Abstract
Abnormalities in the phosphatidylinositol 3-kinase (PI3K)/Akt signaling pathway are commonly observed in human cancers and contribute to chemotherapy resistance. Combination therapy, involving the use of molecular targeted agents and traditional cytotoxic drugs, may represent a promising strategy to lower resistance and enhance cytotoxicity. Here, we demonstrate the efficacy of an Akt inhibitor, MK-2206, in increasing the cytotoxic effect of either paclitaxel (Taxol) or cisplatin against the ovarian cancer cell lines SKOV3 (with constitutively active Akt) and ES2 (with inactive Akt). Sequential treatment of Taxol or cisplatin, followed by MK-2206, induced a synergistic inhibition of cell proliferation and effectively promoted cell death, either by inhibiting the phosphorylation of Akt and its downstream effectors 4E-BP1 and p70S6K in SKOV3 cells or by restoring p53 levels, which were downregulated after Taxol or cisplatin treatment, in ES2 cells. Combination treatment also downregulated the pro-survival protein Bcl-2 in both SKOV3 and ES2 cells, which may have contributed to cell death. In addition, we discovered that Taxol/MK-2206 or cisplatin/MK-2206 combination treatment resulted in significant enhancement of intracellular reactive oxygen species (ROS) induced by MK-2206, in both SKOV3 and ES2 cells; however, MK-2206-induced growth inhibition was reversed by a ROS scavenger only in ES2 cells. MK-2206 also suppressed DNA repair, particularly in SKOV3 cells. Taken together, our results demonstrate that the Akt inhibitor MK-2206 enhances the efficacy of cytotoxic agents in both Akt-active and Akt-inactive ovarian cancer cells but through different mechanisms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ovarian cancer is the most deadly gynecologic cancer and ranks among the top five causes of cancer death in women. Patients with early-stage disease have an 80–95 % survival rate, but the survival rate drops dramatically to 10–30 % in patients with advanced-stage ovarian cancer (Berkenblit and Cannistra 2005). Surgical tumor debulking followed by chemotherapy is currently the standard treatment for advanced ovarian cancer. First-line chemotherapy typically includes platinum-based drugs, such as cisplatin, which are known to form intrastrand and interstrand DNA adducts that inhibit replication and transcription, leading to DNA damage and cell death through apoptosis, and taxanes, such as paclitaxel (Taxol), which bind to intracellular β-tubulin and stabilize microtubules, causing growth arrest and apoptosis (Agarwal and Kaye 2003; DiSaia and Bloss 2003).
Abnormalities in the phosphatidylinositol 3-kinase (PI3K) pathway, such as amplification or activating mutations of the PIK3CA gene, overactivation of the downstream serine/threonine kinase Akt, or loss of PTEN tumor suppressor function, are common in human cancers and play a role in neoplastic transformation (Liu et al. 2009; Courtney et al. 2010). As cells progress from normal to hyperplastic and then invasive stages, PI3K/Akt signaling is activated to a higher degree and is usually accompanied by loss of apoptosis, enhanced survival, and increased proliferation. Upon PI3K activation, Akt is phosphorylated at Thr308 in the kinase domain by PDK-1, and subsequent phosphorylation at Ser473 in the C-terminal regulatory domain by other kinases is required for its full activation (Alessi et al. 1996; Liu et al. 2009). Akt activity is negatively regulated by the tumor suppressor PTEN (Liu et al. 2009; Courtney et al. 2010).
Akt activates another serine/threonine kinase mammalian target of rapamycin (mTOR) which in turn phosphorylates components of the protein synthesis machinery, including p70S6K and 4E-binding protein 1 (4E-BP1). Phosphorylation of 4E-BP1 results in the release of the translation initiation factor eIF4E, allowing for the initiation of protein synthesis. Activation of receptor tyrosine kinases or Ras oncoproteins can also enhance PI3K/Akt signaling (Liu et al. 2009; Courtney et al. 2010). Furthermore, constitutive activation of the PI3K/Akt pathway is associated with resistance to conventional chemotherapy (West et al. 2002). Therefore, targeted inhibition of the PI3K/Akt pathway is a promising strategy for cancer therapy and can also be useful for overcoming chemotherapy resistance when used in combination with other anticancer agents.
MK-2206 is an orally active allosteric Akt inhibitor that can block the interaction of Akt with other proteins via the pleckstrin homology domain, thereby preventing Akt phosphorylation and activation by upstream kinases (Lindsley et al. 2008). It has been reported that MK-2206, when combined with molecular targeted agents such as erlotinib and lapatinib or cytotoxic agents such as docetaxel and carboplatin, can synergistically inhibit proliferation of many human cancer cell lines in vitro and suppress tumor growth in mouse xenograft models (Hirai et al. 2010). Currently, MK-2206 is under development for the treatment of solid tumors. PIK3CA gene amplification and Akt activation have been found in 30~40 % of ovarian cancers and may also be associated with resistance to cisplatin and Taxol (Yuan et al. 2000; Sun et al. 2001; Peng et al. 2010). Thus, MK-2206 has the potential to increase the efficacy of cisplatin and Taxol against ovarian cancer cells.
It has been found that overexpression of constitutively active Akt partially prevents mitochondrial damage, while inhibition of Akt induces mitochondrial impairment associated with opening of the permeability transition pore (Caro and Cederbaum 2006). Therefore, MK-2206 may induce the loss of mitochondrial integrity and the overproduction of reactive oxygen species (ROS) to increase apoptosis. Previous studies also showed that inhibition of mTOR by rapamycin disrupts DNA double-strand break (DSB) repair by impairing the recruitment of proteins essential for homologous recombination (Chen et al. 2011). One such protein is BRCA1, which recognizes DNA damage lesions, translocates to DNA damage sites, forms nuclear foci at DNA lesions, functions in the DNA damage response, and is critical for maintaining genomic integrity and chromosomal stability (Scully et al. 1997; Paull et al. 2000). The Akt inhibitor MK-2206 may be able to disrupt phosphorylation and activation of mTOR and sensitize ovarian cancer cells to DNA damaging agents, such as cisplatin, by compromising DNA repair.
Here, we sought to explore whether MK-2206 could sensitize ovarian cancer cells to Taxol or cisplatin, and whether the effect was associated with Akt status. The molecular mechanisms involved were also investigated.
Materials and methods
Chemicals
MK-2206 was purchased from BioVision (Mountain View, CA, USA). Taxol, cisplatin, 2′,7′-dichlorodihydrofluorescein diacetate (DCFH-DA), and N-acetyl-l-cysteine (NAC) were obtained from Sigma-Aldrich (St. Louis, MO, USA). Stock solutions of MK-2206, Taxol, and DCFH-DA were prepared in DMSO, cisplatin in phosphate-buffered saline (PBS), and NAC in H2O.
Cell lines and cell culture
Human ovarian cancer cells SKOV3 (Akt constitutively active and p53 homozygously mutated) and ES2 (Akt inactive and one allele of p53 mutated) (Concin et al. 2003; El-Gazzar et al. 2010), purchased from ATCC (Manassas, VA, USA), were grown in McCoy’s 5A medium supplemented with 10 % fetal bovine serum and 1.5 mM l-glutamine at 37 °C in a humidified 5 % CO2 atmosphere. Normal ovarian surface epithelial cells were cultured in MCDB105/medium 199 (1:1) supplemented with 15 % fetal bovine serum, 2 mM l-glutamine and penicillin/streptomycin (Hsu et al. 2005).
Drug treatment and MTT assay
Cells were seeded in 24-well plates (1–2 × 104 cells/well) and treated with Taxol or cisplatin for 24 h, followed by MK-2206 for an additional 72 h; monotherapy controls were treated with Taxol or cisplatin for 24 h followed by DMSO for 72 h or treated with MK-2206 for 72 h. Cell viability was determined by the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay, and absorbance was measured by a plate reader at 570 nm, with a reference wavelength of 690 nm.
Combination index analysis
Combination index (CI) analysis is currently the most common method used in evaluating the nature of drug interactions in combination chemotherapy and provides useful quantitative information (Chou and Talalay 1984; Zhao et al. 2004). CI is a numerical value calculated according to the following formula:
C A,X and C B,X represent the concentrations of drug A and drug B, when used in combination to achieve x% drug effect. IC X,A and IC X,B represent the concentrations required for individual monotherapy to achieve the same x% effect. CI < 1 indicates synergy, CI = 1 demonstrates an additive effect, and CI > 1 represents antagonism. IC50 values used to calculate CI50 were obtained using Scientist software (Micromath Scientific Software, St. Louis, MO, USA).
Flow cytometric analysis of the cell cycle and apoptosis
Cells were treated with drugs as described above and then harvested and fixed in cold methanol for 30 min to overnight at 4 °C. Cells were then subjected to propidium iodide (PI) staining and flow cytometric analysis as described previously (Yu et al. 2008). Annexin V/PI two-dimensional flow cytometric analysis was also performed using a BD Annexin V fluorescein isothiocyanate (FITC) apoptosis detection kit to measure apoptosis and necrosis in drug-treated cells according to the manufacturer’s instructions (BD Biosciences, San Jose, CA, USA). Viable cells would be negative for both Annexin V (AnxV) and PI (AnxV−/PI−), while AnxV+/PI− indicates early apoptotic cells, AnxV−/PI+ indicates necrotic cells, and AnxV+/PI+ indicates late apoptotic and necrotic cells.
Western blot analysis
Cells were treated with Taxol or cisplatin for 18 h, followed by DMSO or MK-2206, for 6 or 30 h. Cells were then harvested and lysed in RIPA buffer containing protease inhibitors. Cell lysates containing ~50 μg of protein were subjected to SDS-PAGE and Western analysis as previously described (Yu et al. 2008). Proteolytic cleavage of poly(ADP-ribose) polymerase (PARP) (BD Biosciences, San Jose, CA, USA), phospho-Akt (p-Akt), total Akt, phospho-4E-BP1 (p-4E-BP1), phospho-p70S6K (p-p70S6K), phospho-mTOR (p-mTOR), phospho-p44/42 MAPK (p-ERK) (Cell Signaling, Boston, MA, USA), p53 (Calbiochem, San Diego, CA, USA), Bcl-2 (Dako, Carpinteria, CA, USA), and γ-tubulin (Sigma-Aldrich, St. Louis, MO, USA) antibodies were used.
DNA fragmentation assay
Cells were treated with Taxol or cisplatin for 24 h, followed by DMSO or MK-2206 for another 24 h, and DNA fragmentation, a hallmark of apoptosis, was then measured using the Cell Death Detection ELISAPLUS kit according to the manufacturer’s instructions (Roche Applied Science, Mannheim, Germany). This in vitro assay determines apoptosis by quantitatively measuring mononucleosomes and oligonucleosomes. Briefly, cells were lysed and the cleared lysates were incubated with a mixture of biotin-conjugated anti-histone and peroxidase-conjugated anti-DNA in a streptavidin-coated microplate for 2 h at room temperature. After washing in incubation buffer, ABTS substrate (2,2′-azino-bis(3-ethylbenzothiazoline-6-sulfonic acid)) was added to photometrically determine the amount of peroxdase retained in the immunocomplex. Absorbance was measured at 405 nm using 490 nm as a reference wavelength. The degree of apoptosis was calculated by dividing the absorbance of a drug-treated sample by that of the untreated control.
Detection of intracellular ROS generation
Cells were treated with Taxol or cisplatin for 24 h, followed by DMSO or MK-2206 for 24 h. Treated cells were incubated with 20 μM of DCFH-DA at 37 °C in a humidified atmosphere containing 5 % CO2 for 30 min and then trypsinized and washed with PBS. Cells were then centrifuged, resuspended in PBS, and subjected to flow cytometric analysis.
Immunofluorescence staining
Cells were seeded into 4-well or 8-well chamber slides. Cells were treated with the vehicle control DMSO or 10 μM MK-2206 for 24 h and then treated with 15 μM cisplatin for 1 h. Cisplatin was then washed off, and cells were incubated in medium for an additional 3 h before fixation. Cells were fixed at room temperature for 30 min in PBS-buffered 3 % paraformaldehyde/2 % sucrose solution and permeabilized for 5 min in a buffer containing 0.5 % Triton X-100, 20 mM HEPES, pH 7.4, 50 mM NaCl, 3 mM MgCl2, and 300 mM sucrose (Yu et al. 2008). Primary antibody used was BRCA1 antibody Ab-1 (MS110) (1:100 dilution, Calbiochem) with Texas red-conjugated anti-mouse at a dilution of 1:200 as the secondary antibody or γ-H2AX (1:1000 dilution, Millipore) with FITC-conjugated anti-mouse at a dilution of 1:200 as the secondary antibody. Nuclear counter-staining was performed using DAPI, and slides were mounted with antifade (Invitrogen, Carlsbad, CA, USA). Images were acquired on a fluorescence microscope (Carl Zeiss GmbH, Jena, Germany) with a 100× objective. Two hundred cells were scored for each sample, and the percentage of cells with at least ten BRCA1 nuclear foci was calculated.
Statistical analysis
Results are presented as mean ± standard deviation (SD) or mean ± standard error (SE). Statistical significance was assessed with two-sided t tests, and P values less than 0.05 (P < 0.05) were considered statistically significant.
Results
MK-2206 potentiates Taxol and cisplatin-induced growth inhibition of ovarian cancer cells
To determine whether the Akt inhibitor MK-2206 could enhance the cytotoxicity of the commonly used chemotherapeutic agents Taxol and cisplatin in ovarian cancer cell lines, SKOV3 cells expressing constitutively active Akt and ES2 cells with no active Akt were used in this study. Hirai et al. (2010) demonstrated that the combination of MK-2206 and docetaxel showed a better synergistic cytotoxic effect when MK-2206 was administered following docetaxel in breast cancer cells. In a preliminary study, we found that sequential treatments administering Taxol or cisplatin first followed by MK-2206 also showed better growth inhibitory effects than coadministration or administration of MK-2206 prior to Taxol or cisplatin. Therefore, this sequence of drug treatment was used in most of the studies to assess the combinatorial effect of Taxol/MK-2206 or cisplatin/MK-2206.
Cell viability after drug treatments was determined by the MTT assay, and the CI values, quantitative measures of drug interactions, were calculated (Chou and Talalay 1984; Zhao et al. 2004). The IC50 values of each agent in single or combination treatments, as well as the CI50 values of the Taxol/MK-2206 or cisplatin/MK-2206 combination, are listed in Fig. 1a; the concentration response curves are shown in Fig. 1b–e. The combination of Taxol and MK-2206 at a concentration ratio of 1:500 (0–40 nM of Taxol for 24 h and then 0–20 μM of MK-2206 for 72 h) displayed a significant synergistic effect (CI50 = 0.318) in SKOV3 cells (Fig. 1a, b). A synergistic effect was also observed in ES2 cells, but to a lesser extent (CI50 = 0.764) (Fig. 1a, c). Interestingly, ES2 cells, which do not express active Akt, were also susceptible to MK-2206, and the viability of ES2 cells was even lower than SKOV3 cells at 30 nM Taxol/15 μM MK-2206 or 40 nM Taxol/20 μM MK-2206 treatment concentrations.
Synergistic inhibition of cell proliferation in ovarian cancer cell lines by MK-2206 in combination with Taxol or cisplatin. Cells were treated with Taxol or cisplatin for 24 h followed by DMSO for 72 h (Taxol or cisplatin alone), MK-2206 for 72 h (MK-2206 alone), or Taxol or cisplatin for 24 h followed by MK-2206 for 72 h (Tx → MK or cis → MK). a The IC50 values of each agent in single or combination treatments and CI50 values of the Taxol/MK-2206 or cisplatin/MK-2206 combination. The concentration ratio is indicated in parentheses. b, c SKOV3 and ES2 cells were treated with Taxol alone, MK-2206 alone, or Tx → MK. The concentration ratio was Taxol/MK-2206 = 1:500. d, e SKOV3 and ES2 cells were treated with cisplatin alone, MK-2206 alone, or cis → MK. The concentration ratio was cisplatin/MK-2206 = 1:2. Cell viability was determined by the MTT assay. Data are presented as mean ± SD. Two to three independent experiments were performed in triplicate. Representative results are shown. The differences in cell viability between the combination treatment and two corresponding single treatments were mostly statistically significant except in e. ***P < 0.001; **P < 0.01; *P < 0.05
The combination of cisplatin and MK-2206 at a concentration ratio of 1:2 (0–10 μM of cisplatin and 0–20 μM of MK-2206) also displayed a synergistic effect in SKOV3 cells (CI50 = 0.759) (Fig. 1a, d) but did not result in an additive or synergistic effect in ES2 cells, for which the CI value was greater than 1 (Fig. 1a, e). Compared to SKOV3, ES2 cells were more sensitive to cisplatin, and addition of MK-2206 might have a limited enhancing effect on the cytotoxicity of cisplatin at the dose ratio of 1:2. Indeed, when cisplatin concentrations were lowered, the cisplatin → MK-2206 combination treatment (0–5-μM cisplatin, 0–25 μM MK-2206; concentration ratio 1:5) did exhibit a synergistic effect in ES2 cells, with a CI50 of 0.862 (Supplementary Fig. S1). The differences in cell viability between the combination treatment and two corresponding single treatments were mostly statistically significant in Fig. 1b–d.
Both taxol and cisplatin have been found to induce apoptosis (Agarwal and Kaye 2003). Flow cytometry and Western analysis were then used to ascertain whether MK-2206 could enhance taxol or cisplatin-induced apoptosis. ES2 cells were treated with 40 nM Taxol or 10 μM cisplatin for 24 h, followed by 20 or 10 μM MK-2206 respectively for 72 h (Taxol → MK-2206 or cisplatin → MK-2206) or DMSO for 72 h (Taxol or cispaltin alone). Cells were also treated with 10 or 20 μM MK-2206 for 72 h (MK-2206 alone) or with DMSO for 96 h (control). As shown in Fig. 2a, upper panels, treatment with 10 or 20 μM MK-2206 alone had no obvious effect on cell cycle distribution when compared to the untreated control and did not show any significant sub-G1 population (~5 %). In contrast, the sub-G1 population increased dramatically from 34.1 % in cells treated with 40 nM Taxol to 67.5 % in cells treated with 40 nM Taxol → 20 μM MK-2206 (Fig. 2a, lower left panels). The sub-G1 population was 33.3 % in cells treated with 10 μM cisplatin alone and also rose to 40.4 % in cells treated with 10 μM cisplatin → 10 μM MK-2206 (Fig. 2a, lower right panels).
MK-2206 enhances Taxol- and cisplatin-induced apoptosis. a Taxol → MK-2206 or cisplatin → MK-2206 combination increases sub-G1 levels in ES2 cells. Cells were treated with DMSO for 96 h (control) or treated with Taxol or cisplatin for 24 h followed by treatment with DMSO (Taxol or cisplatin alone) or MK-2206 (Taxol → MK-2206 or cisplatin → MK-2206) for another 72 h or treated with MK-2206 alone for 72 h. Cell cycle distribution was analyzed by flow cytometry. The percentage of sub-G1 cells is indicated. Two independent experiments were performed, and representative results are shown. b, c MK-2206 enhances cisplatin- and Taxol-induced PARP cleavage. Cells were treated with cisplatin (b) or Taxol (c) for 18 h followed by DMSO or MK-2206 for 6 h (total 24 h) or for 30 h (total 48 h). PARP cleavage was determined by Western blot analysis
PARP is considered a marker for apoptosis. SKOV3 or ES2 cells were treated with cisplatin or Taxol for 18 h followed by DMSO (cisplatin or Taxol alone) or MK-2206 (10 μM cisplatin → 10 μM MK-2206 or 30 nM Taxol → 15 μM MK-2206) for 6 h (24 h in total) or 30 h (48 h in total) and subjected to Western analysis. Cisplatin alone induced PARP cleavage in SKOV3 cells, and when combined with MK-2206, PARP cleavage was clearly increased at both 24 and 48 h (Fig. 2b, left panel). Cleaved PARP was weak in cisplatin-treated ES2 cells but increased when cells were treated with cisplatin → MK-2206 at 24 h. Cleaved PARP was more intense in cisplatin-treated ES2 cells than in cisplatin-treated SKOV3 cells at 48 h, and the increase in PARP cleavage was not as obvious after cisplatin → MK-2206 combination treatment (Fig 2b, right panel). The induction of PARP cleavage by Taxol was also detected, and when combined with MK-2206, a slight increase in PARP cleavage was observed at 48 h (Fig. 2c). Due to differences in combination treatment conditions, PARP cleavage enhanced by MK-2206 was not as dramatic as the increase in sub-G1; nevertheless, these results support the idea that MK-2206 may synergize with Taxol and cisplatin by inducing apoptosis.
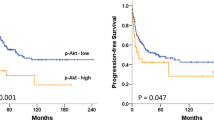
Annexin/PI two-dimensional flow cytometry was then conducted to determine cell death induced by the combination treatment. As illustrated in Supplementary Fig. S2, sequential treatment of ES2 cells with 10 μM cisplatin for 24 h followed by 10 μM MK-2206 for another 24 h mainly induced apoptosis. A more sensitive and quantitative ELISA assay for the detection of DNA fragmentation, a hallmark of apoptosis, was used to further confirm the apoptosis-inducing effects of Taxol/MK-2206 and cisplatin/MK-2206 combination treatments. SKOV3 or ES2 cells were treated with MK-2206 alone for 24 h or treated with 40 nM Taxol or 10 μM cisplatin for 24 h followed by 20 or 10 μM MK-2206 respectively for another 24 h, after which cells were harvested for the apoptosis assay. As illustrated in Fig. 3, MK-2206 alone did not cause substantial apoptosis (<2-fold of the untreated control) in both SKOV3 and ES2 cells. By contrast, Taxol and cisplatin either alone or in combination with MK-2206 significantly induced apoptosis, ranging from 13-fold to 24-fold of the untreated control (P < 0.01 compared to MK-2206 alone). Furthermore, the synergy of Taxol or cisplatin combined with MK-2206 in the induction of apoptosis was also apparent, as the observed increases in apoptosis with combination treatment greatly exceeded those of single treatments. The differences between Taxol or cisplatin single treatments and Taxol/MK-2206 or cisplatin/MK-2206 combination treatments were statistically significant (Taxol vs. Taxol → MK-2206 in SKOV3, 13.3 vs. 18.3, P = 0.047; cisplatin vs. cisplatin → MK-2206 in SKOV3, 17.4 vs. 24.3, P = 0.0018; Taxol vs. Taxol → MK-2206 in ES2, 15.5 vs. 22.1, P = 0.038; cisplatin vs. cisplatin → MK-2206 in ES2, 14.9 vs. 22.9, P = 0.011).
MK-2206 enhances Taxol and cisplatin-induced apoptosis. a SKOV3 cells were treated with Taxol or cisplatin for 24 h followed by DMSO or MK-2206 for 24 h. b ES2 cells were treated with Taxol or cisplatin for 24 h followed by DMSO or MK-2206 for 24 h. The degree of apoptosis was determined by quantitatively measuring mononucleosomes and oligonucleosomes. Results are presented as mean ± SE of two to three experiments. **P < 0.01; *P < 0.05
Taken together, MK-2206 significantly enhanced the cytotoxicity of Taxol and cisplatin in SKOV3 cells with constitutively active Akt, yet surprisingly, MK-2206 was also effective in ES2 cells with no active Akt. This effect of MK-2206 was exerted at least in part by enhancing apoptosis induced by Taxol or cisplatin.
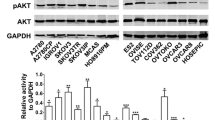
The effects of Taxol → MK-2206 or cisplatin → MK-2206 combination treatments on p-Akt and its downstream effectors
MK-2206 can inhibit the phosphorylation and activation of Akt, as well as downregulate Akt downstream effectors (Hirai et al. 2010). We next evaluated the potential attenuation of the Akt pathway by Taxol → MK-2206 or cisplatin → MK-2206 combination treatments. Western blot analysis showed a marked reduction of p-Akt in SKOV3 cells treated with Taxol → MK-2206 or cisplatin → MK-2206 for 24 or 48 h (Fig. 4a), compared with untreated and Taxol- or cisplatin-treated controls. However, total Akt levels remained unaffected by all treatment conditions. Akt can activate mTOR, which in turn phosphorylates the downstream effectors 4E-BP1 and p70S6K, leading to protein synthesis and cell growth. Phospho-4E-BP1 (T37/46) and p-p70S6K (T389) were downregulated by Taxol → MK-2206 or cisplatin → MK-2206 treatment in SKOV3 cells. By contrast, neither Taxol → MK-2206 nor cisplatin → MK-2206 treatment showed any significant influence on Akt or its downstream effector proteins in ES2 cells (Fig. 4a). These data suggest that suppression of the Akt pathway is associated with Taxol → MK-2206 and cisplatin → MK-2206 treatment-induced growth inhibition and apoptosis in SKOV3 cells, but other mechanisms may regulate cell death in ES2 cells.
The effects of Taxol → MK-2206 or cisplatin → MK-2206 treatments on Akt and ERK signaling as well as p53 and Bcl-2 protein levels. a Cells were treated with Taxol or cisplatin for 18 h, followed by DMSO or MK-2206 for 6 h (total 24 h) or for 30 h (total 48 h). b Cells were treated with Taxol or cisplatin for 18 h, followed by DMSO or MK-2206 for 6 h (total 24 h). Protein levels were determined by Western blot analysis
Although no active Akt was found in ES2 cells, the downstream effectors 4E-BP1 and p70S6K were phosphorylated, and p-4E-BP1 and p-p70S6K were not downregulated by MK-2206. ES2 cells harbor BRAF V600E and MEK1 mutations which may lead to ERK activation and Akt-independent activation of mTOR (Mendoza et al. 2011; Hanrahan et al. 2012). Indeed, as shown in Fig. 4b, mTOR and ERK were phosphorylated and activated in ES2 cells, which were not affected by MK-2206, although Taxol and cisplatin slightly lowered p-ERK. In SKOV3 cells, the levels of p-ERK were very low in untreated controls and were barely detectable after either single or combination drug treatments, whereas p-mTOR was clearly downregulated by MK-2206, indicative of Akt dependence (Fig. 4b).
Effects of Taxol → MK-2206 or cisplatin → MK-2206 treatments on p53 and Bcl-2 protein levels
To further elucidate the molecular mechanisms of MK-2206-mediated apoptosis, Western blot analysis was used to evaluate p53 and pro-survival Bcl-2 protein levels. As shown in Fig. 4b, p53 levels were downregulated by Taxol or cisplatin in ES2 cells. Addition of MK-2206 following Taxol or cisplatin significantly restored p53 levels. However, p53 was not detected in SKOV3, consistent with previous reports that SKOV3 is null for the p53 gene (Concin et al. 2003). ES2 cells express a mutant (S241F) and a wild-type p53 (Concin et al. 2003; El-Gazzar et al. 2010). Therefore, p53 restored by MK-2206 may mediate apoptosis in ES2 cells. Pro-survival Bcl-2 protein levels were decreased by Taxol or cisplatin treatment and could be further downregulated by Taxol → MK-2206 or cisplatin → MK-2206 treatment in both cell lines (Fig. 4b).
ROS are mediators of MK-2206-induced cytotoxicity in ES2 cells
Since ROS are critical regulators of apoptosis and reports have shown that MK-2206 can increase ROS levels (Cheng et al. 2011; Li et al. 2012), we sought to determine the effect of MK-2206 on ROS production. DCFH-DA is nonfluorescent in the reduced state and is hydrolyzed by intracellular esterases to 2,7-dichlorodihydrofluorescein, which is then oxidized to fluorescent 2,7-dichlorofluorescein (DCF) by ROS. The fluorescence intensity of DCF is used to measure intracellular ROS. As illustrated in Fig. 5a, ROS levels were only slightly elevated when SKOV3 and ES2 cells were treated with 20 nM Taxol or 10 μM cisplatin for 24 h, but ROS production significantly increased when cells were subsequently treated with 10 μM MK-2206 for another 24 h. Quantitative analysis revealed that compared with single treatments with Taxol or cisplatin, ROS levels were raised 3.4-fold in SKOV3 cells and 6.4-fold in ES2 cells after Taxol → MK-2206 treatments, while cisplatin → MK-2206 treatments elevated ROS levels 2.7-fold in SKOV3 cells and 4.8-fold in ES2 cells (Fig. 5b), suggesting that MK-2206 may stimulate apoptosis via ROS production.
Intracellular ROS production induced by Taxol → MK-2206 or cisplatin → MK-2206 treatment. a SKOV3 and ES2 cells were treated with Taxol or cisplatin for 24 h followed by DMSO or MK-2206 for another 24 h. The intensity of DCF fluorescence was analyzed by flow cytometry. b Quantitative data showing the mean values of relative ROS levels between Taxol or cisplatin single treatments and combination treatments. Three to four independent experiments were performed, and data are presented as mean ± SE. **P < 0.01; *P < 0.05
When NAC, a ROS scavenger, was coadministered with MK-2206 following pretreatment with 20 nM Taxol, 2 μM cisplatin, or 5 μM cisplatin, the viability of SKOV3 cells was not affected (Fig. 6a). By contrast, ES2 cell viability was significantly restored, particularly when cells were pretreated with 2 μM cisplatin (Fig. 6b). Incubation with NAC alone did not affect cell viability (data not shown). Thus, ROS may play a more important role in mediating cytotoxicity induced by the Taxol → MK-2206 or cisplatin → MK-2206 treatments in ES2 cells.
ROS scavenger NAC reverses MK-2206-induced growth inhibition in ES2 cells but not in SKOV3 cells. SKOV3 (a) and ES2 (b) cells were treated with 20 nM Taxol, 2, or 5 μM cisplatin (Cis2 or Cis5) for 24 h followed by DMSO, or 10 μM MK-2206 alone or together with 2 mM NAC for 72 h. Cell viability was determined by the MTT assay. Experiments were performed in duplicate or triplicate, and data are presented as mean ± SE. ***P < 0.001; *P < 0.05
MK-2206 disrupts BRCA1 foci formation at DNA DSBs induced by cisplatin
BRCA1 can recognize DNA DSBs and regulate DNA repair. It has been shown that inhibition of mTOR suppresses DNA DSB repair (Chen et al. 2011). Therefore, we examined whether inhibition of Akt by MK-2206 had an influence on cisplatin-induced DNA DSBs. BRCA1 expression is cell cycle-dependent and displays a nuclear dot staining pattern. After DNA damage, BRCA1 and other DNA repair proteins are recruited to DNA lesions and form large foci in the nucleus (Scully et al. 1997). As illustrated in Supplementary Fig. S3, untreated control cells in S phase showed clear nuclear dots. Large BRCA1 foci were induced by treatment with 15 μM cisplatin for 1 h in both SKOV3 and ES2 cells; however, BRCA1 foci were diminished when cells were pretreated with 10 μM MK-2206 for 24 h (Fig. 7a). Quantitative analysis revealed that approximately 41.4 and 45.0 % of cells formed large BRCA1 nuclear foci after being treated with 15 μM cisplatin in SKOV3 and ES2 cells, respectively. However, the percentage of cells with BRCA1 foci decreased to 5.4 % in SKOV3 and 25.0 % in ES2 when cells were pretreated with MK-2206 (Fig. 7b). More significant suppression of DSB repair through pretreatment with MK-2206 was observed in SKOV3 cells than in ES2 cells, consistent with the Western blot data in Fig. 4b indicating that phosphorylation of mTOR was more significantly downregulated by MK-2206 in SKOV3 than in ES2 cells. To exclude the possibility that pretreatment with MK-2206 might have a cell cycle effect and that reduced BRCA1 foci might be due to decreased DNA damage induced by cisplatin, SKOV3 and ES2 cells were stained with γ-H2AX, a marker for DNA DSBs. Results shown in Supplementary Fig. S4 indicate that pretreatment with MK-2206 did not substantially affect DNA damage induced by cisplatin. Even though cisplatin showed better growth inhibitory effects on ovarian cancer cells when administered prior to MK-2206, our preliminary data showed that pretreatment of cells with MK-2206 could also enhance the effect of cisplatin. Thus, MK-2206 may enhance the cytotoxic effect of cisplatin in part by compromising DNA repair in SKOV3 and ES-2 cells.
MK-2206 disrupts BRCA1 foci formation at DNA double-strand breaks induced by cisplatin. a Images of cells with BRCA1 foci induced by cisplatin. SKOV3 or ES2 cells were treated with or without MK-2206 for 24 h and then treated with cisplatin for 1 h. Cells were fixed 3 h later and subjected to BRCA1 staining. Images were taken at a magnification of 1,000×. Scale bar = 10 μm. b Quantitative analysis of the percentage of cells with BRCA1 nuclear foci. Each bar represents mean ± SE of three independent experiments. **P < 0.01; *P < 0.05
Discussion
Recently, Hanrahan et al. (2012) analyzed the correlation between genetic alterations and sensitivity to Akt inhibitors in serous ovarian cancer and found that genetic activation of PI3K/Akt signaling was necessary but not sufficient to confer sensitivity to selective inhibition of Akt; furthermore, cells with activated Ras signaling were relatively resistant to Akt inhibitors. SKOV3 cells carry a PIK3CA H1047R mutation that causes Akt activation, while ES2 cells harbor BRAF V600E and MEK1 D67N mutations, which result in activation of the Ras pathway. Their data showed that SKOV3 cells were very sensitive to the Akt inhibitor MK-2206 with IC50 within 0–0.3 μM and ES2 cells were more resistant with IC50 between 1.7 and 3 μM. Surprisingly, our data showed that sensitivity to MK-2206 was not substantially different in SKOV3 cells with constitutively activated Akt and ES2 cells with inactivated Akt and activated Ras signaling, with IC50 values falling within a similar range, ~20 μM (Fig. 1a). Another report indicated that the IC50 of MK-2206 was 5.1 μM in SKOV3 cells (Hirai et al. 2010). The discrepancy of IC50 values obtained by different researchers could be due to different cell culture conditions, treatment durations, or assay methods used. Nevertheless, as illustrated in Supplementary Fig. S5, MK-2206 did not affect the viability of normal ovarian surface epithelial (OSE) cells up to a concentration of 15 μM. At higher concentrations, MK-2206 did show some growth inhibitory effect on OSE cells, but to a much lesser extent (data not shown). Thus, MK-2206 displayed specificity toward ovarian cancer cells and was much less toxic to normal OSE cells.
No previous studies have compared the effects and molecular mechanisms of MK-2206 in combination with Taxol or cisplatin in SKOV3 and ES2 cells. Our results demonstrate that the Akt inhibitor MK-2206, when administered following Taxol or cisplatin, exhibited a better synergistic cytotoxic effect in SKOV3 cells than in ES2 cells. This could be explained by the constitutive phosphorylation and activation of Akt in SKOV3 cells; by inhibiting Akt phosphorylation, MK-2206 enhanced the effects of cisplatin and Taxol. The effects of cisplatin and Taxol were also enhanced by MK-2206, albeit to a lesser extent, in Akt-inactive ES2 cells. ES2 cells carrying BRAF/MEK mutations, which lead to activation of the Ras/ERK and mTOR pathways (Fig. 4), were still sensitive to MK-2206, suggesting that MK-2206 may have certain off-target effects.
Western analysis demonstrated that phosphorylation of Akt and its downstream effectors 4E-BP1 and p70S6K, which regulate protein synthesis and cell proliferation, was inhibited in SKOV3 cells treated with Taxol → MK-2206 or cisplatin → MK-2206, but p-4E-BP1 and p-p70S6K levels remained high in Akt-inactive ES2 cells, possibly due to activation of the Ras/ERK pathway (Fig. 4). However, MK-2206 restored p53 levels downregulated by Taxol or cisplatin treatment in ES2 cells. These findings suggest that MK-2206 may enhance the cytotoxic effect of Taxol and cisplatin through inhibition of protein synthesis in SKOV3 and by p53-mediated apoptosis or other unidentified mechanisms in ES2 cells. Downregulation of Bcl-2 may also contribute to apoptosis induced by Taxol → MK-2206 or cisplatin → MK-2206 in both ovarian cancer cell lines (Fig. 4b).
Previous studies have demonstrated that inhibition of Akt induces mitochondrial impairment (Caro and Cederbaum 2006), which is associated with ROS generation. ROS are crucial regulators of apoptosis, and we discovered that MK-2206 treatment following Taxol or cisplatin increased ROS levels in both SKOV3 and ES2 cells, with a more prominent effect in ES2 cells (Fig. 5a). Furthermore, MK-2206-induced growth inhibition was blocked by NAC in ES2 but not in SKOV3 cells (Fig. 5b). Therefore, production of ROS may account for the enhancement of Taxol or cisplatin cytotoxicity by MK-2206 in ES2 cells.
Inhibition of mTOR has been found to disrupt DNA DSB repair (Chen et al. 2011). As DNA DSBs are induced by cisplatin treatment and BRCA1 is known to participate in DNA repair, we examined whether the enhancement of cisplatin cytotoxicity by MK-2206 was associated with BRCA1-mediated DNA repair. Our results show that MK-2206 treatment prior to cisplatin did disrupt BRCA1 foci formation induced by cisplatin. The percentage of cells with BRCA1 foci was more dramatically decreased by MK-2206 pretreatment in SKOV3 cells as compared to ES2 cells (Fig. 7), suggesting that ES2 cells may still retain a certain level of DNA repair. Thus, suppression of BRCA1 foci formation may partly explain why growth inhibition by cisplatin and MK-2206 combination treatment is more significant in SKOV3 cells as compared to ES2 cells. This is the first demonstration that MK-2206 may compromise DNA repair in ovarian cancer cell lines, particularly in the Akt-constitutively active and p53-deficient SKOV3 cells, and provide a rationale for combination therapy of Akt inhibitors with DNA damaging agents.
In summary, we have demonstrated that MK-2206 treatment may enhance the cytotoxic effects of Taxol and cisplatin in ovarian cancer cells, regardless of Akt status, and thus may be useful in treating ovarian cancers. MK-2206 enhances cytotoxic effects through various mechanisms, and the effect may be dependent or independent of the Akt signaling pathway in different cancer cell lines. Collectively, these data establish a rationale that with the addition of Akt inhibitor MK-2206, we may increase the efficiency of standard chemotherapy and reduce side effects through the use of low-dose cytotoxic agents. More studies are needed to further clarify the detailed mechanisms involved.
References
Agarwal R, Kaye SB (2003) Ovarian cancer: strategies for overcoming resistance to chemotherapy. Nat Rev Cancer 3:502–516. doi:10.1038/nrc1123
Alessi DR, Andjelkovic M, Caudwell B, Cron P, Morrice N, Cohen P, Hemmings BA (1996) Mechanism of activation of protein kinase B by insulin and IGF-1. EMBO J 15:6541–6551
Berkenblit A, Cannistra SA (2005) Advances in the management of epithelial ovarian cancer. J Reprod Med 50:426–438
Caro AA, Cederbaum AI (2006) Role of phosphatidylinositol 3-kinase/AKT as a survival pathway against CYP2E1-dependent toxicity. J Pharmacol Exp Ther 318:360–372. doi:10.1124/jpet.106.102921
Chen H, Ma Z, Vanderwaal RP, Feng Z, Gonzalez-Suarez I, Wang S, Zhang J, Roti Roti JL, Gonzalo S, Zhang J (2011) The mTOR inhibitor rapamycin suppresses DNA double-strand break repair. Radiat Res 175:214–224
Cheng Y, Ren X, Zhang Y, Patel R, Sharma A, Wu H, Robertson GP, Yan L, Rubin E, Yang JM (2011) eEF-2 kinase dictates crosstalk between autophagy and apoptosis induced by Akt inhibition, thereby modulating cytotoxicity of novel Akt inhibitor MK-2206. Cancer Res 71:2654–2663. doi:10.1158/0008-5472.CAN-10-2889
Chou TC, Talalay P (1984) Quantitative analysis of dose-effect relationships: the combined effects of multiple drugs or enzyme inhibitors. Adv Enzym Regul 22:27–55
Concin N, Stimpfl M, Zeillinger C, Wolff U, Hefler LJ, Sedlak J, Leodolter S, Zeillinger R (2003) Role of p53 in G2/M cell cycle arrest and apoptosis in response to gamma-irradiation in ovarian carcinoma cell lines. Int J Oncol 22:51–57
Courtney KD, Corcoran RB, Engelman JA (2010) The PI3K pathway as drug target in human cancer. J Clin Oncol 28:1075–1083. doi:10.1200/JCO.2009.25.3641
DiSaia PJ, Bloss JD (2003) Treatment of ovarian cancer: new strategies. Gynecol Oncol 90:S24–32
El-Gazzar A, Perco P, Eckelhart E, Anees M, Sexl V, Mayer B, Liu Y, Mikulits W, Horvat R, Pangeri T, Zheng D, Krainer M (2010) Natural immunity enhances the activity of a DR5 agonistic antibody and carboplatin in the treatment of ovarian cancer. Mol Cancer Ther 9:1007–1018. doi:10.1158/1535-7163.MCT-09-0933
Hanrahan AJ, Schultz N, Westfal ML, Sakr RA, Giri DD, Scarperi S, Janakiraman M, Olvera N, Stevens EV, She QB, Aghajanian C, King TA, Stanchina E, Spriggs DR, Heguy A, Taylor BS, Sander C, Rosen N, Levine DA, Solit DB (2012) Genomic complexity and AKT dependence in serous ovarian cancer. Cancer Discov 2:56–67
Hirai H, Sootome H, Nakatsuru Y, Miyama K, Taguchi S, Tsujioka K, Ueno Y, Hatch H, Majumder PK, Pan BS, Kotani H (2010) MK-2206, an allosteric Akt inhibitor, enhances antitumor efficacy by standard chemotherapeutic agents or molecular targeted drugs in vitro and in vivo. Mol Cancer Ther 9:1956–1967. doi:10.1158/1535-7163.MCT-09-1012
Hsu LC, Kapali M, DeLoia JA, Gallion HH (2005) Centrosome abnormalities in ovarian cancer. Int J Cancer 113:746–751
Li Z, Yan S, Attayan N, Ramalingam S, Thiele CJ (2012) Combination of an allosteric Akt inhibitor MK-2206 with etoposide or rapamycin enhances the antitumor growth effect in neuroblastoma. Clin Cancer Res 18:3603–3615. doi:10.1158/1078-0432.CCR-11-3321
Lindsley CW, Barnett SF, Layton ME, Bilodeau MT (2008) The PI3K/Akt pathway: recent progress in the development of ATP-competitive and allosteric Akt kinase inhibitors. Curr Cancer Drug Targets 8:7–18
Liu P, Cheng T, Roberts TM, Zhao JJ (2009) Targeting the phosphoinositide 3-kinase pathway in cancer. Nat Rev Drug Discov 8:627–644. doi:10.1038/nrd2926
Mendoza MC, Er EE, Blenis J (2011) The Ras-ERK and PI3K-mTOR pathways: cross-talk and compensation. Trends Biochem Sci 36:320–328
Paull TT, Rogakou EP, Yamazaki V, Kirchgessner CU, Gellert M, Bonner WM (2000) A critical role for histone H2AX in recruitment of repair factors to nuclear foci after DNA damage. Curr Biol 10:886–895
Peng DJ, Wang J, Zhou JY, Wu GS (2010) Role of the Akt/mTOR survival pathway in cisplatin resistance in ovarian cancer cells. Biochem Biophys Res Commun 394:600–605. doi:10.1016/j.bbrc.2010.03.029
Scully R, Chen J, Ochs RL, Keegan K, Hoekstra M, Feunteun J, Livingston DM (1997) Dynamic changes of BRCA1 subnuclear location and phosphorylation state are initiated by DNA damage. Cell 90:425–435
Sun M, Wang G, Paciga JE, Feldman RI, Yuan ZQ, Ma XL, Shelley SA, Jove R, Tsichlis PN, Nicosia SV, Cheng JQ (2001) AKT1/PKBalpha kinase is frequently elevated in human cancers and its constitutive activation is required for oncogenic transformation in NIH3T3 cells. Am J Pathol 159:431–437
West KA, Castillo SS, Dennis PA (2002) Activation of the PI3K/Akt pathway and chemotherapeutic resistance. Drug Resist Updat 5:234–248
Yu YM, Pace SM, Allen SR, Deng CX, Hsu LC (2008) A PP1-binding motif present in BRCA1 plays a role in its DNA repair function. Int J Biol Sci 4:352–361. doi:10.7150/ijbs.4.352
Yuan ZQ, Sun M, Feldman RI (2000) Frequent activation of AKT2 and induction of apoptosis by inhibition of phosphoinositide-3-OH kinase/Akt pathway in human ovarian cancer. Oncogene 19:2324–2330. doi:10.1038/sj.onc.1203598
Zhao L, Wientjes MG, Au JL (2004) Evaluation of combination chemotherapy: integration of nonlinear regression, curve shift, isobologram, and combination index analyses. Clin Cancer Res 10:7994–8004. doi:10.1158/1078-0432.CCR-04-1087
Acknowledgments
This study was supported by funds from the National Taiwan University (L.C.H.). We thank Jui-Ling Hsu, She-Hung Chan, Cheng-Hsiang Huang, and Ching-Chun Huang for technical support and helpful discussion.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 223 kb)
Rights and permissions
About this article
Cite this article
Lin, YH., Chen, B.YH., Lai, WT. et al. The Akt inhibitor MK-2206 enhances the cytotoxicity of paclitaxel (Taxol) and cisplatin in ovarian cancer cells. Naunyn-Schmiedeberg's Arch Pharmacol 388, 19–31 (2015). https://doi.org/10.1007/s00210-014-1032-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-014-1032-y