Abstract
Rationale
Gamma-aminobutyric acid (GABA)-benzodiazepine receptor function is hypothesised to be reduced in alcohol dependence.
Objectives
We used positron emission tomography (PET) with [11C]flumazenil, a non-selective tracer for brain GABA-benzodiazepine (GABA-BDZ) receptor binding, to determine in vivo the relationship between BDZ receptor occupancy by an agonist, midazolam, and its functional effects.
Methods
Abstinent male alcohol dependent subjects underwent [11C]flumazenil PET to measure occupancy of BDZ receptors by midazolam whilst recording its pharmacodynamic effects on behavioural and physiological measures. Rate constants describing the exchange of [11C]flumazenil between the plasma and brain compartments were derived from time activity curves.
Results
A 50% reduction in electroencephalography (EEG)-measured sleep time was seen in the alcohol dependent group despite the same degree of occupancy by midazolam as seen in the control group. The effects of midazolam on other measures of benzodiazepine receptor function, increasing EEG beta1 power and slowing of saccadic eye movements, were similar in the two groups. No differences in midazolam or flumazenil metabolism were found between the groups.
Conclusions
In summary, our study suggests that alcohol dependence in man is associated with a reduced EEG sleep response to the benzodiazepine agonist, midazolam, which is not explained by reduced BDZ receptor occupancy, and is consistent with reduced sensitivity in this measure of GABA-BDZ receptor function in alcohol dependence. The lack of change in other functional measures may reflect a differential involvement of particular subtypes of the GABA-BDZ receptor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adaptive responses, such as tolerance, to exogenous pharmacological agents are a common experience in neuropsychopharmacology. However, understanding the nature of such changes is difficult as, until recently, it has not been possible to control for levels in drug occupation of brain receptors. To overcome this confound, we developed a positron emission tomography (PET) in vivo paradigm that directly measured the relationship between brain gamma-aminobutyric acid (GABA)-benzodiazepine (GABA-BDZ) receptor occupancy and pharmacodynamic effects (Malizia et al. 1996). Using the non-selective BDZ PET tracer, [11C]flumazenil, it was found that increased occupancy of this receptor by the benzodiazepine agonist, midazolam, positively correlated with increases in electroencephalographic (EEG) beta activity.
The GABA-BDZ receptor is hypothesised to function abnormally in a number of different neuropsychiatric conditions including anxiety, epilepsy and alcoholism (Nutt and Malizia 2001). In this study we used [11C]flumazenil PET with concomitant functional measures to test the hypothesis that GABA-BDZ receptor function is reduced in alcohol dependence in man. Clinically, altered sensitivity of the GABAA receptor complex to anaesthetics was raised as a concern in patients who misuse alcohol (Bruce 1983) and there are a number of studies suggesting significant alterations of the function of this receptor in alcohol dependence.
Alcohol affects many neurotransmitter pathways, but augmenting GABA-ergic function is recognised as key in the anxiolytic, hypnotic, sedative and ataxic effects of alcohol (see Nutt 1999). Animal models show that acutely, alcohol increases Cl− flux through the GABA-BDZ receptor (Suzdak et al. 1986) but chronic alcohol exposure results in decreased sensitivity to alcohol and other benzodiazepine agonists, i.e. tolerance (Buck and Harris 1990). Such neuro-adaptation is associated with functional changes in specific subunits of the GABA-BDZ receptor in particular regions of the brain (see Grobin et al. 1998). For instance, reduced levels of α1 subunit mRNA and peptide has been consistently reported in rat cortex (Montpied et al. 1991; Mhatre and Ticku 1992) with increased expression of α4 subunit mRNA (Devaud et al. 1995).
However, it is not yet clear what processes might explain the human experience of tolerance to alcohol and cross-tolerance to other drugs acting at the GABAA receptor. Human post-mortem studies using a variety of radioligands show increases, decreases or no changes in GABA-BDZ receptor levels (Tran et al. 1981; Freund and Ballinger 1988; Dodd et al. 1992; Korpi et al. 1992). One post-mortem study revealed increased expression of α1 subunit mRNA and peptide in the superior frontal cortex of alcoholics, but no such increase was seen either in the motor cortex or in the α3 subunit mRNA and peptide (Lewohl et al. 1997, 2001). By contrast, Mitsuyama et al. (1998) reported no significant increase in α1 subunit mRNA or peptide expression in the frontal cortex of alcohol dependent patients.
In vivo neuroimaging studies using [11C]flumazenil PET or [123I]iomazenil and single photon emission computed tomography (SPECT) to label the GABA-BDZ receptor have consistently shown reduced GABA-BDZ receptor binding, particularly in the frontal cortex in abstinent alcohol dependent subjects (Gilman et al. 1996; Abi-Dargham et al. 1998; Lingford-Hughes et al. 1998). There is also evidence from an [18F]FDG [2-deoxy-2[18F]fluoro-d-glucose] PET study that GABA-BDZ receptor function may be reduced in alcoholism since the inhibitory response to a challenge with the benzodiazepine agonist, lorazepam, was found to be blunted in the orbitofrontal cortex and cingulate gyrus in alcohol dependent subjects abstinent for 8–11 weeks (Volkow et al. 1997).
Conventional ways in which benzodiazepine receptor function has been evaluated in man include effects of agonists on EEG and saccadic eye movements. Benzodiazepines increase EEG beta power, produce sedation and reduce saccadic eye movements in a dose-dependent manner (Domino et al. 1989; Feshchenko et al. 1997; Hommer et al. 1986; Ball et al. 1991). However, the relationship between occupancy at brain benzodiazepine receptors and function had to be inferred from the plasma concentration.
The aim of this study was, therefore, to directly measure for the first time the function of GABA-BDZ receptor in humans to specifically test the hypothesis that alcohol dependence is associated with reduced benzodiazepine receptor sensitivity in man by using PET to simultaneously assess of the brain pharmacokinetics and pharmacodynamics of midazolam.
Materials and methods
Subjects
Abstinent male subjects who fulfilled DSM IV criteria for alcohol dependence were recruited from local alcohol treatment services. They had all been abstinent for at least 6 weeks. The average length of abstinence was 7.3 months (SE±1.5, range 2–18 months). This avoided early withdrawal/abstinence phase, when significant changes in blood flow are reported to occur which might confound comparisons (Volkow et al. 1994). The control group consisted of male subjects who had never fulfilled such criteria, i.e. were non-dependent alcohol drinkers and were recruited through colleagues and advertisements. Subjects with clinical evidence of hepatic, cognitive or neurological impairment or medical disorder were excluded. All subjects had no previous or current history of psychosis or anxiety disorders. One alcohol dependent and one non-dependent control subject each had a history of major depressive disorder; they were not depressed at the time of PET but were receiving treatment with paroxetine and clomipramine, respectively. The effect of depression or chronic serotonergic antidepressants therapy on benzodiazepine receptors is not clear (see Kugaya et al. 2003). All parameters measured for these two subjects were within the range of the other subjects and results of analyses performed with and without them were not different. The results described hereafter therefore include these two subjects. No other prescribed psychotropic drugs were being currently taken and benzodiazepines had not been taken for at least 6 weeks since detoxification in the alcohol dependent group. Recreational or occasional use of illicit drugs (e.g. cannabis), but not dependency (DSM IV defined) was admissible, although for most subjects, drug use was not current. Technical difficulties resulted in rejection of scan data from five subjects. This paper describes the 21 subjects (11 alcohol dependent and ten non-dependent) from whom [11C]flumazenil PET images were analyzable.
All subjects were assessed for their severity of dependency (Severity of Dependency Questionnaire (SADQ), Stockwell et al. 1983). Anxiety and depression were assessed using the Beck Depression Inventory (BDI; Beck et al. 1961), and Spielberger State–Trait Anxiety Inventory (SSAI, STAI; Spielberger 1983).
Informed consent was obtained before participation in the study, which had been approved by the local Ethics Committees and from the UK Administration of Radioactive Substances Advisory Committee.
[11C]Flumazenil PET
[11C]Flumazenil was prepared with >95% radiochemical purity and with a specific radioactivity of ∼24,000 MBq μmol−1 at the end of the synthesis by N-methylation of the corresponding N-desmethyl derivative with [11C]iodomethane, as described previously by Pike et al. (1993).
[11C]Flumazenil scans were performed using an ECAT-953B PET camera in 3D mode (CTI/Siemens, Knoxville, TN, USA) with performance characteristics as described previously by Spinks et al. (1992). The axial field of view was 10.6 cm. The final image resolution (using a Hanning 0.5 filter) was 8.0×8.0×4.3 mm [at full width half maximum (FWHM)].
Subjects were positioned in the scanner such that the transaxial images were parallel to the intercommissural line (AC-PC line) and the majority of the cerebellum was scanned. A bolus injection of [11C]flumazenil (370 MBq, 10 mCi) in ∼2 ml was administered through an intravenous cannula sited in the dominant antecubital fossa vein. Thirty minutes after the start of the scan they received an i.v. infusion of midazolam (50 μg kg−1) over 5 min through an intravenous cannula sited in the non-dominant arm. We chose 50 μg kg−1 of midazolam since this dose produced the most robust effect in a previous study (Malizia et al. 1996).
Each subject had a radial arterial cannula in the non-dominant wrist to allow continuous counting of blood radioactivity concentration with a bismuth germanate (BGO) counter during the course of the experiment. Discrete samples were also taken at 4, 6, 8, 10, 20, 35, 50 and 65 min after injection to derive the metabolite-corrected plasma curve. Fractional concentrations of unchanged [11C]flumazenil and of less lipophilic radioactive metabolites were determined by solid phase extraction of plasma followed by high-performance liquid chromatography (HPLC). Samples were also taken at 5, 20, 35, 50 and 60 min after the start of the midazolam infusion and frozen for later measurement of total plasma midazolam levels using HPLC. The area under the curve (AUC) was then used to derive a measure of the amount of midazolam available during the scan (ng ml−1).
Twenty-six dynamic frames of data in 3D mode were acquired over 105 min (3×1, 19×3, 2 or 3×15 min; except for first three scans where only 2×15 min were acquired) and produced images containing 31 contiguous slices.
Image analysis
The methods used to analyze the resulting images described in Malizia et al. (1996) were slightly modified in this study.
The dynamic images were reconstructed with measured attenuation and dual energy window scatter corrections. Each reconstructed frame of [11C]flumazenil uptake acquired was analysed on a Sun SPARC workstation (Sun Microsystems, Mountain View, CA, USA) using Analyze AVW version 3.1 (Mayo Foundation; Robb and Hanson 1991). Regions of interest (ROI) were drawn on an individual volume of distribution maps of the GABA-BDZ receptor as labelled by [11C]flumazenil with reference to a stereotaxic atlas (Talairach and Tournoux 1988). The same ROI map was used on each dynamic image and moved to correct for any patient movement. The same ROI map was used for all the subjects. The ROIs were placed on the following regions: right/left (R/L) frontal, R/L orbitofrontal, anterior cingulate, and occipital cortices, thalamus and R/L cerebellum. Due to movement during the scan, the position of each ROI was checked on each frame manually, independently by two researchers (A.L.H., S.W.).
For each ROI, time activity curves (TACs) were analysed kinetically using a one-tissue compartment model with a fixed blood volume component [5%]. Estimates of K 1, the unidirectional clearance of [11C]flumazenil from plasma to brain, and k 2, the rate constant for efflux from tissue to plasma, were derived from least squared fits to data from the first 30 min until the midazolam infusion, i.e. pre-displacement (see Fig. 1). It was anticipated that occupancy of BDZ receptors by midazolam would lead to increased efflux of [11C]flumazenil from the brain compartment to plasma (rate constant, k 2d). To achieve an adequate fit for the remainder of the TAC, it was found necessary to include both a k 2d and also a further constant (k back) to fit its tail. The rate constants K 1, k 2 and k back were then fixed and the time activity curve after midazolam was fitted to determine k 2d. The displacement index was then defined as k 2d/k 2 and was taken as a measure of occupancy of midazolam at the benzodiazepine receptor.
Bottom panel: time activity head curve of [11C]flumazenil. Middle panel: concentration of midazolam. Top panel: EEG beta power activity. The infusion of midazolam at 30 min resulted in an increased efflux of [11C]flumazenil coincident with increased EEG beta power (marked with arrows). The graphs are from a typical study
Pharmacodynamic measures
EEG measurements
The EEG was measured continuously throughout the procedure, using silver–silver chloride electrodes placed on the scalp according to the International 10-20 system of electrode placement; recordings made from four channels, F4–C4, P4–O2, F3–C3 and P3–O1. Offline analysis was performed both visually and automatically for the whole period. Spectral analysis with fast Fourier transform was used to derive a measure of power for each 1-Hz band from 1 to 30 for epoch lengths of 77 s (Spike 2, Cambridge Electronic Design). After visual exclusion of epochs containing muscle and movement artefact, total power in each of the EEG bands (delta, 1–4 Hz, theta 4–8 Hz, alpha1 8–10 Hz, alpha2 10–13 Hz, beta1 13–18 Hz, beta2 18–30 Hz) was calculated for each epoch and plotted against time. Peak beta power and AUC were calculated for each subject, and was used as a prime EEG measure of midazolam’s effect, as has been described previously (Malizia et al. 1996). The ratio of the peak beta1 value at F4–C4 after midazolam infusion to that at baseline was used as the pharmacodynamic index.
In addition, the EEG was analysed visually and any sleep was scored according to Rechtschaffen and Kales (1968) criteria. All periods of stage 2 or deeper and lasting longer than 10 s were summed over the whole 60-min period following midazolam infusion and referred to as ‘total EEG sleep time’.
Saccadic eye movements
Saccadic eye movements to a target were measured as described by Ball et al. (1991) using electro-oculography. Only lateral saccades were studied. The subject was asked to fixate on a red light as it appeared on the screen mounted 67 cm on front of him. Data was then collected for 48 eye movements of 15–40° and a main sequence curve obtained, the measurement for peak velocity being the interpolation at 35°.
Anxiety and sedation
Anxiety and sedation were rated by the subjects at regular intervals (30 and 5 min prior to the injection of [11C]flumazenil, and at 15, 25, 35, 50, 65, 80, 90 min afterwards) using a visual analogue scale (1–100).
Cardiac monitoring
Systolic and diastolic blood pressure and heart rate were recorded at the same time points as ratings of anxiety and sedation.
Statistical analysis
Two-tailed Student’s t-test was used to determine differences in the means of other variables (midazolam levels, demographic details) or pharmacodynamic measures between the two groups. The relationship between clinical variables and pharmacokinetic or pharmacodynamic measures was examined using Pearson’s correlation. A repeated measures analysis of variance (ANOVA; with pharmacokinetic data as the dependent variable and regions as the repeated measure) with Greenhouse–Geisser correction using SPSS software (SPSS Inc, Chicago, IL, version 12.0.1) was used to determine whether there were any differences between the groups in any of the pharmacokinetic data (K 1, k 2, k 2d, K 1/k 2, k 2d/k 2) (Sargent et al. 2000). Due to incorrect positioning in the scanner, cerebellar data from one alcohol dependent and one control subject was missing; these were replaced by the mean value of the remainder of the subjects in the group. ANOVA was used to compare the rate constants pre- and post-midazolam, k 2 and k 2d, with Bonferroni correction for multiple comparisons.
Results
Subject details
The alcohol dependent and non-dependent groups were well matched with regard to age (all results presented as mean±SE, 44.45±1.8 and 46.2±2.6, respectively). Predictably, the severity of alcohol dependency questionnaire score for the alcohol dependent subjects was significantly (p<0.001) higher (36.5±3.2) than that for the non-dependent control subjects (4.1±1.8). The average number of years of heavy drinking in the alcohol dependent group was 20.1±2.0 years. No significant (p<0.05) differences were found between the groups in their scores on the BDI, Spielberger SSAI or STAI inventory. Unfortunately due to missing data, not all the questionnaires could be analysed, as described in Table 1.
Midazolam levels
No difference was seen in the plasma concentration of midazolam between the two groups (p<0.05). Only samples from seven alcohol dependent and nine non-dependent subjects were available for analysis due to technical difficulties. In alcohol dependent subjects, the area under the curve for midazolam was 453±50 ng ml−1, while in control subjects, 537±68 ng ml−1.
Pharmacokinetic measures: [11C]flumazenil image analysis
There was no difference in the AUC for levels of parent [11C]flumazenil between the two groups. In the alcohol dependent group, the AUC was 1,153±61% [11C]flumazenil in plasma min−1 and for control group, 1,122±51% [11C]flumazenil in plasma min−1.
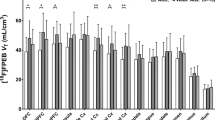
In the nine brain regions studied, K 1 was higher in the alcohol dependent group than in controls. However, a repeated measures ANOVA revealed that there was no main effect of group (F 1, 19=2.267, p>0.05), but there was a significant main effect of region (F 3.771, 71.646=p>0.05) on K 1. No significant group×region interaction (F 3.771, 71.646=0.620; p>0.05) was evident (see Table 2). In all brain regions the k 2 rate constant was higher in the alcohol dependent group compared with controls (see Table 2). A repeated measures ANOVA showed a significant main effect of group (F 1, 19=8.306, p>0.05) and of region (F 3.004, 57.076=248.1, p>0.05) but no significant group×region interaction (F3.004, 57.076=0.811; p>0.05). Post-hoc unpaired t-test revealed significant differences in k 2 between the control and alcohol dependent groups in thalamus, anterior cingulate, left orbitofrontal frontal and cerebellar regions (p>0.05).
The volume of distribution [V D] was calculated [K 1/k 2] and repeated measures ANOVA revealed that there were no significant main effect of group (F 1, 19=0.775; p>0.05) but a significant main effect of region (F 3.346, 63.566=123.5; p>0.05) on V D (see Table 2). There was no significant group×region interaction (F 3.346, 63.566=1.439; p>0.05). As expected though, in some brain regions, such as the orbitofrontal and anterior cingulate cortices, a reduction by 6–8% in GABA-BDZ receptor binding was seen in the alcohol dependent group compared with the control group.
In all brain regions studied, midazolam resulted in an increase in the rate of efflux of [11C]flumazenil as evidenced by the higher k 2d compared to k 2. In the control group, k 2d was significantly higher (p<0.0056 with Bonferroni correction) than k 2 in all regions except right and left cerebellum; although a significant difference (p<0.05) was found between k 2d and k 2 in the right and left orbitofrontal cortex, this did not survive Bonferroni correction. In the alcohol dependent group, k 2d was significantly higher (p<0.0056 with Bonferroni correction) in all regions except for the right and left cerebellum. Concerning k 2d, a repeated measures ANOVA revealed no main effect of group (F 1, 19=3.437, p>0.05), a main effect of region (F 4.204, 79.881=19.714, p<0.05) but no significant group×region interaction (F 4.204, 79.881=1.808; p>0.05) (see Table 2).
Although a higher displacement index (k 2d/k 2) was found in the alcohol dependent group compared with the control group in all brain regions, repeated measures ANOVA showed no main effect of group (F 1, 19=0.847, p>0.05), a main effect of region (F 3.041, 57.771=5.384, p<0.05) but no significant group×region interaction (F 3.041, 57.771=0.916; p>0.05) (see Table 2).
Pharmacodynamic measures
Visual analogue scales
After the midazolam infusion, the majority of the subjects were unable to respond to the request for a rating about how sedated or anxious they were feeling. Even for those that responded, their reply did not necessarily reflect the actual experience since the ratings of sedation were often inaccurate. For instance, subjects sometimes rated themselves very low for sleepiness immediately after being woken by the investigator asking for a response. They were often disorientated and forgetful of previous instructions. In general, however, the sleepiness scores were higher in the non-dependent control group. Due to the low numbers of responses, formal statistical analysis was not undertaken.
Cardiovascular effects
No significant differences were seen in systolic or diastolic blood pressure or heart rate between the groups nor during the procedure (results not shown, see Table 3).
Saccadic eye movements
Subjects were too drowsy at the initial time points after midazolam infusion to complete the task so analysis of the saccadic eye movement data to reflect benzodiazepine receptor function was not possible (see Table 3).
EEG
Sleep. Visual analysis revealed the expected change in the EEG. About halfway through the 5-min infusion, subjects usually closed their eyes, and later fell asleep, with the appearance of low amplitude mixed frequencies and marked rhythmic beta activity at 13–18 Hz. After an interval that varied from subject to subject, they fell asleep with sleep spindles and K complexes characteristic of stage 2 sleep. Subjects spent the rest of the scanning period either asleep or alternating between sleep and waking. EEG beta power and more specifically, drug-related beta1 power does not change during stage 1 and 2 sleep.
The time taken to fall asleep after midazolam infusion (sleep onset latency) was not significantly different in the two groups. However, the total EEG sleep time was significantly lower in the alcohol dependent group [mean±SE (one recording from the alcohol dependent group was uninterpretable due to artefact) alcohol dependent group: 15.7±4.3 min; control group: 33.5±3.8 min; p<0.05; see Fig. 2]. From visual inspection of the data, it was apparent that increasing midazolam AUCs were associated with longer sleep times in the control subjects but this relationship was not evident in the alcohol dependent subjects. However, the limited number of subjects in whom both these data were available precluded formal statistical comparison.
Midazolam resulted in significantly (p<0.05) less time asleep in the alcohol dependent group compared to the non-alcohol dependent group. Sleep was sleep scored according to Rechtschaffen and Kales (1968) criteria. All periods of stage 2 or deeper and lasting longer than 10 s were summed over the whole 60-min period following midazolam infusion
There was a significant correlation between sleep onset latency and score on the STAI (all subjects r=0.6, p<0.05; control r=0.5, p>0.05; alcohol dependent r=0.6, p>0.05), but not between total EEG sleep time (all subjects r=−0.2, p>0.05; control r=−0.2, p>0.05; alcohol dependent r=0.05, p>0.05), suggesting those that were more anxious took longer to show signs of sleep but anxiety did not affect total EEG sleep time. No other questionnaire measures were significantly related to sleep.
EEG betal power. Automatic analysis revealed that in all subjects there was an increase in beta1 power that began between 2 and 5 min into the midazolam infusion and remained increased for 30–60 min (see Fig. 3). One EEG recording in an alcohol dependent subject was uninterpretable due to artefact. There was no significant difference in beta1 power at baseline, and no significant difference in the change (peak/baseline) in EEG beta1 power after the midazolam infusion between the two groups, nor in power in the alpha and theta bands. The EEG beta1 power ratio in the alcohol dependent group was 2.79±0.85 and in the control group, 2.75±1.18. Areas under the curve were calculated for each patient and these also showed no difference between the two groups.
Relationship between pharmacokinetic and pharmacodynamic measures
The relationship between the brain pharmacokinetics of midazolam, i.e. displacement index as defined from the PET scan, and its functional effects was explored, i.e. EEG and sleep measures. There was no correlation between the displacement index and change in EEG beta1 power ratio or any indices of sleep. In addition, we looked at the relationship between plasma midazolam levels and absolute EEG beta1 power at the five time points during the scanning procedure. As expected in most individuals in both groups, there was a strong, significant correlation between EEG beta1 power and plasma midazolam levels supporting previous studies (e.g. Van Steveninck et al. 1993). There was no significant difference between the two groups in terms of these correlations.
Discussion
Using this [11C]flumazenil PET paradigm to directly measure the pharmacokinetics and pharmacodynamics of midazolam at the brain benzodiazepine receptor, we have shown that alcohol dependence is associated with reductions in a pharmacodynamic response (EEG sleep time) in the absence of reduced brain receptor occupancy (indeed, slightly greater receptor occupancy in the alcohol dependent group was seen). This clearly demonstrates reduced sensitivity to this action of the benzodiazepine receptor agonist, midazolam, in alcohol dependence. We found no differences in another index of benzodiazepine function, EEG beta1 power.
This study was technically challenging to perform, requiring simultaneous acquisition of PET imaging and EEG data in one session before and after an infusion of midazolam. Associated movement artefact and loss of arterial input function resulted in the rejection of almost a fifth of the scans obtained (five of 26). Nevertheless, acquiring scan data in a single scan protocol has significant advantages over a two-scan protocol when the volunteers are difficult to recruit and may not tolerate two scans. Videbaek et al. (1993) used a two-scan SPECT [123I]iomazenil protocol to measure the pharmacokinetics of midazolam and ran into difficulties. Subjects fell asleep with the midazolam infusion (6 mg h−1 compared to 3.5 mg bolus in our study), some not waking throughout the procedure and spending the night in intensive care as a precaution. Such an approach does not therefore lend itself to wider clinical experimental use.
The rate constants derived in our present study for the control population are similar to those found by Malizia et al. (1996). Alcohol dependence has been commonly reported to be associated with reduced blood flow and metabolism (Volkow et al. 1992; Adams et al. 1993; Gilman et al. 1996). However, we found no evidence of reduced blood flow since the rate constant K 1 was not lower in the alcohol dependent group compared to control group. Our patients were all abstinent for at least 6 weeks and this likely contributed to the blood flows in the two groups being similar. A study comparable to the present one using patients abstinent for 2 months reported no significant reduction in metabolism, whereas it has been reported in studies using patients abstinent up to about 1 month (Nicolas et al. 1993; Volkow et al. 1994).
Alcohol dependent patients had slightly fewer GABA-BDZ receptors in some brain regions compared to the control group. Lower benzodiazepine receptor levels would be consistent with other studies showing reduced levels of the GABA-BDZ receptor (Lingford-Hughes et al. 1998; Abi-Dargham et al. 1998). The protocol we used was optimal for determining the pharmacokinetics of midazolam at the benzodiazepine receptor rather than the volume of distribution (V D) and so the full [11C]flumazenil washout curve was not available for calculation of V D as in routine neuroimaging protocols. This likely contributed to a probable underestimation and may have reduced our sensitivity to detect group differences (see Lassen et al. 1995).
Several important kinetic factors that could have contributed to the displacement index (k 2/k 2) were considered. Similar to other studies, we could find no evidence that the metabolism of [11C]flumazenil or midazolam was altered in our alcohol dependent patients who were medically, neurologically and cognitively healthy (Abi-Dargham et al. 1998; Bauer et al. 1997). Although we did not measure its major active metabolite, α-hydroxymidazolam, relatively low concentrations of this metabolite have been reported when midazolam is given i.v. as in the present study (Mandema et al. 1992). Changes in blood flow secondary to midazolam will influence the measured rate (k 2d) of efflux of [11C]flumazenil and midazolam has been shown to reduce blood flow in a dose-dependent manner. Veselis et al. (1997) reported that midazolam at doses two to three times higher than in the present study (7.5–9.7 mg compared with 3.5 mg/70 kg) reduced global blood flow by 12%. Therefore in the present study, a smaller reduction is likely and results in a reduced rate of efflux of [11C]flumazenil. This would reduce the likelihood of detecting a difference between the rate constant pre- (k 2) and post-midazolam (k 2d) due to benzodiazepine receptor occupancy by midazolam and of detecting a difference in the displacement index (k 2d/k 2) between the groups.
We found that time spent asleep, as determined by EEG, was significantly different between groups, with alcohol dependent subjects asleep for half the time of that seen in the control group, despite no reduction in occupancy of the benzodiazepine receptor by midazolam. In their study Bauer et al. (1997) found that the same amount of midazolam was required for sleep induction but did not report time asleep. Elsewhere, abstinent alcohol dependence has been reported to be associated with sleep disturbance (Currie et al. 2003). We did not collect detailed information about sleep patterns in our patients, and so cannot fully exclude the possibility that the alcohol dependent group may have had a greater level of ‘pre-existing’ sleep disturbance that contributed to the reduced sedative effects of midazolam seen. In addition, whilst we believe that the benzodiazepine receptor is critical in midazolam induced sleep, we are not able to exclude a contribution from other neurotransmitters involved in modulating sleep (see Brower 2001). However, our finding that alcohol dependence is associated with substantially less time asleep is consistent with pre-clinical models of alcohol dependence, where reduced anaesthetic effect of diazepam and pentobarbital, but not thiopental, have been reported (Newman et al. 1986; Curran et al. 1988; Doudet et al. 1995). In human alcohol dependence, tolerance to anaesthetic agents working through the GABAA receptor (thiopental, propofol) has been reported, including requiring higher doses and shorter time spent asleep, though not consistently (Loft et al. 1982, 1983; Swerdlow et al. 1990; Fassoulaki et al. 1993).
The reduced EEG sleep time seen was in contrast to finding no differences in the other selected benzodiazepine pharmacodynamic indices, saccadic eye movements and EEG beta1 power. We did not find that alcohol dependence was associated with any alteration in baseline EEG or saccadic eye movement parameters or in the effect of midazolam on EEG beta1 power or saccadic eye movements although the data available on the latter was limited due to sedation. Other studies have also reported limited changes in measures typically considered to reflect benzodiazepine receptor function such as no difference in the dose of midazolam required to sedate alcohol dependent (abstinent for 2–3 weeks) and control subjects, nor in EEG responses, including beta power (Ciraulo et al. 1997; Bauer et al. 1997). We chose EEG beta power since it is a well-recognised and validated index of benzodiazepine function (Domino et al. 1989; Feshchenko et al. 1997). Although we found a significant correlation between plasma midazolam levels at the five time points during the scanning procedure and absolute EEG beta1 power, we did not find a significant correlation of EEG beta1 power ratio (peak/baseline) with midazolam occupancy, i.e. displacement index derived from the PET image as Malizia et al. (1996) did using this PET protocol. We believe that we did not see a correlation between brain occupancy and EEG beta1 power ratio since we only used a single dose of midazolam and so had a narrower range of plasma concentrations and effects than in Malizia et al.’s (1996) study, which used three doses of midazolam. In addition, the displacement index gives a single value for each subject which represents the entire period of the central effects of midazolam. We suspect this did not correlate with EEG beta1 power ratio (peak/baseline) because the latter is predominantly determined by the initial rise in midazolam concentrations. Such a lack of attenuation of drug induced EEG beta power in alcohol dependence is consistent with a study showing no attenuation of beta power after chronic benzodiazepine administration (Lee and Lader 1988).
Given the profound differences in midazolam-induced sleep EEG activity, why is reduced sensitivity not seen with all benzodiazepine pharmacodynamic measures? The reason for this is unclear but probably reflects the fact that a number of different subtypes of the GABA-BDZ exist, each of which appears to have a particular association with a specific function (Mohler et al. 2002). For instance, the α1 containing subtype is involved in mediating the sleep promoting effects of benzodiazepines and alcohol (Blednov et al. 2003). We know from animal studies that chronic alcohol exposure differentially affects subunit expression in different brain regions (see Kumar et al. 2004) and our finding of reduced sleep time would therefore be consistent with reports from animal models that chronic alcohol exposure in rat brain leads to reduced levels of the α1 subunit (Montpied et al. 1991). In man, subunit changes have not been systematically investigated with post-mortem studies so far showing increased or no changes in α1 and α3 polypeptide and diazepam-sensitive (α1, α2, α3, α5) benzodiazepine receptor levels in various parts of the cortex (Tran et al. 1981; Dodd et al. 1992; Lewohl et al. 1997, 2001; Mitsuyama et al. 1998). It is not clear which subtype or subtypes are involved in saccadic eye movements or EEG beta-power although recent evidence suggests a role for the α2 subtype in EEG beta frequency (Edenberg et al. 2004). This study cannot inform the important question about which subtypes may be different in alcohol dependence in man since midazolam is an agonist at the α1, α2, α3 and α5 subtypes and [11C]flumazenil is a non-selective ligand (Lingford-Hughes et al. 2002).
In addition, whilst it is clear that chronic alcohol exposure can alter the benzodiazepine receptor subunit profile, it is not apparent what happens in prolonged abstinence or indeed if any of the changes reported in man pre-dated their abuse of alcohol. Previous neuroimaging studies that showed reduced GABA-benzodiazepine receptor levels in alcohol dependence could not determine whether this reduction was secondary to alcohol consumption (Lingford-Hughes et al.1998; Abi-Dargham et al. 1998). There is evidence from neuroimaging and pharmacological challenge studies in people with a family history of alcoholism supporting the hypothesis that reduced GABA-benzodiazepine receptor function is involved in mediating vulnerability to alcoholism (Volkow et al. 1995; Cowley et al. 1994; Sarid-Segal et al. 2000), as well as more recent genetic studies (Loh et al. 1999; Edenberg et al. 2004). In the current study, only two subjects in each group had a family history of alcoholism suggesting that the differences seen here are more likely to be as a result of their alcohol consumption.
In conclusion, the objective of this study was to simultaneously assess the pharmacokinetics and pharmacodynamics of midazolam at the benzodiazepine receptor in man to test the hypothesis that alcohol dependence is associated with reduced benzodiazepine receptor function. Whilst we achieved this, the experiment was challenging to conduct and the sensitivity of the paradigm may not have been great enough to detect differences between two groups of subjects. We acknowledge that the statistical power of the study is limited; however, power calculations revealed that for some parameters derived from this data, an inappropriately large number of subjects would have to be scanned. Nevertheless, we showed that alcohol dependence in man is associated with decreased midazolam induced time asleep, in the absence of reduced occupancy of the benzodiazepine receptor. We propose that this reduced sensitivity in alcohol dependence may reflect a difference in the subunit profile of their GABA-BDZ receptors, either as part of their vulnerability to or as a consequence of their alcohol dependence.
References
Abi-Dargham A, Krystal JH, Anjilvel S, Scanley BE, Zoghbi S, Baldwin RM, Rajeevan N, Ellis S, Petrakis IL, Seibyl JP, Charney DS, Laruelle M, Innis RB (1998) Alterations of benzodiazepine receptors in type II alcoholic subjects measured with SPECT and (123I)iomazenil. Am J Psychiatry 155(11):1550–1555
Adams KM, Gilman S, Koeppe RA, Kluin KJ, Brunberg JA, Dede D, Berent S, Kroll PD (1993) Neuropsychological deficits are correlated with frontal hypometabolism in positron emission tomography studies of older alcoholic patients. Alcohol Clin Exp Res 17(2):205–210
Ball DM, Glue P, Wilson S, Nutt DJ (1991) Pharmacology of saccadic eye movements in man. 1. Effects of the benzodiazepine receptor ligands midazolam and flumazenil. Psychopharmacology 105:361–367
Bauer LO, Gross JB, Meyer RE, Greenblatt DJ (1997) Chronic alcohol abuse and the acute sedative and neurophysiologic effects of midazolam. Psychopharmacology 133(3):293–299
Beck AT, Brown G, Epstein N, Steer RA (1961) An inventory for measuring depression. Arch Gen Psychiatry 53:225–231
Blednov YA, Jung S, Alva H, Wallace D, Rosahl T, Whiting PJ, Harris RA (2003) Deletion of the alpha1 or beta2 subunit of GABAA receptors reduces actions of alcohol and other drugs. J Pharmacol Exp Ther 304(1):30–36
Brower KJ (2001) Alcohol’s effects on sleep in alcoholics. Alcohol Res Health 25(2):110–125
Bruce DL (1983) Alcoholism and anesthesia. Anesth Analg 62(1):84–96
Buck KJ, Harris RA (1990) Benzodiazepine agonist and inverse agonist actions on GABAA receptor-operated chloride channels. II. Chronic effects of ethanol. J Pharmacol Exp Ther 253:713–719
Ciraulo DA, Barnhill JG, Ciraulo AM, Sarid-Segal O, Knapp C, Greenblatt DJ, Shader R (1997) Alterations in pharmacodynamics of anxiolytics in abstinent alcoholic men: subjective responses, abuse liability, and electroencephalographic effects of alprazolam, diazepam, and buspirone. J Clin Pharmacol 37(1):64–73
Cowley DS, Roy-Byrne PP, Radant A, Hommer DW, Greenblatt DJ, Vitaliano PP, Godon C (1994) Eye movement effects of diazepam in sons of alcoholic fathers and male control subjects. Alcohol Clin Exp Res 18(2):324–332
Curran MA, Newman LM, Becker GL (1988) Barbiturate anesthesia and alcohol tolerance in a rat model. Anesth Analg 67(9):868–871
Currie SR, Clark S, Rimac S, Malhotra S (2003) Comprehensive assessment of insomnia in recovering alcoholics using daily sleep diaries and ambulatory monitoring. Alcohol Clin Exp Res 27(8):1262–1269
Devaud LL, Smith FD, Grayson DR, Morrow AL (1995) Chronic ethanol consumption differentially alters the expression of gamma-aminobutyric acidA receptor subunit mRNAs in rat cerebral cortex: competitive, quantitative reverse transcriptase-polymerase chain reaction analysis. Mol Pharmacol 48:861–868
Dodd PR, Thomas GJ, Harper CG, Kril JJ (1992) Amino acid neurotransmitter receptor changes in cerebral cortex in alcoholism: effect of cirrhosis of the liver. J Neurochem 59(4):1506–1515
Domino EF, French J, Pohorecki R, Galus CF, Pandit SK (1989) Further observations on the effects of subhypnotic doses of midazolam in normal volunteers. Psychopharmacol Bull 25(3):460–465
Doudet D, Hommer D, Higley JD, Andreason PJ, Moneman R, Suomi SJ, Linnoila M (1995) Cerebral glucose metabolism, CSF 5-HIAA levels, and aggressive behavior monkeys. Am J Psychiatry 152(12):1782–1787
Edenberg HJ, Dick DM, Xuei X, Tian H, Almasy L, Bauer LO, Crowe RR, Goate A, Hesselbrock V, Jones K, Kwon J, Li TK, Nurnberger JI Jr, O’Connor SJ, Reich T, Rice J, Schuckit MA, Porjesz B, Foroud T, Begleiter H (2004) Variations in GABRA2, encoding the alpha 2 subunit of the GABA(A) receptor, are associated with alcohol dependence and with brain oscillations. Am J Hum Genet 74(4):705–714
Fassoulaki A, Farinotti R, Servin F, Desmonts JM (1993) Chronic alcoholism increases the induction dose of propofol in humans. Anesth Analg 77(3):553–556
Feshchenko VA, Veselis RA, Reinsel RA (1997) Comparison of the EEG effects of midazolam, thiopental, and propofol: the role of underlying oscillatory systems. Neuropsychobiology 35(4):211–220
Freund G, Ballinger WE Jr (1988) Decrease of benzodiazepine receptors in frontal cortex of alcoholics. Alcohol 5(4):275–282
Gilman S, Koeppe RA, Adams K, Johnson-Grenne D, Junck L, Kliun KJ, Brunberg J, Martorello S, Lohman M (1996) Positron emission tomographic studies of cerebral benzodiazepine-receptor binding in chronic alcoholics. Ann Neurol 40(2):163–171
Grobin AC, Matthews DB, Devaud LL, Morrow AL (1998) The role of GABA(A) receptors in the acute and chronic effects of ethanol. Psychopharmacology 139(1–2):2–19
Hommer DW, Matsuo V, Wolkowitz O, Chrousos G, Greenblatt DJ, Weingartner H, Paul SM (1986) Benzodiazepine sensitivity in normal human subjects. Arch Gen Psychiatry 43(6):542–551
Korpi ER, Uusi-Oukari M, Wegelius K, Casanova M, Zito M, Kleinman JE (1992) Cerebellar and frontal cortical benzodiazepine receptors in human alcoholics and chronically alcohol-drinking rats. Biol Psychiatry 31(8):774–786
Kugaya A, Sanacora G, Verhoeff NP, Fujita M, Mason GF, Seneca NM, Bozkurt A, Khan SA, Anand A, Degen K, Charney DS, Zoghbi SS, Baldwin RM, Seibyl JP, Innis RB (2003) Cerebral benzodiazepine receptors in depressed patients measured with (123I)iomazenil SPECT. Biol Psychiatry 54(8):792–799
Kumar S, Fleming RL, Morrow AL (2004) Ethanol regulation of gamma-aminobutyric acid A receptors: genomic and nongenomic mechanisms. Pharmacol Ther 101(3):211–226
Lassen NA, Bartenstein PA, Lammertsma AA, Prevett MC, Turton DR, Luthra SK, Osman S, Bloomfield PM, Jones T, Patsalos PN et al (1995) Benzodiazepine receptor quantification in vivo in humans using (11C)flumazenil and PET: application of the steady-state principle. J Cereb Blood Flow Metab 15(1):152–165
Lee A, Lader M (1988) Tolerance and rebound during and after short-term administration of quazepam, triazolam and placebo to healthy volunteers. Int Clin Psychopharmacol 3:31–47
Lewohl JM, Crane DI, Dodd PR (1997) Expression of the alpha 1, alpha 2 and alpha 3 isoforms of the GABAA receptor in human alcoholic brain. Brain Res 751(1):102–112
Lewohl JM, Huygens F, Crane DI, Dodd PR (2001) GABA(A) receptor alpha-subunit proteins in human chronic alcoholics. J Neurochem 78(3):424–434
Lingford-Hughes AR, Acton PD, Gacinovic S, Suckling J, Busatto GF, Boddington SJ, Bullmore E, Woodruff PW, Costa DC, Pilowsky LS, Ell PJ, Marshall EJ, Kerwin RW (1998) Reduced levels of GABA-benzodiazepine receptor in alcohol dependency in the absence of grey matter atrophy. Br J Psychiatry 173:116–122
Lingford-Hughes A, Hume SP, Feeney A, Hirani E, Osman S, Cunningham VJ, Pike VW, Brooks DJ, Nutt DJ (2002) Imaging the GABA-benzodiazepine receptor subtype containing the alpha5-subunit in vivo with (11C)Ro15 4513 positron emission tomography. J Cereb Blood Flow Metab 22(7):878–889
Loft S, Jensen V, Rorsgaard S, Dyrberg V (1982) Influence of moderate alcohol intake on thiopental anesthesia. Acta Anaesthesiol Scand 26(1):22–26
Loft S, Jensen V, Rorsgaard S (1983) Influence of moderate alcohol intake on wakening plasma thiopental concentration. Acta Anaesthesiol Scand 27(3):266–269
Loh EW, Smith I, Murray R, McLaughlin M, McNulty S, Ball D (1999) Association between variants at the GABAAbeta2, GABAAalpha6 and GABAAgamma2 gene cluster and alcohol dependence in a Scottish population. Mol Psychiatry 4(6):539–544
Malizia AL, Gunn RN, Wilson SJ, Waters SH, Bloomfield PM, Cunningham VJ, Nutt DJ (1996) Benzodiazepine site pharmacokinetic/pharmacodynamic quantification in man: direct measurement of drug occupancy and effects on the human brain in vivo. Neuropharmacology 35(9–10):1483–1491
Mandema JW, Tuk B, van Steveninck AL, Breimer DD, Cohen AF, Danhof M (1992) Pharmacokinetic–pharmacodynamic modeling of the central nervous system effects of midazolam and its main metabolite alpha-hydroxymidazolam in healthy volunteers. Clin Pharmacol Ther 51(6):715–728
Mhatre MC, Ticku MK (1992) Chronic ethanol administration alters gamma-aminobutyric acidA receptor gene expression. Mol Pharmacol 42(3):415–422
Mitsuyama H, Little KY, Sieghart W, Devaud LL, Morrow AL (1998) GABA(A) receptor alpha1, alpha4, and beta3 subunit mRNA and protein expression in the frontal cortex of human alcoholics. Alcohol Clin Exp Res 22(4):815–822
Mohler H, Fritschy JM, Rudolph U (2002) A new benzodiazepine pharmacology. J Pharmacol Exp Ther 300(1):2–8
Montpied P, Morrow AL, Karanian JW, Ginns EI, Martin BM, Paul SM (1991) Prolonged ethanol inhalation decreases gamma-aminobutyric acidA receptor alpha subunit mRNAs in the rat cerebral cortex. Mol Pharmacol 39(2):157–163
Newman LM, Curran MA, Becker GL (1986) Effects of chronic alcohol intake on anesthetic responses to diazepam and thiopental in rats. Anesthesiology 65(2):196–200
Nicolas JM, Catafau AM, Estruch R, Lomena FJ, Salamero M, Herranz R, Monforte R, Cardenal C, Urbano-Marquez A (1993) Regional cerebral blood flow-SPECT in chronic alcoholism: relation to neuropsychological testing. J Nucl Med 34(9):1452–1459
Nutt DJ (1999) Alcohol and the brain: pharmacological insights for psychiatrists. Br J Psychiatry 175:114–119
Nutt DJ, Malizia AL (2001) New insights into the role of the GABA(A)-benzodiazepine receptor in psychiatric disorder. Br J Psychiatry 179:390–396
Pike VW, Halldin C, Crouzel C, Barre L, Nutt DJ, Osman S, Shah F, Turton DR, Waters SL (1993) Radioligands for PET studies of central benzodiazepine receptors and PK (peripheral benzodiazepine) binding sites—current status. Nucl Med Biol 20(4):503–525
Rechtschaffen A, Kales A (1968) A manual of standarized terminology, techniques and scoring system for sleep stages in human subjects. US Government Printing Office, Washington, DC
Robb RA, Hanson DP (1991) A software system for interactive and quantitative visualization of multidimensional biomedical images. Australas Phys Eng Sci Med 14:9–30
Sargent PA, Kjaer KH, Bench CJ, Rabiner EA, Messa C, Meyer J, Gunn RN, Grasby PM, Cowen PJ (2000) Brain serotonin1A receptor binding measured by positron emission tomography with (11C)WAY-100635: effects of depression and antidepressant treatment. Arch Gen Psychiatry 57(2):174–180
Sarid-Segal O, Knapp CM, Ciraulo AM, Greenblatt DJ, Shader RI, Ciraulo DA (2000) Decreased EEG sensitivity to alprazolam in subjects with a parental history of alcoholism. J Clin Pharmacol 40(1):84–90
Spielberger CD (1983) Manual for state–trait anxiety inventory. Consulting Psychologists Press, Palo Alto, CA
Spinks TJ, Jones T, Bailey DL, Townsend DW, Grootoonk S, Bloomfield PM, Gilardi MC, Casey ME, Sipe B, Reed J (1992) Physical performance of a positron tomograph for brain imaging with retractable septa. Phys Med Biol 37(8):1637–1655
Stockwell T, Murphy D, Hodgson R (1983) The severity of alcohol dependence questionnaire: its use, reliability and validity. Br J Addict 78(2):145–155
Suzdak PD, Schwartz RD, Skolnick P, Paul SM (1986) Ethanol stimulates gamma-aminobutyric acid receptor-mediated chloride transport in rat brain synaptoneurosomes. Proc Natl Acad Sci U S A 83(11):4071–4075
Swerdlow BN, Holley FO, Maitre PO, Stanski DR (1990) Chronic alcohol intake does not change thiopental anesthetic requirement, pharmacokinetics, or pharmacodynamics. Anesthesiology 72(3):455–461
Talairach J, Tournoux P (1988) Co-planar stereotaxic atlas of the human brain. Thieme Medical Publisher, New York, 132pp
Tran VT, Snyder SH, Major LF, Hawley RJ (1981) GABA receptors are increased in brains of alcoholics. Ann Neurol 9(3):289–292
Van Steveninck AL, Mandema JW, Tuk B, Van Dijk JG, Schoemaker HC, Danhof M, Cohen AF (1993) A comparison of the concentration–effect relationships of midazolam for EEG-derived parameters and saccadic peak velocity. Br J Clin Pharmacol 36(2):109–115
Veselis RA, Reinsel RA, Beattie BJ, Mawlawi OR, Feshchenko VA, DiResta GR, Larson SM, Blasberg RG (1997) Midazolam changes cerebral blood flow in discrete brain regions: an H2(15)O positron emission tomography study. Anesthesiology 87(5):1106–1117
Videbaek C, Friberg L, Holm S, Wammen S, Foged C, Andersen JV, Dalgaard L, Lassen NA (1993) Benzodiazepine receptor equilibrium constants for flumazenil and midazolam determined in humans with the single photon emission computer tomography tracer (123I)iomazenil. Eur J Pharmacol 249(1):43–51
Volkow ND, Hitzemann R, Wang GJ, Fowler JS, Burr G, Pascani K, Dewey SL, Wolf AP (1992) Decreased brain metabolism in neurologically intact healthy alcoholics. Am J Psychiatry 149(8):1016–1022
Volkow ND, Wang GJ, Hitzemann R, Fowler JS, Overall JE, Burr G, Wolf AP (1994) Recovery of brain glucose metabolism in detoxified alcoholics. Am J Psychiatry 151(2):178–183
Volkow ND, Wang GJ, Begleiter H, Hitzemann R, Pappas N, Burr G, Pascani K, Wong C, Fowler JS, Wolf AP (1995) Regional brain metabolic response to lorazepam in subjects at risk for alcoholism. Alcohol Clin Exp Res 19(2):510–516
Volkow ND, Wang GJ, Overall JE, Hitzemann R, Fowler JS, Pappas N, Frecska E, Piscani K (1997) Regional brain metabolic response to lorazepam in alcoholics during early and late alcohol detoxification. Alcohol Clin Exp Res 21(7):1278–1284
Acknowledgements
We are grateful to Dr. Mike Franklin, Oxford for measurement of midazolam, all staff at Hammersmith Imanet Ltd. (formerly MRC Cyclotron Unit) but particularly Safiye Osman, Jo Holmes, and Andy Blythe, Mr. Lindsay Taylor, University of Bristol and all staff and patients at the Robert Smith Unit, Bristol and ACAD, Weston-super-Mare. This study was funded by an MRC Programme Grant, G9515859.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lingford-Hughes, A.R., Wilson, S.J., Cunningham, V.J. et al. GABA-benzodiazepine receptor function in alcohol dependence: a combined 11C-flumazenil PET and pharmacodynamic study. Psychopharmacology 180, 595–606 (2005). https://doi.org/10.1007/s00213-005-2271-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-005-2271-x