Abstract
Chronic exposure to β2-adrenoceptor agonists, especially fenoterol, has been shown to increase smooth muscle contraction to endothelin-1 in human bronchi partly through tachykinin-mediated pathways. The purpose of this work was to further investigate the role of sensory nerves in fenoterol-induced sensitization of human airways and the effect of nociceptin, a nociceptin/orphanin FQ (NOP) receptor agonist, on the increase in contraction after fenoterol exposure. Human bronchi from 62 patients were sensitized to endothelin-1 by prolonged incubation with fenoterol (0.1 μM, 15 h). The sensitizing effect of fenoterol was inhibited by high concentration of capsaicin (10 μM, 30 min before fenoterol sensitization), which induces depletion of mediators from sensory nerves, or co-incubation of fenoterol and capsazepine (1 μM), a vanilloid TRPV-1 receptor antagonist. Moreover, short pretreatment of bronchi with capsaicin (10 μM) or capsazepine (1 μM) after sensitization by fenoterol decreased the rise in smooth muscle contraction to endothelin-1. Nociceptin (1 μM) also inhibited the increased contraction in fenoterol-sensitized bronchi. Tertiapin (10 μM), an inhibitor of the inward-rectifier K+ channels, but not naloxone (0.1 μM), a DOP/KOP/MOP receptor antagonist, prevented the inhibitory effect of nociceptin. In conclusion, fenoterol induces sensitization of human isolated bronchi to endothelin-1 in part through the stimulation of the vanilloid TRPV-1 receptor on tachykininergic sensory nerves. Nociceptin inhibits airway hyperresponsiveness via NOP receptor activation. This effect involves inward-rectifier K+ channels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nociceptin is a heptadecapeptide isolated in 1995 (Meunier et al. 1995; Reinscheid et al. 1995) which acts through the opioid receptor-like 1 also called nociceptin/orphanin FQ (NOP) receptor. In guinea pig airways, nociceptin inhibits electrical field-induced tachykininergic contraction of isolated bronchus (Fischer et al. 1998), acetylcholine release by trachea (Patel et al. 1997), and capsaicin-induced bronchoconstriction in isolated lung (Corboz et al. 2000). In rat, nociceptin inhibits capsaicin-induced release of substance P (SP) and calcitonin gene-related peptide (CGRP) from trachea (Nemeth et al. 1998). Finally, in vivo studies have shown that nociceptin inhibits cough provoked by capsaicin in the guinea pig or by mechanical stimulation of intra-thoracic airways in the cat (Bolser et al. 2001; McLeod et al. 2001). All these results suggest that nociceptin inhibits both cholinergic and sensory nerves activation in the airways but, to the best of our knowledge, its role in the regulation of human airway hyperresponsiveness has not been studied so far.
Tachykininergic afferent sensory nerves in the respiratory tract include unmyelinated C-fibers and thinly myelinated Aδ fibers which project to the airway epithelium via a dense and continuous pathway (Lamb and Sparrow 2002). They play an important role in the regulation of airway smooth muscle tone and neurogenic inflammation through storage and release of SP and neurokinin A (NKA) acting via the neurokinin NK1 and NK2 receptors, respectively (Canning and Fisher 2001; Goldie et al. 2001; Undem et al. 1999). Sensory nerves are reactive to several stimuli including chemical stimuli such as acidic solution or changes in osmolarity or electrolytes concentration (Hunter et al. 2000; Pedersen et al. 1998; Riccio et al. 1996). They are also stimulated by chemical substances or mediators like capsaicin or lipoxygenase products such as 12 and 15-hydroperoxyeicosatetraenoic acids (12-HPETE and 15-HPETE) and leukotriene B4 (LTB4), which act via the activation of the vanilloid TRPV-1 receptor, a member of the transient receptor potential (TRP) channels superfamily (Hwang and Oh 2002; Tominaga et al. 1998). TRPV-1 receptor activation is also sensitized by protein kinases A and C (PKA and PKC) (Karschin 1999; Olah et al. 2002; Premkumar and Ahern 2000; Vellani et al. 2001).
Fenoterol, a short acting β2-adrenoceptor agonist, has been used as bronchodilatator for several decades in asthma treatment. However, regular single use of β2-adrenoceptor agonists may enhance bronchial hyperresponsiveness leading to a deleterious effect on asthma control. That increased risk was at first underlined, especially with fenoterol, by studies from New Zealand in the two last decades (Sears 2002). Other studies showed that inhaled β2-adrenoceptor agonists, as not only fenoterol, could increase airway responsiveness in human whereas their relaxant effects on the airway smooth muscle were not decreased (Van Schayck et al. 1990; Spitzer et al. 1992; Cockcroft et al. 1993; Taylor et al. 1993). But pathophysiologic mechanisms involving these untoward effects remained unclear. We recently demonstrated that prolonged exposure to β2-adrenoceptor agonists, especially fenoterol, induces sensitization of human bronchi to endothelin-1 (ET-1), a contractile peptide strongly implicated in chronic inflammatory airway diseases such as asthma and chronic obstructive pulmonary disease (Michaël and Markewitz 1996; Hay 1998), and that this phenomenon involves tachykinins (Faisy et al. 2002).
We hypothesized that sensory nerves are involved in fenoterol-induced airways sensitization through the activation of the TRPV-1 receptor, and that nociceptin may reduce this hyperresponsiveness through an inhibition of tachykinin release. The purpose of this work was to further investigate the role of the tachykinergic sensory nerves in the mechanisms of fenoterol-induced human airway sensitization to ET-1 and then to determine the effects of nociceptin on the contraction of the fenoterol-sensitized human bronchi. This would provide a more rational use of β2-adrenoceptor agonists in asthma.
Materials and methods
Human bronchial tissue preparations
The study was approved by our local Ethic Committee. Bronchial tissues were surgically removed from 69 patients (49 men and 20 women, 63±10 years of age) with lung cancer; all patients were smokers or ex-smokers. Tobacco smoke was stopped 4 weeks before surgical procedure in all smokers. Just after resection, segments of human bronchi with an inner diameter of 1–2 mm were collected as far as possible from the malignant lesion. We used only macroscopically normal bronchi and the absence of tumoral infiltration was retrospectively established in all bronchi. They were placed in oxygenated Krebs–Henseleit solution (composition in mM: NaCl 119, KCl 4.7, CaCl2 2.5, KH2PO4 1.2, NaHCO3 25 and glucose 11.7). After removal of adhering lung parenchyma and connective tissues, rings of the same bronchus were prepared (5–7 mm length × 1–2 mm internal diameter) and divided into two paired groups (control and pretreated bronchi). To standardize weight between control and pretreated bronchi, we paired (length and diameter) the rings of the same segment of the dissected bronchus before randomization by another investigator.
Experimental procedures
In a first protocol, one group of bronchi (control) was placed in Krebs–Henseleit solution at room temperature for 15 h. The other group (pretreated) was incubated for 15 h at room temperature with:
-
1.
Fenoterol at 0.1 μM
-
2.
A mixture of fenoterol (0.1 μM) and propranolol (0.1 μM), a non-selective beta-adrenoceptor antagonist
-
3.
Capsazepine (1 μM), a synthetic antagonist of the TRPV-1 receptor
-
4.
A mixture of fenoterol (0.1 μM) and capsazepine (1 μM)
-
5.
Vehicle of capsaicin (1% ethanol)
-
6.
In the last group, bronchi were first pretreated with capsaicin at high concentration (10 μM, 30 min), which induces depletion of tachykinins from C-fibers and degeneration of sensory nerves (Ellis and Undem 1994a; Fischer et al. 1998; Kiraly et al. 1991; Nemeth et al. 1998); bronchi were then bathed with fresh Krebs–Henseleit solution to washout tachykinins and they were finally incubated with fenoterol (0.1 μM, 15 h, room temperature). Capsaicin, capsazepine and fenoterol concentrations, incubation time and temperature were chosen according to previously published data (Faisy et al. 2002; Olah et al. 2002; Pinto et al. 2002; Szallasi et al. 1995; Trevisani et al. 2002). Nociceptin was not used in this protocol because of its rapid degradation (Calo et al. 2000).
After 15 h of incubation at room temperature with tested agents, experiments were performed in parallel (control and pretreated). The bronchial rings were suspended on hooks in 5 ml organ bath containing Krebs–Henseleit solution, gassed with 95% O2, 5% CO2 and maintained at 37°C. Each preparation was connected to a force displacement transducer (Statham UF1) and isometric tension changes were recorded on a polygraph. Preparations were equilibrated for 60 min. Bronchial rings were washed with fresh Krebs–Henseleit solution every 10 min and a load of 1–1.5 g was maintained throughout the first 30 min of the equilibrium period. Cumulative concentration–response curves to ET-1 (0.1 nM to 0.1 μM, with logarithmic increments) were then obtained.
To investigate the mechanisms of changes in ET-1-mediated contraction after sensitization by fenoterol, we conducted a second protocol where drugs were added to the organ bath at 37°C before addition of ET-1, but after 15 h of incubation at room temperature. Bronchi that were previously sensitized with 0.1 μM fenoterol and their controls were treated with:
-
1.
Capsaicin at high concentration (10 μM); addition of capsaicin was followed by a 30-min stabilization period then by washes with fresh Krebs–Henseleit solution and, 30 min later, the concentration–response curves to ET-1 were performed
-
2.
Capsazepine (1 μM) added 20 min before ET-1 contraction
-
3.
Nociceptin (1 μM), a NOP agonist, added 20 min before ET-1 contraction
-
4.
Naloxone (0.1 μM), a non-selective DOP/KOP/MOP receptor antagonist, added 20 min prior to the addition of nociceptin (1 μM) (Calo et al. 2000; Fischer et al. 1998; Patel et al. 1997)
-
5.
Tertiapin (10 μM), an inhibitor of the inward-rectifier K+ channels, added 40 min prior to the addition of nociceptin (1 μM; Drici et al. 2000; Jin and Lu 1998; Yamada 2002). To prevent degradation by endopeptidases, peptidase inhibitors (captopril, amastatin, bestatin and phosphoramidon, 10 μM each) were added in organ bath before nociceptin according to previously published data (Calo et al. 2000, 2002; Jia et al. 2002; Sakurada et al. 2002).
Drugs
Fenoterol, a 50:50 mixture of (R)-isomers and (S)-isomers, was purchased from Boehringer (Ingelheim, Germany); ET-1, amastatin, bestatin, phosphoramidon, propranolol, capsaicin, capsazepine and naloxone from Sigma (St Louis, MO, USA); nociceptin and tertiapin from Bachem (Voisin le Bretonneux, France); captopril from Bristol-Myers Squibb (Épernon, France). All drugs were dissolved in distilled water except capsaicin which was dissolved in ethanol at stock concentration of 25 mM. ET-1 was dissolved in water at stock concentration of 0.25 mM and kept in small aliquots (200 μl) at −20°C until used. A fresh aliquot was used for each experiment.
Data analysis and terminology
Values are means ± SEM. Each experiment was paired with its own control. Contractile responses are expressed in contraction (g) as follow: contraction (g) = total measured tension − basal tone. Emax represents the maximal contraction induced by 0.1 μM ET-1 (Bertrand et al. 1999). ΔEmax represents the difference between Emax obtained with the bronchi pretreated by tested agents and Emax obtained with the paired control human bronchi. ΔEmax is expressed in contraction (g). Because sensitization of human bronchi by fenoterol is characterized by an increase in maximal contraction to 0.1 μM ET-1 (Faisy et al. 2002), analysis of data was performed from the sample of bronchi with ΔEmax of ET-1>0 after 15 h of fenoterol exposure. Statistical analysis of the results was performed using Student’s t-test, two-tailed, for paired sample (StatView 5.0, SAS Institute, Inc., Cary, NC, USA). P<0.05 was considered significant.
Results
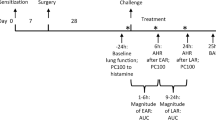
Fenoterol-induced sensitization
Incubation of the 69 bronchi with fenoterol (15 h, 21°C, 0.1 μM) significantly increased their maximal contraction to 0.1 μM ET-1 (2.21±0.12 g in presence of fenoterol versus 1.62±0.08 g in paired control bronchi, ΔEmax=0.59±0.09 g; Fig. 1). Sixty-two bronchi (90%) were sensitized by prolonged exposure to fenoterol. Also, seven bronchi (10%) were discarded from analysis.
Concentration–response curves for endothelin-1 (ET-1) in human bronchi after 15 h of incubation at room temperature with 0.1 μM fenoterol and in paired controls. ΔEmax: difference between maximal contraction to 0.1 μM ET-1 in pretreated bronchi and maximal contraction to 0.1 μM ET-1 in paired control bronchi. Values are means ± SEM (n=69). ***P<0.0001 fenoterol versus paired control
Effect of propranolol on fenoterol-induced sensitization
Incubation of human bronchi with propranolol alone (15 h, 21°C, 0.1 μM) did not change their maximal contraction to ET-1 (n=14, ΔEmax=0.04±0.14 g, not significant). In contrast, propranolol (0.1 μM, coincubated with fenoterol) abolished the rise in maximal response to ET-1 elicited by fenoterol in paired bronchi (Fig. 2).
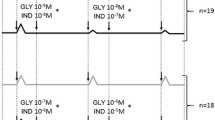
Effect of capsazepine on fenoterol-induced sensitization
Capsazepine alone (1 μM, 15 h, 21°C) had no effect on the Emax of ET-1 (n=10, ΔEmax=0.02±0.13 g, not significant), but, when coincubated with fenoterol, abolished the rise in maximal response to ET-1 elicited by fenoterol (Fig. 3a).
Effect on the increase in Emax of ET-1 induced by 0.1 μM fenoterol of a co-incubation for 15 h at room temperature of capsazepine, an antagonist of the TRPV-1 receptor, with fenoterol (n=10); b pre-incubation with high concentration of capsaicin (10 μ M, 30 min), which induces depletion of tachykinins from C-fibers, before fenoterol exposure (n=7). Values are means ± SEM. *P<0.05 versus paired control
Effect of pre-incubation of bronchi with capsaicin before fenoterol-induced sensitization
In preliminary experiments, incubation of human bronchi with vehicle of capsaicin (1% ethanol, 15 h, 21°C) did not change their maximal contraction to ET-1 (n=11, ΔEmax=−0.07±0.09 g, not significant). In the absence of fenoterol exposure, pre-incubation of bronchi with high concentration of capsaicin (10 μM, 30 min) had no effect on the Emax of ET-1 (n=7, ΔEmax=0±0.17 g, not significant). In paired bronchi, sensitization by fenoterol was significantly decreased by preincubation with high concentration of capsaicin (Fig. 3b).
Effect of capsaicin on ET-1-mediated contraction after sensitization by fenoterol
After 15 h of incubation at room temperature (21°C), a short pretreatment with high concentration of capsaicin (30 min, 37°C, 10 μM) did not change the maximal contraction of human bronchi to ET-1 (n=10, ΔEmax=0.22±0.25 g, not significant). In paired bronchi previously sensitized by fenoterol, short pretreatment with capsaicin abolished the rise in maximal response elicited by fenoterol exposure (Fig. 4a).
Effect of a short pretreatment with a high concentration of capsaicin (30 min, 37°C) followed by washes (n=10); b capsazepine (20 min, 37°C), an antagonist of the TRPV-1 receptor (n=11), on the rise in Emax of ET-1 after sensitization by fenoterol (15 h, 0.1 μM). Values are means ± SEM. *P<0.05; **P<0.01 versus paired control
Effect of capsazepine on ET-1-mediated contraction after sensitization by fenoterol
A short pretreatment (20 min, 37°C) with capsazepine (1 μM) did not change the maximal contraction of human bronchi to ET-1 (n=11, ΔEmax=0.01±0.15 g, not significant). In paired bronchi previously sensitized by fenoterol, short pretreatment with capsazepine significantly decreased the rise in maximal response to ET-1 elicited by fenoterol (Fig. 4b).
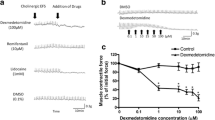
Effect of nociceptin on ET-1-mediated contraction after sensitization by fenoterol
In preliminary experiments we found that short pretreatment (30 min, 37°C) with a combination of protease inhibitors (captopril, amastatin, bestatin and phosphoramidon, 10 μM each) did not change the maximal contraction to ET-1 in the absence or presence of pretreatment with fenoterol (n=19, ΔEmax=−0.09±0.14 g, not significant and ΔEmax=−0.15±0.14 g, not significant, respectively). In the absence of fenoterol exposure, short pretreatment (20 min, 37°C) with nociceptin (1 μM) had no effect on the maximal contraction to ET-1 (n=18, ΔEmax=−0.03±0.15 g, not significant). In paired bronchi previously sensitized by fenoterol, nociceptin (1 μM) abolished the increase of maximal contraction to ET-1 (Fig. 5).
Action of naloxone and tertiapin on the inhibitory effect of nociceptin
In the absence of pretreatment with fenoterol, a short pretreatment with naloxone (20 min, 37°C, 0.1 μM) prior to nociceptin (1 μM) had no effect on the maximal contraction of human bronchi (n=12, ΔEmax=−0.07±0.14 g, not significant). In paired bronchi previously sensitized by fenoterol, naloxone did not alter significantly the inhibitory effect of nociceptin (Fig. 6a). In contrast, addition of tertiapin (40 min, 37°C, 10 μM) prior to nociceptin (1 μM) completely reestablished the fenoterol-induced potentiation of the maximal contraction to ET-1 in sensitized bronchi (Fig. 6b). In the absence of pretreatment with fenoterol, addition of tertiapin (10 μM) followed by nociceptin (1 μM) had no effect on the maximal contraction of paired bronchi (n=17, ΔEmax=−0.09±0.12 g, not significant).
Action of a naloxone, a non-selective DOP/KOP/MOP receptor antagonist (n=12); b tertiapin, an inhibitor of the inward-rectifier K+ channels (n=17), on nociceptin inhibitory effect after sensitization of human bronchi by fenoterol (15 h, 0.1 μM). Values are means ± SEM. **P<0.01 versus paired control. n.s not significant
Discussion
In this study, we demonstrate that sensitization of human isolated bronchi by a prolonged incubation with fenoterol involves in part the release of mediators from sensory nerve endings via the TRPV-1 receptor since sensitization to ET-1 is decreased by both co-incubation with capsazepine and pre-incubation with high concentration of capsaicin. Furthermore, after airway sensitization by fenoterol, short pretreatments with capsaicin at high concentration, capsazepine or nociceptin decrease the rise in maximal contraction to ET-1. This suggests that, in fenoterol-sensitized bronchi, the increase of contraction involves sensitization of TRPV-1 receptors in sensory C-fibers.
Role of sensory nerves in fenoterol-induced airways sensitization
Results of a previous study in our laboratory have suggested that sensory nerves may be involved in the increased response to ET-1 elicited by fenoterol in human isolated bronchi, since a combination of tachykinin NK1, NK2 and NK3 receptor antagonists avoided this airway sensitization (Faisy et al. 2002). Moreover, animal studies underlined that in vitro chronic exposure to fenoterol induced an increased expression of the mRNA for NK1 and NK2 receptors in bovine tracheal smooth muscle and in isolated guinea pig trachea (Katsunuma et al. 1999; Pinto et al. 2002). In contrast to the NK1 and NK3 receptor antagonists SR 140333 and SR 142801, the NK2 receptor antagonist SR 48968 did not reduce the fenoterol-induced hyperreactivity in isolated guinea pig trachea (Pinto et al. 2002). This discrepancy might be explained by the regulatory role of NK2 receptors in airway hyperresponsiveness in nervous components which are not studied in in vitro conditions (Ellis and Undem 1994b).
Sensory nerves release their peptides content (tachykinins, CGRP) after capsaicin-induced activation of the vanilloid TRPV-1 receptor characterized by its responsiveness to noxious stimuli such as acid and heat. Recently, ethanol was shown to cause a release of SP via the TRPV-1 receptor and to enhance nociceptor responses in the rat (Trevisani et al. 2002). Our results differ from these data since incubation of human bronchi with ethanol at the same concentration is unable to elicit the increase of the contractile response to ET-1. Duration of incubation and species differences may constitute possible explanations of these conflicting results. TRPV-1 receptors can also be activated by endogenous lipoxygenase products such as 12-HPETE and 15-HPETE or LTB4, which are known to be released from bronchial epithelial cells (Holtzman 1992; Shelhamer et al. 1995). TRPV-1 receptor activity is also modulated and activated by many factors including adenosine triphosphate, phospholipase C, PKA and PKC (Chuang et al. 2001; De Petrocellis et al. 2001; Kwak et al. 2000; Premkumar and Ahern 2000; Vellani et al. 2001). In this paper, we observe that co-incubation with capsazepine, an antagonist of the TRPV-1 receptor, abolishes the fenoterol-induced sensitizing effect. In addition, a short pre-incubation with capsaicin at high concentration, causing depletion in neuropeptides and neurotoxic axonal degeneration, decreases the fenoterol-induced airway sensitization. This decreased response of tachykinergic C-fibers is in agreement with our precedent results since tachykinins receptor antagonists decrease fenoterol-induced sensitization to ET-1 and abolish the increase of maximal contraction to ET-1 in fenoterol-sensitized bronchi (Faisy et al. 2002). However, although smoking ceased 4 weeks before surgical resection in our smoker patients, chronic tobacco smoke could also influence the responsiveness of the bronchi. Indeed, it has been shown that chronic tobacco smoke enhance lung C-fibers in sensitized guinea pigs (Bergren 2001).
We have also shown in this study that a non-selective beta-adrenoceptor antagonist, propranolol, abolishes the fenoterol-induced sensitization, suggesting the involvement of β2-adrenoceptor stimulation in the cause of airway sensitization (Faisy et al. 2002). Indeed, sensitization of human isolated bronchi to ET-1 is not specific of fenoterol since it is observed with others drugs which increase cAMP and PKA formation, such as forskolin and also β2-adrenoceptor agonists (salbutamol, terbutaline, formoterol and salmeterol) in a range of pharmacological concentrations inducing relaxation of smooth muscle (Faisy et al. 2002). Interestingly, Ho and colleagues demonstrated that prostaglandin E2 (PGE2), a prostanoid which also increases cAMP intracellular concentration (England et al. 1996; Taiwo et al. 1989), induced hypersensitivity of pulmonary C-fibers to chemical and mechanical stimuli in the rat (Ho et al. 2000). It has been shown that PGE2 increases the phosphorylation of the tetrodotoxin-resistant Na+ channel via the cAMP–PKA cascade and reduces the amplitude of voltage-gated K+ currents in the rat ganglion neurons (England et al. 1996). This was also demonstrated in human embryonic kidney cells where forskolin, an adenylate cyclase activator, and the cAMP analogue 8-bromo-cAMP increased the activation of TRPV-1 receptor by anandamide, an agonist of the TRPV-1 receptor (De Petrocellis et al. 2001; Hwang et al. 2000). Forskolin also enhanced the TRPV-1-mediated constriction by anandamide in isolated guinea pig bronchi and the anandamide-induced release of SP in rat dorsal root ganglia slices (De Petrocellis et al. 2001). In addition, PKC activation can sensitize human transfected TRPV-1 receptors to capsaicin in Xenopus oocytes (Crandall et al. 2002). These findings suggest that chronic exposure to fenoterol could sensitize sensory nerves via a kinase-dependent phosphorylation of ion channels and change in membrane potential. We previously established that calphostin C, a PKC inhibitor, is able to inhibit fenoterol-induced human airways sensitization (Faisy et al. 2002). However, the links between the increase of cAMP and the PKC activation, on the one hand, and the C-fibers stimulation, on the other hand, remain unclear and need further investigations.
Effect of nociceptin on ET-1-mediated contraction in sensitized bronchi
Opioid and opioid-like receptors are expressed in sensory nerves and seem to play a crucial role in the regulation of mediator’s release. The NOP receptor agonist nociceptin inhibits capsaicin-induced bronchoconstriction as well as acetylcholine release from airways in guinea pigs (Corboz et al. 2000; Fang et al. 2001; Jia et al. 2002; Peiser et al. 2000; Rizzi et al. 1999). Nociceptin also inhibits cough in the guinea pigs (McLeod et al. 2001) and in the cats (Bolser et al. 2001). In our study, nociceptin inhibits the increased airway smooth muscle contraction in fenoterol-sensitized bronchi. Moreover, we have shown that, in fenoterol-sensitized human bronchi, the inhibition by nociceptin of the raised smooth muscle contraction to ET-1 is naloxone insensitive, suggesting that nociceptin acts on sensory nerves via a receptor different from the classic opioid receptors (Calo et al. 2000; Fischer et al. 1998; Stretton et al. 1992). Nociceptin could inhibit tachykinins release from sensory nerves through a hyperpolarizing K+ current. Indeed, we have established in the present study that the inward-rectifier K+ channels blocker, tertiapin (Drici et al. 2000; Jin and Lu 1998; Kitamura et al. 2000), abolished the inhibitory effect of nociceptin. Jia et al. (2002) also found in isolated guinea pig lung that tertiapin abolished the nociceptin’s inhibition of capsaicin-induced airway smooth muscle contraction, demonstrating that this effect is mediated by inward-rectifier K+ channels activation. In addition, tertiapin antagonizes the inhibitory effect of nociceptin on capsaicin-induced (Ca2+)-rise in isolated guinea-pig nodose ganglia cells (Jia et al. 2002). A membrane hyperpolarizing effect of nociceptin by activation of an inward-rectifier K+ conductance has been reported in other tissues such as β-endomorphin neurons, other neurosecretory cells in the hypothalamic arcuate nucleus and hippocampal pyramidal cells (Ikeda et al. 1997; Lee et al. 1997; Wagner et al. 1998). However, a variety of K+ channels have been identified in the control of the cell membrane potential (Karschin 1999; Sebille et al. 2004) and our study lacks in the recognition of which K+ channel is involved in the fenoterol-sensitization because tertiapin is not a selective inward-rectifier K+ (Kir) channel blocker (Jin and Lu 1998). Although Kir3 channels were activated by NOP receptors in Xenopus oocytes and mammalian cells (Karschin 1999), additional studies are needed to precise this point in human bronchus and potassium channel openers such as cromakalim could be an alternative approach to explore the mechanisms of sensitization induced by fenoterol (Sebille et al. 2004).
In summary, as shown in Fig. 7, our study suggests that prolonged exposure to fenoterol induces a neurosensitization of isolated human bronchi, involving, at least in part, the TRPV-1 receptor of the tachykinergic sensory nerves. Nociceptin, a NOP receptor agonist, inhibits the potentiation of ET-1-mediated contraction in fenoterol-sensitized human bronchi through a pathway involving inward-rectifier K+ channels activation on sensory nerves.
Proposed mechanisms underlying the nociceptin inhibitory effect on human airway neurosensitization induced by fenoterol. Prolonged exposure of human bronchus to fenoterol induces a TRPV-1 receptor activation on sensory nerves, maybe via a pathway involving protein kinases C (see Discussion in the text). Stimulation of the TRPV-1 receptor enhances neuropeptide release and contributes to the rise in ET-1-mediated contraction of airway smooth muscle. Nociceptin counteracts this effect by activating an inward-rectifier K+ channel (Kir), which reduces neuropeptide release from sensory nerve endings via a membrane hyperpolarization. CGRP calcitonin gene-related peptide, NKA neurokinin A, NOP nociceptin/orphanin FQ receptor, SP substance P, TRPV-1 vanilloid TRPV-1 receptor
References
Bergren DR (2001) Enhanced lung C-fiber responsiveness in sensitized adult guinea pigs exposed to chronic tobacco smoke. J Appl Physiol 91:1645–1654
Bertrand C, Naline E, Advenier C (1999) In vitro effects of the endothelins on airway and vascular smooth muscle tone. In: Goldie RG, Hay DWP (eds) Pulmonary actions of the endothelins. Birkhäuser, Basel, pp 107–123
Bolser DC, McLeod RL, Tulshian DB, Hey JA (2001) Antitussive action of nociceptin in the cat. Eur J Pharmacol 430:107–111
Calo G, Guerrini R, Rizzi A, Salvadori S, Regoli D (2000) Pharmacology of nociceptin and its receptor: a novel therapeutic target. Br J Pharmacol 129:1261–1283
Calo G, Rizzi A, Rizzi D, Bigoni R, Guerrini R, Marzola G, Marti M, McDonald J, Morari M, Lambert DG, Salvadori S, Regoli D (2002) [Nphe(1),Arg(14),Lys(15)]nociceptin-NH(2), a novel potent and selective antagonist of the nociceptin/orphanin FQ receptor. Br J Pharmacol 136:303–311
Canning BJ, Fisher A (2001) Neural regulation of airway smooth muscle tone. Respir Physiol 125:113–127
Chuang HH, Prescott ED, Kong H, Shields S, Jordt SE, Basbaum AI, Chao MV, Julius D (2001) Bradykinin and nerve growth factor release the capsaicin receptor from PtdIns(4,5)P2-mediated inhibition. Nature 411:957–962
Cockcroft DW, McParland CP, Britto SA, Swystun VA, Rutherford BC (1993) Regular inhaled salbutamol and airway responsiveness to allergen. Lancet 342:833–837
Corboz MR, Rivelli MA, Egan RW, Tulshian D, Matasi J, Fawzi AB, Benbow L, Smith-Torhan A, Zhang H, Hey JA (2000) Nociceptin inhibits capsaicin-induced bronchoconstriction in isolated guinea pig lung. Eur J Pharmacol 402:171–179
Crandall M, Kwash J, Yu W, White G (2002) Activation of protein kinase C sensitizes human VR1 to capsaicin and to moderate decreases in pH at physiological temperatures in Xenopus oocytes. Pain 98:109–117
De Petrocellis L, Harrison S, Bisogno T, Tognetto M, Brandi I, Smith GD, Cy C, Davis JB, Geppetti P, Di Marzo V (2001) The vanilloid receptor (VR1)-mediated effects of anandamide are potently enhanced by the cAMP-dependent protein kinase. J Neurochem 77:1660–1663
Drici MD, Diochot S, Terrenoire C, Romey G, Lazdunski M (2000) The bee venom peptide tertiapin underlines the role of I(KACh) in acetylcholine-induced atrioventricular blocks. Br J Pharmacol 131:569–577
Ellis JL, Undem BJ (1994a) Inhibition by capsazepine of resiniferatoxin- and capsaicin-induced contractions of guinea pig trachea. J Pharmacol Exp Ther 268:85–89
Ellis JL, Undem BJ (1994b) Pharmacology of nonadrenergic noncholinergic nerves in airway smooth muscle. Pulm Pharmacol 7:205–223
England S, Bevan S, Docherty RJ (1996) PGE2 modulates the tetrodotoxin-resistant sodium current in neonatal rat dorsal root ganglion neurones via the cyclic AMP-protein kinase A cascade. J Physiol 495:429–440
Faisy C, Naline E, Diehl JL, Emonds-Alt X, Chinet T, Advenier C (2002) In vitro sensitization of human bronchus by beta(2)-adrenergic agonists. Am J Physiol Lung Cell Mol Physiol 283:L1033–L1042
Fang LB, Wu Y, Zhang LF, Fang WQ (2001) Inhibition by nociceptin on excitatory non-adrenergic non-cholinergic response in guinea pig airways. Acta Pharmacol Sin 22:561–565
Fischer A, Forssmann WG, Undem BJ (1998) Nociceptin-induced inhibition of tachykinergic neurotransmission in guinea pig bronchus. J Pharmacol Exp Ther 285:902–907
Goldie RG, Rigby PJ, Fernandes LB, Henry PJ (2001) The impact of inflammation on bronchial neuronal networks. Pulm Pharmacol Ther 14:177–182
Hay DW (1998) Endothelin-1: an interesting peptide or an important mediator in pulmonary diseases? Pulm Pharmacol Ther 11:141–146
Ho CY, Gu Q, Hong JL, Lee LY (2000) Prostaglandin E(2) enhances chemical and mechanical sensitivities of pulmonary C fibers in the rat. Am J Respir Crit Care Med 162:528–533
Holtzman MJ (1992) Arachidonic acid metabolism in airway epithelial cells. Annu Rev Physiol 54:303–329
Hunter DD, Myers AC, Undem BJ (2000) Nerve growth factor-induced phenotypic switch in guinea pig airway sensory neurons. Am J Respir Crit Care Med 161:1985–1990
Hwang SW, Oh U (2002) Hot channels in airways: pharmacology of the vanilloid receptor. Curr Opin Pharmacol 2:235–242
Hwang SW, Cho H, Kwak J, Lee SY, Kang CJ, Jung J, Cho S, Min KH, Suh YG, Kim D, Oh U (2000) Direct activation of capsaicin receptors by products of lipoxygenases: endogenous capsaicin-like substances. Proc Natl Acad Sci USA 97:6155–6160
Ikeda K, Kobayashi K, Kobayashi T, Ichikawa T, Kumanishi T, Kishida H, Yano R, Manabe T (1997) Functional coupling of the nociceptin/orphanin FQ receptor with the G-protein-activated K+ (GIRK) channel. Brain Res Mol Brain Res 45:117–126
Jia Y, Wang X, Aponte SI, Rivelli MA, Yang R, Rizzo CA, Corboz MR, Priestley T, Hey JA (2002) Nociceptin/orphanin FQ inhibits capsaicin-induced guinea-pig airway contraction through an inward-rectifier potassium channel. Br J Pharmacol 135:764–770
Jin W, Lu Z (1998) A novel high-affinity inhibitor for inward-rectifier K+ channels. Biochemistry 37:13291–13299
Karschin A (1999) G protein regulation of inwardly rectifying K(+) channels. News Physiol Sci 14:215–220
Katsunuma T, Roffel AF, Elzinga CR, Zaagsma J, Barnes PJ, Mak JC (1999) Beta(2)-adrenoceptor agonist-induced upregulation of tachykinin NK(2) receptor expression and function in airway smooth muscle. Am J Respir Cell Mol Biol 21:409–417
Kiraly E, Jancso G, Hajos M (1991) Possible morphological correlates of capsaicin desensitization. Brain Res 540:279–282
Kitamura H, Yokoyama M, Akita H, Matsushita K, Kurachi Y, Yamada M (2000) Tertiapin potently and selectively blocks muscarinic K(+) channels in rabbit cardiac myocytes. J Pharmacol Exp Ther 29:196–205
Kwak J, Wang MH, Hwang SW, Kim TY, Lee SY, Oh U (2000) Intracellular ATP increases capsaicin-activated channel activity by interacting with nucleotide-binding domains. J Neurosci 20:8298–8304
Lamb JP, Sparrow MP (2002) Three-dimensional mapping of sensory innervation with substance P in porcine bronchial mucosa: comparison with human airways. Am J Respir Crit Care Med 166:1269–1281
Lee K, Nicholson JR, McKnight AT (1997) Nociceptin hyperpolarises neurones in the rat ventromedial hypothalamus. Neurosci Lett 239:37–40
McLeod RL, Parra LE, Mutter JC, Erickson CH, Carey GJ, Tulshian DB, Fawzi AB, Smith-Torhan A, Egan RW, Cuss FM, Hey JA (2001) Nociceptin inhibits cough in the guinea-pig by activation of ORL(1) receptors. Br J Pharmacol 132:1175–1178
Meunier JC, Mollereau C, Toll L, Suaudeau C, Moisand C, Alvinerie P, Butour JL, Guillemot JC, Ferrara P, Monsarrat B (1995) Isolation and structure of the endogenous agonist of opioid receptor-like ORL1 receptor. Nature 377:532–535
Michaël JR, Markewitz BA (1996) Endothelins and the lung. Am J Respir Crit Care Med 154:555–581
Nemeth J, Helyes Z, Oroszi G, Than M, Pinter E, Szolcsanyi J (1998) Inhibition of nociceptin on sensory neuropeptide release and mast cell-mediated plasma extravasation in rats. Eur J Pharmacol 347:101–104
Olah Z, Karai L, Iadarola MJ (2002) Protein kinase C(alpha) is required for vanilloid receptor 1 activation. Evidence for multiple signaling pathways. J Biol Chem 277:35752–35759
Patel HJ, Giembycz MA, Spicuzza L, Barnes PJ, Belvisi MG (1997) Naloxone-insensitive inhibition of acetylcholine release from parasympathetic nerves innervating guinea-pig trachea by the novel opioid, nociceptin. Br J Pharmacol 120:735–736
Pedersen KE, Meeker SN, Riccio MM, Undem BJ (1998) Selective stimulation of jugular ganglion afferent neurons in guinea pig airways by hypertonic saline. J Appl Physiol 84:499–506
Peiser C, Undem BJ, Fischer A (2000) Nociceptin effects in the airways. Peptides 21:995–998
Pinto FM, Saulnier JP, Faisy C, Naline E, Molimard M, Prieto L, Martin JD, Emonds-Alt X, Advenier C, Candenas ML (2002) SR 142801, a tachykinin NK(3) receptor antagonist, prevents beta(2)-adrenoceptor agonist-induced hyperresponsiveness to neurokinin A in guinea-pig isolated trachea. Life Sci 72:307–320
Premkumar LS, Ahern GP (2000) Induction of vanilloid receptor channel activity by protein kinase C. Nature 408:985–990
Reinscheid RK, Nothacker HP, Bourson A, Ardati A, Henningsen RA, Bunzow JR, Grandy DK, Langen H, Monsma FJ, Civelli O (1995) Orphanin FQ: a neuropeptide that activates an opioid-like G protein-coupled receptor. Science 270:792–794
Riccio MM, Myers AC, Undem BJ (1996) Immunomodulation of afferent neurons in guinea-pig isolated airway. J Physiol 491:499–509
Rizzi A, Calo G, Trevisani M, Tognetto M, Fabbri L, Mapp C, Guerrini R, Salvadori S, Regoli D, Geppetti P (1999) Nociceptin receptor activation inhibits tachykinergic non-adrenergic non-cholinergic contraction of guinea pig isolated bronchus. Life Sci 64:PL157–PL163
Sakurada C, Sakurada S, Orito T, Tan-No K, Sakurada T (2002) Degradation of nociceptin (orphanin FQ) by mouse spinal cord synaptic membranes is triggered by endopeptidase-24.11: an in vitro and in vivo study. Biochem Pharmacol 64:1293–1303
Sears MR (2002) Adverse effects of β-agonists. J Allergy Clin Immunol 110:S322–S328
Sebille S, De Tullio P, Boverie S, Antoine MH, Lebrun P, Pirotte B (2004) Recent developments in the chemistry of potassium channel activator: the cromakalim analogs. Curr Med Chem 11:1213–1222
Shelhamer JH, Levine SJ, Wu T, Jacoby DB, Kaliner MA, Rennard SI (1995) NIH conference. Airway inflammation. Ann Intern Med 123:288–304
Spitzer WO, Suissa S, Ernst P, Horwitz RI, Habbick B, Cockcroft D, Boivin JF, McNutt M, Buist AS, Rebuck AS (1992) The use of beta-agonists and the risk of death and near death from asthma. N Engl J Med 326:501–506
Stretton D, Miura M, Belvisi MG, Barnes PJ (1992) Calcium-activated potassium channels mediate prejunctional inhibition of peripheral sensory nerves. Proc Natl Acad Sci USA 89:1325–1329
Szallasi A, Goso C, Manzini S (1995) Resiniferatoxin binding to vanilloid receptors in guinea pig and human airways. Am J Respir Crit Care Med 152:59–63
Taiwo YO, Bjerknes LK, Goetzl EJ, Levine JD (1989) Mediation of primary afferent peripheral hyperalgesia by the cAMP second messenger system. Neuroscience 32:577–580
Taylor DR, Sears MR, Herbison GP, Flannery EM, Print CG, Lake DC, Yates DM, Lucas MK, Li Q (1993) Regular inhaled beta agonist in asthma: effects on exacerbations and lung function. Thorax 48:134–138
Tominaga M, Caterina MJ, Malmberg AB, Rosen TA, Gilbert H, Skinner K, Raumann BE, Basbaum AI, Julius D (1998) The cloned capsaicin receptor integrates multiple pain-producing stimuli. Neuron 21:531–543
Trevisani M, Smart D, Gunthorpe MJ, Tognetto M, Barbieri M, Campi B, Amadesi S, Gray J, Jerman JC, Brough SJ, Owen D, Smith GD, Randall AD, Harrison S, Bianchi A, Davis JB, Geppetti P (2002) Ethanol elicits and potentiates nociceptor responses via the vanilloid receptor-1. Nat Neurosci 5:546–551
Undem BJ, McAlexander M, Hunter DD (1999) Neurobiology of the upper and lower airways. Allergy 54 [Suppl 57]:81–93
Van Schayck CP, Graafsma SJ, Visch MB, Dompeling E, Van Weel C, Van Herwaarden CL (1990) Increased bronchial hyperresponsiveness after inhaling salbutamol during 1 year is not caused by subsensitization to salbutamol. J Allergy Clin Immunol 86:793–800
Vellani V, Mapplebeck S, Moriondo A, Davis JB, McNaughton PA (2001) Protein kinase C activation potentiates gating of the vanilloid receptor VR1 by capsaicin, protons, heat and anandamide. J Physiol 534:813–825
Wagner EJ, Ronnekleiv OK, Grandy DK, Kelly MJ (1998) The peptide orphanin FQ inhibits beta-endorphin neurons and neurosecretory cells in the hypothalamic arcuate nucleus by activating an inwardly-rectifying K+ conductance. Neuroendocrinology 67:73–82
Yamada M (2002) The role of muscarinic K(+) channels in the negative chronotropic effect of a muscarinic agonist. J Pharmacol Exp Ther 300:681–687
Acknowledgements
The authors acknowledge statistical advice of Professor Gilles Chatellier (Department of Medical Informatics and Biostatistics, Hôpital Européen Georges Pompidou).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Faisy, C., Naline, E., Rouget, C. et al. Nociceptin inhibits vanilloid TRPV-1-mediated neurosensitization induced by fenoterol in human isolated bronchi. Naunyn-Schmiedeberg's Arch Pharmacol 370, 167–175 (2004). https://doi.org/10.1007/s00210-004-0974-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-004-0974-x