Abstract
Rationale:
Placebo-controlled studies show that midazolam impairs explicit memory in children undergoing surgery (Buffett-Jerrott et al., Psychopharmacology 168:377–386, 2003; Kain et al., Anesthesiology 93:676–684, 2000). A recent within-subjects study showed that midazolam impaired explicit memory while leaving implicit memory intact in a sample of older children undergoing painful medical procedures (Pringle et al., Health Psychol 22:263–269, 2003).
Objectives:
We attempted to replicate and extend these findings in a randomized, placebo-controlled design with younger children undergoing surgery.
Materials and methods:
Children aged 3–6 years who were undergoing ear tube (myringotomy) surgery were randomly assigned to receive midazolam (n=12) or placebo (n=11). After surgery, they were tested on explicit (recognition) and implicit (priming) memory for pictures encoded before surgery.
Results:
Relative to placebo, the midazolam-treated children showed poorer recognition memory on the explicit task but equivalent priming on the implicit task.
Conclusions:
Overall, it appears that midazolam induces a dissociation between explicit and implicit memory in young children in the pediatric surgery setting. Theoretical and clinical implications of the findings are discussed along with directions for future research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Surgery can be a frightening and stressful experience for children (Kain et al. 1996). Pre-operative anxiety can contribute to surgical complications and post-surgery difficulties (Laycock and McNicol 1988). It has been suggested that a drug with anxiolytic and sedative effects administered before anesthesia might be helpful for children (e.g., DeJong and Verburg 1988).
Benzodiazepines are drugs with anxiolytic, sedative, and muscle relaxant properties (Buffett-Jerrott and Stewart 2002; Curran 1986). These drugs also produce ‘anterograde amnesia’—forgetting of information learned after drug administration. In contrast, benzodiazepines do not induce ‘retrograde amnesia’—forgetting of information learned before drug administration (e.g., Twersky et al. 1993). It has been suggested that these anterograde amnestic effects may be beneficial for children undergoing surgery (e.g., DeJong and Verburg 1988; Kupietzky et al. 1996; Playfor et al. 2000). Midazolam is a benzodiazepine with a short half-life, making it a good candidate for use in the day surgery setting (Smith et al. 1981).
Substantial evidence supports a distinction between two types of memory—explicit and implicit. Explicit memory involves conscious attempts to retrieve information from memory. Implicit memory occurs when performance is influenced by a previous experience without conscious retrieval or awareness (Graf and Schacter 1985). Benzodiazepines may be useful pharmacological tools for dissociating these two memory processes as most studies show that these drugs impair explicit memory while leaving implicit memory intact (Curran 1986).
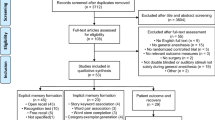
Midazolam is known to impair the explicit memory abilities of adult patients undergoing conscious sedation while leaving their implicit memory abilities intact (e.g., Polster et al. 1993). Several studies have documented impaired explicit memory in pediatric patients administered midazolam. Nonetheless, the large majority of these studies with children have suffered methodological problems including small sample size, lack of placebo control, lack of random assignment, unclear memory assessment, lack of formal memory assessment, few memory stimuli, failure to assess pre-drug memory, and/or lack of control for midazolam’s sedative and attentional effects (e.g., Chen et al. 2000; Cole 1982; Feld et al. 1990; Friedman et al. 1991; Kain et al. 2000; Kupietzky et al. 1996; Payne et al. 1991; Saarnivaara et al. 1988; Saint-Maurice et al. 1990; Sandler et al. 1992; Sievers et al. 1991; Taylor et al. 1986; Twersky et al. 1993).
A recent study by our group (Buffett-Jerrott et al. 2003) was designed to overcome some of these methodological limitations. Forty 4- to 6-year-old children undergoing myringotomy (ear tube surgery) were randomly assigned to either midazolam or placebo. Relative to placebo, midazolam impaired performance on a standardized cued recall task (Greenbaum and Graf 1989) and decreased free recall of hospital events occurring during the window of drug influence.
The only study to date to assess the implicit memory effects of midazolam pre-medication in children (Pringle et al. 2003) was conducted with 6- to 18-year-old children undergoing bone marrow aspiration or lumbar puncture. Relative to pre-drug baseline, midazolam induced impairments in performance on a visual recognition (explicit memory) task while inducing no changes in performance on a visual perceptual facilitation (implicit memory) task. This suggested a midazolam-induced dissociation between explicit and implicit memory in children. However, as no placebo-control group was used in this within-subjects study, alternative interpretations are possible (e.g., the explicit memory task may simply have been more subject to disruptions after the painful medical procedure).
The present study was designed as a replication and extension of the study of Pringle et al. (2003) with the major goal being a further examination of the effects of midazolam on explicit vs implicit memory in children. Methodological improvements to previous research included the use of a randomized, double-blind, placebo-controlled design, use of standardized and age-appropriate memory tasks, control for guessing on the recognition task, control for pre-drug memory performance, and control for the effects of midazolam on sedation and attention. In addition, this study was designed to extend the Pringle et al. results to younger children (aged 3–6 years) and to children undergoing surgery (i.e., myringotomy) rather than painful medical procedures. It was predicted that midazolam would impair explicit memory (hit rates on a visual recognition task) relative to placebo (cf., Buffett-Jerrott et al. 2003; Kain et al. 2000). In contrast, comparable implicit memory performance (i.e., priming level on a visual perceptual facilitation task) was expected among those in the midazolam and placebo groups.
Materials and methods
Participants
The participants were 23 children aged 3–6 years (mean age 5 years and 5 months, SD=11.55 months; 18 males, 5 females) who were scheduled for myringotomy but who were otherwise healthy. Any history of neurological or cognitive impairment or disease, as reported by parents, excluded children from participation. Those with a previous adverse reaction to benzodiazepines or Tylenol® (McNeil Consumer Products, Canada) as reported by parents were also excluded as were children who were taking medication other than antibiotics. The participants were instructed to refrain from eating after midnight the night before the study (normal hospital procedure). Parents provided written informed consent; children provided verbal assent. The study had ethical committee approval.
Only children undergoing purely myringotomy (i.e., not in conjunction with other surgeries) were used in the present study because the procedure and anesthetic are simple and easily standardized. The 3–6 years age range was chosen because preschool children are most likely to require ear tubes (Giebink and Daly 1990) and to control for the poor explicit memory of very young children (Bullock-Drummey and Newcombe 1995; Greenbaum and Graf 1989) and the improvement in explicit memory as children mature (Naito 1990).
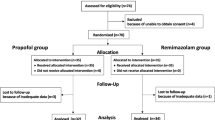
Experimental design and drugs
This study used a randomized, placebo-controlled design. The participants were randomly assigned to the midazolam (n=12) or placebo (n=11) drug group. An independent party conducted this randomization. The active drug group received oral midazolam [Versed® (Roche) for intravenous administration, 5 mg/ml] at a dose of 0.50 mg/kg mixed with acetaminophen [Tylenol® (McNeil Consumer Products, Canada) grape-flavored suspension, 32 mg/ml] at a dose of 15 mg/kg. The placebo group received only Tylenol®, without the midazolam. Drug administration was double-blind; only the nurse administering the drug was aware of the child’s group assignment.
Pilot testing
Twenty-three children, recruited from local daycares, were pilot tested on the explicit and implicit memory tasks used in this study (Bullock-Drummey and Newcombe 1995) to ensure that our computerized versions of these tasks were adequate measures of these memory processes in young children (McGuire 2003). Pilot participants were healthy 3- to 5-year-old children (12 boys). We observed priming on the implicit task. The explicit, but not the implicit, memory task showed improvements with age (cf., Bullock-Drummey and Newcombe 1995).
Tasks and procedure
When a child was scheduled for myringtomy, a letter was sent to the parents followed by a telephone call to explain the study. Ninety minutes before surgery, the researcher met with both the child and the parent(s) to obtain consent/assent. The child’s baseline level of sedation was then experimenter-rated using a five-point rating scale (Wilton et al. 1988) used in previous studies of midazolam as a preoperative medicant in children (e.g., Buffett-Jerrott et al. 2003; Wilton et al. 1988). This scale has excellent inter-rater reliability (Buffett-Jerrott et al. 2003).
When the child entered the day surgery area, a nurse took his/her body weight to determine drug dose. An anesthesiologist also performed a pre-anesthetic assessment to ensure medical eligibility for the study and to order the study medications. Before the midazolam or placebo was administered, children completed a variety of cognitive tasks to ensure pre-drug equivalence between groups. The narrative memory task from the NEPSY (Korkman et al. 1997) – a test of immediate free and cued recall of a short story – was used to assess baseline memory performance. The picture deletion task for preschoolers (PDTP; Corkum et al. 1995) assessed baseline attentional performance. In this task, after a few practice items, children are presented with a page of 60 shapes and asked to scan the page to find all examples of a specific target (ten diamonds or triangles). Children use a bingo marker to mark each target. Time taken to complete the task and omission and commission errors, were measured. The motor deletion task (MDT; Corkum et al. 1995) objectively assessed baseline psychomotor function. In this task, children were presented with a page of 60 circles and asked to put a mark in each circle on the page as quickly as possible, with a 5-min time limit. Time to complete this task as well as omission and commission errors were used as measures of objective sedation. Another observer-rated sedation measure was then taken. At 25 min before surgery, the participants received their assigned drug.
At 10 min post-drug administration, the participants were shown a series of animal pictures. Twenty animal pictures were used for the memory portion of this experiment (cf., Bullock-Drummey and Newcombe 1995). To ensure the ability of our 3- to 6-year-old participants to name the pictures, all of the pictures chosen were at or above the level at which 50% of 2-year-old children can produce the depicted animal name (Fenson et al. 1994). Half of the pictures were obtained from Van Fleet children’s books (1992, 1995, 1998), and the other half were obtained from an Internet search, in which we attempted to closely match the artistic style of Van Fleet. Each picture measured 18.5×24.5 cm. A 300-pixels/cm resolution was used to ensure that the pictures presented in the picture books at encoding were as perceptually similar as possible to those later presented on the laptop in the memory testing phase (Clarke and Morton 1983). The pictures were compiled into two picture books (book A or book B) for use in the pre-surgery encoding phase, with each book containing ten different pictures. The pictures in books A and B were matched for developmental production norm difficulty levels (Fenson et al. 1994). Children were shown only book A or B in the pre-surgery encoding phase; picture book selection was counterbalanced across drug group. The child was shown the pictures one at a time and asked to identify the animal in each picture. If the child was unsure or made an error, the tester told the child the name of the animal and asked the child to repeat it.
After encoding, the tester again rated the child’s sedation. Children were then given the second PDTP (using the target shape that was not presented pre-drug administration) and the MDT. Children were then taken to the operating room. All but two children separated from their parents when leaving the day surgery room. A fourth experimenter-rated sedation score was again assigned at this time. Anesthesia was induced via mask using only halothane/nitrous oxide (N2O).
After the child was awake and returned to the day surgery room, he/she was administered the memory tests (implicit and explicit) to assess his/her memory for the pictures presented in the booklet before surgery, followed by a final rating of sedation. The implicit memory test was always performed first. A laptop was used to present the stimuli in the testing phase. The same computer program used in the pilot testing of daycare children (McGuire 2003) was used in the present study. The program was designed to present the stimuli in a random order, both in a progressively less degraded state (for the implicit task) and in a clear, non-degraded state (for the explicit task). Blurriness was defined by the number of pixels present in the image. At 50% degradation, half of the pixels from the original picture were replaced with random pixels from the 256 colors available to the computer. The pixels to be replaced were selected arbitrarily and replaced with random colors.
The implicit memory task presented ten pre-selected pictures in a random order in progressively less-degraded states. There were ten trials for each participant: five “primed” (i.e., pictures that the child had seen previously in the picture book during the pre-surgery encoding phase) and five “unprimed” (i.e., pictures from the other book to which the child had not been exposed during encoding). One image was presented per trial. The child was asked to identify the picture verbally as soon as he/she knew what it was. Each trial began with a white screen. A small, black cross then appeared on the screen followed by 500 ms of white screen and then the stimulus presentation. There were seven levels of degradation per trial (100, 92, 84, 76, 68, 60, and 52% blurriness). Each degradation level was presented for 1,500 ms. The maximum cumulative identification time per trial was 15,000 ms. The researcher pressed the right or left arrow keys upon the child’s correct identification of the picture. The computer program then automatically recorded the child’s cumulative identification time (latency from trial onset to correct identification). Upon correct identification, the picture was then displayed for 1,500 ms in clear form (0% blurriness). If no response occurred, the trial ended at 52% blurriness and the picture was not presented in clear form. The children were told at the beginning of the task that, when they correctly identified the animal in the picture, they would be presented with the clear form of the picture. Between trials, 500 ms elapsed before the presentation of the small, black cross signaling the start of the next trial.
The explicit memory task immediately followed the implicit task. Different animal pictures were used for the implicit and explicit memory tasks. The explicit memory test was a recognition memory test for the animal pictures. This test involved presentation of ten picture trials: five “old” (i.e., pictures to which the child had been exposed through the picture book presented in the pre-surgery encoding phase) and five “new” (i.e., pictures from the other book to which the child had not been previously exposed). One picture was presented per trial in random order. A small, black cross appeared on the screen, followed by 500 ms of white screen and then the stimulus presentation. The images were presented in clear (non-degraded) form for 10,000 ms each. The participant was asked to indicate whether or not the presented picture was one that they had seen in the picture book just before surgery. The researcher recorded the participant’s response for each trial. Responses were later scored as hits, misses, false alarms, and correct rejections (Green and Swets 1966). Between trials, 500 ms elapsed before the presentation of the small, black cross that signaled the onset of the next trial.
Results
Participant characteristics
A series of chi-square analyses and ANOVAs were conducted to determine if the drug groups differed on any of the demographic control variables. There was no effect of drug group for the number of females (n=5), the number of children who had previously undergone surgery (n=11), the number with parents present in the operating room (n=2), or the age of the child. No children had previously taken midazolam.
Pre-drug cognitive functioning
Pre-drug measures of narrative memory (total memory score from NEPSY), attention (time to complete PDTP and omission and commission errors), psychomotor speed (time to complete MDT and omission and commission errors), and observer-rated sedation (at the two pre-drug testing times) were analyzed with a series of one-way ANOVAs to determine if the drug groups were equivalent before drug administration. There were no significant effects of drug group on any of the pre-drug measures.Footnote 1 Means (SDs) for these pre-drug cognitive measures are displayed in Tables 1, 2, and 3 (for attention, psychomotor speed, and observer-rated sedation, respectively). Means (SDs) on the NEPSY were 10.09 (8.57) and 10.17 (3.27) for placebo and midazolam, respectively.
Memory effects
Implicit memory
Performance on the implicit memory task was assessed by comparing the mean cumulative identification time on primed vs unprimed stimuli across drug groups. The child was required to respond to the presented stimuli within 15,000 ms of trial onset. If no response was provided within this window, the child was assigned a maximum value reaction time of 15,000 ms for that particular trial. Such types of trials occurred relatively rarely (i.e., on only 41 of 230 trials). A 2×2 (drug group × priming level) mixed model ANOVA was performed on the cumulative identification times. There was a significant effect of priming level [F(1, 21)=6.97, p<0.05; power=0.711]: primed pictures were identified significantly more quickly than unprimed pictures (see Fig. 1). There was no main effect of drug group [F(1, 21)=0.08, n.s.; power=0.058] and no drug group × priming level interaction [F(1, 21)=0.02, n.s.; power=0.052] (see Fig. 1).
Explicit memory
Hit rates and false alarm rates, the two explicit memory dependent variables of interest, were expressed as proportional scores. These scores were analyzed in a pair of one-way (drug group) ANOVAs. The first ANOVA indicated that the midazolam group showed a significantly lower hit rate than the placebo controls [F(1, 21)=4.37, p<0.05; power=0.513; see Fig. 2]. In the second ANOVA, there was no significant drug group effect for false alarm rate [F(1, 21)=0.08, n.s; power=0.058; see Fig. 2], indicating that there was no drug group difference in guessing.
Attention task
A set of 2×2 [drug group × drug phase (pre- vs post-drug administration)] ANOVAs was conducted on the three dependent measures from the PDTP. Means (SDs) are presented in Table 1. A significant drug group × drug phase interaction [F(1, 21)=5.66, p<0.05; power=0.621] was observed for completion time. Simple effects tests indicated a marginal effect of drug phase for the midazolam [F(1, 11)=4.31, p=0.062] but not for the placebo-treated participants [F(1, 10)=1.58, n.s.]. Only midazolam-treated participants tended to take longer to complete the task after drug administration compared to their pre-drug performance speed (see Table 1). The ANOVAs on the attentional omissions and commissions indicated no significant effects, but power to detect a drug group × drug phase interaction was relatively low (0.123 and 0.430, respectively), and floor effects were evident on these variables.
Objective sedation
A set of 2×2 (drug group × drug phase) ANOVAs was conducted on the three dependent measures from the MDT. Means (SDs) are presented in Table 2. A significant main effect of drug phase [F(1, 21)=6.41, p<0.05; power=0.675) and a marginally significant drug group × drug phase interaction [F(1, 21)=3.75, p=0.066; power=0.455] were observed for omission errors. Simple effects tests indicated a significant effect of drug phase for midazolam [F(1, 11)=5.93, p<0.05] but not for placebo [F(1, 10)=1.04, n.s.]. Only midazolam-treated participants made more omission errors on the task after drug administration compared to their pre-drug performance (see Table 2). The ANOVA on commission errors indicated no significant effects (see Table 2), although power to detect a drug group × drug phase interaction was low (0.135), and floor effects were again evident. A significant main effect of drug phase [F(1, 21)=10.34, p<0.005; power=0.866] was observed on completion time with completion time increasing from pre- to post-drug administration. No effects involving the drug group factor were observed for completion time, although power to detect a drug group × drug phase interaction was low (0.060).Footnote 2
Observer-rated sedation
Scores on the observer-rated sedation scale were subjected to a 2×5 (drug group × testing time) mixed-model ANOVA. The five testing times were: (a) in the waiting area, (b) at the pre-drug cognitive testing, (c) post-drug, (d) on leaving the day surgery room for the operating room, and (e) in the day surgery room after recovery. Main effects of drug group [F(1, 21)=5.54, p<0.05; power=0.612] and testing time [F(4, 84)=5.25, p<0.005; power=0.963] were obtained that were qualified by a significant drug group × testing time interaction [F(4, 84)=5.50, p<0.005; power=0.970]. Simple effects tests indicated significantly greater sedation scores in the midazolam- vs placebo-treated participants at post-drug administration [F(1, 21)=15.92, p<0.005] and leaving the day surgery room for the operating room [F(1, 21)=7.19, p<0.05] testing points, but no significant sedation rating differences exist between drug groups in the waiting area [F(1, 21)=0.35, n.s.], at the pre-drug cognitive testing [F(1, 21)=0.26, n.s.], or in the day surgery room after recovery [F(1, 21)=0.41, n.s.] (see Table 3).
Analyses of covariance (ANCOVAs)
ANCOVAs were conducted to control for the possible influences of attention, psychomotor impairments, and sedation on midazolam-induced explicit memory impairments. This set of ANCOVAs re-examined the hit rate scores on the recognition memory task while using one index of each of these additional cognitive constructs at the post-drug assessment time as a covariate (i.e., attention time on the PDTP, omission errors on the MDT, and observer-rated sedation at the post-drug administration cognitive assessment time, respectively, each of which were significantly influenced by midazolam). Drug group effects remained significant when controlling for both psychomotor impairments and observer-rated sedation. With respect to the ANCOVA controlling for attention, although covariate-adjusted hit rate index scores remained in the same direction as before covariance (i.e., midazolam placebo), covarying attention speed reduced the drug group effect to marginal significance [F(1, 20)=3.06, p=0.096].
Discussion
The results of our study demonstrate a dissociation between explicit and implicit memory. Relative to placebo, midazolam reduced post-surgery performance on an explicit memory task testing recognition of animal pictures presented before surgery. In contrast, midazolam- and placebo-treated children showed equivalent levels of implicit memory for the same set of animal pictures, as evidenced by equivalent priming on a visual identification task. Thus, when administered in a pediatric surgery context, midazolam appears to exert effects much like those observed for other benzodiazepines with adults (Buffett-Jerrott and Stewart 2002).
The finding that midazolam exerted impairment relative to placebo on the explicit recognition memory task is consistent with the prior literature that therapeutic doses of midazolam induce anterograde amnesia in both adults (e.g., O’Boyle et al. 1987) and children (e.g., Twersky et al. 1993). Unlike some studies of midazolam’s effects on recognition memory in children (e.g., Kain et al. 2000), we controlled for guessing on the recognition memory task. The fact that false alarm rates were unaffected by midazolam ensures that the drug effects observed on the primary dependent measure on our explicit memory task (i.e., hit rate) were not secondary to a decreased willingness to guess “yes” on the recognition task among midazolam-treated children.
Priming effects were observed on the visual identification (implicit memory) task such that pictures previously viewed by children at the encoding phase before surgery were identified much earlier (at greater levels of degradation) than were control pictures not viewed previously. These findings extend to the pediatric surgery context, previous findings that preschool children, as young as age 3, reliably show priming on such facilitation tasks (e.g., Bullock-Drummey and Newcombe 1995; McGuire 2003; Pringle et al. 2003). The active drug and placebo groups showed equivalent levels of priming on this implicit memory task. Thus, although midazolam is commonly considered an amnestic drug, our results show preserved implicit memory for material to which midazolam-treated children were exposed just before surgery.
Midazolam also exerted additional disruptions in cognitive and psychomotor functions, relative to placebo. The finding of slowed performance on a task requiring focused attention (i.e., the PDTP; Corkum et al. 1995) is consistent with our previous findings (Buffett-Jerrott et al. 2003). Relative to placebo, midazolam also induced substantial sedation. First, observer-rated sedation was increased in the midazolam vs placebo group at the two testing points after drug administration and before surgery (cf., Buffett-Jerrott et al. 2003). Like in our previous research (Buffett-Jerrott et al. 2003), we also observed differences between the midazolam and placebo groups on a standardized test of psychomotor function—the MDT (Corkum et al. 1995). However, in the present study, this drug group difference was observed on omission errors (i.e., skipping circles that should have been marked) whereas the drug group effect was observed on completion time in our prior study where errors were not scored (Buffett-Jerrott et al. 2003). In the present study, we observed slowing on the MDT from pre- to post-drug administration, but this effect was not specific to the midazolam-treated children. This slowing may have been due to fatigue effects at the post-drug testing point and/or our inclusion of younger (3 years old) children who may have tired of this task more easily. Regardless of the reasons for this slight discrepancy from the results of our prior study (Buffett-Jerrott et al.), considering the possibility of speed–accuracy trade-offs on such tasks, we recommend that future cognitive psychopharmacology studies with children score such tasks for both speed and accuracy.
Our results further suggest that midazolam-induced explicit memory impairments are not secondary to sedation (cf., Buffett-Jerrott et al. 2003). Covariance analyses results suggested that midazolam-induced attentional impairments may contribute in part to the recognition memory impairments observed in children administered with midazolam. This result is not particularly surprising given the important role of attention at encoding to later explicit memory performance (e.g., Rabinowitz et al. 1982). However, attentional impairments do not appear to completely explain midazolam’s effects in impairing explicit memory, as the drug effect was still marginally significant after attentional performance was covaried out.
The present findings have important theoretical as well as clinical implications. Given the many methodological improvements over prior research incorporated in the present study design, this study adds to a growing body of research supporting benzodiazepines, including midazolam, as a set of pharmacological tools for dissociating explicit and implicit memory processes. The results are consistent with positions that explicit and implicit memory may be subserved by distinct memory systems (e.g., Schacter 1994) as only explicit and not implicit memory performance was disrupted by benzodiazepine administration.
The present findings also have clinical implications for several areas of medical practice where midazolam is administered as a pre-operative or pre-procedural medicant in anxiety prevention/anxiety management. Midazolam is an established anxiolytic for children in the pediatric surgery context. For example, placebo-controlled research has shown midazolam to dampen the increase in anxiety that occurs at mask induction of anesthesia (e.g., Finley et al. 2006). Nonetheless, there are anecdotal reports of children previously administered with midazolam who continue to display anticipatory anxiety at subsequent surgeries/medical procedures (for a review, see Chen et al. 2000). We have also recently found that midazolam-treated children display more anxious behavior shortly after surgery than children administered with placebo (Stewart 2006). The present findings provide a possible explanation for such paradoxical findings: midazolam preserves implicit memory for potentially stressful events occurring just before surgery (e.g., mask induction of anesthetic) but induces poor explicit memory for these same events. Thus, children administered with midazolam as a pre-operative medicant would unconsciously remember these potentially stressful events but at the same time would be unable to pull them consciously to mind to work them through and make sense of them. Thus, suggestions that midazolam’s amnestic effects may be beneficial for children (e.g., DeJong and Verburg 1988) should be tempered by cautions that midazolam may simultaneously interfere with explicit memory while preserving implicit memory. Future research should focus on exploring the consequences of the particular pattern of memory impairments induced by this commonly used pre-medicant (Kain et al. 1997) among pediatric surgery patients.
Notes
Because Levene’s test for equality of variances showed that the equal variance assumption was violated in the case of commission errors on the PDTP (see Table 1), we also compared the two drug groups on this baseline variable using a non-parametric test—specifically, the Mann–Whitney U test. This test confirmed that there were no significant differences between groups on this variable at baseline (Z=−0.736, n.s.).
Given concerns about possible violations of the assumption of equal variances required for ANOVA (see Tables 1 and 2), we also analyzed the variables derived from the PDTP and MDT using non-parametric tests. Wilcoxon signed-ranks tests for dependent samples (Daniel 1978) were specifically used to compare pre- and post-drug performance on each of the six dependent measures in each drug group separately. One-tailed tests were used as directional predictions had been made a priori. These non-parametric tests produced a nearly identical pattern of findings to those reported for the ANOVAs in the main body of the paper. As observed with the ANOVAs, significant effects of drug phase were observed with the Wilcoxon tests for: attention speed in the midazolam group (Z=−1.726, p<0.05), number of omissions on the MDT in the midazolam group (Z=−1.992, p< 0.05), psychomotor speed in the midazolam group (Z=−2.667, p<0.005), and psychomotor speed in the placebo group (Z=−1.784, p<0.05). The Wilcoxon tests revealed an additional significant effect of drug phase for commission errors on the attentional test in the midazolam group (Z=−1.890, p<0.05). In each case, performance was worse at post-drug than at pre-drug baseline.
References
Buffett-Jerrott SE, Stewart SH (2002) Cognitive and sedative effects of benzodiazepine use. Curr Pharm Des 8:45–58
Buffett-Jerrott SE, Stewart SH, Finley GA, Loughlan HL (2003) Effects of benzodiazepines on explicit memory in a paediatric surgery setting. Psychopharmacology 168:377–386
Bullock-Drummey A, Newcombe N (1995) Remembering versus knowing the past: children’s explicit and implicit memories for pictures. J Exp Child Psychol 59:549–565
Chen E, Zeltzer LK, Craske MG, Katz ER (2000) Children’s memories for painful cancer treatment procedures: implications for distress. Child Dev 71:933–947
Clarke R, Morton J (1983) Cross modality facilitation in tachistoscopic word recognition. Q J Exp Psychol A Human Exp Psychol 35:79–96
Cole WHJ (1982) Midazolam in paediatric anaesthesia. Anaesth Intensive Care 10:36–39
Corkum V, Byrne JM, Ellsworth C (1995) Clinical assessment of sustained attention in preschoolers. Child Neuropsychol 1:3–18
Curran HV (1986) Tranquilizing memories: a review of the effects of benzodiazepines on human memory. Biol Psychol 23:179–213
Daniel WW (1978) Applied non-parametric statistics. Houghton Mifflin, Boston, MA
DeJong PC, Verburg MP (1988) Comparison of rectal to intramuscular administration of midazolam and atropine for premedication of children. Acta Anaesthesiol Scand 32:485–489
Feld LH, Negus JB, White PF (1990) Oral midazolam preanesthetic medication in pediatric outpatients. Anesthesiology 73:831–834
Fenson L, Dale PS, Reznick JS, Bates E, Thal DL, Pethick SJ (1994) Variability in early communicative development. Monogr Soc Res Child Dev 59:1–173
Finley GA, Stewart SH, Buffett-Jerrott S, Wright KD, Millington D (2006) High levels of impulsivity may contraindicate midazolam premedication in children. Can J Anaesth 53:73–78
Friedman AG, Mulhern RK, Fairclough D, Ward PM, Baker D, Mirro J, Rivera GK (1991) Midazolam premedication for pediatric bone marrow aspiration and lumbar puncture. Med Pediatr Oncol 19:499–504
Giebink GS, Daly K (1990) Epidemiology and management of otitis media in children. Top Lang Disord 11:1–10
Graf P, Schacter DL (1985) Implicit and explicit memory for new associations in normal and amnesic subjects. J Exp Psychol 11:501–518
Green DM, Swets JA (1966) Signal detection theory and psychophysics. Wiley, New York
Greenbaum JL, Graf P (1989) Preschool period development of implicit and explicit remembering. Bull Psychon Soc 27:417–420
Kain ZN, Mayes LC, O’Connor TZ, Cicchetti DV (1996) Preoperative anxiety in children: predictors and outcomes. Arch Pediatr Adolesc Med 150:1238–1245
Kain ZN, Mayes LC, Bell C, Weisman S, Hofstadter MB, Rimar S (1997) Premedication in the United States: a status report. Anesth Analg 84:427–432
Kain ZN, Hofstadter MB, Mayes LC, Krivutza DM,Alexander G, Wang S, Reznick JS (2000) Midazolam: effects on amnesia and anxiety in children. Anesthesiology 93:676–684
Korkman M, Kirk U, Kemp S (1997) Manual for the NEPSY: a developmental neuropsychological assessment. The Psychological Corporation, New York
Kupietzky A, Holan G, Shapira J (1996) Intranasal midazolam better at effecting amnesia after sedation than oral hydroxyzine: a pilot study. Pediatr Dent 18:32–34
Laycock GJA, McNicol LR (1988) Hypoxamia during induction of anaesthesia—an audit of children who underwent general anaesthesia for routine elective surgery. Anaesthesia 43:981–984
McGuire KA (2003) Developmental changes in children’s implicit and explicit memory abilities from 3 to 5 years of age. Undergraduate honors thesis, Department of Psychology, Dalhousie University
Naito M (1990) Repetition priming in children and adults: age-related dissociation between implicit and explicit memory. J Exp Child Psychol 50:462–484
O’Boyle CA, Barry H, Fox E, Harris D, McCreary C (1987) Benzodiazepine-induced event amnesia following a stressful surgical procedure. Psychopharmacology 91:244–247
Payne KA, Coetzee AR, Mattheyse FJ (1991) Midazolam and amnesia in pediatric premedication. Acta Anaesthesiol Belg 42:101–105
Pringle B, Dahlquist LM, Eskenazi A (2003) Memory in pediatric patients undergoing conscious sedation for aversive medical procedures. Health Psychol 22:263–269
Playfor S, Thomas D, Choonara I (2000) Recollection of children following intensive care. Arch Dis Child 83:445–448
Polster MR, McCarthy RA, O’Sullivan G, Gray PA, Park GR (1993) Midazolam-induced amnesia: implications for the implicit/explicit memory distinction. Brain Cogn 22:244–265
Rabinowitz JC, Craik FI, Ackerman BP (1982) A processing resource account of age differences in recall. Can J Psychol 36:325–344
Saarnivaara L, Lindgren L, Klemola UM (1988) Comparison of chloral hydrate and midazolam by mouth as premedicants in children undergoing otolaryngological surgery. Br J Anaesth 61:390–396
Saint-Maurice C, Landais A, Delleur MM, Esteve C, MacGee K, Murat I (1990) The use of midazolam in diagnostic and short surgical procedures in children. Acta Anaesthesiol Scand 34:39–41
Sandler ES, Weyman C, Conner K, Reilly K, Dickson N, Luzins J, McGorray S (1992) Midazolam versus fentanyl as premedication for painful procedures in children with cancer. Pediatrics 89:631–634
Schacter DL (1994) Priming and multiple memory systems: perceptual mechanisms of implicit memory. In: Schacter DL, Tulving E (eds) Memory systems. Massachusetts Institute of Technology Press, Cambridge, MA, pp 235–268
Sievers TD, Yee JD, Foley ME, Blanding PJ, Berde CB (1991) Midazolam for conscious sedation during pediatric oncology procedures: safety and recovery parameters. Pediatrics 88:1172–1179
Smith MT, Eadie MJ, O’Rourke-Brophy T (1981) The pharmacokinetics of midazolam in man. Eur J Clin Pharmacol 19:271–278
Stewart SH (2006) The use of midazolam in anxiety prevention in the pediatric surgery context. Presented at the Winter Anxiety Summit, Jay Peak, Vermont, February
Taylor MB, Vine PR, Hatch DJ (1986) Intramuscular midazolam premedication in small children. Anaesthesia 41:21–26
Twersky RS, Hartung J, Berger BJ, McClain J, Beaton C (1993) Midazolam enhances anterograde but not retrograde amnesia in pediatric patients. Anesthesiology 78:51–55
Van Fleet M (1992) One yellow lion. Penguin Books, New York
Van Fleet M (1995) Fuzzy yellow ducklings. Dial Books for Young Readers, New York
Van Fleet M (1998) Spotted yellow frogs. Dial Books for Young Readers, New York
Wilton NCT, Leigh J, Rosen DR, Pandit UA (1988) Preanesthetic sedation of preschool children using intranasal midazolam. Anesthesiology 69:972–975
Acknowledgements
This research was supported by a category A grant from the IWK Health Center Research Foundation. We wish to acknowledge the support and cooperation of the surgeons of the Division of Otolaryngology and of the nursing staff in the Day Surgery Unit, Operating Room, and Recovery Room of the IWK Health Center. We also wish to thank the many students and research assistants who helped out in various ways with this project including Allison Eisner, Alyson Currie, Katina Garduno, Courtney Maloney, and Katie McGuire. The assistance of Dr. W. Joseph MacInnes in programming our computer tasks is also gratefully acknowledged. Dr. Stewart is supported by an investigator award from the Canadian Institutes of Health Research and by a Killam research professorship from the Dalhousie University Faculty of Science. Dr. Finley was a Dalhousie University clinical research scholar, and Ms. Wright was supported by a doctoral fellowship from the Canadian Institutes of Health Research at the time this research was conducted.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stewart, S.H., Buffett-Jerrott, S.E., Finley, G.A. et al. Effects of midazolam on explicit vs implicit memory in a pediatric surgery setting. Psychopharmacology 188, 489–497 (2006). https://doi.org/10.1007/s00213-006-0402-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-006-0402-7