience greater pleasurable, and perhaps aversive, effects of nicotine when they first experiment with tobacco, compared to individuals at lower risk for dependence. Greater effects at early exposure may increase the chances of repeated tobacco use, leading to escalation of use and onset of dependence. In several studies, adults who currently smoke reported retrospectively having had greater pleasant sensations the first time they ever smoked, compared to adults who had never smoked regularly but had had some exposure (e.g., Hu et al. 2006; O’Connor et al. 2005; Pomerleau et al. 2004). The sensitivity model is based on animal research showing genetic or other individual differences in sensitivity to nicotine effects (Marks, et al. 1991; Schechter et al. 1995). Rat strains that are more sensitive to nicotine upon initial exposure may show greater subsequent acquisition of nicotine reinforcement (Le et al. 2006).
In summary, impulsivity may be one factor, among others, that increases vulnerability to nicotine dependence by increasing initial sensitivity to the acute rewarding and reinforcing effects of nicotine. In this study, we examined the influence of various dimensions of impulsivity on initial sensitivity to acute nicotine administration in young adult nonsmokers. A number of measures related to impulsivity were examined because of the evidence that impulsivity may comprise several independent factors (Evenden 1999). We chose nonsmokers (i.e., those with minimal tobacco exposure history) to ensure that responses to nicotine would reflect their initial sensitivity to the drug, unaltered by the onset of chronic tolerance to nicotine, which occurs fairly rapidly as teens persist in experimenting with cigarettes (Gervais et al. 2006). Tolerance, by definition, blunts overall sensitivity to nicotine and perhaps the degree of variability in sensitivity between individuals (Perkins et al. 2000, 2001a), thus hampering the identification of factors that explain this variability, such as impulsivity. Our focus was on measures of nicotine reward and reinforcement, but our assessments included measures of mood, physiological, and performance responses that may help explain nicotine reward and reinforcement in naïve users (Eissenberg and Balster 2000).
Materials and methods
Participants
Prospective participants were recruited through flyers and advertisements posted in a university community offering monetary compensation for their research participation. Participants completing the study were 131 young adult “nonsmokers” (51 men, 80 women) aged 21–39, with no more than ten lifetime tobacco exposures (i.e., ten cigarettes or combinations of cigarettes, cigars, smokeless tobacco uses, etc.) and no use in the prior 3 years. In a survey of over 8,000 Americans aged 15–54 (Anthony et al. 1994), about 24% never used tobacco, and another 51% used tobacco but never became dependent. Although many of the latter users used tobacco more than ten times without becoming dependent, these survey results suggest that our criterion of ten or fewer lifetime tobacco exposures characterizes at least half of young adults. Lifetime tobacco use was assessed at two points, during the initial telephone screening and at the subsequent in-person interview, and was required to be consistent on both occasions, for reliability. In addition, participant responses about tobacco history were subsequently corroborated from reports by at least two collaterals, long-time friends or family members, who were asked about the participant’s tobacco use history. The tobacco use history reported by another 47 prospective participants was not corroborated by collaterals, and so they were excluded from participation.
Subjects received a full physical exam by a physician to rule out current or recent medical or psychiatric problems contraindicating participation. The physical exam included lab tests for abnormal heart, liver, or thyroid function. Current problem alcohol use was an exclusion criterion, determined by self-report of more than 24 standard drinks per week. Those with current or recent illicit drug use, determined by self-report or urine drug screen, were excluded, as were those reporting current use of psychiatric medications. Urine drug screen assessed presence of the following: amphetamine, barbiturates, benzodiazepines, benzoylecgonine (cocaine metabolite), methadone, opiates, phencyclidine, and propoxyphene. Based on this medical screening, 11 others were excluded from participation. Another four dropped out prior to completing all sessions, and one dropped out due to adverse responses to the nasal spray. Mean characteristics of the final sample of 131 are presented in Table 1. Men and women did not differ significantly on these characteristics.
Measures of impulsivity
Because a number of characteristics related to impulsivity have been associated with smoking risk, as noted in the “Introduction”, and impulsivity may be multi-dimensional (Evenden 1999), we examined a variety of measures assessing these characteristics. Most of the measures have been used in prior research on impulsivity and smoking or other drug use (e.g., Bickel et al. 1999; Mitchell 1999; Reynolds et al. 2007). These measures were assessed during the screening session prior to any experimental sessions involving nicotine exposure (see “Procedures”, below). Mean scores on these tasks for the men and women in this study, along with normative data on these tasks where available, are provided in Table 2. The first seven are paper-and-pencil self-report measures, and the last three are computer tasks:
-
1.
The SSS (Zuckerman 1994) has four subscales, each containing ten items and labeled: Thrill and Adventure Seeking (TAS), Experience Seeking (ES), Disinhibition (DIS), and Boredom Susceptibility (BS). The range of each subscale is 0–10, and the total SSS score can range from 0 to 40.
-
2.
The Temperament and Character Inventory (TCI; Cloninger et al. 1994) is a 98-item true/false self-report instrument with three dimensions: novelty seeking, harm avoidance, and reward dependence. Its development, scoring, and psychometric properties are discussed in Cloninger et al. (1994). We used only the novelty-seeking subscale as the other two scales have not been consistently related to drug use (Howard et al. 1997).
-
3.
The Barratt Impulsiveness Scale (BIS; see Patton et al. 1995) contains 30 items assessing motor, attentional, and non-planning impulsiveness. We used the total score.
-
4.
The Buss–Durkee Hostility Inventory (BDHI; Buss and Durkee 1957) is a 75-item true–false measure of impulsive aggression consisting of seven subscales. We examined only the verbal aggression subscale. Hostility and anger have been associated with greater sensitivity to nicotine’s acute mood effects (e.g., Jamner et al. 1999).
-
5.
The Eysenck Personality Inventory (EPI; Eysenck and Eysenck 1968) contains 57 items, including extraversion and impulsivity subscales.
-
6.
The Behavioral Inhibition Scale/Behavioral Activation Scale (BIS/BAS; Carver and White 1994) is a 20-item measure of behavioral inhibition (seven items) and behavioral activation (13 items across three subscales combining reward responsiveness, drive, and fun seeking). This measure shows good reliability and validity (Campbell-Sills et al. 2004).
-
7.
The ADHD symptoms scale (Murphy and Schachar 2000) consists of 18 items representing current attention deficit and hyperactive/impulsive symptoms. The total score produced a single summary index of ADHD symptoms.
-
8.
The computerized stop/go task was adapted from that developed by Logan et al. (1997). It required participants to perform a choice reaction time task when presented with a visual target (“go”), requiring a left or right key press contingent on the appearance of an “X” or an “O”, respectively. Occasional (25%) trials also involved a subsequent auditory “stop” signal, indicating they should inhibit the key press response. The delay (in milliseconds) between the target presentation and the stop signal was varied until participants inhibited the response on 50% of the stop trials. Longer delays on stop trials indicate greater impulsivity (Logan et al. 1997). Subjects performed four sets of 64 trials, with an inter-trial interval of 2 s.
-
9.
The computerized delay discounting task was adapted from those used in smoking research by others (Bickel et al. 1999; Mitchell 1999; Ohmura et al. 2005; Reynolds et al. 2007). Participants were given a series of choices, in random order, between receiving $10 at some later time versus a smaller amount available immediately. The delay to receiving the $10 option was 1 day, 7 days, 1 month, 6 months, or 12 months. The alternative choice, the amount of money available immediately, decreased by $1 until the immediate amount was selected at least twice in comparison with each of the delays in the $10 option. Participants were told that one of the choices they made would be selected at random at the end of the session and they would actually get the amount they chose after the delay indicated. In actuality, one of the immediate amounts they chose was always selected, randomly, and the participant immediately received that amount of money. Greater delay discounting (and impulsivity) was indicated by smaller amounts of the immediate money chosen over the various delays to receiving $10. We used the area under the discounting curve as the measure of discounting (i.e., smaller area under the curve indicated greater delay discounting), similar to procedures described by others and found to correlate with amount of smoking (e.g., Ohmura et al. 2005). For purposes of description, the median “k” value for the sample was 0.0076, and the “ED50”, the inverse of k, was 131.7 days. (ED50 provides an index of how long it takes until the delayed reward is discounted by 50%; Yoon and Higgins 2008.)
-
10.
The computerized probability discounting task was adapted from similar tasks used in studies of drug dependence (e.g., Mitchell 1999; Reynolds et al. 2007). Participants were given a starting amount of $4 and instructed to choose between either a “risky” option, in which they could either gain $.50 or lose $.20, or a “time out” involving no gain or loss of money. Responses on the risky option eventually produced a net loss of money (i.e., three times as many $.20 losses as $.50 gains). Greater impulsivity was indicated by the greater percentage of risky choices. Again, participants were told they would receive, and did receive, whatever money they had left at the end of the task.
Impulsivity factors
To reduce the number of statistical comparisons, the impulsivity measures were subjected to a factor analysis, using a principal components analysis with a Promax rotation with Kaiser normalization. Promax rotation was chosen for its conceptual simplicity. Factors with eigenvalues >1 were retained, yielding five factors named by the measures loading most strongly on the factor. (See Table 3 for the factor coefficient scores and Table 4 for the factor intercorrelations.) To standardize the impulsivity factor scores, all were converted to z scores for analyses. For most of the impulsivity measures, the number of missing values was small, ranging from 0 to 2. The exceptions were the BIS/BAS measure (n = 7) and the computerized impulsivity measures (stop/go—n = 13; delay discounting—n = 4; and probability discounting—n = 3), which were not included in the protocol at the very start of the study. Measures loading most heavily onto the five factors (with factor names in parentheses) are as follows:
-
1:
“Novelty seeking”: Buss–Durkee Hostility Inventory—verbal aggression; Sensation-Seeking Scale—experience-seeking and disinhibition subscales; and the Temperament and Character Inventory—novelty-seeking scale
-
2:
“Response Disinhibition”: Attention Deficit Hyperactivity Disorder Scale, Barratt Impulsiveness Scale, stop/go computer task
-
3:
“Extraversion”: Eysenck extraversion subscale; BIS/BAS Behavioral Activation Scale—combined reward responsiveness, drive, and fun-seeking subscales
-
4:
“Inhibition”: BIS/BAS Behavioral Inhibition Scale
-
5:
“Probability/Delay Discounting”: probability discounting and delay discounting computer tasks
Dependent measures
Nicotine sensitivity was determined by acute responses to nicotine via spray on a variety of measures across several response domains: self-report reward and related ratings, subjective mood, physiological effects, performance effects, and a choice measure of reinforcement. However, of primary interest were the reinforcement and reward-related measures.
Nicotine reinforcement
The relative reinforcing effects of nicotine were determined by the number of nicotine (1.25 μg/kg/spray) versus placebo sprays selected in a choice procedure, described below in “Procedures”. Greater nicotine choice via this procedure has been related to greater pleasurable responses to nicotine in nonsmokers, as well as smokers (Perkins et al. 2001b). Nicotine choice also increases in smokers with overnight abstinence (Perkins et al. 1996), predicts greater withdrawal severity and faster relapse in smokers trying to quit (Perkins et al. 2002a, b), and is sensitive to individual difference characteristics, including obesity (Blendy et al. 2005) and genetics (Ray et al. 2006).
Reward and other spray ratings
Spray ratings of nicotine reward, incentive salience, perception, and sensory irritation were assessed with visual analog scales (VAS), scored 0–100, with 0 and 100 anchored by “not at all” and “extremely”, respectively. Nicotine “reward”, or its hedonic value (Everitt and Robbins 2005), was assessed using VAS ratings of “liking” and “satisfying.” Incentive salience was assessed by a similar VAS item of “want more”. Of secondary interest were ratings of perception of the nicotine content in sprays, assessed with VAS items “Feel the effects” and “How much nicotine”. These measures have been shown in other research to be sensitive to nicotine administration and to individual differences in sensitivity to nicotine intake via smoking (Perkins et al. 2001a). We also assessed nasal “irritation” via a similar VAS item for use as a covariate to control for sensory irritation from the spray, which could influence responses independent of the nicotine content of the spray.
Self-reported mood
Mood measures included (a) the Positive And Negative Affect Scale (PANAS; Watson et al. 1988), with positive and negative affect subscales; (b) the Profile of Mood States (POMS; McNair et al. 1971), with subscales labeled tension, anger, fatigue, vigor, depression; and (c) a series of 12 VAS (scored 0–100) items: comfortable, satisfied, pleasant, relaxed, buzzed, jittery, anxious, tired, sedated, alert, stimulated, and nausea. These measures have been shown to be reliable and have been used in many studies of acute nicotine effects in smokers and nonsmokers (e.g., Perkins et al. 2001a, 2003; Kalman and Smith 2005).
Physiological responses
Heart rate (HR; in beats per minute), systolic and diastolic blood pressure (BP, in millimeter Hg), were obtained automatically by Dinamap blood pressure recorder (Critikon Inc., Tampa, FL, USA). Cortisol was obtained by saliva sample using a Sarstedt salivette (dental swab) that was analyzed by Salimetrics, LLC (State College, PA, www.salimetrics.com).
Performance tasks
Performance tasks assessed after each spray administration included finger-tapping performance on two components (fast and slow), handsteadiness, Sternberg rapid information-processing, and memory recall. Most of these tasks, and the dose–response effects of nicotine on them in nonsmokers as well as smokers, have been described elsewhere (Grobe et al. 1998; Perkins et al. 1994a, 2001a) and will be only briefly described here:
-
a.
Finger tapping required tapping with the index finger on one key of a computer keypad. The task involved two contrary components, one requiring rapid responding as quickly as possible (“fast”) and assessed as the time needed to tap 100 times, and the other assessing ability to delay responses to no more than once every 10–12 s. For the latter component, which lasted 60 s, we determined the percentage of times subjects correctly responded within the 10–12-s time window (“slow %”). The slow tap component, based on a similar task in Popke et al. (2000), is a variation on a differential reinforcement of low response rate schedule, or DRL (Mackintosh 1974), which requires inhibition of responding, or patience. Nicotine has been shown to increase response rate on a DRL task in rats, thereby decreasing accuracy (percent correct; Popke et al. 2000). The two components were each presented three times per dosing trial, in alternating fashion.
-
b.
Handsteadiness was assessed by the Gardner Steadiness Tester (Lafayette Instruments, Lafayette, IN, USA).
-
c.
For the Sternberg rapid information-processing task, subjects were given one or five “target” letters to retain in short-term memory. They then were to respond as quickly as possible to a series of letter pairs, indicating whether the given letter pair did (“hits”) or did not (“correct rejections”) contain a target letter. The difference in reaction time in milliseconds between the one- and five-letter trials (“D-prime”) on items requiring correct rejection (involving processing of all target letters) was the primary measure of memory scanning speed (information processing; Schneider and Shiffrin 1977). A different series of target letters was used with each administration of this task. Because responding on this task has been shown to be improved (i.e., faster) by nicotine in smokers under distracting conditions, involving auditory presentation of non-target letters (Grobe et al. 1998), this task was presented in the current study under both distracting and non-distracting conditions, in random order, during each dose trial.
-
d.
Memory recall was assessed by presenting at one time a list of 20 one-syllable nouns 5 min after dosing. Testing for recall occurred 15 min later by presenting 40 words (20 original and 20 new) one at a time. Different word lists were used with each administration of this task. We assessed total correct choices, as well as failures to identify one of the original words (“misses”) and misidentifications of a new word as one of the original (“false alarms”).
Nicotine dosing
Nicotine was administered via a nasal spray procedure developed by us and used in many studies (e.g., Perkins et al. 1986, 1994a, 2001a). Controlled nicotine dosing via tobacco smoking is difficult to do, includes administration of thousands of compounds other than nicotine, and presents very challenging ethical and practical difficulties in research on nicotine effects in naïve participants (Pomerleau et al. 1989). Control of dosing is reasonably good by nasal spray in nonsmokers and smokers (Perkins et al. 1994a, 2001a), can be corrected for participant’s body weight, and results in uptake of nicotine somewhat closer to the speed of uptake with smoking compared to most other nicotine dosing methods (Schneider et al. 1996).
Each participant received 0, 5, and 10 μg/kg doses, spread over eight sprays (two at 30 s), with only one of the doses presented on a given day. Bioavailability of nicotine from nasal spray is about 60–75% (Johansson et al. 1991), and exposure to 5- and 10-μg/kg doses produces plasma nicotine levels comparable to about 1/4 and 1/2 typical cigarette, respectively (Perkins et al. 1994a, 2001a). We selected these relatively low doses because these are typical of amounts naive individuals are likely to absorb in initial experimentation with smoking (Eissenberg and Balster 2000), which we were trying to simulate in these assessments. We also wanted to avoid adverse responses to nicotine, which are common in naïve individuals. To determine actual nicotine exposure, a blood sample was obtained by venipuncture at the end of each session, about 40 min after the third and last spray administration. Samples were analyzed for plasma nicotine concentration by gas chromatography with nitrogen–phosphorus detection using 5-methylnicotine as the internal standard (Jacob et al. 1981). Mean ± SEM plasma nicotine levels following the 5- and 10-μg/kg dose sessions were 2.3 ± 0.1 and 3.4 ± 0.2 ng/ml, respectively.
Procedures
Subjects were first screened at an introductory session, during which they also completed the impulsivity measures described above and were scheduled for their physical exam. Subjects then participated in four sessions: three to assess nicotine sensitivity to most measures and a fourth to assess nicotine reinforcement. Details of each assessment are described below. The first three sessions involved repeated administration of one of three different doses of nicotine spray (0, 5, 10 μg/kg) per session, with the order of doses across sessions counterbalanced. The fourth session, to assess reinforcement, involved choice between sprays administering placebo (0) or 1.25 μg/kg/spray (equivalent to the 10 μg/kg dose, which was delivered in eight sprays). Upon arrival to the lab for each session, subjects first provided expired-air carbon monoxide (CO) assessment (Vitalograph CO analyzer, Breathco, Inc., Lenexa, KS, USA) to further verify absence of any recent smoking exposure (CO < 5 ppm) and breathalyzer assessment (Alco-Sensor III breathalyzer, Intoximeters Inc., St Louis, MO, USA) to verify no recent alcohol intake (BAL = 0.00).
Nicotine sensitivity assessment
The procedure for each 3-h sensitivity session was identical, except for the particular dose administered. Subjects first rested quietly for 5 min in an armchair followed by a baseline assessment of cardiovascular responses, subjective mood, and then the performance measures. This sequence of measures was repeated for two more baseline trials, one every 30 min, to habituate to testing. Then, this assessment sequence was repeated another three times (three dose trials), again once every 30 min, with each assessment following nasal spray dosing. Each dosing involved eight spray administrations and took 2 min, followed by cardiovascular and subjective measures during minutes 3–7 post-dosing and the performance measures during minutes 8–22 post-dosing. Subjects rested comfortably until the subsequent dose administration. A cortisol sample was obtained at the end of baseline and after the third (last) dose trial.
Nicotine reinforcement assessment
At the start of the 2.5-h choice session, participants first engaged in two “sampling” trials. They self-administered the 0- (placebo) or 1.25-μg/kg/spray bottles eight times each (i.e., 0 and 10 μg/kg in all, respectively), waited 20 min, then self-administered the other bottle eight times, in blinded fashion and counterbalanced order. Spray bottles were marked with different colored tapes to distinguish between them. After each set of eight sprays was taken, blood pressure and mood measures were assessed, but participants did not complete the other measures used in the previous three sessions to assess nicotine sensitivity. In the subsequent four “choice” trials, one every 20 min, participants were allowed to select any combination of the two sprays, such that they self-administered a total of eight sprays during each trial. The number of times nicotine was chosen was taken as the measure of reinforcement.
All subjects provided informed consent after the nature and consequences of participation were explained. This research was approved by the Institutional Review Board of the University of Pittsburgh Medical Center.
Data analysis
All analyses were conducted using SPSS 15.0. The number of missing values was small, ranging from 0 to 2 across all responses. We first determined any influence of dose order across sessions on nicotine responses but found no such order effects, allowing us to collapse across order. The primary dependent measures were the nicotine choice measure of reinforcement and the nicotine reward-related ratings (liking, satisfied, want more) obtained after each dosing. For all other measures, the response to each dose (0, 5, 10 μg/kg) was defined by change from pre-dose baseline to the post-dose mean of responses averaged across the three dose administrations per session. As noted in the “Results” where relevant, we followed up significant effects of impulsivity factor scores on these change-score measures by determining whether those effects might be influenced by differences in baseline due to those factor scores (which might suggest ceiling or floor effects; see also Perkins 1999).
Differences in responses to nicotine dose as a function of each of the five impulsivity factors were analyzed separately for each dependent measure using analysis of covariance (ANCOVA). Impulsivity factor score (continuous measure) and sex were the between-subjects factors, and dose was the within-subjects factor. The key effects of interest were the interactions of dose × impulsivity factor and the triple interaction of dose × impulsivity factor × sex, which would suggest differential sensitivity to nicotine dose due to impulsivity or both impulsivity and sex. Due to the continuous nature of impulsivity factor scores, comparisons following up significant dose × impulsivity factor interactions involved ANCOVAs of impulsivity factor effects limited to specific doses (0 versus 5 μg/kg or 0 versus 10 μg/kg) and conducted with only men or only women where sex was also significant. The measure of sensory irritation from the spray was included as a covariate in all analyses. Because of the numerous mood and performance measures, analyses of effects on those responses were first conducted using multivariate ANCOVA (MANCOVA) to reduce the number of comparisons. Significant MANCOVA results were followed up with univariate ANCOVAs. For the choice reinforcement measure, there was no dose effect (i.e., subjects chose either nicotine or placebo), and so ANCOVAs analyzed the influences of impulsivity factor and sex. For the primary dependent measures of reinforcement and reward, we included effect sizes (partial eta-squared values or \(\eta _{\text{p}} ^2 \)) of the effect of impulsivity factor score on reinforcement and of impulsivity factor × dose on reward. Where the interaction also included sex, effect sizes were presented separately for men and women.
To display the results in figures, we conducted median splits on the distribution of each impulsivity factor score, separately for men and women, and presented the means ± SEM for the high and low scoring subgroups for each impulsivity factor that was significantly associated with a nicotine response. (Scatterplots could not present results for all three doses in a single plot and did not clearly display the effects of interest.) To save space, the results of the follow-up comparisons to interactions, described above, are not presented in the text but are shown in each figure by asterisks indicating the significance of the association of impulsivity factor score with response to nicotine (0 versus 5 μg/kg, 0 versus 10 μg/kg). (However, note that the results of follow-up comparisons do not necessarily conform closely to the pattern of means for the high and low subgroups in the figures as those subgroups were not used in any analyses.)
Finally, we conducted exploratory follow-up analyses to examine which of the individual measures loading onto an impulsivity factor may have been responsible for the association between that impulsivity factor and nicotine responses. The rationale was to provide directions for future research as to which of these measures may hold the most promise in identifying specific characteristics of impulsivity related to nicotine sensitivity. (To conserve space, the full results of those exploratory analyses are not presented; we list only the individual measures significantly related to the effects of interest.)
Results
Reinforcement and reward
Reinforcement
The nicotine choice measure of reinforcement was influenced by impulsivity factor 3 (extraversion), F(1, 119) = 6.19, p < 0.05, \(\eta _{\text{p}} ^2 = 0.055\) and by the interaction of sex × impulsivity factor 1 (novelty seeking), F(1, 125) = 10.04, p < 0.005, \(\eta _{\text{p}} ^2 = 0.049\) for men, 0.112 for women. As shown in Fig. 1, higher scores on impulsivity factor 3 were associated with less nicotine choice. In follow-up comparisons of the influence of impulsivity factor 1 scores within each sex, higher scores on impulsivity factor 1 were associated with significantly less choice in women but non-significantly greater choice in men (Fig. 1). (Alternatively, nicotine choice was significantly greater in men versus women among those with high factor 1 scores, while there was no sex difference among those with low factor 1 scores.)
Mean (SEM) number of times nicotine sprays (versus placebo sprays) were chosen in the choice measure of reinforcement (maximum possible of 32), by high and low subgroups on factors 1 (novelty seeking) and 3 (extraversion), and, where relevant, by sex. Data analyses involved regressions of continuous factor scores on the continuous response of nicotine choice, but results are presented here by high and low subgroups for ease of display. Asterisks indicate significant differences between subgroups. *p < 0.05
In exploratory analyses, we examined which of the individual measures loading on to impulsivity factors 1 and 3 were significantly related to nicotine choice. The factor 3 influence on nicotine choice reflected BIS/BAS-combined reward score (although the Eysenck extraversion score was marginally related to nicotine choice). The effect of sex × factor 1 on choice reflected the interactions of sex with Buss–Durkee score, with SSS—experience-seeking score and with TCI—novelty-seeking score.
Reward and related ratings
The interaction of dose × impulsivity factor 1 (novelty seeking) was significant for nicotine ratings of satisfying (reward) and want more (incentive salience), F(2, 250)’s = 3.37 and 3.39, respectively, both p < 0.05, \(\eta _{\text{p}} ^2 = 0.036\;{\text{and}}\;0.035{\text{,}}\) respectively. Satisfying was also influenced by the interaction of dose × sex × impulsivity factor 2 (response disinhibition), F(2, 224) = 3.43, p < 0.05, \(\eta _{\text{p}} ^2 = 0.005\;{\text{for}}\;{\text{men}},\;0.070\;{\text{for}}\;{\text{women}}\). (All of these effects are shown in Fig. 2 separately by sex because of the apparent consistency in the pattern of effects for these two factors and reward, although the interaction effects of dose × sex × impulsivity factor 1 on satisfying and on want more were just marginally significant, F(2, 250)’s = 2.58 and 2.49, respectively, both p < 0.10). As shown in Fig. 2, the follow-up comparisons within each sex showed that the association of factor 1 scores with nicotine’s effects on want more and satisfying were significant in men but not in women. However, higher factor 2 scores were associated with decreases in satisfying due to nicotine in women but not in men (Fig. 2).
Mean (SEM) dose–response effects of nasal spray nicotine (in microgram per kilogram) on self-report measures of incentive motivation (“want more”), reward (“satisfying”), and nicotine perception (“feel effects”), by sex and by high and low subgroups on impulsivity Factors 1 (novelty seeking), 2 (response disinhibition) and 5 (probability/delay discounting). Shown are responses showing significant effects of impulsivity factor × dose or impulsivity factor × dose × sex. Asterisks indicate significant differences due to impulsivity factor scores in the response to nicotine (5 or 10 μg/kg) versus placebo (0). Other details as in Fig. 1
The rating of feel the effects (nicotine perception) was influenced by the interaction of dose × impulsivity factor 5 (probability/delay discounting), F(2, 244) = 3.26, p < 0.05, and by dose × sex × factor 1, F(2, 250) = 3.26, p < 0.05. As also shown in Fig. 2, higher scores on impulsivity factor 5 were associated with greater feel effects in response to 5 μg/kg, but not 10 μg/kg, nicotine. Lower scores on impulsivity factor 1 tended to be associated with larger feel effects in response to the 5-μg/kg dose among men versus women, but follow-up comparisons of factor 1 effects within each sex were not significant (Fig. 2).
Exploratory analyses focused on the individual measures loading on to impulsivity factors 1, 2, and 5. The interaction effects of dose × factor 1 (novelty seeking) on satisfying and want more, noted above, generally reflected the influences of the SSS—experience seeking, TCI—novelty seeking, and Buss–Durkee Hostility scores; SSS—disinhibition had no effects. The interaction of dose × sex × factor 2 (response disinhibition) on satisfying reflected the influence of Barratt Impulsivity Scale score; the ADHD scale and stop/go task had no significant effects. Finally, the influences of impulsivity factor 1 and factor 5 (probability/delay discounting) on feel the effects reflected the influence of Buss–Durkee score and probability discounting, respectively; the other measures loading on to impulsivity factors 1 and 5 were not significantly related to these ratings.
Other nicotine effects
Mood
In the MANCOVAs of mood responses, impulsivity factor 2 (response disinhibition) interacted with dose and with dose × sex, F(24, 424)’s = 3.46 and 3.66, respectively, both p < 0.001. None of the other four impulsivity factors was significantly related to mood responses in MANCOVA analyses, and so were not examined further. In follow-up univariate analyses, the interaction of dose × impulsivity factor 2 was significant for the following mood responses: POMS scales of depression and anger, F(2, 224) = 7.63 and 16.32, respectively, both p < 0.001; POMS fatigue, F(2, 224) = 4.06, p < 0.05; PANAS-negative affect, F(2, 224) = 6.56, p < 0.005; VAS items of buzzed and stimulated, F(2, 224) = 3.09 and 3.43, respectively, both p < 0.05; and VAS relaxed, F(2, 224) = 5.62, p < 0.005. In addition, the triple interaction of dose × sex × impulsivity factor 2 was significant for POMS fatigue, F(2, 224) = 12.89, p < 0.001; PANAS-positive affect, F(2, 224) = 3.31, p < 0.05; VAS-stimulated, F(2, 224) = 3.58, p < 0.05; and VAS nausea, F(2, 224) = 10.23, p < 0.001.
Representative findings are displayed in Fig. 3. As shown there, higher scores on impulsivity factor 2 were associated with greater increase in anger and less decline in relaxed in response to nicotine (versus placebo). Among women, but not men, higher factor 2 scores were associated with greater decrease in fatigue and less decrease in stimulated in response to nicotine. In subsequent analyses, we found that factor 2 and the interaction of factor 2 × sex were associated with baseline levels of several of these mood measures. However, all of the above effects on mood responses to nicotine remained significant after covarying for baseline levels, except that the effect of dose × sex × impulsivity factor 2 on VAS-stimulated became marginally significant (p < 0.10).
Mean (SEM) dose–response effects of nicotine on representative mood responses, by high and low subgroups on impulsivity factor 2 (response disinhibition) and, where relevant, by sex. Data are changes from baseline. Shown are significant associations from the univariate analyses following up the significant results of the multivariate analyses. *p < 0.05, **p < 0.01, ***p < 0.001. Other details as in Figs. 1 and 2
In exploratory analyses of the individual measures loading on to impulsivity factor 2, the interaction effects on mood involving factor 2 generally reflected the influence of Barratt Impulsivity and ADHD scale scores; the stop/go task loading onto impulsivity factor 2 did not relate to these mood responses to nicotine.
Performance tasks
Similar to the mood results, only impulsivity factor 2 was significantly related to performance tasks in MANCOVAs as the interaction of dose × factor 2 was significant, F(26, 418) = 1.53, p < 0.05. In follow-up univariate analyses, the interaction of dose × factor 2 influenced memory recognition (words missed), F(2, 222) = 3.16, p < 0.05; fast tapping, F(2, 222) = 2.96, p = 0.05; and DRL (slow tapping %), F(2, 222) = 3.28, p < 0.05. As shown in Fig. 4, lower scores on impulsivity factor 2 were associated with poorer memory performance (more words missed). Follow-up comparisons of factor 2 scores with finger tapping or DRL responding were not significant. In subsequent analyses, we found no baseline differences due to impulsivity factor 2 on these performance measures.
Mean (SEM) dose–response effects of nicotine on memory recall, fast-tapping speed, and DRL (“slow tap%”) task performance, by high and low subgroups on impulsivity factor 2 (response disinhibition). Data are changes from baseline. Positive values indicate poorer memory recall (number of words missed), slower fast-tapping speed (time in seconds to emit 100 taps), and better DRL performance (greater accuracy in responding within 10–12 s time window). Other details as in Figs. 1, 2 and 3
In the exploratory analyses of the individual measures loading onto impulsivity factor 2, memory recognition was influenced by Barratt Impulsivity Scale score and ADHD scale score. No individual measures were significantly related to fast or slow tapping.
Physiological responses
HR was influenced by the interaction of dose × impulsivity factor 3 (extraversion), F(2, 230) = 3.22, p = 0.05. Diastolic blood pressure (DBP) was influenced by the interactions of dose × sex × impulsivity factor 1, F(2, 242) = 4.50, p = 0.01, and of dose × sex × impulsivity factor 4 (inhibition), F(2, 230) = 3.78, p < 0.05. No factors were related to SBP or to cortisol response. As shown in Fig. 5, higher scores on impulsivity factor 4 (i.e., greater inhibition) were associated with greater DBP response to the 5-μg/kg dose in men but not in women. The other follow-up comparisons of factor 1 scores with DBP by sex and factor 3 scores with HR were not significant. In subsequent analyses, we found no baseline differences due to these impulsivity factor scores, or of factor scores × sex, on these physiological measures.
In exploratory analyses, no individual measures loading onto impulsivity factor 3 were significantly related to HR. DBP was influenced by the Buss–Durkee score and SSS—disinhibition score, both loading on to impulsivity factor 1. Because impulsivity factor 4 largely comprises the BIS/BAS inhibition scale, the above effect of factor 4 on DBP reflects the influence of the BIS/BAS inhibition score.
Discussion
Our primary objective in this study was to examine the relationship between several dimensions of impulsivity and initial sensitivity to the reinforcing and rewarding effects of nicotine. Of secondary interest were associations of impulsivity with other nicotine effects that may help explain nicotine reward and reinforcement in naïve individuals. Our findings should be considered exploratory, given the relatively small sample and the large number of impulsivity factors and comparisons examined. However, we found that higher scores on factor 1 (novelty seeking) were differentially related to nicotine reinforcement and reward between men and women, decreasing reinforcement in women but not in men and increasing reward in men but not in women. Similarly, higher factor 2 (response disinhibition) scores decreased reward in women but not in men. We also found that scores on factor 3 (extraversion) were inversely related to nicotine reinforcement regardless of sex. Although these results require replication, they identify specific components of impulsive personality traits that may relate to initial sensitivity to nicotine reward and reinforcement, and they also provide the first evidence for gender heterogeneity in these effects. Results theoretically could help explain how some facets of impulsivity may promote or deter escalation of tobacco use and onset of dependence among those with some tobacco exposure.
Secondarily, we were interested in associations of impulsivity with other responses to nicotine that may in turn influence reward and reinforcement. Fewer associations were found, although factor 2 (response disinhibition) was related to mood and performance effects of nicotine. Again, however, as with the association of factor 2 with reward, noted above, these associations with mood often differed between men and women, suggesting some consistency in the pattern of factor 2 effects across reward and mood measures of acute nicotine effects. Few nicotine responses were related to the other impulsivity factors, including factors 4 (inhibition) and 5 (probability/delay discounting).
Our findings are largely consistent with the few other prospective studies showing that characteristics related to impulsivity (e.g., sensation-seeking) are associated with greater sensitivity to nicotine (Perkins et al. 2000) and amphetamine (Hutchison et al. 1999; Kelly et al. 2006) in non-dependent young adults. Together, these findings give credence to the notion that impulsivity may increase drug abuse vulnerability by enhancing initial sensitivity to at least some stimulant drugs. Yet, our results address a fairly narrow question, whether personality characteristics related to impulsivity are associated with initial sensitivity to nicotine reward and reinforcement; our purpose was not to demonstrate a causal chain from impulsivity to nicotine dependence risk. Impulsivity could directly or indirectly increase risk of nicotine dependence or be broadly related to risk of all drug use (Kopstein et al. 2001; Kreek et al. 2005), independently of its association with greater sensitivity to particular drug responses.
It is also important to note that these relationships may hold only during initial exposure to nicotine, and the association of these impulsivity factors with nicotine responses could change as exposure escalates (i.e., during onset or persistence of dependence; Krishnan-Sarin et al. 2007; McClernon et al. 2008). Indeed, with novelty seeking, for example, heightened reactivity would be expected only in response to novel stimuli such as drug administration in a naïve individual rather than in a drug-experienced individual. Prior research has shown that sensation-seeking relates to nicotine sensitivity in nonsmokers, as in this study, but not in smokers (Perkins et al. 2000), whose chronic tolerance likely limits the variability in sensitivity to be explained by other factors. Similarly, preclinical research shows that rodent strains most sensitive to nicotine upon initial exposure often acquire the greatest tolerance to nicotine with chronic exposure (Marks et al. 1991).
Contrary to expectations, however, impulsivity factor 3 (extraversion) was inversely related to nicotine reinforcement. If reliable, this finding could suggest that extraversion does not increase risk of dependence by enhancing initial reinforcement from nicotine and must act via some other mechanism. Alternatively, it may be that extraversion in our sample of nonsmoking young adults reflects something different from extraversion in teens likely to experiment with cigarettes. Similarly, the computer tasks loading onto impulsivity factor 5 (probability/delay discounting), which have been shown to be sensitive cross-sectionally to smoking status or amount (Bickel et al. 1999; Mitchell 1999; Ohmura et al. 2005), were not associated with initial nicotine sensitivity in nonsmokers in this study, except for feel the effects (Fig. 2). Therefore, these tasks may be more predictive of differences associated with chronic smoking exposure, rather than as predictors of initial sensitivity to nicotine. Such tasks are also sensitive to acute effects of stimulant drug administration (e.g., deWit and Richards 2004), and future research on initial nicotine sensitivity should determine whether these tasks may be more informative as dependent measures (i.e., responses to nicotine) than as independent variables (i.e., predictors of nicotine sensitivity).
Several of the associations of impulsivity factors with nicotine reinforcement and reward differed by sex. Higher novelty seeking (factor 1) was related to reduced nicotine reinforcement (choice) in women, but not in men. Alternatively, among those with high but not low factor 1 scores, nicotine reinforcement was greater in men versus women. Higher scores on measures related to novelty seeking and response disinhibition (factor 2) tended to be associated with greater nicotine reward in men but less reward or no difference in women. Recent animal research similarly suggests that individual differences in novelty seeking may influence drug reinforcement differentially as a function of sex (e.g., Davis et al. 2008). Our findings could help explain prior research showing greater nicotine reward and reinforcement in men compared to women (Perkins et al. 1999, 2002a, b; Perkins 2008). This sex difference may be partly due to the greater overall levels of novelty seeking or response disinhibition in men versus women, as found in many normative studies (see Table 2). In other words, the sex differences in nicotine reward and reinforcement may result from factors that covary with sex, rather than necessarily being due directly to sex per se (see also Perkins 2004).
The methods of this study, many of them novel, allowed for perhaps the clearest test to date of the association between impulsivity measures and initial sensitivity to nicotine in humans. A key strength of this study was the prospective assessment of nicotine responses, which included standardized measures of mood and responses to nicotine other than self-report, as opposed to the exclusively retrospective self-report of early responses to nicotine via smoking in past studies of initial sensitivity to nicotine (e.g., Pomerleau et al. 1998). Other strengths of this study included the controlled dosing of nicotine doses corrected for body weight, inclusion of placebo and more than one dose of nicotine, and use of nasal irritation as a covariate. We employed 12 measures of impulsivity and then created five homogeneous factors in an attempt to fully characterize dimensions related to impulsivity. We also corroborated subject self-report of no or limited tobacco exposure history with reports by friends or family who were familiar with the subjects’ past, eliminating about one in four prospective participants whose reports of minimal tobacco use was not be corroborated. Verification that subjects were naïve to nicotine increases confidence that their responses to acute nicotine administration reflected their initial sensitivity, unaltered by onset of chronic tolerance due to more extensive smoking.
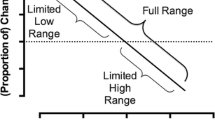
This study also had several limitations. First, we included young adults, rather than adolescents, due to ethical and practical concerns about giving nicotine to naïve adolescents. Adolescence is the age at which those who become smokers usually experience initial exposure, and impulsivity may have more influence on nicotine sensitivity at this age. Second, our sample may have been relatively homogeneous, despite the sample size of 131. For example, these young adults tended to be highly educated (Table 1). We also excluded those with more than ten lifetime uses of tobacco to rule out the presence of chronic tolerance to nicotine, as well as those with current or past drug, alcohol, or psychiatric problems. Consequently, the range of subject responses on the impulsivity measures (Table 2) may have been narrow, making it more difficult for us to observe associations between the impulsivity factor scores comprising these measures and nicotine sensitivity.
In a third limitation, some of these findings may have occurred by chance, given the five impulsivity factors and four primary dependent measures of liking and satisfying for reward, want more for incentive salience, and the choice task of reinforcement, as well as our interest in interactions of dose with sex. The reward-related variables were single-item measures, which may make them less stable than multi-item measures. Moreover, the similarity in the associations of satisfying with both factors 1 and 2 (Fig. 2) may be partly due to the intercorrelation of 0.341 between the two factors (Table 4). We attempted to minimize the number of a priori comparisons by focusing on reward and reinforcement, and we used multivariate analyses of mood and performance effects to further reduce the likelihood of chance findings. However, we included a large number of impulsivity measures and nicotine responses because of the lack of prior findings in this area that could narrowly focus our efforts. We view this research as exploratory in nature and requiring substantial more attention to identify reliable conclusions on the association of impulsivity characteristics and initial nicotine sensitivity.
In addition, despite its strengths, our nicotine administration procedure is also a limitation of the study. Sensitivity to nicotine via nasal spray may not relate to sensitivity to nicotine via cigarette smoking, although one study with smokers suggests generally comparable acute mood responses to nicotine between these methods (Perkins et al. 1994b). A more rapid uptake of nicotine by smoking, or stimuli accompanying smoking (e.g., taste, smell) but not nasal spray, may influence initial sensitivity to nicotine intake by smoking in naive individuals. The doses used were fairly low to simulate amounts consumed during cigarette experimentation (Eissenberg and Balster 2000), i.e., the typical nicotine intake during initial exposure in the natural environment. The influence of impulsivity on nicotine sensitivity may be more apparent in acute testing with larger doses of nicotine. Finally, nicotine administration was presented solely under standardized neutral environmental conditions, and the context of early exposure to nicotine may be very influential in determining responses to that exposure (e.g., Perkins 1999).
In summary, initial sensitivity to nicotine reward and reinforcement was associated with impulsive personality characteristics related to novelty seeking, response disinhibition, and extraversion, but many of these associations differed between men and women. Characteristics loading on to the other factors examined—inhibition and probability/delay discounting—had little association with nicotine sensitivity. Future research should investigate initial sensitivity to a variety of nicotine responses via other methods of administration, especially cigarette smoking, and in more diverse samples of nicotine naïve individuals who may have more widely varying levels of impulsivity. Results could identify directions for targeting efforts at primary prevention of tobacco use to particularly vulnerable children and adolescents, and findings could increase our understanding of why nicotine is reinforcing and rewarding in naïve users.
References
Anthony JC, Warner LA, Kessler RC (1994) Comparative epidemiology of dependence on tobacco, alcohol, controlled substances, and inhalants: basic findings from the National Comorbidity Survey. Exper Clin Psychopharmacol 2:244–268
Audrain-McGovern J, Nigg J, Perkins KA (2008) Endophenotypes for nicotine dependence risk at or before initial nicotine exposure. National Cancer Institute Monograph 22, phenotypes and endophenotypes: foundations for genetic studies of nicotine use and dependence (chapter 7). NCI, Washington DC (in press)
Bickel WK, Odum AL, Madden GJ (1999) Impulsivity and cigarette smoking: delay discounting in current, never, and ex-smokers. Psychopharmacology 146:447–454
Blendy JA, Strasser A, Walters CL, Perkins KA, Patterson F, Berkowitz R, Lerman C (2005) Reduced nicotine reward in obesity: cross comparison in human and mouse. Psychopharmacology 180:306–315
Burke JD, Loeber R, Lahey BB (2001) Which aspects of ADHD are associated with tobacco use in early adolescence. J Child Psychol Psychiatr 42:493–502
Burt RD, Dinh KT, Peterson AV, Sarason IG (2000) Predicting adolescent smoking: a prospective study of personality variables. Prev Med 30:115–125
Buss AH, Durkee A (1957) An inventory for assessing different kinds of hostility. J Consult Psychol 21(4):343–554
Campbell-Sills L, Liverant GI, Brown TA (2004) Psychometric evaluation of the Behavioral Inhibition/Behavioral Activation Scales in a large sample of outpatients with anxiety and mood disorders. Psychol Assess 16:244–254
Carver CS, White TL (1994) Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS scales. J Personal Soc Psychol 67(2):319–334
Cloninger CR, Pryzbeck TR, Svrakic DM, Wetzel RD (1994) The Temperament and Character Inventory (TCI): a guide to its development and use. Center for Psychobiology of Personality, Washington University, St. Louis
Dalley JW, Mar AC, Economidou D, Robbins TW (2008) Neurobehavioral mechanisms of impulsivity: fronto–striatal systems and functional neurochemistry. Pharmacol Biochem Behav 90:250–260
Davis BA, Clinton SM, Akil H, Becker JB (2008) The effects of novelty-seeking phenotypes and sex differences on acquisition of cocaine self-administration in selectively bred High-Responder and Low-Responder rats. Pharmacol Biochem Behav 90:331–338
deBry SC, Tiffany ST (2008) Tobacco-induced neurotoxicity of adolescent cognitive development (TINACD): a proposed model for the development of impulsivity in nicotine dependence. Nic Tobacco Res 10:11–25
deWit H, Richards JB (2004) Dual determinants of drug use in humans: reward and impulsivity. In: Bevins RA, Bardo MT (eds) Motivational factors in the etiology of drug abuse. University of Nebraska Press, Lincoln, pp 19–55
Diergaarde L, Pattij T, Poortvliet I, Hogenboom F, deBries W, Schoffelmeer ANM, deVries TJ (2008) Impulsive choice and impulsive action predict vulnerability to distinct stages of nicotine seeking in rats. Biol Psychiatr 63:301–308
Doran N, Spring B, McChargue D, Pergadia M, Richmond M (2004) Impulsivity and smoking relapse. Nic Tobacco Res 6:641–647
DuPaul GJ, Power TJ, Anastopoulos AD, Reid R, McGoey KE, Ikeda MJ (1997) Teacher ratings of attention deficit hyperactivity disorder symptoms: factor structure and normative data. Psychol Assess 9(4):436–444
Eissenberg T, Balster RL (2000) Initial tobacco use episodes in children and adolescents: current knowledge, future directions. Drug Alc Depend 59(Suppl 1):S41–60
Evenden JL (1999) Varieties of impulsivity. Psychopharmacology 146:348–361
Everitt BJ, Robbins TW (2005) Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nature Neurosci 8:1481–1489
Eysenck HJ, Eysenck BG (1968) Eysenck Personality Inventory. Educational and Industrial Testing Services, San Diego
Gehricke JG, Whalen CK, Jamner LD, Wigal TL, Steinhoff K (2006) The reinforcing effects of nicotine and stimulant medication in the everyday lives of adult smokers with ADHD: a preliminary examination. Nic Tobacco Res 8:37–47
Gervais A, O’Loughlin J, Meshefedjian G, Bancej C, Tremblay M (2006) Milestones in the natural course of onset of cigarette use among adolescents. Can Med Assoc J 175:255–261
Grobe JE, Perkins KA, Goettler-Good J, Fonte C (1998) Importance of environmental distractors in the effects of nicotine on short-term memory. Exper Clin Psychopharmacol 6:209–216
Harakeh Z, Scholte RH, deVries H, Engels RC (2006) Association between personality and adolescent smoking. Addict Behav 31:232–245
Hester RK, Brown WR (1980) Eysenck Personality Inventory: a normative study on an adult industrial population. J Clin Psychol 36(4):937–939
Howard MO, Kivlahan D, Walker RD (1997) Cloninger’s tridimensional theory of personality and psychopathology: applications to substance use disorders. J Stud Alc 58:48–66
Hu MC, Davies M, Kandel DB (2006) Epidemiology and correlates of daily smoking and nicotine dependence among young adults in the United States. Amer J Publ Health 96:299–308
Hughes JR (1991) Distinguishing withdrawal relief and direct effects of smoking. Psychopharmacology 104:409–410
Hutchison KE, Wood MD, Swift R (1999) Personality factors moderate subjective and psychophysiological responses to d-amphetamine in humans. Exper Clin Psychopharmacol 7:493–501
Jacob P, Wilson M, Benowitz NL (1981) Improved gas chromatographic method for the determination of nicotine and cotinine in biologic fluids. J Chromatography 222:61–70
Jamner LD, Shapiro D, Jarvik ME (1999) Nicotine reduces the frequency of anger reports in smokers and nonsmokers with high but not low hostility: an ambulatory study. Exper Clin Psychopharmacol 7:454–463
Johansson C-J, Olsson P, Bende M, Carlsson T, Gunnarsson PO (1991) Absolute bioavailability of nicotine applied to different nasal regions. Eur J Clin Pharmacol 41:585–588
Kalman D, Smith SS (2005) Does nicotine do what we think it does? A meta-analytic review of the subjective effects of nicotine in nasal spray and intravenous studies with smokers and nonsmokers. Nic Tobacco Res 7:317–333
Kelly TH, Robbins G, Martin CA, Fillmore MT, Lane SD, Harrington NG, Rush CR (2006) Individual differences in drug abuse vulnerability: d-amphetamine and sensation-seeking status. Psychopharmacology 189:17–25
Kopstein AN, Crum RM, Celentano DD, Martin SS (2001) Sensation seeking needs among 8th and 11th graders: characteristics associated with cigarette and marijuana use. Drug Alc Depend 62:195–203
Kreek MJ, Nielsen DA, Butelman ER, LaForge KS (2005) Genetic influences on impulsivity, risk taking, stress responsivity and vulnerability to drug abuse and addiction. Nat Neurosci 8:1450–1457
Krishnan-Sarin S, Reynolds B, Duhig AM, Smith A, Liss T, McFetridge A, Cavallo DA, Carroll KM, Potenza MN (2007) Behavioral impulsivity predicts treatment outcome in a smoking cessation program for adolescent smokers. Drug Alc Depend 88:79–82
Lane SD, Cherek DR (2001) Risk taking by adolescents with maladaptive behavior histories. Exper Clin Psychopharmacol 9:74–82
Le AD, Li Z, Funk D, Shram M, Li TK, Shaham Y (2006) Increased vulnerability to nicotine self-administration and relapse in alcohol-naive offspring of rats selectively bred for high alcohol intake. J Neurosci 26:1872–1879
Logan GD, Schachar RJ, Tannock RT (1997) Impulsivity and inhibitory control. Psychol Sci 8:60–64
Mackintosh NJ (1974) The psychology of animal learning. Academic, New York
Marks MJ, Campbell SM, Romm E, Collins AC (1991) Genotype influences the development of tolerance to nicotine in the mouse. J Pharmacol Exper Ther 259:392–402
Masse LC, Tremblay RE (1997) Behavior of boys in kindergarten and the onset of substance use during adolescence. Arch Gen Psychiatr 54:62–68
McClernon FJ, Kollins SH, Lutz AM, Fitzgerald DP, Murray DW, Redman C, Rose JE (2008) Effects of smoking abstinence on adult smokers with and without attention deficit hyperactivity disorder: results of a preliminary study. Psychopharmacology 197:95–105
McNair DM, Loor M, Droppelman LF (1971) Profile of Mood States. Educational and Testing Service, San Diego
Milberger S, Biederman J, Faraone SV, Chen L, Jones J (1997) ADHD is associated with early initiation of cigarette smoking in children and adolescents. J Amer Acad Child Adol Psychiatr 36:37–44
Mitchell SH (1999) Measures of impulsivity in cigarette smokers and non-smokers. Psychopharmacology 146:455–464
Murphy P, Schachar R (2000) Use of self-ratings in the assessment of symptoms of attention deficit hyperactivity disorder in adults. Amer J Psychiatr 157:1156–1159
O’Connor RJ, Kozlowski LT, Vandenbergh DJ, Strasser AA, Grant MD, Vogler GP (2005) An examination of early smoking experiences and smoking status in a national cross-sectional sample. Addiction 100:1352–1357
Ohmura Y, Takahashi T, Kitamura N (2005) Discounting delayed and probabilistic monetary gains and losses by smokers of cigarettes. Psychopharmacology 182:508–515
Pattij T, Vandenschuren LJMJ (2008) The neuropharmacology of impulsive behaviour. Trends Pharmacol Sci 29:192–199
Patton JH, Stanford MS, Barratt ES (1995) Factor structure of the Barratt Impulsiveness Scale. J Clin Psychol 51:768–774
Perkins KA (1999) Baseline-dependency of nicotine effects: a review. Behav Pharmacol 10:597–615
Perkins KA (2004) Commentary: obstacles to determining individual differences in the efficacy of smoking cessation medications. Nic Tobacco Res 6:765–767
Perkins KA (2008) Sex differences in nicotine reinforcement and reward: influences on the persistence of tobacco smoking. In: Bevins R, Caggiula AR (eds) The motivational impact of nicotine and its role in tobacco use. Springer, New York
Perkins KA, Epstein LH, Stiller R, Jennings JR, Christiansen C, McCarthy T (1986) An aerosol spray alternative to cigarette smoking in the study of the behavioral and physiological effects of nicotine. Behav Res Meth Instr Comput 18:420–426
Perkins KA, Grobe JE, Fonte C, Goettler J, Caggiula AR, Reynolds WA, Stiller RL, Scierka A, Jacob RG (1994a) Chronic and acute tolerance to subjective, behavioral, and cardiovascular effects of nicotine in humans. J Pharmacol Exper Ther 270:628–638
Perkins KA, Sexton JE, Reynolds WA, Grobe JE, Fonte C, Stiller RL (1994b) Comparison of acute subjective and heart rate effects of nicotine intake via tobacco smoking vs. nasal spray. Pharmacol Biochem Behav 47:295–299
Perkins KA, Grobe JE, Weiss D, Fonte C, Caggiula A (1996) Nicotine preference in smokers as a function of smoking abstinence. Pharmacol Biochem Behav 55:257–263
Perkins KA, Donny E, Caggiula AR (1999) Sex differences in nicotine effects and self-administration: review of human and animal evidence. Nic Tobacco Res 1:301–315
Perkins KA, Gerlach D, Broge M, Grobe JE, Wilson A (2000) Greater sensitivity to subjective effects of nicotine in nonsmokers high in sensation seeking. Exper Clin Psychopharmacol 8:462–471
Perkins KA, Gerlach D, Broge M, Grobe JE, Sanders M, Fonte C, Vender J, Cherry C, Wilson A (2001a) Dissociation of nicotine tolerance from tobacco dependence in humans. J Pharmacol Exper Ther 296:849–856
Perkins KA, Gerlach D, Broge M, Fonte C, Wilson A (2001b) Reinforcing effects of nicotine as a function of smoking status. Exper Clin Psychopharmacol 9:243–250
Perkins KA, Broge M, Gerlach D, Sanders M, Grobe JE, Cherry C, Wilson AS (2002a) Acute nicotine reinforcement, but not chronic tolerance, predicts withdrawal and relapse after quitting smoking. Health Psychol 21:332–339
Perkins KA, Jacobs L, Sanders M, Caggiula AR (2002b) Sex differences in the subjective and reinforcing effects of cigarette nicotine dose. Psychopharmacology 163:194–201
Perkins KA, Jetton C, Stolinski A, Fonte C, Conklin CA (2003) The consistency of acute responses to nicotine in humans. Nic Tobacco Res 5:877–884
Pomerleau OF (1995) Individual differences in sensitivity to nicotine: implications for genetic research on nicotine dependence. Behav Genet 25:161–177
Pomerleau OF, Pomerleau CS, Rose JE (1989) Controlled dosing of nicotine: a review of problems and progress. Ann Behav Med 11:158–163
Pomerleau OF, Pomerleau CS, Namenek RJ (1998) Early experiences with tobacco among women smokers, ex-smokers, and never-smokers. Addiction 93:595–599
Pomerleau CS, Downey KK, Snedecor SM, Mehringer AM, Marks JL, Pomerleau OF (2003) Smoking patterns and abstinence effects in smokers with no ADHD, childhood ADHD, and adult ADHD symptomatology. Addict Behav 28:1149–1157
Pomerleau CS, Pomerleau OF, Snedecor SM, Gaulrapp S, Kardia SL (2004) Heterogeneity in phenotypes based on smoking status in the Great Lakes Smoker Sibling Registry. Addict Behav 29:1851–1855
Popke EJ, Mayorga AJ, Fogle CM, Paule MG (2000) Effects of acute nicotine on several operant behaviors in rats. Pharmacol Biochem Behav 65:247–254
Potter AS, Newhouse PA (2004) Effects of acute nicotine administration on behavioral inhibition in adolescents with attention-deficit/hyperactivity disorder. Psychopharmacology 176:182–194
Potter AS, Newhouse PA (2008) Acute nicotine improves cognitive deficits in young adults with attention-deficit/hyperactivity disorder. Pharmacol Biochem Behav 88:407–417
Ray R, Jepson C, Patterson F, Strasser AA, Rukstalis M, Perkins K, Lynch K, O’Malley S, Berrettini W, Lerman C (2006) Association of OPRM1 Asn40Asp variant with the relative reinforcing value of nicotine in female smokers. Psychopharmacology 188:355–363
Reynolds B, Patak M, Shroff P, Penfold RB, Melanko S, Duhig AM (2007) Laboratory and self-report assessments of impulsive behavior in adolescent daily smokers and nonsmokers. Exper Clin Psychopharmacol 15:264–271
Schechter MD, Meehan SM, Schechter JB (1995) Genetic selection for nicotine activity in mice correlates with conditioned place preference. Eur J Pharmacol 279:59–64
Schneider W, Shiffrin R (1977) Controlled and automatic human information processing: I. Detection, search, and attention. Psychol Rev 84:1–66
Schneider NG, Lunell E, Olmstead RE, Fagerstrom K-O (1996) Clinical pharmacokinetics of nasal nicotine delivery—a review and comparison to other nicotine systems. Clin Pharmacokin 31:65–80
Watson D, Clark LA, Tellegen A (1988) Development and validation of brief measures of positive and negative affect: the PANAS scales. J Personal Soc Psychol 54:1063–1070
Yoon JH, Higgins ST (2008) Turning k on its head: comments on use of an ED50 in delay discounting research. Drug Alc Depend 95:169–172
Zuckerman M (1994) Behavioral expressions and biosocial bases of sensation seeking. Cambridge Univ Press, Cambridge, UK
Zuckerman M, Kuhlman DM, Thornquist M, Kiers H (1991) Five (or three) robust questionnaire scale factors of personality without culture. Pers Individ Differ 12(9):929–941
Acknowledgments
This research was supported by NIH Grants DA05807 (KAP) and P50 CA/DA84718 (CL). The authors thank Roy Chengappa, Rick Blakesley–Ball, and Jason Keenan for their assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Perkins, K.A., Lerman, C., Coddington, S.B. et al. Initial nicotine sensitivity in humans as a function of impulsivity. Psychopharmacology 200, 529–544 (2008). https://doi.org/10.1007/s00213-008-1231-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-008-1231-7