Abstract
Insulin has been approved for inhaled application, but safety concerns remain, because of un-physiologically high insulin concentrations in the lung. Since insulin may act as growth factor, possible proliferative effects of insulin, insulin analogues and insulin-like growth factor-1 (IGF-1) on human lung fibroblasts were studied. As measure of proliferation [3H]-thymidine incorporation was studied in HEL-299, MRC-5, IMR-90 and primary human lung fibroblasts. In all cells, mRNA encoding IGF-1 receptors and two variants of insulin receptors was detected. Insulin and IGF-1 stimulated [3H]-thymidine incorporation in all cells. Comparison of the concentration-dependent effects in HEL-299 cells showed that IGF-1 and insulin glargine were more potent (EC50, 3 and 6 nM) and more effective (maximum increase, by 135–150%) than insulin and insulin detemir (EC50, 22 and 110 nM; maximum increase: by 80%). Proliferative effects of IGF-1 and insulin were inhibited to the same extent by an antibody (1H7) directed against the IGF-1 receptor α-subunit. Insulin-induced stimulation of [3H]-thymidine incorporation was reduced by 83% after siRNA-mediated down-regulation of IGF-1 receptor by about 75%, but not affected by a similar down-regulation of the insulin receptor. Insulin and IGF-1 caused rapid up-regulation of the early genes FOS, EGR-1 and EGR-2 as well as of the gene coding for IGF-1. In conclusion, in human lung fibroblasts insulin exerts marked proliferative effects and the pharmacological profile of this response as well as specific receptor knock-down experiments suggest mediation via IGF-1 receptors. The risk of unwanted structural lung alterations by long-term inhalative application of insulin should be considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Subcutaneous (s.c.) application of insulin or insulin analogues is part of the standard treatment not only for patients with type I diabetes, but also for many patients with type II diabetes. Although this is a very effective treatment, the regular s.c. injections are a major burden to many patients (Hunt et al. 1997; Zambanini et al. 1999). Consequently, substantial effort has been directed at developing new insulin delivery technologies. With the approval of a formulation for inhaled insulin (Exubera®) in Europe and the USA (Lenzer 2006), an insulin for a new, less invasive route of application became available.
However, concerns questioning the long-term safety of inhaled insulin have been raised, particularly as this treatment is associated with un-physiologically high insulin concentrations in the airways and lung tissue (Lenzer 2006; Ceglia et al. 2006; McMahon and Arky Ronald 2007). Although meanwhile the originator of Exubera® stopped the marketing because of commercial reasons, the safety issue of inhaled insulin remains a burden because this treatment concept is further pursued as evident from several currently running clinical trials with new formulations and more convenient application devices (Siekmeier and Scheuch 2008).
One risk may arise from the potential of insulin not only to activate insulin receptors but also to activate insulin-like growth factor-1 (IGF-1) receptors and thereby to exert proliferative stimuli in various cells. In fact, it could be shown that insulin exerted a week proliferative effect on airway smooth muscle and markedly enhanced the proliferative effect of other mitogens such as platelet derived growth factor (Gosens et al. 2003). Fibroblasts are additional cells of interest since their activation could result in long-term unwanted structural changes (Racké et al. 2008).
Therefore, the present study aimed to describe the expression of insulin and IGF receptors in human lung fibroblasts and to explore possible proliferative effects of insulin, IGF-1 and insulin analogues in these cells.
A preliminary report of the present study has been present at the Spring Meeting of the German Society of Experimental and Clinical Pharmacology (Reitzenstein et al. 2009).
Materials and methods
Culture of lung fibroblasts
HEL-299, IMR-90, and MCR-5 human lung fibroblasts (ATCC, Manassas, USA) were grown in Eagle’s MEM supplemented with 10% FCS, 2 mM l-glutamine, Earle’s BBS adjusted to contain 2.2 g/l sodium bicarbonate, 0.1 mM non-essential amino acids, 1.0 mM sodium pyruvate, 100 U/ml penicillin and 100 μg/ml streptomycin. Cells were grown in a humidified incubator at 37°C and 5% CO2 and passaged by trypsinization at nearly confluence. Early passage cells were used in experiments.
Primary human lung fibroblasts were established as described previously (Matthiesen et al. 2006) from normal areas of surgically resected lung tissue, which was obtained from lung cancer patients after thoracotomy. The protocol for obtaining human tissue was approved by the local ethics review board for human studies (Ethics Committee, Medical Faculty, University of Bonn, Bonn, Germany), and informed consent was obtained from the patient. The identity of the primary cells as being fibroblasts was confirmed by immuno-cytochemistry. At various passages all cells stained homogenously positive for the mesenchymal cell marker vimentin (Lindemann and Racké 2003). In addition, commercially available primary human lung fibroblasts form caucasian healthy donors were purchased from PromoCell (Heidelberg, Germany).
Extraction of RNA, semi-quantitative and real-time reverse transcription-polymerase chain reaction
Total RNA was isolated by help of silica gel-based membranes, according to the manufacturer’s instructions, including an additional DNase digestion step to avoid any contamination by genomic DNA (Qiagen, Hilden, Germany). First-strand cDNA was synthesised using Omniscript reverse transcriptase (Qiagen). Specific oligonucleotide primers were constructed based on human European Molecular Biology Laboratory (EMBL) sequences: human β-actin, 5′-TTCTACAATGAGCTGCGTGTGGC-3 and 5′-CCTGCTTGCTGATCCACATCTGC-3′; human insulin receptor 5′-AATCCGCACGGTGAAGATGACC-3′ and 5′-ACGAGCAGAGCAGCAGAAGAAGC-3′ (this primer pair would allow to amplify mRNA of both splicing variants of the insulin receptor, IR-A and IR-B); human IGF-1 receptor 5′-CATTGAGGAGGTCACAGAC-3′ and 5′-CAAAGACGAAGTTGGAGGC-3′; human IGF-2 receptor 5′-GGTGCCATGCTATGTGTTTG-3′ and 5′-TGGCAGCACTCATTGTTCTC-3′. Polymerase chain reaction (PCR) amplification was performed using Taq DNA polymerase and specific primers in a programmable thermal reactor (Biorad) with initial heating for 3 min at 94°C, followed by 23 cycles for β-actin, 30 cycles for insulin and IGF-1 receptors, and 35 cycles for IGF-2 receptors, 45 s of denaturation at 94°C, annealing (30 s) at 56°C (β-actin, insulin-, IGF-1 and IGF-2 receptor), extension at 72°C (1 min), and a final extension for 10 min at 72°C. PCR cycle number was optimized to obtain an amplification within the linear range. PCR products were separated by a 1.2% agarose gel electrophoresis and documented by a video documentation system and the optical density of the bands was quantified by the RFLPscan 2.01 software (MWG, Ebersberg, Germany).
Transcripts of insulin and IGF-1 receptor and of some additional genes putatively regulated by insulin and/or IGF-1 were further analyzed by quantitative real-time PCR using the fluorescence dye SYBR Green. Quantitative PCR was performed by monitoring the fluorescence of SYBR Green dye on a Stratagene Mx3000P real-time PCR system or a Roche Light Cycler 480 instrument. Applied primer pairs were specific for the sequences of insulin receptor, 5′-AGGAGCCCAATGGTCTGA-3′ and 5′-GAGACGCAGAGATGCAGC-3′; IGF-1 receptor, 5′-CGATGTGTGAGAAGACCACCA-3′ and 5′-ATTTTCTGGCAGCGGTTT-3′; Fos, 5′-ATGATGTTCTCGGGCTTCAACGCA-3 and 5′-GTATCAGTCAGCTCCCTCCTCCGGT-3′, EGR-1, 5′-GCAGCAGCAGCAGCACCTTCAAC-3 and 5′-GACTGGTAGCTGGTATTGAGGGCCTTC-3′, EGR-2, 5′-GAGGAGCAAATGATGACCGCCAAG-3 and 5′-AGGTGGAGGTGGTGGCTGCTGAC-3′, IGF-1, 5′-TGGTGGATGCTCTTCAGTTCGTGTGT-3 and 5′-GATCCTGCGGTGGCATGTCACTCT-3′, and the housekeeping gene GAPDH-(1) 5′-TCCTGTTCGACAGTCAGCCGCAT-3 and 5′-TGAAGACGCCAGTGGACTCCACG-3′ or GAPDH-(2) 5′-CTGCACCACCAACTGCTTAGC-3′ and 5′-GGCATGGACTGTGGTCATGAG-3′, which was used for normalization.
Amplification conditions were as follows: 10 min polymerase activation at 95°C and 45 cycles at 95°C for 30 s, 55°C for 30 s and 72°C for 30 s for insulin receptor, IGF-1 receptor and GAPDH-(2) and for all other primer pairs as follows: pre-incubation 10 min, 95°C to activate the antibody-blocked Taq polymerase (hot start), followed by 45 cycles of 10 s denaturation at 95°C and 105 s of annealing/elongation at 72°C. Fluorescence was measured at 82°C to avoid interference of any small by-products (e.g. primer dimers) if present.
Relative quantification of mRNA levels was based on the crossing point (CP) values of the amplification curves, determined by the second derivative maximum method as previously described (Mayer et al. 2002). The CP value indicates the cycle in which the PCR product begins to increase exponentially. The lower the CP value the higher is the concentration of the target cDNA in the sample and vice versa. The housekeeping gene GAPDH served as internal reference. Standard curves were created to relate change in CP (ΔCP) to fold change. For most primer pairs the amplification efficacy was 1.9-fold per cycle. Fold change is then determined by the equation fold change =1.9ΔCP. Alternatively, changes in the expression mRNA levels were expressed as percent of individual controls using the ΔΔCT methods as described (Haag et al. 2008).
[3H]-thymidine incorporation
Cells were trypsinized, harvested and seeded into 12-well dishes at a density of 105 cells per well in culture medium containing 10% FCS. After a 5 h consolidation period medium was changed to serum-free for 12 h, then test compounds were added and cells were cultered for another 28 h. [3H]-Thymidine (37 kBq) was present for the last 24 h of the experiment. Thereafter, cells were washed twice in ice-cold PBS and radioactivity incorporated into DNA was extracted as described previously (Freitag et al. 1996; Matthiesen et al. 2006). Briefly, cells were denatured in TCA (10%) for 10 min, washed in ice-cold PBS and DNA was extracted during incubation for 1 h in 0.1 M NaOH at 37°C. 300 μl portions of the supernatant solution were neutralised, combined with scintillation cocktail (Lumac LSC, Groningen, Netherlands) and radioactivity was determined by liquid scintillation spectrometry in a Packard 2100 TR liquid scintillation analyzer. External standardisation was used to correct for counting efficiency.
Cell count
Cells were grown in serum-free medium in absence or presence of test substances for 5 days and trypsinized at the end of the incubation period. Cells were resuspended in medium, and 200 μl of cell suspension were diluted into 10 ml of a ready-to-use isotonic saline solution (CASYton®). This dilution was counted immediately in a CASY®CellCounter + Analyzer System (Innovatis, Bielefeld, Germany).
Transfection of siRNA
SiRNA transfection of HEL-299 cells basically followed the previously described protocol (Haag et al. 2008). 24 h after seeding 4 × 104 HEL-299 cells in 12-well plates with 10% FCS containing medium, the latter was changed to FCS- and antibiotic-free condition including a washing step. Cells were transfected with either siRNA oligos against insulin receptor (siRNA 50 nM, s 5′-CUACGUGACAGACUAUUUAtt-3′, as 5′-UAAAUAGUCUGUCACGUAGaa-3′, Applied Biosystems, Foster City, CA), IGF-I receptor (siRNA 50 nM, s 5′-CCGAAGAUUUCACAGUCAAtt-3′, as 5′-UUGACUGUGAAAUCUUCGGct-3′, Applied Biosystems, Foster City, CA) or On-Target plus® siRNA (50 nM, Thermo Fischer Scientific, Waltham, MA) as a negative control using Lipofectamine™ RNAiMAX (1,5 μl/ml, Invitrogen, Karlsruhe, Germany). siRNA complexes containing medium was removed after 12 h and cells were allowed to consolidate for further 12 h under FCS- and antibiotic-free condition prior to be used for analysis of receptor expression (RNA or protein extraction) or proliferation assays. BLOCK-iT™ Fluorescent Oligo (100 nM, Invitrogen, Karlsruhe, Germany) was used to monitor the transfection efficacy.
Western blot analysis
Cellular proteins were extracted in RIPA buffer (50 mM Tris–HCl (pH 7.5), 150 mM NaCl, 0.5% sodium deoxycholat, 1% Nonidet P-40, 0.1% (wt/vol) SDS, 2 mM EDTA (pH 8.0)) containing the protease inhibitors PMSF (1 mM), pepstatin A (0.7 μg/ml), and leupeptin (0.5 μg/ml). A total of 10 μg protein portions were mixed with reducing protein loading buffer (Roti-Load 1; Roth, Karlsruhe, Germany) and boiled for 3 min. Samples were separated on 10% acrylamide trisglycine precast gels (Invitrogen, Karlsruhe, Germany) using the NUPAGE-buffer system (Invitrogen, Karlsruhe, Germany) and transferred (20% methanol, 25 mM Tris, 192 mM glycine) to polyvinylidine difluoride membranes (Millipore, Billerica, MA). Blots were blocked in 5% dried milk protein Tris-buffered saline–Tween (150 mM NaCl, 50 mM Tris, 0.05% Tween 20), and proteins were detected by use of mouse monclonal anti-human insulin receptor (β-subunit) antibody (CT-3) (Calbiochem, Darmstad, Germany) and rabbit polyclonal anti-human IGF-1 receptor (β-subunit) antibody (C-20) (sc-713, Santa Cruz Biotechnology, Santa Cruz, CA). Bands were visualized by peroxidase-conjugated secondary goat antibodies (Bio-Rad, Hercules, CA) employing Boehringer Mannheim chemoluminescence blotting substrate peroxidase (Roche, Mannheim, Germany), then blots were exposed to Hyperfilm enhanced chemiluminescence (Amersham Biosciences, Piscataway, NJ).
2-Deoxy-[3H]-glucose uptake
HEL-299 human lung fibroblasts were trypsinized, harvested and seeded into 12-well dishes at a density of 105 cells per well and cultured to nearly confluency in presence of 10% FCS. Prior to initiating the uptake assay, cells were rapidly washed twice at 37°C with phosphate buffered Krebs–Ringer (PBKR) (NaCl 130 mM, Na2HPO3 10 mM, KCl 5 mM, MgSO4 2,5 mM, CaCl2 1 mM, pH 7,4) followed by 20 min incubation in 1 ml PBKR (37°C) in absence or presence of 1 μM insulin. Sugar uptake was initiated by the addition of 2-deoxy-d-[3H]-glucose (37 kBq) at a final assay concentration of 0.01–100 μM for 10 min at different temperatures (4–37°C). Assays were terminated by two rapid washes with ice-cold PBKR. Cells were solubilized with 0.1% SDS, the supernatant was combined with scintillation cocktail (Lumac LSC, Groningen, The Netherlands) and radioactivity was determined by liquid scintillation spectrometry in a Packard 2100 TR liquid scintillation analyzer.
Statistical analysis
All values are means ± SEM of n experiments. Statistical significance of differences was evaluated by ANOVA followed by Dunnett or Bonferroni test using GraphPad InStat (GraphPad Software, San Diego, USA). P < 0.05 was accepted as significant. IC50 values were calculated by the use of computer programmes (GraphPad Prism, GraphPad Software, San Diego, USA).
Drugs and materials
Human recombinant insulin, penicillin-streptomycin solution, PD 098059 (2-(2′-amino-3′- methoxyphenyl)-oxanaphthalen-4-one), rapamycin, SB 203580 (4-(4-fluorophenyl)-2-(4-methylsulfinylphenyl)-5-(4-pyridyl)-1H-imidazole), thyrphostin AG1024, trypsin, U 73122 (1-(6-((17beta-3-methoxyestra-1,3,5(10)-trien-17-yl)amino)hexyl)-1H-pyrrole-2,5-dione) and wortmannin were purchased from Sigma (Deisenhofen, Germany); insulin detemir (Levemir®, contains 14.2 mg detemir insulin/ml) and human recombinant insulin (Actrapid®, contains 3.5 mg insulin/ml) from Novo Nordisk (Bagsvrd, Denmark); insulin glargine (Lantus®, contains 3.64 mg insulin glargine/ml) from Sanofi Aventis (Frankfurt, Germany); [3H]-thymidine and 2-deoxy-d-[3H]-glucose from Perkin Elmer (Rodgau, Germany); Eagle’s minimal essential medium (MEM) with Earl’s salts and l-glutamine, non-essential amino acids were from PAA (Cölbe, Germany); fetal calf serum (FCS) from Biochrom (Berlin, Germany); mouse monoclonal antibody directed against the α-subunit of IGF-1 receptor (1H7, sc-461) and rabbit polyclonal antibody directed against the β-subunit of IGF-1 receptor (sc-713) (Santa Cruz Biotechnology, Santa Cruz, CA); mouse monoclonal antibody directed against the β-subunit of insulin receptor (CT-3) (Calbiochem, Merck4Bioscience, Darmstadt, Germany); Taq DNA polymerase from Invitrogen (Karlsruhe, Germany); Omniscript reverse transcriptase, RNeasy Mini kit and RNase-free DNase set from Qiagen (Hilden, Germany). Oligodesoxynucleotides for RT-PCR were obtained from MWG Biotech (Ebersberg, Germany).
Results
Expression of insulin and IGF-1 receptors in human lung fibroblasts
Using RT-PCR, expression of mRNA encoding insulin receptors and IGF-1 receptors was detected in different human lung fibroblasts cell lines (HEL-299, MRC-5 and IMR-90) as well as in primary human lung fibroblasts (Fig. 1), whereas IGF-2 receptor mRNA could not be detected in any of these cells (data not shown). Two splicing variants of the insulin receptor have been identified (Kosaki et al. 1998). The primer pair used in the present study for the amplification of insulin receptor mRNA stretched over the splicing region of the insulin receptor gene and therefore allowed to amplify mRNA of both splicing variants of the insulin receptor. In fact, the RT-PCR for insulin receptor showed two amplification products and their size corresponded well to the expected size of amplification products of the respective mRNA for the insulin receptor splicing variants which differ by the absence (IR-A) or presence (IR-B) of exon 11 (36 base pairs) (Seino and Bell 1989; Belfiore et al. 2009). Thus, human lung fibroblasts (cell lines and primary cells) appear to express both splicing variants of the insulin receptor.
Samples of RT-PCRs of human insulin and IGF-1 receptors (R) on RNA isolated from different human lung fibroblasts (primary cells (phLFb) from lung tissue of cancer patients (P) and healthy donors (hD) and the cell lines HEL-299, MRC-5 and IMR-90). Cells were grown in 35 mm culture dishes to confluency, total RNA was isolated, treated with DNase and used for RT-PCR with primers specific for the human insulin and IGF-1 receptors or β-actin. To control quality of RNA preparation and cDNA synthesis, PCR was also performed for β-actin. Shown are two out of at least four similar observations
In all cells studied, the expression of insulin and IGF-1 receptors was confirmed at protein level by immuno-blot analysis (Fig. 2).
Immuno-blot analysis of protein extracts from different human lung fibroblasts cell lines (HEL-299, MRC-5 and IMR-90) as well as primary human lung fibroblasts (phLFb) from lung tissue of cancer patients (P) and healthy donors (hD) using commercially available antibodies against human insulin and IGF-1 receptors (R) and α-tubulin. Cells were grown in 55 mm culture dishes to confluency and cellular proteins were extracted using RIPA buffer (see “Materials and methods”). Given are representative samples of SDS-PAGE loaded with 10 μg proteins onto the gel. Shown are two out of at least four similar observations
Proliferative effects of insulin and IGF-1 in human lung fibroblasts
In a first series of experiments the proliferative effects of insulin and IGF-1 were studied in different human lung fibroblast cell lines (IMR-90, MRC-5 and HEL-299 cells) as well as in primary human lung fibroblasts. In all human lung fibroblasts studied, insulin increased in a concentration-dependent manner the incorporation of [3H]-thymidine (Fig. 3), which is a useful measure of cell proliferation as it reflects de novo DNA synthesis. There were some differences in the magnitude of the maximal effects observed in the different cell lines. The smallest effect, an increase by about 60%, was observed in MRC-5 cells, whereas in primary lung fibroblasts, IMR-90 and HEL-299 cells an increase between about 120% and 200% was detected (Fig. 3a–e). Likewise, IGF-1 caused similar concentration-dependent increases in the incorporation of [3H]-thymidine in the different human lung fibroblast cell lines and primary human lung fibroblasts (Fig. 3f–j). For further studies HEL-299 cells were chosen for most of the following experiments.
Effects of insulin (a–e) and IGF-1 (f–j) on [3H]-thymidine incorporation in different human lung fibroblast cell lines (HEL-299, MRC-5 and IMR-90) and primary human lung fibroblasts from lung tissue of cancer patients (P) and healthy donors (hD). After trypsinization cells were disseminated in 12-well dishes (105 cells/well) and cultured for 5 h in medium containing 10% FCS. Thereafter, medium was changed to serum-free conditions. After 12-h insulin or IGF-1 were added at the concentrations given below the columns, and cells were cultured for additional 28 h. [3H]-Thymidine (37 kBq) was present for the last 24 h. [3H]-Thymidine incorporation is expressed as% of the mean value of the respective controls of each individual cell preparation. Given are means + SEM of n ≥ 9, mostly ≥12. Significances of differences versus controls (Ctr.): *P < 0.05; **P < 0.01; ***P < 0.001
A detailed comparison of the concentration-dependent effects of IGF-1, insulin and the insulin analogues detemir and glargine is given in Fig. 4a. IGF-1 showed a steep concentration response curve and was more potent (EC50, 3 nM) and more effective (maximum increase by about 150%) than insulin (EC50, 22 nM, maximum increase by about 80%). The profile of insulin glargine with an EC50 of 6 nM and a maximum increase by about 135% resembled very much that of IGF-1, whereas insulin detemir showed the lowest potency (EC50, 110 nM) and an effectiveness comparable to that of insulin. Since insulin glargine and insulin detemir were used in the commercially available formulation (Lantus® and Levemir®, respectively), insulin was additionally studied in its commercially available formulation (Actrapid®). The potency of Actrapid® appeared to be similar to that of pure insulin, and up to 1 μM the concentration response curves of Actrapid® and pure insulin were almost super-imposable. However, at higher concentrations the concentration response curve of Actrapid® became bell shaped with some loss of effects at 10 μM (Fig. 4a). In order to test whether the effect of insulin and IGF-1 were additive, the effect of maximally effective concentrations of insulin and IGF-1 were studied in combination. As shown in Fig. 4b, IGF-1 exerted again a stronger stimulatory effect than insulin and the effects of insulin and IGF-1 were not additive. In contrast, the stimulatory effect of IGF-1 in combination with insulin was significantly lower than that of IGF-1 alone.
Effects of IGF-1, insulin (Ins) and its analogues insulin glargine and insulin detemir on [3H]-thymidine incorporation in HEL-299 human lung fibroblasts. After trypsinization cells were disseminated in 12-well dishes (105 cells/well) and cultured for 5 h in medium containing 10% FCS. Thereafter, medium was changed to serum-free conditions. After 12 h test compounds, at the concentrations given, were added and cells were cultured for additional 28 h. [3H]-Thymidine (37 kBq) was present for the last 24 h. [3H]-Thymidine incorporation is expressed as percent of the mean value of the respective controls of each individual cell preparation. Given are means ± SEM of n ≥ 9, mostly ≥12. Significances of differences: ***P < 0.0001, versus controls (Ctr.); #P < 0.0001 versus Ins; +P < 0.05 versus IGF-1
The growth stimulatory effect of insulin and IGF-1 in HEL-299 was also demonstrated by an increased cell count. When cells were cultured under FCS-free condition, 5 days exposure to a maximally effective concentration of insulin or IGF-1 caused an increase in the number of cells by 61 ± 9% and 53 ± 10%, respectively (each n = 12; p < 0.001 and p < 0.01, respectively).
Proliferative effects of insulin in human lung fibroblasts are mediated via IGF-1 receptor
In order to test whether the proliferative effect of insulin and IGF-1 were mediated via IGF-1 receptors, interaction experiments with an antibody (1H7) directed against the α-subunit of the IGF-1 receptor and known to have antagonistic properties at this receptor (Yoshimoto et al. 1999; Maloney et al. 2003; Li et al. 1993) were performed. This antibody caused a slight, but significant reduction of basal proliferation and inhibited the insulin- and IGF-1-induced stimulation of proliferation to the same degree, maximally by about 60% (Fig. 5).
Effects of insulin (Ins) and IGF-1 in absence or presence of the monoclonal antibody 1H7 (sc-461) directed against the IGF-1 receptor α-unit (IGF-Ab) on [3H]-thymidine incorporation in HEL-299 human lung fibroblasts. After trypsinization cells were disseminated in 12-well dishes (105 cells/well) and cultured for 5 h in medium containing 10% FCS. Thereafter, medium was changed to serum-free conditions. After 11.5 h the antibody and in the respective experiments 0.5 h later Ins or IGF-1 were added at the dilutions/concentrations given and cells were cultured for additional 28 h. [3H]-Thymidine (37 kBq) was present for the last 24 h. [3H]-Thymidine incorporation is expressed as percent of the mean value of the respective controls of each individual cell preparation. Given are means + SEM of n ≥ 6, mostly ≥ 12. Significances of differences: **P < 0.01; ***P < 0.001; versus respective controls (Ctr.); +++P < 0.001 versus Ins alone
To further illuminate the role of IGF-1 and/or insulin receptors in mediating the proliferative effects of insulin in human lung fibroblasts, specific knock-down of IGF-1 and insulin receptors by siRNA technique was performed. In initial experiments, it was observed that the stimulatory effect of insulin was abrogated when proliferation was studied immediately following 24 h exposure to the transfection reagent Lipofectamin. However, the proliferative effect of insulin was preserved, when cells were allowed to recover for 12 h after a 12 h exposure period to Lipofectamin (data not shown). Fortunately, a protocol with 12 h transfection with siRNA against insulin or IGF-1 receptor followed by 12 h consolidation under transfection reagent-free condition resulted in a marked (by about 75%) and specific down-regulation of either the insulin or IGF-1 receptor, as demonstrated at the level of mRNA (Fig. 6a) and receptor proteins (Fig. 6b). After transfection of nsRNA, insulin enhanced the [3H]-thymidine incorporation by 97 ± 10% (Fig. 6c), an effect similarly to those observed in different series of experiments in naive cells (compare with data shown in Figs. 3, 4, 5 and 7). However, after transfection of siRNA against IGF-1 receptor, i.e. after down-regulation of this receptor by about 75%, insulin-induced stimulation of [3H]-thymidine incorporation was reduced by 83% (Fig. 6c), whereas after transfection of siRNA against the insulin receptor, insulin-induced stimulation of [3H]-thymidine incorporation remained preserved, although this treatment caused a down-regulation of the insulin receptor comparable to that of the IGF-1 receptor in the corresponding IGF-1 receptor knock-down experiments (Fig. 6a, b). Notably, after insulin-receptor knock-down the proliferative effect of insulin was even slightly, but significantly enhanced (Fig. 6c).
Effects of siRNA directed against the insulin (Ins) or IGF-1 receptor on mRNA (a, determined by real-time PCR) and protein (b and c, determined by Western blot) levels of insulin and IGF-1 receptors and the proliferative response to 10 μM insulin (c, determined by [3H]-thymidine incorporation) in HEL-299 human lung fibroblasts. Cells were cultured for 24 h in presence of 10% FCS. Transfection with specific siRNA or non-silencing (ns) RNA was carried out 24 h after seeding in FCS- and antibiotic-free medium using Lipofectamine™ RNAiMAX. Transfection medium was removed after 12 h and cells were allowed to consolidate for further 12 h under FCS- and antibiotic-free condition. Thereafter, total RNA or proteins were extracted or cells were used for proliferation assay as described in Fig. 3. Height of columns: a mRNA expression as percent of the individual controls (nsRNA) (ln2(ΔΔCT)*100), means + SEM of n = 6. b Samples of original Western blots. c protein expression as percent of the individual controls (densitometric evaluation, arbitrary units normalized over α-tubulin), means + SEM of n = 6. d [3H]-thymidine incorporation expressed as% of the mean value of the respective controls (nsRNA) of each individual cell preparation, means + SEM of n = 9. Significance of differences versus respective controls: **P < 0.01; ***P < 0.001
Effects of insulin (Ins; a–f) or IGF-1 (j–l) in absence and presence of inhibitors of different putative pro-proliferative signal transduction pathways on [3H]-thymidine incorporation in HEL-299 human lung fibroblasts. After trypsinization cells were disseminated in 12-well dishes (105 cells/well) and cultured for 5 h in medium containing 10% FCS. Thereafter, medium was changed to serum-free conditions. After 12 h the inhibitors (at the concentrations given) were added; 30 min later 1 μM insulin or 30 ng/ml IGF-1 were added and cells were cultured for additional 28 h. [3H]-Thymidine (37 kBq) was present for the last 24 h. Given are means + SEM of n ≥ 9. [3H]-Thymidine incorporation is expressed as percent of the mean value of the respective controls (in absence of inhibitors) of each individual cell preparation. Significances of differences: *P < 0.05, ***P < 0.001 vs respective value in absence of insulin or IGF-1; +<0.05, +++P < 0.01 vs Ctr
Analysis of signal pathways involved in the proliferative effects of insulin and IGF-1 in human lung fibroblasts
In order to illuminate possible signal transduction pathways involved in the pro-proliferative effects of insulin and IGF-1, interaction experiments with different specific inhibitors of potentially pro-proliferative pathways were performed. Thyrphostin AG1024, a potent and specific inhibitor of the tyrosine kinase activity of insulin and IGF-1 receptors caused a marked reduction of basal [3H]-thymidine incorporation and almost prevented the stimulatory effects of insulin and IGF-1 (Fig. 7a, g). As shown in Fig. 7, inhibitors of phospholipase C (U 73122), p38 MAP kinase (SB 203580), ERK MAP kinase (PD 098059), PI3 kinase (wortmannin) and mTOR (rapamycin), they all exerted significant inhibitory effects on basal incorporation of [3H]-thymidine, with SB 203580 being the strongest (inhibition of more than 90%) and U 73122 the weakest (inhibition by about 35%) inhibitor (Fig. 7b–f, h–l). Nonetheless, in presence of any of these inhibitors insulin and IGF-1 showed clear stimulatory effects on [3H]-thymidine incorporation (Fig. 7b–f, h–l). In absolute terms, as shown in Fig. 7, these stimulatory effects of insulin and IGF-1 were somewhat smaller, particularly in case of SB 203580 and rapamycin. However, the relative increases in [3H]-thymidine incorporation in relation to the reduced levels in presence of these pathway inhibitors were at least similar to those observed under control conditions or even significantly higher as in presence of SB 203580 (for both insulin and IGF-1) or U 73122 for IGF-1.
Lack of metabolic effect of insulin in human lung fibroblasts
Activation of glucose transport is a classical metabolic effect induced by insulin in various cells. HEL-299 fibroblasts showed a concentration- and temperature-dependent accumulation of 2-deoxy-d-[3H]-glucose (Fig. 8a, b). Neither short nor long time exposure to insulin resulted in significant alterations of 2-deoxy-d-[3H]-glucose uptake (Fig. 8b). In addition to the data shown in Fig. 8, various other incubation and pre-exposure schedules were tested and did not reveal any significant effect of insulin on 2-deoxy-d-[3H]-glucose (data not shown).
Concentration- (a) and temperature-dependent (b) uptake of 2-deoxy-d-[3H]-glucose in HEL-299 human lung fibroblasts and lack of effect of insulin (c). Cells were grown to nearly confluency and serum staved for 20 h, washed twice with phosphate buffered Krebs–Ringer (PBKR, pH 7.4) and incubated for 20 min in PBKR containing 2-deoxy-d-[3H]-glucose at the concentration given (a) or at 100 μM (b, c) at 37°C (310 K; a, c) or different temperatures as indicated (b). In the respective experiments insulin (Ins; 10 μM) was present either 20 min or 20 h prior to the exposure to 2-deoxy-d-[3H]-glucose. 2-Deoxy-d-[3H]-glucose accumulation is expressed in absolute terms (a, b) or as percent of the mean value of the respective controls of each individual cell preparation (c). Given are means ± SEM of n ≥ 3
Concentration-dependent effects of insulin and IGF-1 on the expression of selected genes in human lung fibroblasts
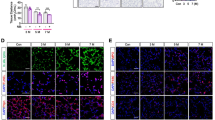
In order to detect further effects of insulin and IGF-1 in human lung fibroblasts potential effects on the expression of various genes were screened. Figure 9 shows samples of genes (Fos, ERG-1 and ERG-2 and IGF-1) in which a marked, concentration-dependent up-regulation was detected after 1 h exposure to insulin or IGF-1. Interestingly, for the up-regulation of the expression of ERG-1 and ERG-2 as well as for IGF-1 mRNA, IGF-1 was substantially more potent than insulin, comparable to the potencies of IGF-1 and insulin in the above described proliferation assays. However, with regard to the induction of Fos, insulin showed a substantially higher potency and was equally potent compared with IGF-1.
Concentration-dependent effects of insulin and IGF-1 on mRNA expression of Fos, EGR-1 and -2 and IGF-1. Hel-299 cells were incubated for 1 h with ascending concentrations of insulin and IGF-I as indicated. The expression of the early genes FOS, EGR-1 and EGR-2 as well as of the gene coding for IGF-1 was determined by quantitative real-time PCR as described in the “Materials and methods” section. Data were normalised to the housekeeping gene GAPDH and are given as fold change versus negative control (no ligand added). Each data point represents the mean ± SEM of n = 3–4
Discussion
The present study demonstrates expression of insulin receptors and IGF-1 receptors in different human lung fibroblast cell lines (HEL-299, MRC-5 and IMR-90) as well as in primary human lung fibroblasts (Fig. 1). Using RT-PCR, mRNA encoding insulin receptors and IGF-1 receptors was detected, whereas transcripts for IGF-2 receptors could not be detected. For the insulin receptor two amplification products were detected (Fig. 1), corresponding to its splicing variants IR-A and IR-B which differ by the absence (IR-A) or presence (IR-B) of exon 11 (36 base pairs) (Seino and Bell 1989; Belfiore et al. 2009). By Western blot analysis the expression of insulin receptors and IGF-1 receptors was confirmed at the protein level in all cell lines studied as well as in the primary human lung fibroblasts (Fig. 2).
In all three cell lines as well as in the primary cells, insulin and IGF-1 exerted clear stimulatory effects on proliferation, but IGF-1 was substantially more potent than insulin (Fig. 3). A more detailed characterization of these proliferative effects was performed in HEL-299 cells. Although the maximum effects caused by insulin and IGF-1 showed some variation in different series of experiments, in all sets, in which insulin and IGF-1 were studied in parallel IGF-1 induced a stronger stimulatory effect than insulin (Figs. 4a, b and 5). Moreover, when present in maximally effective concentrations, the proliferative effects of insulin and IGF-1 were not additive; on the contrary, the proliferative response induced by insulin in combination with IGF-1 was significantly smaller than that caused by IGF-1 alone. One explanation for these observations could be that the proliferative effects of insulin are mediated via activation of IGF-1 receptors, at which insulin may act as partial agonist. Binding studies showed that at the IGF-1 receptor the affinity of insulin glargine is substantially higher and that of insulin detemir significantly lower than that of insulin, whereas at the insulin receptor the affinity constants of both insulin analogues are somewhat lower than that of insulin (Kurtzhals et al. 2000). Thus, the pharmacological profile described in Fig. 4 (rank order of potency: IGF-1 ≥ insulin glargine > > insulin > insulin detemir) also supports the assumption that the proliferative effects of insulin, like those of IGF-1, are mediated via IGF-1 receptors. Unfortunately, selective antagonists for IGF-1 and insulin receptors are not available. However, several antibodies, among them the monoclonal antibody 1H7, directed against the α-subunit of the IGF-1 receptor have been shown to antagonize IGF-1 receptor activation (Yoshimoto et al. 1999; Maloney et al. 2003; Li et al. 1993). The observations, that the proliferative effects of IGF-1 and insulin were inhibit by 1H7 with similar effectiveness (Fig. 5), further supports the conclusion that insulin stimulates proliferation in human lung fibroblasts via activation of IGF-1 receptors. Finally, this conclusion is also supported by the experiments in which either the insulin or the IGF-1 receptor had been down-regulated by siRNA. Down-regulation of IGF-1 receptor by about 75% resulted in a reduction of the insulin-mediated proliferative effect by 83% (Fig. 6c), whereas after a similar down-regulation of the insulin receptor, the proliferative effect of insulin was even slightly stronger (Fig. 6c). Thus, the insulin receptor not only does not contribute to the proliferative effects, but it appears that activation of the insulin receptor may oppose the proliferative effects mediated via IGF-1 receptor. Such an action of insulin could be an alternative explanation for the above discussed observation that insulin attenuated the proliferative effect of IGF-1 (Fig. 4b). Basically in line with the present observations is a recent report showing that in human fibroblasts of which the tissue origin remained unknown, IGF-1 and insulin glargine induced clear proliferative effects, which were markedly reduced by siRNA-mediated IGF-1 receptor knock-down. However, insulin was studied only in a low concentration of 10 nM, which may preferentially activate insulin receptors, and showed only minor proliferative effects (Eckardt et al. 2007).
The insulin receptors expressed in human lung fibroblasts appear not to play a significant role in the regulation of cellular glucose uptake (Fig. 8), a classical metabolic effect of insulin. Whether insulin exerts other “metabolic” effects in human lung fibroblasts was not tested, as the focus of the present study was to characterize putative growth effects of insulin. However, possible effects of insulin and IGF-1 on early response genes, Fos and ERG-1 and ERG-2 were tested and a marked up-regulation of these genes was observed after 1 h exposure to either insulin or IGF-1. Notably, the high potency of insulin to stimulate the expression of Fos (Fig. 9) suggests that this effect might be mediated via the insulin receptor. On the other hand, the potency of insulin to up-regulation of ERG-1 and ERG-2 was substantially lower compared with IGF-1, suggesting that these effects like those on proliferation might be mediated via the IGF-1 receptor.
Unfortunately, at present no data are available about the local insulin concentrations in the airways and lung tissue after inhalative application of insulin. The recommended single therapeutic dose of Exubera® was 6 mg (1.03 μmol) or more. Since according to the product information provided by FDA (http://www.accessdata.fda.gov/drugsatfda_docs/label/2008/021868s016s017lbl.pdf) and EMEA (http://www.emea.europa.eu/humandocs/PDFs/EPAR/exubera/H-588-PI-en.pdf) about 40% of this dose (i.e. around 410 μmol) may reach the lower airways, it is estimated that local peak concentrations after insulin inhalation are likely to be in the higher nanomolar to lower micromolar range. In the present experiments the EC50 for the proliferative effects of insulin in human lung fibroblast was 22 nM, strongly supporting that the present observations are of clinical relevance when insulin is administered by inhalation.
In order to illuminate the down-stream signaling mediating the proliferative effects of insulin and IGF-1 several putative pro-proliferative pathways were inhibited by specific inhibitors. Thyrphostin AG1024, a potent and specific inhibitor of the tyrosine kinase activity of insulin and IGF-1 receptors (Párrizas et al. 1997) prevented both the proliferative effect of insulin and IGF-1 confirming that specific activation of tyrosine kinase is the crucial event for the proliferative effect of insulin and IGF-1. Interestingly, thyrphostin AG1024 caused a marked reduction of basal proliferation suggesting that IGF-1 signaling might drive already basal proliferation. In fact, expression and release of IGF-1 has been described in fibroblasts of different tissues (e.g. Johnson et al. 1998; Ludwig et al. 1999; Saygun et al. 2008) and observations from our laboratory confirm—so far at the level of mRNA—that also MRC-5 clearly express IGF-1 which was even up-regulated after exposure to IGF-1 or insulin, whereby IGF-1 was much more potent than insulin suggesting mediation via IGF-1 receptors (Fig. 9).
In contrast to the effect of thyrphostin AG1024, inhibition of phospholipase C by U 73122, p38 MAP kinase by SB 203580, ERK MAP kinase by PD 098059, PI3 kinase by wortmannin or mTOR by rapamycin did not prevent proliferative effects of insulin and IGF-1, although all these pathways appear to mediate pro-proliferative signals as each of the inhibitors caused significant reduction of the basal proliferation, although at different magnitude. The smallest effect, a reduction by about 35% was caused by the phosholipase C inhibitor U 73122 (Fig. 7b, h) and the strongest effect, a reduction by more than 90%, was observed after inhibition of p38 MAP kinase (Fig. 7d, j). Insulin and IGF-1 were able to exert significant pro-proliferative effects after inhibition of either of these pathways. It is evident from the data shown in Fig. 7 that in absolute terms the increase in proliferation caused by insulin or IGF-1 was reduced, particularly in presence of the p38 MAP kinase inhibitor SB 203580. However, when the reduced levels of proliferation in presence of these inhibitors were taken into account, the relative increases induced by insulin or IGF-1 were comparable to the effects observed under control condition. We tend to conclude from these data that activation of several of these pathways may contribute to the proliferative effects of insulin and IGF-1, but none of them might be crucial because of considerable redundancy.
In conclusion, the present study shows that insulin in concentrations, which are likely to occur locally in the airways when administered by inhalation, exerts marked proliferative effects via activation of IGF-1 receptors. Therefore, the risk that long-term inhalative application of insulin might result in unwanted structural lung changes should be considered.
References
Belfiore A, Frasca F, Pandini G, Sciacca L, Vigneri R (2009) Insulin receptor isoforms and insulin receptor/insulin-like growth factor receptor hybrids in physiology and disease. Endocr Rev 30:586–623
Ceglia L, Lau J, Pittas AG (2006) Meta-analysis: efficacy and safety of inhaled insulin therapy in adults with diabetes mellitus. Ann Intern Med 145:665–675
Eckardt K, May C, Koenen M, Eckel J (2007) IGF-1 receptor signalling determines the mitogenic potency of insulin analogues in human smooth muscle cells and fibroblasts. Diabetologia 50:2534–2543
Freitag A, Reimann A, Wessler I, Racké K (1996) Effects of bacterial lipopolysaccharides (LPS) and tumor necrosis factor-α (TNF-α) on rat tracheal epithelial cells in culture: morphology, proliferation and induction of NO synthase. Pulm Pharmacol 9:149–156
Gosens R, Nelemans SA, Hiemstra M, Grootte Bromhaar MM, Meurs H, Zaagsma J (2003) Insulin induces a hypercontractile airway smooth muscle phenotype. Eur J Pharmacol 481:125–131
Haag S, Warnken M, Juergens UR, Racké K (2008) Role of Epac1 in mediating anti-proliferative effects of prostanoid EP2 receptors and cAMP in human lung fibroblasts. Naunyn-Schmiedeberg’s Arch Pharmacol 378:617–630
Hunt LM, Valenzuela MA, Pugh JA (1997) NIDDM patients’ fears and hopes about insulin therapy. The basis of patient reluctance. Diab Care 20:292–298
Johnson DW, Saunders HJ, Baxter RC, Field MJ, Pollock CA (1998) Paracrine stimulation of human renal fibroblasts by proximal tubule cells. Kidney Int 54:747–757
Kosaki A, Nelson J, Webster NJ (1998) Identification of intron and exon sequences involved in alternative splicing of insulin receptor pre-mRNA. J Biol Chem 273:10331–10337
Kurtzhals P, Schäffer L, Sørensen A, Kristensen C, Jonassen I, Schmid C, Trüb T (2000) Correlations of receptor binding and metabolic and mitogenic potencies of insulin analogs designed for clinical use. Diabetes 49:999–1005
Lenzer J (2006) Inhaled insulin is approved in Europe and United States. BMJ 332:321
Li SL, Kato J, Paz IB, Kasuya J, Fujita-Yamaguchi Y (1993) Two new monoclonal antibodies against the alpha subunit of the human insulin-like growth factor-I receptor. Biochem Biophys Res Commun 196:92–98
Lindemann D, Racké K (2003) Glucocorticoid inhibition of interleukin-4 (IL-4) and interleukin-13 (IL-13) induced up-regulation of arginase in rat airway fibroblasts. Naunyn-Schmiedeberg’s Arch Pharmacol 368:546–550
Ludwig CU, Menke A, Adler G, Lutz MP (1999) Fibroblasts stimulate acinar cell proliferation through IGF-I during regeneration from acute pancreatitis. Am J Physiol 276:G193–G198
Maloney EK, McLaughlin JL, Dagdigian NE, Garrett LM, Connors KM, Zhou XM, Blättler WA, Chittenden T, Singh R (2003) An anti-insulin-like growth factor I receptor antibody that is a potent inhibitor of cancer cell proliferation. Cancer Res 63:5073–5083
Matthiesen S, Bahulayan A, Kempkens S, Fuhrmann R, Stichnote C, Haag S, Juergens UR, Racké K (2006) Muscarinic receptors mediate stimulation of human lung fibroblast proliferation. Am J Respir Cell Mol Biol 35:621–627
Mayer P, Ammon S, Braun H, Tischmeyer H, Riechert U, Kahl E, Höllt V (2002) Gene expression profile after intense second messenger activation in cortical primary neurons. J Neurochem 82:1077–1086
McMahon GT, Arky Ronald A (2007) Inhaled insulin for diabetes mellitus. N Engl J Med 356:497–502
Párrizas M, Gazit A, Levitzki A, Wertheimer E, LeRoith D (1997) Specific inhibition of insulin-like growth factor-1 and insulin receptor tyrosine kinase activity and biological function by tyrphostins. Endocrinology 138:1427–1433
Racke K, Haag S, Bahulayan A, Warnken M (2008) Pulmonary fibroblasts, an emerging target for anti-obstructive drugs. Naunyn-Schmiedeberg’s Arch Pharmacol 378:193–201
Reitzenstein U, Fuhrmann M, Mayer P, Enzmann H, Racké K, Warnken M (2009) Characterization of proliferative effects of insulin in human lung fibroblasts. Naunyn-Schmiedeberg’s Arch Pharmacol 379:Suppl 1–Suppl 10
Saygun I, Karacay S, Serdar M, Ural AU, Sencimen M, Kurtis B (2008) Effects of laser irradiation on the release of basic fibroblast growth factor (bFGF), insulin like growth factor-1 (IGF-1), and receptor of IGF-1 (IGFBP3) from gingival fibroblasts. Lasers Med Sci 23:211–215
Seino S, Bell GI (1989) Alternative splicing of human insulin receptor messenger RNA. Biochem Biophys Res Commun 159:312–316
Siekmeier R, Scheuch G (2008) Inhaled insulin—does it become reality? J Physiol Pharmacol 59(Suppl 6):81–113
Yoshimoto H, Ishihara H, Ohtsuru A, Akino K, Murakami R, Kuroda H, Namba H, Ito M, Fujii T, Yamashita S (1999) Overexpression of insulin-like growth factor-1 (IGF-I) receptor and the invasiveness of cultured keloid fibroblasts. Am J Pathol 154:883–889
Zambanini A, Newson RB, Maisey M, Feher MD (1999) Injection related anxiety in insulin-treated diabetes. Diabetes Res Clin Pract 46:239–246
Acknowledgement
This work was supported by the Federal Institute for Drugs and Medical Devices (V-9908/68602/2007). The paper contains part of the Ph.D. thesis of UR. We thank Sabine Mering for excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
M. Warnken and U. Reitzenstein contributed equally
Rights and permissions
About this article
Cite this article
Warnken, M., Reitzenstein, U., Sommer, A. et al. Characterization of proliferative effects of insulin, insulin analogues and insulin-like growth factor-1 (IGF-1) in human lung fibroblasts. Naunyn-Schmied Arch Pharmacol 382, 511–524 (2010). https://doi.org/10.1007/s00210-010-0561-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-010-0561-2