Abstract
Longitudinal conduction of endothelium-dependent vasodilatation is mediated by intercellular spread of hyperpolarization via gap junctions along the endothelium. If similar electrical signals from the endothelium conduct around the circumference of arteries via smooth muscle cells, then, both longitudinal and circumferential spread of such signals would make it possible for a wide annulus of a large blood vessel like an epicardial coronary artery to dilate to local stimuli. To examine this in vitro, we developed a dual-chambered organ bath in which both membrane potential and force are independently determined in endothelium-intact and -denuded regions of a single annulus of artery. Hyperpolarizations and relaxations to endothelium-dependent vasodilators like bradykinin (BK) and substance P in smooth muscle cells immediately beneath the local endothelium-intact region (local responses) are conducted via smooth muscle cells around the circumference of the artery. The local relaxation was partially inhibited by the nitric oxide synthase inhibitor, N G-nitro-l-arginine (l-NOARG), and subsequently abolished by further treatment with a combination of two characteristic inhibitors of endothelium-dependent hyperpolarization—the Ca2+-activated potassium channel (KCa) channel inhibitors, apamin and charybdotoxin. The conducted hyperpolarizations and relaxations to BK were unaffected by l-NOARG, but were abolished by apamin and charybdotoxin. In conclusion, these studies demonstrate for the first time that NO acts only as a local vasodilator, whereas endothelium-dependent hyperpolarization (EDH) causes local and remote vasodilatation in large coronary arteries. We propose that such a remote EDH-dependent signalling mechanism compensates for the loss of the local NO-dependent vasodilatation in diseased arteries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endothelial cells release NO and prostacyclin (PGI2) and cause smooth muscle hyperpolarization and vasodilatation when stimulated either by agonists such as bradykinin (BK) or by physical forces such as shear stress, flow and pulsatility (for reviews, Campbell and Harder 2001; Busse et al. 2002; Griffith 2004). While the mechanisms by which NO and PGI2 evoke vasodilatation are well characterised, the chemical identity and mechanism of action of endothelium-dependent hyperpolarization (EDH) remain elusive but appear to be both vessel- and species-dependent (Cohen 2005). The first proposal indicates that an endothelium-dependent hyperpolarizing factor (EDHF) be released by the endothelium into the extracellular space, which then diffuses to the underlying smooth muscle in a paracrine-dependent fashion. Three candidates for this paracrine EDHF have been put forth, including K+ ion (Edwards et al. 1998), 11,12 epoxyeicosatrienoic acid (11,12 EET; Campbell et al. 1996; Fisslthaler et al. 1999; Gauthier 2002) or the reactive oxygen specimen, hydrogen peroxide (H2O2; Matoba et al. 2000). The second proposal involves the direct transfer of hyperpolarization from the endothelium to the smooth muscle via myo-endothelial gap junctions (Chaytor et al. 1998; Hill et al. 2000). Despite the many uncertainties regarding EDH, it appears that EDH responses in the majority of vascular beds are sensitive to a combination of two Ca2+-activated K+ channel (KCa) inhibitors, namely apamin (a selective inhibitor of small conductance KCa channels) and charybdotoxin (a non-selective inhibitor of large and intermediate conductance KCa channels; for review, see Feletou and Vanhoutte 2006). It is important to note that in certain blood vessels such as the rat middle cerebral artery, there is no role for SKCa channels in the EDH-mediated dilatation, whereas in porcine coronary artery, both SKCa and intermediate KCa channels underpin these responses (Feletou and Vanhoutte 2006).
EDH has been demonstrated to spread along both endothelial and smooth muscle layers via intercellular pathways to evoke ascending and descending vasodilatation in the microvasculature (for review see Segal 2005; Segal and Duling 1995; Xia and Duling 1995; Segal 1994). For example, in hamster skeletal muscle, ascending spread of hyperpolarization via the endothelium from small muscle arterioles to the main feeder artery causes vasodilatation in the main feeder artery, which increases blood flow during muscle contraction (Segal et al. 1999; Segal 2000; Segal and Jacobs 2001). Similarly, in hamster cheek pouch arterioles, spread of hyperpolarization along both the endothelial and smooth muscle layers has been shown to not only cause ascending and descending vasodilatation along the arterioles themselves (Bartlett and Segal 2000), but also to spread to smaller capillaries (Beach et al. 1998). This electrical continuity between capillaries and arterioles permits overall tissue and organ blood flow to be controlled by chemical mediators within the immediate capillary microenvironment. Thus, intercellular conduction of EDH can be envisaged as a rapid deployment mechanism by which local electrical signals triggered by chemical or other stimuli in one cell can be relayed over large distances to remote cells of the same or different type that cannot be achieved by diffusion of the original activating stimuli. Based on observations made in small arterioles, it is hypothesized that intercellular conduction of EDH generated by the flat monolayer of endothelial cells in larger muscular arteries might be an important mechanism for signalling to underlying medial smooth muscle cells which may otherwise never be directly exposed to the original activating stimulus. Moreover, whilst some stimuli such as shear stress or pulsatility are likely to activate the entire endothelial cell layer to generate NO, PGI2 and EDH within a given annulus of artery, intercellular spread of EDH around the circumference of the artery might allow for the coordination of a similar dilatation in response to stimuli that activate much smaller regions of endothelium within the annulus, such as platelet aggregation. Thus, any remote signalling effects of EDH may be crucial in the regulation of vascular homeostasis in large conduit vessels of the heart and brain, which are susceptible to the development of arterial disease.
To study the potential remote signalling effects of EDH in large coronary arteries, we designed a two-chambered organ bath, which allowed us to focally apply endothelium-dependent vasodilators such as BK to endothelium-intact regions of an artery strip, whilst simultaneously recording membrane potential and tension in remote endothelium-denuded regions of the same strip of artery.
Materials and methods
Tissue preparation
Hearts from freshly slaughtered, white large pigs (n = 97) were obtained from a local abattoir and transported back to the laboratory in ice-cold (∼4°C) Krebs (composition in mM; Na+ 143.1, K+ 5.9, Ca2+ 2.5, Mg2+ 1.2, Cl− 127.8, \({\text{HCO}}^{ - }_{{\text{3}}} \)25.0, \({\text{SO}}^{{{\text{2}} - }}_{{\text{4}}} \) 1.2, \({\text{H}}_{{\text{2}}} {\text{PO}}^{ - }_{4} \) 1.2 and glucose 11.0) solution. The right coronary artery (∼3 mm in diameter) was dissected away from the surrounding myocardium, cleared of fat and connective tissue and then cut into ring segments (3 mm in length).
Dual-chamber organ bath
A strip of pig coronary artery with the orientation of the circular muscle running in parallel with the length of the strip was prepared by ‘cutting open’ an ∼3 mm wide ring segment. After mechanically removing the endothelium from ∼60% of the artery strip with a Krebs-moistened cotton tip, the strip was then anchored to a sylgard-based, horizontally arranged organ chamber with a row of fine gauge pins at the boundary of the endothelium-intact and endothelium-denuded regions (Fig. 1). A second row of pins parallel to the first was then used to further anchor the preparation at a position 1.5 mm from the boundary between the two regions within the endothelium-denuded region. The fixed region of the artery strip without endothelium between the two rows of pins, termed here the ‘conduction zone’, allowed force to be recorded from both ends of each region independently from each other. Changes in isometric force were amplified (BMRI; Melbourne, Australia) and displayed on chart recorders (W &W recorder 330; Basel, Switzerland). To partition the two regions of the artery into separate Krebs-perfused (∼4 ml/min; 37°C) leak-free organ chambers (1 ml), a plastic barrier was placed in between the two rows of pins. Signs of any leak across the tightly fitted barrier were determined at the end of each experiment by perfusing Evans blue dye into one of the chambers and then analysing the amount of Evans blue in the effluent of the other chamber spectrophotometrically. If the dual chamber was leak-free, then region-specific application of agonists and antagonists could be achieved. In some experiments, the plastic partition was removed (open mode) such that agonists and antagonists were applied to both regions of the strip simultaneously.
Schematic diagram showing a top view of the dual chambered organ bath containing a circumferentially arranged strip of pig coronary artery. This arrangement allows independent measurements of force from an endothelium-intact (+E) and endothelium-denuded (−E) region of artery, as well as changes in membrane potential (E m) in smooth muscle cells using standard intracellular microelectrode techniques. In most experiments, a plastic partition, depicted here as a thick black line between each chamber, is placed between the row of anchoring pins to seal each chamber into separate leak proof and Krebs-perfused organ baths. This configuration is referred to as the ‘partitioned’ mode and that with the partition removed, the ‘open’ mode
After a 30-min equilibration period, both regions of the artery strip were independently given a passive resting tension of 1 g for 20 min, after which time, they were stretched again in a similar manner to 1 g. After a stable level of passive force, both regions of the artery strip were then simultaneously exposed to an isotonic high K+ (125 mM) depolarising Krebs solution to obtain a maximum contraction. Once the contraction to high K+ stabilised, the high K+ Krebs solution was replaced with normal K+-containing Krebs solution, and then arteries were allowed a 30-min period to reach a stable level of resting active force. All arteries were then incubated with Krebs solution containing indomethacin (3 μM) to eliminate any contribution of vasoactive prostanoids. At the same time, some arteries were pre-treated with either the NO synthase (NOS) inhibitor, N G-nitro-l-arginine (l-NOARG; 100 μM), the dual combination of the small conductance Ca2+-activated K+ channel inhibitor, apamin (100 nM) and intermediate/large conductance Ca2+-activated K+ channel inhibitor, charybdotoxin (30 nM) or the cytochrome P4502C inhibitor, sulphaphenazole (10 μM). Some l-NOARG (100 μM)-treated arteries were concomitantly exposed to either a combination of apamin (100 nM) and charybdotoxin (30 nM) or sulphaphenazole (10 μM) for 30 min.
Artery strips were contracted to ∼40% of their maximum contraction to high K+ with titrated concentrations of U46619. When a stable level of active force was achieved to U46619, BK, SP, sodium nitroprusside (10 μM) or cromakalim (0.1 mM) was applied either to a specific region (partitioned mode) or to both regions (open mode) of the dual-chamber organ bath. With the perfusing solution flowing at 4 ml/min, the agonist total exposure time was ∼15–20 s.
Electrophysiology
Circumferentially arranged strips of pig coronary artery were pinned with fine-gauge wires with the intimal surface facing up in the open mode chamber and perfused with Krebs solution at (37°C) at 4 ml/min. Standard microelectrode techniques were used to measure changes in membrane potential from either smooth muscle cells underlying the endothelium or from smooth muscle cells that were ∼2.5 mm from the boundary between the endothelium-denuded and -intact regions in the endothelium-denuded region of the artery strip. Briefly, capillary glass microelectrodes (Clark Electromedical Instruments; borosilicate glass capillaries; GC-120F10) ‘backfilled’ with KCl (0.5 mol/l) had resistances in the range 80–120 MΩ. A fine Ag/AgCl− coated electrode connected to a Headstage (HS-2 Axon Instruments, USA) was placed in the lumen of the capillary microelectrode to transmit changes in electrical events occurring in the smooth muscle to the recording devices. These responses were recorded against a second ‘reference’ Ag/AgCl− electrode that was placed in the bath medium adjacent to the strip of artery. Electrical events were amplified (Axonprobe-1A-multipurpose microelectrode amplifier, Axon Instruments), digitized (sampling rate = 1,024 points per record) with an analogue to digital converter (DMA-Interface, Model TL-1, Axon Instruments) and then recorded on a SCAN analysis program on a PC computer. Successful impalement of a smooth muscle cell was determined as follows. The first, sharp negative shift in membrane potential was due to endothelial cell penetration, as the microelectrode was inserted via the intimal surface of the artery. The microelectrode was then further advanced leading to a rapid return of the membrane potential after crossing the endothelial cell and dislodgement of the microelectrode. After further advancing the microelectrode, a second sharp negative shift in membrane potential was taken as a successful impalement of a smooth muscle cell. Agonists were applied to arteries only after a 10-min stable period of impalement.
Data presentation and statistical analyses
Relaxations were expressed as a percentage of the initial contraction to U46619 and calculated as mean±SEM. Differences in responses between treatment groups were compared statistically using Student’s unpaired t tests with significance accepted at the P < 0.05 level. Peak hyperpolarizations from resting membrane potentials were measured in millivolts (mV).
Drugs and their suppliers
Bradykinin acetate salt, 8-methyl-N-vanillyl-6-nonenamide (capsaicin), cromakalim, glibenclamide, N G-nitro-l-arginine, substance P acetate salt, sulphaphenazole, tetrodotoxin citrate (Sigma Chemical, USA); apamin, charybdotoxin, nifedipine, 1,5,5-hydroxy-11-(epoxymethano) prosta-5Z, 13E-dienoic acid (U46619; Sapphire Bioscience, Sydney, Australia); sodium nitroprusside (David Bull Laboratories, Victoria, Australia).
Results
Dual-chamber organ bath studies; control responses in the partitioned mode
Addition of a single concentration of BK (0.5 μM) to the endothelium-intact region of the dual-chamber organ bath caused a near-maximum relaxation in that region (termed here ‘local relaxation’) which was conducted 1.5 mm into the endothelium-denuded region of the strip (termed here ‘conducted relaxation’; Figs. 2 and 4). The conducted relaxations occurred nearly simultaneously with the local relaxations but never preceded them. Subsequent addition of the endothelium-dependent vasodilator thrombin (1 U/ml) specifically to the endothelium-denuded region caused no relaxations in either region of the artery strip, confirming firstly, effective removal of the endothelium in the denuded region and secondly, that a leak-free seal existed between the chambers (Fig. 2). Finally, addition of thrombin (1 U/ml) to the endothelium-intact region of the artery strip caused, like BK, a local relaxation (69.1 ± 1.1%, n = 6), which was conducted into the endothelium-denuded region of the strip (conducted relaxation 56.4 ± 4.0%; n = 6; Fig. 2). A similar pattern of local and conducted relaxation to those obtained with BK and thrombin also occurred with SP (50 nM), 5-HT (10 μM) or ADP (100 μM; Fig. 2).
Demonstration of local and conducted (C) relaxations to bradykinin (BK) and thrombin (Thr) in a single, circumferentially arranged strip of pig coronary artery in the partitioned mode dual-chamber organ bath as described in Fig. 1. In row a, the schematic diagrams of the dual-chamber organ bath show region specific (i.e. +E, endothelium-intact and −E, endothelium-denuded) application of BK or thrombin. Row b shows the digitized recordings of each section of the artery contracted to ∼40% F max with U46619. Breaks in the continuous traces are for clarity. Application of BK to the endothelium-intact (+E) region of the strip caused a local relaxation followed by conducted relaxation in the endothelium-denuded (−E) region. Subsequent application of thrombin to the −E region caused no response in both the +E and −E regions of the artery strip. Finally, application of thrombin to the +E region caused local relaxation and a conducted relaxation in the −E region. c Group data from experiments carried out with the dual-chamber bath in the partitioned mode showing local relaxations (expressed as a percentage of the U46619-induced contraction) and the resultant conducted relaxations in the −E region of the artery to BK, substance P (SP, 50 nM), thrombin, 5-HT (10 μM in the presence of ketanserin) and ADP (100 μM). Histograms represent mean±SEM from n = 6 experiments
Microelectrode impalements of pig coronary artery smooth muscle cells immediately beneath the endothelium-intact region of the artery strip or 2.5 mm downstream within the endothelium-denuded region of the artery strip indicated a resting membrane potential ranging from −40 to −50 mV. This range is consistent with previous reports, which utilised similar pig coronary artery preparations. Under these conditions, the concentration of U46619 (10 nM; similar concentration used in present study), which was required to contract pig coronary artery strips to 40% F max, did not significantly modify the resting membrane potential. Addition of either BK or SP caused local hyperpolarizations (SP, 23.6 ± 2.6 mV, n = 6) that were conducted at least 2.5 mm into the endothelium-denuded region (SP, 11.8 ± 1.1 mV, n = 6, Figs. 3 and 4).
Digitized recordings from pig coronary artery smooth muscle of local and circumferential conduction (C) of endothelium-dependent hyperpolarizations to bradykinin (BK). The schematic diagram of the dual-chamber organ bath shows a single region-specific application of BK. The horizontal time bar applies for both traces
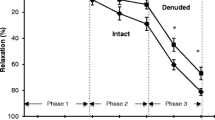
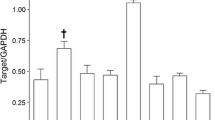
Evidence that circumferential conduction of endothelium-dependent hyperpolarization and relaxation to bradykinin (BK, 0.5 μmol/l) in pig coronary artery is independent of NO, but is due to KCa channel activation. Group data from experiments carried out with the dual-chamber bath in the partitioned mode show local relaxations (expressed as a percentage of the U46619-induced contraction) and hyperpolarizations (in mV) in the endothelium-intact (+E) region and the resultant conducted relaxations and hyperpolarizations in the endothelium-denuded (−E) region of the artery to BK in the absence (control) or presence of either l-NOARG, a combination of apamin (apa) and charybdotoxin (CBTX) or l-NOARG plus apamin and charybdotoxin. Histograms represent mean±SEM from n = 6 experiments. *(P < 0.05) and **(P < 0.01) represent statistical significance from controls
The dual-chamber organ bath is designed in such a way that any mechanical change in tension in one region of the artery strip will not affect the tension recorded in the opposing region. Yet, selective application of BK to the endothelium-intact region of an artery strip elicits a relaxation and hyperpolarization within that region, but also within the remote, opposing region of an endothelium-denuded section of the artery strip. Therefore, it appears that a signal can be generated in the endothelium-intact region, which spreads to the endothelium-denuded region of the artery strip. To determine whether or not the conducted responses occur via an intracellular pathway or whether they are the result of diffusion of a factor, we severed the conduction zone between the two rows of pins of a circumferentially arranged artery strip and then applied BK to the endothelium-intact region. All conducted relaxations to BK were abolished when the conduction zone was mechanically severed; however, the local endothelium-dependent relaxations were unaffected. By contrast, using intact coronary artery strip preparations, both conducted hyperpolarization, and relaxation to BK were unaffected by tetrodotoxin (0.3 μmol/l) and capsaicin (10 μmol/l) treatment (data not shown). These findings indicate that hyperpolarization spreads via the smooth muscle layer and that diffusion of a factor is unlikely to account for the conducted responses.
EDH, but not NO, causes conducted responses in pig coronary artery strips
Application of endothelium-dependent vasodilators to the endothelium-intact region of the artery strip in the dual-chamber organ bath caused local and conducted relaxations and hyperpolarizations into the endothelium-denuded region. To determine the contribution of NO and EDHF to the local and conducted responses, artery strips in the dual-chamber organ bath were exposed selectively to various inhibitors of NO and EDHF. Addition of l-NOARG (100 μM) specifically to the endothelium-intact region of the dual-chamber organ bath caused a local contraction in that region (0.25 ± 0.02 g, n = 7), but failed to cause a conducted contraction in the endothelium-denuded region. Thus, the inhibitory effects of basally released NO influence the contractile status of the underlying smooth muscle, but not that of remote smooth muscle. Also, l-NOARG had no effect on resting membrane potential (control, 44.6 ± 1.1 mV; l-NOARG, 42.1 ± 1.1 mV, n = 7). When l-NOARG was applied to the endothelium-intact region, it caused a small but significant inhibition of the local relaxations to either BK (Fig. 4) or SP (control; 86.2 ± 2.6% vs l-NOARG; 80.9 ± 1.6%, n = 6; P < 0.05), but no effect on the conducted relaxations to BK (Fig. 4) or SP (control; 61.1 ± 7.5% vs l-NOARG; 59.9 ± 5.8%). Also, l-NOARG had no effect on both the local and conducted hyperpolarizations to BK (Fig. 4) and SP (local: control 23.6 ± 2.3 mV, l-NOARG; 22 ± 3.6 mV, conducted: control 11.8 ± 1.1 mV, l-NOARG; 11.5 ± 2.8 mV).
The combination of apamin and charybdotoxin abolished both the local and conducted hyperpolarizations and conducted relaxations to BK (Fig. 4), but had no significant effect on the local relaxation to BK (Fig. 4). Apamin and charybdotoxin, however, abolished the local relaxations to BK in the presence of l-NOARG (Fig. 4). Finally, the inhibitor of cytochrome P4502C, sulphaphenazole (10 μmol/l), had no effect on both the local (83.6 ± 2.1%, n = 5) and conducted relaxations (51.2 ± 11.7%) to BK when it was applied to the endothelium-intact region.
Region-specific application of the NO donor, sodium nitroprusside (SNP, 10 μmol/l), caused a near-maximum local relaxation within that region; however, it failed to cause either smooth muscle hyperpolarization or a conducted relaxation (Fig. 5).
Digitized original traces demonstrating that exogenous application of the NO donor; sodium nitroprusside (SNP) does not cause circumferential conduction of relaxation in pig coronary artery. Each section of the artery was contracted to ∼40% F max with U46619 (indicated), and breaks in the continuous traces are for clarity. Application of SNP to the endothelium-intact (+E) region of a strip of pig coronary artery in the partitioned mode dual-chamber organ bath caused a local relaxation, but no conducted hyperpolarization (not shown) or relaxation into the endothelium-denuded (−E) region. Subsequent application of SNP to the −E region maximally relaxed that region. All responses are representative of six experiments
Next, we determined whether an endothelium-independent hyperpolarizing stimulus could initiate local and conducted responses in pig coronary artery in the dual-chamber organ bath. Application of the KATP channel opener, cromakalim (10 μmol/l), to a single region of the dual-chamber organ bath caused a local relaxation (98.7 ± 1.5%, n = 6) within the region directly exposed to cromakalim, and also a conducted relaxation (90.2 ± 9%; Fig. 6). The KATP channel inhibitor, glibenclamide (10 μM), abolished both the local and conducted relaxations to cromakalim when it was applied to the same region as cromakalim (Fig. 6). However, glibenclamide had no effect on the cromakalim-dependent local and conducted relaxations when it was applied to the opposite region (data not shown). Cromakalim caused a powerful hyperpolarization (27.2 ± 1.7 mV, n = 6) of pig coronary artery smooth muscle (Fig. 6).
Digitized original traces demonstrating circumferential conduction of relaxations and hyperpolarizations to cromakalim (Crom, 10 μM) in pig coronary artery. Each section of the artery was contracted to ∼40% F max with U46619 (indicated), and breaks in the continuous traces are for clarity. In a, application of cromakalim to the endothelium-denuded region caused a local relaxation within that region, as well as a conducted relaxation in the endothelium-intact region of the artery strip. Subsequent application of the KATP channel inhibitor, glibenclamide (10 μM), to the endothelium-intact region for 30 min abolished both local and conducted relaxations to cromakalim applied to the same region as glibenclamide. c Representative original trace showing hyperpolarization to cromakalim in pig coronary artery (n = 6). The horizontal time bar and vertical force bar apply for traces in both a and b
Assay for three-dimensional dissipation of current
Artery strips were modified such that any signal generated by the endothelium could also spread to remote smooth muscle cells in the longitudinal direction (Fig. 7). In these experiments, two longitudinally orientated endothelium-denuded regions of artery of ∼10mm in length were left adjacent to the endothelium-intact region of the artery strip, and force was still only recorded in the endothelium-denuded region within the circular annulus as described previously (Fig. 7). In this mode, BK (0.5 μmol/l) caused conducted relaxations in the endothelium-denuded region (38.2 ± 9.5%) that were unaffected by l-NOARG (Fig. 7) and abolished by apamin and charybdotoxin. The conducted relaxation to BK improved significantly (P < 0.05) when the two longitudinally arranged regions of artery were subsequently mechanically severed (66.3 ± 4.2%; Fig. 7).
a Schematic diagram showing a top view of a modified circumferential preparation of pig coronary artery in open-mode chamber. This preparation allows three-dimensional (3D) spread of current from a local source of endothelial cells (+E) by leaving two endothelium-denuded (−E) regions of artery adjacent to the +E region both upstream and downstream in the longitudinal direction. Thus, any signal generated within the +E region can spread circumferentially, tangentially and longitudinally. Force was recorded from an isolated region of artery as described in Fig. 1. b Histogram shows group data from four experiments as described in a. Open column is the mean±SEM conducted relaxation (expressed as a percentage of the U46619-induced contraction) to BK (0.5 μmol/l) in the presence of l-NOARG (100 μM), allowing for 3D current dissipation. The closed column represents the subsequent response to BK with only two-dimensional current dissipation after the longitudinally orientated smooth muscle regions were severed (dotted line). *P < 0.05 from controls
Discussion
Stimulation of a limited region of endothelium within an arterial annulus with endothelium-dependent vasodilators, like BK and SP, not only results in hyperpolarization and relaxation of smooth muscle directly beneath the region exposed to the agonist, but also hyperpolarization and relaxation in remote smooth muscle cells within the same annulus. These circumferentially conducted responses were not due to either NO, PGI2 or cytochrome P4502C-dependent metabolites of arachidonic acid. They were, however, characteristic of EDH in that they depended on KCa channel activation. This study is the first to demonstrate non-NO-dependent circumferential conduction of hyperpolarization and relaxation in large coronary arteries.
In standard organ baths, rings of large coronary arteries relax to BK in a completely endothelium-dependent manner. This response to BK is partially inhibited by the NOS inhibitor l-NOARG, with the remaining response abolished by a combination of apamin and charybdotoxin (Quignard et al. 1999). In the dual-chamber organ bath, l-NOARG alone or in combination with apamin and charybdotoxin had similar effects on the local relaxations to BK as those demonstrated in standard organ baths. Therefore, the local response to BK observed in both standard organ baths and the dual-chamber organ bath are due to both NO and EDH. However, as the present study demonstrates, only EDH-dependent relaxations were detected in the remote endothelium-denuded region of the same arterial annulus. That is, conducted relaxations initiated within the region of the annulus containing endothelium were completely resistant to l-NOARG, but were abolished by a combination of apamin and charybdotoxin. Our conclusions that these conducted responses are only due to EDH, and not NO, are strengthened by several additional findings. First, acute l-NOARG exposure caused only a local contraction and no conducted contraction, which would indicate that basally released endothelium-derived NO influences only the smooth muscle that is immediately abluminal to it. Second, exogenous application of NO failed to cause either hyperpolarization or a conducted relaxation over similar distances. Therefore, our data from the dual-chamber organ bath clearly differentiate the actions of NO and EDH in large coronary arteries; EDH is a long-distance remote signalling vasodilator mechanism, whereas NO acts only locally at its site of release.
The present study demonstrates that locally generated EDH not only reaches the underlying smooth muscle but it possesses sufficient electrical power to be conducted circumferentially over large distances to remote smooth muscle cells. However, the amount of current that can be conducted in the circumferential direction with the dual-chamber organ bath might have been overestimated, as this arrangement would only allow for current to dissipate in two dimensions (i.e. circumferentially and radially) from a region of endothelial cell activation excluding the third longitudinal dimension. To determine whether or not longitudinal current dissipation occurs and how it affects the circumferentially conducted responses to BK, a modified assay of the dual-chamber organ bath was designed. This set-up involved a standard circumferentially arranged strip of artery, but with two similar in width endothelium-denuded regions of artery, each of ∼10 mm in length, adjacent to either side of its endothelium-intact section in the longitudinal direction. Under these conditions, stimulation with BK of a similarly sized region of endothelium to that used in the original dual-chamber set-up was still able to generate a non-NO, EDH-dependent local signal that had sufficient electrical power to be conducted over 1.5 mm of circumferentially arranged smooth muscle cells to cause relaxation. These experiments clearly demonstrate that regardless of large ratios of unstimulated to stimulated regions of artery, circumferential spread of EDH can still take place, being favoured perhaps by the fact that smooth muscle cells are elongated in the circumferential direction. It is worth mentioning that the magnitude of relaxation that is conducted to the remote unstimulated site of the artery is dependent on the agonist used to stimulate endothelium-dependent hyperpolarization. For example, from the present study, although 5-HT caused a conducted relaxation, the magnitude of this response was markedly lower than those caused by all other agonists tested, including BK, SP, thrombin and ADP. A likely explanation for this is that 5-HT is less efficacious at stimulating EDH compared with the other agonists examined. Indeed, 5-HT has been previously demonstrated to cause endothelium-dependent hyperpolarization of pig coronary artery with a peak magnitude of ∼10 mV (Thollon et al. 1999), which is approximately half of that caused by BK (∼23 mV) and SP in the present study.
In addition to EDH spreading circumferentially in large coronary arteries as demonstrated here, EDH also spreads along the length of smaller arteries like the hamster feed artery via the endothelium (Emerson and Segal 2000). Segal and colleagues demonstrated that selective damage of the endothelial cell layer in the hamster feed artery inhibited the conducted vasodilatation to Ach, whereas selective damage of the smooth muscle layer in the intervening region between the activation site and the recording site had no effect (Emerson and Segal 2000). Such an endothelial cell pathway is suggestive from morphological studies, which demonstrate that endothelial cells are elongated longitudinally by the natural forces of blood flow (Haas and Duling 1997). Thus, for an electrical signal to cover a given length of arteriole, the path most likely offering the least electrical resistance is through the endothelium, as fewer endothelial cell membranes would need to be traversed compared with smooth muscle cells, which are also elongated but are aligned circumferentially. In the present study, selective damage of a zone of endothelium located between the stimulation region (endothelium-intact region) and the recording region (endothelium-denuded region) in pig coronary artery did not affect the conducted responses, indicating that the smooth muscle media acted as the pathway for circumferential spread of hyperpolarization and relaxation in this vessel. This was confirmed by two additional observations. First, BK was unable to evoke relaxation in the endothelium-denuded region of the artery strip when the smooth muscle within the conduction zone was mechanically severed. Second, smooth muscle hyperpolarization caused directly by activation of smooth muscle KATP channels with cromakalim was also conducted in a circumferential manner. It is noteworthy that endothelial cells are electrically and dye-coupled in situ in pig coronary artery (Beny and Gribi 1989) and are able to conduct a regenerative Ca2+ wave (Domenighetti et al. 1998). Therefore, like Ca2+ waves, an electrical signal such as EDH may spread via the endothelium along the longitudinal axis of such arteries. This, together with conduction of EDH around the circumference of the artery via medial smooth muscle cells, has the potential to mediate endothelium-dependent vasodilatation in a wide region of artery in response to localised stimuli.
Longitudinal conduction of vasodilatation in hamster cheek pouch arterioles is the result of spread of hyperpolarization through the endothelium via a passive non-regenerative mechanism (Xia and Duling 1995). In the present study, the circumferential spread of hyperpolarization in pig coronary smooth muscle also faded with distance. The local hyperpolarization to BK was ∼20 mV, but the conducted response measured at a distance of 2.5 mm away from the site of BK application was ∼10 mV. The fading property of EDH, together with our findings that the circumferentially conducted responses occurred nearly simultaneously with the local responses, indicate that the spread of hyperpolarization most likely occurs via passive electrotonic, non-regenerative mechanisms consistent with the cable properties of smooth muscle cells in pig coronary arteries (Pacicca et al. 1996). However, a cAMP-dependent regenerative mechanism such as the one demonstrated by Griffith et al. (2002) using rabbit iliac arteries cannot be ruled out, which may enhance passive electrotonic conduction.
In large conduit arteries, the radial transfer of EDH from the activated endothelial cells to underlying smooth muscle cells could be the result of a paracrine EDHF such as a cytochrome P450-dependent EET (Campbell et al. 1996; Fisslthaler et al. 1999), K+ (Edwards et al. 1998) or H2O2 (Matoba et al. 2000). We have previously shown in large bovine coronary arteries that non-NO, non-prostanoid-dependent relaxations are unlikely to be due to cytochrome P450 (Drummond et al. 2000). In the present study, we have additional evidence which indicates that the EDH-dependent remote responses in pig coronary arteries are also unlikely to be due to cytochrome P450-derived metabolites of arachidonic acid, as these responses were unaffected by sulphaphenazole (Fisslthaler et al. 1999). It is also unlikely that EDH-dependent responses are due to K+ ion in large coronary arteries (Drummond et al. 2000). An alternative possibility for the radial transfer of EDH from endothelium to smooth muscle is by electrotonic conduction of current via myoendothelial gap junctions (Cohen 2005; Griffith 2004).
In conclusion, our studies, together with several previous reports, suggest that electrotonic EDH can signal both longitudinally and circumferentially to remote endothelial cells and smooth muscle cells, respectively. These electrical properties would endow large muscular arteries with a remarkable capacity to maintain constant flow when endothelium-derived NO is compromised during vascular inflammation and oxidative stress.
References
Bartlett IS, Segal SS (2000) Resolution of smooth muscle and endothelial pathways for conduction along hamster cheek pouch arterioles. Am J Physiol 278:H604–H612
Beach JM, McGahren ED, Duling BR (1998) Capillaries and arterioles are electrically coupled in hamster cheek pouch. Am J Physiol 275:H1489–H1496
Beny JL, Gribi F (1989) Dye and electrical coupling of endothelial cells in situ. Tissue Cell 21:797–802
Busse R, Edward G, Feletou M, Fleming I, Vanhoutte P, Weston AH (2002) EDHF: bringing the concepts together. Trends Pharmacol Sci 23:374–380
Campbell WB, Harder DR (2001) Prologue: EDHF—what is it? Am J Physiol 280:H2413–H2416
Campbell WB, Gebremedhin D, Pratt PF, Harder DR (1996) Identification of epoxyeicosatrienoic acids as endothelium-derived hyperpolarizing factors. Circ Res 78:415–423
Chaytor AT, Evans WH, Griffith TH (1998) Peptides homologous to extracellular loop motifs of connexin 43 reversibly abolish rhythmic contractile activity in rabbit arteries. J Physiol 508:561–573
Cohen RA (2005) The endothelium-derived hyperpolarizing factor puzzle: a mechanism without a mediator? Circulation 111(6):724–727
Domenighetti AA, Beny JL, Chabaud F, Frieden MJ (1998) An intercellular regenerative calcium wave in porcine coronary artery endothelial cells in primary culture. Physiol 513:103–116
Drummond GR, Selemidis S, Cocks TM (2000) Apamin-sensitive, non-nitric oxide (NO) endothelium-dependent relaxations to bradykinin in the bovine isolated coronary artery: no role for cytochrome P450 and K+. Br J Pharmacol 129:811–819
Edwards G, Dora KA, Gardener MJ, Garland CJ, Weston AH (1998) K+ is an endothelium-derived hyperpolarizing factor in rat arteries. Nature 396:269–271
Emerson GG, Segal SS (2000) Endothelial cell pathway for conduction of hyperpolarization and vasodilation along hamster feed artery. Circ Res 86:94–100
Feletou M, Vanhoutte PM (2006) Endothelium-derived hyperpolarizing factor: where are we now? Anterioscler Thromb Vasc Biol 26:1215–1225
Fisslthaler B, Popp R, Kiss L, Potente M, Harder DR, Fleming I, Busse R (1999) Cytochrome P450 2C is an EDHF synthase in coronary arteries. Nature 401:493–497
Gauthier KM, Deeter C, Krishna UM, Reddy YK, Bondlela M, Falck JR, Campbell WB (2002) 14,15-Epoxyeicosa-5 (Z)-enoic acid: a selective epoxyeicosatrienoic acid antagonist that inhibits endothelium-dependent hyperpolarization and relaxation in coronary arteries. Circ Res 90:1028–1036
Griffith TM (2004) Endothelium-dependent smooth muscle hyperpolarization: do gap junctions provide a unifying hypothesis? Br J Pharmacol 141:881–903
Griffith TM, Chaytor AT, Taylor HJ, Giddings BD, Edwards DH (2002) cAMP facilitates EDHF-type relaxations in conduit arteries by enhancing electrotonic conduction via gap junctions. Proc Natl Acad Sci USA 99:6392–6397
Haas TL, Duling BR (1997) Morphology favors an endothelial cell pathway for longitudinal conduction within arterioles. Microvasc Res 53:113–120
Hill CE, Hickey H, Sandow SL (2000) Role of gap junctions in acetylcholine-induced vasodilation of proximal and distal arteries of the rat mesentery. J Auton Nerv Sys 81:122–127
Matoba T, Shimokawa H, Nakashima M, Hirakawa Y, Mukai Y, Hirano K, Kanaide H, Takeshita A (2000) Hydrogen peroxide is an endothelium-derived hyperpolarizing factor in mice. J Clin Invest 106:1521–1530
Pacicca C, Schaad O, Beny JL (1996) Electrotonic propagation of kinin-induced, endothelium-dependent hyperpolarization in pig coronary smooth muscle. J Vasc Res 33:380–385
Quignard J-F, Feletou M, Thollon C, Vilaine JP, Duhault J, Vanhoutte PM (1999) Potassium ions and endothelium-derived hyperpolarizing factor in guinea-pig carotid and porcine coronary arteries. Br J Pharmacol 127:27–34
Segal SS (1994) Cell-to-cell communication coordinates blood flow control. Hypertension 23(Part 2):1113–1120
Segal SS (2000) Integration of blood flow control to skeletal muscle: key role of feed arteries. Acta Physiol Scand 168:511–518
Segal SS (2005) Regulation of blood flow in the microcirculation. Microcirculation 12:33–45
Segal SS, Duling BR (1995) Flow control among microvessels coordinated by intercellular conduction. Science 234:868–870
Segal SS, Jacobs TL (2001) Role for endothelial cell conduction in ascending vasodilatation and exercise hyperaemia in hamster skeletal muscle. J Physiol 536:937–946
Segal SS, Welsh DG, Kurjiaka DT (1999) Spread of vasodilatation and vasoconstriction along feed arteries and arterioles of hamster skeletal muscle. J Physiol 516:283–291
Thollon C, Bidouard JP, Cambarrat C, Delescluse I, Villeneuve N, Vanhoutte PM, Vilaine JP (1999) Alteration of endothelium-dependent hyperpolarizations in porcine coronary arteries with regenerated endothelium. Circ Res 84:371–377
Xia J, Duling BR (1995) Electromechanical coupling and the conducted vasomotor response. Am J Physiol 269:H2022–H2030
Acknowledgements
This work was supported by grants from the National Health and Medical Research Council (NHMRC) of Australia. SS is supported by a NHMRC Peter Doherty Research Fellowship, whereas NHMRC provide support for TC.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Selemidis, S., Cocks, T. Smooth muscle mediates circumferential conduction of hyperpolarization and relaxation to focal endothelial cell activation in large coronary arteries. Naunyn-Schmied Arch Pharmacol 375, 85–94 (2007). https://doi.org/10.1007/s00210-007-0149-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-007-0149-7