Abstract
The aim of this study was to characterise the types of interactions between gabapentin (GBP), tiagabine (TGB) and three second-generation antiepileptic drugs (AEDs) with different mechanisms of action (felbamate [FBM], loreclezole [LCZ], and oxcarbazepine [OXC]) by isobolographic analysis. Anticonvulsant and acute neurotoxic adverse effect profiles of combinations of GBP and TGB with other AEDs at fixed ratios of 1:3, 1:1 and 3:1 were investigated in pentylenetetrazole (PTZ)-induced seizures and the chimney test (as a measure of motor impairment) in mice so as to identify optimal combinations. Protective indices (PIs) and benefit indices (BIs) were calculated for each combination in order to properly classify the investigated interactions. Isobolographic analysis revealed that only the combination of GBP with OXC at the fixed ratio of 1:1 exerted supra-additive (synergistic) interaction (P<0.05) against PTZ-induced seizures. The other combinations tested between GBP and OXC (1:3 and 3:1), as well as all combinations of GBP with FBM or LCZ (1:3, 1:1 and 3:1) were additive in the PTZ test. Similarly, all combinations of TGB with FBM LCZ, and OXC (at the fixed ratios of 1:3, 1:1 and 3:1) were associated with additive interactions against PTZ-induced seizures in mice. In the chimney test, the isobolographic analysis revealed that the combinations of GBP and OXC (at the fixed ratios of 1:3 and 1:1), GBP and LCZ (at 1:1), as well as TGB and OXC (at 1:3 and 1:1) were sub-additive (antagonistic; P<0.05 and P<0.01). In contrast, only one combination tested (TGB and LCZ at the fixed ratio of 1:1) was supra-additive (synergistic; P<0.05) in the chimney test, whereas the other combinations of GBP and TGB with OXC, FBM, and LCZ displayed barely additivity. Based upon the current preclinical data, GBP and OXC appear to be a particularly favourable combination. Also, the combinations of GBP with FBM, GBP with LCZ, and TGB with OXC are beneficial. In contrast, during the combining of TGB with FBM, or TGB with LCZ, the utmost caution is advised because of their unfavourable profiles in this preclinical study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite advanced knowledge of the pathophysiological processes involved in seizure initiation, amplification and propagation in the brain, as well as the introduction of several novel (second- and third-generation) antiepileptic drugs (AEDs) into the therapy of epilepsy, there are still ∼30% of patients unsuccessfully medicated with currently available AEDs in monotherapy (Kwan and Brodie 2000a, 2000b). Refractory epilepsy in ∼30% of sufferers is still a significant clinical problem and a challenging issue for clinicians and researchers. Once the drug of choice has failed, the primary concern is to find a highly efficacious combination of two or more AEDs in an attempt to enhance seizure control (Arroyo et al. 2002). Generally, the addition of a second or a third AED may provide enhanced seizure control in ∼14% of these patients (Kwan and Brodie 2000a, 2000b). Because of the ethical and methodological difficulties during the evaluation of AED combinations in the clinical setting, preclinical studies in animals can provide invaluable information allowing the preselection of useful AED combinations. The aim of such studies is to identify AED combinations whose anticonvulsant effects offer optimal protection against seizures and, simultaneously, are devoid of any serious neurotoxic side effects (Löscher and Wauquier 1996).
From a pharmacological viewpoint, a combination of two or more drugs may exert supra-additivity (synergy), additivity or sub-additivity (antagonism). Synergy between AEDs is observed when the final antiseizure effect of the AED mixture is stronger than expected, based on the sum of individual anticonvulsant effects of the component drugs. Additivity is present if the anticonvulsant effect of the drug mixture is the sum of the partial protective effects of individual component AEDs. Antagonism between AEDs is observed when the experimentally-derived protective effect of the drug mixture is less than the expected effect resulting from the component AEDs (Berenbaum 1989; Greco et al. 1995; Perucca 1995). Undoubtedly, the AED combinations exerting synergy with respect to seizure control and/or antagonism in terms of acute neurotoxic adverse effects possess great clinical relevance (Perucca 1995).
Generally, no theoretical presumptions, rules and guidelines exist that would allow preselection of synergistic interactions between AEDs as to the seizure suppression and/or antagonistic interactions with respect to acute neurotoxic adverse effects. The combining of two AEDs with similar mechanisms of action, in experimental conditions, may result either in sub-additivity (antagonism—for the combinations of oxcarbazepine [OXC] with lamotrigine or phenytoin; Luszczki et al. 2003a; Luszczki and Czuczwar 2004b) or in additivity (for the combinations of OXC with carbamazepine, Luszczki et al. 2003a). Likewise, the AEDs with diverse complementary mechanisms of action may exert either supra-additive (for the combinations of topiramate with OXC and felbamate [FBM], Luszczki and Czuczwar 2004b, as well as the combination of tiagabine [TGB] with gabapentin [GBP], Luszczki and Czuczwar 2004a) or sub-additive interactions (for the combination of vigabatrin [VGB] with carbamazepine; unpublished data). Thus, only experimental evaluation of AED combinations in preclinical studies on animals may provide reliable and convincing evidence of advantageous interactions between AEDs, which could be beneficial in patients with refractory epilepsy.
On the other hand, there is no consensus, as yet, whether to combine the AEDs affecting the same neurotransmitter system and reach a stronger therapeutic effect or choose the AEDs influencing diverse neurotransmitter systems for rational polytherapy (Deckers et al. 2000). To date, few experimental and clinical data exist reporting the combined treatment with AEDs that selectively activates the GABA-ergic inhibitory system within CNS, despite GABA being a well-known endogenous inhibitory agent that potently reduces seizure activity in the brain (Meldrum 1995; Treiman 2001; Olsen and Avoli 1997). It has been found experimentally that some combinations of two drugs, influencing exclusively the GABA-ergic neurotransmitter system (through diverse mechanisms), may result in synergistic interactions with respect to seizure suppression. Among them, the synergistic combinations of TGB with valproate (VPA), GBP or VGB, as well as the combinations of GBP with VPA and VGB are of importance for further clinical setting (Leach and Brodie 1994; Stringer and Aribi 2002; Kohling et al. 2002; Luszczki et al. 2003c; Luszczki and Czuczwar 2004a).
The objective of this study was to characterise the pharmacological profiles of interactions among TGB, GBP and some other second-generation AEDs (FBM, loreclezole [LCZ], and OXC) with respect to their anticonvulsant activities against pentylenetetrazole (PTZ)-induced seizures in mice. As for the PTZ test in rodents, the seizures induced by PTZ are thought to be a model of myoclonic seizures in humans (Löscher and Schmidt 1988; Löscher et al. 1991). Additionally, the acute neurotoxic adverse effect profiles of the different AED combinations were investigated in relation to motor impairment in the chimney test. Pharmacological characterisation of interactions in both PTZ and chimney tests was performed by using isobolographic analysis for three various fixed drug–dose ratio combinations of 1:3, 1:1 and 3:1, so that a ranking in relation to advantageous combination could be ascertained using paradigms of protective indices (PI) and benefit indices (BI). To date, isobolography is considered as the optimal method that allows the classification of AED interactions in experimental models of epilepsy as follows: additive, supra-additive, sub-additive, indifferent or infra-additive (Berenbaum 1989; Tallarida 2000; Greco et al. 1995).
Materials and methods
Animal and experimental conditions
All experiments were performed on adult male Swiss mice weighing 22–26 g. The mice were kept in colony cages with free access to food and tap water ad libitum, under standardised housing conditions (12 h of a light–dark cycle, temperature was 21±1°C). After 7 days of adaptation to laboratory conditions, the animals were randomly assigned to experimental groups consisting of eight mice. Each mouse participated in only one experiment. All tests were performed between 9.00 a.m. and 3.00 p.m. Procedures involving animals and their care were conducted in accordance with current European Community and Polish legislation on animal experimentation. Additionally, all efforts were made to minimise animal suffering and to use only the number of animals necessary to produce reliable scientific data. The experimental protocols and procedures described in this manuscript were approved by the Local Ethics Committee at the Medical University of Lublin and complied with the European Communities Council Directive of 24 November 1986 (86/609/EEC)—(License no: 425/2003/451/03).
Drugs
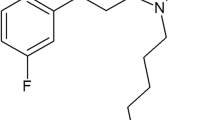
The following AEDs were used in this study: TGB (Gabitril; Sanofi Winthrop, Gentilly, France), GBP (Neurontin; Parke-Davis, Freiburg, Germany), FBM (Taloxa; Schering Plough, Levallois Perret, France), LCZ (Janssen Research Foundation, Beerse, Belgium) and OXC (Trileptal; Novartis Pharma AG, Basel, Switzerland). All drugs were suspended in a 1% solution of Tween 80 (Sigma, St. Louis, MO, USA) in saline and administered by intraperitoneal (i.p.) injection in a volume of 0.005 ml g−1 body weight. Fresh drug solutions were prepared ex tempore on each day of experimentation and administered as follows: TGB—15 min; OXC—30 min; GBP, LCZ and FBM—60 min before PTZ-induced seizures and motor coordination evaluation. These pretreatment times were chosen based upon information about their biological activity from the literature and our previous studies (Borowicz et al. 2002; Luszczki et al. 2003d, 2005).
Pentylenetetrazole (Sigma, St. Louis, MO, USA) was dissolved in distilled water and administered subcutaneously (s.c.) into a loose fold of skin in the midline of the neck with a volume of 0.005 ml g−1 body weight.
Pentylenetetrazole-induced convulsions
Clonic convulsions were induced in mice by the s.c. administration of PTZ at doses that ranged between 70 and 120 mg kg−1. Following PTZ administration, mice were placed separately into transparent Plexiglas cages (25×15×10 cm) and observed for 30 min for the occurrence of clonic seizures. To classify the seizure activity in mice we used a scale for clonic seizures adapted from Löscher et al. (1991). This scale comprises five stages:
-
1.
One or more generalised myoclonic twitches of the whole body
-
2.
Repeated clonic seizures of fore- and hindlimbs without loss of righting reflexes
-
3.
Generalised clonic seizures lasting for over 3 s with loss of righting reflexes, whereby the animals fall onto their side during the generalised clonus
-
4.
Loss of righting reflexes followed by tonic forelimb seizure
-
5.
Loss of righting reflexes with tonic fore- and hindlimb seizure
In our study, the first generalised clonic seizures accompanied by loss of righting reflexes (stage 3) were used as the endpoint. The number of animals convulsing out of the total number of mice tested was noted for each treatment regimen. The convulsive action of PTZ was evaluated as the CD97 (convulsive dose 97, i.e., the dose of PTZ that produced clonic seizures in 97% of animals). In order to determine the CD97, four or five different doses of PTZ were administered to animals (eight mice per group). Subsequently, a dose–response relationship line was calculated from the percentage of mice convulsing according to the log probit method described by Litchfield and Wilcoxon (1949).
The anticonvulsant activities of GBP, TGB, FBM, LCZ and OXC against the clonic PTZ-induced seizures were determined after s.c. administration of PTZ at its CD97 (100 mg kg−1). The animals were administered with increasing doses of the AEDs, and the anticonvulsant activity of each drug was evaluated as the ED50 (median effective dose of an AED, protecting 50% of mice against clonic convulsions). At least four groups of animals were used to estimate each ED50 value calculated from the respective dose–response relationship line according to Litchfield and Wilcoxon (1949). Similarly, the anticonvulsant activity of mixtures of GBP or TGB with FBM, LCZ and OXC was evaluated and expressed as ED50 mix, corresponding to the dose of a two-drug mixture required to protect 50% of animals tested for PTZ-induced clonic convulsions. This experimental procedure was described in more detail in our earlier study (Luszczki and Czuczwar 2004a).
Chimney test
The acute neurotoxic adverse effects of newer AEDs (GBP, TGB, OXC, FBM and LCZ) on motor performance impairment were quantified with the chimney test of Boissier et al. (1960). In this test, animals had to climb backwards up a plastic tube (3 cm inner diameter, 25 cm in length), and motor impairment was indicated by the inability of the animals to do so within 60 s. The acute neurotoxic (adverse) effects of AEDs alone were expressed as their median toxic doses (TD50 in mg kg−1), representing the doses at which the respective AEDs impaired motor coordination in 50% of the tested animals. To evaluate each TD50 value, at least four groups of animals (each group consisted of eight mice) injected with various doses of the drugs were challenged with the chimney test. A dose–response relationship line was calculated on the basis of the percentage of mice showing motor deficits by means of the log-probit method according to Litchfield and Wilcoxon (1949). Similarly, the combinations of GBP or TGB with AEDs were challenged with the chimney test in order to determine TD50 mix values, corresponding to the doses of mixtures of AEDs necessary to produce motor impairment in 50% of animals tested.
Isobolographic analysis of interactions
It is widely accepted that isobolography allows the determination of equieffective doses of AEDs and the classification of observed interactions as: supra-additive (synergistic), sub-additive (antagonistic), indifferent or additive (Berenbaum 1989; Greco et al. 1995; Tallarida 2000). Interactions between GBP or TGB and FBM, LCZ and OXC against PTZ-induced seizures and in the chimney test were analysed according to the methodology previously detailed in our earlier studies, where the precise descriptions of theoretical background with the respective equations showing how to undertake isobolographic calculations have been presented (Luszczki et al. 2003a, 2003b; Luszczki and Czuczwar 2003a, 2004a).
Briefly, with isobolographic analysis, both purely additive ED50 add (±SE) and TD50 add (±SE) values for mixtures of the examined AEDs at three fixed drug–dose ratio combinations (1:3, 1:1 and 3:1) were calculated. The ED50 add represents a total additive dose of the drugs in the mixture, theoretically providing a 50% protection against PTZ-induced seizures, whereas the TD50 add corresponds to a total dose of the drugs in the mixture, which theoretically impairs motor performance in 50% of animals challenged with the chimney test. Subsequently, using the log-probit method we determined the ED50 mix (±SE) and TD50 mix (±SE) values for the corresponding fixed ratio AED combinations. The ED50 mix is an experimentally-derived total dose of a mixture of two component drugs sufficient for 50% protective effect against PTZ-induced seizures. Analogously, the TD50 mix is an experimentally determined total dose of a mixture of two drugs sufficient for 50% impairment of motor coordination in the chimney test in mice. Statistical comparison of the experimentally-derived ED50 mix or TD50 mix values with their corresponding theoretically additive ED50 add or TD50 add values was performed by the use of the unpaired Student’s t test, according to Porreca et al. (1990) and Tallarida (2000). Finally, to visualise the interactions between AEDs, the experimentally denoted ED50 mix and TD50 mix values were plotted graphically into the Cartesian plot system as isobolograms.
Moreover, in this study, the protective index (PI) for each AED was calculated by dividing a given TD50 value, evaluated in the chimney test, by the respective ED50 value determined in the PTZ test. The PI is considered an index of the margin of safety and tolerability between anticonvulsant doses and doses of AEDs exerting acute adverse effects (e.g., sedation, ataxia, impairment of motor coordination or other neurotoxic manifestations) in preclinical studies (Löscher and Nolting 1991). Subsequently, the isobolographic parameter benefit index (BI) was calculated for all combinations examined as a quotient of PI mix and PI add of respective fixed ratio combinations. PImix is experimentally determined from the corresponding TD50 mix and ED50 mix values, whereas PIadd is theoretically calculated from the equation of additivity for the PTZ and chimney tests as a ratio of TD50 add and ED50 add values. The BI provides the rationale for combining the respective AEDs in clinical practice, if its value greatly exceeds the value of 1.3, whereas BI lower than 0.7 indicates unfavourable combinations of AEDs (Luszczki et al. 2003a, 2003b).
Statistical evaluation of data
The ED50s and TD50s with their 95% confidence limits were calculated by computer log-probit analysis (Litchfield and Wilcoxon 1949). The 95% confidence limits were transformed to standard errors (SEs) as described previously (Luszczki et al. 2003a, 2003b). Statistical evaluation of the isobolographic interactions was performed by the use of the Student’s t test to detect the differences between experimental (ED50 mix or TD50 mix) and theoretical additive (ED50 add or TD50 add) values, according to Porreca et al. (1990) and Tallarida (2000).
Results
Anticonvulsant and neurotoxic profile of AEDs administered separately in mice
All five AEDs (FBM, GBP, LCZ, OXC and TGB) administered alone exhibited a clear-cut anticonvulsant activity against clonic PTZ-induced seizures in mice. The ED50 values for AEDs are presented in Table 1. Similarly, in the chimney test, it was possible to determine TD50 values for all the AEDs (Table 1). Simultaneous evaluation of TD50 and ED50 values for all AEDs allowed the determination of their PIs, describing the safety and tolerability profile of AEDs administered singly (Table 1). The highest PI was associated with TGB (12.67), whereas OXC had the lowest value (2.51). LCZ, FBM and GBP had PIs that ranged between 4.59 and 9.98 (Table 1).
Isobolographic assessment of interactions between GBP, TGB and FBM, LCZ and OXC against the clonic PTZ-induced seizures
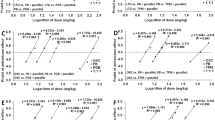
Gabapentin co-administered with OXC at the fixed ratio of 1:1 exerted a supra-additive (synergistic) interaction (at P<0.05; Fig. 1a; Table 2). In contrast, in the fixed ratios of 1:3 and 3:1 GBP and OXC in combination showed additivity in isobolography, although a tendency towards supra-additivity was observed (Fig. 1a; Table 2). All fixed ratio combinations of GBP with FBM or LCZ examined were additive in the PTZ test (Fig. 1b,c; Table 2). The difference between the observed and the theoretical ED50 values was not statistically significant, displaying only a tendency towards supra-additivity (Fig. 1b,c).
Isobolograms illustrating interactions between gabapentin and oxcarbazepine, felbamate and loreclezole in the pentylenetetrazole (PTZ) test in mice. The median effective dose (ED50) for gabapentin (GBP) is plotted graphically on the X-axis, whereas the ED50 of the AEDs examined (oxcarbazepine [OXC], felbamate [FBM] or loreclezole [LCZ]) is placed on the Y-axis (a–c). The solid lines on the X and Y axes represent the 95% confidence limits (CLs) for the AEDs administered alone. The straight line connecting these two ED50 values on each graph represents the theoretical line of additivity for a continuum of different fixed dose ratios, whereas the dashed lines represent on each isobologram the theoretical additive 95% CLs of the ED50 add values. The open circles depict the experimentally-derived ED50 mix values (with 95% CLs as the error bars) for total dose expressed as the proportion of GBP and an AED that produced a 50% anticonvulsant effect. a Interactions between GBP and OXC. The experimental ED50 mix of the mixture of GBP+OXC for the fixed ratio of 1:1 is significantly below the theoretical line of additivity, indicating supra-additive interaction at *P<0.05. The ED50 mix values for the fixed ratios of 1:3 and 3:1 are close to the line of additivity and thus display a tendency towards supra-additivity. b Interactions between GBP and FBM. The experimental ED50 mix values of the mixture of GBP+FBM, for the fixed ratios of 3:1, 1:1 and 3:1 are close to the theoretical line of additivity, indicating additive interaction and a tendency towards supra-additivity in the PTZ test. c Interactions between GBP and LCZ. The experimental ED50 mix values are near to the line of additivity and thus display almost pure additive interactions
In the cases of the combinations of TGB with LCZ and OXC, it was found that all the fixed ratio combinations tested (1:3, 1:1 and 3:1) showed additivity in the PTZ test, although a tendency towards supra-additivity was observed (Fig. 2a, c; Table 3). Moreover, the combination between TGB and FBM (at all fixed ratios examined) exerted additivity in the PTZ test; however, the interactions displayed a tendency towards sub-additivity (Fig. 2b; Table 3).
Isobolograms showing interactions between tiagabine (TGB) and OXC, FBM and LCZ against PTZ-induced seizures in mice. The median effective dose (ED50) for TGB is plotted graphically on the X-axis, whereas the ED50 of the AEDs examined (OXC, FBM or LCZ) is placed on the Y-axis (a–c). For more details see the legend to Fig. 1. a Interactions between TGB and OXC. The experimental ED50 mix values of the mixture of GBP+OXC for the fixed ratios of 3:1, 1:1 and 3:1 are close to the theoretical line of additivity, indicating additive interactions in the PTZ test, although a tendency towards supra-additivity is observed. b Interactions between TGB and FBM. The experimental ED50 mix values of the mixture of GBP+FBM, for all fixed ratios of 3:1, 1:1 and 3:1 are above the line of additivity, although they did not statistically differ from the ED50 add values. A tendency towards sub-additivity (antagonism) was displayed for all fixed ratios investigated in the PTZ test. c Interactions between TGB and LCZ. The experimental ED50 mix values are near to the line of additivity, displaying additive interactions with a tendency towards supra-additivity in the PTZ test
Isobolographic analysis of interactions among GBP, TGB and FBM, LCZ and OXC in the chimney test
It was observed that GBP combined with OXC at the fixed ratios of 1:3 and 1:1 exerted sub-additive (antagonistic) interactions in the chimney test (at P<0.05; Fig. 3a; Table 4). Similarly, the interaction between GBP and LCZ at the fixed ratio of 1:1 was sub-additive (antagonistic) in the chimney test (at P<0.05; Fig. 3c; Table 4). The remaining combinations of GBP and OXC at the fixed ratio of 3:1, as well as GBP and LCZ at the fixed ratios of 1:3 and 3:1 displayed additivity in the chimney test, although a tendency towards sub-additivity was observed (Fig. 3a, c). Moreover, all combinations of GBP with FBM (at the fixed ratios of 1:3, 1:1 and 3:1) were additive, showing a tendency to sub-additivity (Fig. 3b).
Isobolograms illustrating interactions among GBP and OXC, FBM and LCZ in the chimney test in mice. The median toxic dose (TD50) for GBP is plotted graphically on the X-axis, whereas the TD50 of the AED examined (OXC, FBM or LCZ) is placed on the Y-axis (a–c). For more details see the legend to Fig. 1. a Interactions between GBP and OXC. The experimental TD50 mix values of the mixture of GBP+OXC for the fixed ratios of 1:3 and 1:1 are significantly above the theoretical line of additivity, indicating sub-additive (antagonistic) interactions at *P<0.05. The TD50 mix for the fixed ratio of 3:1 is close to the line of additivity and thus displays a tendency towards sub-additivity. b Interactions between GBP and FBM. The experimental TD50 mix values of the mixture of GBP+FBM, for the fixed ratios of 3:1, 1:1 and 3:1 are close to the theoretical line of additivity, indicating additive interactions in the chimney test, although a tendency towards sub-additivity is observed. c Interactions between GBP and LCZ. The experimental TD50 mix of the of GBP+LCZ for the fixed ratio of 1:1 is significantly above the theoretical line of additivity, indicating sub-additive interaction at *P<0.05. The other TD50 mix values for the fixed ratios of 1:3 and 3:1 are close to the line of additivity and thus display a tendency towards sub-additivity
The combinations of TGB and OXC at the fixed ratios of 1:3 and 1:1 exerted sub-additive interactions in the chimney test (at P<0.05 and P<0.01; Fig. 4a; Table 5). Only, the combination of TGB with OXC at the fixed ratio of 3:1 was additive, displaying a tendency towards sub-additivity (Fig. 4a). In contrast, the co-administration of TGB with LCZ at the fixed ratio of 1:1 resulted in a supra-additive (synergistic) interaction in the chimney test (P<0.05; Fig. 4c; Table 5). The remaining combinations of TGB with LCZ (at the fixed ratios of 1:3 and 3:1) were additive, although a tendency towards synergy was observed for these combinations (Fig. 4c). The combinations of TGB and FBM examined in the present study (at the fixed ratios of 1:3, 1:1 and 3:1) were associated with additivity in the chimney test, although the tendency towards sub-additivity was observed for all combinations (Fig. 4b; Table 5).
Isobolograms showing interactions between TGB and OXC, FBM and LCZ in the chimney test in mice. The median toxic dose (TD50) for TGB is plotted graphically on the X-axis, whereas the TD50 of the AED examined (OXC, FBM or LCZ) is placed on the Y-axis (a–c). For more details see the legend to Fig. 1. a Interactions between TGB and OXC. The experimental TD50 mix values of the mixture of TBP+OXC for the fixed ratios of 1:3 and 1:1 are significantly above the theoretical line of additivity, indicating sub-additive (antagonistic) interactions at *P<0.05 and **P<0.01 respectively. Only the TD50 mix for the fixed ratio of 3:1 is close to the line of additivity and thus displays a tendency towards sub-additivity. b Interactions between TGB and FBM. The experimental TD50 mix values of the mixture of TGB+FBM, for all fixed ratios of 3:1, 1:1 and 3:1, are above the line of additivity, although they did not statistically differ from the TD50 add values. The tendency towards sub-additivity (antagonism) was displayed for all fixed ratios investigated in the chimney test. c Interactions between TGB and LCZ. The experimental TD50 mix of the mixture of TGB+LCZ for the fixed ratio of 1:1 is significantly below the theoretical line of additivity, indicating supra-additive (synergistic) interaction at *P<0.05. The TD50 mix values for the fixed ratios of 1:3 and 3:1 are close to the line of additivity and thus display a tendency towards supra-additivity
Isobolographic parameter evaluation
In the present study, 10 out of the 18 fixed ratio combinations investigated could be considered to be favourable, having BI values higher than the border value of 1.3. The highest BI value for the combination of GBP and OXC was associated with the fixed ratio combination of 1:1 and was 3.31, whereas the BI values for GBP with OXC at the fixed ratios of 3:1 and 1:3 were 2.16 and 2.08 respectively (Table 6). In these cases, the supra-additivity (synergy) in the PTZ test associated with sub-additivity (antagonism) in terms of acute neurotoxic effects in the chimney test fulfilled a criterion of the most advantageous AED combination. Similarly, the combinations of GBP with LCZ or FBM may also be considered advantageous since their BIs were higher than the border value of 1.3 (Table 6).
The combination of TGB with OXC at all fixed ratios may also be considered as advantageous because their BI values ranged between 1.32 and 1.5 (Table 6), due to the existence of a tendency towards supra-additivity against PTZ-induced seizures and sub-additivity in the chimney test. In contrast, in the present study, the combinations of TGB with FBM were unfavourable, as their BI values were near to or lower than 0.7 (Table 6). Furthermore, the BI values calculated for the combination of TGB with LCZ ranged between 0.93 and 1.13, indicating that these combinations were at best neutral (Table 6).
Discussion
The results presented herein indicate that only one combination tested between GBP and OXC at the fixed ratio of 1:1 exerted a supra-additive (synergistic) interaction in the PTZ test. The remaining fixed ratio combinations of GBP and OXC (i.e., 1:3 and 3:1) and all fixed ratios for the combinations of GBP with LCZ or FBM, as well as the combinations of TGB with FBM, LCZ or OXC, had merely additive effects on PTZ-induced seizures in mice. In the chimney test, evaluating the acute neurotoxic adverse effects, it was found that the combinations of GBP with OXC and LCZ, as well as the combinations of TGB with OXC, produced sub-additive (antagonistic) interactions. Only one combination of TGB and LCZ at the fixed ratio of 1:1 was supra-additive in the chimney test, whereas the other combinations tested were additive.
As already mentioned, from a preclinical point of view, the most favourable combination is that exerting supra-additivity with respect to seizure suppression and simultaneously sub-additivity in terms of neurotoxic adverse effects. Theoretically, such a combination provides full antiseizure protection and is devoid of acute neurotoxic side effects. Based on the classification of interactions in preclinical study, the combination of GBP with OXC, showing synergy in seizure suppression and antagonism with respect to neurotoxic adverse effects, may be considered to be the best AED combination (Luszczki et al. 2003b). In contrast, the combination of TGB with LCZ that produced synergy in the chimney test and additivity in the PTZ test was classified as unfavourable. The remaining combinations between GBP and FBM or LCZ, as well as those between TGB and OXC, were classified as neutral combinations, displaying additivity in both antiseizure and neurotoxic adverse effects (Luszczki et al. 2003b). It is worth noting that BI values provided us with more subtle information about the final pharmacological profile of AED combinations with regard to their antiseizure and acute neurotoxic effects. Based on BI values, the combinations of TGB with FBM were unfavourable, whereas those between TGB and LCZ were neutral from a preclinical point of view.
We can attempt to explain the observed synergy between GBP and OXC in the PTZ test on the basis of their molecular mechanisms of action. It is worth mentioning that the exact mechanisms of action of GBP are still unknown; however, several potential mechanisms may account for its anticonvulsant activity. Despite its chemical similarity to GABA, GBP inhibits Ca2+ voltage-gated channels through the interaction with the alpha2delta subunit (Gee et al. 1996). The drug activates glutamate decarboxylase (GAD) and weakly inhibits GABA transaminase (GABA-T)—contributing to the increment in GABA concentration, as well as activating glutamate dehydrogenase (GDH) and potently inhibiting branched-chain aminotransferase (BCAA-T)—decreasing glutamate concentration (Goldlust et al. 1995). GBP competes with the transport of branched-chain amino acids (L-leucine, L-valine, L-phenylalanine), and thus the drug affects cytosolic concentrations of endogenous amino acids in neurons (Taylor et al. 1998). Moreover, the drug increases the conductance of hyperpolarisation-activated cation currents (Ih) contributing to the protection of neurons against excessive synaptic or intrinsic activity, and stabilising the neuronal network within the hippocampus (Surges et al. 2003). More recently, it has been found that GBP selectively activates presynaptic GABAB heteroreceptors (but not GABAB autoreceptors) decreasing the release of neurotransmitters by reducing Ca2+ conductance in neurons of the CNS (Ng et al. 2001; Parker et al. 2004).
With regard to the mechanisms of action of OXC, compelling evidence indicates that the drug and its rapidly formed 10-monohydroxy derivative (MHD), at therapeutically relevant concentrations: reduce high-frequency repetitive firing of neurons by an action on voltage-dependent Na+ channels; decrease the frequency of penicillin-induced epileptiform spike discharges in neurons suggesting an effect on K+ currents; and inhibit high-voltage-activated N-type Ca2+ channels (Schmutz et al. 1994; Stefani et al. 1995). Considering the mechanisms of action of both AEDs, the synergistic interaction between GBP and OXC at the fixed ratio of 1:1 in the PTZ test seems to be closely related to Ca2+ channel blockade, mediated by both AEDs. Nevertheless, all the above-mentioned mechanisms of anticonvulsant activity of the two AEDs could contribute to their synergistic interaction against PTZ-induced seizures. A similar situation was also documented for the combination of GBP with OXC in maximal electroshock (MES)-induced seizures in mice. Indeed it has been found isobolographically that GBP synergistically potentiated the antiseizure effects of OXC on maximal electroconvulsions in mice (Luszczki et al. 2005).
Relatively recently, it has been found that GBP interacted synergistically with TGB and VGB in the PTZ-test in mice (Luszczki and Czuczwar 2003b, 2004a). Noticeably, TGB is a second-generation AED, acting as a potent GABA re-uptake inhibitor into neurons and glia, which by blocking the GABA transporter 1 (GAT-1) in mice increases GABA concentration into the synaptic clefts of neurons and prolongs the duration of GABA-related inhibitory synaptic potentials (Nielsen et al. 1991; Czuczwar and Patsalos 2001). VGB is also a second-generation AED, whose anticonvulsant action is related with irreversible inhibition of GABA-transaminase, the enzyme responsible for the metabolic degradation of GABA in neurons and glia (Brodie and Schachter 2001). It should be stressed that the anticonvulsant activities of VGB, TGB and GBP are closely related with the increment in GABA content within the brain and thus, the enhancement of GABA-ergic inhibitory neurotransmission (Czuczwar and Patsalos 2001). Surprisingly, in the present study, GBP interacted synergistically only with OXC, but not with LCZ—an AED that exerts its modulatory effect on two separate allosteric regulatory sites on GABAA receptors (Wingrove et al. 1994; Wafford et al. 1994). Neurochemical studies have revealed that LCZ potentiates GABAA receptor-mediated Cl− currents through a site present on the β2 and β3 (but not β1) subunits of GABAA receptors (Wafford et al. 1994). The drug also acts in an inhibitory manner, increasing the rate and degree of apparent desensitisation of GABAA receptor-mediated currents via a novel site independent on the benzodiazepine and picrotoxin binding sites (Donnelly and Macdonald 1996).
In case of FBM, electrophysiological and neurochemical studies have indicated that the drug interferes with voltage-gated Na+ channels, inhibiting the sustained repetitive neuronal firing, and thereby, preventing the seizure spread (White et al. 1992). Moreover, FBM indirectly antagonises N-methyl-D-aspartate (NMDA) by interfering with the binding of glycine to strychnine-insensitive glycine receptors, leading to a reduction of NMDA receptor-modulated cationic conductance (McCabe et al. 1993). The drug suppresses dose-dependently the seizures induced by kainate, alpha-amino-3-hydroxy-5-methylisoxazole-4-propionic acid (AMPA), quisqualate (De Sarro et al. 1994) and PTZ (Borowicz et al. 2004), as well as, it inhibits voltage-activated Ca2+ currents (Stefani et al. 1997). Previously, we have reported a supra-additive interaction between FBM and phenobarbital at the fixed-ratio of 1:3 in the PTZ-test in mice (Borowicz et al. 2004). Moreover, in the PTZ-test, a sub-additive interaction has been observed for the combination of FBM with valproate at the fixed-ratio of 3:1. The other combinations tested between FBM and phenobarbital or valproate, as well as, those between FBM and clonazepam or ethosuximide had an additive effect on PTZ-induced seizures in mice (Borowicz et al. 2004). In this study, it was found that all combinations of FBM and GBP or TGB had an additive effect in the PTZ test in mice.
Surprisingly, TGB did not interact synergistically with LCZ, FBM and OXC. In our previous studies, it was found that TGB synergistically enhanced the anticonvulsant action of GBP and VGB in the PTZ test in mice (Luszczki et al. 2003d; Luszczki and Czuczwar 2003b, 2004a). Moreover, one clinical report exists that documented that the combination of TGB with VGB considerably improved the control of seizure attacks in refractory epileptic patients (Leach and Brodie 1994). Additionally, it has been experimentally confirmed that low doses of VGB co-administered with TGB significantly reduced GABA uptake from synaptic clefts (Leach et al. 1996) resulting in an increase in GABA concentration in the whole mouse neocortex (Leach et al. 1997). Likewise, the drugs applied together (TGB and VGB) drastically and firmly inhibited the experimentally-induced epileptic potentials from hippocampal slices of guinea pigs (Kohling et al. 2002). Thus, the previously documented synergistic interactions for the combinations of TGB with GBP, TGB with VGB and GBP with VGB may suggest that the activation of various mechanisms within the same neurotransmitter system (GABA) may exert advantageous effects offering a significant reduction in seizure activity. In the light of this fact, it is surprising that neither GBP nor TGB interacted synergistically with LCZ, although all AEDs influence the GABA-ergic inhibitory neurotransmission system. Relatively recently, a similar situation was reported in an experimental study by Jonker et al. (2003), who found that the combination of midazolam (an allosteric modulator of the GABAA receptor) with TGB was additive in nature.
Another fact should be discussed here, since the supra-additive interaction between GBP and OXC in the PTZ test is similar in nature to the supra-additivity reported previously in the MES test in mice (Luszczki et al. 2005). Moreover, the additive interactions between TGB and FBM observed in this study confirmed our previous findings, also demonstrating the additivity between these AEDs in the MES test in mice (Luszczki et al. 2003c). Additionally, it has been documented that the combination of TGB with GBP exerted supra-additive interactions in both MES and PTZ tests (Luszczki and Czuczwar 2004a). Thus, considering the isobolographic characteristics of the above-mentioned combinations and their identical interactions in both MES and PTZ tests, the existence of a good correlation between AED interactions and seizure models used in preclinical studies can be ascertained.
As mentioned above, the PTZ-induced seizures are considered to be an experimental animal model of myoclonic convulsions in man (Löscher and Schmidt 1988; Löscher et al. 1991). In the light of this fact, it should be stressed that TGB and GBP, although they protect animals against the clonic seizures induced by PTZ, the drugs are not only ineffective in suppressing myoclonic seizures in patients, but they may even contribute to the aggravation of absence seizures and/or the induction of non-convulsive status epilepticus in patients (Genton 2000; Schapel and Chadwick 1996; Mangano et al. 2003). It has also been found experimentally that TGB (administered i.p. at doses of 3 and 10 mg kg−1) enhanced both the number and mean duration of spike-and-wave discharges in WAG/Rij rats (an animal model of generalised non-convulsive absence epilepsy), indicating evidently that the drug aggravated absence seizures in rats (Coenen et al. 1995). The question arises whether the combinations of AEDs effective in the MES and/or PTZ tests would be also effective in other epileptic syndromes that have no representation in experimental animal models. For example, to date, there is no firmly established animal model reflecting the Lennox-Gastaut or West syndrome in children. Hence, it is questionable whether the combinations of two AEDs effective in the MES or PTZ tests would be effective in these syndromes. Since a close correlation exists between the results from the MES and PTZ tests in preclinical studies, it can be supposed that some AED combinations may also exert anticonvulsant properties in various epileptic syndromes in humans. Noticeably, there are no preclinical methods, except for isobolography, that allow the adequate examination and pre-selection of the anticonvulsant efficacy of AEDs in combinations.
Recently, numbers of various AEDs in combination with topiramate have been tested in two models of experimental epilepsy (in the MES and PTZ tests), even if they were virtually ineffective in one of these models (Sills et al. 2004). The authors have demonstrated that levetiracetam (50 and 250 mg kg−1), clobazam (1 and 5 mg kg−1) and lamotrigine (2.5 and 12.5 mg kg−1), although when administered singly did not suppress PTZ-induced seizures, when combined with topiramate (5, 25 and 125 mg kg−1), an AED that was also ineffective in the PTZ test, strongly inhibited PTZ-induced seizures in mice, indicating that the AED combinations may have a broader spectrum of antiseizure activity in preclinical study, producing entirely different anticonvulsant properties than the constituent AEDs when administered separately (Sills et al. 2004). With regard to clobazam, experimental evidence indicates that the drug (at a dose range of 1–7.5 mg kg−1) was fully effective in suppressing both minimal clonic seizures and generalised tonic–clonic convulsions induced by PTZ in rats at various developmental stages (18-, 25- and 90-day-old rats; Haugvicova et al. 1999). Hence, the observed difference between the anticonvulsant action of clobazam in the PTZ test in rats and its inactivity in the mouse model of PTZ-induced seizures requires explanation in further neuropharmacological studies.
Moreover, in the study by Sills et al. (2004), TGB (0.2, 1 and 5 mg kg−1), GBP (5, 25 and 125 mg kg−1) and VGB (10, 50 and 250 mg kg−1), the AEDs possessing a high inclination to aggravate myoclonic and absence seizures in patients, were tested in combination with topiramate (5, 25 and 125 mg kg−1), showing no significant effect on the clonic PTZ-induced seizures in mice. On the other hand, it is surprising that the authors have tested combinations of AEDs in the PTZ test that are never prescribed for patients with myoclonic and absence seizures, such as: phenytoin (2, 10 and 50 mg kg−1) and carbamazepine (2, 10 and 50 mg kg−1) with topiramate (5, 25 and 125 mg kg−1). Obviously, no changes in the latency to the clonic PTZ-induced seizures were found for the combinations of these AEDs in mice (Sills et al. 2004). Noticeably, Sills et al. (2004) set a precedent for studying and examining AEDs in the PTZ test in mice, even if the AEDs aggravate seizure in the clinical setting.
Generally, in isobolography, the observed interactions between the AEDs studied represent the final pharmacological effects of AED combinations in vivo, whose nature may be pharmacokinetic, pharmacodynamic or mixed. In this study, we evaluated the final effects of AED combinations against clonic PTZ-induced seizures as well as in the chimney test in mice. Since the isobolographically denoted interactions had barely additive effects on PTZ-induced seizures, except for the combination of GBP with OXC at the fixed ratio of 1:1, the AED combinations were not pharmacokinetically verified in this study. We are fully aware of the possibility of the existence of pharmacokinetic interactions among the AEDs studied in the biophase of experimental animals; however, in this study we determined the isobolographic characteristics of interactions without differentiating their pharmacokinetic or pharmacodynamic nature.
Conclusions
The aim of this study was to investigate the interactions among GBP, TGB and some other newer AEDs with different mechanisms of action to provide evidence of whether or not to combine AEDs with different or similar mechanisms of action. Moreover, this study served as a screening process to preselect favourable combinations with respect to both anticonvulsant and neurotoxic adverse effects in preclinical study. Based on the BI, which is a composite measure of the anticonvulsant effects in the PTZ test and of motor impairment in the chimney test, the combination of GBP and OXC appears to be particularly beneficial. Additionally, the combinations of GBP with LCZ or FBM, as well as TGB with OXC, are also advantageous using these test paradigms. In contrast, the combinations of TGB with FBM or LCZ were unfavourable from a preclinical point of view.
Abbreviations
- AED:
-
Antiepileptic drug
- BI:
-
Benefit index
- CNS:
-
Central nervous system
- ED50:
-
Median effective dose
- FBM:
-
Felbamate
- GABA:
-
γ-Aminobutyric acid
- GBP:
-
Gabapentin
- LCZ:
-
Loreclezole
- OXC:
-
Oxcarbazepine
- PI:
-
Protective (therapeutic) index
- PTZ:
-
Pentylenetetrazole
- TD50:
-
Median toxic dose
- TGB:
-
Tiagabine
- VGB:
-
Vigabatrin
References
Arroyo S, Brodie MJ, Avanzini G, Baumgartner C, Chiron C, Dulac O, French JA, Serratosa JM (2002) Is refractory epilepsy preventable? Epilepsia 43:437–444
Berenbaum MC (1989) What is synergy? Pharmacol Rev 41:93–141; erratum in (1990) Pharmacol Rev 41:422
Boissier JR, Tardy J, Diverres JC (1960) Une nouvelle méthode simple pour explorer l’action tranquilisante: le test de la cheminée. Med Exp (Basel) 3:81–84
Borowicz KK, Swiader M, Luszczki J, Czuczwar SJ (2002) Effect of gabapentin on the anticonvulsant activity of antiepileptic drugs against electroconvulsions in mice—an isobolographic analysis. Epilepsia 43:956–963
Borowicz KK, Luszczki JJ, Czuczwar SJ (2004) Isobolographic and subthreshold analysis of interactions among felbamate and four conventional antiepileptic drugs in pentylenetetrazole-induced seizures in mice. Epilepsia 45:1176–1183
Brodie MJ, Schachter SC (2001) Fast facts. Epilepsy, 2nd edn. Health Press, Oxford, p 82
Coenen AM, Blezer EH, van Luijtelaar EL (1995) Effects of the GABA-uptake inhibitor tiagabine on electroencephalogram, spike-wave discharges and behaviour of rats. Epilepsy Res 21:89–94
Czuczwar SJ, Patsalos NP (2001) The new generation of GABA enhancers. Potential in the treatment of epilepsy. CNS Drugs 15:339–350
Deckers CLP, Czuczwar SJ, Hekster YA, Keyser A, Kubova H, Meinardi H, Patsalos P, Renier WO, van Rijn CM (2000) Selection of antiepileptic drug polytherapy based on mechanism of action: the evidence reviewed. Epilepsia 41:1364–1374
De Sarro G, Ongini E, Bertorelli R, Aguglia U, De Sarro A (1994) Excitatory amino acid neurotransmission through both NMDA and non-NMDA receptors is involved in the anticonvulsant activity of felbamate in DBA/2 mice. Eur J Pharmacol 262:11–19
Donnelly JL, Macdonald RL (1996) Loreclezole enhances apparent desensitization of recombinant GABAA receptor currents. Neuropharmacology 35:1233–1241
Gee NS, Brown JP, Dissanayake VUK, Offord J, Thurlow R, Woodruff GN (1996) The novel anticonvulsant drug, gabapentin (neurontin), binds to the alpha2delta subunit of calcium channel. J Biol Chem 271:5768–5776
Genton P (2000) When antiepileptic drugs aggravate epilepsy. Brain Dev 22:75–80
Goldlust A, Su TZ, Welty DF, Taylor CP, Oxender DL (1995) Effects of anticonvulsant drug gabapentin on the enzymes in metabolic pathways of glutamate and GABA. Epilepsy Res 22:1–11
Greco WR, Bravo G, Parsons JC (1995) The search for synergy: a critical review from a response surface perspective. Pharmacol Rev 47:331–385
Haugvicova R, Kubova H, Mares P (1999) Antipentylenetetrazol action of clobazam in developing rats. Physiol Res 48:501–507
Jonker DM, Vermeij DA, Edelbroek PM, Voskuyl RA, Piotrovsky VK, Danhof M (2003) Pharmacodynamic analysis of the interaction between tiagabine and midazolam with an allosteric model that incorporates signal transduction. Epilepsia 44:329–338
Kohling R, Konig K, Lucke A, Mayer T, Wolf P, Speckmann EJ (2002) Pre- rather than co-application of vigabatrin increases the efficacy of tiagabine in hippocampal slices. Epilepsia 43:1455–1461
Kwan P, Brodie MJ (2000a) Early identification of refractory epilepsy. N Engl J Med 342:314–319
Kwan P, Brodie MJ (2000b) Epilepsy after the first drug fails: substitution or add-on? Seizure 9:464–468
Leach JP, Brodie MJ (1994) Synergism with GABAergic drugs in refractory epilepsy. Lancet 343:1650
Leach JP, Sills GJ, Majid A, Butler E, Carswell A, Thompson GG, Brodie MJ (1996) Effects of tiagabine and vigabatrin on GABA uptake into primary cultures of rat cortical astrocytes. Seizure 5:229–234
Leach JP, Sills GJ, Butler E, Forrest G, Thompson GG, Brodie MJ (1997) Neurochemical actions of gabapentin in mouse brain. Epilepsy Res 27:175–180
Litchfield JT, Wilcoxon F (1949) A simplified method of evaluating dose-effect experiments. J Pharmacol Exp Ther 96:99–113
Löscher W, Nolting B (1991) The role of technical, biological and pharmacological factors in the laboratory evaluation of anticonvulsant drugs. IV. Protective indices. Epilepsy Res 9:1–10
Löscher W, Schmidt D (1988) Which animal models should be used in the search for new antiepileptic drugs? A proposal based on experimental and clinical considerations. Epilepsy Res 2:145–181
Löscher W, Wauquier A (1996) Use of animal models in developing guiding principles for polypharmacy in epilepsy. Epilepsy Res Suppl 11:61–65
Löscher W, Honack D, Fassbender CP, Nolting B (1991) The role of technical, biological and pharmacological factors in the laboratory evaluation of anticonvulsant drugs. III. Pentylenetetrazole seizure models. Epilepsy Res 8:171–189
Luszczki JJ, Czuczwar SJ (2003a) Isobolographic and subthreshold methods in the detection of interactions between oxcarbazepine and conventional antiepileptics—a comparative study. Epilepsy Res 56:27–42
Luszczki JJ, Czuczwar SJ (2003b) Isobolographic assessment of interactions between tiagabine and some newer antiepileptic drugs in pentylenetetrazole-induced seizures in mice [abstract]. Pol J Pharmacol 55:500–501
Luszczki JJ, Czuczwar SJ (2004a) Isobolographic profile of interactions between tiagabine and gabapentin: a preclinical study. Naunyn Schmiedebergs Arch Pharmacol 369:434–446
Luszczki JJ, Czuczwar SJ (2004b) Preclinical profile of combinations of some second-generation antiepileptic drugs: an isobolographic analysis. Epilepsia 45:895–907
Luszczki JJ, Borowicz KK, Swiader M, Czuczwar SJ (2003a) Interactions between oxcarbazepine and conventional antiepileptic drugs in the maximal electroshock test in mice: an isobolographic analysis. Epilepsia 44:489–499
Luszczki JJ, Czuczwar M, Kis J, Krysa J, Pasztelan I, Swiader M, Czuczwar SJ (2003b) Interactions of lamotrigine with topiramate and first-generation antiepileptic drugs in the maximal electroshock test in mice: an isobolographic analysis. Epilepsia 44:1003–1013
Luszczki JJ, Swiader M, Czuczwar M, Kis J, Czuczwar SJ (2003c) Interactions of tiagabine with some antiepileptics in the maximal electroshock in mice. Pharmacol Biochem Behav 75:319–327
Luszczki JJ, Swiader M, Parada-Turska J, Czuczwar SJ (2003d) Tiagabine synergistically interacts with gabapentin in the electroconvulsive threshold test in mice. Neuropsychopharmacology 28:1817–1830
Luszczki JJ, Andres MM, Czuczwar SJ (2005) Synergistic interaction of gabapentin and oxcarbazepine in the mouse maximal electroshock seizure model—an isobolographic analysis. Eur J Pharmacol 515:54–61
Mangano S, Cusumano L, Fontana A (2003) Non-convulsive status epilepticus associated with tiagabine in a pediatric patient. Brain Dev 25:518–521
McCabe RT, Wasterlain CG, Kucharczyk N, Sofia RD, Vogel JR (1993) Evidence for anticonvulsant and neuroprotectant action of felbamate mediate by strychnine-insensitive glycine receptors. J Pharmacol Exp Ther 264:1248–1252
Meldrum B (1995) Epilepsy. Taking up GABA again. Nature 376:122–123
Ng GY, Bertrand S, Sullivan R, Ethier N, Wang J, Yergey J, Belley M, Trimble L, Bateman K, Alder L, Smith A, McKernan R, Metters K, O’Neill GP, Lacaille JC, Hebert TE (2001) Gamma-aminobutyric acid type B receptors with specific heterodimer composition and postsynaptic actions in hippocampal neurons are targets of anticonvulsant gabapentin action. Mol Pharmacol 59:144–152
Nielsen EB, Suzdak PD, Anderson KE, Knutsen LJ, Sonnewald U, Braestrup C (1991) Characterization of tiagabine (NO-328), a new potent and selective GABA uptake inhibitor. Eur J Pharmacol 196:257–266
Olsen RW, Avoli M (1997) GABA and epileptogenesis. Epilepsia 38:399–407
Parker DAS, Ong J, Marino V, Kerr DIB (2004) Gabapentin activates presynaptic GABAB heteroreceptors in rat cortical slices. Eur J Pharmacol 495:137–143
Perucca E (1995) Pharmacological principles as a basis for polytherapy. Acta Neurol Scand Suppl 162:31–34
Porreca F, Jiang Q, Tallarida RJ (1990) Modulation of morphine antinociception by peripheral [Leu5]enkephalin: a synergistic interaction. Eur J Pharmacol 179:463–468
Schapel G, Chadwick D (1996) Tiagabine and non-convulsive status epilepticus. Seizure 5:153–156
Schmutz M, Brugger F, Gentsch C, McLean MJ, Olpe HR (1994) Oxcarbazepine: preclinical anticonvulsant profile and putative mechanisms of action. Epilepsia 35 [Suppl 5]:S47–S50
Sills GJ, Butler E, Thompson GG, Brodie MJ (2004) Pharmacodynamic interaction studies with topiramate in the pentylenetetrazol and maximal electroshock seizure models. Seizure 13:287–295
Stefani A, Pisani A, De Murtas M, Mercuri NB, Marciani MG, Calabresi P (1995) Action of GP 47779, the active metabolite of oxcarbazepine, on the corticostriatal system. II. Modulation of high-voltage-activated calcium currents. Epilepsia 36:997–1002
Stefani A, Spadoni F, Bernardi G (1997) Voltage-activated calcium channels: targets of antiepileptic drug activity? Epilepsia 38:959–965
Stringer JL, Aribi AM (2002) Modulation of the in vivo effects of gabapentin by vigabatrin and SKF89976A. Epilepsy Res 52:129–137
Surges R, Freiman TM, Feuerstein TJ (2003) Gabapentin increases the hyperpolarization-activated cation current Ih in rat CA1 pyramidal cells. Epilepsia 44:150–156
Tallarida RJ (2000) Drug synergism and dose-effect data analysis. Chapman & Hall/CRC, Boca Raton, pp 247
Taylor CP, Gee NS, Su TZ, Kocsis JD, Welty DF, Brown JP, Dooley DJ, Boden P, Singh L (1998) A summary of mechanistic hypotheses of gabapentin pharmacology. Epilepsy Res 29:233–249
Treiman DM (2001) GABAergic mechanisms in epilepsy. Epilepsia 42 [Suppl 3]:8–12
Wafford KA, Bain CJ, Quirk K, Mckernan RM, Wingrove PB, Whiting PJ, Kemp JA (1994) A novel allosteric modulatory site on the GABAA receptor beta subunit. Neuron 12:775–782
White HS, Wolf HH, Swinyard EA, Skeen GA, Sofia RD (1992) A neuropharmacological evaluation of felbamate as a novel anticonvulsant. Epilepsia 33:564–572
Wingrove PB, Wafford KA, Bain C, Whiting PJ (1994) The modulatory action of loreclezole at the gamma-aminobutyric acid type A receptor is determined by a single amino acid in the beta 2 and beta 3 subunit. Proc Natl Acad Sci U S A 91:4569–4573
Acknowledgements
This study was supported by a grant from the Medical University of Lublin. The authors express their thanks to Miss K. Darocha and Miss J. Depa for their excellent technical assistance. Dr. J.J. Luszczki is a recipient of the Fellowship for Young Researchers from the Foundation for Polish Science.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Luszczki, J.J., Czuczwar, S.J. Isobolographic characterisation of interactions among selected newer antiepileptic drugs in the mouse pentylenetetrazole-induced seizure model. Naunyn Schmied Arch Pharmacol 372, 41–54 (2005). https://doi.org/10.1007/s00210-005-1088-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-005-1088-9