Abstract
Rationale
Accumulated data suggest that N-methyl-d-aspartate (NMDA) receptors are involved in the reinforcing properties of nicotine. However, less is known about the role of α-amino-3-hydroxy-5-methyl-4-isoxazoleproprionate (AMPA) receptors in this context.
Objectives
To study the effect of the novel systemically administered AMPA receptor antagonist ZK200775 ([1,2,3,4-tetrahydro-7-morpholinyl-2,3-dioxo-6-(fluoromethyl) quinoxalin-1-yl] methylphosphonate) on nicotine-induced dopamine (DA) release in the nucleus accumbens (NAcc) and nicotine-stimulated locomotor activity (LMA) and particularly the relative role of NMDA and AMPA receptors in nicotine-stimulated DA release and LMA.
Methods
Male Wistar rats were administered ZK200775, CGP39551 or NBQX 30 min prior to nicotine and DA release and LMA was measured using in vivo microdialysis or photocell equipped activity boxes. Glutamate-produced neurotoxicity in cultured brain cells and binding assays were performed to determine the glutamate receptor subtype selectivity and affinity to nicotine receptors of ZK200775, respectively.
Results
ZK200775 (3.0 but not 1.5 or 6.0 mg/kg) significantly decreased the nicotine-induced (0.6 mg/kg) DA release in the NAcc and nicotine-stimulated LMA. ZK200775 (1.5, 3.0, 6.0 mg/kg) alone influenced neither DA release nor LMA. ZK200775 showed 34-fold selectivity for AMPA receptors compared to NMDA receptors and no affinity to nicotine receptors. The NMDA receptor antagonist CGP39551 (10 mg/kg) significantly decreased both the nicotine-induced DA release and nicotine-stimulated LMA whereas the AMPA receptor antagonist NBQX (10 mg/kg) had no effect. Notably, CGP39551 and ZK200775 (3.0 mg/kg) displayed a different pattern in inhibition of nicotine-induced DA release.
Conclusions
Both NMDA- and AMPA receptors are involved in nicotine’s dependence-producing properties, although in a spatiotemporally differential manner.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nicotine, the main dependence-producing constituent in tobacco, is a highly psychoactive substance and it is generally accepted that the reinforcing properties of nicotine at least partially are mediated through the mesocorticolimbic dopamine (DA) system (Imperato et al. 1986; Corrigall et al. 1992; Nisell et al. 1994). The mesocorticolimbic DA system originates in the ventral tegmental area (VTA) and projects via the medial forebrain bundle to the nucleus accumbens (NAcc), the medial prefrontal cortex (mPFC), the amygdala, the septal area, and the olfactory tubercle and is considered to be of particular importance in the brain reward system, since most drugs of abuse activate this system (Wise and Bozarth 1987; Koob and Bloom 1988). For instance, systemic administration of amphetamine, cocaine, morphine, ethanol or nicotine increases the extracellular DA levels in the NAcc as measured by in vivo microdialysis (Di Chiara and Imperato 1986; Imperato and Di Chiara 1986; Imperato et al. 1986; Hernandez et al. 1987; Kuhar et al. 1991). In analogy, systemically administered nicotine, or locally infused in the VTA or in the NAcc increases accumbal DA release (Mifsud et al. 1989; Benwell and Balfour 1992; Ferrari et al. 2002). However, systemically administered nicotine exerts a wide variety of psychopharmacological effects with profound influence on many other transmitter systems such as the serotonergic, adrenergic, endogenous peptide pathways, and the glutamatergic systems (McGehee and Role 1995; Picciotto 1998). Accumulated evidence shows that nicotine facilitates glutamatergic transmission. For example, nicotine increases glutamate release in forebrain areas (Toth et al. 1993), in the NAcc (Reid et al. 2000) and in the VTA (Fu et al. 2000). Furthermore, nicotine-induced DA release is blocked when glutamate transmission is antagonized, suggesting a pivotal role of glutamate in nicotine’s reinforcing effects. Thus, intra-tegmental infusion of the competitive NMDA receptor antagonists 2-amino-5-phosphopentanoic acid (AP-5) (Schilstrom et al. 1998; Fu et al. 2000) or cis-4-phosphonomethyl-2-piperidine carboxylic acid (CGS 19755) (Fu et al. 2000) significantly reduces nicotine-induced DA release in NAcc. In contrast to available data on NMDA receptors, it is less clear whether α-amino-3-hydroxy-5-methyl-4-isoxazoleproprionate (AMPA) subtype glutamate receptors are involved in the reinforcing effects of nicotine. Studies have so far demonstrated that neither intra-tegmental nor intra-accumbal infusion of the competitive AMPA receptor antagonist 6-cyano-7-nitro-quinoxaline-2,3-dione (CNQX) alter nicotine-induced DA release in the NAcc (Schilstrom et al. 1998; Fu et al. 2000; Sziraki et al. 2002). In addition, intra-tegmental infusion of the non-competitive AMPA receptor antagonist GYKI52466 leaves the nicotine-induced DA levels in the NAcc unchanged. Studies investigating AMPA receptor operated mechanisms have so far involved the use of AMPA receptor antagonists with relatively low selectivity, poor solubility, and short duration of action (Jackson et al. 2000). CNQX, for instance, also possesses affinity for the strychnine-insensitive glycine site at the NMDA receptor (Harris and Miller 1989; Kessler et al. 1989; Lester et al. 1989; Pellegrini-Giampietro et al. 1989; Mead and Stephens 1999). More recently, other AMPA receptor antagonists, such as LY293558 (Liljequist et al. 1995; Schoepp et al. 1995) and [1,2,3,4-tetrahydro-7-morpholinyl-2,3-dioxo-6-(fluoromethyl)quinoxalin-1-yl] methylphosphonate (ZK200775) (cf. Turski et al. 2000) have become available. The competitive AMPA receptor antagonist ZK200775 displays, in contrast to the first generation of AMPA receptor antagonists, more favorable pharmacokinetic properties and a beneficial side-effect profile. Furthermore, the potency and selectivity of ZK200775 in vitro are very similar to those of 2,3-dihydroxy-6-nitro-7-sulfamoyl-benzo(F)quinoxaline (NBQX), which has been demonstrated with primary cultures of hippocampal neurons and cortical membranes (Turski et al. 2000). In addition, ZK200775 and NBQX show very similar profiles in rodent models of brain ischemia and brain trauma, and also of in vivo activity in which muscle relaxant, anxiogenic, anticonvulsant and analgesic effects have been investigated. Moreover, ZK200775 is water soluble at physiological pH with retained high selectivity at the AMPA receptors, and shows, in the dose range effective in neuroprotection, no deleterious side effects on motor behavior. Neither has, at least to our knowledge, any actions in cardiovascular status or respiratory systems been detected in the animals (Turski et al. 2000). Given this favorable pharmacological profile of ZK200775, we considered it of interest to investigate the effect of systemic administration of ZK200775 in an attempt to elucidate further the role of AMPA receptors in nicotine stimulated locomotor activity and nicotine-induced DA release in the NAcc. In addition, using primary cultures of cerebellar granule cells (Cebers et al. 1997, 1998; Cebere and Liljequist 2003), we wanted to further explore the selectivity of ZK200775 on AMPA receptors compared to NMDA receptors and also, by carrying out receptor binding experiments exclude the possibility that ZK200775 has affinity for brain nicotine receptors.
Materials and methods
Animals
All experiments were approved by the Ethical Committee for Use of Animal Subjects at Karolinska Institutet and carried out in compliance with local animal care guidelines. For in vivo microdialysis, locomotor activity measurements and binding assays, adult male Wistar rats (B&K Universal, Sollentuna, Sweden) weighing 260–330 g, were given free access to standard rat chow and water. Upon arrival to the animal facility the animals were housed in groups of 4 in a temperature (25°C) and humidity (50%) controlled environment on a 12-h light/dark cycle (lights on at 7 a.m. and off at 7 p.m.) for at least 7 days before handling or surgery. Primary cultures of cerebellar granule cells were prepared from 8-day-old Sprague-Dawley rats (B&K Universal). The pups arrived together with the female at the age of 1 day and were housed together until day 8.
Drugs
Cerebellar granule cell assay
Fetal calf serum, gentamicin, and Eagle’s medium were from Life Technologies (Paisley, UK). NMDA, glycine hydrochloride, MTT, trypsin, poly-l-lysine, DNase, cytosine-α-furanoside, soybean trypsin inhibitor, isopropanol were bought from Sigma (St Louis, Mo., USA). AMPA and NBQX disodium salt were purchased from Tocris Cookson (St Louis, Mo., USA). Cyclothiazide was a generous gift from Eli Lilly Research Laboratories (Indianapolis, Ind., USA).
Nicotine receptor binding assay
[3H]epibatidine (56.2 Ci/mmol) was purchased from PerkinElmer Life Sciences (Boston, Mass., USA). EDTA, HEPES, phenylmethylsulphonyl fluoride and sodium azide were obtained from Sigma.
Microdialysis and locomotor activity measurements
Pentobarbital sodium and bipuvacaine (Apoteket AB, Stockholm, Sweden) were given at 60 mg/kg IP and 0.3 ml, respectively. (−)Nicotine hydrogen tartrate (Sigma) was dissolved in saline (0.9%), pH-adjusted to 7.2±0.2 with diluted NaOH and administered at doses of 0.3 or 0.6 mg/kg (SC) free base in a volume of 1 ml/kg. NBQX disodium salt (Tocris Cookson) and CGP39551 (a generous gift from Novartis Basel, Switzerland) were dissolved in saline and administered at 10 mg/kg (IP) in a volume of 2 ml/kg. ZK200775 (a generous gift from Schering AG Gmbh, Berlin, Germany) was dissolved in saline, pH-adjusted with diluted NaOH to 7.45±0.1 and administered in doses of 1.5, 3.0, and 6.0 mg/kg (IP) in a volume of 2 ml/kg.
Procedure
Primary cultures of cerebellar granule cells
Primary cultures of cerebellar granule cells were prepared from 8-day-old Sprague-Dawley rat (B&K Universal) cerebellum as previously described (Cebers et al. 1996). Briefly, after dissection, 8 cerebelli were pooled and sliced with a McIlwain tissue chopper in two orthogonal directions (slices were 0.3 mm thick), incubated in a 0.025% trypsin solution, and dispersed by trituration in a DNase and soybean trypsin inhibitor containing solution (0.01% and 0.05%, respectively). Cells were plated (2×106 cells/2 ml/dish) onto six-well plates coated with 5 μg/ml of poly-l-lysine (MW=30,000–70,000). Cells were cultured for 8 days at 37°C in an atmosphere of 5% CO2/95% air in Basal Eagle’s medium supplemented with 10% heat-inactivated fetal calf serum, 25 mM KCL, 2 mM glutamine, and 100 μg/ml gentamicin. Cytosine-β-arabinofuranoside (10 μM) was added 24 h after plating to limit the number of non-neuronal cells. The medium was not changed until the cultures were used in the experiment.
Drug treatment
NMDA and AMPA receptor-mediated neurotoxicity, and its modulation by ZK200775 was examined by applying the relevant drug concentrations dissolved in Mg2+-free Locke’s buffer containing 154 mM NaCl, 5.6 mM KCL, 2.3 mM CaCl2, 3.6 mM NaHCO3, 5.5 mM d-glucose, and 5 mM HEPES (pH 7.4). To begin the experiment on DIV 8, the medium was collected from cerebellar granule cells, after which they were washed once with pre-warmed Mg2+-free Locke’s buffer to remove traces of the growth medium before the drug-containing Mg2+-free Locke’s buffer was added. ZK200775 was added at concentrations of 0.03, 0.1, 0.3, 1.0, 3.0, 10, 30, 100, and 300 μM. The collected medium was filter-sterilized and stored until needed. After 2 h incubation at 37°C, the buffer was removed; cells were washed with pre-warmed drug-free Locke’s buffer containing 1 mM Mg2+ and returned to the original culture medium collected previously. Cell viability was assessed 24 h later.
Assessment of cell viability
The MTT assay was used to assess the viability of cerebellar granule cells in culture. It has been widely assumed that mitochondrial dehydrogenases in living cells convert soluble MTT (3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazolium bromide) into an insoluble blue formazan product that can be dissolved in isopropanol and the colour intensity measured spectrophotometrically (Mossman 1983). In this way, the MTT assay would assess the integrity of mitochondria characteristic of viable cells. However, recent findings suggest that MTT is taken into cells through endocytosis and reduced primarily in the endosome/lysosome compartment instead of the mitochondria (Liu et al. 1997). Nevertheless, the MTT assay, as a measure of cell viability, is still valid because it measures endocytosis, a fundamental feature of most living cells. The MTT assay was performed as described previously (Cebers et al. 1996). The assay was initiated by removing the culture medium and adding MTT (0.3 mg/ml) dissolved in serum-free culture medium. Following 1 h incubation at 37°C, the medium was aspirated and 0.5 ml isopropanol added to lyse the cells and to dissolve the formazan crystals. Aliquots (100 μl) of this solution were pipetted into 96-well microplates and absorbency was recorded at 570 nm using a microplate reader. Cell viability was expressed as percentage of the absorption in control cells (100%).
Nicotine receptor binding assay
Tissue preparation
Rats were killed by decapitation and the brains were removed and the cerebral cortex was dissected on an ice-cold glass plate and stored at −80ºC until use. The membranes were prepared using a modified version of the method by Romano and Goldstein (1980). The tissue was homogenized in an ice-cold hypotonic buffer solution (0.1×Hepes buffer: 118 mM NaCl, 4.8 mM KCl, 2.5 mM CaCl2, 1.2 mM MgSO4, 20 mM Hepes, pH 7.4, 1 mM EDTA, 0.1 mM phenylmethylsulphonyl fluoride, 0.02% w/v sodium azide) using a Polytron (Kinematica, Switzerland) homogenizer (10 s at setting 5). Several cortices were pooled to acquire enough tissue for the binding assays. The crude particulate fraction was obtained by centrifugation at 15,000 rpm for 15 min at 4ºC. The supernatant was discarded and the pellet was washed twice more by resuspension in ice-cold homogenization buffer using a glass-Teflon tissue grinder and centrifugation. The final pellet was stored at −80ºC until use.
Binding assay
On the day of binding assay, the pellet was resuspended in Hepes buffer (pH 7.4) and the protein concentration was measured using Bio-Rad protein assay (by Bradford) with bovine serum albumin as the standard. The [3H]epibatidine (56.2 Ci/mmol; PerkinElmer Life Sciences, Inc., Boston, Mass., USA) binding assay was performed according to Houghtling et al. (1995) with minor modifications. Aliquots of tissue homogenates (0.1–0.2 mg protein) in triplicates were incubated in polypropylene test tubes in 50 mM Tris-Hepes buffer (118 mM NaCl, 4.8 mM KCl, 2.5 mM CaCl2, 1.2 mM MgSO4, 20 mM Hepes, pH 7.4), containing 100 pM [3H]epibatidine. The concentration of [3H]epibatidine was chosen based on a previously done saturation binding curve resulting in a Kd of 10.4±1.4 pM (data not shown) where also non-specific binding was determined in the presence of 100 μM (−)-nicotine hydrogen tartrate. Increasing concentrations of ZK200775 or nicotine (1 pM to 100 μM) were added to the polypropylene test tubes. Final assay volumes amounted to 5 ml to avoid ligand depletion. The reaction was started by the addition of tissue and the mixture was incubated for 2 h at room temperature in the dark. Incubation was terminated by vacuum filtration through Whatman GF/C filter, presoaked in binding buffer containing 0.5% polyethyleneimine using a Brandel cell harvester (Gaithersburg, Md., USA). The filter was rapidly washed 4 times with 4-ml aliquots of cold 50 mM Tris-HCl buffer (pH 7.4). Subsequently, filters were placed in scintillation vials with 5 ml Ready Safe liquid scintillation cocktail (Beckman Coulter, Calif., USA) and counted in a β-counter (Wallac, Finland) at 45% counting efficiency. The IC50 value was calculated from the curve in the graph, which was fitted by non-linear regression analysis (Prism; Graph Pad Software, Calif., USA).
Microdialysis
Rats were anaesthetized with sodium pentobarbital and mounted in a stereotaxic frame (David Kopf Instruments, Tujunga, Calif., USA). Guide cannulas for the probe (CMA 12; CMA Microdialysis, Stockholm, Sweden) were implanted into the NAcc (AP: 1.6, ML; 1.2 and DV: −8.0, according to the atlas of Paxinos and Watson 1986) and anchored to the skull with stainless steel screws and dental cement. After surgery, bupivacaine was applied on the wound to induce post-surgical analgesia. The animals were housed individually in single housing cages for 3 days before the start of microdialysis which was conducted in awake freely moving rats. On the morning of the experimental day the animals were transferred to an isolated room and microdialysis probes (CMA12/2 mm; CMA Microdialysis), were inserted and connected to a perfusion line via a two-channel liquid swivel (AgnTho’s AB, Sweden) where the perfusion solution (artificial cerebrospinal fluid containing 147 mM NaCl, 3.0 mM KCL, 1.3 mM CaCl2, 1.0 mM MgCl2, 1 mM Na2HPO4, and 0.2 mM NaH2PO4) was perfused via a Univentor 801 syringe pump (AgnTho’s AB) and collected in a refrigerated Univentor 820 microsampler (AgnTho’s AB) at a flow rate of 1 μl/min. Following the probe insertion a 2-h wash out period preceded the sampling of a total of 17 samples where the first six samples served as baseline samples. Thirty min following the first injection of saline or either of the glutamate subtype receptor antagonists, the rats were administered nicotine. The sample vials were prefilled with 10 μl of 0.3 mM perchloric acid and the temperature of the microsampler was constantly held at 8°C. Samples were collected every 20 min and were immediately frozen at −80°C.
At the end of each experiment the animals were given a anesthetic dose of sodium pentobarbital, decapitated and the brains were removed and immediately frozen in dry-ice chilled acetone. Probe position was verified histologically with sectioning of the brains performed in a cryostat (Zeiss 500) with 20 μm thick coronal slices mounted on slides followed by staining with thionin. The probe placements were determined according to the brain atlas of Paxinos and Watson (1986). Only data obtained from animals with probes correctly placed within the NAcc were used in the study.
Analysis of dialysate
The concentration of DA was analyzed with reverse phase high performance liquid chromatography (HPLC) systems (ESA, Inc., Chelmsford, Mass., USA) with electrochemical detection using a Coulochem II detector (5200A) with a conditioning cell (5021) and an analytical cell (5011) where one of the systems only had the analytical cell (5011). The mobile phase consisting of Na-acetate; 7.465 mg/l, Na2EDTA; 3.7 mg/l, octanesulfonic acid monohydrate; 140.79 mg/l, and HPLC-grade methanol; 110 ml/l with pH adjusted to 4.1 with concentrated acetic acid was delivered by an HPLC-pump (Model 582; ESA, Inc.) through a C18-AQ column (Reprosil-Pur; 150×4 mm, 5 μm) at a flow rate of 1 ml/min. The dialysate, that is 25 μl of the perfusate, was automatically injected by an autosampler (Model 830; Midas, Spark Holland BV). The oxidizing potentials were set as follows; HPLC-system 1: conditioning cell: +175 mV, analytical cell R2 +400 mV and HPLC-system 2: analytical cell R1 +75 mV, R2 +350 mV. The microdialysis samples were randomly assigned to one of the two HPLC systems; all samples from a given subject were analyzed with the same system. Chromatographic analysis was done using CSW 1.7 software (DataApex Ltd, Czech Republic).
Locomotor activity
Locomotor activity was measured using AccuScan activity meters (42×42×30 cm) (AccuScan Instruments Inc., Ohio, USA) equipped with three rows of infrared photo sensors. Each row consisted of 16 sensors, 2.5 cm apart where two rows were placed on a 90° angle along the front and side of the floor of the cage, and the third row was placed 10 cm above the floor to measure vertical activity.
All rats were habituated to the locomotor activity boxes for 2 days before any drug treatment commenced. The first day of habituation the rats were allowed to freely explore the locomotor activity boxes for 1 h. The second day of habituation was designed to habituate the rats to the injections. Thus, the rats were again allowed to freely explore the activity boxes, however, after 30 min of free exploration saline was administered (IP). Following the saline injection the rats were returned to the activity boxes and after another 30 min, the rats were again administered saline (SC). Following the second saline injection the rats were again returned to the activity boxes and left there for an additional 60 min. On day 3, after 2 days of habituation, the rats (n=6–8) were placed in the activity boxes and, as was performed on day 2 of habituation, allowed to calm down for 30 min. Thereafter, the first injection was given of either saline, ZK200775 (1.5, 3.0, or 6.0 mg/kg, IP) or CGP39551 (10 mg/kg, IP), after which they were returned to the boxes. Thirty minutes later, the rats were administered nicotine (0.6 mg/kg, SC). Locomotor activity was recorded during the entire session and continued for 60 min after nicotine administration, i.e. a total time of 120 min. Thus, the effects of ZK200775 and CGP39551 on nicotine-stimulated locomotor activity are presented, as total horizontal locomotor activity or as a time-course recorded during 60 min after the second injection, i.e. administration of nicotine. The effects of ZK200775 (1.5, 3.0, or 6.0 mg/kg, IP) or CGP39551 (10 mg/kg, IP) on spontaneous locomotor activity are the data recorded during 30 min after the first injection of the respective compound prior to nicotine administration.
The experiment was performed following an independent group design. Each time a photo beam was crossed, it was recorded as one activity count. All locomotor data are presented as horizontal activity either as total counts over a certain time period (30 or 60 min) or as a time-course divided into twelve 5-min intervals.
Data analysis
Statistical analysis of the microdialysis results was performed with DA levels expressed as percent of baseline. Baseline, to which all subsequent measurements were compared, was defined as the average of the three samples immediately preceding treatment. The mean percent changes were then calculated for each 20-min sample for all rats in each group. Data were analyzed with two-way ANOVA (treatment×time) with repeated measures followed by Bonferroni’s test for multiple comparisons when appropriate. Each treatment group is pooled from randomly assigned rats in the microdialysis experiments covering a time period of 12 months. The data from the acute locomotor activity studies were statistically evaluated using one-way ANOVA followed by Bonferroni’s test for multiple comparisons when appropriate (total horizontal locomotor activity) or two-way ANOVA (treatment×time) with repeated measures followed by Bonferroni’s test for multiple comparisons when appropriate (horizontal activity) over the 5-min intervals.
Results
Neuroprotective effects of ZK200775 in primary cultures of cerebellar granule cells
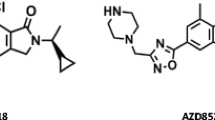
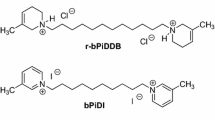
Measuring NMDA- or AMPA-produced neurotoxicity in primary cultures of cerebellar granule cells assessed the selectivity of ZK200775 on AMPA receptors over NMDA receptors. Increasing concentrations of ZK200775 (0.03–300 μM) augmented cell viability in medium containing NMDA (300 μM)+glycine (10 μM) or AMPA (30 μM)+cyclothiazide (30 μM) with an EC50=11.27 μM and 0.337 μM, respectively (Fig. 1). These data suggest that although ZK200775 is 34 times more potent at the AMPA receptors, higher concentrations of this compound can no longer be considered AMPA-selective, since they also block NMDA receptors.
ZK200775-induced reversal (0.03–300 μM) of NMDA- and AMPA-induced neurotoxicity in cerebellar granule cell cultures. Data are presented as a percentage of cell viability in the absence of antagonist (=0%) in cultures treated with NMDA (300 μM)+glycine (10 μM) or AMPA (30 μM)+cyclothiazide (30 μM). Each data point is the mean of three determinations (±SEM). The EC50values of ZK200775 effect on NMDA and AMPA-induced neurotoxicity are 11.27 μM and 0.337 μM, respectively
Nicotine receptor binding assay
As can be seen from Fig. 2, (−)-nicotine hydrogen tartrate effectively inhibited binding of 100 pM [3H]epibatidine in a concentration dependent manner (1 pM to 100 μM). In contrast, increasing concentrations of ZK200775 up to 100 μM did not inhibit [3H]epibatidine. The IC50 value for (−)-nicotine hydrogen tartrate was 6.8 nM, whereas no binding at any concentration was observed for ZK200775, which would thus suggest that, at least in the concentration range tested here, no interaction between ZK200775 and brain nicotine receptors exists.
Inhibition of [3H]epibatidine binding in rat cortex by nicotine and ZK200775. Aliquots of tissue homogenates (0.1–0.2 mg protein) were incubated with100 pM [3H]epibatidine and the indicated concentrations of (−)-nicotine hydrogen tartrate and ZK200775. Each point is the mean of six determinations (±SEM). The curve in the graph was fitted by non-linear regression analysis
Microdialysis
Figure 3 reveals the placements of the microdialysis probes. Twenty probe positions are depicted representing the most medial, lateral, rostral, and caudal positions. The remaining microdialysis probes were found within these borders. The release of DA in the extracellular space of NAcc is measured as mean (±SEM) percent change of the baseline levels in the collected dialysate. The mean baseline concentration of DA in the dialysate was 24.21±0.26 fmol/20 μl (n=84). Acute administration of nicotine dose-dependently (0.3 mg/kg and 0.6 mg/kg, SC) and significantly increased the DA levels in the NAcc with main effects of Sal+Sal versus Sal+Nic0.3 [F treatment(1,13)=17.86, P=0.0003. F time(12,156)=12.26, P=0.091] and Sal+Sal versus Sal+Nic0.6 [F treatment(1,20)=52.2, P<0.0001, F time(12,24)=9.6, P=0.002] (Fig. 4). As shown in Fig. 5, pretreatment with ZK200775 (3.0 mg/kg, IP) significantly antagonized the nicotine-induced DA release in the NAcc [Ftreatment(1,23)=18.83, P<0.0001, F time(12,276)=13.33, P=0.002]. Importantly, a post-hoc test revealed that this significant reduction was only observed during the initial 40 min (P<0.0001 and P<0.05, respectively) after the injection of nicotine (0.6 mg/kg; SC). For the remaining time the DA levels slowly increased to the levels observed when nicotine (0.6 mg/kg, SC) was given alone. Pretreatment with ZK200775 (1.5 or 6.0 mg/kg) had no effect on the nicotine-induced DA-release in the NAcc (Fig. 5); ZK1.5+Nic0.6 versus Sal+Nic0.6 [F treatment(1,19)=1.64, P=0.19] and ZK6.0+Nic0.6 versus Sal+Nic0.6 [F treatment(1,20)=1.09, P=0.074]. When ZK200775 (1.5, 3.0, 6.0 mg/kg, IP) was administered alone, no changes in the DA levels were seen (Fig. 6). Administration of NBQX (10 mg/kg, IP) prior to nicotine (0.6 mg/kg, SC) did not influence the nicotine-induced DA release in the NAcc, whereas pretreatment with CGP39551 (10 mg/kg, IP) significantly reduced the nicotine-induced DA release with main effects of treatment and time [F treatment(1,17)=15.72, F time(12,204)=24.44, P=0.0005] (Fig. 7). Interestingly, CGP39551 displayed a differential pattern in the reduction of the nicotine-induced DA levels in the NAcc as compared to ZK200775 (3.0 mg/kg, IP). Thus, CGP39551 reduced the nicotine-induced (0.6 mg/kg, SC) DA levels in the NAcc during the initial 60 min after nicotine administration and abolished it completely for the remaining time of the microdialysis session. In contrast, ZK200775 (3.0 mg/kg, IP) caused a marked reduction in nicotine-induced DA-release during the initial 40 min after nicotine administration where the DA levels returned to the values observed at this time point with nicotine alone. However, although a trend could be observed, there was no statistical difference in nicotine-induced DA release between ZK200775 and CGP39551 pretreatment.
Schematic representation of the anatomical locations of 20 representative 2 mm microdialysis probes within the nucleus accumbens (adapted from Paxinos and Watson 1986). The probe locations of the remaining rats were all within the designated coordinates but were left out for illustrative purposes
Effect of nicotine (0.3 mg/kg or 0.6 mg/kg, SC) on the dopamine release in the nucleus accumbens. Data are presented as the mean (±SEM) percent change of baseline and were analyzed using two-way ANOVA with repeated measures followed by Bonferroni’s test for multiple comparisons, Sal+Sal, n=9, Sal+Nic0.3, n=5, Sal+Nic0.6, n=12. ***P<0.001, +P<0.05 compared with sal+sal
Effect of ZK200775 (1.5, 3.0, 6.0 mg/kg, IP) on the nicotine-induced (0.6 mg /kg, SC) dopamine release in the nucleus accumbens. Data are presented as the mean (±SEM) percent change of baseline, n=8–12. Data were analyzed using two-way ANOVA with repeated measures followed by Bonferroni’s test for multiple comparisons. ***P<0.001, *P<0.05 compared with sal+nic0.6
Effect of NBQX (10 mg/kg, IP) or CGP39551 (10 mg/kg, IP) on nicotine-induced (0.6 mg/kg, SC) dopamine release in the nucleus accumbens. Sal+Nic0.6, n=12; CGP+Nic0.6, n=6; NBQX+Nic0.6, n=5. Data are presented as the mean (±SEM) percent change of baseline. Data were analyzed using two-way ANOVA with repeated measures followed by Bonferroni’s test for multiple comparisons. *P<0.05 compared to sal+nic0.6
Locomotor activity
As can been seen in Fig. 8, acute nicotine treatment (0.6 mg/kg; SC) significantly increased total horizontal locomotor activity as compared to saline over 60 min of recording (P<0.0001) [F(5,45)=8.01, P<0.0001]. Post-hoc analysis revealed that administration of ZK200775 (3.0 mg/kg, IP) or CGP39551 (10 mg/kg, IP) 30 min prior to nicotine significantly reduced (P<0.01 and P<0.05, respectively), the nicotine-induced increase in total horizontal locomotor activity over 60 min, whereas pretreatment with the two other doses of ZK200775 (1.5 or 6.0 mg/kg, IP) had no effect. In panels A–E in Fig. 9, a time-course of horizontal locomotor activity over the 60-min period of recorded activity after nicotine administration divided into 5-min intervals is presented, in which a similar profile in activity is observed compared to total horizontal activity in Fig. 8. Thus, panel A (Sal+Sal versus Sal+Nic0.6) reveals a significant difference in activity [F treatment(1,15)=10.40, P<0.0001, F time(11,165)=18.66, P=0.0008]. Also, in panels C and E, a significant difference can be seen in the Sal+Nic0.6 versus CGP+Nic0.6 group [F treatment(1,13)=11.1, F time(11,143)=27.31, P<0.0001] and in the Sal+Nic0.6 versus ZK3+Nic0.6 group [F treatment(1,15)=3.4, P=0.0027, F time(11,165)=37.4, P<0.0001]. As shown in panels B and D, no differences were observed in the ZK1.5+Nic0.6 versus Sal+Nic0.6 and ZK6.0+Nic0.6 versus Sal+Nic0.6 groups. Furthermore, ZK200775 (1.5, 3.0, 6.0 mg/kg, IP) or CGP 39551 (10 mg/kg, IP) alone had no effect on spontaneous total horizontal locomotor activity over 30 min as compared to saline [F(5,45)=0.41, P=0.8], (Fig. 10).
Effect of ZK200775 (1.5, 3.0, 6.0 mg/kg, IP) or CGP39551 (10 mg/kg, IP) on nicotine-stimulated (0.6 mg/kg, SC) locomotor activity. Data are presented as mean (±SEM) total horizontal activity over 60 min after nicotine has been administered, n=6–8. Data were analyzed using one-way ANOVA followed by Bonferroni’s test for multiple comparisons. ***P<0.001, **P<0.01, *P<0.05 compared to sal+nic0.6
Time-course of the effect of ZK200775 (1.5, 3.0, 6.0 mg/kg, IP) and CGP39551 (10 mg/kg, IP) on nicotine-stimulated (0.6 mg/kg, SC) locomotor activity. Data are presented as mean (±SEM) horizontal activity divided in 5-min intervals over 60 min after nicotine has been administered, n=6–8. Data were analyzed using two-way ANOVA with repeated measures followed by Bonferroni’s test for multiple comparisons when appropriate. *P<0.05 compared to sal+nic0.6. A Sal+Sal vs Sal+Nic0.6; B Sal+Nic0.6 vs ZK1.5+Nic0.6; C Sal+Nic0.6 vs ZK3.0+Nic0.6; D Sal+Nic0.6 vs ZK6.0+Nic0.6; E Sal+Nic0.6 vs CGP+Nic0.6
Effect of systemically administered ZK200775 (1.5, 3.0, 6.0 mg/kg, IP) and CGP39551 mg/kg, IP on spontaneous locomotor activity. Data are presented as mean (±SEM) total horizontal activity over 30 min after administration of the respective drug, n=6–8. Data were analyzed using one-way ANOVA. No significant effects were found
Discussion
In agreement with previous studies nicotine dose-dependently (0.3 mg/kg and 0.6 mg/kg, SC) increased the release of DA in the NAcc (Imperato et al. 1986; Benwell et al. 1993) and enhanced the locomotor activity as compared to animals treated with saline (Benwell and Balfour 1992). One of the major findings in the present study was that systemic administration of the water-soluble competitive AMPA receptor antagonist ZK200775 (Turski et al. 2000) inhibited the nicotine-induced DA release in NAcc in an inverted U-shaped manner. Thus, the medium dose of ZK200775 (3.0 mg/kg, IP) significantly reduced the nicotine-induced DA release in the NAcc, whereas the low and high doses (1.5 mg/kg and 6.0 mg/kg, IP), respectively, had no effect. Administration of increasing doses of ZK200775 (1.5, 3.0, and 6.0 mg/kg, IP) 30 min prior to nicotine (0.6 mg/kg, SC) altered the nicotine-stimulated locomotor activity in a similar fashion as in the microdialysis experiments. Thus, ZK200775 (3.0 mg/kg, IP) significantly reduced the nicotine-stimulated locomotor activity, whereas ZK200775 (1.5 mg/kg and 6.0 mg/kg, IP) had no effect. Administration of ZK200775 (1.5, 3.0 and 6.0 mg/kg, IP) or CGP39551 (10 mg/kg, IP) alone influenced neither the DA levels in the NAcc nor the locomotor activity as compared to saline treated control animals.
Existing data show that ZK200775 has high affinity for AMPA receptors and a considerably lower affinity for NMDA receptors and no affinity for non-glutamatergic receptor binding sites (Turski et al. 1998, 2000), which we also demonstrated in this study by measuring the effect of ZK200775 on NMDA or AMPA-produced neurotoxicity in primary cultures of cerebellar granule cells and also by investigating the affinity of ZK200775 to nicotine receptors. In our hands ZK200775 showed no affinity to nicotine receptors and displayed distinct selectivity at AMPA receptors with a 34-fold higher potency as compared to NMDA receptors, suggesting that higher doses of ZK200775 may recruit also NMDA receptors. These data indicate that the above observed effect is mediated by AMPA receptors. However, when animals were pretreated with the in vivo active dose of the competitive AMPA receptor antagonist NBQX (10 mg/kg, IP) (Sheardown et al. 1990; Karcz-Kubicha and Liljequist 1995) no effect on the nicotine-stimulated DA release was observed, which is in line with earlier microdialysis studies where infusion of the AMPA/kainate receptor antagonists CNQX or GYKI52466 into the VTA or into the NAcc has no effect on the nicotine-induced DA release in the NAcc following concomitant systemic administration of nicotine (Schilstrom et al. 1998; Fu et al. 2000; Sziraki et al. 2002). Although one explanation for the lack of effect of NBQX in this study could be that the given NBQX dose was too low to alter the nicotine-induced DA release in the NAcc, this dose has been shown to be effective in for example neuroprotection (Sheardown et al. 1990), in inducing anxiety (Karcz-Kubicha and Liljequist 1995), and, in even lower doses, in disrupting operant oral self-administration of ethanol (Stephens and Brown 1999). On the other hand, higher doses of NBQX have muscle-relaxant properties and can suppress spinal reflexes (Turski et al. 1992), reduce spontaneous locomotion (Mares et al. 1997; Vanover 1998), and decrease basal DA levels in the striatum per se (Sakai et al. 1997). Based upon these considerations it is difficult to differentiate further the relative role of NMDA and AMPA receptors, respectively using the functional effects of ZK200775 and NBQX. Given that ZK200775 exerts its effects via AMPA receptors, it could be that it shows differential affinity for certain AMPA receptor populations in one of several regions as compared to NBQX, suggesting that the regional distribution of AMPA receptors and/or the stoichiometry of the subunit composition may be crucial factors leading to a differential selectivity of ZK200775 as compared with NBQX (Monaghan et al. 1984; Martin et al. 1993; Breese et al. 1996). Indeed, there are studies demonstrating substantial regional variations in the pharmacology of AMPA receptors, which most likely is due to differences in the AMPA receptor subunit composition (Porter and Greenamyre 1994; Kessler et al. 1998). To our knowledge, with the exception of the paper from Ferrari et al. (2002) who demonstrated an increase in the GluR1 mRNA levels in the VTA 24 h after nicotine administration, there are currently no studies available where AMPA receptor subunit specificity during the influence of nicotine has been investigated. However, in analogy with recent evidence regarding NMDA receptors, there is substantial knowledge suggesting that a certain subunit composition determines the functional properties, as demonstrated by the NMDA receptor NR2B-subunit receptor antagonists, e.g. ifenprodil and CP101606 (Menniti et al. 1997; Williams 2001). Another possibility could be that ZK200775 activates a different sub-population of AMPA receptors, which results in an altered net effect (Loftis and Janowsky 2003). This assumption could thus provide an answer to why the higher dose of ZK200775 (6.0 mg/kg) leaves the nicotine-induced DA release unchanged.
However, in this context, it should be noted that autoradiographic studies have shown that [3H]CNQX and [3H]NBQX have an almost identical distribution in the rat brain which overlaps with that of [3H]AMPA (Nielsen et al. 1990; Dev et al. 1996). Furthermore, ZK200775 and NBQX have been shown to be equipotent in inhibiting the binding of [3H]CNQX and [3H]AMPA, and in various functional tests of AMPA receptor activity (Turski et al. 2000). Thus, based upon the present data, it is difficult to explain the contrasting results obtained after pretreatment with NBQX and ZK200775, respectively, as being due to differential affinity for certain subgroups of AMPA receptors.
Another major finding in this study was that the competitive NMDA receptor antagonist CGP39551, which fails to significantly alter cocaine responding when self-administered intravenously (Hyytia et al. 1999), and only in very high doses per se increases the levels of DA in the NAcc (Marcus et al. 2001), significantly decreased both nicotine-induced DA release in NAcc and the nicotine-stimulated locomotor activity. Although in vitro studies have demonstrated that mesocortical DA neurons possess both AMPA and NMDA receptors and that the excitation induced by nicotine in midbrain DA neurons can blocked by both AMPA and NMDA receptor antagonists (Wang and French 1993; Grillner and Svensson 2000), accumulated in vivo data suggest that only when the NMDA mediated glutamate transmission is antagonized can the nicotine-induced DA release in the NAcc be abolished (Schilstrom et al. 1998; Fu et al. 2000; Sziráki et al. 2002). Thus, since ZK200775 in high doses also acts on NMDA receptors, it could be argued that the reason for the observed ZK200775 induced inhibition is that the dose is within the range of recruiting NMDA receptors. If this were the case, one would expect that also the higher dose of ZK200775 (6.0 mg/kg) should have inhibited the nicotine-induced DA release in the NAcc. However, no such reduction was observed here. In an attempt to explore a possible NMDA-mediated involvement of ZK200775 in the inhibitory effect of the nicotine-induced DA release, animals were pretreated with the competitive NMDA receptor antagonist CGP39551. Interestingly, although both CGP39551 and ZK200775 significantly reduced the nicotine-induced DA release, they displayed marked differences in their effect in the resulting DA release pattern. Using CGP39551, approximately 60 min after nicotine administration, the DA levels returned to baseline levels whereas after pretreatment with ZK200775, the DA levels slowly returned to the DA levels observed in animals treated with nicotine alone. Thus, the differential effect in the pattern of the inhibition in the nicotine-induced DA release in NAcc produced by ZK200775 (3.0 mg/kg) and CGP39551, respectively, could further imply that involvement of NMDA and AMPA receptors in the regulation of DA release is conveyed via different mechanisms of action. Nevertheless, the possibility still exists that the effect of ZK200775 could be mediated through yet unknown mechanisms unrelated to either NMDA or AMPA receptors.
In conclusion, the putative competitive AMPA receptor antagonist, ZK200775, significantly inhibited nicotine-induced DA release in the NAcc in an inverted U-shaped manner. The biochemical findings were confirmed with locomotor activity data in that only pretreatment with the medium dose of ZK200775, 3.0 mg/kg, but not 1.5 or 6.0 mg/kg, significantly reduced nicotine-stimulated locomotor activity. Also, the competitive NMDA receptor antagonist CGP39551 significantly decreased both the nicotine-induced DA release and nicotine-stimulated locomotor activity. To our knowledge, this is the first study demonstrating that systemic administration of a putative AMPA receptor antagonist ZK200775, and the competitive NMDA receptor antagonist CGP39551 inhibit both nicotine-induced DA release in the NAcc and reduce nicotine-stimulated locomotor activity. To what extent the effect of ZK200775 is specifically due to a blockade of AMPA receptors cannot be fully clarified on the basis of our current findings.
References
Benwell MW, Balfour DJ (1992) The effects of acute and repeated nicotine treatment on nucleus accumbens dopamine and locomotor activity. Br J Pharmacol 105:849–856
Benwell MW, Balfour DJ, Birrel CE (1993) The influence of tetrodotoxin and calcium on the stimulation of mesolimbic dopamine activity evoked by systemic nicotine. Psychopharmacology 112:467–471
Breese CR, Logel J, Adams C, Leonard SS (1996) Regional gene expression of the glutamate receptor subtypes GluR1, GluR2, and GluR3 in human postmortem brain. J Mol Neurosci 7:277–289
Cebere A, Liljequist S (2003) Ethanol differentially inhibits homoquinolinic acid- and NMDA-induced neurotoxicity in primary cultures of cerebellar granule cells. Neurochem Res 28:1193–1199
Cebers G, Cebere A, Zharkovsky A, Liljequist S (1996) Glycine does not reverse the inhibitory actions of ethanol on NMDA receptor functions in cerebellar granule cells. Naunyn Schmiedeberg’s Arch Pharmacol 354:736–745
Cebers G, Zhivotovsky B, Ankarcrona M, Liljequist S (1997) AMPA neurotoxicity in cultured cerebellar granule neurons: mode of cell death. Brain Res Bull 43:393–403
Cebers G, Cebere A, Liljequist S (1998) Metabolic inhibition potentiates AMPA-induced Ca2+ fluxes and neurotoxicity in rat cerebellar granule cells. Brain Res 779:194–204
Corrigall WA, Franklin KB, Coen KM, Clarke PB (1992) The mesolimbic dopaminergic system is implicated in the reinforcing effects of nicotine. Psychopharmacology 107:285–289
Dev KK, Petersen V, Honore T, Henley JM (1996) Pharmacology and regional distribution of the binding of 6-[3H]nitro-7-sulphamoylbenzo[f]-quinoxaline-2,3-dione to rat brain. J Neurochem 67:2609–2612
Di Chiara G, Imperato A (1986) Preferential stimulation of dopamine release in the nucleus accumbens by opiates, alcohol, and barbiturates: studies with transcerebral dialysis in freely moving rats. Ann N Y Acad Sci 473:367–381
Ferrari R, Le Nowere N, Picciotto MR, Changeux JP, Zoli M (2002) Acute and long-term changes in the mesolimbic dopamine pathway after systemic or local single nicotine injections. Eur J Neurosci 15:1810–1818
Fu Y, Matta SG, Gao W, Brower VG, Sharp BM (2000) Systemic nicotine stimulates dopamine release in nucleus accumbens: re-evaluation of the role of N-methyl-d-aspartate receptors in the ventral tegmental area. J Pharmacol Exp Ther 294:458–465
Grillner P, Svensson TH (2000) Nicotine-induced excitation of midbrain dopamine neurons in vitro involves ionotropic glutamate receptor activation. Synapse 38:1–9
Harris KM, Miller RJ (1989) CNQX (6-cyano-7-nitroquinoxaline-2,3-dione) antagonizes NMDA-evoked [3H]GABA release from cultured cortical neurons via an inhibitory action at the strychnine-insensitive glycine site. Brain Res 489: 85–89
Hernandez L, Lee F, Hoebel BG (1987) Simultaneous microdialysis and amphetamine infusion in the nucleus accumbens and striatum of freely moving rats: increase in extracellular dopamine and serotonin. Brain Res Bull 19 23–28
Houghtling RA, Davila-Garcia MI, Kellar KJ (1995) Characterization of (±)(-)[3H]epibatidine binding to nicotinic cholinergic receptors in rat and human brain. Mol Pharmacol 48:280–287
Hyytia P, Backstrom P, Liljequist S (1999) Site-specific NMDA receptor antagonists produce differential effects on cocaine self-administration in rats. Eur J Pharmacol 378:9–16
Imperato A, Di Chiara G (1986) Preferential stimulation of dopamine release in the nucleus accumbens of freely moving rats by ethanol. J Pharmacol Exp Ther 239:219–228
Imperato A, Mulas A, Di Chiara G (1986) Nicotine preferentially stimulates dopamine release in the limbic system of freely moving rats. Eur J Pharmacol 132:337–338
Jackson A, Mead AN, Stephens DN (2000) Behavioural effects of alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionate-receptor antagonists and their relevance to substance abuse. Pharmacol Ther 88:59–76
Karcz-Kubicha M, Liljequist S (1995) Evidence for an anxiogenic action of AMPA receptor antagonists in the plus-maze test. Eur J Pharmacol 279:171–177
Kessler M, Baudry M, Lynch G (1989) Quinoxaline derivatives are high-affinity antagonists of the NMDA receptor-associated glycine sites. Brain Res 489: 377–382
Kessler M, Mutneja MS, Rogers G, Lynch G (1998) Regional preferences of AMPA receptor modulators determined through agonist binding autoradiography. Brain Res 783: 121–126
Koob GF, Bloom FE (1988) Cellular and molecular mechanisms of drug dependence. Science 242:715–723
Kuhar MJ, Ritz MC, Boja JW (1991) The dopamine hypothesis of the reinforcing properties of cocaine. Trends Neurosci 14:299–302
Lester RA, Quarum ML, Parker JD, Weber E, Jahr CE (1989) Interaction of 6-cyano-7-nitroquinoxaline-2,3-dione with the N-methyl-d-aspartate receptor-associated glycine binding site. Mol Pharmacol 35:565–570
Liu Y, Peterson DA, Kimura H, Schubert D (1997) Mechanism of cellular 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) reduction. J Neurochem 69:581–593
Liljequist S, Cebers G, Kalda A (1995) Effects of decahydroisoquinoline-3-carboxylic acid monohydrate, a novel AMPA receptor antagonist, on glutamate-induced Ca2+ responses and neurotoxicity in rat cortical and cerebellar granule neurons. Biochem Pharmacol 50:1761–1774
Loftis JM, Janowsky A (2003) The N-methyl-d-aspartate receptor subunit NR2B: localization, functional properties, regulation, and clinical implications. Pharmacol Ther 97:55–85
Marcus MM, Mathe JM, Nomikos GG, Svensson TH (2001) Effects of competitive and non-competitive NMDA receptor antagonists on dopamine output in the shell and core subdivisions of the nucleus accumbens. Neuropharmacology 40:482–490
Mares P, Mikulecka A, Pometlova M (1997) Anticonvulsant action of 2,3-dihydroxy-6-nitro-7-sulfamoyl-benzo(f)quinoxaline in immature rats: comparison with the effects on motor performance. J Pharmacol Exp Ther 281:1120–1126
Martin LJ, Blackstone CD, Levey AI, Huganir RL, Price DL (1993) AMPA glutamate receptor subunits are differentially distributed in rat brain. Neuroscience 53:327–358
McGehee DA, Role LW (1995) Physiological diversity of nicotinic acetylcholine receptors expressed by vertebrate neurons. Annu Rev Physiol 57:521–546
Mead AN, Stephens DN (1999) CNQX but not NBQX prevents expression of amphetamine-induced place preference conditioning: a role for the glycine site of the NMDA receptor, but not AMPA receptors. J Pharmacol Exp Ther 290:9–15
Menniti F, Chenard B, Collins M, Ducat M, Shalaby I, White F (1997) CP-101,606, a potent neuroprotectant selective for forebrain neurons. Eur J Pharmacol 331:117–126
Mifsud JD, Hernandez L, and Hoeberl BG (1989) Nicotine infused into the nucleus accumbens increases synaptic dopamine as measured by in vivo microdialysis. Brain Res 478:365–367
Monaghan DT, Yao D, Cotman CW (1984) Distribution of [3H]AMPA binding sites in rat brain as determined by quantitative autoradiography. Brain Res 324:160–164
Mossman T (1983) Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Meth 65:55–63
Nielsen EO, Drejer J, Cha JH, Young AB, Honore T (1990) Autoradiographic characterization and localization of quisqualate binding sites in rat brain using the antagonist [3H]6-cyano-7-nitroquinoxaline-2,3-dione: comparison with (R,S)-[3H]alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid binding sites. J Neurochem 54:686–695
Nisell M, Nomikos GG and Svensson TH (1994) Infusion of nicotine in the ventral tegmental area or the nucleus accumbens of rat differentially affects accumbal dopamine release. Pharmacol Toxicol 75:348–352
Paxinos G, Watson C (1986) The rat brain in stereotaxic coordinates, 4th edn. Academic Press, New York
Picciotto MR (1998) Common aspects of the action of nicotine and other drugs of abuse. Drug Alcohol Depend 51:165–172
Pellegrini-Giampietro DE, Galli A, Alesiani M, Cherici G, Moroni F (1989) Quinoxalines interact with the glycine recognition site of NMDA receptors: studies in guinea-pig myenteric plexus and in rat cortical membranes. Br J Pharmacol 98:1281–1286
Porter RH, Greenamyre JT (1994) Regional variations in the pharmacology of AMPA receptors as revealed by receptor autoradiography. Brain Res 664:202–206
Reid MS, Fox L, Ho LB, Berger SP (2000) Nicotine stimulation of extracellular glutamate levels in the nucleus accumbens: neuropharmacological characterization. Synapse 35:129–136
Romano C, Goldstein A (1980) Stereospecific nicotine receptors on rat brain membranes. Science 210:647–650
Sakai K, Akiyama K, Kashihara K, Tsuchida K, Ujike H, Kuroda S, Shohmori T (1997) AMPA receptors modulate dopamine release in the striatum, as measured by brain microdialysis. Neurochem Int 30:329–336
Schilstrom B, Nomikos GG, Nisell M, Hertel P, Svensson TH (1998) N-Methyl-d-aspartate receptor antagonism in the ventral tegmental area diminishes the systemic nicotine-induced dopamine release in the nucleus accumbens. Neuroscience 82:781–789
Schoepp DD, Lodge D, Bleakman D, Leander JD, Tizzano JP, Wright RA, Palmer AJ, Salhoff CR, Ornstein PL (1995) In vitro and in vivo antagonism of AMPA receptor activation by (3S, 4aR, 6R, 8aR)-6-[2-(1(2)H-tetrazole-5-yl) ethyl] decahydroisoquinoline-3-carboxylic acid. Neuropharmacology 34:1159–1168
Sheardown MJ, Nielsen EO, Hansen AJ, Jacobsen P, Honore T (1990) 2,3-Dihydroxy-6-nitro-7-sulfamoyl-benzo(F)quinoxaline: a neuroprotectant for cerebral ischemia. Science 247:571–574
Stephens DN, Brown G (1999) Disruption of operant oral self-administration of ethanol, sucrose, and saccharin by the AMPA/kainate antagonist, NBQX, but not the AMPA antagonist, GYKI 52466. Alcohol Clin Exp Res 23:1914–1920
Sziraki I, Sershen H, Hashim A, Lajtha A (2002) Receptors in the ventral tegmental area mediating nicotine-induced dopamine release in the nucleus accumbens. Neurochem Res 27:253–261
Toth E, Vizi ES, Lajtha A (1993) Effect of nicotine on levels of extracellular amino acids in regions of the rat brain in vivo. Neuropharmacology 32:827–832
Turski L, Jaconsen P, Honoré T, Stephens DN (1992) Relief of experimental plasticity and anxiolytic/anticonvulscant actions of the alpha-amino-3-hydroxy-5-methyl-4-isoxazole propionate antagonist, 2,3-dihydro-6-nitro-7-sulfamoyl-benzo(F)quinoxaline. J Pharmacol Exp Ther 260:742–747
Turski L, Huth A, Sheardown M, McDonald F, Neuhaus R, Schneider HH, Dirnagl U, Wiegand F, Jacobsen P, Ottow E (1998) ZK200775: a phosphonate quinoxalinedione AMPA antagonist for neuroprotection in stroke and trauma. Proc Natl Acad Sci USA 95:10960–10965
Turski L, Schneider HH, Neuhaus R, McDonald F, Jones GH, Lofberg B, Schweinfurth H, Huth A, Kruger M, Ottow E (2000) Phosphonate quinoxalinedione AMPA antagonists. Restor Neurol Neurosci 17:45–59
Vanover KE (1998) Effects of AMPA receptor antagonists on dopamine-mediated behaviors in mice. Psychopharmacology 136:123–131
Wang T, French ED (1993) Electrophysiological evidence for the existence of NMDA and non-NMDA receptors on rat ventral tegmental dopamine neurons. Synapse 13:270–277
Williams K (2001) Ifenprodil, a novel NMDA receptor antagonist: site and mechanism of action. Curr Drug Targets 2:285–298
Wise RA, Bozarth MA (1987). A psychomotor stimulant theory of addiction. Psychol Rev 94:469–492
Acknowledgements
This study was supported by the Swedish Medical Research Council (project no. 7688), Sigurd and Elsa Golje’s Minne Foundation for Medical Research, Swedish Match Foundation for Nicotine Research, and funds from the Karolinska Institutet.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kosowski, A.R., Cebers, G., Cebere, A. et al. Nicotine-induced dopamine release in the nucleus accumbens is inhibited by the novel AMPA antagonist ZK200775 and the NMDA antagonist CGP39551. Psychopharmacology 175, 114–123 (2004). https://doi.org/10.1007/s00213-004-1797-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-004-1797-7