Abstract
Rationale
The most simple and efficient method to study the physiological role of enkephalins is to increase the lifetime of these endogenous opioid peptides by inhibiting their inactivating enzymes. Enkephalins are degraded by the concomitant action of two metallopeptidases: neutral endopeptidase (NEP, EC3.4.21.11) and aminopeptidase N (APN, EC3.4.11.2), both enzymes releasing inactive metabolites.
Objectives
Potent dual inhibitors have been developed, such as RB101. However, NEP and APN have a broad specificity and can cleave various peptides in vitro. Therefore, it was essential to investigate the specific involvement of enkephalins in the various pharmacological responses induced by dual inhibitors.
Materials and methods
We compared the pharmacological responses induced by RB101 in wild-type and preproenkephalin-deficient mice (Penk1−/−) using several behavioural assays.
Results
In all the tests used (hot plate test, force swim test, castor-oil-induced diarrhoea), RB101 induced strong effects in wild-type animals, whereas slight effects were observed in Penk1−/− animals. These residual effects are blocked by pre-administration of the opioid antagonist naloxone, supporting the involvement of the opioid receptors in the responses observed.
Conclusions
The pharmacological effects induced by dual inhibitors acting on both NEP and APN are mainly due to the protection of the endogenous enkephalins at supraspinal and peripheral levels. It could be speculated that the residual effects observed in Penk1−/− mice after RB101 administration could be due to the direct action of other opioid peptides or through an indirect effect involving the protection of other peptide substrates of NEP or APN, as substance P or angiotensin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the discovery of the opioid receptors in the 1970s, several decades preceding their molecular cloning (reviewed by Dhawan et al. 1996), the pharmacology of the opioid system has been widely explored using more or less selective exogenous ligands (review in Bodnar and Klein 2006). Nevertheless, this approach does not provide any direct information about the physiological roles of the endogenous opioid peptides.
The endogenous opioid systems are constituted by four distinct neuronal systems that are widely distributed throughout the CNS and peripheral organs. The four precursors are proopiomelanocortin, proenkephalin, prodynorphin and pronociceptin/orphanin FQ, each generating biologically active peptides that are released at the synaptic terminals of opioidergic neurons. These peptides exert their physiological actions by interacting with the various classes of opioid receptors present on both pre- and post-synaptic membranes of opioid and opioid target neurons. The pentapeptide enkephalins [Tyr–Gly–Gly–Phe–Met(Leu); Hughes et al. 1975] seem to play a major role in pain perception, cognitive functions, affective behaviours, and locomotion (Diaz and Asai 1990; Konig et al. 1996; Roques 2000). These peptides interact with a higher affinity than morphine with both the mu and delta receptors [Ki values of morphine for mu and delta receptors are 14 nM and >1,000 nM, respectively; Ki values of Leu-enkephalin are 3.4 and 4 nM, respectively; Ki values of Met-enkephalin are 0.7 and 1.7 nM, respectively (reviewed by Raynor et al. 1994)]. Moreover, it has been shown that the mu receptor is critically involved in the control of nociception (Matthes et al. 1996), whereas the delta seems to be implicated in emotional control (Calenco-Choukroun et al. 1991; Filliol et al. 2000). However, in absence of external stimuli, the tonic release of enkephalins appears too weak to produce clear pharmacological responses as shown by the lack or very weak effects observed after administration of the opioid antagonist naloxone (Akil et al. 1976; Jacob and Ramabadran 1977). This problem could be overcome either by a stress- or nociception-induced increase in secretion of enkephalins leading to significant pharmacological responses (Akil et al. 1984; Bourgoin et al. 1990). Such enhanced levels of circulating enkephalins can also be obtained by graft of cells producing enkephalins (Sagen et al. 1993) or by viral-driven enkephalin overproduction (Braz et al. 2001).
Nevertheless, the most simple and efficient method to study the physiological role of the enkephalins is to increase the lifetime of these endogenous opioid peptides by inhibiting their inactivating enzymes. This approach is similar to those used successfully with the angiotensin-converting enzymes or MAO inhibitors (Fournie-Zaluski et al. 2004; Ondetti et al. 1977; Yamada and Yasuhara 2004). Enkephalins are degraded by the concomitant action of two membrane-bound zinc metallopeptidases: the neutral endopeptidase (neprilysin or NEP, EC3.4.21.11) and the aminopeptidase N (APN, EC3.4.11.2), both enzymes releasing inactive metabolites (reviewed by Roques et al. 1993). This well-admitted interruption by the two peptidases of the messages conveyed by enkephalins is in good agreement with the demonstration of a co-localisation of NEP and APN in brain areas where opioid peptides and receptors are present (Mansour and Watson 1993; Noble et al. 2001; Waksman et al. 1986). Therefore, to investigate the pharmacological functions of the endogenous enkephalins, potent dual inhibitors have been developed (Fournié-Zaluski et al. 1984; Roques et al. 1993). Among these inhibitors with nanomolar affinities both for NEP and for APN, RB101 was found to be systemically active (Fournié-Zaluski et al. 1992) leading to a large increase in extra-cellular levels of Met-enkephalin (Dauge et al. 1996; Le Guen et al. 2003). However, NEP and APN have a broad specificity and can cleave various peptides in vitro (Turner et al. 1987). Using selective or dual inhibitors substance P was demonstrated to behave as NEP substrate in rat striatum (Mauborgne et al. 1987), and regulatory peptides such as atrial natriuretic peptide, endothelin and bradykinin were cleaved in vivo by NEP (Roques et al. 1993).Therefore, it was essential to investigate the specific involvement of enkephalins in the various pharmacological responses induced by dual inhibitors. With this aim, we compared the pharmacological responses induced by RB101 in wild-type and preproenkephalin-deficient mice (Penk1−/−) using several behavioural assays (hot plate test, force swim test, castor-oil induced diarrhoea).
Materials and methods
Animals
To obtain Penk1 mutant mice on DBA/2J inbred congenic genetic background, we mated heterozygous (Penk+/−) mice from a mixed (129 and C57BL/6J) genetic background (Konig et al. 1996) to wild-type DBA/2J mice (Charles River Laboratories) for ten generations. The Penk+/− mice from the F10 generation were then intercrossed to obtain homozygous animals. The mice for behavioural studies were derived from these homozygous animals. The male Penk1−/− and Penk1+/+ mice (3–4 months old on a DBA/2J genetic background) were kept under standard animal housing conditions in a 12-h light–dark cycle (8:00 a.m.–8:00 p.m.) and maintained in a temperature controlled room (21 ± 1°C). Food and water were available ad libitum. Behavioural tests and care of the animals were in accordance with guidelines of the European Communities directive 86/609/EEC, and under control of the local ethical committee.
Chemicals
RB101 (N-[(R,S)-2-benzyl-3[(S)(2-amino-4-methylthio)butyldithio]-1-oxopropyl]-l-phenylalanine benzyl ester) was synthesised in the laboratory (Fournié-Zaluski et al. 1992). It was dissolved in a vehicle containing ethanol (10%), cremophor EL (10%), and distilled water (80%). The highest dose of RB 101 that can be used by i.v. route was 80 mg/kg, due to the low solubility of this compound. Cremophor was purchased from Sigma (Saint-Quentin Fallavier, France). Naloxone was purchased from Sigma (Saint-Quentin Fallavier, France) and dissolved in saline (0.9% sodium chloride in water). Morphine HCl, purchased from Francopia (Gentilly, France), was dissolved in saline. Castor oil was purchased from Sigma (Saint-Quentin Fallavier, France).
RB101, morphine and control vehicle were intravenously administered (i.v.) 10 min before the behavioural tests. Naloxone and naltrindole were subcutaneously administered (s.c.) 20 min before the test. Volumes of injection were 0.1 ml per 10 g of body weight.
Hot-plate test
The test was based on that described by Eddy and Leimbach (Eddy and Leimbach 1953). A glass cylinder (16-cm high, 16-cm diameter) was used to keep the mouse on the heated surface of the plate, which was kept at a temperature of 52 ± 0.5°C using a thermoregulated water-circulating pump. The latency period until the mouse jumped was registered by means of a stopwatch (cut-off time = 240 s). The results were expressed as means of jump latency ± SEM, or as a percent of analgesia using the following equation: \( \% \,{\text{analgesia}} = {{\left( {{\text{test}}\,{\text{latency}} - {\text{control}}\,{\text{latency}}} \right)}} \mathord{\left/ {\vphantom {{{\left( {{\text{test}}\,{\text{latency}} - {\text{control}}\,{\text{latency}}} \right)}} {{\left( {{\text{cut - off}}\,{\text{time}} - {\text{control}}\,{\text{latency}}} \right)} \times 100}}} \right. \kern-\nulldelimiterspace} {{\left( {{\text{cut - off}}\,{\text{time}} - {\text{control}}\,{\text{latency}}} \right)} \times 100} \).
Forced swim test
The test was based on that described by Porsolt et al. (Porsolt et al. 1977). This test possesses good predictive validity with respect to anti-depressant activity. The mice were placed in a narrow cylinder (10 × 15 cm) from which they cannot escape. We placed each mouse in the cylinder containing water to a depth of 9 cm at 21–23°C, so that the tail of the mouse could not reach the bottom of the apparatus. After a brief period of vigorous activity, the mice adopted a characteristic immobile posture. After the first 2 min, the total duration of immobility was measured during a 4-min test. The mice were judged to be immobile when they remained floating passively in the water (the very small movements necessary to keep their head above water were not taken into account). The results were expressed as means of duration of immobility ± SEM.
Anti-diarrhoeal activity
The anti-diarrhoeal effect of RB101 was studied as described by Goldenberg et al. 1975. Diarrhoea was induced in mice by oral administration of castor oil. Briefly, mice were treated i.v. with RB101 or vehicle. After 15 min, 0.2 ml/mouse of castor oil were administered by gavage, and animals were immediately put into individual cages, placed over white and clean filter paper. Ninety minutes later, the cages were inspected one by one for the presence of the characteristic diarrhoeal droppings.
Statistical analysis
Two-way (genotype, treatment) or one-way (treatment) analysis of variance (ANOVA) were conducted using computer software (Statview) for comparison across the experimental conditions. When a significant difference among the treatments was obtained in the ANOVA, the Newman-Keuls’ post hoc test was applied to define which group contributed to these differences. Significance was accepted with P < 0.05.
Results
Effects induced by morphine and RB101 in the hot plate test
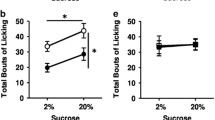
In the hot-plate test, the two-way ANOVA indicated a significant treatment effect (F 2,36 = 327.11, p < 0.0001), genotype effect (F 1,36 = 401.7, p < 0.0001) and interaction between treatment and genotype (F 2,36 = 223.6, p < 0.0001). As shown in Fig. 1a, the jump latency after i.v. administration of vehicle was reduced in proenkephalin knockout mice as compared to wild-type littermates (p < 0.01). Administration of RB101 (20 mg/kg, i.v.) induced after 10 min a strong anti-nociceptive response in the hot plate test in wild-type animals (p < 0.01), whereas only a slight effect (p < 0.05) was observed in proenkephalin KO mice. This effect was of the same magnitude at 20 mg/kg and at the highest dose of RB 101 (80 mg/kg) that can be used. The increase in jump latencies induced by RB101 in both genotypes were abolished by administration of the opioid antagonist naloxone (0.1 mg/kg, s.c., 20 min before the test; Fig. 1b), supporting the involvement of the opioid receptors in the anti-nociceptive response.
a Antinociceptive effects of RB 101 in wild type and Penk1−/− mice in the hot plate test. Jump latencies were measured at 10 min after i.v. administration of RB101 (20 mg/kg). Data are expressed as mean ± SEM of latencies (n = 9–12 mice per group). b Effects of naloxone (0.1 mg/kg, s.c. 20 min before testing) on the anticociceptive responses induced by RB101 (20 mg/kg, i.v., 10 min before the test) in wild type and Penk1−/− mice in the hot plate test. Data are expressed as mean ± SEM of latencies (n = 5–7 mice per group). Double asterisk, P < 0.01 as compared to wild type control group; number sign, P < 0.05 and double number sign, P < 0.01 as compared to the group indicated (Newman-Keul’s test)
As shown in Fig. 2, morphine produced a significant dose-dependent anti-nociceptive response 10 min after i.v. administration. The two-way ANOVA indicated a significant treatment effect (F 3,60 = 52.4, p < 0.0001), but no genotype effect (F 1,60 = 0.702, p = 0.406) and no interaction between treatment and genotype (F 3,60 = 0.948, p = 0.423). This result shows that the effects of morphine are of the same magnitude in both wild-type and proenkephalin KO mice. No difference between the dose-response curves obtained in wild-type animal and in proenkephalin knockout mice was observed (Fig. 2). The anti-nociceptive responses induced by morphine in wild-type and KO mice were blocked by the opioid antagonist naloxone (0.1 mg/kg s.c., 20 min before the test), but not by the delta selective antagonist naltrindole (2 mg/kg, s.c. 20 min before the test; Fig. 3).
Antinociceptive effects of morphine in wild type and Penk1−/− mice in the hot plate test. Jump latencies were measured at 10 min after i.v. administration of morphine. a Data are expressed as mean ± SEM of latencies (n = 9–12 mice per group). b Data are expressed as mean ± SEM of percentage of analgesia (n = 9–12 mice per group)
Effects of naloxone (0.1 mg/kg, s.c. 20 min before testing) or naltrindole (2 mg/kg, s.c. 20 min before testing) on the anticociceptive responses induced by morphine (20 mg/kg, i.v., 10 min before the test) in wild type and Penk1−/− mice in the hot plate test. Data are expressed as mean ± SEM of latencies (n = 5–7 mice per group). Double asterisk, P < 0.01 as compared to control group; double number sign P < 0.01 as compared to morphine alone (Newman Keul’s test)
Antidepressant-like effects induced by RB101 in the forced swim test
The two-way ANOVA indicated a significant treatment effect (F 3,42 = 79.2, p < 0.0001), genotype effect (F 1,42 = 72.47, p < 0.0001) and interaction between treatment and genotype (F 3,42 = 19.52, p < 0.0001). As shown in Fig. 4, RB101 (5 and 10 mg/kg i.v.), 10 min after its administration, shortened the observed immobility time of wild-type mice, whereas a small but significant effect was observed at 10, 20 and 80 mg/kg (i.v.) of RB101 in proenkephalin knockout mice. The opioid receptor antagonist naloxone (0.1 mg/kg s.c. 20 min before the test), without effect by itself, inhibited the shortening of immobility time induced by RB101 alone (10 mg/kg i.v, 10 min before the test) in both genotypes (data not shown).
Effects of RB101 (i.v. 10 min before the test) in the mouse forced swim test in wild type and Penk1−/− animals. Results represent the mean ± SEM of immobility time (n = 9–12 mice per group). Asterisk, P < 0.05 and double asterisk, P < 0.01 as compared to the control group of the same genotype (Newman-Keul’s test)
Effects of RB101 on castor-oil-induced diarrhoea in mice
Both NEP (Pollard et al. 1991) and APN (Noble et al. 2001) are present in the gastrointestinal tract, and proenkephalin, proopiomelanocortin and prodynorphin are synthesised and processed locally in gut tissues. Opioid target receptors are found in the nervous plexi innervating gastrointestinal wall with an enrichment in delta opioid receptors in the distal part of intestine. The two-way ANOVA indicated a significant treatment effect (F 1,30 = 47.211, p < 0.0001), genotype effect (F 1,30 = 13.614, p = 0.0009) and interaction between treatment and genotype (F 1,30 = 6.478, p = 0.0163). As shown in Fig. 5, the castor-oil-induced diarrhoea was reduced by RB101 (20 mg/kg i.v.) in both genotypes. However, the effect was stronger in wild-type mice as compared to proenkephalin knockout littermates (p < 0.01).
Effects of RB101 (20 mg/kg i.v.) on castor-oil-induced diarrhea in wild type and Penk1−/− mice. Data are expressed as mean ± SEM of percentage of hard faeces compared to total faeces (n = 9–12 mice per group). Asterisk, P < 0.05 and double asterisk, P < 0.01 as compared to the control group of the same genotype (Newman Keul’s test)
Discussion
The aim of this study was to investigate, by using preproenkephalin knockout mice, the specific implication of endogenous enkephalins in the pharmacological effects induced by the potent inhibitor of the two metabolising enzymes of these peptide effectors. In addition, the results of this study are expected to give direct information of the physiological role of the enkephalins in the behaviours tested.
Synthetic inhibitors of enkephalin-degrading enzymes have been shown in several experiments to induce strong, dose-dependent anti-nociceptive responses in different animal models of pain in rodents (al-Rodhan et al. 1990; Noble et al. 1997, 1992; Roques 2000; Roques et al. 1980). Similarly, opiorphin, a short peptide discovered in human brain tissue was reported to elicit moderate anti-nociceptive properties through inhibition of NEP and APN (Wisner et al. 2006). Consistent with the involvement of enkephalins in the anti-nociceptive actions of dual inhibitors, the strength and time course of the responses in a centrally controlled thermal nociceptive stimulus, was found correlated with the increased levels of these peptides in the periaqueductal grey matter (Le Guen et al. 2003). In control animals, the results observed in absence of RB101 (Fig. 1a) confirmed the important role played by endogenous enkephalin in pain perception, after an intense thermal nociceptive stimulus, recruiting supraspinal pathways. The jump latency was slightly decreased in Penk1−/− mice as compared to wild-type littermates, in agreement with previous studies (Bilkei-Gorzo et al. 2004; Konig et al. 1996). This could not be due to changes in basal locomotor behaviour in the knockout mice, as no differences were observed between Penk1−/− mice and wild-type control animals (Bilkei-Gorzo et al. 2007). This hyperalgesia is very likely related to a direct consequence of the lack of enkephalins, but could also be due to an induced change in respective levels of different endogenous peptides. This has been suggested by the results obtained by Fischer et al. (2002), showing that the slight hyperalgesia observed in NEP knockout mice results from an imbalance between bradykinin-opioid systems, in which the expected analgesic effects of enkephalins are masked by hyperalgesic effects of bradykinin.
RB101 at the dose of 20 mg/kg i.v. induced a strong anti-nociceptive response in the hot plate test in wild-type animals, and this effect was found to be severely decreased in Penk1−/− mice. However, a slight residual effect was observed in knockout animals that disappeared by pre-administration of the opioid antagonist, naloxone. It is noteworthy to observe that the anti-nociceptive dose-response curves, obtained with morphine in the hot plate test, were similar in wild-type and knockout mice (Fig. 2), and were antagonised by naloxone in both genotypes, but not by the delta selective antagonist, naltrindole (Fig. 3). This suggests a lack of compensatory changes at the level of mu opioid receptors during preproenkephalin knockout mice development in brain regions involved in the control of pain, despite the often reported receptor up-regulation when its cognate ligand is genetically ablated (Cammalleri et al. 2006; Clarke et al. 2003a). This is consistent with the lack of modification reported in these regions in Penk1−/− mice (Brady et al. 1999; Clarke et al. 2003b).
Several hypotheses could be proposed to explain the slight residual analgesic effects of RB101 in Penk1−/− mice. Previous studies have demonstrated a predominant involvement of mu opioid receptors in endogenous opioid-induced analgesia, at least with respect to thermal nociceptive stimuli (Dauge et al. 1987; Fang et al. 1986; Gacel et al. 1981; Matthes et al. 1996; Noble et al. 1992). It has been shown that, probably for conformational reasons, other opioid peptides, such as β-endorphin and/or endomorphins, which have a great affinity for mu receptors, appear to be resistant to NEP, but to a lesser extent to APN (Champion et al. 1997; Turner et al. 1987). Thus, the inhibition of aminopeptidases were shown to protect efficiently the endomorphins from their degradation (Tomboly et al. 2002). Thus, it could be speculated that the weak anti-nociceptive effect obtained after i.v. administration of RB101 in Penk1−/− mice could be due to the direct action of β-endorphin and/or endomorphin at the mu receptors level. Another hypothesis could involve a reduction in the increased substance P (SP) release evoked by the noxious stimulus. Indeed, it was shown that in the periaqueductal grey, opioid agonists can suppress transmission of nociceptive information by inhibiting SP release (Xin et al. 1997).
Bradykinin could also be involved in the response observed. Thus, while hyperalgesia may be observed through peripheral actions, central administration of bradykinin induces analgesia. In the presence of RB 101, the slight residual anti-nociceptive response could be also due to central protection of bradykinin. However, this latter hypothesis seems unlikely, as this effect was reversed by the opioid antagonist naloxone, used at a low dose (0.1 mg/kg), unable to block anti-nociceptive response induced by i.c.v. administration of bradykinin in the hot plate test (Germany et al. 1996).
We then compared the effects induced by RB101 in emotion-related responses of wild-type and Penk1−/− mice in the forced swim test. The dual inhibitors of enkephalin catabolism have been previously reported to elicit antidepressant-like effects in several animal models (Baamonde et al. 1992; Jutkiewicz et al. 2006; Nieto et al. 2005; Tejedor-Real et al. 1998). As expected, in the forced swim test, RB101 induced a highly significant decrease in the immobility time in wild-type mice, whereas a slight and plateauing reduction in immobility time was observed for the highest doses of the dual inhibitor in Penk1−/− animals (Fig. 4). These antidepressant-like effects were related to the stimulation of opioid receptors as they were antagonised by naloxone in both genotypes. Interestingly, it could be noticed in Penk1−/− mice that the residual effect induced by RB101 in the forced swim test is more marked than in the hot plate test (Fig. 4). One possible explanation could originate from the reported specific up-regulation of delta receptors in limbic structures of Penk1−/− mice (Clarke et al. 2003b). This hypothesis is in agreement with previous studies, showing clearly that the antidepressant-like effects observed after RB101 administration were related to stimulation of delta opioid receptors by the endogenous enkephalins protected from their enzymatic degradation (Baamonde et al. 1992; Jutkiewicz et al. 2006; Nieto et al. 2005). Moreover, in a recent study, we have already demonstrated that the residual antidepressant-like effect of RB 101 in Penk1−/− mice was blocked by the delta opioid selective antagonist, naltrindole (Bilkei-Gorzo et al. 2007). Therefore, the activation of over-expressed delta receptor by β-endorphin could produce the rather unexpected decrease in time of immobility in Penk1−/− mice at 10 mg/kg of RB101. However, this hypothesis must be taken with caution, as in rats it has been shown that β-endorphin induced depressant-like effects, mainly through activation of mu receptors (Zhang et al. 2006). β-Endorphin has the same affinity for mu and delta receptors (1 nM; Raynor et al. 1994). The over-expression of delta receptors in Penk1−/− mice could facilitate action of β-endorphin with antidepressant-like effects.
Enkephalins can also be produced from dynorphin precursors (Brownstein 1980; Sei et al. 1989). Thus, we could consider the possibility that enkephalin is still present in the absence of Penk. However, in a recent study, we have shown that RB101 still had an antidepressant-like effect in Penk/Pdyn double KO mice (Bilkei-Gorzo et al. 2007), suggesting that the effects of RB 101 cannot be exclusively dependent on the elevation of enkephalin levels.
Moreover, one cannot exclude that in absence of enkephalins, the two enzymes NEP and APN inactivate another peptide directly or indirectly involved in antidepressant-like responses. This could be the case of SP, demonstrated to be cleaved by NEP in striatum (Michael-Titus et al. 2002), although this hypothesis is unlikely since SP is anxiogenic. Moreover, antagonists of SP, such as SR140333, are unable to reverse the antidepressant-like effects of RB101 in this study (not shown), consistent with the reported lack of antidepressant effects of SP antagonists in animals and humans (Keller et al. 2006; Ranga and Krishnan 2002). Another hypothesis could be related to the brain renin-angiotensin system, where it has been shown that Ang III acts as ligand of angiotensin receptors, as pretreatment with the angiotensin receptor antagonist losartan provided protection from immobility in the forced swim test (Gard 2002). Indeed, it has been demonstrated that the active angiotensin fragment Ang III is protected from degradation by APN inhibitor (Zini et al. 1996).
Morphine is well known to produce constipation that is one of its most severe drawbacks. This was related to the stimulation of mu opioid receptors regulating negatively the intestinal peristaltism and was clinically exploited in anti-diarrhoeal agents as the mu agonist loperamide. A possible tonic participation of endogenous enkephalins at different levels of the gastrointestinal tract has been demonstrated by the naloxone-antagonised anti-diarrhoeal effects in different animal models and humans elicited by the NEP inhibitor thiorphan (Roge et al. 1993; Roques et al. 1980; Wang et al. 2005). The results obtained in the model of castor-oil-induced diarrhoea in mice, clearly showed a strong anti-diarrhoeal effect of RB101 in wild-type animals, whereas only a slight effect was observed in Penk1−/− mice, consistent with an in vivo role of endogenous enkephalins in the control of feces progression.
In conclusion, this study indicates that the pharmacological effects induced by dual inhibitors acting on both NEP and APN are mainly due to the protection of the endogenous enkephalins at supraspinal and peripheral levels. Numerous previous studies already suggested that despite a relatively broad specificity, a certain in vivo specificity of a given peptidase seems to be achieved, governed by both its distribution and that of its potential substrates and target receptors. However, the present study provides perhaps the most clear and direct demonstration of the in vivo selectivity of the dual NEP/APN inhibitors, even if we cannot exclude a minor role of both peptidases in the degradation of other peptides. Nevertheless, these putative substrates appear to play a minor role in the various responses elicited by endogenous activation of opioid receptors supporting the use of the dual inhibitors as useful mean to investigate the functions of the native opioid peptides in vivo.
References
Akil H, Mayer DJ, Liebeskind JC (1976) Antagonism of stimulation-produced analgesia by naloxone, a narcotic antagonist. Science 191:961–962
Akil H, Watson SJ, Young E, Lewis ME, Khachaturian H, Walker JM (1984) Endogenous opioids: biology and function. Annu Rev Neurosci 7:223–255
al-Rodhan N, Chipkin R, Yaksh TL (1990) The antinociceptive effects of SCH-32615, a neutral endopeptidase (enkephalinase) inhibitor, microinjected into the periaqueductal, ventral medulla and amygdala. Brain Res 520:123–130
Baamonde A, Daugé V, Ruiz-Gayo M, Fulga IG, Turcaud S, Fournié-Zaluski MC, Roques BP (1992) Antidepressant-type effects of endogenous enkephalins protected by systemic RB 101 are mediated by opioid d and dopamine D1 receptor stimulation. Eur J Pharmacol 216:157–166
Bilkei-Gorzo A, Racz I, Michel K, Zimmer A, Klingmuller D (2004) Behavioral phenotype of pre-proenkephalin-deficient mice on diverse congenic backgrounds. Psychopharmacology (Berl) 176:343–352
Bilkei-Gorzo A, Michel K, Noble F, Roques BP, Zimmer A (2007) Preproenkephalin knockout mice show no depression-related phenotype. Neuropsychopharmacology (in press)
Bodnar RJ, Klein GE (2006) Endogenous opiates and behavior: 2005. Peptides 27:3391–3478
Bourgoin S, Le Bars D, Clot AM, Hamon M, Cesselin F (1990) Subcutaneous formalin induces a segmental release of Met-enkephalin-like material from the rat spinal cord. Pain 41:323–329
Brady LS, Herkenham M, Rothman RB, Partilla JS, Konig M, Zimmer AM, Zimmer A (1999) Region-specific up-regulation of opioid receptor binding in enkephalin knockout mice. Brain Res Mol Brain Res 68:193–197
Braz J, Beaufour C, Coutaux A, Epstein AL, Cesselin F, Hamon M, Pohl M (2001) Therapeutic efficacy in experimental polyarthritis of viral-driven enkephalin overproduction in sensory neurons. J Neurosci 21:7881–7888
Brownstein MJ (1980) Opioid peptides: search for the precursors. Nature 287:678–679
Calenco-Choukroun G, Dauge V, Gacel G, Feger J, Roques BP (1991) Opioid delta agonists and endogenous enkephalins induce different emotional reactivity than mu agonists after injection in the rat ventral tegmental area. Psychopharmacology (Berl) 103:493–502
Cammalleri M, Cervia D, Dal Monte M, Martini D, Langenegger D, Fehlmann D, Feuerbach D, Pavan B, Hoyer D, Bagnoli P (2006) Compensatory changes in the hippocampus of somatostatin knockout mice: upregulation of somatostatin receptor 2 and its function in the control of bursting activity and synaptic transmission. Eur J Neurosci 23:2404–2422
Champion HC, Zadina JE, Kastin AJ, Hackler L, Ge LJ, Kadowitz PJ (1997) Endomorphin 1 and 2, endogenous ligands for the mu-opioid receptor, decrease cardiac output, and total peripheral resistance in the rat. Peptides 18:1393–1397
Clarke S, Chen Z, Hsu MS, Hill RG, Pintar JE, Kitchen I (2003a) Nociceptin/orphanin FQ knockout mice display up-regulation of the opioid receptor-like 1 receptor and alterations in opioid receptor expression in the brain. Neuroscience 117:157–168
Clarke S, Zimmer A, Zimmer AM, Hill RG, Kitchen I (2003b) Region selective up-regulation of micro-, delta- and kappa-opioid receptors but not opioid receptor-like 1 receptors in the brains of enkephalin and dynorphin knockout mice. Neuroscience 122:479–489
Dauge V, Petit F, Rossignol P, Roques BP (1987) Use of mu and delta opioid peptides of various selectivity gives further evidence of specific involvement of mu opioid receptors in supraspinal analgesia (tail-flick test). Eur J Pharmacol 141:171–178
Dauge V, Mauborgne A, Cesselin F, Fournie-Zaluski MC, Roques BP (1996) The dual peptidase inhibitor RB101 induces a long-lasting increase in the extracellular level of Met-enkephalin-like material in the nucleus accumbens of freely moving rats. J Neurochem 67:1301–1308
Dhawan BN, Cesselin F, Raghubir R, Reisine T, Bradley PB, Portoghese PS, Hamon M (1996) International Union of Pharmacology. XII. Classification of opioid receptors. Pharmacol Rev 48:567–592
Diaz JL, Asai M (1990) Dominant mice show much lower concentrations of methionine–enkephalin in brain tissue than subordinates: cause or effect? Behav Brain Res 39:275–280
Eddy NB, Leimbach D (1953) Synthetic analgesics. II. Dithienylbutenyl- and dithienylbutylamines. J Pharmacol Exp Ther 107:385–393
Fang FG, Fields HL, Lee NM (1986) Action at the mu receptor is sufficient to explain the supraspinal analgesic effect of opiates. J Pharmacol Exp Ther 238:1039–1044
Filliol D, Ghozland S, Chluba J, Martin M, Matthes HW, Simonin F, Befort K, Gaveriaux-Ruff C, Dierich A, LeMeur M, Valverde O, Maldonado R, Kieffer BL (2000) Mice deficient for delta- and mu-opioid receptors exhibit opposing alterations of emotional responses. Nat Genet 25:195–200
Fischer HS, Zernig G, Hauser KF, Gerard C, Hersh LB, Saria A (2002) Neutral endopeptidase knockout induces hyperalgesia in a model of visceral pain, an effect related to bradykinin and nitric oxide. J Mol Neurosci 18:129–134
Fournié-Zaluski MC, Chaillet P, Bouboutou R, Coulaud A, Chérot P, Waksman G, Costentin J, Roques BP (1984) Analgesic effects of kelatorphan, a new highly potent inhibitor of multiple enkephalin degrading enzymes. Eur J Pharmacol 102:525–528
Fournié-Zaluski MC, Coric P, Turcaud S, Lucas E, Noble F, Maldonado R, Roques BP (1992) Mixed-inhibitor-prodrug as a new approach towards systemically active inhibitors of enkephalin degrading enzymes. J Med Chem 35:2474–2481
Fournie-Zaluski MC, Fassot C, Valentin B, Djordjijevic D, Reaux-Le Goazigo A, Corvol P, Roques BP, Llorens-Cortes C (2004) Brain renin-angiotensin system blockade by systemically active aminopeptidase A inhibitors: a potential treatment of salt-dependent hypertension. Proc Natl Acad Sci USA 101:7775–7780
Gacel G, Fournie-Zaluski MC, Fellion E, Roques BP (1981) Evidence of the preferential involvement of mu receptors in analgesia using enkephalins highly selective for peripheral mu or delta receptors. J Med Chem 24:1119–1124
Gard PR (2002) The role of angiotensin II in cognition and behaviour. Eur J Pharmacol 438:1–14
Germany A, Gonzalez P, Contreras E (1996) Possible role of nitric oxide in the antinociceptive action of intraventricular bradykinin in mice. Eur J Pharmacol 310:123–127
Goldenberg MM, Honkomp LJ, Castellion AW (1975) The antidiarrheal action of bismuth subsalicylate in the mouse and the rat. Am J Dig Dis 20:955–960
Hughes J, Smith TW, Kosterlitz HW, Fothergill LA, Morgan BA, Morris HR (1975) Identification of two related pentapeptides from the brain with potent opiate agonist activity. Nature 258:577–580
Jacob JJ, Ramabadran K (1977) Opioid antagonists, endogenous ligands and nociception. Eur J Pharmacol 46:393–394
Jutkiewicz EM, Torregrossa MM, Sobczyk-Kojiro K, Mosberg HI, Folk JE, Rice KC, Watson SJ, Woods JH (2006) Behavioral and neurobiological effects of the enkephalinase inhibitor RB101 relative to its antidepressant effects. Eur J Pharmacol 531:151–159
Keller M, Montgomery S, Ball W, Morrison M, Snavely D, Liu G, Hargreaves R, Hietala J, Lines C, Beebe K, Reines S (2006) Lack of efficacy of the substance p (neurokinin1 receptor) antagonist aprepitant in the treatment of major depressive disorder. Biol Psychiatry 59:216–223
Konig M, Zimmer AM, Steiner H, Holmes PV, Crawley JN, Brownstein MJ, Zimmer A (1996) Pain responses, anxiety and aggression in mice deficient in pre-proenkephalin. Nature 383:535–538
Le Guen S, Mas Nieto M, Canestrelli C, Chen H, Fournie-Zaluski MC, Cupo A, Maldonado R, Roques BP, Noble F (2003) Pain management by a new series of dual inhibitors of enkephalin degrading enzymes: long lasting antinociceptive properties and potentiation by CCK2 antagonist or methadone. Pain 104:139–148
Mansour A, Watson SJ (1993) Anatomical distribution of opioid receptors in mammalians : an overview. In: Herz A, Akil H, Simon AJ (eds) Handbook of experimental pharmacology. Opioids I. Springer, Berlin, pp 79–105
Matthes HW, Maldonado R, Simonin F, Valverde O, Slowe S, Kitchen I, Befort K, Dierich A, Le Meur M, Dolle P, Tzavara E, Hanoune J, Roques BP, Kieffer BL (1996) Loss of morphine-induced analgesia, reward effect and withdrawal symptoms in mice lacking the mu-opioid-receptor gene. Nature 383:819–823
Mauborgne A, Bourgoin S, Benoliel JJ, Hirsch M, Berthier JL, Hamon M, Cesselin F (1987) Enkephalinase is involved in the degradation of endogenous substance P released from slices of rat substantia nigra. J Pharmacol Exp Ther 243:674–680
Michael-Titus AT, Fernandes K, Setty H, Whelpton R (2002) In vivo metabolism and clearance of substance P and co-expressed tachykinins in rat striatum. Neuroscience 110:277–286
Nieto MM, Guen SL, Kieffer BL, Roques BP, Noble F (2005) Physiological control of emotion-related behaviors by endogenous enkephalins involves essentially the delta opioid receptors. Neuroscience 135:305–313
Noble F, Soleilhac JM, Soroca-Lucas E, Turcaud S, Fournié-Zaluski MC, Roques BP (1992) Inhibition of the enkephalin-metabolizing enzymes by the first systemically active mixed inhibitor prodrug RB 101 induces potent analgesic responses in mice and rats. J Pharmacol Exp Ther 261:181–190
Noble F, Smadja C, Valverde O, Maldonado R, Coric C, Turcaud S, Fournié-Zaluski MC, Roques BP (1997) Pain-suppressive effects on various nociceptive stimuli (thermal, chemical, electrical and inflammatory) of the first orally active enkephalin-metabolizing enzyme inhibitor RB 120. Pain 73:383–391
Noble F, Banisadr G, Jardinaud F, Popovici T, Lai-Kuen R, Chen H, Bischoff L, Melik Parsadaniantz S, Fournié-Zaluski MC, Roques BP (2001) First discrete autoradiographic distribution of aminopeptidase N in various structures of rat brain and spinal cord using the selective iodinated inhibitor [125I]RB 129. Neuroscience 105:479–488
Ondetti MA, Rubin B, Cushman DW (1977) Design of specific inhibitors of angiotensin-converting enzyme: new class of orally active antihypertensive agents. Science 196:441–444
Pollard H, Moreau J, Ronco P, Verroust P, Schwartz JC (1991) Immunoautoradiographic localisation of enkephalinase (EC 3.4.24.11) in rat gastrointestinal tract. Neuropeptides 19:169–178
Porsolt RD, Le Pichon M, Jalfre M (1977) Depression: a new animal model sensitive to antidepressant treatments. Nature 266:730–732
Ranga K, Krishnan R (2002) Clinical experience with substance P receptor (NK1) antagonists in depression. J Clin Psychiatry 63(Suppl 11):25–29
Raynor K, Kong H, Chen Y, Yasuda K, Yu L, Bell GI, Reisine T (1994) Pharmacological characterization of the cloned kappa-, delta-, and mu-opioid receptors. Mol Pharmacol 45:330–334
Roge J, Baumer P, Berard H, Schwartz JC, Lecomte JM (1993) The enkephalinase inhibitor, acetorphan, in acute diarrhoea. A double-blind, controlled clinical trial versus loperamide. Scand J Gastroenterol 28:352–354
Roques BP (2000) Novel approaches to targeting neuropeptide systems. Trends Pharmacol Sci 21:475–483
Roques BP, Fournie-Zaluski MC, Soroca E, Lecomte JM, Malfroy B, Llorens C, Schwartz JC (1980) The enkephalinase inhibitor thiorphan shows antinociceptive activity in mice. Nature 288:286–288
Roques BP, Noble F, Daugé V, Fournié-Zaluski MC, Beaumont A (1993) Neutral endopeptidase 24.11 : structure, inhibition, and experimental and clinical pharmacology. Pharmacol Rev 45:87–146
Sagen J, Wang H, Tresco PA, Aebischer P (1993) Transplants of immunologically isolated xenogeneic chromaffin cells provide a long-term source of pain-reducing neuroactive substances. J Neurosci 13:2415–2423
Sei CA, Richard R, Dores RM (1989) Steady-state levels of pro-dynorphin-related end-products from the brain of the amphibian, Xenopus laevis. Brain Res 479:162–166
Tejedor-Real P, Mico JA, Smadja C, Maldonado R, Roques BP, Gilbert-Rahola J (1998) Involvement of delta-opioid receptors in the effects induced by endogenous enkephalins on learned helplessness model. Eur J Pharmacol 354:1–7
Tomboly C, Peter A, Toth G (2002) In vitro quantitative study of the degradation of endomorphins. Peptides 23:1573–1580
Turner AJ, Hooper NM, Kenny AJ (1987) Metabolism of neuropeptides. In: Kenny AJ, Turner AJ (eds) Mammalian Ectoenzymes. Elsevier, Amsterdam, The Netherlands, pp 211–248
Waksman G, Hamel E, Fournié-Zaluski MC, Roques BP (1986) Autoradiographic comparison of the distribution of the neutral endopeptidase “enkephalinase” and of mu and delta opioid receptors in rat brain. Proc Natl Acad Sci USA 83:1523–1527
Wang HH, Shieh MJ, Liao KF (2005) A blind, randomized comparison of racecadotril and loperamide for stopping acute diarrhea in adults. World J Gastroenterol 11:1540–1543
Wisner A, Dufour E, Messaoudi M, Nejdi A, Marcel A, Ungeheuer MN, Rougeot C (2006) Human Opiorphin, a natural antinociceptive modulator of opioid-dependent pathways. Proc Natl Acad Sci USA 103:17979–17984
Xin L, Geller EB, Liu-Chen LY, Chen C, Adler MW (1997) Substance P release in the rat periaqueductal gray and preoptic anterior hypothalamus after noxious cold stimulation: effect of selective mu and kappa opioid agonists. J Pharmacol Exp Ther 282:1055–1063
Yamada M, Yasuhara H (2004) Clinical pharmacology of MAO inhibitors: safety and future. Neurotoxicology 25:215–221
Zhang H, Torregrossa MM, Jutkiewicz EM, Shi YG, Rice KC, Woods JH, Watson SJ, Ko MC (2006) Endogenous opioids upregulate brain-derived neurotrophic factor mRNA through delta- and micro-opioid receptors independent of antidepressant-like effects. Eur J Neurosci 23:984–994
Zini S, Fournie-Zaluski MC, Chauvel E, Roques BP, Corvol P, Llorens-Cortes C (1996) Identification of metabolic pathways of brain angiotensin II and III using specific aminopeptidase inhibitors: predominant role of angiotensin III in the control of vasopressin release. Proc Natl Acad Sci USA 93:11968–11973
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Noble, F., Benturquia, N., Bilkei-Gorzo, A. et al. Use of preproenkephalin knockout mice and selective inhibitors of enkephalinases to investigate the role of enkephalins in various behaviours. Psychopharmacology 196, 327–335 (2008). https://doi.org/10.1007/s00213-007-0964-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-007-0964-z