Abstract
Formaldehyde (FA), an economically important and ubiquitous chemical, has been classified as a human carcinogen and myeloid leukemogen. However, the underlying mechanisms of leukemogenesis remain unclear. Unlike many classical leukemogens that damage hematopoietic stem/progenitor cells (HSC/HPC) directly in the bone marrow, FA—as the smallest, most reactive aldehyde—is thought to be incapable of reaching the bone marrow through inhalation exposure. A recent breakthrough study discovered that mouse lung contains functional HSC/HPC that can produce blood cells and travel bi-directionally between the lung and bone marrow, while another early study reported the presence of HSC/HPC in rat nose. Based on these findings, we hypothesized that FA inhalation could induce toxicity in HSC/HPC present in mouse lung and/or nose rather than in the bone marrow. To test this hypothesis, we adapted a commercially available protocol for culturing burst-forming unit-erythroid (BFU-E) and colony-forming unit-granulocyte, macrophage (CFU-GM) colonies from bone marrow and spleen to also enable culture of these colonies from mouse lung and nose, a novel application of this assay. We reported that in vivo exposure to FA at 3 mg/m3 or ex vivo exposure up to 400 µM FA decreased the formation of both colony types from mouse lung and nose as well as from bone marrow and spleen. These findings, to the best of our knowledge, are the first empirically to show that FA exposure can damage mouse pulmonary and olfactory HSC/HPC and provide potential biological plausibility for the induction of leukemia at the sites of entry rather than the bone marrow.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Formaldehyde (FA) is a ubiquitous chemical extensively used in various industries (Tang et al. 2009; Duong et al. 2011). Exposure to FA mainly occurs via inhalation or skin absorption in workers in certain occupational settings including the production of FA resins and textiles, as well as embalming and medical laboratories (Zhang et al. 2009; McGwin et al. 2010). The general public is routinely exposed to FA from multiple sources, such as building materials, cigarette smoking and some manufactured wood or fabric products (Leng et al. 2019; Nikle et al. 2019). This widespread occupational and/or environmental exposure to FA raises concerns about potential adverse health effects.
The International Agency for Research on Cancer (IARC) classified FA as a Group I human carcinogen based on sufficient evidence that FA causes nasopharyngeal cancer (Cogliano et al. 2005; IARC 2006) and is associated with myeloid leukemia (IARC 2012). A number of earlier large cohort studies on FA-exposed workers (Hauptmann 2003; Pinkerton 2004) and follow-up studies (Beane Freeman et al. 2009; Hauptmann et al. 2009) support the association between FA exposure and myeloid leukemia. Previously, we reported that FA induced hematotoxicity and chromosomal aneuploidy in the circulating myeloid progenitor cells of exposed workers (Zhang et al. 2010b; Lan et al. 2015). Additionally, we found that FA induced toxicity in bone marrow (BM) and hematopoietic stem/progenitor cells (HSC/HPC) of exposed mice via inhalation (Zhang et al. 2013b; Ye et al. 2013; Wei et al. 2017).
Most classical leukemogens (e.g., chemotherapeutic drugs and benzene) initiate leukemogenesis by directly damaging the HSC/HPC in the BM (Zhang et al. 2009, 2010a). However, FA—as the simplest and most reactive aldehyde—is unlikely to reach the bone marrow to cause toxicity and initiate leukemia, based on current studies. Several studies showed that exogenous DNA adducts were detectable in the nasal epithelium, but not in BM, of the exposed rats (Lu et al. 2010, 2011). Thus, the site and mechanism of leukemia initiation by FA remain uncertain. A number of alternative models were proposed hypothesizing potential targets (e.g., circulating HSC/HPC in blood or pluripotent nasal/oral stem cells) of inhaled FA that could initiate leukemogenesis outside of BM (Zhang et al. 2009).
Recently, a breakthrough study from Dr. Looney and his colleagues revealed that a large number of megakaryocytes along with progenitors residing in mouse lung can release platelets and circulate bi-directionally between the lung and BM (Lefrançais et al. 2017). In addition, an earlier study reported that cells dissociated from rat olfactory epithelium gave rise to multiple cells of hematopoietic lineages, including lymphoid and myeloid cells, when injected into irradiated rats (Murrell et al. 2005). Based on these discoveries that the lung and nose contain functional HSC/HPC, we primarily proposed an unconventional hypothesis (Zhang 2018). Instead of damaging HSC/HPC in BM directly, FA may induce HSC/HPC toxicity in mouse lung and nose, the portals of entry for inhaled FA exposure.
Hematopoiesis is a process whereby HSC/HPC undergo differentiation into mature blood cells (Orkin and Zon 2008; Jagannathan-Bogdan and Zon 2013). HSC continuously replenish the blood system through a series of lineage differentiation steps and the early steps involve the development of the myeloid and lymphoid cell lineages (Kondo 2010). The myeloid lineage includes erythrocytes (E), granulocytes and macrophages (GM) and megakaryocytes (M), while the lymphoid lineage includes T lymphocytes, B lymphocytes and natural killer cells (Kondo et al. 2003).
In the present study, we aimed to examine FA-induced toxicity in HSC/HPC from mouse lung and nose, in both in vivo (inhalation) and ex vivo experiments. We applied a colony assay from StemCell Technologies™ to evaluate the growth and number of HSC/HPC in multiple mouse tissue types, including lung, nose, bone marrow and spleen. Two colony types, burst-forming unit-erythroid (BFU-E) and colony-forming unit, granulocytes and macrophages (CFU-GM), predominantly are cultured from committed myeloid stem/progenitor cells using this assay.
Materials and methods
Animals and mouse tissues
Specific pathogen-free male BALB/c mice (5 weeks old) were purchased from Hubei Experimental Animal Center (Wuhan, China) (in vivo) and Jackson Laboratory (Bar Harbor, ME) (ex vivo), respectively. They were housed in the Experimental Animal Center of Central China Normal University (in vivo) and Northwest Animal Facility of University of California, Berkeley (ex vivo) and maintained under a 12 h daily light cycle. All mice had free access to clean food and water. They were adapted to the environment for one week before any treatments. All procedures involving animals were conducted in accordance with Institutional Animal Care and Use Committee of Central China Normal University and Animal Care and Use Committee of University of California, Berkeley.
Four types of tissue including BM, spleen, lung and nose were selected for the downstream colony assay. As the two main sites containing HSC/HPC, BM and spleen were chosen as control tissue types. According to previous findings that functional HSC/HPC are also present in lung (Lefrançais et al. 2017) and nose (Murrell et al. 2005), these two tissues were chosen as experimental tissues. Theoretically, the amount of HSC/HPC in lung and nose would be much lower than in BM and spleen. To acquire adequate cell numbers for downstream (colony) analyses, the lung and nose tissues from 3 mice in each treatment group were combined.
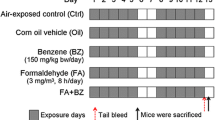
FA inhalation exposure (in vivo)
FA inhalation exposure was conducted in Central China Normal University. BALB/c mice were randomly divided into two groups, vehicle group (control) and FA-exposed group. Briefly, the mice in each group were exposed to ambient air prepared from double-distilled (DD) water or 3 mg/m3 FA prepared from 10% formalin (Sigma-Aldrich, St Louis, MO, USA), using an environmentally controlled 8.4 L glass chamber. During exposure, the air FA concentration in the chamber was monitored every 2 h using a Gaseous FA Analyzer 4160-2 (Interscan, Simi Valley, CA, USA). Air temperature, humidity and ventilation rate were maintained at 23 ± 0.5 °C, 45 ± 5.0% and 1.5 L/min, respectively. Mice were exposed from 9 a.m. to 5 p.m., 8 h/day, 5 days/week, for 2 weeks (Fig. 1a). Two researchers independently conducted two experiments and the results are shown as experiment I (Expt. I) and experiment II (Expt. II).
Biological sample preparation (in vivo)
On the 13th day of treatment, mice were anesthetized by intraperitoneal injection of 100 mg/kg (body weight) pentobarbital sodium and then sacrificed by cervical dislocation. BM, spleen, lung, and nose tissues were collected. BM cells were flushed from femurs with ice-cold Iscove’s Modified Dulbecco’s Medium (IMDM) containing 1% penicillin–streptomycin and 2% fetal bovine serum (FBS). Spleens and lungs were rinsed 3–4 times with IMDM containing 1% penicillin–streptomycin and 2% FBS and cells were flushed out with the same media using 1 mL syringes with needles (23 gauge). Nasal tissue, mainly olfactory mucosa from the nasal septum, were cut into pieces after opening the nasal cavity. Nasal cells were isolated and harvested by digestion using 0.25% trypsin at 37 °C for 45 min. The collected cells were then filtered through 40 µm strainers and the erythrocytes were lysed by red blood cell (RBC) lysing reagent (150 mM NH4Cl, 10 mM KHCO3, 1 mM EDTA). Lung, nose, BM and spleen cell counts were determined using a blood cell analyzer (Motenu MTN-21, Changchun, China).
Biological sample preparation and FA treatment (ex vivo)
The ex vivo experiment was conducted at University of California, Berkeley. After 1-week adaptation, mice were euthanized by CO2 inhalation. BM cells were flushed from femurs with phosphate-buffered saline (PBS). Lung, nose and spleen cell samples were prepared following the same protocol as for the in vivo experiments. Briefly, all three tissues were removed from mice and rinsed with PBS to remove debris. The tissues were minced finely and digested enzymatically using digestion buffer (2 mL PBS + 10 µL Dnase + 0.25 mg liberase per tissue) at 37 °C for 45 min. The collected cells were then filtered through 40 µm strainers, subjected to RBC lysis, resuspended and counted using Vi-CELL™ Cell Counter for Cell Viability Analyzer (Beckman-Coulter, Brea, CA, USA). Lung, nose, BM and spleen cells were plated (see below for cell density) and treated with 0, 50, 100, 200, 400 µM FA (Thermo Fisher Scientific, Waltham, MA, USA) for 1 h at 37 °C (Fig. 1b).
Myeloid progenitor colony formation assay both in vivo and ex vivo
Cells harvested from all tissues after treatment and preparation were seeded in MethoCult™ GF M3434 (StemCell Technologies™, Vancouver, Canada), a methylcellulose-based medium enriched in the recombinant cytokines including erythropoietin (EPO), in 30 mm petri dishes. GF M3434 supports the generation of colonies from stem or progenitor cells that are present. According to the protocol of StemCell Technologies™ and the results of our pilot study, the optimal seeding concentrations by tissue type were as follows: lung 1 × 106 cells/dish, nose 3 × 105 cells/dish, BM 5 × 104 cells/dish, and spleen 4 × 105 cells/dish, with 1.2 mL medium per dish. Cells were plated in duplicate and cultured for 10–12 days at 37 °C. Two colony types, BFU-E and CFU-GM, were predominantly cultured using medium in this colony-forming unit (CFU) assay.
Colonies, defined as containing more than 50 cells, were verified and counted under the microscope by two researchers after 10–12 days culture based on colony phenotypes indicated by StemCell Technologies™ instructions.
Statistical analysis
Data are presented as mean ± SEM. GraphPad Prism 6.0 was used for the statistical analysis. Student’s t test was used to test the significance of differences between groups. ptrend was analyzed with linear regression. Statistical significance was considered to be p < 0.05.
Results
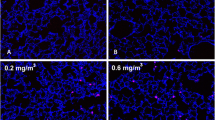
Culture of BFU-E and CFU-GM colonies from mouse lung and nose
BFU-E and CFU-GM, two major colony types formed from more committed myeloid progenitors, were cultured from BM and spleen, major reservoirs of blood cell precursors. In addition, both colony types were cultured from the lung and nose of mice and were shown to be morphologically similar to those cultured from BM and spleen (Fig. 2).
BFU-E and CFU-GM colonies cultured from the lung, nose, BM and spleen of BALB/c mice. Based on a guideline from StemCell TechnologiesTM, erythroid cells tend to grow together forming a “wrinkled” cluster (BFU-E) in which individual cells cannot be distinguished. In contrast, in the CFU-GM colonies, individual cells are “phase-bright” or “clear” in appearance, enabling the identification of this colony type
FA exposure in vivo decreased the formation of both BFU-E and CFU-GM colonies in lung and nose as well as in BM and spleen
A greater number of BFU-E (Fig. 3a) than CFU-GM colonies (Fig. 3b) were cultured from all four tissue types in two independent experiments (Expt. I and Expt. II). FA exposure (3 mg/m3) significantly reduced BFU-E colony formation from lung in Expt. II only (Fig. 3a A1, p < 0.05) and from nose in both experiments (Fig. 3a A2, p < 0.001 and p < 0.05, respectively), compared to unexposed controls. FA exposure significantly reduced CFU-GM colony formation from lung in experiment Expt. II only (Fig. 3b B1, p < 0.05) and from nose in Expt. I only (Fig. 3b B2, p < 0.05), compared to control.
The formation of both BFU-E and CFU-GM colonies from all four tissues (lung, nose, BM and spleen) of BALB/c mice exposed to vehicle or 3 mg/m3 FA in vivo. The experiments were conducted independently by two researchers and the results are shown as Expt. I and Expt. II. Each tissue type was cultured in duplicate. Each data point represents one replicate of each tissue type. Data are presented as mean ± SEM. *p < 0.05, **p < 0.01 and ***p < 0.001, as compared to control
FA exposure significantly reduced BFU-E colony formation from BM in both Expt. I and II (Fig. 3a A3, p < 0.01 and p < 0.001, respectively) and from spleen in Expt. II (Fig. 3a A4, p < 0.001). FA exposure significantly reduced CFU-GM colony formation from BM in both Expt. I and Expt. II (Fig. 3b B3, p < 0.001 and p < 0.01, respectively) and from spleen in Expt. I and Expt. II (Fig. 3b B4, p < 0.05 and p < 0.01, respectively).
Ex vivo FA exposure significantly decreased the formation of both BFU-E and CFU-GM colonies in nose, BM and spleen but not in lung
We conducted ex vivo experiments to confirm the HSC/HPC toxicities induced by FA inhalation. FA treatment (0–400 µM) statistically reduced the formation of both BFU-E (Fig. 4a) and CFU-GM (Fig. 4b) colonies from mouse nose, BM and spleen (ptrend < 0.05). However, the decrease of colonies in the lung was not statistically significant (ptrend > 0.05). Further, 400 µM FA induced a significant (p < 0.05) reduction in BFU-E from mouse nose, BM and spleen (Fig. 4a A2–A4) and in CFU-GM from spleen (Fig. 4b B4).
The formation of both BFU-E and CFU-GM colonies from all four tissues (lung, nose, BM and spleen) of BALB/c mice exposed to vehicle or FA ex vivo. The experiments were independently repeated 5 times for lung, BM and spleen, and 4 times for nose. Data at each dose were merged from 4–5 repeated experiments. Each tissue type was cultured in duplicate. The average of the duplicate for each tissue type represents each individual experiment. Data are presented as mean ± SEM. *p < 0.05 as compared to control
Discussion
Detection of HSC/HPC in BALB/c mouse lung and nose using a modified CFU assay
The CFU assay has been widely applied in research to evaluate the growth of HSC/HPC (North et al. 2007; Tomar et al. 2010; Kobayashi et al. 2010; Zhang et al. 2013a). Basically, when cultured in a semi-solid matrix supplemented with appropriate growth factors and/or cytokines, each individual stem or progenitor cell, the so-called CFU, proliferates and differentiates to form one colony. Using the CFU assay, extensive studies have investigated the growth of HSC/HPC residing in peripheral blood, BM and spleen (Ratajczak et al. 2010; Loh et al. 2010; Lafuse et al. 2013). Moreover, our previous studies revealed HSC/HPC toxicity induced by benzene and FA in the peripheral blood of exposed workers (Lan et al. 2004; Zhang et al. 2010b) and in BM of FA-inhaled mice (Ge et al. 2020; Wei et al. 2017). However, the CFU assay was not previously applied to study the growth of HSC/HPC present in the lung and nose. To our knowledge, this is the first study to do so.
We adapted the CFU assay from StemCell Technologies™ to culture BFU-E and CFU-GM colonies from HSC/HPC present in mouse lung and nose for the first time. We utilized BALB/c mice for comparability with our previous studies of FA-induced toxicity (Zhang et al. 2013b; Wei et al. 2017). Thus, our findings have confirmed the presence of viable HSC/HPC in lung and nose in a second mouse strain. The presence of hematopoietic precursors in lung (Lefrançais et al. 2017) and nose (Murrell et al. 2005) was originally reported in mice (C57/BL6) and rats (RT7.2-positive and RT7.2-negative), respectively. Notably, this novel detection of viable HSC/HPC was successful at laboratories both in China and in the U.S. as well as both in vivo and ex vivo.
Colony numbers differed across tissues and type of experiment
In the present study, many more BFU-E than CFU-GM colonies were generated from all tissues in the in vivo experiments, which is similar to what we previously reported in our studies of human cells treated with FA (Zhang et al. 2010b) and workers exposed to benzene (Lan et al. 2004). However, our previous in vivo study in BALB/c mice, conducted using a different type of media, produced a higher level of CFU-GM than BFU-E from BM (Ge et al. 2020; Wei et al. 2017). On the other hand, similar numbers of both colony types were generated from the ex vivo experiments. This could have arisen, in part, from the different tissue preparation protocols used in the in vivo and ex vivo experiments, especially the utilization of different digestive enzymes. As expected, fewer colonies were cultured from lung and nose than from BM and spleen, the main sites of HSC/HPC and hematopoiesis, though more colonies were generated from nose than from lung in our experiments both in vivo and ex vivo. It is unclear if this reflects actual numbers of HSC/HPC present in those tissues; thus, more investigations are warranted.
FA exposure in vivo and ex vivo damaged HSC/HPC in lung, nose, BM and spleen
Leukemogenesis is an evolutionary process which may be initiated by the transformation of primitive HSC into leukemic stem cells (LSC) (Passegue et al. 2003; Renneville et al. 2008). The LSC arises from the accumulation of multiple genetic events, such as genomic alterations and/or chromosomal aberrations (Dash and Gilliland 2001; Renneville et al. 2008). Previously, our epidemiologic study in China showed a significant elevation of leukemia-specific chromosomal aneuploidy in the circulating myeloid progenitor cells of FA-exposed workers (Zhang et al. 2010b; Lan et al. 2015). Correspondingly, our previous animal studies indicated FA-induced toxicity in mouse BM (Zhang et al. 2013b; Ye et al. 2013; Wei et al. 2017). Consistent with the previous findings, it was confirmed in the current study that FA exposure damaged the HSC/HPC in BM. Furthermore, for the first time, we have shown that FA exposure impaired the formation of colonies from HSC/HPC in spleen, again supporting the role of FA in causing hematotoxicity in leukemia-relevant tissues.
In the present study, inhalation of 3 mg/m3 FA decreased the formation of both BFU-E and CFU-GM colonies in mouse lung and nose, demonstrating that FA can exert toxicity to pulmonary/olfactory HSC/HPC. In addition, FA exposure ex vivo suppressed colony formation in nose tissue in a dose-dependent manner, while the decreased colony formation was not statistically significant in lung. A strength of this study is the general consistency between the in vivo and ex vivo experiments both of which showed the nose to be more sensitive than lung to FA toxicity. Possibly, this could reflect a higher dose of FA via a shorter inhalation route and/or the greater inhalation intake through nose than lung in mice (Fig. 5). However, due to the relatively low yield of colonies from lung, further studies are needed to confirm this difference in sensitivity. In summary, our findings provide direct evidence to support our hypothesis that FA may induce leukemogenesis without reaching BM, by damaging HSC/HPC at the sites of entry, nose and lung.
Implications and conclusion
To address the controversy over the association of myeloid leukemia and FA exposure in humans, we hypothesized that FA inhalation could damage HSC/HPC in the lung and/or nose (Zhang 2018), and that these damaged cells might travel to bone marrow to initiate leukemogenesis (Fig. 5). Our hypothesis has been tested in a mouse model in the current study. A colony assay was adapted to examine FA-induced toxicity in HSC/HPC presented in mouse lung and nose in comparison with BM and spleen. We first successfully cultured two main type of colonies, BFU-E and CFU-GM, and then detected the FA-reduced growth of colonies from lung and nose in vivo and ex vivo. Our findings suggest that nasal stem and progenitor cells may be another target of FA exposure. This is also supported by previous studies, for example, FA induces DPCs and other toxicities in nasal passages of animals (Lu et al. 2010, 2011; Moeller et al. 2011) as well as nasal and oral mucosa of exposed humans (Ballarin et al. 1992). Potentially, FA-induced DNA damage and lesions in the pluripotent stem cells in nose could result in damaged olfactory HSC/HPC travelling to the BM, acquiring a subsequent mutation, and initiating leukemogenesis.

adapted from https://www.pngwing.com.)
Overview of our study hypothesis, testing model and experimental design for detection of HSC/HPC toxicity induced by FA in mouse lung and nose. (Note: the image of human background figure is
In conclusion, for the first time, we have demonstrated the induction of HSC/HPC toxicity in mouse lung and nose by FA exposure both in vivo and ex vivo, providing biological plausibility to an alternative model of leukemia induction outside of the BM. It could also deepen and improve our understanding of chemically-induced leukemogenesis.
References
Ballarin C, Sarto F, Giacomelli L et al (1992) Micronucleated cells in nasal mucosa of formaldehyde-exposed workers. Mutat Res/Genet Toxicol 280:1–7. https://doi.org/10.1016/0165-1218(92)90012-O
Beane Freeman LE, Blair A, Lubin JH et al (2009) Mortality from lymphohematopoietic malignancies among workers in formaldehyde industries: the National Cancer Institute cohort. JNCI J Nat Cancer Inst 101:751–761. https://doi.org/10.1093/jnci/djp096
Cogliano VJ, Grosse Y, Baan RA et al (2005) Meeting report: summary of IARC Monographs on formaldehyde, 2-butoxyethanol, and 1-tert-butoxy-2-propanol. Environ Health Perspect 113:1205–1208. https://doi.org/10.1289/ehp.7542
Dash A, Gilliland DG (2001) Molecular genetics of acute myeloid leukaemia. Best Pract Res ClinHaematol 14:49–64. https://doi.org/10.1053/beha.2000.0115
Duong A, Steinmaus C, McHale CM et al (2011) Reproductive and developmental toxicity of formaldehyde: a systematic review. Mutat Res/Rev Mutat Res 728:118–138. https://doi.org/10.1016/j.mrrev.2011.07.003
Ge J, Yang H, Lu X et al (2020) Combined exposure to formaldehyde and PM2.5: hematopoietic toxicity and molecular mechanism in mice. Environ Int 144:106050
Hauptmann M (2003) Mortality from lymphohematopoietic malignancies among workers in formaldehyde industries. Cancer SpectrKnowl Environ 95:1615–1623. https://doi.org/10.1093/jnci/djg083
Hauptmann M, Stewart PA, Lubin JH et al (2009) Mortality from lymphohematopoietic malignancies and brain cancer among embalmers exposed to formaldehyde. JNCI J Nat Cancer Inst 101:1696–1708. https://doi.org/10.1093/jnci/djp416
International Agency for Research on Cancer, Weltgesundheitsorganisation (eds) (2012) IARC monographs on the evaluation of carcinogenic risks to humans, volume 100 F, chemical agents and related occupations: this publication represents the views and expert opinions of an IARC Working Group on the Evaluation of Carcinogenic Risks to Humans, which met in Lyon, 20–27 October 2009. IARC, Lyon
International Agency for Research on Cancer (ed) (2006) IARC monographs on the evaluation of carcinogenic risks to humans, volume 88, formaldehyde, 2-butoxyethanol and 1-tert-butoxypropan-2-ol: this publication represents the views and expert opinions of an IARC Working Group on the Evaluation of Carcinogenic Risks to Humans, which met in Lyon, 2–9 June 2004. IARC, Lyon
Jagannathan-Bogdan M, Zon LI (2013) Hematopoiesis. Development 140:2463–2467. https://doi.org/10.1242/dev.083147
Kobayashi H, Butler JM, O’Donnell R et al (2010) Angiocrine factors from Akt-activated endothelial cells balance self-renewal and differentiation of haematopoietic stem cells. Nat Cell Biol 12:1046–1056. https://doi.org/10.1038/ncb2108
Kondo M (2010) Lymphoid and myeloid lineage commitment in multipotent hematopoietic progenitors: roles of bone marrow microenvironment. Immunol Rev 238:37–46. https://doi.org/10.1111/j.1600-065X.2010.00963.x
Kondo M, Wagers AJ, Manz MG et al (2003) Biology of hematopoietic stem cells and progenitors: implications for clinical application. Annu Rev Immunol 21:759–806. https://doi.org/10.1146/annurev.immunol.21.120601.141007
Lafuse WP, Story R, Mahylis J et al (2013) Leishmaniadonovani infection induces anemia in hamsters by differentially altering erythropoiesis in bone marrow and spleen. PLoS ONE 8:e59509. https://doi.org/10.1371/journal.pone.0059509
Lan Q, Zhang L, Li G et al (2004) Hematotoxicity in workers exposed to low levels of benzene. Science 306:1774–1776. https://doi.org/10.1126/science.1102443
Lan Q, Smith MT, Tang X et al (2015) Chromosome-wide aneuploidy study of cultured circulating myeloid progenitor cells from workers occupationally exposed to formaldehyde. Carcinogenesis 36:160–167. https://doi.org/10.1093/carcin/bgu229
Lefrançais E, Ortiz-Muñoz G, Caudrillier A et al (2017) The lung is a site of platelet biogenesis and a reservoir for haematopoietic progenitors. Nature 544:105–109. https://doi.org/10.1038/nature21706
Leng J, Liu C, Hartwell HJ et al (2019) Evaluation of inhaled low-dose formaldehyde-induced DNA adducts and DNA–protein cross-links by liquid chromatography–tandem mass spectrometry. Arch Toxicol 93:763–773. https://doi.org/10.1007/s00204-019-02393-x
Loh Y-H, Hartung O, Li H et al (2010) Reprogramming of T cells from human peripheral blood. Cell Stem Cell 7:15–19. https://doi.org/10.1016/j.stem.2010.06.004
Lu K, Collins LB, Ru H et al (2010) Distribution of DNA adducts caused by inhaled formaldehyde is consistent with induction of nasal carcinoma but not leukemia. ToxicolSci 116:441–451. https://doi.org/10.1093/toxsci/kfq061
Lu K, Moeller B, Doyle-Eisele M et al (2011) Molecular dosimetry of N2-hydroxymethyl-dG DNA adducts in rats exposed to formaldehyde. Chem Res Toxicol 24:159–161. https://doi.org/10.1021/tx1003886
McGwin G, Lienert J, Kennedy JI (2010) Formaldehyde exposure and asthma in children: a systematic review. Environ Health Perspect 118:313–317. https://doi.org/10.1289/ehp.0901143
Moeller BC, Lu K, Doyle-Eisele M et al (2011) Determination of N2-hydroxymethyl-dG adducts in the nasal epithelium and bone marrow of nonhuman primates following 13CD2-formaldehyde inhalation exposure. Chem Res Toxicol 24:162–164. https://doi.org/10.1021/tx1004166
Murrell W, Féron F, Wetzig A et al (2005) Multipotent stem cells from adult olfactory mucosa. Dev Dyn 233:496–515. https://doi.org/10.1002/dvdy.20360
Nikle A, Liou Y, Ericson M et al (2019) Formaldehyde release from clothing and upholstery fabrics using the chromotropic acid method. Dermatitis 30:255–258. https://doi.org/10.1097/0000000000000460
North TE, Goessling W, Walkley CR et al (2007) Prostaglandin E2 regulates vertebrate haematopoietic stem cell homeostasis. Nature 447:1007–1011. https://doi.org/10.1038/nature05883
Orkin SH, Zon LI (2008) Hematopoiesis: an evolving paradigm for stem cell biology. Cell 132:631–644. https://doi.org/10.1016/j.cell.2008.01.025
Passegue E, Jamieson CHM, Ailles LE, Weissman IL (2003) Normal and leukemic hematopoiesis: are leukemias a stem cell disorder or a reacquisition of stem cell characteristics? Proc Natl AcadSci 100:11842–11849. https://doi.org/10.1073/pnas.2034201100
Pinkerton LE (2004) Mortality among a cohort of garment workers exposed to formaldehyde: an update. Occup Environ Med 61:193–200. https://doi.org/10.1136/oem.2003.007476
Ratajczak MZ, Lee H, Wysoczynski M et al (2010) Novel insight into stem cell mobilization-plasma sphingosine-1-phosphate is a major chemoattractant that directs the egress of hematopoietic stem progenitor cells from the bone marrow and its level in peripheral blood increases during mobilization due to activation of complement cascade/membrane attack complex. Leukemia 24:976–985. https://doi.org/10.1038/leu.2010.53
Renneville A, Roumier C, Biggio V et al (2008) Cooperating gene mutations in acute myeloid leukemia: a review of the literature. Leukemia 22:915–931. https://doi.org/10.1038/leu.2008.19
Tang X, Bai Y, Duong A et al (2009) Formaldehyde in China: production, consumption, exposure levels, and health effects. Environ Int 35:1210–1224. https://doi.org/10.1016/j.envint.2009.06.002
Tomar GB, Srivastava RK, Gupta N et al (2010) Human gingiva-derived mesenchymal stem cells are superior to bone marrow-derived mesenchymal stem cells for cell therapy in regenerative medicine. BiochemBiophys Res Commun 393:377–383. https://doi.org/10.1016/j.bbrc.2010.01.126
Wei C, Wen H, Yuan L et al (2017) Formaldehyde induces toxicity in mouse bone marrow and hematopoietic stem/progenitor cells and enhances benzene-induced adverse effects. Arch Toxicol 91:921–933. https://doi.org/10.1007/s00204-016-1760-5
Ye X, Ji Z, Wei C et al (2013) Inhaled formaldehyde induces DNA–protein crosslinks and oxidative stress in bone marrow and other distant organs of exposed mice: formaldehyde inhalation induces distant toxicity in mice. Environ Mol Mutagen 54:705–718. https://doi.org/10.1002/em.21821
Zhang, L (2018) Formaldehyde: exposure, toxicity and health effects. R Soc Chem 37
Zhang L, Steinmaus C, Eastmond DA et al (2009) Formaldehyde exposure and leukemia: a new meta-analysis and potential mechanisms. Mutat Res/Rev Mutat Res 681:150–168. https://doi.org/10.1016/j.mrrev.2008.07.002
Zhang L, Freeman LEB, Nakamura J et al (2010a) Formaldehyde and leukemia: epidemiology, potential mechanisms, and implications for risk assessment. Environ Mol Mutagen 51:181–191. https://doi.org/10.1002/em.20534
Zhang L, Tang X, Rothman N et al (2010b) Occupational exposure to formaldehyde, hematotoxicity, and leukemia-specific chromosome changes in cultured myeloid progenitor cells. Cancer EpidemiolBiomarkPrev 19:80–88. https://doi.org/10.1158/1055-9965.EPI-09-0762
Zhang L, Prak L, Rayon-Estrada V et al (2013) ZFP36L2 is required for self-renewal of early burst-forming unit erythroid progenitors. Nature 499:92–96. https://doi.org/10.1038/nature12215
Zhang Y, Liu X, McHale C et al (2013) Bone marrow injury induced via oxidative stress in mice by inhalation exposure to formaldehyde. PLoS ONE 8:e74974. https://doi.org/10.1371/journal.pone.0074974
Acknowledgements
This project was partially supported by NIEHS Superfund research grant P42ES004705 and Chau Hoi Shuen Foundation Women in Science Program Award at University of California at Berkeley (L Zhang), as well as the National Key Research and Development Program of China (2017YFC0702700) (R Li). The content is solely the responsibility of the authors and does not necessarily represent the official views of NIEHS and other funding agencies. We thank Dr. Zhe Liu from University of California, San Francisco (UCSF) at Dr. Looney's lab for her valuable suggestions on the protocol of lung cell extraction. YZ is a recipient of the China Scholarship Council for a graduate fellowship to UC Berkeley for 2 years (201706770048).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All of the authors declare no potential competing financial interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhao, Y., Magaña, L.C., Cui, H. et al. Formaldehyde-induced hematopoietic stem and progenitor cell toxicity in mouse lung and nose. Arch Toxicol 95, 693–701 (2021). https://doi.org/10.1007/s00204-020-02932-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00204-020-02932-x