Abstract
Recent evidence suggests that metformin shows beneficial effects in experimental models of neuroinflammatory diseases. The aim of the present study was to determine the effect of metformin on phagocytosis and acidification of lysosomal/endosomal compartments in rat primary microglia in the presence of lipopolysaccharide (LPS) and/or beta-peptides (25–35), (1–40), and (1–42). Metformin increased the phagocytosis of fluorescent microspheres in the presence or absence of all the beta-peptides. However, the drug had no effect on the phagocytosis in LPS-stimulated microglia regardless of the presence of all the beta-peptides. Metformin acidified the lysosomal/endosomal compartments in the presence or absence of the beta-peptide 1–40 in both resting and activated microglia. To elucidate the mechanism of metformin action, we used 5-aminoimidazole-4-carboxamide-1-β-d-ribofuranoside as an activator of adenosine monophosphate-activated protein kinase (AMPK) and compound C as a confirmed pharmacological inhibitor of AMPK. We have shown that metformin increased AMPK activity in microglial cells and that all observed effects are AMPK-dependent because the pretreatment of microglia with compound C reversed the effects of the drug. Since degradation of proteins in lysosomal/endosomal compartments depends largely on their phagocytosis and acidification, metformin may be beneficial in proteinopathies affecting the brain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Microglia constantly control the content and evaluate the safety of neuronal microenvironment, which reciprocally regulates these cells. Microglia, functionally resembling peripheral macrophages, tackle their task with the presentation of antigens, phagocytosis, and the production of cytokines and toxic molecules (Hanisch and Kettenmann 2007). Phagocytosis and degradation of abnormal proteins with neurotoxic properties, such as fibrillar forms of amyloid β-peptides, are the main mechanism of limiting brain pathologies associated with their accumulation. The experimental data imply that increased acidification of lysosomes may be the key factor that determines the ability of microglia to internalize and degrade amyloid plaques (Majumdar et al. 2007). For this reason, the potential therapeutic strategies that both acidify microglial lysosomes and attenuate the inflammatory response might be particularly beneficial.
Metformin, introduced clinically in Europe in the 1950s, is the only drug of the biguanide class currently used in the treatment for type 2 diabetes. The results of recent clinical and experimental studies suggest that metformin, apart from its hypoglycemic action, may attenuate both peripheral and central inflammatory reactions. It was shown that metformin attenuated pro-inflammatory response in endothelial cells (Isoda et al. 2006), diminished human aortic smooth muscle cell proliferation (Li et al. 2005) and ameliorated macrophage activation (Mamputu et al. 2003). Lately, metformin is increasingly recognized as a drug directly acting on the central nervous system. Importantly, it was proved that the drug crosses the blood–brain barrier and accumulates in the rodent brain (Wilcock and Bailey 1994). For this reason, metformin is increasingly recognized as a drug acting directly on the central nervous system and being tested in various experimental models of neurodegeneration and neuroinflammation (Wilcock and Bailey 1994). So far, it was shown that metformin prolonged the survival time in the transgenic mouse model of Huntington’s disease and in the rat model of cancer-induced anorexia (Ma et al. 2007; Ropelle et al. 2007). Furthermore, the drug deteriorated the migration and invasion of U87 and LN229 glioma cells (Beckner et al. 2005), attenuated the induction of experimental autoimmune encephalomyelitis (Nath et al. 2009), and exhibited neuroprotective effect against etoposide-induced apoptosis in primary cortical neurons (El-Mir et al. 2008).
Adenosine monophosphate (AMP)-activated protein kinase (AMPK) activation constitutes the best known mechanism of metformin action (Zhou et al. 2001). At present, it is also known that some of metformin biological responses are not limited to activation of AMPK but mediated by AMPK-independent mechanisms including inhibition of such different cellular targets as p70S6K1 (Vazquez-Martin et al. 2009), p38 mitogen-activated protein kinase, and protein kinase C (Saeedi et al. 2008).
AMPK is a highly conserved heterotrimeric serine/threonine kinase involved in the regulation of cellular metabolism and energy distribution. AMPK is an intracellular metabolic sensor which, through the reduction of adenosine-5′-triphosphate (ATP)-consuming processes and stimulation of ATP-generating pathways, maintains cellular energy homeostasis. AMPK activation occurs through phosphorylation at a specific threonine residue (Thr172) on the α subunit (Towler and Hardie 2007). Recently, it was also shown that AMPK is involved in the regulation of endosome and lysosome pH through direct interaction with electrogenic H+-pumping V-ATPase (Hallows et al. 2009).
Based on the properties of metformin described above, we hypothesized that it may affect the phagocytosis and acidification of the lysosomal/endosomal compartments in microglia in the presence of lipopolysaccharide (LPS) and/or beta-peptides (25–35), (1–40), and (1–42). Additionally, to determine if mechanism of metformin action is AMPK-dependent, we measured phospho-AMPK/AMPK ratio and AMPK activity and, in parallel experiments, we applied 5-aminoimidazole-4-carboxamide-1-β-d-ribofuranoside (AICAR) as an activator of AMPK and compound C as a confirmed pharmacological inhibitor of AMPK.
Materials and methods
Reagents
Metformin (1,1-dimethylbiguanide hydrochloride); AICAR (5-aminoimidazole-4-carboxamide-1-β-d-ribofuranoside); compound C (6-[4-(2-piperidin-1-yl-etoxy)-phenyl]-3-pyridin-4-yl-pyrazolo[1,5-a] pyrimidine); beta-amyloid peptides (1–40), (1–42), and (25–35); LPS (lipopolysaccharide, Escherichia coli serotype 0111:B4); trypan blue; 5-bromo-2′-deoxyuridine (BrdU); 3-(4,5-dimethylthazol-2-yl)-2,5-diphenyltetrazolinum bromide (MTT); dimethyl sulphoxide (DMSO); pH buffers (pH 4.5–8.0); adenosine-5′-triphosphate; adenosine monophosphate; nigericin; cytochalasin D; hydrochloric acid; ammonium sulfate; hydrogen peroxide; fetal bovine serum (FBS); Dulbecco's modified Eagle's medium (DMEM); digitonin; phosphate buffer solution (PBS); and poly-d-lysine were purchased from Sigma-Aldrich (St. Louise, MO). Carboxylate-modified Fluospheres® (1 μm in diameter, yellow-green, 505/515 nm range) and dextran (molecular mass of 70 kDa) double-labeled with fluorescein (FITC) and tetramethylrhodamine (TMR) were from Molecular Probes (Eugene, OR). SAMS peptide was from Millipore (Billerica, MA). [γ-32P]ATP (6000 Ci/mmol, EasyTides) was purchased from PerkinElmer Life Sciences (Boston, USA). Antibiotic–antimycotic solution (penicillin, streptomycin, and fungizone) and trypsin were obtained from Invitrogen (Carlsbad, CA). Antibodies against AMPK and phospho-AMPK (phospho-AMP-activated protein kinase, Thr172) were obtained from Santa Cruz Biotechnology (Santa Cruz, CA). Antibody against glial fibrillary acetic protein (GFAP), microtubule associating protein-2 (MAP-2), BrdU, and β-actin were from ABCAM Inc. (Cambridge, MA). Lectin Ricinus Communis Agglutinin-1 (RCA-1) was from Vector Laboratories (Burlingame, CA).
Cell cultures and drug treatment
Primary mixed glial cultures were prepared from 2-day-old postnatal Wistar rat pups as described previously (Labuzek et al. 2005). Briefly, their cerebral cortices were aseptically excised and carefully stripped off the blood vessels and meninges on ice. Cerebral cortical fragments were dissociated by soft trituration in ice-cold culture medium [Dulbecco’s/DMEM (4.5 g glucose/L)] with 10% heat-inactivated FBS, 2 mM glutamine, 100 IU/mL penicillin, 100 μg/mL streptomycin, and 5 μg/mL fungizone, resuspended in culture medium, and brought to a single-cell suspension by repeated pipeting. The suspension was filtered sequentially through a cell strainer 70 and 40 μm meshes (Becton Dickinson, NJ). Dissociated cells were seeded (20 × 106 cells per dish) on poly-d-lysine-coated 100 mm Petri dishes (Becton Dickinson, NJ) and incubated at 37°C in humidified 5% CO2/95% air (CO2 incubator, Haereus, Germany). The medium was replenished 1 day after plating and changed every 4–6 days. After plating, the cells were cultured for 13–15 days until confluence.
To identify astrocytes, the cultures were stained immunocytochemically with GFAP, a specific marker for astrocytes. Analysis of the cultures has shown that 70–75% were GFAP-positive. About 25–30% cells in cultures reacted with RCA-1. No neurons were detected, as confirmed by immunostaining method, using monoclonal antibody against MAP-2.
Rat microglial cultures were received by shaking the primary mixed glial cultures (200 rpm, 5 h, 37°C) with maximum yields between days 12 and 14. The suspension of floating cells was filtered through 40 μM nylon mesh, centrifuged at 1,200 rpm for 10 min, suspended in 200 μL culture medium, placed into 96-well tissue culture plates (5 × 104 cells/well), and incubated at 37°C for 15 min in humidified 5% CO2/95% air. Afterwards, the wells were washed 4 times with 200 μL of culture medium to remove non-adhering cells. Microglia cells, which firmly adhered to the bottom of the well, were incubated overnight before the experiment. Compound C was dissolved in DMSO at the initial concentration of 20 mM. Further dilutions were performed in the appropriate medium. Corresponding amounts of DMSO were added to the control cultures. The final DMSO concentration in medium did not exceed 0.05% and, as previously checked, did not show any effect on microglia cell cultures.
The cells destined for Western blot analysis were sieved onto plastic dishes of 100 mm in diameter at the density of 15 × 106/dish. Viability was determined using 0.1% trypan blue and MTT. More than 96% of cultured cells reacted with RCA-l (microglia cells), and 3–4% were GFAP-positive (astrocytes). Each group of culture plates was repeated in three independent experiments. On the day of experiment, the culture medium was replaced with a fresh medium containing metformin, AICAR, compound C, LPS, and beta-peptides.
Microglia counts and cell viability assay
Cells in 96-well tissue culture plates were treated with metformin, AICAR, compound C, LPS, and beta-peptides in various concentrations. After 48 h, the number of cells was determined by reaction with RCA-1, a lectin that binds to the surface glycoproteins on microglial cells (Satoh and Kim 1995). Under ×20 objective, nine fields of 0.135 mm2 were photographed and counted for lectin-positive cells per well. After 48 h, cytotoxic effects of treatments were determined by measuring the microglial cell membrane integrity with 0.1% Trypan Blue Exclusion Test.
MTT conversion
Cell viability of microglia treated with studied compounds was evaluated with MTT conversion method (Mosmann 1983). The cell’s ability to convert MTT indicates mitochondrial integrity and activity, which might in turn indicate cell viability. The cleavage of tetrazoline ring in MTT takes place mainly with the participation of the mitochondrial succinate dehydrogenase and depends on the activity of the respiratory chain and the redox state of the mitochondria (Mosmann 1983). MTT (final concentration 0.25 mg/mL) was added to the medium 3 h before the scheduled end of the experiment, and then the cultures were incubated at 37°C, 5% CO2/95% air in proper conditions. At the end of the experiment, after being washed twice with PBS, cells were lysed in 100 μL DMSO, which enabled the release of the blue reaction product formasan (room temperature (RT), 10 min in the dark). One hundred microliters of lysate was transferred to 96-well plates. Absorbance at the wavelength of 570 nm was read on a microplate reader (Dynex Technologies) in four independent experiments. MTT conversion of untreated cells in control was set to 100%. The results are mean ± standard deviation (SD) of four independent experiments. Asterisks (*) indicate significant differences between control (100%) and treated groups (p < 0.05).
5-Bromo-2′-deoxyuridine incorporation
To visualize dividing cells, cultures of microglia were labeled with BrdU at 10 μM for 2 h and fixed with 4% paraformaldehyde for 20 min. Cultures were washed twice with distilled water and then incubated twice in 2 M HCl at 50°C for 15 min. After that, cultures were washed twice with 0.1 M borate buffer for 10 min at RT. The cells were then immunoreacted with anti-BrdU antibody conjugated with FITC and visualized under an epifluorescent microscope Eclipse TE200 (Nikon, Japan) (Satoh and Kim 1995). The results were expressed as a percentage of control (100%) of four independent experiments.
Preparation of aged beta-amyloid peptides (25–35), (1–40), and (1–42)
The method used to induce fibril formation of beta-peptides has been well characterized by Lorenzo and Yankner (1994). The beta-amyloid peptides were fibrilized by dissolving separately in sterile distilled water, at the concentration of 1 mM, sonicated for 1 min (ultrasonic cell disruptor, Microson® XL, Farmingdale, NY), and incubated at 37°C in humidified 5% CO2/95% air (CO2 incubator, Haereus, Germany) for 1 week. The fibrillar solutions prepared in this way may contain beta-amyloid oligomers as well as fibrils. The beta-amyloid peptides (25–35), (1–40), and (1–42) were used at final concentrations of 50, 10, and 5 μM, respectively (Kopec and Carroll 1998; Koenigsknecht and Landreth 2004). To mimic the inflammatory responses, rat microglial cultures were treated with LPS with or without beta-amyloid peptides (Ayasolla et al. 2005).
Preparation of fluorescent microspheres
The FluoSpheres® (yellow-green fluorescent carboxylate-modified microspheres, 1 μm, 505/515 nm) were prepared according to manufacturer’s recommendation and added to the cultures. Briefly, the 2% fluospheres beads stock was mixed for 5 min by sonication to break clumps. The fluospheres were washed three times by centrifugation at 10,000 rpm for 10 min in 500 μL of PBS and resuspended in PBS containing albumin (2 mg/mL) to facilitate phagocytosis. After 30 min of the horizontal rotation in darkness at RT, the fluospheres suspension was washed three times with 500 μL of PBS by centrifugation at 10,000 rpm for 5 min and resuspended in PBS.
In vitro phagocytosis assay
The phagocytosis assay was performed as described previously (Koenigsknecht and Landreth 2004). The microglial cells destined for in vitro analysis of phagocytosis were placed into 24-well tissue culture plates (3 × 105 cells/well, glass bottom imaging plate, PAA Laboratories, GmbH) and incubated with cultured medium without serum at 37°C for 40 min in humidified 5% CO2/95% air. Afterwards, the wells were washed three times with 500 μL of culture medium to remove non-adhering cells. Microglia cells, which adhered to the bottom of the well, were incubated overnight before the experiment. After 24 h, the medium was replaced with the medium containing metformin (2 mM), AICAR (2 mM), compound C (20 μM), or LPS (1 μg/mL) for 12, 24, or 48 h at 37°C and 5% CO2/95% air. To activate AMPK, the microglia were pre-incubated with metformin (2 mM) and AICAR (2 mM) for 2 h. Afterwards, LPS (1 μg/mL) was added for 12, 24, and 48 h. To inhibit AMPK, the microglia were pre-incubated with compound C (20 μM) for 1 h, and metformin (2 mM) or AICAR (2 mM) was added for another 2 h. After this time, LPS (1 μg/mL) was administered for 12, 24, and 48 h. In cultures containing beta-amyloid peptides together with other compounds, the former were added 24 h earlier. Then, metformin, AICAR, compound C, and LPS were administrated for another 24 h. Ten microliters of sonicated and diluted fluospheres suspension (to yield 0.01% solid mass) was added to the center of the microglial culture wells containing applied compounds. After 1 min of gentle shaking, the cultures were incubated at 37°C and 5% CO2/95% air. After 3 h, the wells were gently washed two times with 500 μL of culture medium to remove excess of non-adhering and non-phagocytosed fluospheres (multi-channel aspirator, Costar) and replaced with 300 μL of PBS (without fenol red). To confirm qualitatively that the fluospheres were accumulated intracellularly in lysosomes/endosomes, three random fields of cells (>100 cells) were counted on the confocal laser scanning microscopy (IX70 Olympus Optical, Co. GmbH, ×60 objective, ex/em 505/515 nm). Only microglia containing more than three fluospheres in the section were scored as phagocyting cells (Koenigsknecht and Landreth 2004). Neither aggregate of fluospheres nor aggregate of microglial cells were found in the evaluated fields. Received images were quantified using Image Pro Plus software package (Media Cybernetics, Silver Spring, MD). Results were expressed as a percentage of the phagocytosed fluospheres measured in control cultures. To confirm the power of fluorescence, the microplate fluorometer was used (Dynex Technologies, 485/520 nm). As a background, the cultures without fluospheres were used (blank wells). As a negative control, the cells were incubated for 40 min prior to fluosphere addition with 5 μM of cytochalasin D (Kopec and Carroll 1998). This substance inhibits ingestion of fluospheres but not their adhesion to the microglial cell surface. Control cultures were treated with medium containing fluospheres, without the studied compound. Each group of experiments was made up of six wells and repeated in four independent experiments. More than 95% of cultured cells exposed to the procedures did not react with 0.1% trypan blue but reacted with MTT.
Lysosomal and endosomal pH measurement
The fluorescence ratio of pH insensitive TMR/pH-sensitive FITC attached to the dextran (molecular mass 70 kDa) was used to determine the lysosomal and endosomal pH, according to manufacturer’s recommendation. Applied procedures were earlier described by Kurz et al. (2004), Dunn et al. (1994), and Zen et al. (1992). The microglial cells were incubated in 24-well tissue culture plates (3 × 105 cells/well, glass bottom imaging plate) with culture medium (without serum) containing beta-amyloid peptides with or without metformin (2 mM), AICAR (2 mM), compound C (20 μM), and LPS (1 μg/mL) for 24 h at 37°C and 5% CO2/95% air (CO2 incubator, Haereus, Germany). Beta-amyloid peptides were added 24 h earlier than other compounds. After 24 h, 5 mg/mL of FITC-TMR-dextran was added for 16 h, carefully shaken and incubated at 37°C in humidified 5% CO2/95% air. Afterwards, the microglial cultures were washed three times with 500 μL of culture medium to remove excess of non-phagocytosed dextran, and they were incubated with the medium (without serum and fenol red) containing mentioned compounds at the same concentrations at 5% CO2/95% air for another 6 h. Under these conditions, 10–25 endosomes were counted and analyzed in each microglial cell. All the images were saved from an IX70 laser scanning confocal microscope (Olympus Optical, Co. GmbH). According to Dunn et al. (1994), 0.3 to 0.5 μm vertical steps were used with <1.0 μm of axial resolution. The images were analyzed using Image Pro Plus software package. The curves of calibration were generated after fixing and equilibrating the FITC-TMR-dextran loaded microglial cells. Subsequently, we added buffers containing 5 mM of nigericin from the range of 4.5 to 8.0 pH (Zen et al. 1992). While equilibrium pH was achieved in <2 min, there was no pH change upon further incubation for >10 min. The images were collected from ten separate microglial cells in every group, and the TMR/FITC fluorescence ratio for individual lysosomes/endosomes were calculated (50 endocytic vesicles in every cell).
The ratio of the TMR/FITC fluorescence was sensitive to differential photobleaching, which was minimized by the short exposure of the cells to the laser radiation and attenuation of the laser intensity. The effect of photobleaching on TMR/FITC ratio was negligible and consistent for all the images. To evaluate the spectrum of fluorescence, the USB4000 spectrometer (Ocean Optics, Inc) was used with Toshiba TCD1304AP 3648 pixels linear CCD array with 300:1 signal to noise ratio at full signal. The dynamic range is 1,300:1 for a single acquisition in 16-bit A/D resolution. The spectral range of this configuration of spectrometer was 350–850 nm. The control of image acquisition, including timing, shutter control, filter selection, size definition, data reading, and storage was programmed on the HP computer using Spectra Suite program (Ocean Optics, Inc). Each group of experiments was made up of five wells and repeated in four independent experiments.
Western blot analysis
Western blot analysis of phospho-AMPK and total AMPK was performed as described previously (Towbin et al. 1979; Medeiros et al. 2007; Stott 1989; Sun et al. 2006).
AMPK activity assay
AMPK activity, determined with radioisotope method evaluating the phosphorylation of SAMS peptide, was assayed as described previously (Davies et al. 1989; Kim et al. 2001; Giri et al. 2004; Sun et al. 2006).
Statistical analysis
Results are expressed as the mean ± SD. The normality of distribution was evaluated using Shapiro–Wilk’s test. The statistical analysis of the data was performed using one-way ANOVA followed by the post hoc Tukey’s honestly significant difference test. The Bonferroni adjustment was applied for multiple comparisons. If the data were not normally distributed, then Kruskal–Wallis test followed by Mann–Whitney test was performed. Differences were considered significant for p < 0.05. Statistical analysis was performed using a SPSS statistical software package (SPSS 16.0 for Windows, Chicago, Illinois).
Results
Evaluation of compound toxicity, their influence on proliferation, and selection of the concentrations used
To be sure that the effects of compounds employed in this study did not result from their toxicity but only from their regulatory action, we assayed cell viability with trypan blue exclusion test, MTT conversion test, and RCA-1 staining. The tests measure cell membrane permeability and mitochondrial activity, while the staining method enables a precise measurement of microglia quantity (Mosmann 1983; Labuzek et al. 2005). The choice of the AICAR and compound C concentrations was based on literature data (Zhou et al. 2001; Giri et al. 2004).
Results from trypan blue exclusion test paralleled those from RCA-1 (data not shown). Neither compound C nor AICAR and LPS had any influence on these parameters. Not only did any of drug combinations impair mitochondrial function but most of them also enhanced the mitochondrial oxydoreductive potential (Fig. 1). Compound C (20–40 μM) did not impair cell viability assayed with MTT (Fig. 1). The results of MTT assay, described above, depend on the activation state of mitochondria, their total number, the cell cycle phase, and the number of cells in the culture (Mosmann 1983). The increase in the number of microglial cells in the culture was excluded earlier with RCA-1. To exclude that the examined drugs activated cell cycle progression, we evaluated DNA synthesis in the culture with BrdU assay. In this case, compound C at 40 and 80 μM, AICAR at 4 mM, and LPS at 2 μg/mL impaired BrdU incorporation (data not shown). However, each of the treatments which did not impair cell viability assayed with trypan blue exclusion test and RCA-1 had no significant influence on DNA synthesis (data not shown). Therefore, the enhanced cell metabolic activity (previously assayed with MTT) appears to result from either intensified mitochondrial activity or the increased number of mitochondria in microglia.
Effects of metformin (MET), 5-aminoimidazole-4-carboxamide-1-β-d-ribofuranoside (AICAR), compound C (C-C), and lipopolysaccharide (LPS) on 3-(4,5-dimethylthazol-2-yl)-2,5-diphenyltetrazolinum bromide (MTT) conversion in microglial cell cultures. Microglia were treated with MET (0.2–4 mM), AICAR (0.2–4 mM), C-C (20–80 μM) and LPS (1 μg/mL) for 24 h. To activate AMPK, the microglia were pre-incubated with MET (0.2–4 mM) or AICAR (0.2–4 mM) for 2 h, and LPS (1 μg/mL) was added for 24 h. To prevent AMPK activation, the microglia were pre-incubated with C-C (20 and 40 μM) for 1 h, and MET (2 mM) or AICAR (2 mM) was added. After another 2 h, LPS was administered for 24 h. MTT conversion of untreated cells in control was set to 100%. The results are mean ± SD of four independent experiments. *p < 0.05 significant differences between control (100%) and treated groups (p < 0.05)
Based on results obtained in initial experiments for the next steps of the study, we choose metformin at 2 mM, AICAR at 2 mM, compound C at 20 μM, and LPS at 1 μg/mL. The intervals used in our study were within limits used in in vitro experiments considering microglia, metformin, AICAR, compound C, and LPS (Zhou et al. 2001; Giri et al. 2004; Labuzek et al. 2005).
Influence of metformin on the phagocytosis of fluorescent microspheres
The phagocytosis of fluorescent microspheres was evaluated 12, 24, and 48 h after the addition of given compounds to the culture medium in non-stimulated (Fig. 2a) and LPS-stimulated microglia (Fig. 2b). In unstimulated microglia, metformin increased the phagocytosis compared to the control in all the intervals (Fig. 2a). The phagocytosis was increased after 24 h compared to the one observed after 12 h. However, there was no further change in phagocytosis after 48 h. In all the intervals, AICAR increased the phagocytosis compared to the control. There was no significant difference between the values obtained in different time points. Compound C did not affect phagocytosis in all the time points in comparison with the control. Preincubation of microglia with compound C reversed the metformin action on the phagocytosis, while the AICAR effect remained unreversed in all the time points.
a, b Effects of metformin (MET), 5-aminoimidazole-4-carboxamide-1-β-d-ribofuranoside (AICAR), compound C (C-C), and lipopolysaccharide (LPS) on phagocytosis in microglial cell cultures using FluoSpheres® (yellow-green fluorescent carboxylate-modified microspheres). Microglia were treated with MET (2 mM), AICAR (2 mM), C-C (20 μM), and LPS (1 μg/mL) for 12, 24, and 48 h. To activate AMPK, the microglia were pre-incubated with MET (2 mM) and AICAR (2 mM) for 2 h, and LPS (1 μg/mL) was added for 12, 24, and 48 h. To prevent AMPK activation, the microglia were pre-incubated with C-C (20 μM) for 1 h, and MET (2 mM) or AICAR (2 mM) was added. After another 2 h, LPS (1 μg/mL) was administered for 12, 24, and 48 h. After these intervals, the FluoSpheres® were added for 3 h, and the cultures were evaluated using confocal laser scanning microscopy. Results were expressed as a percentage of the phagocytosed fluospheres measured in control and set to 100%. The results are mean ± SD of four independent experiments. *p < 0.01 significant differences between treated groups and control. The number signs (#) indicate significant differences between treated groups and LPS (1 μg/mL) alone (p < 0.05)
The stimulation of microglia with LPS increased the phagocytosis of microspheres compared to the control (Fig. 2b). The phagocytosis was significantly increased after 24 h compared to the value observed after 12 h. However, there was no further change in phagocytosis after 48 h. The treatment of LPS-stimulated microglia with given compounds elicited no change in the phagocytosis except for experimental groups treated with AICAR, or with compound C and AICAR after 12 h of incubation.
Influence of metformin on the phagocytosis of fluorescent microspheres in the presence of amyloid beta-peptides (25–35), (1–40), and (1–42)
The phagocytosis of fluorescent microspheres was evaluated 24 h after the addition of the studied compounds to the culture medium in both unstimulated and stimulated microglia treated with beta-peptides (25–35), (1–40), and (1–42) (Fig. 3).
a, b Effects of metformin (MET), 5-aminoimidazole-4-carboxamide-1-β-d-ribofuranoside (AICAR), compound C (C-C), lipopolysaccharide (LPS), and the aged beta-peptides (β-p) on phagocytosis in microglial cell cultures using FluoSpheres® (yellow-green fluorescent carboxylate-modified microspheres). Microglia were treated with MET (2 mM), AICAR (2 mM), C-C (20 μM), LPS (1 μg/mL), and β-p [(5 μM of 1–42), (10 μM of 1–40), (50 μM of 25–35)] for 24 h. In cultures containing β-p together with studied compounds, β-p was added 24 h earlier, and MET, AICAR, C-C, and LPS were added for another 24 h. To activate AMPK, the microglia were pre-incubated with MET (2 mM) or AICAR (2 mM) for 2 h, and LPS (1 μg/mL) was added for 24 h. To prevent AMPK activation, the microglia were pre-incubated with C-C (20 μM) for 1 h, and MET (2 mM) or AICAR (2 mM) was added. After another 2 h, LPS (1 μg/mL) was administered. After 24 h, the FluoSpheres® were added for 3 h, and the cultures were evaluated using the confocal laser scanning microscopy. Results were expressed as a percentage of the phagocytosed fluospheres measured in control and set to 100%. The results are mean ± SD of four independent experiments
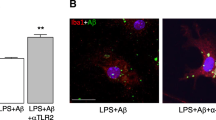
The phagocytosis of microspheres was increased in the presence of all the beta-peptides in non-stimulated microglia (Fig. 3a). Both pharmacological activators of AMPK further increased the phagocytosis of microspheres in the presence of all beta-peptides. The pharmacological inhibition of AMPK with compound C reversed the effects of metformin on the phagocytosis of microspheres in the presence of (1–40) and (1–42) beta-peptides. While compound C additionally reversed metformin effect on the phagocytosis of microspheres in the presence of beta-peptides (25–35), the effect of AICAR remained unaffected in these conditions.
The phagocytosis of microspheres was increased in the presence of all beta-peptides in LPS-stimulated microglia (Fig. 3b). Simultaneously, treatment of LPS-stimulated microglia with beta-peptides, and given compounds elicited no change in the phagocytosis.
Influence of metformin on the acidification of lysosomal/endosomal compartments
The acidification of lysosomal/endosomal compartments was evaluated 24 h after the addition of given compounds to the culture medium in both resting (Fig. 5a) and LPS-activated microglia (Fig. 5b). The values of pH were calculated from the calibration curve of TMR/FITC emission ratio to buffer pH (Fig. 4) according to Zen et al. (1992) and Kurz et al. (2004). Both pharmacological activators of AMPK acidified the lysosomal/endosomal compartments in non-activated (Fig. 5a) as well as in LPS-stimulated microglia (Fig 5b). Furthermore, the pharmacological inhibition of AMPK with compound C reversed the effect of both activators of AMPK. Compound C alone had no influence on pH of the lysosomal/endosomal compartments in non-stimulated and LPS-stimulated microglia. The lysosomal/endosomal compartments were more acidified in LPS-activated than in resting microglia.
Dependence of the fluorescence ratio on pH in lysosomes/endosomes measured in microglial cells by using dextran (molecular mass of 70 kDa) double-labeled with fluorescein (FITC) and tetramethylrhodamine (TMR). Microglial cells were incubated with 5 mg/mL FITC-TMR-dextran for 30 min, rinsed, fixed, and equilibrated with pH buffers ranging from pH 4.5 to 8.0 containing nigericin (5 μM) to equilibrate lysosomal/endosomal and extracellular pH. Laser scanning confocal microscopy and spectroscopy were used to collect and analyze the images from ten separate microglial cells in every group (see “Material and methods”), and TMR/FITC fluorescence ratio for individual lysosomes/endosomes was calculated (50 endocytic vesicles in every cell). The results are mean ± SD of four independent experiments
a, b Effects of metformin (MET), 5-aminoimidazole-4-carboxamide-1-β-d-ribofuranoside (AICAR), compound C (C-C), and lipopolysaccharide (LPS) on lysosomal/endosomal pH measured in microglial cells by using dextran (molecular mass of 70 kDa) double-labeled with fluorescein and tetramethylrhodamine. Microglia were treated with MET (2 mM), AICAR (2 mM), C-C (20 μM), and LPS (1 μg/mL) for 24 h. To activate AMPK, the microglia were pre-incubated with MET (2 mM) and AICAR (2 mM) for 2 h, and LPS (1 μg/mL) was added for 24 h. To prevent AMPK activation, the microglia were pre-incubated with C-C (20 μM) for 1 h, and MET (2 mM) or AICAR (2 mM) was added. After 2 h, LPS (1 μg/mL) was administered for 24 h. TMR/FITC fluorescence ratio was used to express the lysosomal/endosomal pH measurement. The procedure was based on laser scanning confocal microscopy and spectroscopy. The results are mean ± SD of four independent experiments. *p < 0.05 significant differences between treated groups and control. The number signs (#) indicate significant differences between treated groups and LPS (1 μg/mL) alone (p < 0.05)
Influence of metformin on the acidification of lysosomal/endosomal compartments in the presence of beta-peptide (1–40)
The acidification of lysosomal/endosomal compartments was evaluated in the presence of beta-peptide (1–40) 24 h after the addition of given compounds to the medium of non-stimulated (Fig. 6a) and LPS-activated microglial cultures (Fig. 6b). The values of pH were calculated from the calibration curve of TMR/FITC emission ratio to buffer pH (Fig. 4). Beta-peptide (1–40) alone had no influence on the pH of lysosomal/endosomal compartments in resting microglia (Fig. 6a). However, we have observed that metformin lowered the pH in the presence of beta-peptide (1–40), which was reversible after the addition of compound C (the pharmacological inhibitor of AMPK). AICAR did not alter the pH in the presence of beta-peptide (1–40). Furthermore, the pharmacological inhibition of AMPK also had no effect on the pH. Compound C alone had no effect on the pH in the presence of beta-peptide (1–40). On the other hand, the addition of LPS to the cultures pretreated with beta-peptide (1–40) lowered the pH of lysosomal/endosomal compartments in microglia (Fig. 6b). Both metformin and AICAR lowered the pH in microglia stimulated with LPS and beta-peptide (1–40). The pharmacological inhibition of AMPK with compound C reversed this effect. Compound C alone has no effect on the pH in microglia stimulated with LPS and beta-peptide (1–40).
a, b Effects of metformin (MET), 5-aminoimidazole-4-carboxamide-1-β-d-ribofuranoside (AICAR), compound C (C-C), lipopolysaccharide (LPS), and the beta-peptide (1–40) (β-p 1–40) on lysosomal/endosomal pH measured in microglial cells by using dextran (molecular mass of 70 kDa) double-labeled with fluorescein and tetramethylrhodamine. Microglia were treated with MET (2 mM), AICAR (2 mM), C-C (20 μM), LPS (1 μg/mL), and β-p (1–40) for 24 h. In cultures containing β-p (1–40) together with studied compounds, β-p (1–40) was added 24 h earlier, and MET, AICAR, C-C, and LPS were added for another 24 h. To activate AMPK, the microglia were pre-incubated with MET (2 mM) and AICAR (2 mM) for 2 h, and LPS (1 μg/mL) was added for 24 h. To prevent AMPK activation, the microglia were pre-incubated with C-C (20 μM) for 1 h, and MET (2 mM) or AICAR (2 mM) was added. After 2 h, LPS (1 μg/mL) was administered for 24 h. TMR/FITC fluorescence ratio was used to describe the lysosomal/endosomal pH measurement. The procedure was based on laser scanning confocal microscopy and spectroscopy. The results are mean ± SD of four independent experiments. The dollar signs ($) indicate significant differences between treated groups and β-p (1–40) alone (p < 0.05)
Influence of metformin on phospho-AMPK/AMPK ratio
Both metformin and AICAR are well-established AMPK activators. It seems that metformin activates AMPK by decreasing cellular energy charge or by redox signaling which then enhances the interaction between AMPK and its upstream serine/threonine protein kinase 11 (Zou et al. 2004). On the other hand, AICAR activates AMPK via a direct allosteric mechanism and indirectly by inhibiting dephosphorylation of Thr172 (Sanders et al. 2007). It was also proved that AICAR induces upstream kinase (AMPKK) activity, and the phosphorylation of AMPK by AMPKK is necessary for its full activity (Hawley et al. 1996; Giri et al. 2004). We confirmed that metformin and AICAR (both at 2 mM) comparably and significantly increased phospho-AMPK/AMPK ratio in microglial cells at 2 h of incubation (Fig. 7). Compound C, the pharmacological inhibitor of AMPK, prevented metformin- and AICAR-mediated increase in phospho-AMPK/AMPK ratio in non-activated microglia.
Effects of lipopolysaccharide (LPS), metformin (MET), 5-aminoimidazole-4-carboxamide-1-β-d-ribofuranoside (AICAR), and compound C (C-C) on phospho-AMPK/AMPK ratio in microglial cell cultures. Microglia were treated with MET (2 mM), AICAR (2 mM), C-C (20 μM), and LPS (1 μg/mL) for 2 h. To prevent AMPK activation, the microglia were pre-incubated with C-C (20 μM) for 1 h, and MET (2 mM) or AICAR (2 mM) was added for 2 h. Phospho-AMPK/AMPK ratio was evaluated by Western blot analysis using antibody specific for phospho-AMPK, AMPK, and β-actin. Results were subjected to densitometric analysis and presented as phospho-AMPK/AMPK ratio. The control was set to 1.00. The results are mean ± SD of three independent experiments. *p < 0.05 significant differences between control (1.00) and treated groups
Because LPS boosts ROS production and increases calcium intracellular concentration (Hanisch and Kettenmann 2007), factors known to activate AMPKK (Tamas et al. 2006), we investigated whether LPS activates the enzyme in microglia. We observed that LPS at 1 μg/mL significantly increased phospho-AMPK/AMPK ratio at the second hour of incubation. There were no significant differences between results of phospho-AMPK/AMPK ratio obtained in LPS-stimulated microglial cells as well as in non-activated microglia pretreated with metformin or AICAR (Fig. 7).
Influence of metformin on AMPK activity
AMPK activity, which reflects the phosphorylation of SAMS peptide (engineered and dedicated substrate for AMPK), was determined with radioisotope method, as described in the “Materials and methods” section.
First, we determined the incubation time at which AMPK activity achieved maximum level after the addition of metformin at the concentration of 2 mM. Peak AMPK activity was observed at 40 min of incubation in conditions defined above (Fig. 8a). This period was chosen for further evaluation of AMPK activity.
a, b Effects of lipopolysaccharide (LPS), metformin (MET), 5-aminoimidazole-4-carboxamide-1-β-d-ribofuranoside (AICAR), and compound C (C-C) on AMPK activity in microglial cell cultures. Microglial cells were incubated with MET (2 mM) for 10, 20, 40, 60, and 120 min (a). Then, microglia were also treated with medium: (a) alone (control), (b) containing LPS (1 μg/mL), (c) MET (2 mM), (d) AICAR (2 mM), (e) C-C (20 μM), (f) MET (2 mM, 1-h preincubation) with LPS (1 μg/mL), (g) C-C (20 μM, 1-h preincubation) with MET (2 mM) and LPS (1 μg/mL), (h) C-C (20 μM, 1-h preincubation) with AICAR (2 mM) and LPS (1 μg/mL), (i) C-C (20 μM, 1-h preincubation) with LPS (1 μg/mL) (b). AMPK activity was assessed using SAMS peptide and (γ-32P)ATP used as substrate. The results are mean ± SD of three independent experiments. The control was set to 1.00. *p < 0.05 significant differences between control and treated groups
Secondly, we tried to activate AMPK with metformin, AICAR, and LPS. Metformin (2 mM), AICAR (2 mM), and LPS (1 μg/mL) comparably activated AMPK (Fig. 8b).
Thirdly, we determined the influence of compound C on activation of AMPK mediated by these compounds. Compound C at the concentration of 20 μM effectively inhibited the activation of AMPK mediated by metformin, AICAR, and LPS (Fig. 8b).
Discussion
In this study, we demonstrated that metformin affected the phagocytosis in non-stimulated microglia treated with or without beta-peptides (25–35), (1–40), and (1–42) as well as it intensified the acidification of the lysosomal/endosomal compartments in primary rat microglia independently of their activation state.
To assay phagocytosis, we used carboxylate-modified Fluospheres® beads as described previously (Koenigsknecht and Landreth 2004). Two kinds of phagocytosis were evaluated: bulk fluid phagocytosis (in the absence of fibrillar beta-peptides) and the phagocytosis dependent on scavenger receptors (in the presence of fibrillar beta-peptides). The evaluation took place in microglia both stimulated and non-stimulated with LPS. To determine the optimal interval of incubation, we measured phagocytosis at three time points: 12, 24, and 48 h after administration of the studied compounds. Based on the intensity of phagocytosis at these time points (Fig. 2), in subsequent experiments we decided to measure phagocytosis after 24 h of incubation. Metformin increased both bulk fluid phagocytosis in resting microglia and the phagocytosis dependent on fibrillar beta-peptide receptors. Stimulation of microglia with LPS seems to produce maximum level of bulk fluid phagocytosis (Fig. 2). However, the intensity of the phagocytosis of fibrillar beta-peptides dependent on scavenger receptors was no further increased in LPS-stimulated microglial cultures pretreated with metformin (Fig. 2b). Considering the fact that metformin crosses the blood–brain barrier and accumulates in the brain (Wilcock and Bailey 1994), we suppose that the drug may increase microglial phagocytosis in the brain extracellular matrix both in the presence and absence of fibrillar beta-peptides. However, in heavy inflammation encountered in situations such as brain infections, metformin may have no positive effect on phagocytosis.
The fate of phagocytosed material in microglia depends on lysosomal processing which is mediated by lysosomal proteases (dipeptidyl peptidase I, tripeptidyl peptidase I, and cathepsins B and D) (Majumdar et al. 2007). In in vitro conditions, microglia with acidified lysosomes degrade ingested macromolecular forms of fibrillar beta-peptides, whereas microglia with lysosomes at basal state release them back to the medium (Majumdar et al. 2007). For this reason, we determined the pH of the lysosomal/endosomal compartments in microglia treated with metformin in the presence of LPS and/or beta-peptide (1–40). It was shown that microglia stimulated with LPS for at least 16 h efficiently degraded fibrillar beta-peptides in microglia cultures and that this effect is ascribed to decline in lysosomal pH from the value of 5.9 to the value of 5.3 (Majumdar et al. 2007). In our experiment, we stimulated microglia with LPS for 24 h and achieved the drop in pH from the value of 6.1 to the value of 5.4. Interestingly, metformin alone lowered pH to the value of 5.6. Although this drop in pH may be insufficient for the activation of lysosomal enzymes in microglia, this result was statistically insignificant in comparison with that obtained for LPS-activated microglia (Fig. 5). Furthermore, the addition of the beta-peptide (1–40) into the medium with metformin lowered the pH to the value of 5.4, which was also statistically insignificant in comparison with the result obtained for LPS (Fig. 6). It is important that beta-peptide (1–40) alone did not significantly lower the pH in comparison with the control. Metformin achieved even further drop in the pH to the values of 4.9 and 4.8 in the presence of LPS and LPS with beta-peptide (1–40), respectively (Figs. 5 and 6). Therefore, metformin decreases pH to the values required for the activation of lysosomal proteases, which results in the effective degradation of the fibrillar beta-peptides.
Metformin was shown to act through AMPK activation in many cells of peripheral organs (Zhou et al. 2001). However, it remains controversial whether this enzyme is expressed and activated in microglia. As shown in Fig. 7, both metformin and AICAR up-regulated the enzyme phosphorylation state, which resulted in the increased activity of AMPK in rat primary microglial cultures (Fig. 8). Our observations are in accordance with results obtained by Giri et al. (2004), who also observed activation of AMPK in the microglial cell line BV2.
To determine whether the influence of metformin on the analyzed parameters coincides or results from AMPK activation, we have tried to reverse the effects of the drug with compound C (pharmacological inhibitor of AMPK). As shown in Fig. 7, compound C prevented metformin- and AICAR-mediated increase in phospho-AMPK/AMPK ratio in non-activated microglia. Moreover, compound C alone did not affect phospho-AMPK/AMPK ratio and AMPK activity (Figs. 7 and 8) in comparison with the control, showing that our experimental settings did not activate AMPK in resting microglia. It should be noted that the pharmacological inhibition of AMPK with compound C reversed all the observed effects of metformin. However, compound C alone influenced neither phagocytosis nor lysosomal acidification (Figs. 2, 3, 5, and 6). Despite the fact that LPS-activated AMPK, the inhibition of AMPK activation with compound C did not reverse the action of LPS. This observation may point out that AMPK does not play a significant role in the LPS mode of action. However, LPS may synergize in action with the pharmacological activators of AMPK as shown in the results for pH obtained with AICAR in the lysosomal/endosomal compartments in microglia (Fig. 5). All the effects of metformin were reversed with the pharmacological inhibition of AMPK, which has not been observed in the case of AICAR. Therefore, metformin proved to be a more specific AMPK activator in microglia regarding phagocytosis and the acidification of the lysosomal/endosomal compartments.
Despite the fact that the concentration of metformin employed in this study far exceeds that encountered in plasma of diabetic patients treated with this drug, it was still chosen for several reasons. First, metformin may accumulate in various tissues at values up to 100 times higher in comparison with plasma levels occurring after single oral administration (Wilcock and Bailey 1994). Metformin accumulates mainly in mitochondrial compartment of the cell (Wilcock et al 1991), and microglia, being highly active and versatile cells, have numerous mitochondria in their cytoplasm (Banati et al 2004). Metformin accumulation in mitochondria is concentration- and time-dependent. Higher concentrations of metformin allows to achieve the steady concentration of metformin in mitochondria in shorter periods (Zhou et al. 2001). Secondly, it was demonstrated that higher concentrations of metformin may be used instead of longer time of exposition in in vitro conditions (Zhou et al. 2001). Accordingly, higher concentrations of metformin used in in vitro studies may compensate for years of metformin administration in patients with type 2 diabetes. Finally, in the present study, microglial cell cultures were treated with metformin at a concentration which did not produce toxic effects and is commonly used in scientific works on neuroinflammation (Kuo et al. 2008; Nath et al. 2009). Although metformin is an inhibitor of mitochondrial respiratory chain complex I and may have toxic effects at higher concentrations (Zhou et al. 2001), in our study we did not observe diminished viability of cells treated with metformin (Fig. 1).
In conclusion, we demonstrated for the first time that metformin increases bulk fluid phagocytosis and the phagocytosis dependent on fibrillar beta-peptide receptors as well as it acidifies the lysosomal/ endosomal compartments. Furthermore, those effects seem to be AMPK-dependent. These new findings may point at new targets of metformin action involving the increased ingestion and degradation rate of beta-amyloid peptides by lysosomes/endosomes in microglial cells.
Abbreviations
- AICAR:
-
5-Aminoimidazole-4-carboxamide-1-β-d-ribofuranoside
- AMPK:
-
Adenosine monophosphate-activated protein kinase
- BrdU:
-
5-Bromo-2′-deoxyuridine
- DMEM:
-
Dulbecco's modified Eagle's medium
- FBS:
-
Fetal bovine serum
- GFAP:
-
Glial fibrillary acidic protein
- IOD:
-
Integrated optical density
- LPS:
-
Lipopolysaccharide
- MAP-2:
-
Microtubule associating protein-2
- MTT:
-
3-(4,5-Dimethylthazol-2-yl)-2,5-diphenyltetrazolinum bromide
- RCA-1:
-
Ricinus Communis Agglutinin-1
- RPMI-1640 Medium:
-
Roswell Park Memorial Institute-1640 Medium
- TBST:
-
Tris-buffered saline Tween 20
- SD:
-
Standard deviation
References
Ayasolla KR, Singh AK, Singh I (2005) 5-aminoimidazole-4-carboxamide-1-beta-4-ribofuranoside (AICAR) attenuates the expression of LPS- and Abeta peptide-induced inflammatory mediators in astroglia. J Neuroinflammation 20:2–21
Banati RB, Egensperger R, Maassen A, Hager G, Kreutzberg GW, Graeber MB (2004) Mitochondria in activated microglia in vitro. J Neurocytol 33:535–541
Beckner ME, Gobbel GT, Abounader R, Burovic F, Agostino NR, Laterra J, Pollack IF (2005) Glycolytic glioma cells with active glycogen synthase are sensitive to PTEN and inhibitors of PI3K and gluconeogenesis. Lab Invest 85:1457–1470
Davies SP, Carling DG, Hardie DG (1989) Tissue distribution of the AMP-activated protein kinase and lack of activation by cyclic-AMP-dependent protein kinase studied using a specific and sensitive peptide assay. Eur J Biochem 186:123–128
Dunn KW, Park J, Semrad CE, Gelman DL, Shevell T, McGraw TE (1994) Regulation of endocytic trafficking and acidification are independent of the cystic fibrosis transmembrane regulator. J Biol Chem 269:5336–5345
El-Mir MY, Detaille D, R-Villanueva G, Delgado-Esteban M, Guigas B, Attia S, Fontaine E, Almeida A, Leverve X (2008) Neuroprotective role of antidiabetic drug metformin against apoptotic cell death in primary cortical neurons. J Mo Neurosci 34:77–87
Giri S, Nath N, Smith B, Viollet B, Singh AK, Singh I (2004) 5-Aminoimidazole-4-carboxamide-1-beta-4-ribofuranoside inhibits proinflammatory response in glial cells: a possible role of AMP-activated protein kinase. J Neurosci 24:479–487
Hallows KR, Alzamora R, Li H, Gong F, Smolak C, Neumann D, Pastor-Soler NM (2009) AMP-activated protein kinase inhibits alkaline pH- and PKA-induced apical vacuolar H+-ATPase accumulation in epididymal clear cells. Am J Physiol Cell Physiol 296:672–681
Hanisch UK, Kettenmann H (2007) Microglia active sensor and versatile effectors cells in the normal and pathologic brain. Nat Neurosci 10:1387–1394
Hawley SA, Davison M, Woods A, Davies SP, Beri RK, Carling D, Hardie DG (1996) Characterization of the AMP-activated protein kinase kinase from rat liver and identification of threonine 172 as the major site at which it phosphorylates AMP-activated protein kinase. J Biol Chem 271:27879–27887
Isoda K, Young JL, Zirlik A, MacFarlane LA, Tsuboi N, Gerdes N, Schönbeck U, Libby P (2006) Metformin inhibits proinflammatory responses and nuclear factor-kappaB in human vascular wall cells. Arterioscler Thromb Vasc Biol 26:611–617
Kim J, Yoon MY, Choi SL, Kang I, Kim SS, Kim YS, Choi YK, Ha J (2001) Effects of stimulation of AMP-activated protein kinase on insulin-like growth factor 1- and epidermal growth factor-dependent extracellular signal-regulated kinase pathway. J Biol Chem 276:19102–19110
Koenigsknecht J, Landreth G (2004) Microglial phagocytosis of fibrillar beta-amyloid through a beta1 integrin-dependent mechanism. J Neurosci 3:9838–9846
Kopec KK, Carroll RT (1998) Alzheimer's beta-amyloid peptide 1–42 induces a phagocytic response in murine microglia. J Neurochem 71:2123–2131
Kuo CL, Ho FM, Chang MY, Prakash E, Lin WW (2008) Inhibition of lipopolysaccharide-induced inducible nitric oxide synthase and cyclooxygenase-2 gene expression by 5- aminoimidazole-4-carboxamide riboside is independent of AMP-activated protein kinase. J Cell Biochem 103:931–940
Kurz T, Leake A, von Zglinicki T, Brunk UT (2004) Relocalized redox-active lysosomal iron is an important mediator of oxidative-stress-induced DNA damage. Biochem J 378:1039–1045
Labuzek K, Kowalski J, Gabryel B, Herman ZS (2005) Chlorpromazine and loxapine reduce interleukin-1beta and interleukin-2 release by rat mixed glial and microglial cell cultures. Eur Neuropsychopharmacol 5:23–30
Li L, Mamputu JC, Wiernsperger N, Renier G (2005) Signaling pathways involved in human vascular smooth muscle cell proliferation and matrix metalloproteinase-2 expression induced by leptin: inhibitory effect of metformin. Diabetes 54:2227–2234
Lorenzo A, Yankner BA (1994) Beta-amyloid neurotoxicity requires fibril formation and is inhibited by congo red. Proc Natl Acad Sci U S A 91:12243–12247
Ma TC, Buescher JL, Oatis B, Funk JA, Nash AJ, Carrier RL, Hoyt KR (2007) Metformin therapy in a transgenic mouse model of Huntington's disease. Neurosci Lett 411:98–103
Majumdar A, Cruz D, Asamoah N, Buxbaum A, Sohar I, Lobel P, Maxfield FR (2007) Activation of microglia acidifies lysosomes and leads to degradation of Alzheimer amyloid fibrils. Mol Biol Cell 18:1490–1496
Mamputu JC, Wiernsperger NF, Renier G (2003) Antiatherogenic properties of metformin: the experimental evidence. Diabetes Metab 29:6S71–6S76
Medeiros R, Prediger RD, Passos GF, Pandolfo P, Duarte FS, Franco JL, Dafre AL, Di Giunta G, Figueiredo CP, Takahashi RN, Campos MM, Calixto JB (2007) Connecting TNF alpha signaling pathways to iNOS expression in a mouse model of Alzheimer's disease: relevance for the behavioral and synaptic deficits induced by amyloid beta protein. J Neurosci 27:5394–5404
Mosmann T (1983) Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Method 65:55–63
Nath N, Khan M, Paintlia MK, Hoda MN, Giri S (2009) Metformin attenuated the autoimmune disease of the central nervous system in animal models of multiple sclerosis. J Immunol 182:8005–8014
Ropelle ER, Pauli JR, Zecchin KG, Ueno M, de Souza CT, Morari J, Faria MC, Velloso LA, Saad MJ, Carvalheira JB (2007) A central role for neuronal adenosine 5′-monophosphate-activated protein kinase in cancer-induced anorexia. Endocrinology 148:5220–5229
Saeedi R, Parsons HL, Wambolt RB, Paulson K, Sharma V, Dyck JR, Brownsey RW, Allard MF (2008) Metabolic actions of metformin in the heart can occur by AMPK- independent mechanisms. Am J Physiol Heart Circ Physiol 294:2497–2506
Sanders MJ, Grondin PO, Hegarty BD, Snowden MA, Carling D (2007) Investigating the mechanism for AMP activation of the AMP-activated protein kinase cascade. Biochem J 403:139–148
Satoh J, Kim SU (1995) Ganglioside markers GD3, GD2, and A2B5 in fetal human neurons and glial cells in culture. Dev Neurosci 17:137–148
Stott DI (1989) Immunoblotting and dot blotting. J Immunol Methods 119:153–187
Sun W, Lee TS, Zhu M, Gu C, Wang Y, Zhu Y, Shyy JY (2006) Statins activate AMP-activated protein kinase in vitro and in vivo. Circulation 114:2655–2662
Tamás P, Hawley SA, Clarke RG, Mustard KJ, Green K, Hardie DG, Cantrell DA (2006) Regulation of the energy sensor AMP-activated protein kinase by antigen receptor and Ca2+ in T lymphocytes. J Exp Med 203:1665–1670
Towbin H, Staehelin T, Gordon J (1979) Electrophoretic transfer of proteins from polyacrylamide gels to nitrocellulose sheets: procedure and some applications. Proc Natl Acad Sci U S A 76:4350–4354
Towler MC, Hardie DG (2007) AMP-activated protein kinase in metabolic control and insulin signaling. Circ Res 100:328–341
Vazquez-Martin A, Oliveras-Ferraros C, Menendez JA (2009) The antidiabetic drug metformin suppresses HER2 (erbB-2) oncoprotein overexpression via inhibition of the mTOR effector p70S6K1 in human breast carcinoma cells. Cell Cycle 8:88–96
Wilcock C, Bailey CJ (1994) Accumulation of metformin by tissues of the normal and diabetic mouse. Xenobiotica 24:49–57
Wilcock C, Wyre ND, Bailey CJ (1991) Subcellular distribution of metformin in rat liver. J Pharm Pharmacol 43:442–444
Zen K, Biwersi J, Periasamy N, Verkman AS (1992) Second messengers regulate endosomal acidification in Swiss 3 T3 fibroblasts. J Cell Biol 119:99–110
Zhou G, Myers R, Li Y, Chen Y, Shen X, Fenyk-Melody J, Wu M, Ventre J, Doebber T, Fujii N, Musi N, Hirshman MF, Goodyear LJ, Moller DE (2001) Role of AMP-activated protein kinase in mechanism of metformin action. J Clin Invest 108:1167–1174
Zou MH, Kirkpatrick SS, Davis BJ, Nelson JS, Wiles WG 4th, Schlattner U, Neumann D, Brownlee M, Freeman MB, Goldman MH (2004) Activation of the AMP-activated protein kinase by the anti-diabetic drug metformin in vivo. Role of mitochondrial reactive nitrogen species. J Biol Chem 279:43940–43951
Acknowledgements
The authors are thankful to Mrs. Jaroslawa Sprada, Mrs. Halina Klimas, and Mrs. Anna Bielecka for their excellent technical support. This work was supported by a research grant KNW-2-092/09 from Medical University of Silesia, Katowice, Poland. None of the authors has any conflict of interest. The study was approved by the Ethical Committee of the Medical University of Silesia. The experiments comply with the current law of Poland.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/s00210-017-1350-y.
Electronic supplementary materials
Below is the link to the electronic supplementary material.
Supplement 1
PDF 1.44 MB
Rights and permissions
About this article
Cite this article
Łabuzek, K., Liber, S., Gabryel, B. et al. Metformin increases phagocytosis and acidifies lysosomal/endosomal compartments in AMPK-dependent manner in rat primary microglia. Naunyn-Schmied Arch Pharmacol 381, 171–186 (2010). https://doi.org/10.1007/s00210-009-0477-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-009-0477-x