Abstract
Rationale
Cortisol hypersecretion is regarded as important in the pathophysiology of major depression. However, recent studies in community-based samples have been inconclusive.
Objective
To determine whether acutely depressed, medication-free subjects show an exaggerated release of cortisol in saliva in relation to awakening.
Methods
We studied the pattern of waking salivary cortisol in 20 unmedicated acutely depressed subjects and 40 healthy controls.
Results
In both groups, salivary cortisol increased rapidly after waking, peaking at 30 min. Overall, patients with acute depression secreted approximately 25% more cortisol than controls, though 60 min after waking, their cortisol levels were similar.
Conclusions
Depressed patients in the community appear to have increased early morning cortisol secretion, but the demonstration of this effect requires control for time of waking.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The notion that depressive illness is associated with hypersecretion of cortisol has reached the status of a textbook truism, but the phenomenon can prove elusive particularly in depressed subjects recruited from community and primary care sources (Posener et al. 2000). More recently, measurement of salivary cortisol levels has been used as a simple noninvasive index of free circulating cortisol levels. However, in a large community study, there was no evidence of increased salivary cortisol levels in depressed subjects relative to controls either at 9:00 a.m. or 11.00 p.m. (Strickland et al. 2002). The difficulty of demonstrating increased cortisol levels in the majority of moderately depressed patients has led some to suggest that hypersecretion of cortisol may be confined to severely depressed inpatients (Maes et al. 1994). This would have important implications for our understanding of the role of hypothalamic–pituitary–adrenal (HPA) axis dysfunction in depression in primary care.
The rise in salivary-free cortisol that follows waking is a simple and reliable means of assessing the dynamic activity of the HPA axis activity and may therefore offer advantages over isolated measures of basal salivary cortisol (Clow et al. 2004; Wust et al. 2000). We have recently shown that euthymic, medication-free subjects recovered from depression have an exaggerated increase in salivary cortisol levels in relation to waking (Bhagwagar et al. 2003). In a sample of healthy male college students, higher levels of self-reported depressive symptomatology were associated with a greater cortisol response after awakening (Pruessner et al. 2003). Here we study the pattern of waking salivary cortisol secretion in a cohort of acutely depressed unmedicated subjects recruited from primary care sources.
Materials and methods
Subjects
Twenty patients (mean age, 43.6±11.0 years; 10 men and 10 women) recruited from primary care sources and 40 controls (40.5±13.6 years; 19 men and 21 women) gave informed consent for the study, which was approved by the Oxfordshire Psychiatric Research Ethics Committee. All subjects had been off psychotropic medication for at least 4 weeks and were not misusing alcohol or illicit substances. Exclusion criterion for all groups included current or past serious medical or neurological illness, alcohol or illicit substance dependence, and Axis I disorders other than those described. They were screened by an experienced clinician using the Structured Clinical Interview for DSM-IV Disorders (SCID) (First et al. 1997).
Patients met criteria for a major depressive disorder, whereas control subjects had no current or past Axis I disorders. Patients had a mean 17-item Hamilton Depression Rating Scale (HAM-D) score of 19.8 (range 17–27) and a Beck Depression Inventory (BDI) score of 26.8 (range 17–45).
Procedure
Saliva samples were collected fasting, by the subjects at home, in Salivettes (Sarstedt, Germany) with the first sample being taken immediately on waking and continuing at 15-min intervals for the next hour. Adherence to the sampling protocol was assessed by self report and also cross checking self-reported times of sampling. The time of the menstrual cycle in female subjects was not controlled, but the premenstrual week was avoided; otherwise, the day of sampling was chosen by the subject without specifying a weekend or weekday for sampling. Two controls and three patients were on oral contraceptives at the time of the study.
Biochemical measures
Salivary cortisol was measured with an in-house double antibody radioimmunoassay with intraassay and interassay coefficients of variation of 3% and 10%, respectively. Missing salivary cortisol values (n=3) were substituted with the mean of the value before and after the missing value except for the first and last samples. None of the subjects had a missing first or last sample.
Statistical analysis
Statistical analysis employed analysis of variance (ANOVA) and unpaired t tests (two-tailed). Area under the curve (AUC) was measured by the trapezoid method. Correlations were carried out using Pearson's product moment. Values are given as mean±standard error of the mean (SEM).
Results
There was no significant difference between the groups for time of awakening (patients 7:18 a.m.±15 min, controls 7:34 a.m.±15 min, p>0.05) or hours of sleep (7.7±0.4 h, controls 8.0±0.3 h, p>0.05).
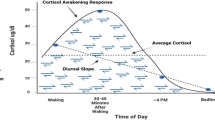
An ANOVA of the salivary cortisol levels showed a significant main effect of group (F=6.56, p=0.013), a main effect of time (F=55, p<0.001), but no interaction of group with time (F=0.79, p=0.46). There were no main or interactive effects of age or gender on salivary cortisol levels when included as covariates in the ANOVA. Post hoc analyses of the individual time points showed that salivary cortisol levels were significantly higher in patients at 15, 30, and 45 min after waking (see Fig. 1). There was a trend toward an increase in levels of salivary cortisol at the point of awakening in the patients (27.0±3.1 nmol/l vs. 21.6±1.2 nmol/l, t=1.93, p=0.059). By 60 min, however, cortisol levels in the two groups were very similar. The AUC of salivary cortisol secretion was significantly greater in patients than controls (33.9±2.5 nmol h/l vs. 27.5±1.3 nmol h/l, F=6.39, p=0.014). There was no correlation of salivary cortisol AUC with age (r=−0.06, p=0.65), hours of sleep (r=0.050, p=0.79), and time of awakening (r=−0.1, p=0.58, respectively). In addition, there was no correlation of salivary cortisol AUC with BDI (r=−0.22, p=0.46) or HAM-D (r=0.41, p=0.12) scores in the small sample of depressed patients studied.
Morning salivary cortisol levels in relation to waking in acutely depressed subjects (n=20) and controls (n=40). Values are given as mean±SEM. *Patients have significantly increased levels of salivary cortisol at 15 min (t=−2.21, p=0.036), 30 min (t=−2.22, p=0.030), and 45 min (t=−2.36, p=0.022) compared with controls
Discussion
Our findings indicate that medication-free subjects with a diagnosis of major depression secrete significantly greater amounts of salivary cortisol in relation to waking in comparison to a healthy control group. Our methodology contrasts with usual practice when measuring salivary cortisol in depressed subjects where samples are generally taken at standard clock times. For example, a morning measurement (commonly at 8 a.m. or 9 a.m.]) is used to quantify the peak diurnal cortisol level whereas an evening sample reflects the nadir (see, e.g., Goodyer et al. 2003; Strickland et al. 2002).
Figure 1 illustrates that the value of a single early morning salivary cortisol measurement could vary substantially depending on when the sample was collected in relation to the time of waking. In this sample of mildly depressed patients, no difference in waking time was noted. However, it is common for patients with moderate to severe depression to wake early in the morning, in which case, their “morning” (8:00–9:00 a.m.) sample will be relatively later in relation to waking than the same sample for the control group. Additionally, even without systematic bias of this nature, the fact that individuals will be sampled at differing times around their 30-min postwaking cortisol peak increases the variance of the cortisol measure, which in turn will make it harder to show differences between depressed subjects and controls. Finally, our data suggest that increase in salivary cortisol secretion in depressed patients is relatively short-lived because an hour after waking, cortisol levels in depressed patients and controls were very similar. Thus, timing the collection of saliva samples in relation to waking could lead to more reliable detection of HPA axis abnormalities in depressed patients.
The increase in waking cortisol levels in the depressed patients in the current study does not seem related to severity of depression or other sociodemographic variables such as age, gender, hours of sleep, or time of awakening. In addition, we have previously found similarly increased cortisol levels after waking in medication-free, euthymic subjects with a past history of recurrent depression (Bhagwagar et al. 2003). This suggests that hypersecretion of salivary cortisol in relation to waking may represent a trait marker of depression because it appears to persist when patients are clinically recovered. It is not yet clear whether this cortisol abnormality represents a marker of biological vulnerability to depression or a neuroendocrine “scar” of previous episodes of illness.
Another factor that can affect waking salivary cortisol is whether the samples are collected on a work or nonwork day. Morning increases in cortisol are usually somewhat higher on work days. In fact, in the present study, the majority of the depressed sample was not working so this would seem an unlikely reason for elevated morning cortisol levels in the depressed subjects. However, it is clearly important that this factor is controlled for in future investigations.
One important caveat is that how far the increased salivary cortisol response to waking actually represents significant cortisol hypersecretion. As we did not sample salivary cortisol levels throughout the day, we cannot comment on the possibility that the groups may differ at later time points. However, it does not necessarily follow that total daily cortisol output will be elevated in these depressed subjects. If total cortisol secretion is not increased in moderately depressed subjects, it will be important to determine the possible physiological importance of a single increased “pulse” of cortisol on waking.
Whatever the origin of the increase in waking cortisol in depression, persistent abnormalities of HPA axis function could have general health implications (Ward et al. 2004). For example, increased cortisol secretion has been associated with cognitive dysfunction (Lupien et al. 1998), low bone density (Raff et al. 1999), and increased morbidity related to cardiovascular disease (Malach and Imperato 2004; Otte et al. 2004; Rozanski et al. 1999; Rudisch and Nemeroff 2003). Increased morning salivary cortisol could therefore mark a vulnerability to the development of certain general medical disorders, as well as perhaps providing a means of monitoring the prophylactic effects of psychological and pharmacological therapies used to decrease the risk of recurrent depression.
As noted in the Introduction, it is widely believed that depression is associated with hypercortisolemia, though this has not been shown consistently in more recent studies that have examined HPA axis function in depression. For example, in a 24-h study of plasma cortisol and ACTH levels in acutely depressed nonpsychotic patients, the 24-h cortisol amplitude was significantly reduced in comparison with control subjects, whereas ACTH indices did not differ between patients and the control group (Posener et al. 2000). Similarly, a study of 8 a.m. and 8 p.m. salivary cortisol levels also did not find any difference between controls and depressed subjects (Young et al. 2002). Our data suggest that the waking salivary cortisol measure described in this study may be a more sensitive method of detecting HPA axis dysfunction in depression. However, further studies are required to elucidate the mechanism of this abnormality and its possible clinical relevance.
References
Bhagwagar Z, Hafizi S, Cowen PJ (2003) Increase in concentration of waking salivary cortisol in recovered patients with depression. Am J Psychiatry 160:1890–1891
Clow A, Thorn L, Evans P, Hucklebridge F (2004) The awakening cortisol response: methodological issues and significance. Stress 7:29–37
First MB, Spitzer RL, Gibbon M, Williams JBW (1997) Structured Clinical Interview for DSM-IV Axis I disorders—Clinician Version (SCID-CV). American Psychiatric Press, Washington, DC
Goodyer IM, Herbert J, Tamplin A (2003) Psychoendocrine antecedents of persistent first-episode major depression in adolescents: a community-based longitudinal enquiry. Psychol Med 33:601–610
Lupien SJ, de Leon M, de Santi S et al (1998) Cortisol levels during human aging predict hippocampal atrophy and memory deficits. Nat Neurosci 1:69–73
Maes M, Calabrese J, Meltzer HY (1994) The relevance of the in- versus outpatient status for studies on HPA-axis in depression: spontaneous hypercortisolism is a feature of major depressed inpatients and not of major depression per se. Prog Neuro-psychopharmacol Biol Psychiatry 18:503–517
Malach M, Imperato PJ (2004) Depression and acute myocardial infarction. Prev Cardiol 7:83–90 (quiz 91–2)
Otte C, Marmar CR, Pipkin SS, Moos R, Browner WS, Whooley MA (2004) Depression and 24-hour urinary cortisol in medical outpatients with coronary heart disease: the heart and soul study. Biol Psychiatry 56:241–247
Posener JA, DeBattista C, Williams GH, Chmura Kraemer H, Kalehzan BM, Schatzberg AF (2000) 24-Hour monitoring of cortisol and corticotropin secretion in psychotic and nonpsychotic major depression. Arch Gen Psychiatry 57:755–760
Pruessner M, Hellhammer DH, Pruessner JC, Lupien SJ (2003) Self-reported depressive symptoms and stress levels in healthy young men: associations with the cortisol response to awakening. Psychosom Med 65:92–99
Raff H, Raff JL, Duthie EH et al (1999) Elevated salivary cortisol in the evening in healthy elderly men and women: correlation with bone mineral density. J Gerontol A Biol Sci Med Sci 54:M479–M483
Rozanski A, Blumenthal JA, Kaplan J (1999) Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation 99:2192–2217
Rudisch B, Nemeroff CB (2003) Epidemiology of comorbid coronary artery disease and depression. Biol Psychiatry 54:227–240
Strickland PL, Deakin JF, Percival C, Dixon J, Gater RA, Goldberg DP (2002) Bio-social origins of depression in the community. Interactions between social adversity, cortisol and serotonin neurotransmission. Br J Psychiatry 180:168–173
Ward AM, Syddall HE, Wood PJ, Dennison EM, Phillips DI (2004) Central hypothalamic–pituitary–adrenal activity and the metabolic syndrome: studies using the corticotrophin-releasing hormone test. Metabolism 53:720–726
Wust S, Wolf J, Hellhammer DH, Federenko I, Schommer N, Kirschbaum C (2000) The cortisol awakening response—normal values and confounds. Noise Health 2:79–88
Young AH, Gallagher P, Porter RJ (2002) Elevation of the cortisol–dehydroepiandrosterone ratio in drug-free depressed patients. Am J Psychiatry 159:1237–1239
Acknowledgements
The study was supported by the Medical Research Council. The authors thank Alison Reed for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bhagwagar, Z., Hafizi, S. & Cowen, P.J. Increased salivary cortisol after waking in depression. Psychopharmacology 182, 54–57 (2005). https://doi.org/10.1007/s00213-005-0062-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-005-0062-z