Abstract
Reactive oxygen species (ROS) play a role in cardiovascular diseases such as heart failure and hypertension. Furthermore, increasing evidence has accumulated suggesting that ROS can also be formed subsequent to the stimulation of various receptors, thus functioning as second messengers.
The objective of the present study was to elucidate the role of intracellular-generated ROS in the inotropic and chronotropic effects of the α1- and β-adrenoceptor and the ET-receptor stimulation in isolated rat atria. In addition, we investigated whether the MAPKerk pathway is involved in the ROS-provoked rise of contractile force. For this purpose hydrogen peroxide was applied, which is known to serve several endogenous functions as a second messenger. Moreover, hydrogen peroxide readily crosses cell membranes, which thus allows to mimic the intracellular formation.
Preincubation of atria with EUK 8 (400 μM), a cell permeable superoxide dismutase- and catalase-mimetic, reduced the positive inotropic effect upon α1-adrenoceptor and ET-receptor stimulation. The responsiveness to β-adrenoceptor stimulation remained unaffected by this pretreatment. The chronotropic effects were not altered by preincubation with EUK 8. In contrast to the MAPKp38 inhibitor SB203580 (2 and 10 μM), the two MKKmek inhibitors PD98059 (30 and 100 μM) and U0126 (10 μM) significantly attenuated the positive inotropic response to hydrogen peroxide in isolated rat left atria. In addition, inhibition of the Na+/H+ exchange (NHE) by cariporide (1 μM) counteracted ROS-provoked increase of contractile force.
From the present study we conclude that the inotropic responses to α1-adrenoceptor and ET-receptor stimulation are, at least partially, caused by intracellular-formed ROS, that subsequently may activate the MAPKerk pathway and the NHE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The presence of reactive oxygen species (ROS) such as hydroxyl radicals, hydrogen peroxide and superoxide anions has been associated with noxious reactions within the cardiovascular system during pathological conditions like heart failure, atherosclerosis and hypertension (Dhalla et al. 2000). Furthermore, increasing evidence has accumulated suggesting that ROS may play a physiological role in the responses to hormones and neurotransmitters. Accordingly, ROS may be defined as second messengers when receptor stimulation initiates endogenous ROS formation, which subsequently mediates signaling by targeting signal transduction proteins. An active role of ROS as second messengers has for instance been shown in the signal transduction of bradykinin (Greene et al. 2000), for the ATI-receptor (Griendling et al. 1994), for α1-adrenoceptors (Amin et al. 2001; Hirotani et al. 2002; Xiao et al. 2002), the endothelin (ET)-receptor (Cheng et al. 1999; Hirotani et al. 2002) and 5HT-receptor (Lee et al. 1997).
The mitogenic and apoptotic effects of intracellular-generated ROS have been studied in detail, but investigations addressing the relationship between receptor-mediated ROS-formation and the impact on agonist-induced change of contractile behaviour and frequency of beating in isolated cardiac tissues are lacking so far.
Peters et al. (2002) recently reported that the inotropic but not the chronotropic effects caused by adrenoceptor and ET-receptor stimulation is partially mediated by the mitogen-activated protein kinase (MAPKerk) pathway. MAPKs have predominantly been linked to phosphorylation and activation of transcription factors, thereby inducing cellular growth (for review see Michel et al. 2001).
Hirotani et al. (2002) demonstrated that stimulation of cardiac α1-adrenoceptors and ET-receptor is associated with an increase of ROS production. In addition, certain members of the MAPKerk pathway are sensitive towards oxidative stress and certain ROS (like for example hydrogen peroxide) can provoke activation of the aforementioned kinases (Aikawara et al. 1997; Snabaitis et al. 2002; Xiao et al. 2002).
Accordingly, the present study was performed in order to clarify:
-
1.
Whether adrenoceptor and ET-receptor stimulation-mediated inotropic and chronotropic effects are, at least partially, based on intracellular generated ROS and
-
2.
Whether MAPKerk pathway might be involved in the ROS-induced increase in contractile force
For this purpose, we studied the influence of EUK 8 (Tanguy et al. 1996; Siwik et al. 1999; Pimentel et al. 2001), which is a cell-permeable superoxide dismutase- and catalase-mimetic on the inotropic and chronotropic responses to adrenoceptor and endothelin ET-receptor stimulation in isolated rat left atria.
In order to mimic intracellular ROS production we applied the cell-permeable ROS hydrogen peroxide and investigated the mechanisms of the hydrogen peroxide-induced positive inotropic effects by adding inhibitors of the MAPKerk pathway as well as cariporide, an inhibitor of the Na+/H+ exchanger (NHE).
Materials and methods
Atrial contraction studies
Male Wister rats (240–300 g) were sacrificed by stunning and decapitation. The hearts were removed quickly and placed in a buffer solution of the following composition (in mM): NaCl 119; KCl 4.5; MgCl2 0.5; CaCl2 2.5; glucose 11; Tris 30 at pH 7.4 at room temperature. The medium was gassed with 100% oxygen. The isolated left atria were suspended in water jacketed organ baths (kept at 37°C and gassed with 100% oxygen) filled with 4 ml buffer solution (pH adjusted to 7.4 at 37°C), and connected with a silk thread to an isometric force transducer connected to a Power Lab/8 s data acquisition system (ADInstruments, Australia). The left atria were paced with a field stimulator (Hugo Sachs Electronic, Germany) at a frequency of 3 Hz, whereas right atria were allowed to beat spontaneously. The resting tension was adjusted to 5 mN.
Studies with EUK 8 on receptor stimulation
The left and right atria were allowed to equilibrate for at least 20 min. Thereafter, the atria were incubated for 30 min with EUK 8 (400 μM) or vehicle. Subsequently, the α1-adrenoceptor agonist methoxamine (300 μM), the β-adrenoceptor agonist isoprenaline (3 μM) or ET-1 (50 nM) was added.
Positive inotropic effect of hydrogen peroxide
After the equilibration period the atria were incubated with the MKKmek inhibitors U0146 (10 μM), PD98059 (30 and 100 μM), the p38 kinase inhibitor SB203580 (2 and 10 μM), the NHE inhibitor cariporide (1 μM) or with vehicle (DMSO 0.2%) for 45 min. Hydrogen peroxide (250 μM) was administered and the increase of contractile force was assessed 3–5 min after its addition.
Statistics
Data are expressed as means ± SEM. The concentration response curves (CRC) were analyzed by using a computer program (Graph Pad, Institute for Scientific Informatics, San Diego, CA, USA).
Statistical significance was determined by ANOVA followed by Bonferroni Multiple Comparison post test or a two-tailed Student's t-test.
P values <0.05 were considered to be statistically significant.
Chemicals and drugs used
Methoxamine and isoprenaline were purchased from Sigma Chemical, St. Louis (MO, USA), EUK 8 (a N, N'-bis-salicyden aminoethane-manganese complex) from Merk Eurolab, Amsterdam (the Netherlands), PD98059 (2'-amino-3'-methoxyflavone), SB203580 ([4-(4-fluorophenyl)-2-(4-methylsulfinylphenyl)-5-(4-pyridyl)1H-imidazole) from Alexis, Nottingham (United Kingdom), U0126 (1,4 diamino-2,3 dicyano-1,4-bis(2-aminophenylthio)butadiene) from Promega, Madison (WI, USA), ET-1 from BACHEM, Bubendorf (Switzerland), hydrogen peroxide form ACROS Organics, Geel (Belgium).
Cariporide was a kind gift from Aventis, Frankfurt am Main (Germany). All drugs were dissolved in distilled water except for U0126, PD98059, SB203580 and cariporide, which were dissolved in DMSO.
Results
Atrial contraction studies
The initial contractile force of the paced left atria amounted 7.9±0.1 mN (n=83) and the initial heart rate of the spontaneously beating right atria was 253±5 bpm (n=32). EUK 8 affected neither the initial contractile force in left atrial preparations nor the initial beating rate of isolated right atria.
EUK 8 attenuated the rise of contractile force after α1-adrenoceptor and ET-receptor stimulation when compared to vehicle (saline) treated preparations (0.84±0. 2 mN vs. 2.5±0.2 mN, 1.4±0.3 mN vs. 2.4±0.4 mN, respectively, n=6–7, p<0.05). The positive inotropic effect of isoprenaline was not affected by EUK 8 (4.0±0.5 mN vs. 4.3±0.6 mN, n=6–7, n.s., respectively) (Fig. 1).
The influence of the cell permeable superoxide dismutase- and catalase-mimetic EUK 8 on the positive inotropic effects triggered by adrenoceptor and ET-receptor stimulation. Isolated rat left atria were incubated with either EUK 8 (400 μM) or vehicle for 30 min followed by the addition of either methoxamine (300 μM), isoprenaline (3 μM) or ET-1 (50 nM). *p<0.05 vs. control preparations, n=6–7
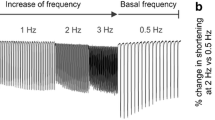
The chronotropic effects of isoprenaline, ET-1 and methoxamine were not influenced by EUK 8 (n=4–6) (Fig. 2).
The influence of EUK 8 (400 μM), a cell permeable superoxide dismutase- and catalase mimetic, on the chronotropic effects triggered by adrenoceptor and ET-receptor stimulation. Isolated rat right atria were incubated with either EUK 8 (400 μM) or vehicle for 30 min followed by the addition of either methoxamine (300 μM), isoprenaline (3 μM) or ET-1 (50 nM). No attenuation was observed (n=4–6)
Hydrogen peroxide (250 μM) provoked a transient increase of contractile force of 0.9±0.2 mN (n=12). Preincubation of the rat left atria with the MKKmek inhibitors PD98059 (30 and 100 μM) and U0126 (10 μM) inhibited the hydrogen peroxide-induced rise of contractile force completely (−0.3±0.2 mN, −0.5±0.1 mN, 0.1±0.2 mN, respectively, n=5–6, p<0.05). In addition, the NHE inhibitor cariporide (1 μM) also counteracted the increase in contractile force provoked by hydrogen peroxide (0.1±0.1 mN, n=5, p<0.05).
In contrast, the contractile response to hydrogen peroxide remained unaffected by the MAPKp38 inhibitor SB203580 (2 and 10 μM) (0.7±0.1 and 0.5±0.1 mN, respectively, n=4–6) (Fig. 3).
The influence of the MKKmek inhibitors PD98058 and U0126, the MAPKp38 inhibitor SB203580 and the NHE inhibitor cariporide on the hydrogen peroxide-induced increase in contractile force. Isolated rat left atria were incubated with either MKKmek inhibitors U0126 (10 μM), PD98059 (30 and 100 μM), the MAPKp38 SB203580 (2 and 10 μM) or the NHE inhibitor cariporide (1 μM) for 45 min with a subsequent addition of hydrogen peroxide (250 μM). *p<0.05 vs. control preparations, n=4–12
Discussion
There is a growing body of evidence suggesting that reactive oxygen species (ROS) are not just noxious entities that contribute to the pathophysiology and etiology of various cardiovascular diseases like atherosclerosis, hypertension and heart failure. ROS can interfere very specifically with signal transduction pathways and may thus affect physiological functions of cardiac and vascular cells (Dhalla et al. 2000). Moreover, ROS should also be considered as cellular messengers based on the observation that receptor stimulation may trigger the generation of these highly active entities (for review see Suzuki et al. 1997). In addition, various studies demonstrated that stimulation of both cardiac α1-adrenoceptors and ET-receptors leads to myocardial hypertrophy. This effect is mediated partly by intracellular generated ROS and the intermediate activation of the MAPKerk pathway (Cheng et al. 1999; Amin et al. 2001). The role of these ROS in inotropic and chronotropic responses to adrenoceptor and ET-receptor stimulation has not been studied in detail so far.
Peters et al. (2002) recently demonstrated that the MAPKerk pathway is involved in the positive inotropic effect of α1-adrenoceptor and ET-receptor stimulation. Since these kinases are known to be activated by ROS, we hypothesized that adrenoceptor and ET-receptor stimulation-induced increase of contractile force might (at least partially) be dependent on intracellular formed ROS-dependent MAPKerk activation.
We studied the influence of the cell-permeable superoxide dismutase- and catalase-mimetic EUK 8 on α1- and β-adrenoceptor as well as on ET-receptor stimulation in isolated rat left atria. As shown in Fig. 1, EUK 8 applied in a supra-maximal concentration (Tanguy et al. 1996; Siwik et al. 1999; Pimentel et al. 2001), reduced the positive inotropic response to α1-adrenoceptor and ET-receptor stimulation, but not to β-adrenoceptor stimulation. This finding indicates that ROS production initiated by α1-adrenoceptor and ET-receptor stimulation contributes to their contractile responsiveness. Although β-adrenoceptor stimulation has been associated with endogenous ROS formation (Singh et al. 2001), EUK 8 did not influence the contractile response by isoprenaline addition. First of all, this observation suggests that, although ROS formation is triggered by receptor stimulation, it does not necessarily mean that generated ROS contribute to the subsequent positive inotropic response. Furthermore, this result excludes that EUK 8 unselectively attenuates all receptor-triggered inotropic responses.
In contrast to its effects on the contractile force, EUK 8 did not affect the chronotropic effects of the agonists applied in the present study (see Fig. 2). We reported that MKKmek inhibitors only affected the inotropic but not the chronotropic responses to the stimulation of the receptors studied (Peters et al. 2002). Those data therefore support our hypothesis that ROS are likely to be involved in the MAPKerk-dependent rise of contractile force but not in changes of beating frequency.
Hydrogen peroxide has been shown to increase intracellular Ca2+ concentrations by different mechanisms including for instance the activation of protein kinase C (Ward and Moffat 1995), stimulation of Ca2+-induced Ca2+-release from sarcoplasmatic reticulum (Suzuki et al. 1997) and an increase of plasmalemmal Ca2+ leak channel activity (Wang et al. 1995).
Hydrogen peroxide is a putative second messenger and moreover, it readily crosses cell membranes, thus allowing its exogenous application as a tool. In order to prove that ROS can lead to a positive inotropic effect by activating members of the MAPKerk pathway, we added hydrogen peroxide to MKKmek inhibitors-pretreated isolated rat left atria. 250 μM of hydrogen peroxide was used, since this concentration proved to be the lowest concentration that enhanced intracellular Ca2+ levels in cardiomyocytes (Wang et al. 1999). As shown in Fig. 3, the MKKmek inhibitors PD98059 (30 and 100 μM) and U0126 (10 μM) counteracted the hydrogen peroxide-induced increase of contractile force, indicating the involvement of the MAPKerk pathway. In contrast, SB203580 (2 and 10 μM) did not reduce the positive inotropic effect of hydrogen peroxide. These results are also in agreement with our hypothesis, that only the MAPKerk but not the MAPKp38 pathway contributes to the responsiveness to positive inotropic stimuli (Peters et al. 2002).
Moreover, we applied the NHE inhibitor cariporide in order to illuminate the signaling downstream of the MAPKerk pathway. As shown in Fig. 3, cariporide significantly attenuated the rise of contractile force provoked by hydrogen peroxide, indicating a contribution of NHE. These findings are supported by the observation of Snabaitis et al. (2002). These authors have demonstrated that hydrogen peroxide activates the NHE by a MAPKerk-dependent but MAPKp38-independent pathway in rat cardiomyocytes. It has also been reported that
-
1.
Both α1-adrenoceptor and the ET-receptor can activate the NHE (Snabaitis et al. 2000; Fliegel 2001)
-
2.
Inhibition of NHE may attenuate the positive inotropic responses to stimulation of these receptors (Talukder and Endoh 1997)
Therefore, we propose the following alternative pathway (Fig. 4): α1-adrenoceptor as well as the ET-receptor stimulation cause an increase of endogenous ROS [presumably by activation of NADH/NAD(P)H oxidases (Tanaka et al. 2000; Xiao et al. 2002)] with a subsequent stimulation of the MAPKerk pathway, thereby inducing an increase of NHE activity, which might contribute to the positive inotropic effect of the aforementioned receptors.
Proposed signal transduction cascade (bold) for the α1-adrenoceptor and ET-receptor. Contractile effects are partially mediated by ROS-induced activation of the MAPKerk pathway followed by an increase of NHE activity. PLC phospholipase C, DAG diacylglycerol, IP 3 inositoltrisphosphate, PKC protein kinase C, NHE Na+/H+ exchanger
In conclusion, our data provide strong indications that cardiac α1-adrenoceptor as well as ET-receptor but not β-adrenoceptor stimulation mediates their positive inotropic effects, at least partially, by ROS-induced MAPKerk activation. Conversely, the chronotropic effects of these stimuli seem to be independent from intracellular ROS formation.
References
Aikawara R, Kumoro I, Yamazaki T et al (1997) Oxidative stress activates extracellular signal regulated kinases through Src and Ras in cultured cardiac myocytes of neonatal rats. J Clin Invest 100:1813–1821
Amin JK, Xiao L, Pimental DR, Pagano PJ, Singh K, Sawyer DB, Colucci WS (2001) Reactive oxygen species mediate alpha-adrenergic receptor-stimulated hypertrophy in adult rat ventricular myocytes. J Mol Cell Cardiol 33:131–139
Cheng TH, Shih NL, Chen SY, Wang DL, Chen JJ (1999) Reactive oxygen species modulate endothelin-1-induced c-fos gene expression in cardiomyocytes. Cardiovasc Res 41:654–662
Dhalla NS, Temsah RM, Netticadan T (2000) Role of oxidative stress in cardiovascular diseases. J Hypertens 18:655–673
Fliegel L (2001) Regulation of myocardial Na+/H+ exchanger activity. Basic Res Cardiol 96:301–305
Greene EL, Velarde V, Jaffa AA (2000) Role of reactive oxygen species in bradykinin-induced mitogen-activated protein kinase and c-fos induction in vascular cells. Hypertension 35:942–947
Griendling KK, Minieri CA, Ollerenshaw JD, Alexander RW (1994) Angiotensin II stimulates NADH and NADPH oxidase activity in cultured vascular smooth muscle cells. Circ Res 74:1141–1148
Hirotani S, Otsu K, Nishida K, Higushi Y, Morita T et al (2002) Involvement of nuclear factor-κB and apoptosis signal-regulating kinase 1 in G-protein-coupled receptor agonist-induced cardiomyocyte hypertrophy. Circulation 105:509–515
Lee SL, Wan WW, Fanburg BL (1998) Superoxide as an intermediate signal for serotonin-induced mitogenesis. Free Radic Biol Med 24:855–858
Michel MC, Li Y, Heusch G (2001) Mitogen-activated protein kinases in the heart. Naunyn-Schmiedebergs Arch Pharmacol 363:245–266
Peters SL, Sand C, Michel MC, Pfaffendorf M, van Zwieten PA (2002) A mitogen-activated protein kinase is involved in the inotropic but not chronotropic actions of adrenoceptor agonists and endothelin-1. Naunyn-Schmiedebergs Arch Pharmacol 366:189–191
Pimentel DR, Amin JK, Xiao L, Miller T, Viereck J, Oliver-Krasinski J, Baliga R, Wang J, Siwik DA, Singh K, Pagano P, Colucci WS, Sawyer DB (2001) Reactive oxygen species mediate amplitude-dependent hypertrophic and apoptotic responses to mechanical stretch in cardiac myocytes. Circ Res 89:453–460
Singh K, Xiao L, Remondino A, Sawyer DB, Colucci WS (2001) Adrenergic regulation of cardiac myocyte apoptosis. J Cell Physiol 189:257–265
Siwik DA, Tzortzis JD, Pimental DR, Chang DL, Pagano PJ, Singh K, Sawyer DB, Colucci WS (1999) Inhibition of copper-zinc superoxide dismutase induces cell growth, hypertrophic phenotype, and apoptosis in neonatal rat cardiac myocytes in vitro. Circ Res 85:147–153
Snabaitis AK, Yokoyama H, Avikran M (2000) Roles of mitogen-activated kinases and protein kinase C in α1A-adrenoceptor mediated stimulation of the sacrolemmal Na+/H+ exchanger. Circ Res 86:214–220
Snabaitis AK, Hearse DJ, Avikran M (2002) Regulation of sacrolemmal Na+/H+ exchange by hydrogen peroxide in adult rat ventricular myocytes. Cardiovasc Res 53:470–480
Suzuki YJ, Forman HJ, Sevanian A (1997) Oxidants as stimulators of signal transduction. Free Radic Biol Med 22:269–285
Talukder MA, Endoh M (1997) Pharmacological differentiation of synergistic contribution of L-type Ca2+ channels and Na+/H+ exchange to the positive inotropic effect of phenylephrine, endothelin-3 and angiotensin II in rabbit ventricular myocardium. Naunyn-Schmiedebergs Arch Pharmacol 355:87–96
Tanaka K, Honda M, Takabatake T (2001) Redox regulation of MAPK pathways and cardiac hypertrophy in adult rat cardiac myocyte. J Am Coll Cardiol 37:676–685
Tanguy S, Boucher FR, Malfroy B, de Leiris JG (1996) Free radicals in reperfusion-induced arrhythmias: study with EUK 8, a novel nonprotein catalytic antioxidant. Free Radic Biol Med 21:945–954
Wang SY, Clague JR, Langer GA (1995) Increase in calcium leak channel activity by metabolic inhibition or hydrogen peroxide in rat ventricular myocytes and its inhibition by polycation. J Mol Cell Cardiol 27:211–222
Wang X, Takeda S, Mochizuki S, Jindal R, Dhalla NS (1999) Mechanisms of hydrogen peroxide-induced increase in intracellular calcium in cardiomyocytes. J Cardiovasc Pharmacol Ther 4:41–48
Ward CA, Moffat MP (1995) Role of protein kinase C in mediating effects of hydrogen peroxide in guinea-pig ventricular myocytes. J Mol Cell Cardiol 27:1089–1097
Xiao L, Pimentel DR, Wang J, Singh K, Colucci WS, Sawyer DB (2002) Role of reactive oxygen species and NAD(P)H oxidase in alpha(1)-adrenoceptor signaling in adult rat cardiac myocytes. Am J Physiol Cell Physiol 282:C926–934
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sand, C., Peters, S.L.M., Pfaffendorf, M. et al. The influence of endogenously generated reactive oxygen species on the inotropic and chronotropic effects of adrenoceptor and ET-receptor stimulation. Naunyn-Schmiedeberg's Arch Pharmacol 367, 635–639 (2003). https://doi.org/10.1007/s00210-003-0745-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-003-0745-0