Abstract
Rationale
Previous results indicate that peripheral administration of secretin leads to robust Fos protein expression in the central nucleus of the rat amygdala. The implications of this observation on rat brain function, if any, remain unclear.
Objectives
We examined the effect of systemic secretin administration on the expression of fear-potentiated startle in rats, a behavioral response known to require an intact, functional central nucleus of the amygdala.
Methods
Rats were trained to associate a neutral light conditioned stimulus (CS) with footshock, a fear-inducing unconditioned stimulus (US). Twenty-four hours later, rats were administered secretin or vehicle and were tested immediately for their startle response to a loud noise in the presence or absence of the light.
Results
Within a dose range relevant to its clinical use in autistic children, secretin dose-dependently decreased the magnitude of fear-potentiated startle in rats.
Conclusions
This investigation provides additional evidence that systemically administered secretin can influence a neural network implicated in the acquisition and expression of emotional behaviors, including fear and anxiety.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Secretin, the first recognized hormone, was discovered by Bayliss and Starling in 1902 (Bayliss and Starling 1902). It was subsequently identified as a positive regulator of pancreatic fluid secretion (Mutt 1980; Ulrich et al. 1993) and negative regulator of gastric acid release (Lu and Owyang 1995). Secretin (Itoh et al. 1991; Kopin et al. 1991; Lan et al. 1994) and its receptor (Ishihara et al. 1991; Ulrich et al. 1993) have been cloned and the endocrine role of this receptor-ligand pair extensively studied (Leiter et al. 1993). The secretin receptor is a member of the G-protein coupled receptor class II family characterized by a large amino-terminal ectodomain containing six conserved cysteine residues (Segre and Goldring 1993; Asmann et al. 2000). In addition to their expression in the periphery, secretin and its receptor have been detected in brain at the mRNA and protein levels (Fremeau et al. 1983; Whitmore et al. 2000; Yung et al. 2001; Ng et al. 2002; Nozaki et al. 2002).
Intracerebroventricular (ICV) administration of secretin upregulates dopamine turnover and tyrosine hydroxylase activity in the hypothalamus, and inhibits prolactin release (Fuxe et al. 1979; Babu and Vijayan 1983; Samson et al. 1984). Stimulation of cAMP production by secretin was observed in cultured brain cells and in brain slice preparations (Propst et al. 1979; van Calker et al. 1980; Fremeau et al. 1986). Using cerebellum slices, secretin was shown to modulate the sensitivity of Purkinje neurons to the neurotransmitter GABA (Yung et al. 2001).
In contrast to known effects following ICV administration, there is little information regarding the central effects of peripherally administered secretin. A recent study established that peripheral, intravenous (IV) or intraperitoneal (IP), administration of secretin in rats resulted in gene expression changes in several brain regions, including most notably the central nucleus of the amygdala (Goulet et al. 2003). In addition, Fos expression was found to be upregulated in the area postrema, a circumventricular organ, suggesting that peripheral secretin could influence brain gene expression without a requirement for it to cross the blood-brain barrier (Goulet et al. 2003). The peak blood levels of secretin that induced Fos protein expression in rats were similar to the peak blood levels observed during IV treatment with secretin in humans. Additional studies using a radiolabeled secretin analog provided evidence that secretin administered IV at a clinical dose would have the ability to enter brain tissue intact and in biologically relevant concentrations (Banks et al. 2002).
An interest in secretin as a potential treatment for autism emerged when autistic children given secretin as part of a “secretin challenge” test for evaluation of pancreas function showed improvement in autistic symptoms (Horvath et al. 1998). The use of secretin in autism is controversial as additional studies both supported and refuted the conclusions reached in the original study (Sandler et al. 1999; Coniglio et al. 2001; Roberts et al. 2001). A molecular and/or biochemical definition of the mechanism(s) by which secretin may improve autism symptoms could help explain the reason for the discrepancies between clinical studies.
In this regard, the observation that peripheral secretin administration targets the amygdala may be important. A link between amygdala dysfunction and autism was suggested based on post mortem as well as structural and functional imaging studies (Bauman and Kemper 1985, 1994; Courchesne 1991; Abell et al. 1999; Baron-Cohen et al. 2000; Howard et al. 2000; Rasia-Filho et al. 2000). Moreover, the known role of the amygdala in modulating responses to social cues such as gaze, body movement and facial expressions of fear suggests that this brain structure is important for the normal development of social cognition, a core deficit in autism. These connections between autism and amygdala function lead us to postulate that the observed effect of secretin on amygdala gene expression may explain, at least in part, the mechanism of action of this peptide in autism. Here, we were interested in determining whether or not peripheral administration of secretin in rats could modulate the expression of fear-potentiated startle, a measure of fear in rodents that depends on the central nucleus of the amygdala and is sensitive to compounds that decrease fear and anxiety in humans (Davis et al. 1993).
We report the first evidence that peripherally administered secretin can modify behavior in this experimental paradigm. Because the neural circuitry of fear-potentiated startle has been well characterized, it may ultimately represent a useful experimental paradigm to determine how secretin acts in the brain to modulate amygdala-dependent responses.
Materials and methods
Animals
A total of 72 male Sprague-Dawley rats (Charles River, Portage, Mich., USA) weighing 350–450 g were used. Animals were maintained on a 12:12-h light-dark cycle (lights on at 0700 hours) with food and water continuously available. All rats were housed in group cages of four rats each in a temperature controlled (24°C) animal colony.
Apparatus
Animals were trained and tested in 8×15×15 cm Plexiglas and wire-mesh cages. The cage floor consisted of four 6.0 mm diameter stainless steel bars spaced 18 mm apart. Each cage was suspended between compression springs within a steel frame and located within a custom designed 90×70×70 cm ventilated sound-attenuating chamber. Background noise (60 dB wideband) was provided by a General Radio Type 1390-B noise generator (Concord, Mass., USA) and delivered through high frequency speakers (Radio Shack Supertweeter; Tandy, Fort Worth, Tex., USA) located 5 cm in front of each cage. Sound level measurements (sound pressure level) were made with a Bruel & Kjaer (Marlborough, Mass., USA) model 2235 sound level meter (A scale; random input) with the microphone (type 4176) located 7 cm from the center of the speaker (approximating the distance of the rat’s ear from the speaker).
Startle responses were evoked by 50 ms, 95 dB white noise bursts (5 ms rise-decay) generated by a Macintosh G3 computer soundfile (0–22 kHz), amplified by a Radio Shack amplifier (100 W; model MPA-200; Tandy), and delivered through the same speakers used to provide background noise. An accelerometer (model U321A02; PCB Piezotronics, Depew, N.Y., USA) affixed to the bottom of each cage produced a voltage output proportional to the velocity of cage movement. This output was amplified (model 483B21; PCB Piezotronics) and digitized on a scale of 0–2500 U by an InstruNET device (model 100B; GW Instruments, Somerville, Mass., USA) interfaced to a Macintosh G3 computer. Startle amplitude was defined as the maximal peak-to-peak voltage that occurred during the first 200 ms after onset of the startle eliciting stimulus.
The CS was a 3.7-s light (80 lux) produced by an 8-W fluorescent bulb (100 μs rise time) located 10 cm behind each cage. Luminosity was measured using a VWR light meter (Atlanta, Ga., USA). The US was a 0.5-s shock, delivered to the floorbars and produced by a shock generator (SGS-004; LeHigh Valley, Beltsville, Md., USA). Shock intensities (measured as in Cassella and Davis 1986) were 0.4 mA. The presentation and sequencing of all stimuli were under the control of the Macintosh G3 computer using custom designed software (The Experimenter; Glassbeads Inc., Newton, Conn., USA).
Drug administration
Secretin (Repligen Corp., Waltham, Mass., USA) (1, 3, 10, 30, and 100 μg/kg) was freshly dissolved in vehicle (10 mM trisodium citrate, pH 6.8; 0.004% polysorbate 80) and injected intraperitoneally immediately prior to testing. The drug concentration range selected for this study was chosen to bracket the Cmax attained in humans when secretin is administered IV at 0.4 µg/kg. This dose, which is used in Repligen sponsored autism clinical trials, attains a Cmax of 21.1 ng/ml. In rats, a similar Cmax is observed at a dose of 40 µg/kg. Thus, the selected doses are considered to be relevant for understanding secretin’s clinical activity.
Behavioral procedures
The experiment was run in four replications. Total group ns were as follows: vehicle (n=16), 1 μg/kg (n=12), 3 μg/kg (n=12), 10 μg/kg (n=12), 30 μg/kg (n=12), 100 μg/kg (n=8).
Matching
On each of 2 days, animals were placed in the test chambers and presented with 30, 95 dB noise bursts at a 30-s interstimulus interval (ISI). The mean startle amplitude across the 30 stimuli on the second day was used to match rats into groups with similar startle amplitudes.
Fear conditioning
On each of the next 2 days, rats were returned to the test chambers and 5 min later given the first of ten light-footshock pairings. The 0.4 mA, 0.5 s shock was delivered during the last 0.5 s of the 3.7 s light. The average intertrial interval (ITI) was 4 min (range, 3–5 min).
Testing
Twenty-four hours after the last fear conditioning session, rats were injected IP with secretin (1, 3, 10, 30, or 100 μg/kg) or vehicle and immediately were placed into the test chambers. After 5 min they received 30, 95 dB noise bursts (30 s ISI) to habituate the startle response to a stable baseline prior to the test trials. Each test trial (18 total) involved the presentation of a noise burst of one of three intensities (95, 100, or 105 dB); half of these occurred in the presence and half in the absence of the light CS. On the CS trials the startle stimulus was presented 3.2 s after the onset of the 3.7 s light. Trial types were presented in a balanced, irregular order (30 s ITI) with the restriction that each of the six trial types had to occur once within each of the three trial blocks (www.randomizer.org).
Data analysis
The initial startle stimuli of the test session were used to habituate startle responses to asymptotic levels and were not included in statistical analyses. To evaluate the effects of secretin on baseline startle amplitude, the data from the noise burst alone test trials were analyzed with a two-way ANOVA using intensity (95, 100, 105 dB) as a within-subjects variable and group (vehicle or dose of secretin) as a between-subjects variable. Fear potentiation of startle was computed for each animal by (a) subtracting mean startle amplitudes on CS test trials from those on noise burst alone test trials (“difference scores”), and (b) computing a value equal to [(mean startle amplitude on CS test trials−mean startle amplitude on noise burst alone test trials)/mean startle amplitude on noise burst alone test trials×100] (“percent scores”; Walker and Davis 2002). The potentiated startle data were analyzed with one-way ANOVAs using group as a between-subjects factor.
Results
Effect of secretin on baseline startle amplitude
Higher doses of secretin tended to suppress baseline startle, as indicated by a trend towards lower mean startle amplitudes to the leaders (data not shown) and the startle stimulus alone test trials (Fig. 1) in the groups receiving 10, 30, or 100 μg/kg but not in the other dose groups. However, these trends were not significant [Fs=1.177 and 1.688, respectively; Ps>0.05]. There was a reliable main effect of startle stimulus intensity [F(2,132)=47.525, P<0.01] and a significant linear trend relating startle amplitude to test intensity [F(1,66)=70.258; P<0.01], indicating that noise bursts of higher intensities elicited startle responses of greater amplitudes. However, the group by intensity interaction was not statistically significant [F(5,66)=1.06; P>0.05], indicating that secretin did not alter the relationship between startle amplitude and test intensity.
Effect of secretin on baseline startle amplitude. Mean startle amplitude to noise bursts of three different intensities are plotted for each group. Higher doses of secretin tended to suppress baseline startle, although this effect was not statistically significant. Stimuli of higher intensities elicited startle responses of significantly greater amplitude
Effect of secretin on expression of fear-potentiated startle
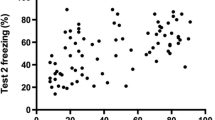
The upper panel of Fig. 2 shows that secretin dose-dependently reduced the expression of fear-potentiated startle, measured as difference scores, when administered immediately prior to testing, with the greatest reduction occurring in the group given 10 µg/kg. Statistical analysis confirmed these observations, as a one-way ANOVA revealed a significant main effect of group [F(5,66)=2.394; P<0.05] and a significant quadratic trend [F(1,66)=4.653; P<0.05].
A very similar picture emerged when percent scores were used as an alternative measure of fear potentiation of startle, as indicated in the lower panel of Fig. 2. Here the main effect of group [F(5,66)=2.284; P=0.056] just missed significance. However, post-hoc comparisons using Tukey’s HSD test indicated that the group receiving 10 μg/kg exhibited significantly less startle potentiation than did the group receiving 1 μg/kg (P<0.05), consistent with the observation that the fear potentiated startle in the 10 μg/kg group was the most reduced when difference scores were taken as the measure of interest. No other group differences reached significance.
Discussion
Our findings demonstrate that peripheral administration of secretin at clinically relevant doses can reduce significantly the expression of fear-potentiated startle. The effect of secretin on fear-potentiated startle was found to be non-monotonically related to dose, with maximal reduction at 10 µg/kg administered IP. At the higher doses, there was a trend for secretin to suppress baseline startle amplitude, perhaps reflecting a general reduction in anxiety. This effect was not significant, although it might be interesting to perform comparative studies of the effect of secretin on baseline startle in rat strains known to differ in their level of baseline anxiety, or to evaluate its effects in other putative models of anxiety in rats.
To our knowledge, this is the first time that a peripherally administered peptide has been demonstrated to influence fear-potentiated startle. Previous studies investigating the effect of small peptides on fear-potentiated startle have relied on ICV administration or direct microinjections of test substances into specific brain structures. It was recently shown that secretin administered IV can cross into the brain as an intact peptide (Banks et al. 2002), as well as stimulate neurons in the area postrema, a circumventricular organ (Goulet et al. 2003). Thus, at least two routes are available for peripheral secretin to influence brain activity related to a fear behavior. It is also possible that the central effect of secretin is mediated through vagal nerve stimulation. Militating against this latter possibility are recent results in capsaicin treated rats suggesting that the vagal nerve is not required for the ability of secretin to induce Fos expression in brain (Y. Tache, personal communication).
It is generally believed that the processing of visual information with fear evoking properties proceeds serially, initially activating the basolateral amygdala and then the central nucleus of the amygdala. It is clear that the basolateral and central nuclei of the amygdala are required for the acquisition and expression of conditioned fear (cf. Davis 2000; LeDoux 2000; Davis and Whalen 2001). We have shown previously that peripheral administration of secretin to rats upregulates Fos protein in the central nucleus of the amygdala but not in other nuclei, including the basolateral amygdala (Goulet et al. 2003). In humans, an fMRI investigation using BOLD changes in response to fearful face stimuli suggests that secretin alters amygdala responsiveness to affective stimuli (D. Yurgelun-Todd, personal communication). We postulate that in the fear-potentiated startle paradigm, secretin modulates the expression of conditioned fear memories by acting at the level of the central nucleus of the amygdala.
It is known that projections from the central nucleus of the amygdala reach hypothalamic and brainstem areas that mediate specific signs related to the expression of fear and anxiety (i.e. behavioral, neuroendocrine, autonomic), and that blocking transmission in this amygdala nucleus can alter many different measures of fear (Davis and Whalen 2001). Interestingly, the anxiolytic benzodiazepine, diazepam, used to treat anxiety disorders in humans, also blocks expression of fear-potentiated startle (Davis 1979) and increases cfos mRNA in the lateral division of the central nucleus of the amygdala in rats (Beck and Fibiger 1995). This division of the central nucleus has high concentrations of GABA-containing neurons that project to the adjacent medial division of the central nucleus, the part of the central nucleus that projects to hypothalmic and brainstem targets to produce many of the symptoms of the fear reaction. Hence, it is possible that both diazepam and secretin exert their anxiolytic effects by activating the GABA containing neurons in the lateral division of the central nucleus of the amygdala, which then inhibit amygdala output via inhibition of the medial division of the central nucleus. However, this effect in the central nucleus may result from actions initiated in the basolateral nucleus of the amygdala, because most studies looking at local infusion of benzodiazepines in the amygdala find anxiolytic effects after infusion into the basolateral rather than the central nucleus (Davis 2000). Future studies using local infusion of secretin into different amygdala nuclei could be used to test these ideas.
In conclusion, this investigation provides additional evidence that peripheral administration of secretin can influence a neural network previously implicated in the acquisition and expression of a variety of emotional behaviors including, but not limited to, those associated with fear, anxiety and other stressors. Further studies currently underway will help identify the cellular and biochemical targets of secretin within this particular neural network. In turn, these results may help explain the beneficial therapeutic effect of secretin in autism.
References
Abell F, Krams M, Ashburner J, Passingham R, Friston K, Frackowiak R, Happe F, Frith C, Frith U (1999) The neuroanatomy of autism: a voxel-based whole brain analysis of structural scans. Neuroreport 10:1647–1651
Asmann YW, Dong M, Ganguli S, Hadac EM, Miller LJ (2000) Structural insights into the amino-terminus of the secretin receptor: I. Status of cysteine and cystine residues. Mol Pharmacol 58:911–919
Babu GN, Vijayan E (1983) Plasma gonadotropin, prolactin levels and hypothalamic tyrosine hydroxylase activity following intraventricular bombesin and secretin in ovariectomized conscious rats. Brain Res Bull 11:25–29
Banks WA, Goulet M, Rusche JR, Niehoff ML, Boismenu R (2002) Differential transport of a secretin analog across the blood-brain and blood-cerebrospinal fluid barriers of the mouse. J Pharmacol Exp Ther 302:1062–1069
Baron-Cohen S, Ring HA, Bullmore ET, Wheelwright S, Ashwin C, Williams SC (2000) The amygdala theory of autism. Neurosci Biobehav Rev 24:355–364
Bauman M, Kemper TL (1985) Histoanatomic observations of the brain in early infantile autism. Neurology 35:866–874
Bauman ML, Kemper TL (1994) Neuroanatomic observations of the brain in autism. In: Bauman ML, Kemper TL (eds) The neurobiology of autism. John Hopkins University Press, Baltimore, pp 119–145
Bayliss WM, Starling EH (1902) The mechanism of pancreatic secretion. J Physiol 28:325–353
Beck CHM, Fibiger HC (1995) Conditioned fear-induced changes in behavior and in the expression of the immediate early gene c-fos: with and without diazepam pretreatment. J Neurosci 15:709–720
Cassella JV, Davis M (1986) The design and calibration of a startle measurement system. Physiol Behav 36:377–383
Coniglio SJ, Lewis JD, Lang C, Burns TG, Subhani-Siddique R, Weintraub A, Schub H, Holden EW (2001) A randomized, double-blind, placebo-controlled trial of single-dose intravenous secretin as treatment for children with autism. J Pediatr 138:649–655
Courchesne E (1991) Neuroanatomic imaging in autism. Pediatrics 87:781–790
Davis M (1979) Diazepam and flurazepam: effects on conditioned fear as measured with the potentiated startle paradigm. Psychopharmacology 62:1–7
Davis M (2000) The role of the amygdala in conditioned and unconditioned fear and anxiety. In: Aggleton JP (ed) The amygdala (vol 2) Oxford University Press, Oxford, pp 213–287
Davis M, Falls WA, Campeau S, Kim M (1993) Fear-potentiated startle: a neural and pharmacological analysis. Behav Brain Res 58:175–198
Davis M, Whalen P (2001) The amygdala: vigilance and emotion. Mol Psychiatr 6:13–34
Fremeau RT, Jensen RT, Charlton CG, Miller RL, O’Donohue TL, Moody TW (1983) Secretin: specific binding to rat brain membranes. J Neurosci 3:1620–1625
Fremeau RT, Korman LY, Moody TW (1986) Secretin stimulates cyclic AMP formation in the rat brain. J Neurochem 46:1947–1955
Fuxe K, Andersson K, Hokfelt T, Mutt V, Ferland L, Agnati LF, Ganten D, Said S, Eneroth P, Gustafsson JA (1979) Localization and possible function of peptidergic neurons and their interactions with central catecholamine neurons, and the central actions of gut hormones. Fed Proc 38:2333–2340
Goulet M, Shiromani PJ, Ware CM, Strong RA, Boismenu R, Rusche J (2003) A secretin I.V. infusion activates gene expression in the central amygdala of rats. Neuroscience 118:881–888
Horvath K, Stefanatos G, Sokolski KN, Wachtel R, Nabors L, Tildon J T (1998) Improved social and language skills after secretin administration in patients with autistic spectrum disorders. J Assoc Acad Minor Physicians 9:9–15
Howard MA, Cowell PE, Boucher J, Broks P, Mayes A, Farrant A, Roberts N (2000) Convergent neuroanatomical and behavioural evidence of an amygdala hypothesis of autism. Neuroreport 11:2931–2935
Ishihara T, Nakamura S, Kaziro Y, Takahashi T, Takahashi K, Nagata S (1991) Molecular cloning and expression of a cDNA encoding the secretin receptor. EMBO J 10:1635–1641
Itoh N, Furuya T, Ozaki K, Ohta M, Kawasaki T (1991) The secretin precursor gene. Structure of the coding region and expression in the brain. J Biol Chem 266:12595–12598
Kopin AS, Wheeler MB, Nishitani J, McBride EW, Chang TM, Chey WY, Leiter AB (1991) The secretin gene: evolutionary history, alternative splicing, and developmental regulation. Proc Natl Acad Sci USA 88:5335–5339
Lan MS, Kajiyama W, Donadel G, Lu J, Notkins AL (1994) cDNA sequence and genomic organization of mouse secretin. Biochem Biophys Res Commun 200:1066–1071
LeDoux JE (2000) The amygdala and emotion: a view through fear. In: Aggleton JP (ed) The amygdala and emotion: a view through fear. Oxford University Press, New York, pp 289–310
Leiter AB, Chey WY, Koplin AS (1993) Secretin. In: Walsh JH, Dockray G (eds) Gut peptides. Raven Press, New York, pp 147–174
Lu Y, Owyang C (1995) Secretin at physiological doses inhibits gastric motility via a vagal afferent pathway. Am J Physiol 268:1012–1016
Mutt V (1980) Secretin: isolation, structure and function. In: Glass GBJ (ed) Gastrointestinal hormones. Raven Press, New York, pp 85–126
Ng SS, Yung WH, Chow BK (2002) Secretin as a neuropeptide. Mol Neurobiol 26:97–107
Nozaki S, Nakata R, Mizuma H, Nishimura N, Watanabe Y, Kohashi R (2002) In vitro autoradiographic localization of (125)i-secretin receptor binding sites in rat brain. Biochem Biophys Res Commun 292:133–137
Propst F, Moroder L, Wunsch E, Hamprecht B (1979) The influence of secretin, glucagon and other peptides, of amino acids, prostaglandin endoperoxide analogues and diazepam on the level of adenosine 3’,5’-cyclic monophosphate in neuroblastoma×glioma hybrid cells. J Neurochem 32:1495–1500
Rasia-Filho AA, Londero RG, Achaval M (2000) Functional activities of the amygdala: an overview. J Psychiatr Neurosci 25:14–23
Roberts W, Weaver L, Brian J, Bryson S, Emelianova S, Griffiths AM, MacKinnon B, Yim C, Wolpin J, Koren G (2001) Repeated doses of porcine secretin in the treatment of autism: a randomized, placebo-controlled trial. Pediatrics 107:E71
Samson WK, Lumpkin MD, McCann SM (1984) Presence and possible site of action of secretin in the rat pituitary and hypothalamus. Life Sci 34:155–163
Sandler AD, Sutton KA, DeWeese J, Girardi MA, Sheppard V, Bodfish JW (1999) Lack of benefit of a single dose of synthetic human secretin in the treatment of autism and pervasive developmental disorder. N Engl J Med 341:1801–1806
Segre GV, Goldring SR (1993) Receptors for secretin, calcitonin, parathyroid hormone (PTH)/PTH-related peptide, vasoactive intestinal peptide, glucagon-like peptide 1, growth hormone-releasing hormone, and glucagon belong to a newly discovered G-protein linked receptor family. Trends Endocrinol Metab 4:309–314
Ulrich CD, Pinon DI, Hadac EM, Holicky EL, Chang-Miller A, Gates LK, Miller LJ (1993) Intrinsic photoaffinity labeling of native and recombinant rat pancreatic secretin receptors. Gastroenterology 105:1534–1543
van Calker D, Muller M, Hamprecht B (1980) Regulation by secretin, vasoactive intestinal peptide, and somatostatin of cyclic AMP accumulation in cultured brain cells. Proc Natl Acad Sci USA 77:6907–6911
Walker DL, Davis M (2002) Quantifying fear potentiated startle using absolute versus proportional increase scoring methods: implications for the neurocircuitry of fear and anxiety. Psychopharmacology 164:318–328
Whitmore TE, Holloway JL, Lofton-Day CE, Maurer MF, Chen L, Quinton TJ, Vincent JB, Scherer SW, Lok S (2000) Human secretin (SCT): gene structure, chromosome location, and distribution of mRNA. Cytogenet Cell Genet 90:7–52
Yung WH, Leung PS, Ng SS, Zhang J, Chan SC, Chow BK (2001) Secretin facilitates GABA transmission in the cerebellum. J Neurosci 21:7063–7068
Acknowledgement
This work was supported by the Repligen Corporation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Myers, K., Goulet, M., Rusche, J. et al. Inhibition of fear potentiated startle in rats following peripheral administration of secretin. Psychopharmacology 172, 94–99 (2004). https://doi.org/10.1007/s00213-003-1633-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-003-1633-5