Abstract
Objectives
The effect of gender and female menstrual cycle on human striatal dopamine transporters (DATs) was investigated with single-photon emission computed tomography (SPECT) using the ligand 2β-carbomethoxy-3β-(4-[123I]iodophenyl)tropane.
Methods
Ten female subjects aged 18–40 years (25.3±7.3 years) were scanned twice during the early follicular and the mid-luteal phases to detect any hormone-mediated changes in DAT availability in the striatum or serotonin transporter (SERT) availability in brainstem–diencephalon. Plasma estradiol and progesterone levels were obtained at the time of SPECT and confirmed the expected increases from the follicular to the luteal phases. Finally, in a post hoc analysis of a previously published healthy-subject sample, striatal DAT availability was compared between 70 male and 52 female subjects who ranged in age from 18 to 88 years.
Results
In the ten menstrual cycle subjects, DAT availability (V3″) in striatum and SERT availability in brainstem–diencephalon did not differ between follicular and luteal phases. Moreover, change in V3″ for striatum or brainstem–diencephalon was uncorrelated with change in plasma estradiol or progesterone from the follicular to the luteal phase. In the larger healthy-subject sample, there was no significant effect of gender or the interaction of age and gender on striatal V3″.
Conclusions
These findings suggest that in using DAT or SERT ligands in the study of neuropsychiatric disorders, matching of female subjects according to a menstrual cycle phase is unnecessary. Although the present investigation did not confirm previous reports of gender differences in striatal DAT availability, controlling for gender in such studies still seems advisable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A growing body of research has examined the modulation of brain dopaminergic systems by estrogen and other sex steroids (for a review, see Di Paolo 1994). A number of neuropsychiatric disorders thought to be linked to dopaminergic neurotransmission exhibit gender differences such as Parkinson's disease (Kuopio et al. 1999), schizophrenia (Seeman 1982), and substance abuse (Brady et al. 1993; Sofuoglu et al. 1999). Moreover, many of these same disorders may show menstrual cycle effects among female subjects. For example, the phase of menstrual cycle has been observed to influence psychotic symptoms in women with schizophrenia (Seeman 1996) as well as subjective effects of cocaine in female cocaine users (Sofuoglu et al. 1999).
Whether alterations in specific dopaminergic elements underlie these clinical phenomena is unclear. Autoradiographic studies in rats with the ligand [3H]GBR-12935 have demonstrated higher striatal dopamine transporter (DAT) density in intact females than in males (Morissette and Di Paolo 1993; Rivest et al. 1995) or ovariectomized females (Bossé et al. 1997; Morissette and Di Paolo 1993). Striatal DAT density has also been shown to fluctuate during the female estrous cycle (Morissette and Di Paolo 1993), with the peaking of the B max at proestrus coinciding with the time of peak levels of striatal dopamine. Conversely, rodent studies have not shown significant gender differences in adult levels of striatal D1 and D2 receptors (Andersen et al. 1997). Human postmortem studies of gender differences in DAT and dopamine receptor concentrations are comparatively lacking.
With the advent of functional neuroimaging, it has become possible to probe the effects of hormones on neural systems in living subjects. Two positron emission tomography (PET) imaging groups have examined the relationship between female menstrual cycle and one dopaminergic element—the D2 receptor. Wong et al. (1988) studied fluctuations of the binding rate constant k 3 using (3-N-[11C]-methyl)spiperone ([11C]NMSP) in the caudate during the menstrual cycle in six healthy women. They observed a trend for a slight increase in k 3 between the follicular and the luteal phases. Nördstrom et al. (1998) examined four healthy women with [11C]raclopride at two different phases of their menstrual cycle and found no cycle-dependent variation in D2 receptor density in the putamen. To date, no study has investigated the effect of the female menstrual cycle on DAT availability in humans.
Several previous in vivo imaging studies have explored the effect of gender on dopamine receptors and DATs. PET studies that have examined male–female differences in D2-like dopamine receptor binding potentials or densities have reported higher values in women in the anterior cingulate cortex using [11C]FLB 457 (Kaasinen et al. 2001), but not in the striatum using [11C]raclopride (Farde et al. 1995; Pohjalainen et al. 1998). A number of previous single-photon emission computed tomography (SPECT) studies have analyzed the effect of gender on striatal DATs (van Dyck et al. 1995; Kuikka et al. 1997; Lavalaye et al. 2000; Mozley et al. 2001; Staley et al. 2001) and have found either no gender differences in DAT availability (van Dyck et al. 1995; Kuikka et al. 1997) [but greater spatial heterogeneity of striatal tracer uptake in females (Kuikka et al. 1997)] or increased DAT binding in women (Lavalaye et al. 2000; Mozley et al. 2001; Staley et al. 2001).
2β-Carbomethoxy-3β-(4-[123I]iodophenyl)tropane ([123I]β-CIT) is a potent cocaine analog with a high affinity for the DAT (Boja et al. 1991; Carroll et al. 1991) and the serotonin transporter (SERT) (Neumeyer et al. 1991). In humans and nonhuman primates, the tracer concentrates in striatum, diencephalon, and brainstem (Innis et al. 1993; Laruelle et al. 1993; Seibyl et al. 1994). Pharmacological characterization of regional [123I]β-CIT uptake has indicated that striatal activity is associated almost exclusively with DAT, whereas binding in brainstem and diencephalon is specific for the SERT (Laruelle et al. 1993). [123I]β-CIT has shown good test–retest reproducibility (Seibyl et al. 1996). As a ligand of DATs, it has shown promise as a research tool in idiopathic Parkinson's disease (Innis et al. 1993; Seibyl et al. 1995), cocaine addiction (Malison et al. 1998a), alcoholism (Tiihonen et al. 1995), Tourette's syndrome (Malison et al. 1995), attention deficit hyperactivity disorder (ADHD) (van Dyck et al. 2002a), schizophrenia (Laruelle et al. 2000), and healthy aging (van Dyck et al. 1995, 2002b). As a ligand of SERTs, it has shown additional research potential in depression (Malison et al. 1998b), cocaine addiction (Jacobsen et al. 2000), alcoholism (Heinz et al. 1998), and healthy aging (van Dyck et al. 2000). In clinical research, however, an understanding of the effects of gender and female menstrual cycle on [123I]β-CIT binding is essential for subject selection and experimental design.
In the present study, we examined the effect of the female menstrual cycle phase on DAT availability in the striatum. Since uptake of tracer in brainstem–diencephalon is associated primarily with the SERT, we also analyzed the relationship between menstrual cycle and SERT binding in this brain region.
Finally, in a larger healthy-subject sample that has been previously published (van Dyck et al. 2000, 2002b), we conducted a secondary post hoc analysis of the effect of gender on striatal DAT availability. The lack of an effect of gender on central SERT availability by [123I]β-CIT has been previously reported for this sample (van Dyck et al. 2000) and is not reanalyzed here. Briefly, that analysis showed that SERT availability in brainstem–diencephalon declined by 29.5% over the age range 18–88, or approximately 4.2% per decade. However, the addition of gender (with or without the interaction of age and gender) did not significantly improve the prediction of V3″ after controlling for the contribution of age, nor was there an effect of gender when premenopausal (<50 years) and postmenopausal age ranges were examined separately.
Methods
Subjects
The primary study population consisted of ten female subjects aged 18–40 years (25.3±7.3 years; seven Caucasian, two Asian, and one African-American). These subjects participated in a menstrual cycle study in which they were scanned twice, during the early follicular phase (days 5–7 of the cycle, counting the first day of menses as day 1) and during the mid-luteal phase (days 4–9 after the luteinizing hormone (LH) surge, counting the day of the positive result as day 1). All menstrual cycle subjects had regular predictable menstrual cycles (varying by 3 days or less, ranging from 25 to 32 days in duration; 28.9±2.1) and had not received oral contraceptives or any other hormonal therapy within the preceding 6 months. They were asked to keep a careful menstrual calendar and to use a urine LH test kit (Ovu-Quick; Quidel Corp., San Diego, CA) daily for several days prior to their anticipated LH surge (beginning at cycle days 9–11 for the women in this sample, based on individual cycle length). To avoid a potential order effect, SPECT scans were counterbalanced such that approximately half of the subjects were scanned initially during the follicular phase (six subjects), and the other half was scanned during the luteal phase (four subjects). Subjects were scanned during the same or consecutive menstrual cycles insofar as possible (eight of ten cases). The interscan interval ranged from 14 to 114 days (35±39). At the time of follicular- and luteal-phase SPECT (specifically, immediately prior to [123I]β-CIT injection or about 24 h prior to scanning), blood samples were drawn for measurement of plasma estradiol and progesterone concentrations by a double-antibody radioimmunoassay using a commercial kit (Biodata Corporation, Rome, Italy).
In addition, a larger healthy-subject population published previously (van Dyck et al. 2000, 2002b) was reanalyzed post hoc for possible gender effects. This secondary population consisted of 122 healthy volunteers (70 males and 52 females) whose ages ranged from 18 to 88 (46±19 years; 101 Caucasians, 10 African-Americans, 8 Asians, and 3 Hispanics). Those subjects who were at least 55 years of age (n=31) were also required to have no significant evidence of cognitive impairment as indicated by a Folstein Mini-Mental State Examination (MMSE) (Folstein et al. 1975) score of at least 27. Those subjects who were at least 68 years old (n=25) were required to have a normal brain magnetic resonance imaging (MRI) scan. No subject was taking medication that is known to affect the brain dopamine or serotonin systems, and no female subject was taking oral contraceptives or hormone replacement therapy. The present study population is a subset of the sample (N=126) in which we previously reported age-related declines in dopamine (van Dyck et al. 2002b) and serotonin (van Dyck et al. 2000) transporters using the same [123I]β-CIT SPECT scans; however, it eliminates three women from that sample who were receiving hormone replacement therapy and one who was receiving oral contraceptives.
All subjects underwent a clinical examination by a research psychiatrist to exclude any neurological or psychiatric disease, alcohol, or substance abuse. Screening procedures included a physical and neurological examination, electrocardiogram (EKG), serum chemistries, thyroid function studies, complete blood count (CBC), urinalysis, and urine toxicology screening. Female subjects of childbearing potential were required to have a negative pregnancy test (serum at screening, urine immediately prior to tracer injection). Subjects gave written informed consent to the research protocol approved by the Yale Human Investigation Committee and conducted in accordance with the 1964 Declaration of Helsinki.
SPECT imaging
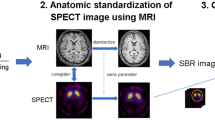
All subjects received a 0.6-g saturated solution of potassium iodide (SSKI) in the 24 h prior to tracer administration. They then received an injection of [123I]β-CIT (6.0±0.8 mCi; specific activity >5,000 Ci/mmol) followed 23.2±1.8 h later by a 24-min scan with a Picker (Cleveland, OH) PRISM 3000 (n=87) or 3000XP (n=35) SPECT camera equipped with a low-energy, high-resolution (LEHR) fanbeam collimator (128×128 matrix, 120° angular range, 3° angular step, 40 steps, 36 s/step, 15.5 cm radius of rotation). In this configuration, the PRISM 3000 acquires images at a reconstructed full width at half-maximum resolution of 12.3 mm as determined by a 123I point source in water. Comparability of the two cameras has been previously confirmed by imaging 26 subjects on both cameras from a single [123I]β-CIT injection (van Dyck et al. 2000, 2002b). All of the menstrual cycle subjects were scanned on the PRISM 3000. Previous studies have demonstrated that [123I]β-CIT reaches equilibrium binding in the brain by 18–24 h (Laruelle et al. 1994; van Dyck et al. 1995), yielding a simple unitless ratio of regional radioactivities [V3″ = specific/nondisplaceable binding = (region−occipital)/occipital] in estimating DAT number (i.e., B max). Prior to scanning, four or five fiducial markers filled with 5 μCi of Na99mTcO4 were attached to the skin along the canthomeatal plane to identify this plane during image analysis.
Images were reconstructed from photopeak counts (159±16 keV) using standard filtered backprojection methods (Butterworth, power 10, cutoff 0.24 cm−1) and displayed as a 128×128×64 matrix with a voxel size of 2.07×2.07×3.56 mm (15.25 mm3). Subsequent image analysis was performed by an operator who was unaware of subject demographics. SPECT data were reoriented to correct for deviations from the canthomeatal plane, as identified by the fiducial markers. Eight contiguous transaxial slices, with the highest uptakes in brainstem–diencephalon and striatum, respectively, were identified from a reconstructed midsagittal image and digitally summed to yield two transaxial slices, each 28.5 mm thick. Attenuation correction was performed using a Chang zero-order method (attenuation coefficient μ=0.15 cm−1) within an ellipse drawn around the skull. Standard region of interest (ROI) templates for left and right caudate (424 voxels or 6.5 ml each), left and right putamen (824 voxels or 12.6 ml each), brainstem–diencephalon (432 voxels or 6.6 ml), and occipital cortex (7,912 voxels or 120.6 ml) [similar to those previously published (van Dyck et al. 1995, 2000)] were positioned on the summed slice.
The caudate and putamen may be smaller in females than in males, as some (Gunning-Dixon et al. 1998), but not all (Jernigan et al. 1991; Murphy 1985), volumetric MRI studies have reported. To minimize the effects of group differences in striatal volume (i.e., greater partial volume effects in females), smaller ROIs for the caudate and putamen [96 voxels or 1.5 ml each, as previously published (Seibyl et al. 1995)] were also analyzed.
Statistical analysis
V3″ for striatum, striatal subregions (caudate and putamen), and brainstem–diencephalon was computed without conversion of SPECT counts per minute (cpm) to absolute units of radioactivity as [(cpm/voxel)region − (cpm/voxel)occipital)] / (cpm/voxel)occipital. The effect of the menstrual cycle phase (follicular vs luteal) on plasma estradiol and progesterone levels and on V3″ in striatum and brainstem–diencephalon was analyzed by paired t tests. The relationship between change in hormonal levels and change in V3″ from the follicular to the luteal phase was examined by Pearson's product moment correlation coefficient (r).
The effect of gender on striatal V3″ was then analyzed post hoc in the previously published sample by analysis of covariance (ANCOVA), controlling for age which has been strongly correlated with striatal V3″ in previous studies with [123I]β-CIT (van Dyck et al. 1995, 2002b). In light of evidence for different gender effects on DATs in intact vs ovariectomized female rats (Morissette and Di Paolo 1993; Bossé et al. 1997) and in younger vs older women (Mozley et al. 2001), separate ANCOVAs were also performed on the pre- and postmenopausal age groups. A simple age cutoff could not be used for female subjects, since one premenopausal subject (48 years old) was older than the two youngest postmenopausal subjects (45 and 48 years old). Premenopausal females were compared to males who were less than 50 years old, and postmenopausal females to males who were more than 50 years old. Statistical analyses utilized the SPSS (SPSS Inc., Chicago, IL) or PASS 2005 (for power calculations; NCSS Inc., Kaysville, UT) software packages and employed two-tailed tests of significance.
Results
Effect of menstrual cycle phase on hormone levels and [123I]β-CIT binding
Demographic and hormonal data for the ten menstrual cycle subjects are displayed in Table 1. These subjects' average cycles ranged from 25 to 32 days. Their early follicular-phase scans actually occurred on cycle days 5–7, and their mid-luteal-phase scans on days 4–9 after the LH surge (or cycle days 19–28). The LH surge for these subjects, as determined by a urine LH test kit, occurred on cycle days 12–23. Plasma estradiol levels showed considerable intersubject variability in both the follicular [coefficient of variation (CV) 59%] and luteal (CV 40%) phases. Estradiol levels increased significantly from 39.3±23.3 pg/ml for the follicular-phase scan to 95.7±38.6 pg/ml for the luteal-phase scan (t (9)=3.5, p=0.007; paired t test), although three subjects (1, 5, and 10) exhibited no increase between follicular and luteal phases. Plasma progesterone levels similarly demonstrated considerable intersubject variability in both the follicular (CV 27%) and luteal (CV 76%) phases. Progesterone levels increased from 0.4±0.1 pg/ml for the follicular-phase scan to 11.3±8.6 pg/ml for the luteal-phase scan (t (9)=4.0; p=0.003). Two subjects (4 and 6) evidenced no luteal-phase rise in plasma progesterone, suggesting that they had anovulatory cycles, as occurs in as many as 38% of cycles in young women (Metcalf and Mackenzie 1980). Therefore, a separate analysis was performed excluding these two subjects.
Striatal [123I]β-CIT SPECT data for the ten menstrual cycle subjects are displayed in Fig. 1. The values of striatal V3″ ranged from 6.1 to 10.8 (7.7±1.4) for the ten menstrual cycle subjects (including both scans for each subject). Mean values of striatal V3″ did not differ between follicular (7.6±1.6) and luteal (7.8±1.1) phases (t (9)=0.57; p=0.59; paired t test). When the two subjects with dubious ovulation were eliminated from the analysis, the result was the same (follicular, 7.7±1.7; luteal, 7.8±1.2; t (7)=0.24; p=0.82; paired t test). Moreover, change in striatal V3″ was uncorrelated with change in plasma estradiol (r=−0.06; n=10; p=0.87) or progesterone (r=0.10; n=10; p=0.79) from the follicular to the luteal phase. Finally, when striatal subregions (caudate and putamen) were considered separately, all of these analyses remained insignificant (data not shown).
Dopamine transporter (DAT) availability (V3″) in striatum, as measured by [123I]β-CIT and SPECT in healthy female subjects (n=10) at early follicular and mid-luteal phases of menstrual cycle. Circles denote individual subjects; lines link subjects. Mean values of striatal V3″ did not differ between follicular (7.6±1.6) and luteal (7.8±1.1) phases (t (9)=0.67; p=0.59; paired t test). When two subjects with dubious ovulation (denoted by open circles and dashed lines) were eliminated from the analysis, the results did not differ
Brainstem–diencephalon [123I]β-CIT SPECT data for the ten menstrual cycle subjects are displayed in Fig. 2. The values of V3″ for brainstem–diencephalon ranged from 1.9 to 3.3 (2.5±0.4) for the ten menstrual cycle subjects (including both scans for each subject). Mean values of V3″ for brainstem–diencephalon did not differ between follicular (2.5±0.5) and luteal (2.5±0.3) phases (t (9)=0.67; p=0.52, paired t test). When the two subjects with dubious ovulation were eliminated from the analysis, the result was the same (follicular, 2.5±0.5; luteal, 2.5±0.4; t (7)=0.49; p=0.64; paired t test). Finally, change in V3″ for brainstem–diencephalon was uncorrelated with change in plasma estradiol (r=−0.18; n=10; p=0.63) or progesterone (r=0.10; n=10; p=0.79) from the follicular to the luteal phase.
Serotonin transporter (SERT) availability (V3″) in brainstem–diencephalon, as measured by [123I]β-CIT and SPECT in healthy female subjects (n=10) at early follicular and mid-luteal phases of menstrual cycle. Circles denote individual subjects; lines link subjects. Mean values of V3″ for brainstem–diencephalon did not differ between follicular (2.5±0.5) and luteal (2.5±0.3) phases (t (9)=0.67; p=0.52; paired t test). When two subjects with dubious ovulation (denoted by open circles and dashed lines) were eliminated from the analysis, the results did not differ
Effect of gender on [123I]β-CIT binding in striatum
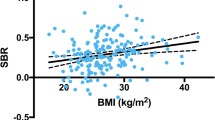
Figure 3 displays the relationship between striatal V3″ and age for the previously published healthy-subject sample (van Dyck et al. 2000, 2002b), with males and females denoted separately. Since no effect of menstrual cycle was observed, the ten menstrual cycle subjects were included in this sample, with each subject's first scan analyzed (six follicular and four luteal). Phase of menstrual cycle was not a criterion of entry for the remaining female subjects and was not recorded. When the effect of age was controlled for, striatal V3″ was found to be unrelated to gender (F (1,121)=0.04; p=0.84; ANCOVA). The effect of age was significant in the ANCOVA model (t (121)=−9.13; p<0.001).
Dopamine transporter (DAT) availability (V3″) in the striatum, as measured by [123I]β-CIT and SPECT, vs age in 122 healthy subjects. Closed circles represent females and, open triangles represent males. There was an age-dependent decline in striatal V3″ for both males (r=−0.66; n=70; p<0.0001) and females (r=−0.63; n=52; p<0.0001). When the effect of age was controlled for, striatal V3″ was found to be unrelated to gender (F (1,121)=0.04; p=0.84; ANCOVA) or the interaction of age × gender (F (1,121)=0.39, p=0.53)
The interaction of age × gender was not significant (F (1,121)=0.39; p=0.53), indicating no significant gender differences in the age-related rate of decline in striatal V3″. An age-dependent decline was observed for both males (r=−0.66, n=70, p<0.0001) and females (r=−0.63, n=52, p<0.0001). Linear regression analysis revealed that V3″ declined by 50% for males and 42% for females over the age range 18–88, or approximately 7.2% per decade for males and 6.0% per decade for females. There was still no effect of gender when premenopausal (F (1,78)=0.00; p=0.99; ANCOVA) and postmenopausal (F (1,42)=1.08; p=0.30) subjects were considered separately.
The results were similar with small ROIs for caudate and putamen. When the effect of age was controlled for, V3″ was found to be unrelated to gender for caudate (F (1,121)=0.00; p=0.98; ANCOVA), putamen (F (1,121)=0.02, p=0.88), and striatum (F (1,121)=0.01; p=0.93).
Discussion
We investigated the effect of gender and menstrual cycle phase on [123I]β-CIT uptake. In ten menstruating female subjects, the availability of DAT in striatum and SERT in brainstem–diencephalon did not differ between follicular and luteal phases of the menstrual cycle. Moreover, change in V3″ for striatum or brainstem–diencephalon was uncorrelated with change in plasma estradiol or progesterone from the follicular to the luteal phase. Finally, there was no effect of gender or the interaction of age and gender on striatal DAT availability in a larger, previously published (van Dyck et al. 2000, 2002b), healthy-subject sample that included the ten menstrual cycle subjects.
Effect of menstrual cycle on DAT and SERT availability
Our failure to detect an effect of menstrual cycle phase on DAT or SERT availability may have been limited by a number of factors, including anovulatory cycles and scanning at suboptimal cycle times for some subjects. However, our results did not differ when two subjects with dubious ovulation were eliminated from the analysis. Despite the challenge of synchronizing a busy SPECT schedule with female menstrual cycles, our subjects generally complied well with the LH test kits, and all luteal-phase scans were able to be scheduled within the prescribed 4–9 days after an LH surge. The final cycle days for some subjects (3, 7, and 8, scanned on days 26–28) were less likely mid-luteal than late-luteal (when circulating levels of estradiol and progesterone are falling). Nonetheless, hormonal levels obtained at the time of scanning confirmed substantial luteal-phase rises for these subjects as well as robust increases for the overall sample.
Autoradiographic studies in rats with the ligand [3H]GBR-12935 have demonstrated fluctuations in DAT density during the female estrous cycle (Morissette and Di Paolo 1993), with peaking of the B max at proestrus coinciding with time of peak levels of striatal dopamine. The differences in our results may represent species differences or possibly ligand differences, as [3H]GBR-12935 has been shown to bind to sites other than the DAT (Allard et al. 1994; Soucy et al. 1997). We cannot exclude the possibility that our human-subject sample was too small to detect a significant effect of menstrual cycle phase. However, our study had 80% power (α=0.05, two-tailed paired t test) to detect a 13.8% increase (17.4% increase with the elimination of the two subjects with dubious ovulation) in striatal V3″ from follicular to luteal menstrual cycle phases—far smaller than the roughly 25% increase observed at proestrus in rodent studies (Morissette and Di Paolo 1993).
To our knowledge, no previous human imaging studies have examined the effects of female menstrual cycle on the DAT, although two groups have measured another dopaminergic marker, the D2 receptor, in relation to cycle phase. Wong et al. (1988) investigated the effect of menstrual cycle on D2 dopamine receptor binding in caudate using PET and [11C]NMSP binding in six women. They found a small but definite trend (no statistics presented) for the binding rate constant (k 3) to be lower in the follicular phase and higher in the periovulatory and luteal phases. No hormonal levels were reported. Nördstrom et al. (1998) examined four healthy women with PET and [11C]raclopride at two different phases of their menstrual cycle and observed no menstrual-cycle-dependent variation in D2 receptor density. Finally, one previous imaging study has examined the effect of estrogen replacement therapy on DAT availability using SPECT and [99mTc]TRODAT-1 in healthy postmenopausal women (Gardiner et al. 2004). Those investigators observed a modest but statistically significant increase in DAT availability in the left anterior putamen after 4 weeks of conjugated equine estrogens and in both the left and right anterior putamen when medroxyprogesterone acetate was added to the regimen for an additional 2 weeks.
Prior imaging studies have also neglected the effects of female menstrual cycle on central SERT availability. Human platelet investigations have shown increased [3H]imipramine binding during the luteal phase compared with the follicular phase (Rojansky et al. 1991; Steege et al. 1992), although one study found no effect of the menstrual cycle phase (Poirier et al. 1986). However, since platelet SERT binding appears to correlate poorly with central SERT binding (Malison et al. 1998b), a direct examination of the brain is necessary. We are likewise unaware of any animal studies that have examined menstrual cycle effects on SERT binding in the brain. Although we lack a predicted effect size for formal power calculations, our study had 80% power (α=0.05, two-tailed paired t test) to detect a 14.8% increase (16.3% increase with the elimination of the two subjects with dubious ovulation) in V3″ for brainstem–diencephalon from the follicular to the luteal menstrual cycle phases.
Effect of gender on DAT availability
We were unable to measure an effect of gender on striatal DAT availability in our previously published (van Dyck et al. 2000, 2002b) healthy-subject sample, the largest such sample analyzed to date. This negative finding follows discrepant results in several previous investigations of male–female differences in striatal DATs, including two from our group. Van Dyck et al. (1995) examined 28 healthy subjects (14 males and 14 females) from age 18–83 with [123I]β-CIT SPECT and observed no effect of gender on striatal V3″. Kuikka et al. (1997) studied 39 healthy subjects (23 males and 16 females) from age 20–75 with [123I]β-CIT SPECT and fractal analysis and reported greater spatial heterogeneity of striatal tracer uptake in females. In this sample, the authors observed no gender differences in overall striatal DAT availability (J. Kuikka, personal communication). Lavalaye et al. (2000) performed [123I]FP-CIT SPECT scans in 45 healthy volunteers (23 males and 22 females) from age 18 to 83 and found significantly higher striatal binding ratios in females than in males (an effect that was unrelated to age). Staley et al. (2001) studied 21 healthy nonsmokers and 21 smokers (18 males and 24 females) from age 26 to 54 with [123I]β-CIT SPECT and observed significantly higher values of V3″ in the striatum, midbrain, and diencephalon in females than in males regardless of smoking status. Mozley et al. (2001) evaluated 66 healthy subjects (30 males and 36 females) from age 18 to 75 with [99mTc]TRODAT-1 and reported higher tracer-specific uptake (k3/k4 at equilibrium) in the caudate and putamen in females, as well as significant age × gender interactions (with greater sex differences in younger subjects). We cannot exclude the possibility that the present study lacked statistical power to detect a small effect of gender. However, our study had 80% power (α=0.05, two-tailed ANCOVA, age) to detect a 12.5% increase in striatal V3″ in females vs in males as compared to the 16% increase observed by Lavalaye et al. (2000) or the 10.5% increase observed by Staley et al. (2001). We also cannot discount the possibility that our negative gender results could be influenced by a small effect of menstrual cycle (that was missed in our ten-subject sample). Since gender studies of DAT availability have not controlled for cycle phase (van Dyck et al. 1995; Kuikka et al. 1997; Lavalaye et al. 2000; Staley et al. 2001; Mozley et al. 2001), scanning women at different phases of the menstrual cycle might contribute to discrepant gender effects across studies.
Divergent results among these studies—three positive and three negative (including the present one) for gender differences—are potentially attributable to a number of differences in imaging methodologies. The three negative reports all used [123I]β-CIT (van Dyck et al. 1995; Kuikka et al. 1997), whereas two of the three positive studies used the more DAT-selective ligands [123I]FP-CIT (Lavalaye et al. 2000) or [99mTc]TRODAT-1 (Mozley et al. 2001). However, ligand differences are unlikely to account for discrepant gender effects given that striatal uptake of [123I]β-CIT is associated almost exclusively with the DAT, and one study (Staley et al. 2001) found male–female differences with this ligand. Only Staley et al. (2001) employed MRI coregistration for ROI placement, enabling the use of the cerebellum as the reference region, whereas other investigators used the occipital cortex as the reference region (van Dyck et al. 1995; Lavalaye et al. 2000; Mozley et al. 2001). Although a previous primate SPECT investigation (Laruelle et al. 1993) demonstrated no displaceable component of cortical [123I]β-CIT uptake, human postmortem studies have found low but measurable levels of SERT in the occipital cortex (Cortes et al. 1988; Laruelle et al. 1988), including those with [123I]β-CIT (Staley et al. 1994).
Among the technical factors that are more likely to introduce systematic bias in gender analyses are photon attenuation and partial volume effects, owing to male–female differences in head size, skull thickness, and brain morphometry. Only Staley et al. (2001) performed transmission scanning for measured attenuation correction. The other studies all assumed uniform attenuation within an ellipse drawn around the skull (van Dyck et al. 1995; Kuikka et al. 1997; Lavalaye et al. 2000; Mozley et al. 2001). The assumption of uniform attenuation might boost brain activities more in females than in males—given a relatively greater skull thickness in males—yielding spurious gender differences. This phenomenon is thus unlikely to produce a false-negative result in the three negative studies or a false-positive finding in the study employing measured attenuation correction (Staley et al. 2001).
None of the studies incorporated a formal “partial-volume” correction (Sorenson and Phelps 1987), although caudate and putamen may be smaller in females than in males (Gunning-Dixon et al. 1998). Failure to correct for volume differences might tend to suppress striatal activities more in females than in males and cause gender differences to be missed by the negative studies. To minimize this possibility, we undertook a secondary analysis using smaller ROIs [1.5 ml each for caudate and putamen, well below actual volumes which are approximately 3.4 ml for caudate and 4.2 ml for the putamen (Gunning-Dixon et al. 1998)] but still observed no gender differences. However, future studies would still benefit from formal partial-volume correction.
Autoradiographic studies in rats with the ligand [3H]GBR-12935 have demonstrated higher DAT density in intact females than in males (Morissette and Di Paolo 1993; Rivest et al. 1995) or ovariectomized females (Morissette and Di Paolo 1993; Bossé et al. 1997), although we are unaware of any postmortem human studies that have examined the effects of gender on DAT binding. Such studies would be most valuable, as they would circumvent the aforementioned gender differences in skull thickness and brain morphometry which may inherently bias imaging studies.
In summary, imaging studies of gender effects on DAT availability are currently divided between those that show higher DAT availability in females vs those that show no gender differences. These discrepancies are not readily accounted for by methodological differences. Given the potential for systematic gender biases in head size, skull thickness, and brain morphometry, future studies would benefit from measured attenuation correction (Staley et al. 2001) as well as the introduction of formal partial-volume correction. Given the unclarity of this issue, prudence would dictate that DAT imaging studies of neuropsychiatric disorders should still employ gender matching. However, our results suggest that in using [123I]β-CIT and other ligands of the DAT and SERT in the study of most neuropsychiatric disorders, matching of female subjects according to menstrual cycle phase is probably unnecessary.
References
Allard P, Marcusson JO, Ross SB (1994) [3H]GBR-12935 binding to cytochrome P450 in the human brain. J Neurochem 62:342–348
Andersen SL, Rutstein M, Benzo JM, Hostetter JC, Teicher MH (1997) Sex differences in dopamine receptor overproduction and elimination. Neuroreport 8:1495–1498
Boja JW, Patel A, Carroll FI, Rahman MA, Philip A, Lewin AH, Kopajtic TA, Kuhar MJ (1991) [125I]RTI-55: a potent ligand for dopamine transporters. Eur J Pharmacol 194:133–134
Bossé R, Rivest R, Di Paolo T (1997) Ovariectomy and estradiol treatment affect the dopamine transporter and its gene expression in the rat brain. Brain Res Mol Brain Res 46:343–346
Brady KT, Grice DE, Dustan Cl, Randall C (1993) Gender differences in substance use disorders. Am J Psychiatry 150:1707–1711
Carroll FI, Rahman MA, Abraham P, Parham K, Lewin AH, Dannals RF, Shaya E, Scheffel U, Wong DF, Boja JW, Kuhar MJ (1991) [123I]3β-(4-iodophenyl)tropan-2β-carboxylic acid methyl ester (RTI-55), a unique cocaine receptor ligand for imaging the dopamine and serotonin transporters in vivo. Med Chem Res 1:289–294
Cortes R, Soranoi E, Pazos A, Probst A, Palacios J (1988) Autoradiography of antidepressant binding sites in the human brain: localization using [3H]imipramine and [3H]paroxetine. Neuroscience 27:473–496
Di Paolo T (1994) Modulation of brain dopamine transmission by sex steroids. Rev Neurosci 5:27–42
Farde L, Hall H, Pauli S, Halldin C (1995) Variability in D2-dopamine receptor density and affinity: a PET study with [11C]raclopride in man. Synapse 20:200–208
Folstein MF, Fostein SE, McHugh PR (1975) “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Gardiner SA, Morrison MF, Mozley PD, Mozley LH, Brensinger C, Bilker W, Newberg A, Battistini M (2004) Pilot study on the effect of estrogen replacement therapy on brain dopamine transporter availability in healthy, postmenopausal women. Am J Geriatr Psychiatry 12:621–630
Gunning-Dixon FM, Head D, McQuain J, Acker JD, Raz N (1998) Differential aging of the human striatum: a prospective MR imaging study. AJNR Am J Neuroradiol 19:1501–1507
Heinz A, Ragan P, Jones DW, Hommer D, Williams W, Knable MB, Gorey JG, Doty L, Geyer C, Lee KS, Coppola R, Weinberger DR, Linnoila M (1998) Reduced central serotonin transporters in alcoholism. Am J Psychiatry 155:1544–1549
Innis RB, Seibyl JP, Scanley BE, Laruelle M, Abi-Dargham A, Wallace E, Baldwin RM, Zea-Ponce Y, Zoghbi S, Wang S, Gao Y, Neumeyer JL, Charney DS, Hoffer PB, Marek KL (1993) Single photon emission computed tomographic imaging demonstrates loss of striatal dopamine transporters in Parkinson disease. Proc Natl Acad Sci U S A 90:11965–11969
Jacobsen LK, Staley JK, Malison RT, Zoghbi SS, Seibyl JP, Kosten TR, Innis RB (2000) Elevated central serotonin transporter binding availability in acutely abstinent cocaine-dependent patients. Am J Psychiatry 157:1134–1140
Jernigan TL, Archibald SL, Berhow MT, Sowell ER, Foster DS, Hesselink JR (1991) Cerebral structure on MRI, Part I: localization of age-related changes. Biol Psychiatry 29:55–67
Kaasinen V, Nagren K, Hietala J, Farde L, Rinne JO (2001) Sex differences in extrastriatal dopamine d(2)-like receptors in the human brain. Am J Psychiatry 158:308–311
Kuikka JT, Tiihonen J, Karhu J, Bergström KA, Räsänen P (1997) Fractal analysis of striatal dopamine re-uptake sites. Eur J Nucl Med 24:1085–1090
Kuopio AM, Marttila RJ, Helenius H, Rinne UK (1999) Changing epidemiology of Parkinson's disease in southwestern Finland. Neurology 52:302–308
Laruelle M, Vanisberg M-A, Maloteaux J-M (1988) Regional and subcellular localization in human brain of [3H]paroxetine binding, a marker of serotonin uptake sites. Biol Psychiatry 24:299–309
Laruelle M, Baldwin RM, Malison RT, Zea-Ponce Y, Zoghbi SS, Al-Tikriti MS, Sybirska EH, Zimmermann R, Wisniewski G, Neumeyer JL, Milius RA, Wang S, Smith EO, Roth RH, Charney DS, Hoffer PB, Innis RB (1993) SPECT imaging of dopamine and serotonin transporters with [123I]β-CIT: pharmacological characterization of brain uptake in nonhuman primates. Synapse 13:295–309
Laruelle M, Wallace E, Seibyl JP, Baldwin RM, Zea-Ponce Y, Zoghbi SS, Neumeyer JL, Charney DS, Hoffer PB, Innis RB (1994) Graphical, kinetic, and equilibrium analyses of in vivo [123I]β-CIT binding to dopamine transporters in healthy human subjects. J Cereb Blood Flow Metab 14:982–994
Laruelle M, Abi-Dargham A, van Dyck CH, Gil R, De Souza C, Krystal JH, Seibyl JP, Baldwin RM, Innis RB (2000) Dopamine and serotonin transporters in patients with schizophrenia: an imaging study with [123I]β-CIT SPECT. Biol Psychiatry 47:371–379
Lavalaye J, Booij J, Reneman L, Habraken JBA, van Royen EA (2000) Effect of age and gender on dopamine transporter imaging with [123I]FP-CIT SPET in healthy volunteers. Eur J Nucl Med 27:867–869
Malison RT, McDougle CJ, van Dyck C, Scahill L, Baldwin RM, Price LH, Leckman JF, Innis RB (1995) [123I]β-CIT SPECT imaging demonstrates increased striatal dopamine transporter binding in Tourette's syndrome. Am J Psychiatry 152:1359–1361
Malison RT, Best SE, van Dyck CH, McCance EF, Wallace EA, Laruelle M, Baldwin RM, Seibyl JP, Price LH, Kosten TR, Innis RB (1998a) Elevated striatal dopamine transporters during acute cocaine abstinence as measured by [123I]β-CIT SPECT. Am J Psychiatry 155:832–834
Malison RT, Price LH, Berman RM, van Dyck CH, Pelton GH, Carpenter LL, Sanacora G, Owens MJ, Nemeroff CB, Rajeevan N, Baldwin RM, Seibyl JP, Innis RB, Charney DS (1998b) Reduced brain serotonin transporter availability in major depression as measured by [123I]-2β-carbomethoxy-3β-(4-iodophenyl)tropane and single photon emission computed tomography. Biol Psychiatry 44:1090–1098
Metcalf MG, Mackenzie JA (1980) Incidence of ovulation in young women. J Biosoc Sci:345–352
Morissette M, Di Paolo T (1993) Sex and estrous cycle variations of rat striatal dopamine uptake sites. Neuroendocrinology 58:16–22
Mozley LH, Gur RC, Mozley PD, Gur RE (2001) Striatal dopamine transporters and cognitive functioning in healthy men and women. Am J Psychiatry 158:1492–1499
Murphy GM Jr (1985) The human corpus striatum and dentate nucleus: volumetric analysis for hemispheric asymmetries, sex differences, and aging changes. Exp Neurol 89:134–145
Neumeyer JL, Wang S, Milius RA, Baldwin RM, Zea-Ponce Y, Hoffer PB, Sybirska E, Al-Tikriti M, Charney DS, Malison RT, Laruelle MA, Innis RB (1991) [123I]-2-β-Carbomethoxy-3-β-(4-iodophenyl)-tropane (β-CIT): high affinity SPECT radiotracer of monoamine reuptake sites in brain. J Med Chem 34:3144–3146
Nördstrom A-L, Olsson H, Halldin C (1998) A PET study of D2 dopamine receptor density at different phases of the menstrual cycle. Psychiatry Res 83:1–6
Pohjalainen T, Rinne JO, Någren K, Syvälahti E, Hietala J (1998) Sex differences in the striatal dopamine D2 receptor binding characteristics in vivo. Am J Psychiatry 155:768–773
Poirier M-F, Benkelfat C, Galzin A-M, Langer SZ (1986) Platelet 3H-imipramine binding and steroid hormones serum concentrations during the menstrual cycle. Psychopharmacology (Berl) 88:86–89
Rivest R, Falardeau P, Di Paolo T (1995) Brain dopamine transporter: gender differences and effect of chronic haloperidol. Brain Res 692:269–272
Rojansky N, Halbreich U, Zander K, Barkai A, Goldstein S (1991) Imipramine receptor binding and serotonin uptake in platelets of women with premenstrual changes. Gynecol Obstet Invest 31:146–152
Seeman MV (1982) Gender differences in schizophrenia. Can J Psychiatry 27:107–112
Seeman MV (1996) The role of estrogen in schizophrenia. J Psychiatry Neurosci 21:123–127
Seibyl JP, Wallace E, Smith EO, Stabin M, Baldwin RM, Zea-Ponce Y, Gao Y, Zhang YW, Neumeyer JL, Zubal IG, Charney DS, Hoffer PB, Innis RB (1994) Whole-body biodistribution, radiation absorbed dose, and brain SPECT imaging with iodine-123-β-CIT in healthy human subjects. J Nucl Med 35:764–770
Seibyl JP, Marek KL, Quinlan D, Sheff K, Zoghbi SS, Zea-Ponce Y, Baldwin RM, Fussell B, Smith EO, Charney DS, van Dyck CH, Hoffer PB, Innis RB (1995) Decreased single-photon emission computed tomographic [123I]β-CIT striatal uptake correlates with symptom severity in Parkinson's disease. Ann Neurol 38:589–598
Seibyl JP, Laruelle M, van Dyck CH, Wallace E, Baldwin RM, Zoghbi SS, Zea-Ponce Y, Neumeyer J, Charney DS, Hoffer PB, Innis RB (1996) Reproducibility of iodine-123-β-CIT SPECT brain measurement of dopamine transporters. J Nucl Med 37:222–228
Sofuoglu M, Dudish-Poulsen S, Nelson D, Pentel PR, Hatsukami DK (1999) Sex and menstrual cycle differences in the subjective effects from smoked cocaine in humans. Exp Clin Psychopharmacol 7:274–283
Sorenson JA, Phelps ME (1987) Physics in nuclear medicine. Saunders, Philadelphia
Soucy J-P, Mrini A, Lafaille F, Doucet G, Descarries L (1997) Comparative evaluation of [3H]WIN 35428 and [3H]GBR 12935 as markers of dopamine innervation density in brain. Synapse 25:163–175
Staley JK, Basile M, Flynn DD, Mash DC (1994) Visualizing dopamine and serotonin transporters in the human brain with the potent cocaine analogue [125I]RTI-55: in vitro binding and autoradiographic characterization. J Neurochem 62:549–555
Staley JK, Krishnan-Sarin S, Zoghbi SS, Tamagnan G, Fujita M, Seibyl JP, Maciejewski PK, O'Malley S, Innis RB (2001) Sex differences in [123I]β-CIT SPECT measures of dopamine and serotonin transporter availability in healthy smokers and nonsmokers. Synapse 41:275–284
Steege JG, Stout AL, Knight DL, Nemeroff CB (1992) Reduced platelet tritium-labeled imipramine binding sites in women with premenstrual syndrome. Am J Obstet Gynecol 167:168–172
Tiihonen J, Kuikka J, Bergström K, Hakola P, Karhu J, Ryynänen O-P, Föhr J (1995) Altered striatal dopamine re-uptake site densities in habitually violent and non-violent alcoholics. Nat Med 1:654–657
van Dyck CH, Seibyl JP, Malison RT, Wallace E, Zoghbi SS, Zea-Ponce Y, Baldwin RM, Charney DS, Hoffer PB, Innis RB (1995) Age-related decline in dopamine transporter binding in human striatum with [123I]β-CIT SPECT. J Nucl Med 36:1175–1181
van Dyck CH, Malison RT, Seibyl JP, Laruelle M, Klumpp H, Zoghbi SS, Baldwin RM, Innis RB (2000) Age-related decline in central serotonin transporter availability with [123I]β-CIT SPECT. Neurobiol Aging 21:497–501
van Dyck CH, Quinlan DM, Cretella LM, Staley JK, Malison RT, Baldwin RM, Seibyl JP, Innis RB (2002a) Unaltered dopamine transporter availability in adult attention deficit hyperactivity disorder. Am J Psychiatry 159:309–312
van Dyck CH, Seibyl JP, Malison RT, Laruelle M, Zoghbi SS, Baldwin RM, Innis RB (2002b) Age-related decline in dopamine transporters: analysis of striatal subregions, nonlinear effects, and hemispheric asymmetries. Am J Geriatr Psychiatry 10:36–43
Wong DF, Broussolle EP, Wand G, Villemagne V, Dannals RF, Links JM, Zacur HA, Harris J, Naidu S, Braestrup C, Wagner HN, Gjedde A (1988) In vivo measurement of dopamine receptors in human brain by positron emission tomography: age and sex differences. Ann N Y Acad Sci 515:203–214
Acknowledgements
The authors wish to thank H. Klumpp, M. Early, E.O. Smith, G. Wisniewski, and L. Amici for excellent technical assistance, and L. Muenz, Ph.D. for statistical advice. This research was supported by the American Federation for Aging Research (AFAR) (C.H.vD, PI), generous gifts from Rose and Philip Hoffer, and by funds from the Department of Veterans Affairs (Research Enhancement Award in Depression) and the National Institute of Mental Health (R43-MH48243 and MH58620). The research protocols described herein comply with the current laws of the USA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Best, S.E., Sarrel, P.M., Malison, R.T. et al. Striatal dopamine transporter availability with [123I]β-CIT SPECT is unrelated to gender or menstrual cycle. Psychopharmacology 183, 181–189 (2005). https://doi.org/10.1007/s00213-005-0158-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-005-0158-5