Abstract
Rationale
Smokers report enhanced concentration after cigarette smoking and difficulty concentrating when abstinent from smoking. These perceived effects may contribute to smoking cessation failures, and if so, clarification of their cognitive bases could inform treatment strategies. Selective attention may be important in this regard, but earlier literature presents inconsistent findings on how smoking abstinence and resumption of smoking influence this cognitive function.
Objectives
We aimed to compare smokers and nonsmokers on selective attention, and in smokers, to test the effects of overnight abstinence from smoking and of acute smoking on selective attention.
Materials and methods
Smokers and nonsmokers (n = 43) performed a Stroop test (two test days, two test blocks per day). Smokers participated after overnight abstinence and also within 1-h of ad libitum smoking. Smokers each smoked a cigarette between test blocks on each day; nonsmokers did not.
Results
Smokers demonstrated longer response latencies for both congruent and incongruent stimuli after overnight than brief abstinence, but no deficit specifically related to selective attention. Whereas nonsmokers showed no changes in performance in the second test block, smoking between blocks reduced the Stroop effect when smokers were abstinent overnight.
Conclusions
These data are consistent with the hypothesis that abstinence from smoking among nicotine-dependent individuals has deleterious effects on cognitive performance, but do not indicate that selective attention is adversely effected. Improvement in selective attention after terminating abstinence with one cigarette may also contribute to smokers’ perceived enhanced ability to concentrate after smoking.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Worldwide, almost 5 million people die prematurely each year as a result of smoking (World Health Organization 2003). Abstinence from cigarette smoking has generally been associated with self-reports of decreased ability to concentrate (Hatsukami et al. 1984; Hughes et al. 1984; Hughes and Hatsukami 1986; West et al. 1984, 1987) and this perceived difficulty concentrating could pose a barrier to smoking cessation (for review, see Hughes et al. 1990). Consistent with this, self-reported increases in inattention during abstinence predict relapse to smoking (Rukstalis et al. 2005). A more precise understanding of the nature of cognitive deficits that are associated with abstinence from smoking might suggest therapeutic targets. Results from several studies that included cognitive testing indicate that abstinence from smoking is associated with impairment of sustained attention (Hughes et al. 1989; Sacco et al. 2005). It is less clear, however, whether abstinence from smoking is associated with deficits in inhibitory control processes.
The Stroop task is the most frequently used measure of inhibitory control functioning. It measures the ability to focus attention on relevant stimuli while ignoring distracters and to suppress a prepotent response (i.e., word reading) in favor of an atypical one (i.e., color naming) (Stroop 1935). Performance is measured by response latency (i.e., reaction time, RT) and/or accuracy; and specific deficiencies in attention are reflected in a “Stroop effect”, which indicates the degradation in performance caused by interference in the incongruent condition (e.g., the word red displayed in blue). In a study of female smokers (n = 13), 12-h abstinence from smoking was associated with slower response times across conditions of the Stroop task, but not with an increase in the Stroop effect (relative to ad libitum smoking, 5 min after the last cigarette; Pomerleau et al. 1994). Other studies, however, showed no significant impairment after the initiation and maintenance of abstinence compared with baseline performance. These studies involved smokers who were abstinent for a week [22 schizophrenic smokers (Evins et al. 2005); 23 schizophrenic and 29 nonschizophrenic smokers (George et al. 2002)] or who were abstinent overnight [25 schizophrenic and 25 nonschizophrenic smokers (Sacco et al. 2005)]. However, cognitive testing during abstinence in these three studies followed cognitive testing in a nondeprived state, making it possible that practice effects masked abstinence-related deficits in Stroop performance.
In addition to reporting difficulty concentrating during withdrawal from smoking (Hatsukami et al. 1984; Hughes et al. 1984; Hughes and Hatsukami 1986; West et al. 1984, 1987), smokers report enhanced ability to concentrate immediately after smoking a cigarette (Russell et al. 1974; Warburton and Wesnes 1984). The Stroop task has also been used to test the immediate effect of smoking on response inhibition, relative to a presmoking level. For example, in a sample of 16 adolescent smokers tested without a requirement for abstinence before a presmoking test, smoking one cigarette reduced RT but not the Stroop effect (Zack et al. 2001). In studies of adult smokers, smoking a cigarette did not significantly affect Stroop task performance after 12-h of abstinence [(n = 16 and 7, respectively) (Parrott and Craig 1992; Xu and Domino 2000)], nor did smoking two cigarettes change the Stroop effect in 12 subjects after 9-h of abstinence (Ilan and Polich 2001). The small sample sizes used in these studies, however, markedly limit the conclusiveness of these predominantly null findings.
Given the role of difficulty concentrating in the nicotine withdrawal syndrome (American Psychiatric Association 1994), we reasoned that a clearer understanding of the nature of this problem during the initiation of smoking abstinence and its possible reversal by smoking could help identify therapeutic targets. Within this context, we used the Stroop task in a study larger than those cited above, asking the following questions related to performance on the task: (1) Are there differences in performance between nonsmokers and smokers when abstinent only briefly (≤1-h)? (2) Does overnight abstinence from smoking impair performance compared to that observed when smokers are ≤1-h abstinent? (3) Does smoking one cigarette affect the performance of smokers (either after ≥13-h abstinence or after ≤1-h abstinence)? Given findings that cue-elicited tobacco craving disrupts performance on cognitive tasks (Cepeda-Benito and Tiffany 1996; Madden and Zwaan 2001; Sayette and Hufford 1994; Zwaan et al. 2000), we also tested whether cigarette craving influenced performance on the Stroop task.
We were particularly interested in effects of cigarette abstinence and smoking on selective attention given the implications such effects could have for smoking cessation. We chose to measure selective attention using the Stroop task because this task has been studied extensively using brain imaging (Banich et al. 2000; Bench et al. 1993; Brown et al. 1999; Carter et al. 1995; Gruber et al. 2002; Mead et al. 2002; Milham and Banich 2005; Pardo et al. 1990; Taylor et al. 1997) and findings from behavioral studies using this task could, therefore, be readily extended to investigate of underlying brain mechanism in future studies.
Materials and methods
Participants
Forty-three smokers and 43 nonsmokers completed testing with a Stroop task. Potential participants were recruited from flyers and newspaper ads. They were excluded from participation during a telephone interview if they indicated any one of the following criteria: current use of medications that may affect cognition, any medical or psychiatric condition, age of less than 18 or more than 50 years, a history of head trauma, color blindness, smoking marijuana more than once per week, drinking more than 10 alcoholic drinks per week, or regularly abusing substances other than alcohol or marijuana. In addition, nonsmoker participants were excluded if they had a lifetime history of smoking more than five cigarettes. Smokers were excluded if they reported smoking fewer than 15 or more than 40 cigarettes per day, or had not been smoking regularly for at least 2 years.
Participants received a detailed explanation of the study, signed a consent form that was approved by the UCLA Institutional Review Board, and were paid for their participation. During a baseline assessment, additional measures were obtained to determine eligibility. Carbon monoxide (CO) in expired air was taken as an objective measure of recent smoking (Micro Smokerlyzer II, Bedfont Scientific Instruments). The inclusion criteria were ≤5 parts per million (ppm) for nonsmokers and ≥10 ppm for smokers. Participants also completed questionnaires assessing medical history, smoking history [including the Fagerström Test for Nicotine Dependence (Heatherton et al. 1991)], childhood attention deficit hyperactivity disorder (Wender Utah Rating Scale; WURS) (Ward et al. 1993), and demographic information. A participant was excluded if he or she had a score of ≥47 on the WURS. Of the 299 individuals who provided informed consent to participate, 107 smokers and 44 nonsmokers met one or more exclusion criteria. Twenty smokers and 19 nonsmokers withdrew from participating. Only data from participants who completed all four test blocks were included in the analyses. This excluded 23 more participants, leaving 43 subjects per group.
Procedure
Subsequent to baseline assessments, both groups were tested in two blocks on each of two separate days (see Fig. 1). On 1 day, the smokers were tested after 13- to 16-h abstinence and on the other, after 15- to 60-min abstinence. On both days, smokers smoked one cigarette (their usual brands) during a break between the two blocks and nonsmokers rested but did not smoke. Testing resumed within 5 min of the break. Cigarette craving and withdrawal were assessed before and after the Stroop task was administered to the smokers. Twenty-one smokers completed the overnight (≥13-h) abstinence session first and 22 completed the brief (≤1-h) abstinence session first.
On each test day, expired CO was assayed to verify recent smoking or overnight abstinence, with a criterion of ≤10 ppm at the start of the ≥13-h abstinence test (Perpina et al. 1993; Stormark et al. 2000). One participant was allowed to complete the ≥13-h abstinence test with an expired CO level of 13 ppm because this value was less than half of the value obtained after ≤1-h abstinence. To diminish the effect of learning, participants received training on the tasks before each testing session until they became habituated to which finger they were to use to indicate colors on the keyboard. Data collection commenced immediately after training. All testing took place between 14:00 and 17:00 h.
Measures
Self-report measures of withdrawal from smoking were collected using the Shiffman/Jarvik Withdrawal Scale (SJWS) (Shiffman and Jarvik 1976), which includes five subscales (see Table 2). Cigarette craving was assessed using the Urge to Smoke (UTS) scale (Jarvik et al. 2000). The maximum score possible on each of the five SJWS subscales was “7”, as was the total score on the UTS, with higher numbers indicating greater severity of symptoms.
Stroop task
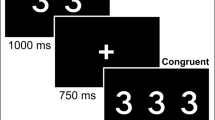
The Stroop task was presented in SuperLab (Cedrus Corporation 1997) on a MacIntosh laptop computer with a 10-in. monitor. Participants were pretrained to respond to each stimulus by pressing a specific key on the keyboard that corresponded to each of the three response options (red, green, and blue). Reaction time (RT) and accuracy were recorded, with no feedback on errors provided to the subjects. The task presented a total of four counterbalanced blocks, consisting of 18 trials each, of congruent color words and incongruent color words. For the congruent condition, the color in which a word appeared matched its meaning (e.g., the word red displayed in red). For the incongruent condition, the meaning of the word differed from the color in which it was presented (e.g., the word red displayed in blue), producing interference because the meaning of the word must be ignored for successful performance. Stimuli were presented one word at a time in the center of the screen in Helvetica style, font size 72, for 200 ms. A fixation cross was presented for 1,300 ms between trials, and 21-s rest was provided between sets. The total time for the test was 12 min.
Data analysis
Only data from participants who completed all four tests were included. Individual trials in which RTs were ≤200 or ≥1,500 ms were censored from the analyses. Only the response times to correct responses were included in the analyses. Error rates, calculated as the percent of incorrect responses of the total trials, were analyzed separately.
The performance of nonsmokers was compared to that of smokers during the precigarette test block of the ≤1-h abstinence session. The analysis was conducted as a repeated measures analysis of variance (ANOVA) with Stroop condition (congruent vs incongruent) included as a within-subject independent variable, and group included as a between-subjects independent variable. To assess the effect of overnight abstinence on Stroop performance of smokers, a repeated measures ANOVA was conducted comparing performance of smokers on the task after ≤1-h abstinence with corresponding performance after ≥13-h abstinence (using only data from the first test block of the session). Again, Stroop condition was also included as a within-subjects variable. Analysis of whether smoking a cigarette affected Stroop performance was complicated by the fact that smoking was confounded with test order. We therefore conducted repeated measures ANOVAs, comparing the performance of smokers and nonsmokers before and after the break. Because only smokers smoked during the break, we tested for an interaction between group and test block as an indication of whether smoking during the break affected the performance of the smokers. Because smoking one cigarette might have a different effect based on the duration of abstinence before smoking, we conducted this analysis separately for performance of smokers during the ≥13-h abstinent session, and for the ≤1-h abstinent session.
All analyses were performed for both RT scores and (normalized) error rates. The interactions between Stroop condition and independent variables of interest (i.e., group, session, and test block) were included to identify effects specifically related to selective attention. Any demographic variable that differed significantly across groups was included as a covariate in all analyses in which group was included. Finally, for all significant findings, follow-up analyses were conducted to assess whether effects on Stroop performance were associated with variability in cigarette craving and withdrawal, as assessed by the UTS scale and SJWS.
Results
Participants
Table 1 presents the demographic characteristics of study participants. Nonsmokers were significantly younger than smokers (30.0 ± 9.15 vs 37.1 ± 10.52; t (84) = 3.37, p < 0.01). Therefore, all analyses involving group as a factor included age as a covariate. Smokers had consumed an average of 20 ± 6 cigarettes per day for 16 ± 9 years. Smokers were moderately dependent, with an average score on the Fagerström test for nicotine dependence of 5.1 ± 1.8.
Measures of withdrawal and cigarette craving
The mean expired CO levels and scores on the UTS and SJWS scales, recorded at each test block, on each test day, are presented in Table 2. These data were partially missing for five participants, who were, therefore, not included in this table. As expected, CO in expired breath was lower and measures of craving and withdrawal were generally higher during the presmoking block of the overnight abstinence session. Also as expected, CO increased and craving and withdrawal decreased after smoking during the break between test blocks, and these changes were generally more pronounced after ≥13-h abstinence than after ≤1-h abstinence. A paired-samples t test demonstrated a significant difference between the change in CO from before to after the break for the ≥13- and ≤1-h abstinence sessions (t(39) = 4.00, p < 0.05).
Stroop task
Table 3 presents RT and error rate summary scores for all conditions of the Stroop task. Because the distribution of error rates was positively skewed across participants, error data were subjected to a square root transformation before statistical analysis. Summary data presented in Table 3, however, are based on nontransformed error rates. As anticipated, a significant main effect of Stroop condition reflected the fact that both RT and error rates were considerably higher for incongruent than for congruent stimuli (incongruent stimuli: overall RT = 505 ± 110, error rate = 3.6% ± 3.3; congruent stimuli: overall RT = 410 ± 84, error rate = 1.8% ± 2.1; p < 0.001).
Primary analyses
In the comparison of nonsmokers to smokers ≤1-h abstinent (age included as a covariate), there were no significant groups differences in RT (F(1,83) = 0.02, p = 0.90) or error rates (F(1,82) = 0.40, p = 0.53), nor was there a significant interaction between group and Stroop condition for RT (F(1,83) = 0.01, p = 0.99) or error rates (F(1,82) = 0.01, p = 0.94).
In the comparison of performance of smokers during the first test block of the ≤1-h abstinence session and the ≥13-h abstinence session (effect of test session), a significant main effect was observed, as smokers generally responded more slowly (F(1,42) = 5.33, p = 0.03, η 2 = 0.11) after ≥13-h abstinence. Overall error rates among smokers in the two-test sessions (2.7% ± 2.9 after ≤1-h abstinence and 2.8% ± 2.8 after ≥13-h abstinence) did not differ significantly (F(1,42) = 0.80, p = 0.38). No interaction was observed between session and Stroop condition as predictors of either RT (F(1,42) = 0.02, p = 0.89) or error rates (F(1,42) = 0.11, p = 0.74). To help interpret the null result for the effect of overnight abstinence on Stroop interference (as inferred through RT) a 95% confidence interval was calculated for the true underlying effect. The observed interval range in true effect size was −0.44 to 0.40.
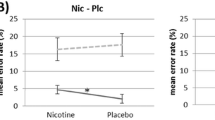
A repeated measures ANOVA was performed in which RTs of nonsmokers and of smokers in the ≥13-h abstinence session were modeled as a function of group, test block, and Stroop condition. A significant interaction was observed between the three independent variables (F(1,83) = 5.85, p = 0.018, η 2 = 0.07) (Table 3). Specifically, while the Stroop effect (RT for incongruent words – RT for congruent words) did not change for nonsmokers across the two test blocks (98 ± 42 vs 100 ± 43), the Stroop effect was significantly reduced for smokers after the cigarette break (99 ± 55 vs 79 ± 51, t(42) = 2.789, p = 0.008). Although the interaction was not significant (F(1,83) = 2.11, p = 0.15), inspection of error data suggested a similar pattern (Table 3). No interactions between group and test block were present in repeated measures ANOVAs comparing the performance of nonsmokers to that of smokers in the ≤1-h abstinence session (all values of p > 0.05).
Correlations of cigarette craving and withdrawal with performance
In accord with our a priori analytical plan, correlation analyses were conducted to relate the effect of abstinence and acute smoking on craving and withdrawal to each observed significant effect of the smoking manipulations on task performance. Differences in craving or withdrawal across conditions were not significantly associated with the main effect of abstinence on RT during performance of the Stroop task (UTS, r = 0.33; SJWS craving score, r = 0.06; p > 0.05) or with the reduction in Stroop interference observed among smokers in the ≥13-h abstinence session subsequent to smoking (UTS, r = 0.04; SJWS craving score, r = 0.19; p > 0.05). To assess whether dose of nicotine (or some other constituent of cigarette smoke) underlies the different effects of acute smoking in the ≥13-h abstinent vs ≤1-h abstinent conditions, we tested covariance of CO differences across sessions (a proxy for nicotine intake). The correlation between the differences in CO and the Stroop interference (≥13-h abstinence session minus ≤1 h) was 0.08, p > 0.05.
Discussion
Both smokers and nonsmokers showed longer latencies and less accuracy on the incongruent than the congruent condition of the Stroop test. In addition, smokers demonstrated longer response latencies (across Stroop conditions) after overnight abstinence than after brief abstinence. Nonsmokers showed no reduction in Stroop interference score in the second test block, but smokers abstinent ≥13-h (but not ≤1-h) demonstrated a reduction in Stroop interference score after smoking a single cigarette. The differences in individuals’ cigarette craving between testing conditions were not correlated with corresponding differences in Stroop performance across conditions (e.g., individuals who showed the greatest difference in craving between the ≥13- and ≤1-h abstinence test sessions did not show the greatest difference in task performance in the ≥13- and ≤1-h abstinence sessions). In contrast to studies examining sustained attention, we found no evidence that selective attention was affected by abstinence.
Our finding that acute smoking reduced the Stroop effect suggests a specific effect on selective attention in abstinent smokers. This effect may be because of an action of nicotine per se. Such an effect would be in keeping with the dose-dependent reduction of the Stroop effect with no effect in a congruent condition by oral nicotine, observed in a group of six heavy smokers and six nonsmokers (Wesnes and Warburton 1978), and the subsequent finding in 24 nonsmokers that nicotine gum reduced the time to name the color in the incongruent condition without an effect of simple color naming (Provost and Woodward 1991). Another study of 12 smokers indicated that administration of nicotine via transdermal patches showed positive responses, with significant reduction in time to completion both in the control and the interference conditions, with no significant effect on Stroop interference, albeit in a relatively small sample (Mancuso et al. 1999).
It is plausible that the absence of reduction of the Stroop effect in smokers after brief but not overnight abstinence may reflect desensitization of nicotinic acetylcholine receptors (nAChRs). About 70% of nAChRs of the α4β2 subtype in cultured cells are desensitized after brief exposure to 10-nM nicotine (1.6 ng/ml) (Paradiso and Steinbach 2003). By comparison, smoking one cigarette can elevate arterial plasma nicotine concentrations above 180 nM (30 ng/ml) for more than 20 min (Gourlay and Benowitz 1997), and can produce >88% occupancy of α4β2 nAChRs in smokers for at least 4-h (Brody et al. 2006). To the extent that nAChRs in human brain respond to nicotine with desensitization as shown in vitro, smoking ad libitum until 45–60 min before testing could render central nAChRs less responsive to activation by nicotine. If smokers had a large proportion of their cerebral α4β2 nAChRs desensitized during testing, the positive effect of smoking one cigarette on selective attention could reflect activation of a population α4β2 nAChRs that are resistant to desensitization or activation of another nAChR subtype. Alternatively, the effect may reflect nonnicotine components of tobacco smoke or of the smoking experience.
It is unclear how much of the improvement in selective attention that we observed reflected effects of nicotine and how much reflected other factors associated with smoking. Substantial research indicates that non-nicotine components of smoking contribute to nicotine dependence (see Robinson et al. 2000 and Rose 2005 for reviews). As several studies have consistently shown, smoking denicotinized cigarettes provides relief from craving and withdrawal symptoms in abstinent smokers (Gross et al. 1997; Pickworth et al. 1999; Westman et al. 1996), but does not reverse the cognitive deficits associated with abstinence (Baldinger et al. 1995). Related research assessing prepulse inhibition (PPI) of startle in overnight abstinent smokers found that smokers did not exhibit significantly lower PPI when abstinent overnight compared to findings on an ad libitum smoking day. However, as we observed with Stroop performance, acute smoking significantly increased PPI. Acute smoking after overnight abstinence produced a significant increase in PPI such that gating in the smokers exceeded that of the nonsmokers (Duncan et al. 2001). It is important to note, however, that the tendency towards lower interference scores among smokers who just smoked a cigarette after ≥13-h abstinence that was observed in the present study was not based on particularly short latencies for responses to incongruent stimuli. As can be seen from inspection of Table 3, mean response times for both congruent and incongruent stimuli were in the direction of faster among nonsmokers than among smokers across study conditions.
Several reviews of the literature on the Stroop task have indicated that results are influenced by methodological factors that may explain the discrepant results found across studies in the smoking literature. These include the use of a nonsmoking control group, verification of abstinence, reliance on within-subject or between-subject analyses, and variation in sample size. Research on selective attention, which can be measured by the Stroop task, has been compromised generally by small sample sizes. In the literature reviewed, the samples ranged from 7 to 25 subjects. The present study was somewhat larger, and thus the absence of an effect of ≥13-h abstinence on Stroop interference scores is more interpretable than previous null findings. The 95% confidence interval calculated for the true underlying effect size of abstinence on Stroop interference (−0.44 to 0.40) provides statistical evidence that moderate to large effects are not present (though small effects, of course, cannot be ruled out).
The present findings should be interpreted with the following caveats in mind. While our sample was larger than most studies on this topic (Johnsen et al. 1997; Mogg and Bradley 2002; Rusted et al. 2000; Zack et al. 2001), it was still modest. In addition, we used a Stroop task that was programmed with a facilitation condition (congruent) and inhibition condition (incongruent) but without neutral conditions (e.g., nonwords displayed in colors). We could not, therefore, distinguish the effect of facilitation during the congruent condition from interference during the incongruent condition.
Smoking was conducted in an unblinded manner and this type of procedure has been considered to be a limitation in the relevant literature (Heishman 1998). In addition, it is likely that the dose of nicotine delivered after ≥13-h abstinence was greater than after ≤1-h abstinence. Consistent with this, the data of Table 2 indicate that CO boosts after smoking one cigarette tended to be larger in the ≥13-h abstinence than in the ≤1-h abstinence session. As we did not assay plasma nicotine, it is not possible to determine to what extent the interaction showing a reduction of the Stroop effect by acute smoking after overnight but not brief abstinence reflected a dose effect. Finally, allowing participants to smoke only one cigarette between test blocks may not have been an adequate manipulation to overcome ≥13-h of abstinence.
Caveats not withstanding, the present findings suggest that when abstinent overnight, smokers exhibit cognitive deficits that detrimentally affect performance across conditions of the Stroop task, but do not support for the hypothesis that smokers abstinent for this period exhibit deficits in selective attention. These data do suggest, however, that after overnight abstinence, selective attention is improved subsequent to smoking a cigarette. Both effects may contribute to the high rate of failure in attempts to quit smoking.
References
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders-fourth edition (DSM-IV). American Psychiatric Association, Washington, DC
Baldinger B, Hasenfratz M, Battig K (1995) Comparison of the effects of nicotine on a fixed rate and a subject-paced version of the rapid information processing task. Psychopharmacology (Berl) 121:396–400
Banich MT, Milham MP, Atchley RA, Cohen NJ, Webb A, Wszalek T, Kramer AF, Liang Z, Barad V, Gullett D, Shah C, Brown C (2000) Prefrontal regions play a predominant role in imposing an attentional ‘set’: evidence from fMRI. Cogn Brain Res 10:1–9
Bench CJ, Frith CD, Grasby PM, Friston KJ, Paulesu E, Frackowiak RS, Dolan RJ (1993) Investigations of the functional anatomy of attention using the Stroop test. Neuropsychologia 31:907–922
Brody AL, Mandelkern MA, London ED, Olmstead RE, Farahi J, Scheibal D, Jou J, Allen V, Tiongson E, Chefer SI, Koren AO, Mukhin AG (2006) Cigarette smoking saturates brain alpha 4 beta 2 nicotinic acetylcholine receptors. Arch Gen Psychiatry 63:907–915
Brown GG, Kindermann SS, Siegle GJ, Granholm E, Wong EC, Buxton RB (1999). Brain activation and pupil response during covert performance of the Stroop Color Word task. J Int Neuropsychol Soc 5:308–319
Carter CS, Mintun MA, Cohen JD (1995) Interference and facilitation effects during selective attention: an H2 15O PET study of Stroop task performance. Neuroimage 2:264–272
Cepeda-Benito A, Tiffany ST (1996) The use of a dual-task procedure for the assessment of cognitive effort associated with cigarette craving. Psychopharmacology (Berl) 127:155–163
Duncan E, Madonick S, Chakravorty S, Parwani A, Szilagyi S, Efferen T, Gonzenbach S, Angrist B, Rotrosen J (2001) Effects of smoking on acoustic startle and prepulse inhibition in humans. Psychopharmacology (Berl) 156:266–272
Evins AE, Deckersbach T, Cather C, Freudenreich O, Culhane MA, Henderson DC, Green MF, Schoenfeld DA, Rigotti NA, Goff DC (2005) Independent effects of tobacco abstinence and bupropion on cognitive function in schizophrenia. J Clin Psychiatry 66:1184–1190
George TP, Vessicchio JC, Termine A, Sahady DM, Head CA, Pepper WT, Kosten TR, Wexler BE (2002) Effects of smoking abstinence on visuospatial working memory function in schizophrenia. Neuropsychopharmacology 26:75–85
Gourlay SG, Benowitz NL (1997) Arteriovenous differences in plasma concentration of nicotine and catecholamines and related cardiovascular effects after smoking, nicotine nasal spray, and intravenous nicotine. Clin Pharmacol Ther 62:453–463
Gross J, Lee J, Stitzer ML (1997) Nicotine-containing versus de-nicotinized cigarettes: effects on craving and withdrawal. Pharmacol Biochem Behav 57:159–165
Gruber SA, Rogowska J, Holcomb P, Soraci S, Yurgelun-Todd D (2002) Stroop performance in normal control subjects: an fMRI study. Neuroimage 16:349–360
Hatsukami DK, Hughes JR, Pickens RW, Svikis D (1984) Tobacco withdrawal symptoms: an experimental analysis. Psychopharmacology (Berl) 84:231–236
Heatherton TF, Kozlowski LT, Frecker RC, Fägerström KO (1991) The Fägerström test for nicotine dependence: a revision of the Fägerström tolerance questionnaire. Br J Addict 86:1119–1127
Heishman SJ (1998) What aspects of human performance are truly enhanced by nicotine? Addiction 93:317–320
Hughes JR, Hatsukami D (1986) Signs and symptoms of tobacco withdrawal. Arch Gen Psychiatry 43:289–294
Hughes JR, Hatsukami DK, Pickens RW, Krahn D, Malin S, Luknic A (1984) Effect of nicotine on the tobacco withdrawal syndrome. Psychopharmacology (Berl) 83:82–87
Hughes JR, Keenan RM, Yellin A (1989) Effect of tobacco withdrawal on sustained attention. Addict Behav 14:577–580
Hughes JR, Higgins ST, Hatsukami DK (1990) Effects of abstinence from tobacco: a critical review. In: Kozlowski LT, Annis HM, Cappell HD, Glaser FB, Goodstadt MS, Israel Y, Kalant H, Sellers EM, Vingilis ER (Eds) Research advances in alcohol and drug problems, vol. 10. Plenum Press, New York, pp 317–398
Ilan AB, Polich J (2001) Tobacco smoking and event-related brain potentials in a Stroop task. Int J Psychophysiol 40:109–118
Jarvik ME, Madsen DC, Olmstead RE, Iwamoto-Schaap PN, Elins JL, Benowitz NL (2000) Nicotine blood levels and subjective craving for cigarettes. Pharmacol Biochem Behav 66:553–558
Johnsen BH, Thayer JF, Laberg JC, Asbjornsen AE (1997) Attentional bias in active smokers, abstinent smokers, and nonsmokers. Addict Behav 22:813–817
Madden CJ, Zwaan RA (2001) The impact of smoking urges on working memory performance. Exp Clin Psychopharmacol 9:418–424
Mancuso G, Warburton DM, Melen M, Sherwood N, Tirelli E (1999) Selective effects of nicotine on attentional processes. Psychopharmacology (Berl) 146:199–204
Mead LA, Mayer AR, Bobholz JA, Woodley SJ, Cunningham JM, Hammeke TA, Rao SM (2002) Neural basis of the Stroop interference task: response competition or selective attention? J Int Neuropsychol Soc 8:735–742
Milham MP, Banich MT (2005) Anterior cingulate cortex: an fMRI analysis of conflict specificity and functional differentiation. Hum Brain Mapp 25:328–335
Mogg K, Bradley BP (2002) Selective processing of smoking-related cues in smokers: manipulation of deprivation level and comparison of three measures of processing bias. J Psychopharmacol 16:385–392
Paradiso KG, Steinbach JH (2003) Nicotine is highly effective at producing desensitization of rat alpha4beta2 neuronal nicotinic receptors. J Physiol 553:857–871
Pardo JV, Pardo PJ, Janer KW, Raichle ME (1990) The anterior cingulate cortex mediates processing selection in the Stroop attentional conflict paradigm. Proc Natl Acad Sci U S A 87:256–259
Parrott AC, Craig D (1992) Cigarette smoking and nicotine gum (0, 2 and 4 mg): effects upon four visual attention tasks. Neuropsychobiology 25:34–43
Perpina C, Hemsley D, Treasure J, de Silva P (1993) Is the selective information processing of food and body words specific to patients with eating disorders? Int J Eat Disord 14:359–366
Pickworth WB, Fant RV, Nelson RA, Rohrer MS, Henningfield JE (1999) Pharmacodynamic effects of new de-nicotinized cigarettes. Nicotine Tob Res 1:357–364
Pomerleau CS, Teuscher F, Goeters S, Pomerleau OF (1994) Effects of nicotine abstinence and menstrual phase on task performance. Addict Behav 19:357–362
Provost SC, Woodward R (1991) Effects of nicotine gum on repeated administration of the Stroop test. Psychopharmacology (Berl) 104:536–540
Robinson ML, Houtsmuller EJ, Moolchan ET, Pickworth WB (2000) Placebo cigarettes in smoking research. Exp Clin Psychopharmacol 8:326–332
Rose JE (2005) Nicotine and nonnicotine factors in cigarette addiction. Psychopharmacology (Berl) 1–12
Rukstalis M, Jepson C, Patterson F, Lerman C (2005) Increases in hyperactive-impulsive symptoms predict relapse among smokers in nicotine replacement therapy. J Subst Abuse Treat 28:297–304
Russell MAH, Peto J, Patel VA (1974) The classification of smoking by a factorial structure of motives. J R Stat Soc 137:313–346
Rusted JM, Caulfield D, King L, Goode A (2000) Moving out of the laboratory: does nicotine improve everyday attention? Behav Pharmacol 11:621–629
Sacco KA, Termine A, Seyal A, Dudas MM, Vessicchio JC, Krishnan-Sarin S, Jatlow PI, Wexler BE, George TP (2005) Effects of cigarette smoking on spatial working memory and attentional deficits in schizophrenia: involvement of nicotinic receptor mechanisms. Arch Gen Psychiatry 62:649–659
Sayette MA, Hufford MR (1994) Effects of cue exposure and deprivation on cognitive resources in smokers. J Abnorm Psychology 103:812–818
Shiffman SM, Jarvik ME (1976) Smoking withdrawal symptoms in two weeks of abstinence. Psychopharmacology (Berl) 50:35–39
Stormark KM, Laberg JC, Nordby H, Hugdahl K (2000) Alcoholics’ selective attention to alcohol stimuli: automated processing? J Stud Alcohol 61:18–23
Stroop JR (1935) Studies of interference in serial verbal reactions. J Exp Psychol 18:643–662
Taylor SF, Kornblum S, Lauber EJ, Minoshima S, Koeppe RA (1997) Isolation of specific interference processing in the Stroop task: PET activation studies. Neuroimage 6:81–92
Warburton DM, Wesnes K (1984) Mechanisms for habitual substance use: food, alcohol, and cigarettes. In: Gale A, Edwards J (eds) Physiological correlates of human behavior, vol 1.: basic issues. Academic, London pp 277–297
Ward MF, Wender PH, Reimherr FW (1993) The Wender Utah rating scale: an aid in the retrospective diagnosis of childhood attention deficit hyperactivity disorder. Am J Psychiatry 150:885–890
Wesnes KA, Warburton DM (1978) The effects of cigarette smoking and nicotine tablets upon human attention. In: Thorton RE (ed) Smoking behaviour: physiological and psychological influences. Churchill-Livingston, London, pp 131–147
West RJ, Jarvis MJ, Russell MA, Carruthers ME, Feyerabend C (1984) Effect of nicotine replacement on the cigarette withdrawal syndrome. Br J Addict 79:215–219
West RJ, Hajek P, Belcher M (1987) Time course of cigarette withdrawal symptoms during four weeks of treatment with nicotine chewing gum. Addict Behav 12:199–203
Westman EC, Behm FM, Rose JE (1996) Dissociating the nicotine and airway sensory effects of smoking. Pharmacol Biochem Behav 53:309–315
World Health Organization (2003) World Health Report 2003. Available at http://www.who.int/whr/2003/en/overview_en.pdf
Xu X, Domino EF (2000) Effects of tobacco smoking on topographic EEG and Stroop test in smoking deprived smokers. Prog Neuropsychopharmacol Biol Psychiatry 24:535–546
Zack M, Belsito L, Scher R, Eissenberg T, Corrigall WA (2001) Effects of abstinence and smoking on information processing in adolescent smokers. Psychopharmacology (Berl) 153:249–257
Zwaan RA, Stanfield RA, Madden CJ (2000) How persistent is the effect of smoking urges on cognitive performance? Exp Clin Psychopharmacol 8:518–523
Acknowledgements
Supported by NIH grants RO1 DA014093.03 (EDL), RO1 DA015059 (ALB), and MOIRR 00865; UC Tobacco-Related Disease Research Program awards 10RT-0091 (EDL) and 11RT-0024 (ALB), a VA Merit Review Type I Award (ALB), and Philip Morris USA and Philip Morris International (EDL). Experiments comply with the current laws of the United States.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Domier, C.P., Monterosso, J.R., Brody, A.L. et al. Effects of cigarette smoking and abstinence on stroop task performance. Psychopharmacology 195, 1–9 (2007). https://doi.org/10.1007/s00213-007-0869-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-007-0869-x