Abstract
Endothelin may contribute to the development of inflammatory events such as leukocyte recruitment and nociception. Herein, we investigated whether endothelin-mediated mechanical hypernociception (decreased nociceptive threshold, evaluated by electronic pressure-meter) and neutrophil migration (myeloperoxidase activity) are inter-dependent in antigen challenge-induced Th1-driven hind-paw inflammation. In antigen challenge-induced inflammation, endothelin (ET) ETA and ETB receptor antagonism inhibited both hypernociception and neutrophil migration. Interestingly, ET-1 peptide-induced hypernociception was not altered by inhibiting neutrophil migration or endothelin ETB receptor antagonism, but rather by endothelin ETA receptor antagonism. Furthermore, endothelin ETA, but not ETB, receptor antagonism inhibited antigen-induced PGE2 production, whereas either selective or combined blockade of endothelin ETA and/or ETB receptors reduced hypernociception and neutrophil recruitment caused by antigen challenge. Concluding, this study advances knowledge into the role for endothelin in inflammatory mechanisms and further supports the potential of endothelin receptor antagonists in controlling inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endothelin-1 (ET-1) was discovered as a peptide secreted by endothelial cells, which produced the most potent known vasoconstriction activity (Yanagisawa et al. 1988). Endothelin comprises of a family of three peptides of 21 amino acids (ET-1, ET-2, and ET-3) encoded by distinct genes, with unequal tissue distribution. These peptides are produced as prepro-endothelin, which are cleaved by endothelin-converting enzymes forming big-endothelin and then the active peptide (for review, see Dhaun et al. 2007). Endothelin acts through the activation of two endothelin receptors in mammals, endothelin ETA and ETB receptors. These receptors seem to have a relevant function in pulmonary arterial hypertension, hypertension, atherosclerosis, cerebral vasospasm, and inflammatory signals, including pain (Ferreira et al. 1989; for review, see Dhaun et al. 2007; for review, see Verri et al. 2006a). In 1989, it was already demonstrated that ET-1 injection induces wheal and flare responses in humans, mechanical hypernociception (decrease in nociceptive threshold) in rats, and writhing response (overt nociception) in mice. Furthermore, although ET-1 injection in the knee joint does not induce motor incapacitation in dogs, it potentiates the motor incapacitation induced by PGE2 administration into the knee joint. This was a seminal finding indicating a role for ET-1 in inflammatory pain (Ferreira et al. 1989).
Thereafter, endothelin receptor antagonists were developed and helped to ascertain the nociceptive role of endogenous endothelin in different models. For instance, the antagonism of endothelin receptors diminishes ovalbumin challenge-induced licking (Piovezan et al. 2004), carrageenin-induced thermal and mechanical hypernociception (Baamonde et al. 2004), and phenyl-p-benzoquinone-induced writhes (Griswold et al. 1999; Verri et al. 2008a). Depending on the nociceptive method, endothelin induces hypernociception or visceral nociception acting on endothelin ETA and/or ETB receptors (Ferreira et al. 1989; Raffa et al. 1996; Davar et al. 1998; Griswold et al. 1999; Menéndez et al. 2003; Verri et al. 2004, 2006b, 2008a, b). On the other hand, endothelin ETB receptors mediate antinociception, which relate to high doses of endothelin ETB receptor agonists. In fact, a shift from antinociceptive to pronociceptive was detected with increasing doses of endothelin ETB receptor agonist (Piovezan et al. 1998; 2000; Khodorova et al. 2002; Piovezan et al. 2004; Chichorro et al. 2006). These apparent discrepancies could be due to distinct experimental models, doses of stimulus, and animal species.
Focusing on neutrophil migration, endothelin ETA receptor antagonists inhibit LPS-induced neutrophil migration in vivo (Sampaio et al. 2004), and ET-1 induces an increase of neutrophil chemokinetics in vitro (Elferink and de Koster 1994). Both endothelin ETA/ETB receptors also mediate zymosan-induced neutrophil migration to the knee joint of mice (Conte et al. 2008). Furthermore, suggesting a dual role of endothelin ETB receptors activation as detected in nociception, there is evidence that the endothelin ETB agonist sarafotoxin S6c at low doses induces and at high doses inhibits neutrophil migration (Elferink and de Koster 1996). Thus, there are similarities in endothelin receptor modulation of nociception and neutrophil migration when concerning this dual role of endothelin ETB receptors.
The migrated neutrophils seem to have a significant role in the development of nociception, since the depletion of circulating neutrophil and/or inhibition of neutrophil migration with fucoidin (which binds l-selectin, thus inhibiting neutrophil migration) inhibits the hypernociception induced by carrageenin, LTB4 and C5a (Levine et al. 1984; Guerrero et al. 2008; Ting et al. 2007; Cunha et al. 2008a, b) as well as this LTB4-induced pain in humans presents the same temporal profile of neutrophil migration (Bisgaard and Kristensen 1985). In the present study, we addressed the involvement of endothelin receptors in antigen challenge-induced mechanical hypernociception and neutrophil migration as well as a possible inter-dependence between these effects.
Materials and methods
Animals
Balb/c mice from the Faculty of Medicine of Ribeirao Preto (University of Sao Paulo, Sao Paulo, Brazil) were used in this study. Mice were housed in standard clear plastic cages with free access to food and water, light/dark cycle (12:12 h) and kept at 21°C. All behavioral testing was performed between 9:00 a.m. and 5:00 p.m. in a temperature-controlled room. Animal care and handling procedures were in accordance with the International Association for the Study of Pain (IASP) guidelines (Zimmermann 1983) and with the approval of the Ethics Committee of the Faculty of Medicine of Ribeirao Preto (University of Sao Paulo). All efforts were made to minimize the number of animals used and their suffering.
Leukocyte migration to the paw skin tissue
The leukocyte migration to the subcutaneous plantar tissue of mice hind paw was evaluated by the myeloperoxidase (MPO) kinetic-colorimetric assay as previously described (Bradley et al. 1982; Casagrande et al. 2006). Samples of subcutaneous plantar tissue were collected in 50 mM K2HPO4 buffer (pH 6.0) containing 0.5% hexadecyl trimethylammonium bromide and kept at −80°C until use. Samples were homogenized using a Polytron (PT3100) and centrifuged at 16,100×g for 4 min, and the resulting supernatant assayed spectrophotometrically for MPO activity determination at 450 nm (Spectra max), with three readings in 1 min. The MPO activity of samples was compared to a standard curve of neutrophils. Briefly, 10 μl of sample was mixed with 200 μl of 50 mM phosphate buffer pH 6.0 containing 0.167 mg/ml O-dianisidine dihydrochloride and 0.0005% hydrogen peroxide. The results were presented as the MPO activity (Neutrophils × 104/mg of tissue).
Electronic pressure-meter test
We use the term hypernociception rather than hyperalgesia or allodynia to define nociceptor sensitization (for a detailed discussion, see Verri et al. 2006a; Cunha et al. 2007). Mechanical hypernociception was tested in mice as previously reported (Cunha et al. 2004). The test consisted of evoking hind-paw flexion reflex with a hand-held force transducer (electronic anesthesiometer; IITC Life Science, Woodland Hills, CA, USA) adapted with a 0.5-mm2 polypropylene tip. The end point was characterized by the active removal of the paw followed by clear flinching movements. The intensity of pressure which elicited paw withdrawal was automatically recorded. The value for the response was obtained by averaging three measurements. The animals were tested before and after treatments. The results were expressed by delta (Δ) withdrawal threshold (in grams) calculated by subtracting the zero-time mean measurements (base line) from the mean measurements 3 h after stimulus. This time point was determined as the peak of response in a previous study (Verri et al. 2006b). Withdrawal threshold was 9.0 ± 0.6 g (mean ± SEM; n = 40) before injection of the hypernociceptive agents.
Immunization procedure
Mice were immunized as described previously (Canetti et al. 2001). Briefly, ovalbumin (OVA; 100 μg) emulsified in complete Freund’s adjuvant (CFA) plus saline (1:1) was injected subcutaneously in mice on day 0. The mice received a subcutaneous booster with OVA (100 μg) emulsified in incomplete Freund’s adjuvant plus saline (1:1) on days 7 and 14 (ovalbumin-immunized mice—OVA Im). Control mice (sham-immunized—Sham Im) received the same emulsions without OVA. Mice were challenged on day 21 by intraplantar (i.pl.) injection of 3 μg of OVA (dose established in Verri et al. 2006b). CFA was used as adjuvant in this protocol of immunization, because it induces mainly Th1-driven response (Su et al. 2005, Canetti et al. 2001).
Determination of endothelin and PGE2 production
The paw skin tissues were collected after i.pl. (3 h) injection of OVA as previously described (Pontiroli et al. 2004; Verri et al. 2007a). Briefly, paw skin samples were collected in 0.5 ml of a mixture of acetone: 1 M HCl/water (10:1:5, v/v/v). After homogenizing the samples using a polytron (paw samples), they were centrifuged (20 min at 2,000×g at 4°C), and the supernatant was decanted before drying the pellet in a centrifugal evaporator at 37°C. The pellet was reconstituted in 0.21 ml of the kit sample diluent and immediately assayed by enzyme-linked immunosorbent assay (ELISA) to determine ET-1 levels according to the manufacturer’s instructions (Endothelin-1 Biotrack ELISA System—Amersham Biosciences). For PGE2 production, paw skin tissue samples were collected 3 h after i.pl. injection of OVA in 0.5 ml of a mixture of isopropanol, ethylacetate, and 0.1 M HCl (3:3:1, v/v/v). After homogenizing with a polytron, the samples were centrifuged at 1,500×g for 10 min at 4°C, and the supernatant (organic phase) was separated and dried in a centrifugal evaporator at 37°C. The pellet was reconstituted in 1 ml of phosphate buffer 7.4 with 0.8% of NaN3, 0.1% of gelatin. The concentrations of PGE2 were determined by RIA (Amersham, Paisley, UK; Verri et al. 2008b).
Protocols
Mechanical hypernociception was evaluated before (basal response) and after (3 and 5 h) the i.pl. injection of ET-1 (10–100 pmol/paw) in normal mice. OVA (3 μg/paw) hypernociception was evaluated in sham-immunized (Sham Im) and immunized (OVA Im) mice. Furthermore, some mice were treated with bosentan (mixed endothelin ETA/ETB receptor antagonist, 100 mg/kg, p.o., 5% acacia gum mucilage in water, 1 h beforehand), BQ-123 (endothelin ETA receptor antagonist, 30 nmol/paw, in saline, 30 min beforehand), or BQ-788 (endothelin ETB receptor antagonist, 30 nmol/paw, in saline, 30 min beforehand) before stimulus injection. For MPO activity assay, OVA Im mice were treated with BQ-123 or BQ-788 (same doses above) before OVA challenge. Sham Im and OVA Im mice were challenged with OVA. Furthermore, mice were treated with fucoidin (which binds l-selectin and inhibits neutrophil migration, 20 mg/kg/i.v., in saline, 15 min beforehand) before ET-1 (30 and 100 pmol/paw) stimulus and samples were collected after 5 h for MPO assay. Carrageenin was used as a positive control for increased MPO activity (Valerio et al. 2007). For ET-1 and PGE2 levels, samples of paw tissue were collected 3 h after stimulus injection. The adequacy of these time points for sample collection was determined previously (Verri et al. 2006b, 2007a). Control animals were always treated in identical fashion with the corresponding vehicles.
Drugs and cytokines
The following materials were obtained from the sources indicated: bosentan (Actelion Pharmaceuticals, Allschwil, Switzerland); BQ123 sodium salt (Novabiochem, La Jolla, CA, USA); BQ788 sodium salt (Calbiochem, La Jolla, CA, USA); carrageenin (FMC Corp., Philadelphia, PA, USA); CFA, fucoidin, and ovalbumin (Sigma, St. Louis, MO, USA); and human endothelin-1 (referred to as ET-1, American Peptide Company, Sunnyvale, CA, USA).
Statistical analyses
Results are presented as means ± SEM and are representative of two separate experiments. The statistical analyses for both separate experiments were similar. The “n” of each experiment is indicated in the respective legends, and if a numerical interval is indicated (e.g., 4–5), it means that each of the two experiments was performed with different n, and the total number of animals is the summation of interval (e.g., 9). Treatment with the vehicles alone did not alter nociceptive baseline thresholds or the effects of inflammatory stimuli (data not shown). Differences between responses were evaluated by one-way ANOVA followed by Bonferroni’s t test. Statistical differences were considered to be significant at P < 0.05.
Results
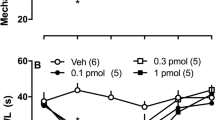
ET-1 induces dose-dependent mechanical hypernociception acting on endothelin ETA receptors
Firstly, i.pl. ET-1 (10, 30, and 100 pmol/paw) injection induced dose-dependent mechanical hypernociception compared to saline (25 μl) injection (Fig. 1a). Further confirming our previous findings (Verri et al. 2006b), the development of the hypernociception induced by 30 pmol of ET-1 at 3 and 5 h was reduced by prior treatment (at 30 nmol, i.pl., 30 min beforehand) with BQ-123, but not BQ-788 (Fig. 1b shows data at 3 h after ET-1 only). In addition, treatment with the dual ETA/ETB receptor antagonist bosentan (100 mg/kg, p.o., 5% acacia gum mucilage in water, 1 h beforehand) also alleviated ET-1-induced hypernociception (Fig. 1c). Thus, ET-1-induced mechanical hypernociception depends on endothelin ETA receptors in mice. We next investigated if this same receptor mediated the hypernociception associated with OVA challenge-induced inflammation.
ET-1 induces dose-dependent mechanical hypernociception acting on endothelin ETA receptors. a Mice received an i.pl. injection of ET-1 (10, 30, and 100 pmol/paw) or saline (25 μl). b Mice were treated with BQ-123 (30 nmol/paw, in saline, 30 min beforehand) or BQ-788 (same dose) before ET-1 (30 pmol/paw). c Mice were treated with bosentan (100 mg/kg, p.o., 5% acacia gum mucilage in water, 1 h beforehand) before ET-1 i.pl. injection. The mechanical hypernociceptive responses were evaluated 3 h after by the electronic pressure-meter. Bars represent means ± SEM of the delta reaction threshold, n = 4–5 per group per experiment, twp separate experiments. *P < 0.05 compared to saline group and #P < 0.05 compared to the lower dose of ET-1 (a) or vehicle group (b and c). One-way ANOVA followed by Bonferroni’s multiple comparison t test
OVA challenge induces endothelin-mediated mechanical hypernociception
Mice immunized with OVA (OVA Im) were treated with bosentan, BQ-123, or BQ-788 (doses described for Fig. 1) before OVA challenge (3 μg/paw). Sham-immunized mice (Sham Im) were also challenged with OVA. It was detected that bosentan (Fig. 2a), BQ-123, and BQ-788 (Fig. 2b) treatments inhibited OVA challenge-induced mechanical hypernociception 3 (Fig. 2a and b) and 5 h (data not shown) after antigen injection. These results suggest that endothelin acting on endothelin ETA and ETB receptors mediate OVA challenge-induced mechanical hypernociception in mice. This endothelin role in OVA challenge-induced inflammation was confirmed by the detection of ET-1 production in the paw skin 3 h after OVA challenge in OVA Im compared to Sham Im mice (Fig. 2c).
OVA challenge induces endothelin-mediated mechanical hypernociception and ET-1 production. a Immunized mice (OVA Im) were treated with bosentan, as described in Fig. 1 before OVA challenge (3 μg/paw) or saline (25 μl). b OVA Im mice were treated with BQ-123 or BQ-788 as described in Fig. 1 before OVA challenge or saline. Sham-immunized mice (Sham Im) were also challenged with OVA. The hypernociceptive responses were evaluated 3 h after by the electronic pressure-meter. Bars represent means ± SEM of the delta reaction threshold, n = 4–5 per group per experiment, two separate experiments. c ET-1 levels in hind-paw skin collected 3 h after OVA Im mice were challenged with OVA or saline, and Sham Im mice were challenged with OVA. Bars represent means ± SEM values (n = 4 per group per experiment, two separate experiments). *P < 0.05 compared to saline and Sham Im control groups and #P < 0.05 compared to vehicle group (a and b). One-way ANOVA followed by Bonferroni’s multiple comparison t test
OVA challenge induces neutrophil migration to the paw tissue mediated by endothelin acting on endothelin ETA and ETB receptors in mice
OVA Im mice were treated with BQ-123 or BQ-788 before OVA challenge (doses described for Fig. 1). Sham Im mice were also challenged with OVA (Fig. 3). It was detected that BQ-123 and BQ-788 treatments inhibited OVA challenge-induced neutrophil migration to the paw skin tissue as detected by the increase in MPO activity 5 h after challenge (Fig. 3). This result suggests that endothelin acting on endothelin ETA and ETB receptors mediates OVA challenge-induced neutrophil migration to the paw skin.
OVA challenge induces neutrophil migration to the paw mediated by endothelin acting on endothelin ETA and ETB receptors in mice. Immunized mice (OVA Im) were treated with BQ-123 or BQ-788 as described in Fig. 1 before OVA challenge (as described in Fig. 2). Sham-immunized mice (Sham Im) were also challenged with OVA. Bars represent means ± SEM, n = 5 per group per experiment, two separate experiments. *P < 0.05 compared to saline and Sham Im control groups; #P < 0.05 compared to vehicles group. One-way ANOVA followed by Bonferroni’s multiple comparison t test
ET-1-induced mechanical hypernociception is neutrophil independent
ET-1 at the doses of 30 and 100 pmol/paw induced mechanical hypernociception, which was not inhibited by the pretreatment with fucoidin (20 mg/kg/i.v., in saline, 15 min beforehand) at 3 (Fig. 4a) and 5 h (data not shown). Fucoidin is a drug that binds l-selectin and, therefore, inhibits neutrophil migration. Other studies inhibited neutrophil-dependent mechanical hypernociception by using anti-neutrophil antibody and/or fucoidin treatments (Guerrero et al. 2008; Ting et al. 2007). Corroborating the absence of neutrophil participation in ET-1-induced mechanical hypernociception, ET-1 did not induce significant increase in neutrophil number in paw skin (Fig. 4b). The i.pl. injection of carrageenin (Cg, 100 μg/paw) was used as a control, which induced significant mechanical hypernociception (Fig. 4a) and increase of MPO activity in the same experiment performed with ET-1 (Fig. 4b). Both effects of Cg were inhibited by fucoidin treatment (Fig. 4a and b).
Endothelin induces neutrophil-independent hypernociception. a Mice were treated with fucoidin (20 mg/kg, i.v., in saline, 15 min beforehand) before i.pl. injection of ET-1 (30 or 100 pmol/paw) or carrageenin (Cg, 100 μg/paw). Mechanical hypernociception was evaluated after 3 h. b Samples of paw tissue were harvested 5 h after ET-1 or Cg injection as described for a and processed for MPO activity determination. Bars represent means ± SEM, n = 5 per group per experiment, two separate experiments. *P < 0.05 compared to saline control group; #P < 0.05 compared to vehicle group. One-way ANOVA followed by Bonferroni’s multiple comparison t test
OVA challenge induces PGE2 production in the paw skin tissue acting on endothelin ETA, but not endothelin ETB receptors in mice
OVA Im mice were treated with bosentan, BQ-123, or BQ-788 before OVA challenge (doses described for Fig. 1). Sham Im mice were also challenged with OVA (Fig. 5). Bosentan (Fig. 5a) and BQ-123, but not BQ-788 (Fig. 5b) treatments inhibited OVA challenge-induced PGE2 production 3 h after antigen challenge. This result suggests that endothelin acting on endothelin ETA, but not endothelin ETB receptors, mediate OVA challenge-induced PGE2 production in the paw skin.
OVA challenge induces endothelin ETA receptor-dependent PGE2 production in the mice paw skin. a Immunized mice (OVA Im) were treated with bosentan as described in Fig. 1 before OVA challenge (as described in Fig. 2). b OVA Im mice were treated with BQ-123 or BQ-788 as described in Fig. 1 before OVA challenge or saline. Sham-immunized mice (Sham Im) were also challenged with OVA. Samples of paw skin tissue were harvested after 3 h and processed for PGE2 measurement. Bars represent means ± SEM, n = 3–4 per group per experiment, two separate experiments. *P < 0.05 compared to saline and Sham Im control groups; #P < 0.05 compared to vehicles group. One-way ANOVA followed by Bonferroni’s multiple comparison t test
Discussion
The activation of endothelin receptors, mainly by ET-1, contributes to the development of inflammatory events such as leukocyte recruitment and nociception in inflammatory models (Ferreira et al. 1989; Raffa et al. 1996; Davar et al. 1998; Griswold et al. 1999; Griswold et al. 1999; Menéndez et al. 2003; Piovezan et al. 2000, 2004; Baamonde et al. 2004; Sampaio et al. 2004; Verri et al. 2005, 2007a, b, 2008a, b). In an attempt to further advance our understanding of the role of ETs in inflammation, we have herein addressed their possible participation in the inter-dependence between mechanical hypernociception and neutrophil recruitment in a model of immune inflammatory response triggered in the hind paw. The present results are in accordance with the hypothesis that during inflammation, endothelin ETA and ETB receptor activation is involved in the cascade of events responsible for hypernociception, at least in part, through up-regulation of neutrophil migration. Importantly, the activation of endothelin ETA receptors also contributed to the genesis of hypernociception by triggering PGE2 production.
ET-1 injection induces writhing in mice and mechanical hypernociception in rats and potentiates PGE2-induced knee joint incapacitation in dogs (Ferreira et al. 1989). Its injection also potentiates the formalin- and capsaicin-induced flinches in rats and mice (Piovezan et al. 1997; 1998) and induces mechanical and thermal hypernociception in mice and rats (Raffa et al. 1996; Menendez et al. 2003; Baamonde et al. 2004; da Cunha et al. 2004; Verri et al. 2004, 2005, 2007a). Thus, it is consistent in the literature that ET-1 injection induces overt nociception and hypernociception. These reports suggest that the nociceptive role of endothelin ETA and/or ETB receptors depends on the model, species, and dose of stimulus.
The finding that prior treatment with selective endothelin ETA and ETB receptor antagonists inhibited both neutrophil recruitment and mechanical hypernociception induced by OVA lines up well with the increased levels of ET-1 detected in the skin of the challenged hind paw. These results are in accordance with the data demonstrating the role of endothelin acting on both receptors to mediate OVA challenge-induced licking in mice (Piovezan et al. 2004). Nevertheless, the present study and that of Piovezan et al. (2004) differ in the type of behavior analyzed (licking versus mechanical hypernociception). In this regard, the doses of an algogen required to activate nociceptors to elicit overt nociception are usually higher than those needed to sensitize nociceptors to cause hypernociception. In addition, the study of Piovezan et al. (2004) used a protocol to induce a Th2 type of response, and we used a protocol to induce Th1 inflammation (Su et al. 2005; Du et al. 2005). Thus, it is likely that ET-1 is a mediator crucial for inflammatory hypernociception in both Th1 and Th2 responses. In fact, ET-1 seems to be important for other immune reactions such as anaphylactic shock (Filep et al. 1993).
The present results on neutrophil migration differ in experimental conditions compared to others reporting that endothelin is not involved in the acute (4 h) OVA challenge-induced neutrophil migration to the pleural cavity (Sampaio et al. 2000). Therefore, other factors such as resident cell profiles in each inflammatory foci (pleural cavity versus paw skin) might be also important. Recruited neutrophils may contribute to the development of hypernociception (Levine et al. 1984; Lavich et al. 2006; Guerrero et al. 2008; Ting et al. 2007; Cunha et al. 2008a, b). For instance, chemokines (chemotatic cytokines), cytokines (Cunha et al. 2008a, b), LTB4 (Levine et al. 1984; Guerrero et al. 2008), and C5a (Ting et al. 2007) induce hypernociception that is inhibited by neutrophil depletion (anti-neutrophil antibody or antineoplasic drugs) and/or neutrophil migration inhibition (fucoidin treatment). Furthermore, the kinetics of LTB4-induced pain in humans (Bisgaard and Kristensen 1985) and zymosan-induced articular hypernociception in mice (Guerrero et al. 2006) are the same as for neutrophil migration. In mice, neutrophils produce LTB4 and PGE2 and thus mediate zymosan hypernociception (Guerrero et al. 2008). In the present experiment, although both endothelin receptors mediate neutrophil migration and hypernociception during OVA inflammation, the injection of ET-1 induces ETA-mediated hypernociception independently of neutrophil recruitment. Indeed, the neutrophil migration in vivo is a complex multi-mediate event that requires the induction of the locomotion (chemotaxis) and activation of endothelial cells and neutrophils with consequent expression of adhesion molecules (Verri et al. 2007c; for review, see Petri et al. 2008). Therefore, if in our experimental condition ET-1 mediates one of these events, it might explain why the inhibition of its receptors blocks OVA-induced neutrophil migration, but the peptide administration was not able to promote neutrophil recruitment.
Besides the role of both endothelin receptors in mediating neutrophil migration and consequently the development of hypernociception during OVA-induced inflammation, it seems that ET-1 via the endothelin ETA receptor present in resident cells also mediated hypernociception by directly inducing PGE2 production, which in turn sensitizes the nociceptor. This suggestion is based on the following observation: (a) indomethacin treatment (cycloxygenase inhibitor) inhibits ET-1-induced writhing response and mechanical hypernociception in mice (Ferreira et al. 1989; Verri et al. 2006b); (b) at doses that do not induce an increase of MPO activity, ET-1 induces ETA-dependent and ETB-independent production of PGE2 (Verri et al. 2007a); (c) the mixed endothelin ETA/ETB or the selective endothelin ETA receptor antagonists, but not the selective endothelin ETB receptor antagonists, inhibited OVA-induced PGE2 production in the paw skin; (d) ET-1 induces PGE2 production by several cell types such as mesangial (Zoja et al. 1990; Coroneos et al. 1995) and peripheral lung microvascular smooth muscle cells (Chen et al. 2003).
The results also suggested that neutrophils recruited in response to ET-1 action on endothelin ETA/ETB receptors could contribute to OVA challenge-induced hypernociception by further production of other hypernociceptive mediators. In this sense, neutrophils produce different inflammatory mediators, including cytokines (Ethuin et al. 2001; 2004; Verri et al. 2007c), lipid metabolites (Tolone et al. 1977; for review, see Siminiak and Ozawa, 1993), and reactive oxygen species (Ishida et al. 1990; Nagase et al. 1990; Lund et al. 2005), and even ET-1 (Sessa et al. 1991; Cambiaggi et al. 2001).
Concluding, neutrophil migration and hypernociception during antigen (OVA) challenge-induced inflammation are amenable to endothelin ETA and ETB receptor antagonists. This study advances our understanding of the role of endothelin-mediated mechanisms during inflammation and further supports therapies directed at endothelin to inhibit inflammatory hypernociception and neutrophil migration.
References
Baamonde A, Lastra A, Villazon M, Bordallo J, Hidalgo A, Menendez L (2004) Involvement of endogenous endothelins in thermal and mechanical inflammatory hyperalgesia in mice. Naunyn Schmiedebergs Arch Pharmacol 369:245–251
Bisgaard H, Kristensen JK (1985) Leukotriene B4 produces hyperalgesia in humans. Prostaglandins 30:791–797
Bradley PP, Priebat DA, Christensen RD, Rothstein G (1982) Measurement of cutaneous inflammation: estimation of neutrophil content with an enzyme marker. J Invest Dermatol 78:206–209
Cambiaggi C, Mencarelli M, Muscettola M, Grasso G (2001) Gene expression of endothelin-1 (ET-1) and release of mature peptide by activated human neutrophils. Cytokine 14:230–233
Canetti C, Silva JS, Ferreira SH, Cunha FQ (2001) Tumour necrosis factor-alpha and leukotriene B(4) mediate the neutrophil migration in immune inflammation. Br J Pharmacol 134:1619–1628
Casagrande R, Georgetti SR, Verri WA Jr., Dorta DJ, dos Santos AC, Fonseca MJ (2006) Protective effect of topical formulations containing quercetin against UVB-induced oxidative stress in hairless mice. J Photochem Photobiol B 84:21–27
Chen D, Balyakina EV, Lawrence M, Christman BW, Meyrick B (2003) Cyclooxygenase is regulated by ET-1 and MAPKs in peripheral lung microvascular smooth muscle cells. Am J Physiol Lung Cell Mol Physiol 284:L614–621
Chichorro JG, Zampronio AR, Rae GA (2006) Endothelin ET(B) receptor antagonist reduces mechanical allodynia in rats with trigeminal neuropathic pain. Exp Biol Med (Maywood, NJ) 231:1136–1140
Conte FD, Barja-Fidalgo C, Verri WA Jr, Cunha FQ, Rae GA, Penido C, Henriques MD (2008) Endothelins modulate inflammatory reaction in zymosan-induced arthritis: participation of LTB4, TNF-α, and CXCL-1. J Leukoc Biol 84:652–660
Coroneos E, Kester M, Thomas P, Dunn MJ (1995) Endothelin regulates PGE2 formation in rat mesangial cells through induction of prostaglandin endoperoxide synthase-2. Adv Prostaglandin Thromboxane Leukot Res 23:117–119
Cunha TM, Verri WA Jr, Poole S, Parada CA, Cunha FQ, Ferreira SH (2007) Pain facilitation by proinflammatory cytokine actions at peripheral nerve terminals. In: Sorkin L, DeLeo J, Watkins LR (eds) Immune and glial regulation of pain. IASP, Seattle
Cunha TM, Barsante MM, Guerrero AT, Verri WA Jr., Ferreira SH, Coelho FM, Bertini R, Di Giacinto C, Allegretti M, Cunha FQ, Teixeira MM (2008a) Treatment with DF 2162, a non-competitive allosteric inhibitor of CXCR1/2, diminishes neutrophil influx and inflammatory hypernociception in mice. Br J Pharmacol 154:460–470
Cunha TM, Verri WA Jr, Schivo IR, Napimoga MH, Parada CA, Poole S, Teixeira MM, Ferreira SH, Cunha FQ (2008b) Crucial role of neutrophils in the development of mechanical inflammatory hypernociception. J Leukoc Biol 83:824–832
Cunha TM, Verri WA Jr., Vivancos GG, Moreira IF, Reis S, Parada CA, Cunha FQ, Ferreira SH (2004) An electronic pressure-meter nociception paw test for mice. Braz J Med Biol Res 37:401–407
da Cunha JM, Rae GA, Ferreira SH, Cunha FQ (2004) Endothelins induce ETB receptor-mediated mechanical hypernociception in rat hindpaw: roles of cAMP and protein kinase C. Eur J Pharmacol 501:87–94
Davar G, Hans G, Fareed MU, Sinnott C, Strichartz G (1998) Behavioral signs of acute pain produced by application of endothelin-1 to rat sciatic nerve. Neuroreport 9:2279–2283
Dhaun N, Pollock DM, Goddard J, Webb DJ (2007) Selective and mixed endothelin receptor antagonism in cardiovascular disease. Trends Pharmacol Sci 28:573–579
Du X, Tabeta K, Mann N, Crozat K, Mudd S, Beutler B (2005) An essential role for Rxr alpha in the development of Th2 responses. Eur J Immunol 35:3414–3423
Elferink JG, de Koster BM (1994) Endothelin-induced activation of neutrophil migration. Biochem Pharmacol 48:865–871
Elferink JG, de Koster BM (1996) Modulation of human neutrophil chemotaxis by the endothelin-B receptor agonist sarafotoxin S6c. Chem Biol Interact 101:165–174
Ethuin F, Delarche C, Benslama S, Gougerot-Pocidalo MA, Jacob L, Chollet-Martin S (2001) Interleukin-12 increases interleukin 8 production and release by human polymorphonuclear neutrophils. J Leukoc Biol 70:439–446
Ethuin F, Gerard B, Benna JE, Boutten A, Gougereot-Pocidalo MA, Jacob L, Chollet-Martin S (2004) Human neutrophils produce interferon gamma upon stimulation by interleukin-12. Lab Invest 84:1363–1371
Ferreira SH, Romitelli M, de Nucci G (1989) Endothelin-1 participation in overt and inflammatory pain. J Cardiovasc Pharmacol 13(Suppl 5):S220–222
Filep JG, Telemaque S, Battistini B, Sirois P, D’Orleans-Juste P (1993) Increased plasma levels of endothelin during anaphylactic shock in the guinea-pig. Eur J Pharmacol 239:231–236
Griswold DE, Douglas SA, Martin LD, Davis TG, Davis L, Ao Z, Luttmann MA, Pullen M, Nambi P, Hay DW, Ohlstein EH (1999) Endothelin B receptor modulates inflammatory pain and cutaneous inflammation. Mol Pharmacol 56:807–812
Guerrero AT, Verri WA Jr., Cunha TM, Silva TA, Rocha FA, Ferreira SH, Cunha FQ, Parada CA (2006) Hypernociception elicited by tibio-tarsal joint flexion in mice: a novel experimental arthritis model for pharmacological screening. Pharmacol Biochem Behav 84:244–251
Guerrero AT, Verri WA Jr., Cunha TM, Silva TA, Schivo IR, Dal-Secco D, Canetti C, Rocha FA, Parada CA, Cunha FQ, Ferreira SH (2008) Involvement of LTB4 in zymosan-induced joint nociception in mice: participation of neutrophils and PGE2. J Leukoc Biol 83:122–130
Ishida K, Takeshige K, Minakami S (1990) Endothelin-1 enhances superoxide generation of human neutrophils stimulated by the chemotactic peptide N-formyl-methionyl-leucyl-phenylalanine. Biochem Biophys Res Commun 173:496–500
Khodorova A, Fareed MU, Gokin A, Strichartz GR, Davar G (2002) Local injection of a selective endothelin-B receptor agonist inhibits endothelin-1-induced pain-like behavior and excitation of nociceptors in a naloxone-sensitive manner. J Neurosci 22:7788–7796
Lavich TR, Siqueira Rde A, Farias-Filho FA, Cordeiro RS, Rodrigues e Silva PM, Martins MA (2006) Neutrophil infiltration is implicated in the sustained thermal hyperalgesic response evoked by allergen provocation in actively sensitized rats. Pain 125:180–187
Levine JD, Lau W, Kwiat G, Goetzl EJ (1984) Leukotriene B4 produces hyperalgesia that is dependent on polymorphonuclear leukocytes. Science 225:743–745
Lund AK, Peterson SL, Timmins GS, Walker MK (2005) Endothelin-1-mediated increase in reactive oxygen species and NADPH oxidase activity in hearts of aryl hydrocarbon receptor (AhR) null mice. Toxicol Sci 88:265–273
Menendez L, Lastra A, Hidalgo A, Baamonde A (2003) Nociceptive reaction and thermal hyperalgesia induced by local ET-1 in mice: a behavioral and Fos study. Naunyn Schmiedebergs Arch Pharmacol 367:28–34
Nagase T, Fukuchi Y, Jo C, Teramoto S, Uejima Y, Ishida K, Shimizu T, Orimo H (1990) Endothelin-1 stimulates arachidonate 15-lipoxygenase activity and oxygen radical formation in the rat distal lung. Biochem Biophys Res Commun 168:485–489
Petri B, Phillipson M, Kubes P (2008) The physiology of leukocyte recruitment: an in vivo perspective. J Immunol 180:6439–6446
Piovezan AP, D’Orleans-Juste P, Tonussi CR, Rae GA (1997) Endothelins potentiate formalin-induced nociception and paw edema in mice. Can J Physiol Pharmacol 75:596–600
Piovezan AP, D’Orleans-Juste P, Tonussi CR, Rae GA (1998) Effects of endothelin-1 on capsaicin-induced nociception in mice. Eur J Pharmacol 351:15–22
Piovezan AP, D’Orleans-Juste P, Souza GE, Rae GA (2000) Endothelin-1-induced ET(A) receptor-mediated nociception, hyperalgesia and oedema in the mouse hind-paw: modulation by simultaneous ET(B) receptor activation. Br J Pharmacol 129:961–968
Piovezan AP, D’Orleans-Juste P, Frighetto M, Souza GE, Henriques MG, Rae GA (2004) Endothelins contribute towards nociception induced by antigen in ovalbumin-sensitised mice. Br J Pharmacol 141:755–763
Pontiroli AE, Pizzocri P, Koprivec D, Vedani P, Marchi M, Arcelloni C, Paroni R, Esposito K, Giugliano D (2004) Body weight and glucose metabolism have a different effect on circulating levels of ICAM-1, E-selectin, and endothelin-1 in humans. Eur J Endocrinol 150:195–200
Raffa RB, Schupsky JJ, Jacoby HI (1996) Endothelin-induced nociception in mice: mediation by ETA and ETB receptors. J Pharmacol Exp Ther 276:647–651
Sampaio AL, Rae GA, Henriques MG (2000) Participation of endogenous endothelins in delayed eosinophil and neutrophil recruitment in mouse pleurisy. Inflamm Res 49:170–176
Sampaio AL, Rae GA, Henriques MG (2004) Effects of endothelin ETA receptor antagonism on granulocyte and lymphocyte accumulation in LPS-induced inflammation. J Leukoc Biol 76:210–216
Sessa WC, Kaw S, Hecker M, Vane JR (1991) The biosynthesis of endothelin-1 by human polymorphonuclear leukocytes. Biochem Biophys Res Commun 174:613–618
Siminiak T, Ozawa T (1993) Neutrophil mediated myocardial injury. Int J Biochem 25:147–156
Su SB, Silver PB, Grajewski RS, Agarwal RK, Tang J, Chan CC, Caspi RR (2005) Essential role of the MyD88 pathway, but nonessential roles of TLRs 2, 4, and 9, in the adjuvant effect promoting Th1-mediated autoimmunity. J Immunol 175:6303–6310
Ting E, Guerrero AT, Cunha TM, Verri WA Jr, Taylor SM, Woodruff TM, Cunha FQ, Ferreira SH (2007) Role of complement C5a in mechanical inflammatory hypernociception: potential use of C5a receptor antagonists to control inflammatory pain. Br J Pharmacol 153:1043–1053
Tolone G, Bonasera L, Tolone C (1977) PGE2 production by human polymorphonuclear leukocytes. Boll Ist Sieroter Milan 56:399–400
Valerio DA, Cunha TM, Arakawa NS, Lemos HP, Da Costa FB, Parada CA, Ferreira SH, Cunha FQ, Verri WA Jr (2007) Anti-inflammatory and analgesic effects of the sesquiterpene lactone budlein A in mice: inhibition of cytokine production-dependent mechanism. Eur J Pharmacol 562:155–163
Verri WA Jr, Schivo IR, Cunha TM, Liew FY, Ferreira SH, Cunha FQ (2004) Interleukin-18 induces mechanical hypernociception in rats via endothelin acting on ETB receptors in a morphine-sensitive manner. J Pharmacol Exp Ther 310:710–717
Verri WA Jr, Molina RO, Schivo IR, Cunha TM, Parada CA, Poole S, Ferreira SH, Cunha FQ (2005) Nociceptive effect of subcutaneously injected interleukin-12 is mediated by endothelin (ET) acting on ETB receptors in rats. J Pharmacol Exp Ther 315:609–615
Verri WA Jr, Cunha TM, Parada CA, Poole S, Cunha FQ, Ferreira SH (2006a) Hypernociceptive role of cytokines and chemokines: targets for analgesic drug development? Pharmacol Ther 112:116–138
Verri WA Jr, Cunha TM, Parada CA, Wei XQ, Ferreira SH, Liew FY, Cunha FQ (2006b) IL-15 mediates immune inflammatory hypernociception by triggering a sequential release of IFN-γ, endothelin, and prostaglandin. Proc Natl Acad Sci U S A 103:9721–9725
Verri WA Jr, Cunha TM, Parada CA, Poole S, Liew FY, Ferreira SH, Cunha FQ (2007a) Antigen-induced inflammatory mechanical hypernociception in mice is mediated by IL-18. Brain Behav Immun 21:535–543
Verri WA Jr, Cunha TM, Poole S, Ferreira SH, Cunha FQ (2007b) Cytokine inhibitors and pain control. Rev Bras Reumatol 47(5):341–353
Verri WA Jr, Cunha TM, Ferreira SH, Wei X, Leung BP, Fraser A, McInnes IB, Liew FY, Cunha FQ (2007c) IL-15 mediates antigen-induced neutrophil migration by triggering IL-18 production. Eur J Immunol 37:3373–3380
Verri WA Jr, Cunha TM, Magro DA, Domingues AC, Vieira SM, Souza GR, Liew FY, Ferreira SH, Cunha FQ (2008a) Role of IL-18 in overt pain-like behaviour in mice. Eur J Pharmacol 588:207–212
Verri WA Jr., Guerrero AT, Fukada SY, Valerio DA, Cunha TM, Xu D, Ferreira SH, Liew FY, Cunha FQ (2008b) IL-33 mediates antigen-induced cutaneous and articular hypernociception in mice. Proc Natl Acad Sci U S A 105:2723–2728
Yanagisawa M, Kurihara H, Kimura S, Tomobe Y, Kobayashi M, Mitsui Y, Yazaki Y, Goto K, Masaki T (1988) A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature 332:411–415
Zimmermann M (1983) Ethical guidelines for investigations of experimental pain in conscious animals. Pain 16:109–110
Zoja C, Benigni A, Renzi D, Piccinelli A, Perico N, Remuzzi G (1990) Endothelin and eicosanoid synthesis in cultured mesangial cells. Kidney Int 37:927–933
Acknowledgments
We thank Ieda R.S. Schivo, Giuliana B. Francisco, and Sérgio R. Rosa for technical assistance. We also thank Actelion Pharmaceuticals Ltd (Allschwil, Switzerland) for the generous gift of bosentan. This work was supported by grants from Fundação de Amparo à Pesquisa do Estado de São Paulo, Conselho Nacional de Pesquisa, and Coordenadoria de Aperfeiçoamento de Pessoal de Nível Superior, Brazil. WAVJ and TMC contributed equally to this work.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Verri Jr, W.A., Cunha, T.M., Magro, D.A. et al. Targeting endothelin ETA and ETB receptors inhibits antigen-induced neutrophil migration and mechanical hypernociception in mice. Naunyn-Schmied Arch Pharmacol 379, 271–279 (2009). https://doi.org/10.1007/s00210-008-0360-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-008-0360-1