Abstract
Rationale
Sedation following antihistamine use poses a danger to ambulant patients involved in daily activities such as driving.
Objective
To investigate effects of levocetirizine (5 mg), diphenhydramine (50 mg), and placebo on driving ability during normal traffic.
Methods
Forty-eight healthy volunteers participated in a double-blind, placebo-controlled, randomized clinical trial. Treatments were administrated on days 1, 2, 3 and 4, exactly 1.5 h before the start of the standardized driving test (performed on day 1 and day 4). In the standardized driving test, subjects were instructed to drive with a steady lateral position, while maintaining a constant speed (95 km/h). Primary parameter was the standard deviation of lateral position (SDLP; cm). Statistical analyses were performed separately for day 1 and day 4, using analysis of variance and an equivalence test. Equivalence to placebo was evidenced if the 95% confidence interval lay between −2.6 cm and +2.6 cm.
Results
SDLP after levocetirizine was equivalent to placebo on both day 1 (−0.66 cm; +1.12 cm) and day 4 (−0.37 cm; +1.28 cm). In contrast, SDLP after diphenhydramine differed significantly from placebo on both day 1 (P<0.0001) and day 4 (P<0.0003). On day 1, the 95% confidence interval of diphenhydramine (+1.85 cm; +3.63 cm) was partially above the upper equivalence limit (+2.6 cm), indicating clinically relevant driving impairment. On day 4, however, the 95% confidence interval of diphenhydramine (+0.74 cm; +2.38 cm) was contained within the acceptance range.
Conclusion
In contrast to diphenhydramine, driving performance was not significantly affected while using 5 mg levocetirizine once daily.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although antihistamines are intended to act peripherally, the first-generation antihistamines can easily penetrate the blood–brain barrier. In the brain, they bind non-selectively to H1 receptors. First-generation antihistamines such as triprolidine and diphenhydramine cause central nervous system (CNS) adverse effects, including sleepiness, drowsiness, and sedation. Hence, ambulatory use of these antihistamines may interfere with daily activities that require mental alertness, such as driving (Volkerts et al. 1992; Ramaekers and O'Hanlon 1994).
During the last two decades, more selective antihistamines were developed that showed equal therapeutic efficacy to those of the first-generation, but demonstrated an improved balance between CNS and peripheral effects. These second-generation antihistamines cross the blood–brain barrier less easily (Simons 1999; Kay 2000), but also bind to H1 receptors. Moreover, unlike the first-generation compounds, second-generation antihistamines have low affinity for other receptor sites in the brain (Snyder and Snowman 1987; Kay 2000), and anticholinergic adverse effects, such as blurred vision and dry mouth, are generally absent.
Levocetirizine, the R-enantiomer of cetirizine, was recently introduced as a new antihistamine drug. The recommended daily dose of levocetirizine is 5 mg, and its therapeutic indications are seasonal allergic rhinitis, perennial allergic rhinitis, and chronic idiopathic urticaria (Leynadier et al. 2001). Levocetirizine has high affinity but also a high selectivity for H1 receptors (twofold higher than that of cetirizine), whereas the S-enantiomer of cetirizine is inactive (Gillard et al. 2002). It has been established that 5 mg levocetirizine is clinically equivalent to the histamine-induced inhibition of the wheal and flare of 10 mg cetirizine (Clough et al. 2001; Wang et al. 2001) and 50 mg diphenhydramine. This equal efficacy was also demonstrated for 2.5 mg levocetirizine and 5 mg cetirizine (Devalia et al. 2001). Levocetirizine is rapidly and extensively absorbed following oral administration. Peak plasma concentrations are achieved 0.9 h after dosing, and steady state is achieved after 2 days. Peak plasma concentrations are typically 270 ng/ml and 308 ng/ml following a single 5-mg dose and 5-mg once-daily dose, respectively. Absorption is dose independent and is not altered by food. The plasma half-life in adults is 7.9±1.9 h; the mean apparent total body clearance is 0.63 ml/min/kg. Most commonly reported adverse effects (Leynadier et al. 2001) following 5-mg levocetirizine administration are of mild intensity and comprise headache (8.6%) and fatigue (5.2%).
In a study by Hindmarch and colleagues (2001), the acute (day 1) and sub-chronic (day 4) effects on cognitive function and psychomotor performance of levocetirizine (5 mg), cetirizine (10 mg), promethazine (30 mg), and loratadine (10 mg) were determined in 20 healthy volunteers. Tests comprised a critical flicker fusion test, a choice reaction time test, and a continuous tracking test. Promethazine, the reference drug, showed significant impairment on all tests on day 1. On day 4, these effects were not significant. In contrast, on both day 1 and day 4, levocetirizine, cetirizine, and loratadine did not significantly impair performance on the psychometric tests.
Gandon and Allain (2002) compared the effects of levocetirizine (5 mg) and diphenhydramine (50 mg) with placebo after acute (day 1) and sub-chronic (day 5) administration on tests of critical flicker fusion, body sway, choice reaction time, and a learning memory test. On both day 1 and day 5, levocetirizine did not significantly affect performance on any test. In contrast, on day 1 diphenhydramine significantly impaired performance on the critical flicker fusion and choice reaction tests. On day 5, diphenhydramine caused no significant impairment.
The objective of the present study was to determine the effects of levocetirizine (5 mg) on driving ability after single (day 1) and repeated (day 4) administration. A standardized on-the-road driving test, developed in the 1980s (O'Hanlon et al. 1982; O'Hanlon 1984), was used to assess driving ability. Over the years, the on-the-road driving test has been applied in a great number of studies and has been shown to be sensitive to drug-induced impairment. The major advantage of this test is its realistic nature, an aspect that is difficult to simulate in the laboratory. Several studies showed that first-generation antihistamine drugs significantly affected driving performance in the standard test (O'Hanlon and Ramaekers 1995). For example, 5 mg triprolidine (Volkerts et al. 1992) and 50 mg diphenhydramine (Ramaekers and O'Hanlon 1994) caused the subjects to operate with markedly elevated standard deviation of the lateral position (SDLP) over the entire test circuit.
The sedative effects of diphenhydramine are well known and have been demonstrated repeatedly (Roth et al. 1987; Roehrs et al. 1993a, 1993b). Behavioral studies have shown significant performance impairment on a variety of psychometric tests (Mattila et al. 1986; Moskowitz and Burns 1988; Rice and Snyder 1993; Kay et al. 1997), simulated driving (Gengo and Gabos 1987; Gengo et al. 1989, 1990; Weiler et al. 2000) and on-the-road driving during normal traffic (Ramaekers and O'Hanlon 1994). Referring to the latter, diphenhydramine is included in the present study as a positive control. In addition, a placebo condition is included in the study serving as a negative control, in order to assess baseline performance on the driving test.
The clinically relevant SDLP difference from placebo was defined as a change of at least 2.6 cm. An increment of 2.6 cm equals a SDLP elevation observed after a blood alcohol concentration of 0.05% (Louwerens et al. 1987), the legal limit for driving in The Netherlands, and corresponds to a significant rise in traffic accident risk (Borkenstein et al. 1964). It was hypothesized that levocetirizine does not significantly impair driving ability after single and repeated dosing. In contrast, diphenhydramine is expected to significantly impair driving ability on both day 1 and day 4.
Methods
Design and treatments
The study was conducted according to a double-blind, placebo-controlled, randomized, three-way, crossover design. Levocetirizine (5 mg), diphenhydramine (50 mg), and placebo were administrated orally with 240 ml tap water once daily during treatment periods comprising four successive days. All treatments were capsules of identical shape, size and color, to allow double-blind administration. They were concealed in three boxes, labeled with treatment period (1, 2 or 3) and the subject's randomization number. Treatment periods were separated by a washout period of at least 4 days. Tests were performed after both acute (day 1) and sub-chronic (day 4) administration.
Subjects
Subjects were recruited by local advertisement. The medical ethics committee of the University Medical Center Utrecht approved the study protocol, and subjects were treated according to guidelines for Good Clinical Practice and the Declaration of Helsinki and its amendments (1996). Each subject was informed beforehand about the possible risks of the driving test and the adverse effects of the treatments involved in the study. Written informed consent was obtained before their inclusion in the study, and subjects were paid for their participation. Fifty-one subjects participated in the study. One subject voluntarily withdrew from further participation in the study after completion of one treatment week, due to an adverse event (moderate nervousness). Furthermore, two subjects were non-compliant during the first treatment period. Forty-eight healthy volunteers (24 men and 24 women) completed the study. Their mean±SEM age was 23.3±2.2 years (men: 23.8±2.2 years; women: 22.8±2.0 years), mean±SEM weight was 69.8±10.3 kg (men: 75.6±9.7 kg; women: 64.0±7.2 kg), and mean±SEM height was 1.78±0.09 m (men: 1.84±0.09 m; women: 1.73±0.06 m). To confirm compliance, at all visits subjects were tested on the presence of alcohol (breath alcohol analysis) and drugs of abuse (urine drug screen, including amphetamines, barbiturates, cannabinoids, benzodiazepines, cocaine and opioids). In addition, female subjects underwent a urine β-HCG (beta human chorionic gonatropin) pregnancy test. None of the subjects was positive on any of these tests. Subjects were medically screened, used no concomitant medication other than paracetamol and oral contraceptives, and had no history of alcohol or drug abuse. They had no personal history of allergy, asthma, or of taking H1 antagonists. Before the start and at the end of the study, blood chemistry, hematology, urinalysis and 12-lead electrocardiogram were determined. These assessments were within normal limits. Subjects possessed a valid driver's license for at least 3 years, and reported having driven at least 5000 km per year, for the last 3 years. Before the start of the study, all subjects were trained on the driving test, to become familiar with test procedures, the experimental vehicle and the test circuit. To be included, an SDLP less than 22 cm was required, since it has been demonstrated that the average SDLP from placebo conditions of various studies ranges from 18 cm to 22 cm (Volkerts and Van Laar 1995). The subjects in the present study were trained to attain baseline performance, and their SDLP was smaller than 22 cm. The group mean SDLP in the training phase was 16.8 cm.
Procedure
Two subjects were scheduled each test day, and their activities were offset by 1.5 h in order to share the use of the single test vehicle. On day 1, the subjects were transported to the institute at 0800 hours. They were in a fasting condition, and nicotine and caffeine use were not allowed. After arrival at the institute, a urine drug screening, β-HCG pregnancy test, and a breath alcohol test were conducted, and all subjects were in compliance with instructions. A physical examination was completed and vital signs were checked. At 0830 hours (or 1000 hours), subjects consumed a light, standardized breakfast. Treatments were administrated in the presence of study personnel at 0900 hours (or 1030 hours). At 1015 hours (or 1145 hours), the subjects were transported to the highway circuit. Exactly 1.5 h after treatment administration the driving test started. After the driving test, visual analog scales were completed and the subjects were transported back to the institute. After arrival, subjects performed a laboratory test battery (Verster et al. 2003), followed by a medical check. Subjects remained at the institute under medical supervision until feeling capable to resume normal activities. Thereafter, they were transported back home, and cautioned not to drive their own vehicles or engage in potentially dangerous activities. Alcohol consumption was prohibited during each treatment period. On day 2 and day 3, subjects traveled by public transport to the institute and received their medication at the same time as on day 1, and remained at the institute until they felt capable of traveling home by public transport. On day 4, procedures were exactly the same as on day 1.
Driving test
A standardized driving test was performed on a two-lane primary highway during normal traffic, on a 100-km track between the cities of Utrecht and Arnhem. The test vehicle was an extensively modified Volvo station wagon. A camera, mounted on the roof of the car, measured the vehicle's lateral position relative to the painted stripe road delineation. Speed was measured from a pulse generator triggered by magnetic induction at a rate proportional to the revolutions of the wheels. The vehicle's speed and lateral position were continuously recorded, digitally sampled at 2 Hz and edited off-line to remove data that were disturbed by extraneous events (e.g., overtaking maneuvers, traffic jam). Subjects were instructed to drive with a steady lateral position within the right (slower) traffic lane, while maintaining a constant speed of 95 km/h (60 mph). Subjects were allowed to deviate from the instructions to overtake a slower moving vehicle in the same traffic lane. A licensed driving instructor who had access to dual controls sat in the right front seat, guarding the subject's safety during the driving test. Driving tests could be terminated before completion if the driving instructor or the subject felt it was unsafe to continue.
The amount of weaving of the car, measured by the SDLP (cm), is an index of driving safety, and the primary outcome parameter of the driving test. The standard deviation of speed (km/h) is a secondary parameter. Mean lateral position and speed are control variables. Time-on-task of the driving test was approximately 75 min.
Subjective assessments
Before and after the driving test, subjects rated their alertness on a 41-point equal-interval scale. After the driving test, subjects indicated the perceived quality of their driving performance on a visual analog scale, which ranged from "I drove exceptionally poorly" to "I drove exceptionally well" around a midpoint of "I drove normally". The level of effort they had to invest in performing the task was indicated on a 15-cm equal-interval scale.
Adverse events
All adverse events and undesirable experiences occurring during the study were reported.
Sample size and statistical analysis
All statistical analyses are performed separately for acute (day 1) and sub-chronic (day 4) effects. Only those subjects that completed the study (n=48) were included in the statistical analyses. A global linear model for analysis of variance was applied, including the factors subject, period, sequence, gender and treatment. Paired comparisons (levocetirizine versus placebo and diphenhydramine versus placebo) were performed two-sided (α=5%).
A test for equivalence was used to compare the outcome of the primary parameter (SDLP) of the driving test. The purpose of equivalence testing was to show whether performance after drug treatment differed from predefined limits of acceptable performance (usually performance after administration of placebo or an active treatment). Thus, in addition to statistical analyses to demonstrate whether an effect was significantly different from placebo, equivalence testing showed whether changes in test performance were also clinically relevant (Jones et al. 1996; Röhmel 1998). To test equivalence, two-sided 95% confidence intervals of the SDLP difference between each treatment and placebo were constructed and compared with the acceptance interval (−2.6 cm; +2.6 cm). With a standard deviation of 2.5, and taking an expected SDLP difference of 1 cm into account, 48 subjects were needed to reach a power of 90% for showing equivalence. Subjects were randomized using Latin squares stratified for treatment sequence.
The possible outcomes of the equivalence test were as follows:
-
1.
The 95% confidence interval lies within the acceptance range (−2.6 cm; +2.6 cm): equivalence to placebo will be accepted.
-
2.
The 95% confidence interval is entirely below 2.6 cm: clinically relevant improvement relative to placebo.
-
3.
The 95% confidence interval is entirely above +2.6 cm: clinically relevant impairment relative to placebo.
-
4.
All others: equivalence to placebo is not shown.
Results
Driving test
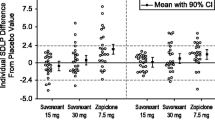
All subjects completed their driving tests. Mean±SEM scores on the driving test parameters and results from the statistical analyses are presented in Table 1. In addition, individual SDLPs (changes from placebo) are depicted in Fig. 1 (day 1) and Fig. 2 (day 4) to show the between-subjects variability in drug-induced driving impairment that accompanies many drugs.
Acute effects
It is evident from Fig. 1 that the majority of individual SDLPs after levocetirizine match placebo. Only 16.7% (8 of 48 subjects) of the SDLPs exceeded the acceptance limit of +2.6 cm. In contrast, in the diphenhydramine condition, 43.8% (21 of 48 subjects) of the subjects drove worse than the legal limit for driving in The Netherlands. Statistical analysis revealed a significant (F 2,90=23.06, P<0.0001) overall treatment effect. Paired comparisons showed that SDLP of diphenhydramine differed significantly (F 1,90=37.43, P<0.0001) from placebo. In contrast, SDLP after levocetirizine matched placebo (F<1). Moreover, equivalence testing revealed that the 95% confidence interval of diphenhydramine (+1.85 cm; +3.63 cm) fell partly above the equivalence range of placebo (−2.6 cm; +2.6 cm), whereas the 95% confidence interval of levocetirizine (−0.66 cm; +1.12 cm) was well contained within the predefined acceptance range. The effect of gender and the interaction between treatment and gender were not significant. No significant effects were found for the other parameters of the driving test.
Sub-chronic effects
It is evident from Fig. 2 that the majority of individual SDLPs after levocetirizine match placebo. Only 16.7% (8 of 48 subjects) drove worse than the acceptance limit (+2.6 cm). In contrast, in the diphenhydramine condition, 31.1% (15 of 48 subjects) drove worse than the legal limits for driving in The Netherlands. Statistical analysis revealed a significant (F 2,90=7.49, P<0.001) overall treatment effect for SDLP. Paired comparisons showed that SDLP after diphenhydramine differed significantly (F 1,90=14.17, P<0.0003) from placebo, and that SDLP after levocetirizine again matched placebo. However, in contrast to day 1, equivalence testing showed that the 95% confidence interval after both diphenhydramine (+0.74 cm; +2.38 cm) and levocetirizine (−0.37 cm; +1.28 cm) were contained within the equivalence limits (−2.6 cm; +2.6 cm). The effect of gender, and the interaction between treatment and gender were not significant for SDLP. No significant effects were found for the other parameters of the driving test.
Subjective assessments
Acute effects
Subjective assessments showed that diphenhydramine significantly reduced driving quality (P<0.0001), increased mental effort during driving (P<0.0001), and reduced alertness (P<0.0001). In contrast, no significant differences were found between levocetirizine and placebo.
Sub-chronic effects
Subjective driving quality and mental effort during driving did not significantly differ between the treatments. Relative to placebo, alertness was significantly reduced after diphenhydramine (P<0.005). In contrast, the level of alertness did not significantly differ between levocetirizine and placebo.
Adverse events
No serious adverse events were reported. One adverse event (moderate nervousness, occurring during the first washout period, 3 days after terminating the 4-day treatment with diphenhydramine) led to a premature discontinuation of the study. This subject was replaced.
Discussion
Sedation may be a direct result of histamine overload during allergic reactions in patients suffering from seasonal or perennial rhinitis. This sedation results in impaired cognitive and psychomotor functioning (Marshall and Colon 1993), decreased productivity (Blanc et al. 2001), impaired learning (Vuurman et al. 1993, 1996), poorer psychological functioning (Cauci et al. 1993), and reduced quality of life (Spaeth et al. 1996; Nolen 1997; Didier et al. 2000). Thus, allergic rhinitis itself interferes with daily activities. Treatment of allergic rhinitis with first-generation antihistamines may worsen this, due to CNS adverse effects. By enhancing the impairing effects on cognitive and psychomotor performance, antihistamines may therefore exert more discomfort than the allergic reaction itself (Vuurman et al. 1993, 1996). This led to the development of a number of new compounds, the second-generation antihistamines, which show equal efficacy to the first-generation antihistamines, but have an improved safety profile.
Levocetirizine is the active isomer of the second-generation antihistamine cetirizine and is marketed in Europe for clinical use as an antihistamine. In this context, the aim of this study with healthy volunteers was to demonstrate the effects of levocetirizine (5 mg) on car driving, probably the most common potentially dangerous daily activity.
Levocetirizine
Our results revealed no significant impairment on the driving test parameters after both single and repeated dose administration of levocetirizine. Moreover, most individual SDLPs matched placebo (85.4%), and results of the equivalence test showed that driving ability after acute and sub-chronic administration of levocetirizine was equivalent to that after placebo. Subjective assessments confirmed the objective findings of not significantly impaired driving ability. Together, these results suggest that it is safe to drive a car when treated with 5 mg levocetirizine once daily.
Diphenhydramine
Diphenhydramine significantly impaired driving ability on day 1 and day 4, thereby showing the sensitivity of the driving test.
On day 1, statistical analysis showed that SDLP after diphenhydramine was not equivalent to placebo. Subjective assessments were in line with the objective findings of significant driving impairment. That is, participants reported significantly increased mental effort during driving, decreased driving quality and reduced alertness. On day 4, driving ability was also statistically significantly impaired, but less pronounced relative to day 1. Tolerance to the effects of diphenhydramine after sub-chronic use has been previously reported by other behavioral studies (Schweitzer et al. 1994; Kay et al. 1997). However, we agree that tolerance lasts only as long as therapy is continued (Schweitzer et al. 1994; Nolen 1997) and, since antihistamines are often used only if needed, performance impairment will reappear each time therapy is initiated.
Of concern was the observation that our subjects reported equal driving quality after diphenhydramine and placebo on day 4, while driving ability was objectively impaired. It has been reported previously (Kay et al. 1997) that subjects did not recognize their driving impairment after diphenhydramine use. This is rather worrisome, because epidemiological studies showed increased traffic accident risk (Kay and Quig 2001), work-related injury (Gilmore et al. 1996; Fireman 1997) and hip fractures (Boonyaratevej et al. 2001) after first-generation antihistamine use on a daily basis. The unawareness of performance impairment is unlikely to stimulate users of sedative antihistamines to travel by public transport, instead of driving their own car.
Clinical relevance
The above-mentioned data imply that patients using diphenhydramine should be warned not to drive a car, since results from the equivalence test show that the 95% confidence interval lies partly above the acceptance limit. Although the SDLP magnitude of diphenhydramine (20.5 cm) is within the SDLP range of 18–22 cm generally observed under placebo conditions (Volkerts and van Laar 1995), it must be stressed that SDLP values both after placebo administration (day 1: SDLP=17.7 cm, day 4: SDLP=17.0 cm) and at baseline (SDLP=16.8 cm) were below this range. Our study population comprised young, healthy volunteers. Driving impairment of patients is likely to be worse than the effects found with healthy volunteers, since diphenhydramine-induced impairing effects must be added to the impairing effects of allergic rhinitis (Marshall et al. 1993; Nolen 1997; Blanc et al. 2001; Wilken et al. 2002). An on-the-road driving study in patients with untreated allergic rhinitis should be conducted to examine whether driving performance is worse than that of healthy control subjects, and to establish whether the effects on driving ability of levocetirizine and diphenhydramine are similar in patients and healthy controls.
Results from a laboratory test battery performed 3 h after administration by the same subjects (Verster et al. 2003) are in line with results from previous studies with levocetirizine (Hindmarch et al. 2001; Gandon and Allain 2002). That is, relative to placebo, after both acute and sub-chronic administration, levocetirizine did not significantly impair performance on any test. In contrast, performance was significantly impaired on all laboratory tests after acute administration of diphenhydramine. After sub-chronic administration of diphenhydramine, performance was also impaired but did not reach significance.
The major conclusion of this study is that after both acute and sub-chronic use of levocetirizine (5 mg), performance on the standardized driving test was not significantly affected.
References
Blanc PD, Trupin L, Eisner M et al. (2001) The work impact of asthma and rhinitis: findings from a population-based survey. J Clin Epidemiol 54:610–618
Boonyaratevej N, Suriyawongpaisal P, Takkinsatien A, Wanvarie S, Rajatanavin R, Apiyasawat P, the Thai Osteoporosis Study Group (2001) Physical activity and risk factors for hip fractures in Thai women. Osteoporos Int 12:244–248
Borkenstein RF, Crowther RP, Shumate RP, Ziel HB, Zylman R (1964) The role of the drinking driver in traffic accidents. Dept. of Police Administration, Indiana University, Bloomington, Indiana
Cauci M, King MG, Saxarra H, Tulloch BJ, Husband AJ (1993) A Minnesota Multiphasic Personality Inventory profile of women with allergic rhinitis. Psychosom Med 55:533–540
Clough GF, Boutsiouki P, Church MK (2001) Comparison of the effects of levocetirizine and loratadine on histamine-induced wheal, flare, and itch in human skin. Allergy 56:985–988
Devalia JL, De Vos C, Hanotte F, Baltes E (2001) A randomized, double-blind, crossover comparison among cetirizine, levocetirizine and UCB 28557 on histamine-induced cutaneous responses in healthy adult volunteers. Allergy 56:50–57
Didier A, Doussau-Thuron S, Murris-Espin M (2000) Comparative analysis of sedative effects of mequitazine and other antihistamine drugs: review of the literature. Curr Ther Res Clin Exp 61:770–780
Fireman P (1997) Treatment of allergic rhinitis: effect on occupation productivity and work force costs. Allergy Asthma Proc 18:63–67
Gandon JM, Allain H (2002) Lack of effect of single and repeated doses of levocetirizine, a new antihistamine drug, on cognitive and psychomotor functions in healthy volunteers. Br J Clin Pharmacol 54:51–58
Gengo FM, Gabos C (1987) Antihistamines, drowsiness, and psychomotor impairment: central nervous system effect of cetirizine. Ann Allergy 59:53–57
Gengo FM, Gabos C, Miller JK (1989) The pharmacodynamics of diphenhydramine-induced drowsiness and changes in mental performance. Clin Pharmacol Ther 45:15–21
Gengo FM, Gabos C, Mechtler L (1990) Quantitative effects of cetirizine and diphenhydramine on mental performance measured using an automobile driving simulator. Ann Allergy 64:520–526
Gillard M, Van der Perren C, Moguilevsky N, Massingham R, Chatelain P (2002) Binding characteristics of cetirizine and levocetirizine to human H1 histamine receptors: contribution of Lys191 and Thr194. Mol Pharmacol 61:391–399
Gilmore TM, Alexander BH, Mueller BA, Rivara FP (1996) Occupational injuries and medication use. Am J Ind Med 30:234–239
Hindmarch I, Johnson S, Meadows R, Kirkpatrick T, Shamsi Z (2001) The acute and sub-chronic effects of levocetirizine, cetirizine, loratadine, promethazine and placebo on cognitive function, psychomotor performance, and weal and flare. Curr Med Res Opin 17:241–255
Jones B, Jarvis P, Lewis JA, Ebbutt AF (1996) Trials to assess equivalence: the importance of rigorous methods. BMJ 313:36–39
Kay GG (2000) The effects of antihistamines on cognition and performance. J Allergy Clin Immunol 105:S622–S627
Kay GG, Quig ME (2001) Impact of sedating antihistamines on safety and productivity. Allergy Asthma Proc 22:281–283
Kay GG, Berman B, Mockoviak SH, Morris CE, Reeves D, Starbuck V et al (1997) Initial and steady-state effects of diphenhydramine and loratadine on sedation, cognition, mood and psychomotor performance. Arch Intern Med 157:2350–2356
Leynadier F, Mees K, Arendt C, Pinelli M-E (2001) Efficacy and safety of levocetirizine in seasonal allergic rhinitis. Acta Otorhinolaryngol Belg 55:305–312
Louwerens JW, Gloerich ABM, De Vries G, Brookhuis KA, O'Hanlon JF (1987) The relationship between drivers' blood alcohol concentration (BAC) and actual driving performance during high speed travel. In: Noordzij PC, Roszbach R (eds) Alcohol, drugs and traffic safety. Proceedings of the 10th International Conference on Alcohol, Drugs and Traffic Safety, Amsterdam, Excerpta Medica, pp 183–192
Marshall PS, Colon EA (1993) Effects of allergy season on mood and cognitive function. Ann Allergy 71:251–258
Mattila MJ, Mattila M, Konno K (1986) Acute and subacute actions on human performance and interactions with diazepam of temelastine (SK&F93944) and diphenhydramine. Eur J Clin Pharmacol 31:291–298
Moskowitz H, Burns M (1988) Effects of terfenadine, diphenhydramine, and placebo on skills performance. Cutis 42:14–18
Nolen TM (1997) Sedative effects of antihistamines: safety, performance, learning and quality of life. Clin Ther 19:39–55
O' Hanlon JF (1984) Driving performance under the influence of drugs: rationale for, and application of, a new test. Br J Clin Pharmacol 18:121S–129S
O'Hanlon JF, Ramaekers JG (1995) Antihistamine effects on actual driving performance in a standard test: a summary of Dutch experience. Allergy 50:234–242
O'Hanlon JF, Haak TW, Blaauw GJ, Riemersma JBJ (1982) Diazepam impairs lateral position control in highway driving. Science 217:79–81
Ramaekers JG, O'Hanlon JF (1994) Acrivastine, terfenadine and diphenhydramine effects on driving performance as a function of dose and time after dosing. J Clin Pharmacol 47:261–266
Rice VJ, Snyder HL (1993) The effects of Benadryl and Histamal on psychomotor performance and perceived performance. Aviat Space Environ Med 64:726–734
Roehrs T, Zwyghuizen-Doorenbos, Roth T (1993a) Sedative effects and plasma concentrations following single doses of triazolam, diphenhydramine, ethanol and placebo. Sleep 16:301–305
Roehrs T, Claiborue D, Knox M, Roth T (1993b) Effects of ethanol, diphenhydramine, and triazolam after a nap. Neuropsychopharmacology 9:239–245
Röhmel J (1998) Therapeutic equivalence investigations. Statistical considerations. Stat Med 17:1703–1714
Roth T, Roehrs T, Koshorek G, Sicklesteel J, Zorick F (1987) Sedative effects of antihistamines. J Allergy Clin Immunol 80:94–98
Schweitzer PK, Meuhibach MJ, Walsh JK (1994) Sleepiness and performance during three-day administration of cetirizine or diphenhydramine. J Allergy Clin Immunol 94:716–724
Simons FER (1999) H1-receptor antagonists: safety issues. Ann Allergy Asthma Immunol 83:481–488
Snyder SH, Snowman AM (1987) Receptor effects of cetirizine. Ann Allergy 59:4–8
Spaeth J, Klimek I, Mösges R (1996) Sedation in allergic rhinitis is caused by the condition and not by the antihistamine treatment. Allergy 51:893–906
Verster JC, Volkerts ER, van Oosterwijck AWWA, Aarab M, Bijtjes SIR, de Weert AM, Eijken EJE, Verbaten MN (2003) Acute and subchronic effects of levocetirizine and diphenhydramine on memory functioning, psychomotor performance, and mood. J Allergy Clin Immunol 111:623–627
Volkerts ER, Van Laar MW (1995) Specific review of psychometric effects of cetirizine. Allergy 50:55–60
Volkerts ER, van Willigenburg PP, van Laar MW, Maes RAA (1992) Does cetirizine belong to the new generation of antihistamines? An investigation into its acute and subchronic effects on highway driving, psychometric test performance, and EEG during driving. Hum Psychopharmacol 7:227–238
Vuurman EPFM, Van Veggel LMA, Uiterwijk MMC, Leutner D, O'Hanlon JF (1993) Seasonal allergic rhinitis and antihistamine effects on children's learning. Ann Allergy 71:121–126
Vuurman EFPM, Van Veggel LMA, Sanders RL, Muntjewerff ND, O'Hanlon JF (1996) Effects of semprex-D and diphenhydramine on learning in young adults with seasonal allergic rhinitis. Ann Allergy Asthma Immunol 76:247–252
Wang DY, Hanotte F, De Vos C, Clement P (2001) Effect of cetirizine, levocetirizine, and dextrocetirizine on histamine-induced nasal response in healthy adult volunteers. Allergy 56:339–343
Weiler JM, Bloomfield JR, Woodworth GG, Grant AR, Layton TA, Brown TL et al (2000) Effects of fexofenadine, diphenhydramine, and alcohol on driving performance. Ann Intern Med 132:354–362
Wilken JA, Berkowitz R, Kane R (2002) Decrements in vigilance and cognitive functioning associated with ragweed-induced allergic rhinitis. Ann Allergy Asthma Immunol 89:372–380
Acknowledgement
This study was financially supported by UCB Pharma.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Verster, J.C., de Weert, A.M., Bijtjes, S.I.R. et al. Driving ability after acute and sub-chronic administration of levocetirizine and diphenhydramine: a randomized, double-blind, placebo-controlled trial. Psychopharmacology 169, 84–90 (2003). https://doi.org/10.1007/s00213-003-1462-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-003-1462-6